Abstract
Background:
Social disconnection is associated with all-cause mortality and suicide. Measures of social disconnection with reliable cut-off scores are needed to aid in the assessment of clinically significant change.
Aims:
The current study sought to identify reliable clinical cut-off scores for the 15-item Interpersonal Needs Questionnaire (INQ-15), which assesses two indices of social disconnection associated with suicide ideation – thwarted belonging (TB) and perceived burden (PB) on others.
Methods:
The INQ-15 and measures of suicide ideation were administered to psychiatric outpatients (Nsample1 = 493; Nsample2 = 213) and psychiatric inpatients (Nsample3 = 79; Nsample4 = 87).
Results:
Reliable cut-off scores discriminating between the presence and absence of suicide ideation were identified across samples (TB ≥ 36 for psychiatric outpatients and ≥ 32 for inpatients; PB ≥ 12 for both psychiatric outpatients and inpatients).
Limitations:
Data are cross-sectional; thus, conclusions cannot be made about the predictive utility of INQ scores for future suicide ideation, attempts, or death.
Conclusions:
The INQ-15 yields scores with reliable cut-off scores for both TB and PB that represent clinically significant levels of social disconnection. These cut-off scores can be used in treatment trials and clinical practice to assess clinical improvement (or decline) in belonging and perceived burden.
Keywords: thwarted belonging, perceived burden, clinical cut-off scores
Social disconnection is linked to a range of negative mental health outcomes across the lifespan (Beutel et al., 2017), including suicide ideation (Van Orden et al., 2008), attempts (You et al., 2011), and deaths (Tsai et al., 2014, 2015). Social disconnection can be characterized by objective dimensions (i.e., number of family and friends), as well as subjective dimensions (i.e., perceptions of connection/isolation; Holt-Lunstad et al., 2017). Although objective and subjective dimensions are important for health and well-being, subjective perceptions are especially relevant for psychiatric morbidity and mortality (Cornwell & Waite, 2009).
Two dimensions of social disconnection particularly relevant for the development of suicide ideation, according to the interpersonal theory of suicide (Joiner, 2005), are the subjective perception that one does not belong to positive and meaningful relationships (i.e., thwarted belonging) and that one is a burden on others (i.e., perceived burden). Indeed, the individual and joint presence of thwarted belonging and perceived burden has been associated with suicide ideation over and above other robust risk factors for ideation and behavior, including depressive symptoms (Chu et al., 2017). Accordingly, interventions targeting thwarted belonging and perceived burden hold special promise for suicide prevention.
Clinical trials testing connectedness interventions for suicide, however, are lacking (Szanto & Whitman, 2021). Randomized clinical trials (RCTs) are also often underpowered to detect statistically significant differences (p < .05; Moher et al., 1994), which impedes development of novel interventions. Indicators of clinical significance (e.g., percent scoring below a cut-off score/no longer meeting diagnostic criteria; Faulkner et al., 2008) can help detect potential signals of efficacy. Indicators of clinical significance for measures of social disconnection, particularly cut-off scores, are needed in the context of suicide prevention RCTs to advance the development and subsequent testing of novel interventions.
The Interpersonal Needs Questionnaire (INQ ; Van Orden et al., 2012) is a commonly used self-report measure of thwarted belonging and perceived burden. At present, studies identifying cut points on the INQ to indicate clinically significant levels of thwarted belonging and perceived burden, based on increased likelihood of suicide ideation, are inconsistent. Mitchell et al. (2017), examining two inpatient samples, proposed the following cut-off scores for the INQ-15 for perceived burden and thwarted belonging, respectively: 17 and 22 for distress due to ideation, 17 and 33 for desire for death, and 22 and 31 for desire for suicide. In a sample of psychiatric outpatients, Mitchell et al. (2020) suggested cut-off scores for perceived burden and thwarted belonging, respectively, of 19 and 35 for desire for death and 30 and 50 for desire for suicide. The association between perceived burden and desire for death was further moderated by gender (i.e., stronger association for men), with a perceived burden cut-off score of 17 suggested for women and 22 for men. Finally, among a nonpsychiatric sample of women with chronic physical illness, Brookings and Pederson (2019) suggested cut-off scores of 17 for perceived burden and 37 for thwarted belonging for suicide ideation (Brookings & Pederson, 2019).
