Abstract
Introduction
Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) is a rare congenital heart disease that usually presents with heart failure symptoms in infants. Without surgical correction, the condition has a high infant mortality rate. However, patients with ALCAPA can remain asymptomatic for decades in some cases, and the risk of sudden death decreases in adulthood.
Presentation of case
We present the case of a 52-year-old female who was incidentally diagnosed with ALCAPA during a routine medical evaluation. As the patient age, was asymptomatic, had good coronary collateral circulation, a medical treatment strategy was chosen and the patient was discharged in a good physical condition. And during the three-month follow-up, no cardiovascular complications were observed.
Discussion
The appearance and severity of symptoms in patients with ALCAPA can vary depending on factors such as the closure of the patent ductus arteriosus (PDA), pressure gradient between arteries, collateral development, and coronary anatomy. Surgical intervention is typically recommended, but in select cases such us, conservative management may be considered for elderly patients due to increased surgical risks and potentially lower risk of sudden cardiac death. Individualized patient assessment is crucial in determining the optimal treatment strategy for ALCAPA, considering the available evidence and limitations.
Conclusion
The management of asymptomatic patients with ALCAPA remains a subject of discussion, and further research is needed to standardize the clinical approach for this subgroup of patients and to compare survival rates between surgical correction and medical therapy.
Keywords: Case report, Coronary artery anomaly, ALCAPA, Anomalous origin of the left coronary artery from the pulmonary artery, Bland–White–Garland syndrome
1. Introduction
Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA; also called Bland–White–Garland syndrome) is a rare congenital coronary artery anomaly that affects 1 in 300,000 newborns and accounts for 0.5 % of all congenital heart diseases [1]. Patients with usually show clinical signs of heart failure at about the age of 3 months when their pulmonary artery (PA) pressure decreases [2]. Without surgical correction, approximately 90 % of children die within the first year of life [3,4]. It is very uncommon for the ALCAPA to be diagnosed in adulthood.
We present a case of an adult female with anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) incidentally detected during a routine medical evaluation. Our case underscores the potential for ALCAPA to remain asymptomatic for decades owing to efficient collateral circulation.
The Local Bioethics Committee approved this study and written informed consent was obtained from the patient for publication of this case report and accompanying images.
The work has been reported in line with the SCARE criteria [5].
2. Presentation of case
We present the case of a 52-year-old asymptomatic female who was referred to a cardiologist in November 2022 due to the identification of abnormal findings in her transthoracic echocardiography during a routine medical assessment. The imaging revealed a markedly dilated right coronary artery (Fig. 1a). The patient has an unremarkable medical history and does not have a past medical or surgical history: she was active in childhood. She has not reported any concerns or symptoms with regular physical activities. She did not have diabetes and did not have any past history of cardiac or lung disease. There were no congenital or genetic disorders in the family. She had four normal pregnancies and deliveries without any complications. Further tests, including echocardiography, computed tomography scan (CT), right-left heart catheterization and coronary angiography confirmed the presence of the coronary anomaly.
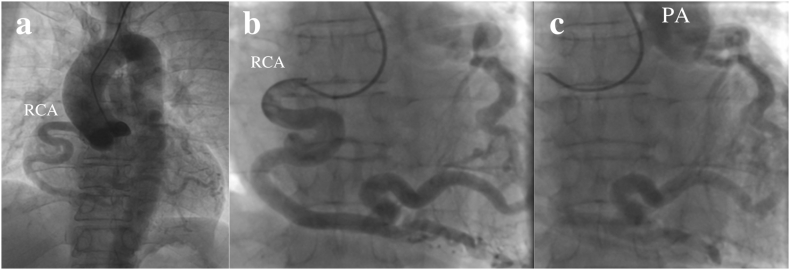
Fig. 2.
Rotational aortography and coronary angiography revealed an enlarged right coronary artery (RCA) with collaterals retrograde filling of the left anterior descending artery and main pulmonary artery (PA) (Fig. 2.
