Abstract
Background:
The selection and description of participants in clinical trials enables health care providers to determine generalizability of findings to the populations they serve. Limited diversity of participants in trials restricts evidence-based decision-making.
Objectives:
To determine the extent to which diverse participants are being included in clinical trials of rehabilitation interventions for people with multiple sclerosis (MS).
Methods:
We conducted a scoping review of MS rehabilitation trials published since January 2002 using MEDLINE, CINAHL, and Web of Science. Covidence was used to facilitate the review. Article selection required randomized control design, a rehabilitation intervention, and a functional status outcome. Data extracted included details of intervention(s), outcomes, and participant selection and description using a social determinants of health framework.
Result:
A total of 243 studies were included. Exercise interventions and impairment-focused outcomes were most common. Most studies used only a MS Clinic for recruitment. Common exclusion criteria were physical or mental comorbidities, disability, age, and cognitive impairment. Participant age and sex were reported for almost all trials; reporting of other social determinants of health was atypical.
Conclusion:
MS rehabilitation trials have used limited recruitment methods, restricted samples, and reported few participant descriptors. Changes are required to enhance participant diversity and the descriptions of participant characteristics.
Keywords: Rehabilitation, health equity, diversity, equity, inclusion, review, social determinants of health, patient selection, selection bias
Introduction
Rehabilitation is a critical component of comprehensive multiple sclerosis (MS) care 1 and of health systems overall. 2 By definition, rehabilitation focuses on optimizing functioning by targeting a person’s capacity and/or the physical, social, and attitudinal factors in the environment that impact their abilities and opportunities to perform everyday activities.3,4 To optimize functioning, rehabilitation providers must consider the contextual factors that influence the daily lives of people with MS (e.g. life stage, income, education, living situation, employment, community features) during assessment, goal setting, intervention selection, and outcome evaluation. 5 These contextual factors mirror social determinants of health (SDoH), which have been described as the non-medical factors that influence health outcomes and contribute to systematic differences in health status across groups (i.e. health inequity). 6
In addition to context, rehabilitation providers must also consider the availability and generalizability of research evidence during the MS rehabilitation process. 7 Rehabilitation providers use research evidence to guide the selection, application, and evaluation of specific rehabilitation approaches for an individual client, given their functional problems and contextual situation. The extent to which evidence can be used confidently to guide clinical practice depends, in part, on the information provided in published studies. Information about the selection and description of research participants is particularly important. 8 If research participants lack the diversity of individuals seen in clinical practice or if their context is inadequately described in published studies, it is difficult for rehabilitation providers to determine whether interventions and their findings can be applied to their own clients.7 –9
One of the goals of a 2-day workshop hosted by the International Advisory Committee on Clinical Trials in MS in December 2022 was to discuss strategies to enhance diversity of clinical trial populations and review implications for study design, recruitment, and cultural safety. 10 This scoping review was conducted to inform these discussions. We applied a SDoH lens to ask the following questions: To what extent do MS rehabilitation researchers include people from diverse backgrounds in their clinical trials? What strategies are being used to recruit participants into MS rehabilitation trials? Who is being excluded, explicitly or implicitly, from these trials? What participant characteristics are being reported in trial findings? Our overall goals were to summarize the extent to which the diversity of people with MS has been addressed in rehabilitation trials over the past 20 years and to reflect on strategies that could be applied in future rehabilitation trials to support equity and diversity in both research and clinical decision-making.
Methods
This scoping review was guided by the Arksey and O’Malley 11 framework. Since PROSPERO does not include scoping review protocols, no protocol was registered for this review.
Search strategy
We searched OVID MEDLINE, CINAHL, and Web of Science to capture research literature in the health sciences. After consulting with a librarian, we used keyword and index or subject heading terms to identify articles that included the following key concepts: multiple sclerosis, rehabilitation (including terms for physical therapy, occupational therapy, exercise, cognitive rehabilitation, vocational rehabilitation, symptom management, self-management), and randomized controlled trials (RCTs; including terms for clinical trials, comparative study, evaluation study). Full search details are available from the corresponding author upon request. Searches were limited to articles published over the past 20 years, starting January 2002. No other search filters were used. The last search was conducted on 13 May 2022. Results were imported into Covidence (https://www.covidence.org/) to facilitate screening, full-text review, and extraction.
Screening for inclusion
Two phases of screening were performed: title and abstract, followed by full text. All authors were involved in both screening phases, with two reviewers independently examining each article in each phase. Initial screening identified studies that summarized primary research using an RCT design of any rehabilitation intervention that included persons with MS. Eligible studies had at least one functional outcome, as described by the International Classification of Functioning, Disability and Health (ICF). 5 Citations were excluded if the abstract was not available in English, the publication source was a patient magazine (e.g. MS Momentum), or if the citation was for a dissertation, letter to the editor, a conference abstract, a case report, a psychometric study, or a meta-analysis, systematic, scoping, or narrative review. Animal research was excluded as were trials of dietary interventions and combination interventions that included a pharmaceutical product.