Reliable cut points are needed to aid in selecting treatment targets and interpretation of changes over time, as well as guide decisions in designing RCTs that necessarily rely on binary choices, such as inclusion criteria for those with elevated levels of these constructs. The lack of convergence across studies regarding optimal cut-off scores for the INQ may be due to measurement limitations for suicide ideation (e.g., use of single items in Mitchell et al., 2017, 2020), differences in analytical decisions (criterion used to select cut-off scores), or actual population differences (clinical severity) that indicate a need for population-specific cut-off scores. The present study aimed to address these limitations by conducting ROC analyses across multiple samples that differed in clinical severity (two psychiatric outpatient samples and two psychiatric inpatient samples) and used a variety of measures of suicide ideation (including those with validated cut points for suicide ideation outcomes), while holding analytic methods constant and synthesizing findings. We also looked for convergence across sample characteristics and outcome measures within populations of clinical severity.
Methods
Study procedures were approved by university-affiliated institutional review boards for each sample. Participants completed all self-report measures at initial screening or intake for services. See Table 1 for sample severity characteristics.
Table 1.
Sample severity characteristics
| Current suicide ideation | Suicide attempt history | Depression | TBel | PBurd | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outpatient | Present | Absent | Missing | Present | Absent | Missing | M(SD) | M(SD) | M(SD) | |||
| Sample 1 (N = 493) | DSI-SS | 157 (31.8%) | 336 (68.2%) | 0 (0.0%) | BSS#20 | 100 (20.3%) | 391 (79.3%) | 2 (0.4%) | BDI-II | 18.63 (12.84) mild |
31.19 (14.09) range: 9–61 |
12.55 (8.09) range: 6–42 |
| BSS | 120 (24.3%) | 371 (75.3%) | 2 (0.4%) | |||||||||
| Sample 2 (N = 213) | BDI#9 | 88 (41.3%) | 114 (53.5%) | 11 (5.2%) | Clinical interview | 89 (41.8%) | 124 (58.2%) | 0 (0.0%) | BDI-II | 26.11 (13.31) moderate |
34.71 (13.14) range: 9–63 |
15.03 (9.59) range: 6–42 |
| Current suicide ideation | Admit reasona | Depression | TBel | PBurd | ||||||||
| Inpatient | Present | Absent | Missing | Attempt | Ideation | Neither | M(SD) | M(SD) | M(SD) | |||
| Sample 3 (N = 79) | DSI-SS | 38 (48.1%) | 38 (48.1%) | 3 (3.9%) | Clinical interview |
17 (21.5%) | 47 (59.5%) | 15 (19.0%) | PHQ-9 | 15.08 (7.40) moderately severe | 31.13 (12.71) range: 9–57 | 14.70 (8.87) range: 6–42 |
| Suicide attempt history | ||||||||||||
| Present |
Absent |
Missing |
||||||||||
| Sample 4 (N = 87) | BSS | 49 (56.3%) | 33 (37.9%) | 5 (5.7%) | BSS#20 | 47 (54.0%) | 38 (43.7%) | 2 (2.3%) | BDI-II | 19.86 (12.69) moderate |
33.34 (14.06) range: 9–63 |
14.75 (11.21) range: 6–42 |
Note. BDI-II = Beck Depression Inventory-II; BDI#9 = BDI-II Item 9; BSS = Beck Scale for Suicide Ideation (Items 1–19); BSS#20 = BSS Item 20; DSI-SS = Depressive Symptom inventory-Suicidality Subscale; PHQ-9 = Patient Health Questionnaire; TBel = thwarted belonging; PBurd = perceived burdensomeness. For sample 1, BDI-II respondents were n = 481. For Sample 2, BDI-II respondents were n = 201. For Sample 3, PHQ-9 respondents were n = 73. For Sample 4, BDI-II respondents were N = 87. aSuicide attempt history was not available for Sample 3.
Participants and Settings
Sample 1
The sample included 493 outpatients (58.4% female, 41.4% male, 0.2% not reported) seeking services at a university-affiliated community-based psychology clinic in the Southeastern United States. The mean age of the sample was 27.60 years (SD = 10.56; range: 18–64). Approximately, 71.6% identified as White (Non-Hispanic), 12.4% Black, 10.1% Hispanic, 2.0% Asian/Pacific Islander, and 1.4% American Indian/Alaskan Native and 2.4% not reported. The average Global Assessment of Functioning (GAF) score based on DSM-IV-TR was 65.12 (SD = 11.32; range: 31–91). The GAF scale represents a clinician’s judgment of an individual’s overall level of functioning at time of evaluation scored from 0 to 100, with higher scores indicating better functioning. The GAF scale is divided into 10 ranges of functioning, reflecting either symptom severity or level of functioning (psychological, social, occupational), whichever is worse. The current sample’s average GAF score was indicative of some mild symptoms or some difficulty in social, occupational, or school functioning.