Fig. 3.
Computed tomography scan (CT): right coronary artery (RCA) and abnormal outflow of the left coronary artery (LCA) from main pulmonary artery (Fig. 3).
Fig. 1.
Transthoracic echocardiography revealed an enlarged right coronary artery (8 mm), left atrial dilation (Fig. 1a), and sub-endomyocardial fibrosis of the anterolateral papillary muscle (Fig. 1b). In addition, mild to moderate mitral regurgitation due to prolapse of the anterior leaflet of the mitral valve associated with chronic ischemia of the anterolateral wall of the left ventricle and anterolateral papillary muscle was observed (Fig. 1c, d).
Stress echocardiography examination demonstrated moderate exercise capacity, hypokinesis of the anteroseptal segments from the middle to apical portion of the left ventricle without angina symptoms.
Based on data obtained from cardiac catheterization, the following parameters were measured: the end-diastolic pressure in the left ventricle (EDP LV) 16 mmHg, the systemic vascular resistance - 12.6 Indexed Wood Units, the pulmonary vascular resistance - 0.7 Indexed Wood Units and the pulmonary artery mean pressure (PAPm) 18 mmHg. Oxygen saturation from the main pulmonary artery 81.1% and from the coronary sinus (CS) at 30.4 %. The calculated pulmonary-to-systemic blood flow ratio (Qp/Qs) was 1.6:1 indicating a significant left-to-right shunt.
Considering the patient had good coronary collateral circulation, thus it was unclear whether there would be any benefit from either surgical ligation of the LCA or re-implanting the anomalous artery. A thorough discussion was conducted with the patient regarding the available treatment options, during which all risks and potential outcomes associated with medical and surgical interventions were explained. The patient actively participated in the conversation and expressed a preference for conservative medical management. Therefore, a medical treatment strategy was chosen and the patient was discharged in a good physical condition with a follow-up. The discharge medications included bisoprolol extended release 5 mg o.d., perindopril release 4 mg o.d., spironolactone 25 mg o.d., dapagliflozine 10 mg o.d.
After three months of follow-up, the patient remains asymptomatic with good exercise tolerance. Further follow-up is planned in six months. Essential follow-up assessments consist of stress echocardiography, ECG, transthoracic echocardiography, and MRI, all of which play a crucial role in evaluating physical activity, functional class, and cardiovascular status.
3. Discussion
The appearance of symptoms after birth and the degree of myocardial dysfunction depends on various factors, such as the timing of the closure of the patent ductus arteriosus (PDA), the pressure gradient between the pulmonary and coronary arteries, and the development of collaterals, as well as the type of coronary anatomy [4,6]. ALCAPA patients are typically classified into two types based on the presence of collaterals: the adult type for those with well-established collaterals and the infantile type for those without collaterals. In some cases, such as the one we present, the existence of well-developed adult collateral circulation can mitigate the risk of adverse cardiovascular events in adulthood.
A comprehensive review conducted by JM Yau et al. on 151 adult patients from 1908 to 2008 demonstrated that minorities of patients (14 %) were asymptomatic, and the risk of sudden death decreased after the age of 50 years [4]. Surgery is recommended in patients with ALCAPA, even in the absence of symptoms or a significant left-to-right shunt syndrome, given the risk of ventricular arrhythmias and sudden death [8]. However, in elderly patients over 50 years of age, conservative management may be considered due to the elevated surgical risk, and evidence suggests a potentially lower risk of sudden cardiac death with this approach, as suggested by the authors [4,7]. Survival depends on factors such as the ratio of the left and right bypass, the development of collateral circulation, and the predominance of the right coronary artery. Medical treatment was chosen for our patient based on age, good collateral development and absence of symptoms.
Based on the available literature, our decision to choose medical treatment for this adult patient with ALCAPA is supported by findings suggesting favorable outcomes with conservative management in select cases. However, it is important to acknowledge the limitations of the available evidence and the need for individualized patient assessment in determining the optimal treatment strategy for ALCAPA.
