Abstract
Objectives. To assess the impacts of ambient temperature on hospitalizations of people experiencing homelessness.
Methods. We used daily time-series regression analysis employing distributed lag nonlinear models of 148 177 emergency inpatient admissions with “no fixed abode” and 20 804 admissions with a diagnosis of homelessness in London, United Kingdom, in 2011 through 2019.
Results. There was a significantly increased risk of hospitalization associated with high temperature; at 25°C versus the minimum morbidity temperature (MMT), relative risks were 1.359 (95% confidence interval [CI] = 1.216, 1.580) and 1.351 (95% CI = 1.039, 1.757) for admissions with “no fixed abode” and admissions with a homelessness diagnosis, respectively. Between 14.5% and 18.9% of admissions were attributable to temperatures above the MMT. No significant associations were observed with cold.
Conclusions. There is an elevated risk of hospitalization associated with even moderately high temperatures in individuals experiencing homelessness. Risks are larger than those reported in the general population.
Public Health Implications. Greater emphasis should be placed on addressing homeless vulnerabilities during hot weather rather than cold. Activation thresholds for interventions such as the Severe Weather Emergency Protocol (SWEP) could be better aligned with health risks. Given elevated risks at even moderate temperatures, our findings support prioritization of prevention-oriented measures, rather than crisis response, to address homelessness. (Am J Public Health. 2023;113(9):981–984. https://doi.org/10.2105/AJPH.2023.307351)
The impacts of climate change and extreme weather on the health of people who lack adequate shelter have received little attention.1 Homeless populations have specific health and social vulnerabilities that heighten risk of illness and death during severe weather. Climate change means that rough sleepers are exposed not only to severe winter weather but also increasingly higher ambient temperatures, particularly in heavily urbanized cities such as London, United Kingdom, where heat stress can be amplified because of the Urban Heat Island.2 Heat impacts are also intensified by risk factors common in rough sleepers and those with insecure housing, such as the presence of underlying physical and mental health conditions, drug and alcohol dependencies, reduced access to air-conditioned environments and drinking water, and social isolation.3
As the United Kingdom continues to experience greater climate extremes, there is an urgent need to assess the health impacts of ambient heat and cold exposure in homeless populations. People experiencing homelessness face barriers accessing primary health care, leading to higher rates of attendance at emergency departments. Health care costs for people experiencing homelessness are 8 times greater than for the general population and hospital stays are 3 times longer,4 so evidence-informed interventions can help ease burdens on the National Health Service (NHS).
We aimed to characterize the impacts of ambient temperature on emergency hospital admissions by people experiencing homelessness in Greater London, which hosts about 30% of the country’s homeless population. Given the heightened exposures and vulnerabilities of the homeless population, we hypothesized that adverse impacts occur at even moderate temperatures.
METHODS
We collected daily counts of emergency hospital inpatient admissions between 2011 and 2019 recorded on the Hospital Episode Statistics database by NHS Digital. We identified contacts by individuals experiencing homelessness using 2 fields: (1) all-cause admissions, where residential address was recorded as “no fixed abode” (pseudo postal district code ZZ99); (2) where a primary or secondary diagnosis of homelessness was recorded (International Classification of Diseases, 10th Revision [ICD-10], code Z59.0). Days with admission counts of 5 or fewer were not available to preserve patient anonymity and so were set to missing. We obtained daily maximum and minimum temperature data from the Met Office using the HadUK-Grid data set, which interpolates observations from land-surface monitoring stations onto a uniform 1-km grid.5 From this, we created composite temperature series representing the whole of London by averaging values from contributing grid cells.
We used Quasi–Poisson time-series regression to assess short-term associations between daily temperature (maximum or minimum) and hospital counts, adjusting for trends and underlying seasonal patterns (unrelated to temperature) using natural cubic splines with 7 degrees of freedom per year and indicator terms for day of week.6 The trend and seasonal controls ensure that temporal changes in the size of the population and other confounding factors that change slowly over time are inherently controlled for. We used distributed lag nonlinear models (DLNMs) employing cross-basis functions to flexibly model nonlinear and delayed effects of temperature.7 This framework allows quantification of risk at different values of the nonlinear temperature or lag distribution, as well as the summed effect. The model is summarized:
| (1) |
where E[Yi] is expected admissions on day i, Ti,j is the cross-basis matrix of temperature and lag j up to 21 days, ncs = natural cubic spline functions, and dow = day-of-week indicator. Although we considered lagged effects up to 21 days, heat impacts in particular are likely to be more immediate and so we also considered shorter lag structures in the DLNMs, but results were robust to such specifications.