Sample 2
The sample included 213 psychiatric outpatients (74.6% female, 25.4% male) seeking services through a University Department of Psychiatry outpatient clinic in New York City. The mean age of the sample was 36.76 (SD = 13.39; range: 18–64). Most of the sample (58.7%) identified as Hispanic, 23.9% as Black (Non-Hispanic), 9.4% as White (Non-Hispanic), 0.9% as Black Hispanic, and 7.0% as Other. The average GAF score was 52.80 (SD = 6.93; range: 25–70), indicating moderate symptoms or moderate difficulty in social, occupational, or school functioning.
Sample 3
The sample consisted of 79 adult psychiatric inpatients (51.9% female, 46.8% male) receiving services at a university-affiliated hospital in Western New York. Most (83.5%) identified as White, 10.1% Black/African-American, 2.5% American Indian/Alaska Native Asian, 1.3% Asian, and 1.3% Native Hawaiian/Other Pacific Islander. 1.3% of the overall sample identified their ethnicity as Hispanic/Latino. The mean age of the sample was 46.71 years (SD = 15.69; range: 18–79). GAF was not available for this sample.
Sample 4
The sample consisted of 87 adult psychiatric inpatients (60.9% female, 37.9% male, 1.1% other) receiving services at a psychiatric hospital in the Southeastern United States. Most identified as White (41.4%) or Black/African-American/Caribbean-American (47.1%), with 8.0% identifying as multiracial, 1.1% as Native Hawaiian/Pacific-Islander, 1.1% as American Indian, and 1.1% as Other. 8.0% of the overall sample identified their ethnicity as Hispanic/Latino. The mean age of the sample was 37.76 years (SD = 12.66; range: 18–68). GAF was not available for this sample.
Materials
Social Disconnection
Interpersonal Needs Questionnaire (INQ; Van Orden et al., 2012)
The INQ is a 15-item questionnaire consisting of two subscales: thwarted belonging (nine items) and perceived burden (six items). Participants rate how they have been feeling recently on a scale ranging from 1 (not at all true for me) to 7 (very true for me). Total scores range 7–63 for thwarted belonging and 6–42 for perceived burden. The INQ has demonstrated strong psychometric properties, including factorial validity, as well as construct validity, including a prospective association with suicide ideation. Participants in all four samples completed the INQ-15. Both subscales were significantly correlated with each other (r = .47–.65, p < .001) and displayed good-to-excellent internal consistency in all four samples (perceived burden α = .87–.94, thwarted belonging α = .84–.91).
Suicide Ideation
Suicide ideation was measured across the four samples using three different measures (i.e., Beck Depression Inventory-II [BDI-II] suicide item, Beck Scale for Suicide Ideation [BSS], Depressive Symptom Inventory-Suicidality Subscale [DSI-SS]; described below) as different sites used different measures in their clinical intake process. Suicide ideation ranges in severity from passive ideation (i.e., desire to be dead) to active ideation (i.e., desire to kill oneself). Although the BDI-II suicide item and the DSI-SS are thought to capture active suicide ideation, they have demonstrated good concurrent validity with the BSS (Gallyer et al., 2020; Green et al., 2015), which captures the full range.
Beck Depression Inventory-II (Beck et al., 1996)
The BDI-II is a measure of depressive symptom severity over the past 2 weeks that contains 21 groups of statements. Items are rated on a scale from 0 to 3. The BDI-II has been found to have high internal consistency and average test-retest reliability. BDI-II Item 9 (suicidal thoughts and wishes) was used to assess suicide ideation in Sample 2 as the criterion for ROC analyses. For use in analyses, BDI-II Item 9 total scores were coded dichotomously (i.e., ideation present vs. absent). Presence of suicide ideation was defined as a score of 1 or above, as previous research has found that a score ≥ 1 is associated with death by suicide (Green et al., 2015).
Beck Scale for Suicide Ideation (Beck & Steer, 1991)
The BSS consists of 19 groups of statements assessing the nature, frequency, and severity of suicide ideation in the past week. Participants rate each statement on a scale from 0 to 2. The BSS has displayed adequate internal consistency, high construct validity, and adequate test-retest reliability. Total scores were coded dichotomously (i.e., ideation present vs. absent) for analyses. Presence of suicide ideation was defined as a score ≥ 3, as previous research has found that a score ≥ 3 is associated with a seven-fold increased risk for death by suicide (Brown et al., 2000). Of note, this cut-off score may represent a conservative cut point. A different cut point on the BSS could lead to different cut-off scores on the INQ-15 subscales in these samples. The BSS was used in Sample 1 (α = .88) and Sample 4 (α = .91) as the criterion for ROC analyses.