4. Conclusions
ALCAPA is a rare congenital heart disease associated with high infant mortality. However, some adult patients may present with symptoms for the first time in adulthood. Our case report highlights the possibility that ALCAPA can remain undiagnosed for decades without symptoms. Despite the high incidence of sudden death in childhood and early adulthood, the risk appears to decreases with age even in cases with infrequent surgical intervention in this population. The management approach for ALCAPA in asymptomatic patients remains a subject of discussion, and the choice of intervention is based on individualized considerations and patient preference. Further data collection is necessary to inform the management of asymptomatic patients, and to standardize the clinical approach for this subgroup of patients, with a focus on comparing survival rates between surgical correction and medical therapy.
Ethical approval
This study was approved by the Local Bioethics Committee of National Research Cardiac Surgery Center 2023/029/CR from 17.02.2023 and informed consent was taken from the patient.
Sources of funding
None declared.
Author contribution
- the conception and design of data: Sandugash Talkhatova 1*, Marat Aripov (associate professor, PhD) 2, Abdurashid Mussaev (PhD) 3
- drafting the article or revising it critically for important intellectual content: Sandugash Talkhatova 1* Abdurashid Mussayev (PhD) 3
- final approval of the version to be submitted: Serik Alimbayev (PhD) 4, Erik Otarbayev 5 and Yuri Pya (Professor, PhD) 6
Guarantor
Sandugash Talkhatova 1*
Consent statement
Written informed consent was obtained from the patient(s).
Declaration of competing interest
The Author(s) declare(s) that there is no conflict of interest.
References
- 1.Pachon R., Bravo C., Niemiera M. Anomalous origin of the left coronary artery from pulmonary artery (ALCAPA) J. Clin. Exp. Cardiolog. 2014;5:1000341. [Google Scholar]
- 2.Gribaa R., Slim M., Ben Salem H., et al. Anomalous origin of the left coronary artery from the pulmonary artery presenting as dilated cardiomyopathy: a case report. J. Med. Case Rep. 2014;8:170. doi: 10.1186/1752-1947-8-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moodie D.S., Fyfe D., Gill C.C., CooK S.A., Lytle B.W., Taylor P.C., et al. Anomalous origin of the left coronary artery from the pulmonary artery (bland-white-Garland syndrome) in adult patients: long-term follow-up after surgery. Am. Heart J. 1983;106:381–388. doi: 10.1016/0002-8703(83)90207-7. [DOI] [PubMed] [Google Scholar]
- 4.Yau J.R., Singh R., Halpern E.J., Fischman D. Anomalous origin of the left coronary artery from the pulmonary artery in adults: a comprehensive review of 151 adult cases and a new diagnosis in a 53-year-old woman. Clin. Cardiol. 2011;34:204–210. doi: 10.1002/clc.20848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Barbetakis N, Efstathiou A, Efstathiou N, Papagiannopoulou P, Soulountsi V, Fessatidis I. A long-term survivor of Bland-White-Garland syndrome with systemic collateral supply: a case report and review of the literature. BMC Surg. 2005;5:23. doi: 10.1186/1471-2482-5-23. PMID: 16356181; PMCID: PMC1325261. [DOI] [PMC free article] [PubMed]
- 7.Eno-Martin L, Külliki K, Mehis M, Märt E. Late adult presentation of ALCAPA syndrome: need for a new clinical classification? A case report and literature overview, Eur. Heart J. Case Rep. 2020; 4/6: 1–5. https://doi.org/10.1093/ehjcr/ytaa318. [DOI] [PMC free article] [PubMed]
- 8.Alexi-Meskishvili V., Berger F., Weng Y., Lange P., Hetzer R. Anomalous origin of the left coronary artery from the pulmonary artery in adults. J. Card. Surg. 1995;10:309–315. doi: 10.1111/j.1540-8191.1995.tb00617.x. [DOI] [PubMed] [Google Scholar]