For each field, we identified the minimum morbidity temperature (MMT) at which risk of admission is lowest, and estimated the relative risk (RR) of admission at selected temperatures compared with the MMT. We also quantified attributable fractions of temperatures above the MMT.
RESULTS
During 2011 to 2019, there was a minimum of 148 177 emergency inpatient admissions in London categorized as “no fixed abode” and 20 804 where the primary or secondary diagnosis was recorded as homelessness. Figure A (available as a supplement to the online version of this article at http://www.ajph.org) shows daily counts of admissions with “no fixed abode,” which generally exhibits yearly summertime peaks. The trend of increasing admissions mirrors general increases in hospitalization numbers,8 although the number of rough sleepers in London is also known to have increased during this period.9 The average daily counts for the “no fixed abode” and homelessness diagnosis variables were 45.9 and 10.2, respectively.
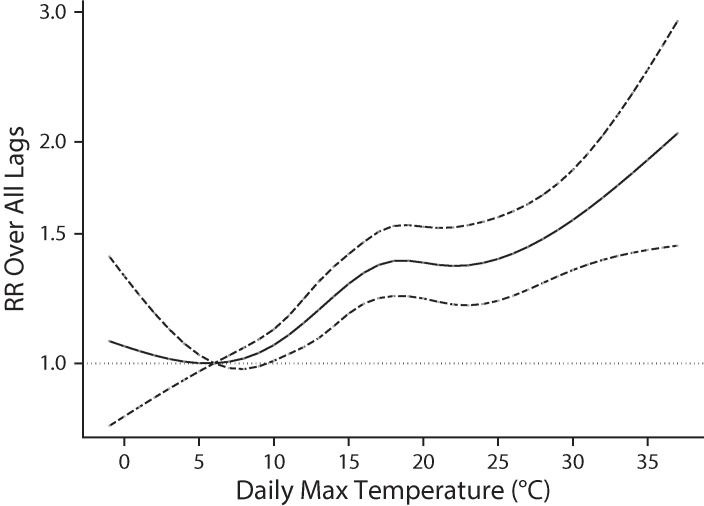
Figure 1 shows the seasonally adjusted relationship between daily maximum temperature and the relative risk of admission for those with “no fixed abode.” The figure shows increased risk of admission associated with high temperature. Compared with a MMT of 6°C, a value of 25°C (approximately the 93rd percentile) was associated with an RR of 1.359 (95% confidence interval [CI] = 1.216, 1.580). Temperatures above the MMT accounted for 18.9% of all admissions. We observed a similar relationship with the homelessness diagnosis outcome (not shown), with an RR of 1.351 (95% CI = 1.039, 1.757) at 25°C compared with a MMT of 9°C, and temperatures above the MMT accounting for 14.5% of admissions. Cold effects were not statistically significant, including when minimum temperature was the exposure.
FIGURE 1—
Seasonally Adjusted Relationship Between Daily Maximum Temperature (°C) and Relative Risk (RR) of Emergency Hospital Admissions Classified as “No Fixed Abode”: London, United Kingdom, 2011–2019
Note. The dashed lines indicate 95% confidence intervals.
DISCUSSION
Our results show that ambient heat is an important risk factor for emergency hospital admissions among people experiencing homelessness. Risks are greater than those recently reported for the general population of England using a similar methodology,10 reflecting heightened vulnerabilities for individuals experiencing homelessness. Likewise, US studies have shown particularly high odds of emergency department visits and deaths in homeless groups during hot weather.11,12 We observed no significantly raised risk associated with low temperatures, which agrees with evidence from emergency department attendances in North England.13 This may reflect better risk perception and preventative action taken by individuals experiencing homelessness and by homeless organizations during cold weather.
Admissions by individuals experiencing homelessness are likely to be underreported because a homelessness diagnosis is only recorded if a clinician considers it clinically relevant. Our reliance on this as a diagnosis had evident power limitations, so we also considered “no fixed abode” as an alternative indicator of homelessness, which is more numerous but less specific because it also captures people not experiencing homelessness who may wish to conceal their real address. The 2 outcomes, however, yielded very similar results. Days with 0 to 5 admission counts were unavailable, so their exclusion may have introduced bias; however, this applied to only 1.8% of days for “no fixed abode,” and results were largely unchanged when these days were assigned a nominal count of 3 for both outcomes in sensitivity analysis. Although we observed little cold effect, future research could consider potential impacts of other wintry weather such as snowfall and rainfall.