Depressive Symptom Inventory-Suicidality Subscale (Metalsky & Joiner, 1997)
The DSI-SS is a 4-item self-report questionnaire that assesses the frequency and intensity of suicide ideation and impulses in the past 2 weeks. Scores range from 0 to 3 on each item. The DSI-SS has displayed good psychometric properties and construct validity. For use in analyses, DSI-SS total scores were coded dichotomously (i.e., ideation present vs. absent); the presence of suicide ideation was defined as a total score of 1 or above. Cut points have not been established for the DSI-SS; however, given that all DSI-SS items reflect active suicide ideation, we chose a lower cut point on this measure than the BSS (as a score ≥ 3 on the BSS could reflect only passive suicide ideation) to make these gold standards as comparable as possible for ROC analyses. The DSI-SS was used in Sample 1 (α = .91) and Sample 3 (α = .95) as the criterion for ROC analyses.
Data Analytic Strategy
ROC analysis was conducted for all four samples, and the area under the curve (AUC) for each test was examined (i.e., probability that the INQ subscales will produce a higher value for a randomly selected individual with suicide ideation than one without). For the INQ, missing data were handled using mean imputation for the respective missing item (note: there was no missing data for the INQ for Samples 1, 2, and 4; four participants in Sample 3 were missing data on one item). Participants with missing data on measures of suicide ideation were not included in ROC analyses. We calculated sensitivity (proportion of true positives identified as positive) and specificity (proportion of true negatives identified as negative) for each total score value of the INQ subscales, as well as simultaneous net sensitivity and specificity. For net sensitivity, a case is included in the numerator if identified as positive by either only one or both tests; for net specificity, a case is included in the numerator only if identified as negative by both tests. These metrics were chosen to illustrate how well subscale total scores performed individually and simultaneously with regards to identifying a clinically significant level of social disconnection (with suicide ideation as a criterion) rather than as a means of predicting/detecting suicide ideation as would be done in a clinical risk assessment.
In line with previous studies identifying cut-off scores for measures of depression and suicide ideation (e.g., Cukrowicz et al., 2011; von Glischinski et al., 2016), optimal cut points were identified as those that resulted in the smallest absolute difference between sensitivity and specificity. Although simultaneously maximizing sensitivity and specificity, this empirical method does not take into consideration the cost of a false negative (i.e., failing to detect ideation when present) compared to that of a false positive (i.e., identifying ideation when absent), for example, the cost of not receiving necessary medical attention versus delivering unnecessary medical intervention, respectively. For our purposes, we calculated the absolute difference to initially inform cut points for each sample and then took into consideration cut points that maximized sensitivity over specificity when making overall final recommendations.
Results
Sample 1
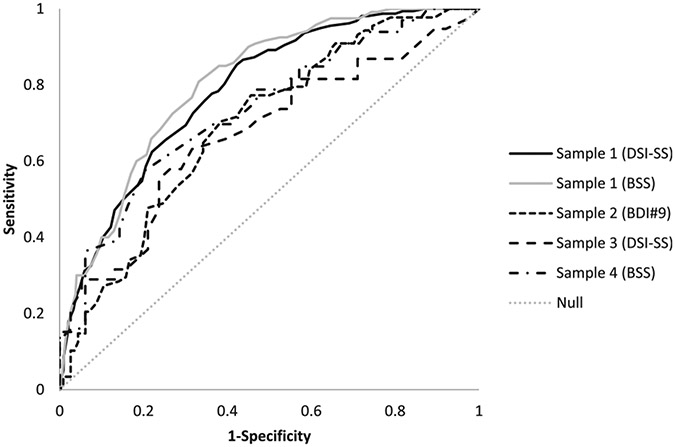
Thwarted belonging subscale scores discriminated between the presence and absence of suicide ideation on the DSI-SS (AUC = .79, p < .001) and a score of 3 or greater on the BSS (AUC = .80, p < .001) in a sample of psychiatric outpatients (see Table 2 and Figure 1). A value ≥ 36 maximized sensitivity and specificity for the DSI-SS (.69 & .70), whereas ≥ 37 was indicated for the BSS (.77 & .68). As a lower cut point would aid sensitivity (i.e., reduce false negatives), we chose the value of 36 instead of 37 for this sample.
Table 2.
Area under the curve (AUC), standard error (SE), p-value, and 95% confidence interval (CI)
| Sample | N | Thwarted belonging |
Perceived burden |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AUC | SE | p | 95% CI | AUC | SE | p | 95% CI | |||
| S1 | DSI-SS | 493 | .79 | .02 | <.001 | [.74–.83] | .826 | .019 | <.001 | [.79–.86] |
| BSS | 491 | .80 | .02 | <.001 | [.76–.85] | .840 | .020 | <.001 | [.80–.88] | |
| S2 | BDI#9 | 202 | .69 | .04 | <.001 | [.62–.77] | .675 | .038 | <.001 | [.60–.75] |
| S3 | DSI-SS | 76 | .67 | .06 | <.01 | [.55–.79] | .731 | .059 | <.001 | [.62–.85] |
| S4 | BSS | 82 | .73 | .06 | <.001 | [.62–.84] | .790 | .052 | <.001 | [.69–.89] |
Note. DSI-SS = Depressive Symptom Inventory-Suicidality Subscale; BSS = Beck Scale for Suicide Ideation; BDI#9 = Beck Depression Inventory-II Item 9.
Figure 1.
ROC curves for thwarted belonging.
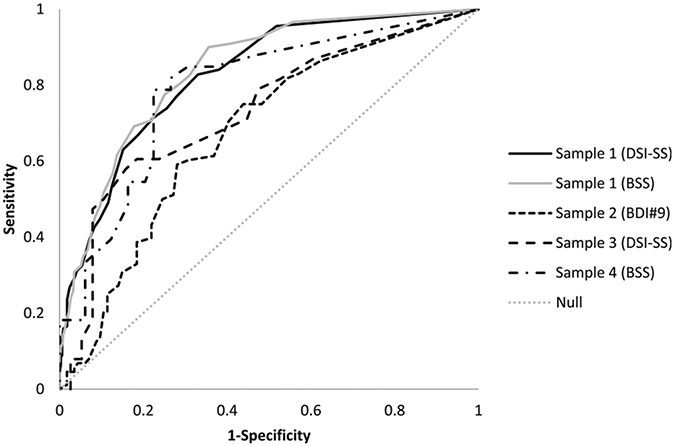
Perceived burden subscale scores also discriminated between the presence and absence of suicide ideation on the DSI-SS (AUC = .83, p < .001) and a score of 3 or greater on the BSS (AUC = .84, p < .001); see Table 2 and Figure 2. A value ≥ 12 maximized sensitivity and specificity for the DSI-SS (.74 and .74) whereas ≥ 13 was indicated for the BSS (.80 and .72). The value of 12 was selected to prioritize sensitivity.
Figure 2.
ROC curves for perceived burden.
The net sensitivity and specificity using the selected cut points for each subscale simultaneously were .92 and .52, respectively, with the DSI-SS and .95 and .49, respectively, with the BSS (see Table 3).
Table 3.
Optimal cut points with associated sensitivity and specificity
| Sample | Cut point | Sensitivity | Specificity | |
|---|---|---|---|---|
| Thwarted belonging | ||||
| S1 | DSI-SS | 36 | .69 | .70 |
| BSS | 36 | .77 | .68 | |
| S2 | BDI#9 | 37 | .65 | .66 |
| S3 | DSI-SS | 32 | .63 | .68 |
| S4 | BSS | 38 | .67 | .67 |
| Perceived burden | ||||
| S1 | DSI-SS | 12 | .74 | .74 |
| BSS | 12 | .80 | .72 | |
| S2 | BDI#9 | 13 | .61 | .63 |
| S3 | DSI-SS | 12 | .68 | .61 |
| S4 | BSS | 12 | .79 | .78 |
| Net sensitivity | Net specificity | |||
| S1 | DSI-SS | .92 | .52 | |
| BSS | .95 | .49 | ||
| S2 | BDI#9 | .86 | .42 | |
| S3 | DSI-SS | .88 | .41 | |
| S4 | BSS | .93 | .52 | |
Note. DSI-SS = Depressive Symptom Inventory-Suicidality Subscale; BSS = Beck Scale for Suicide Ideation; BDI#9 = Beck Depression Inventory-II Item 9.
Sample 2
Thwarted belonging (AUC = .69, p < .001) and perceived burden (AUC = .68, p < .001) subscale scores discriminated between the presence and absence of ideation on the BDI-II in a sample of relatively more psychiatrically ill outpatients (i.e., lower GAF scores compared to Sample 1); see Table 2, Figures 1 and 2. A value ≥ 37 on the thwarted belonging subscale maximized sensitivity (.65) and specificity (.66) for ideation. A value ≥ 13 on the perceived burden subscale maximized sensitivity (.61) and specificity (.63) for ideation. The net sensitivity and specificity using the selected sub-scale cut points simultaneously was .86 and .42, respectively (see Table 3).