PUBLIC HEALTH IMPLICATIONS
Our study indicates that more emphasis should be placed on addressing homeless vulnerabilities during hot weather rather than cold. In England, the main recognition of climate vulnerabilities in the homeless population is through the Severe Weather Emergency Protocol (SWEP), which supports local authorities to issue an emergency response during extreme weather.14 Traditionally focused on cold weather, heat wave guidance is also now incorporated into SWEP, although our results indicate that the summertime SWEP activation threshold of 25°C maximum temperature is already associated with a 35% increased risk of hospitalization. Adverse health impacts occur at even moderate temperatures, and the high estimated heat-attributable fractions are mostly from moderate temperature days rather than the infrequent extreme temperature days when SWEP operates. Although SWEP is primarily an emergency response designed to provide overnight shelter for rough sleepers rather than engagement with health services, our results suggest that if it seeks to reach individuals experiencing homelessness before their health is compromised, existing activation thresholds may need to be revised. The elevated health risks observed in our study at even moderate temperatures support prioritization of prevention-oriented measures, rather than crisis response, to address homelessness.
ACKNOWLEDGMENTS
This study was partly funded by the National Institute for Health and Care Research (NIHR) Health Protection Research Unit in Environmental Change and Health (NIHR200909), a partnership between the London School of Hygiene & Tropical Medicine, the UK Health Security Agency, University College London, and the Met Office.
Note. The views expressed are those of the authors and not necessarily those of the NIHR, UK Health Security Agency, or the Department of Health and Social Care.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study did not involve human participants.
REFERENCES
- 1.Kidd SA, Hajat S, Bezgrebelna M, McKenzie K. The climate change–homelessness nexus. Lancet. 2021;397(10286):1693–1694. doi: 10.1016/S0140-6736(21)00834-5. [DOI] [PubMed] [Google Scholar]
- 2.Ramin B, Svoboda T. Health of the homeless and climate change. J Urban Health. 2009;86(4):654–664. doi: 10.1007/s11524-009-9354-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375(9717):856–863. doi: 10.1016/S0140-6736(09)61711-6. [DOI] [PubMed] [Google Scholar]
- 4.Thomas B. Homelessness Kills: An Analysis of the Mortality of Homeless People in Early Twenty-First Century England. London, UK: University of Sheffield and Crisis; 2012. [Google Scholar]
- 5.HadUK-Grid. https://www.metoffice.gov.uk/research/climate/maps-and-data/data/haduk-grid/haduk-grid
- 6.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187–1195. doi: 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology. 2006;17(6):624–631. doi: 10.1097/01.ede.0000239732.50999.8f. [DOI] [PubMed] [Google Scholar]
- 8.NHS England. 2020. https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity
- 9.Ministry of Housing, Communities and Local Government. 2020. https://www.gov.uk/government/statistics/rough-sleeping-snapshot-in-england-autumn-2019/rough-sleeping-snapshot-in-england-autumn-2019#annex-regional-maps
- 10.Rizmie D, de Preux L, Miraldo M, Atun R. Impact of extreme temperatures on emergency hospital admissions by age and socio-economic deprivation in England. Soc Sci Med. 2022;308:115193. doi: 10.1016/j.socscimed.2022.115193. [DOI] [PubMed] [Google Scholar]
- 11.Schwarz L, Castillo EM, Chan TC, et al. Heat waves and emergency department visits among the homeless, San Diego, 2012–2019. Am J Public Health. 2022;112(1):98–106. doi: 10.2105/AJPH.2021.306557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect. 2013;121(2):197–204. doi: 10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown AJ, Goodacre SW, Cross S. Do emergency department attendances by homeless people increase in cold weather? Emerg Med J. 2010;27(7):526–529. doi: 10.1136/emj.2009.076679. [DOI] [PubMed] [Google Scholar]
- 14.Severe Weather Emergency Protocol. 2022. https://homelesslink-1b54.kxcdn.com/media/documents/Severe_Weather_Emergency_Protocol_FAQs_February_2020_9KRmXPP.pdf