Sample 3
Thwarted belonging (AUC = .67, p = .01) and perceived burden (AUC = .73, p = .001) subscale scores discriminated between the presence and absence of suicide ideation on the DSI-SS in a sample of psychiatric inpatients (see Table 2; Figures 1, 2). A value ≥ 32 on the thwarted belonging subscale maximized sensitivity (.63) and specificity (.68). A value ≥ 12 on the perceived burden subscale maximized sensitivity (.68) and specificity (.61). The net sensitivity and specificity using the selected subscale cut points simultaneously was .88 and .41, respectively (see Table 3).
Sample 4
Thwarted belonging (AUC = .73, p < .001) and perceived burden (AUC = .79, p < .001) subscale scores discriminated between the presence and absence of suicide ideation on the BSS in a sample of psychiatric inpatients (see Table 2; Figures 1, 2). A value ≥ 38 on the thwarted belonging subscale maximized sensitivity (.67) and specificity (.67). A value ≥ 12 on the perceived burden subscale maximized sensitivity (.79) and specificity (.78). The net sensitivity and specificity using the selected subscale cut points simultaneously was .93 and .52, respectively (see Table 3).
Recommended Cut-Off Scores
Based on the current study results across four different clinical samples, optimal cut-off scores for thwarted belonging converged from 36 to 37 for clinical outpatients and 32 to 38 for inpatients. The optimal cut-off scores for perceived burden were 12–13 for outpatients and was 12 among inpatients. It has been suggested that higher cut-off scores may be appropriate among less severe populations due to a lower prevalence of the condition of interest (Streiner & Cairney, 2007). Therefore, among outpatients, we recommend a cut-off score of 36 for thwarted belonging and 12 for perceived burden to indicate clinically significant levels of social disconnection. Among inpatients, a cut-off score of 32 for thwarted belonging and 12 for perceived burden is recommended. The use of both scales simultaneously increased the ability to identify clinically significant level social disconnection. As such, the simultaneous use of both subscales is recommended.
Discussion
In the present study, we sought to identify optimal cut-off scores for the INQ-15 that can be used in treatment settings or in suicide prevention studies to identify when clinically significant levels of thwarted belonging and perceived burden are present and/or when clinically significant change has occurred. The cut-off scores identified for the INQ are clinically significant as related to suicide ideation and are reliable across different clinical samples and with different measures of ideation.
The cut-off scores suggested here are notably lower, particularly for perceived burden, than those suggested by previous studies for active ideation (Brookings & Pederson, 2019; Mitchell et al., 2017, 2020). Compared to our samples, only the inpatient samples in Mitchell et al. (2017) were seemingly more symptomatic, as indicated by greater prevalence of attempts and higher means and SDs on the INQ subscales, especially for perceived burden. However, lower cut-off scores are actually more appropriate among more severe samples given a higher prevalence of the condition of interest (Streiner & Cairney, 2007).
Despite these discrepancies, we recommend the cut-off scores identified here for the INQ because of their consistency across different psychiatric samples. It is noteworthy, that even when using different measures of suicide ideation in the current study, clinical cut-off scores for the INQ were generally consistent across samples. Simultaneous use of the subscales also improved sensitivity, such that a respondent may be considered at a clinically significant level of social disconnection if at or above the cutoff on either one of the subscales.
Researchers and clinicians may, however, consider different cutoffs based on cost-benefit analyses for their specific context (e.g., Habibzadeh et al., 2016). In a context with a high cost to false diagnosis (e.g., involuntary hospitalization), a higher cut point might be chosen to maximize specificity (i.e., reduce false positives); when the cost of missing a diagnosis has high or potentially fatal consequence (e.g., death by suicide), a lower cut point may be chosen to maximize sensitivity (i.e., reduce false negatives). Research settings, for example, might prefer higher cut-off scores to reduce variability in their samples, whereas clinical settings might prefer lower cut-off scores and engaging in further assessment to minimize a false negative.
Limitations
The results should be considered in the context of study limitations. First, due to the smaller sample sizes among psychiatric inpatients, not all possible total scores on the INQ-15 were endorsed in those samples. Second, we used multiple measures of ideation, which resulted in slightly different cut points (even in the same sample). However, differences were minimal and unlikely to make a difference in the practical application of these cut points. Third, due to the cross-sectional nature of the study, conclusions cannot be made about the predictive utility of INQ scores for future suicide ideation, attempts, or death. Thus, the recommended cut-off scores on the INQ-15 cannot be used to predict future suicide ideation or behavior. Finally, we do not have information about INQ scores over time in response to treatment to provide information about what magnitude of change in scores reflects clinically meaningful improvement. Establishing clinically meaningful change (i.e., smallest degree of change which those with lived experience perceive as beneficial) is an important direction for future research, especially in understanding potential costs of false negatives or positives.
Conclusion
Overall, the current study provides scores on the INQ that can be used as indicators of clinically significant levels of thwarted belonging and perceived burden for suicide prevention and treatment studies seeking to measure social disconnection. Clinical cut-off scores for the INQ can be used to identify treatment targets (e.g., if a patient endorses clinical levels of either), inform treatment approaches, and measure changes in these targets over time. They can also guide decisions in designing and powering RCTs targeting social disconnection to reduce suicide by acting as markers for inclusion criteria or clinical significance (on top of or in lieu of statistical significance). Published RCTs of psychological therapies often focus on statistical significance but neglect clinical significance (Faulkner et al., 2008). Importantly, statistical significance does not guarantee clinical significance, and lack of statistical significance does not preclude potentially clinically significant effects. Establishing guidelines for clinical significance on dimensional measures of social disconnection is critical for identifying promising interventions in suicide prevention, particularly at the pilot stage.
Funding
This research was supported in part by grants from the National Institute of Mental Health (K23MH125078; K23MH096936; T32MH020061) and the National Center for Advancing Translational Sciences (KL2 TR001999).
Biographies
Caroline Silva, PhD, is a clinical psychologist and assistant professor in the Department of Psychiatry at the University of Rochester School of Medicine, NY, USA. Dr. Silva’s research is focused on integrating the interpersonal theory of suicide with cultural determinants of health to inform the development/evaluation of suicide prevention interventions for at-risk Hispanics.
Phillip Smith, PhD, is a clinical psychologist and professor in the Department of Psychology at the University of South Alabama, USA. Dr. Smith’s research interests center on the understanding and prevention of suicide and other forms of violence, particularly psychological and social risk processes within an individual’s cultural and social context.
Megan Rogers, PhD, is a clinical psychologist and assistant professor in the Department of Psychology at Texas State University, USA. Dr. Roger’s research primarily focuses on short-term cognitive, physiological, affective, and behavioral risk factors for suicidal thoughts and behaviors, with an emphasis on the phenomenology, etiology, and assessment of acute suicidal crises.
Thomas E. Joiner, PhD, is the Robert O. Lawton Distinguished Professor of Psychology in the Department of Psychology at the Florida State University, USA. Dr. Joiner’s research focuses primarily on the study of the nature, causes, and management of suicidal behavior and related disorders, including refining and testing the interpersonal theory of suicide.
Brad Foote, MD, is a psychiatrist in private practice in New York City, USA. Dr. Foote specializes in the treatment of dissociative identity disorders, as well as complex posttraumatic stress disorder and borderline personality disorder.
Kimberly A. Van Orden, PhD, is a clinical psychologist and associate professor in the Department of Psychiatry at the University of Rochester School of Medicine, NY, USA. Dr. Van Orden’s research is focused on developing and testing new interventions to promote social connectedness and reduce risk for suicide in late life.
Footnotes
Conflict of Interest
The authors have none to report.
Open Data
The data that support the findings of this study are available from the corresponding author on reasonable request.
References
- Beck AT, & Steer RA (1991). Manual for the beck scale for suicide ideation. Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation. [Google Scholar]
- Beutel ME, Klein EM, Brahler E, Reiner I, Junger C, Michal M, Wiltink J, Wild PS, Münzel T, Lackner KJ, & Tibubos AN (2017). Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry, 17(1), Article 97. 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookings JB, & Pederson CL (2019). INQ-15 cut-off scores for suicidal ideation screening of women with chronic, invisible illnesses. Clinical Psychology & Psychotherapy, 26(2), 273–275. 10.1002/cpp.2343 [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, & Grisham JR (2000). Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology, 68(3), 371–377. 10.1037/0022-006X.68.3.371 [DOI] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Stanley IH, Hom MA, Tucker RP, Hagan CR, Rogers ML, Podlogar MC, Chiurliza B, Ringer FB, Michaels MS, Patros CHG, & Joiner TE Jr. (2017). The interpersonal theory of suicide: A systematic review and meta-analysis of a decade of cross-national research. Psychological Bulletin, 143(12), 1313–1345. 10.1037/bul0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz KC, Schlegel EF, Smith PN, Jacobs MP, Van Orden KA, Paukert AL, Pettit JW, & Joiner TE Jr. (2011). Suicide ideation among college students evidencing subclinical depression. Journal of American College Health, 59(7), 575–581. 10.1080/07448481.2010.483710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner C, Fidler F, & Cumming G (2008). The value of RCT evidence depends on the quality of statistical analysis. Behaviour Research and Therapy, 46(2), 270–281. 10.1016/j.brat.2007.12.001 [DOI] [PubMed] [Google Scholar]
- Gallyer AJ, Chu C, Klein KM, Quintana J, Carlton C, Dougherty SP, & Joiner TE Jr. (2020). Routinized categorization of suicide risk into actionable strata: Establishing the validity of an existing suicide risk assessment framework in an outpatient sample. Journal of Clinical Psychology, 76(12), 2264–2282. 10.1002/jclp.22994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KL, Brown GK, Jager-Hyman S, Cha J, Steer RA, & Beck AT (2015). The predictive validity of the beck depression inventory suicide item. Journal of Clinical Psychiatry, 76(12), Article 15048. 10.4088/JCP.14m09391 [DOI] [PubMed] [Google Scholar]
- Habibzadeh F, Habibzadeh P, & Yadollahie M (2016). On determining the most appropriate test cut-off value: The case of tests with continuous results. Biochemia Medica, 26(3), 297–307. 10.11613/BM.2016.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, & Sbarra DA (2017). Advancing social connection as a public health priority in the United States. American Psychologist, 72(6), 517–530. 10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE Jr. (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Metalsky GI, & Joiner TE Jr. (1997). The Hopelessness depression symptom questionnaire. Cognitive Therapy and Research, 21(3), 359–384. 10.1023/A:1021882717784 [DOI] [Google Scholar]
- Mitchell SM, Brown SL, Roush JF, Bolanos AD, Littlefield AK, Marshall AJ, Jahn DR, Morgan RD, & Cukrowicz KC (2017). The clinical application of suicide risk assessment: A theory-driven approach. Clinical Psychology and Psychotherapy, 24(6), 1406–1420. 10.1002/cpp.2086 [DOI] [PubMed] [Google Scholar]
- Mitchell SM, Brown SL, Roush JF, Tucker RP, Cukrowicz KC, & Joiner TE Jr. (2020). The Interpersonal Needs Questionnaire: Statistical considerations for improved clinical application. Assessment, 27(3), 621–637. 10.1177/1073191118824660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Dulberg CS, & Wells GA (1994). Statistical power, sample size, and their reporting in randomized controlled trials. JAMA, 272(2), 122–124 [PubMed] [Google Scholar]
- Streiner DL, & Cairney J (2007). What’s under the ROC? An introduction to receiver operating characteristics curves. Canadian Journal of Psychiatry, 52(2), 121–128. 10.1177/070674370705200210 [DOI] [PubMed] [Google Scholar]
- Szanto K, & Whitman K (2021). Improving social connections to reduce suicide risk: A promising intervention target? American Journal of Geriatric Psychiatry, 29(8), 801–803. 10.1016/j.jagp.2021.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Lucas M, & Kawachi I (2015). Association between social integration and suicide among women in the United States. JAMA Psychiatry, 72(10), 987–993. 10.1001/jamapsychiatry.2015.1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Lucas M, Sania A, Kim D, & Kawachi I (2014). Social integration and suicide mortality among men: 24-year cohort study of U.S. health professionals. Annals of Internal Medicine, 161(2), 85–95. 10.7326/M13-1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, & Joiner TE Jr. (2012). Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychological Assessment, 24(1), 197–215. 10.1037/a0025358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, & Joiner TE Jr. (2008). Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology, 76(1), 72–83. 10.1037/0022-006X.76.1.72 [DOI] [PubMed] [Google Scholar]
- von Glischinski M, Teismann T, Prinz S, Gebauer JE, & Hirschfeld G (2016). Depressive symptom Inventory Suicidality subscale: Optimal cut points for clinical and non-clinical samples. Clinical Psychology & Psychotherapy, 23(6), 543–549. 10.1002/cpp.2007 [DOI] [PubMed] [Google Scholar]
- You S, Van Orden KA, & Conner KR (2011). Social connections and suicidal thoughts and behavior. Psychology of Addictive Behaviors, 25(1), 180–184. 10.1037/a0020936 [DOI] [PMC free article] [PubMed] [Google Scholar]