During full-text review, initial screening criteria were reapplied. In addition, studies that included people with MS but did not report results of people with MS separately from other populations were excluded. Studies reporting only the qualitative evaluations of an RCT were excluded. When reviewers disagreed about the inclusion status of a citation, the third reviewer examined the citation and a three-way discussion was held until consensus was reached.
Data extraction and analysis
All authors contributed to data extraction using the Covidence 2.0 customizable template. The template was developed by the first author and included journal, publication time period, study purpose, country, intervention details (e.g. setting, focus, method of delivery, number of groups, number of sessions, comparator(s), primary outcome), details of participant recruitment (e.g. number recruited, methods, explicit and implicit eligibility criteria), and participant descriptors, with a focus on SDoH. The first and second authors piloted the template, which led to the inclusion of “not reported” options for several items, as well as adding examples to some item definitions to enhance consistency and ease of use. Dual extraction was completed on the first 140 articles to ensure consistency. No formal measures of agreement were used because differences in capitalization and punctuation generated messages of inconsistency even if the critical content was the same between extractors. The remaining articles were extracted by a single author and checked by another one to ensure that all extraction categories were complete. We did not conduct quality appraisals because our focus was on synthesis of descriptive features of studies, not on synthesis of actual study results.
Completed extractions were exported from Covidence and then imported into Microsoft Excel for data review, checking, and cleaning. The final dataset was imported into SPSS version 28.0.0.1 to facilitate descriptive analysis and data synthesis, focusing on when and where rehabilitation trials have been conducted, the focus and characteristics of trials, participant recruitment methods, who is being explicitly or implicitly excluded, and how participants are being described. Bivariate analyses (Fisher’s exact text) explored whether there were associations between trial characteristics and (a) recruitment methods, (b) exclusion criteria, and (c) reporting of participant descriptors. No statistical adjustment was done for multiple testing.
Results
Selection of sources of evidence
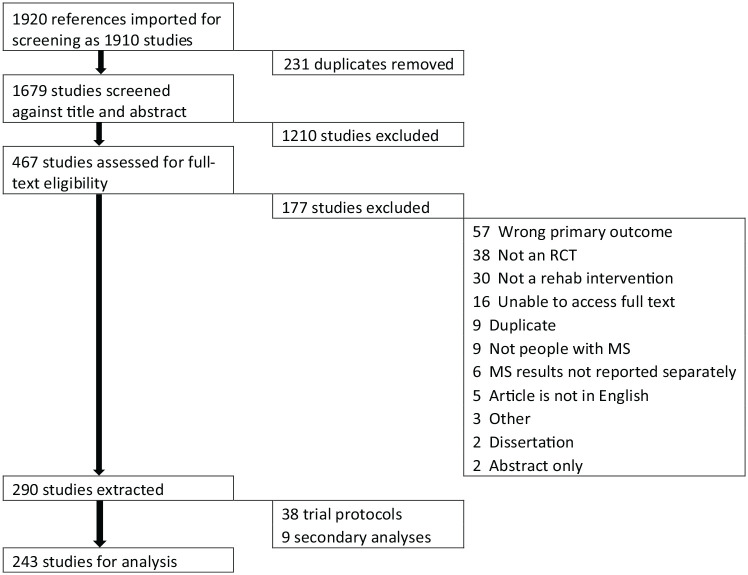
A total of 1920 citations were identified in the search process (see Figure 1). A total of 231 duplicates were removed by Covidence. A total of 1679 citations were screened (titles and abstracts), 1210 were deemed irrelevant, and 467 moved to full-text review. A total of 177 studies were excluded at the full-text review stage, most often because none of the outcomes reflected functioning (n = 57), the study was not an RCT (n = 31), or the intervention was not one typically provided by a rehabilitation professional (n = 26). Two hundred and ninety articles were included in data extraction. Of these papers, 38 were trial protocols and 9 were secondary analyses of trial data. These articles were not included in the final analyses to reduce the risk of double-counting information from an individual study, leaving a total of 243.
Figure 1.
PRISMA chart for search and selection of articles for the scoping review.
Characteristics of sources of evidence
Supplementary file 1 summarizes the key characteristics of the 243 included studies. Studies were conducted across 30 different countries, with 3 (1.2%) involving multi-country investigations. Findings were published in 88 different journals, 55 of which contained only a single article. The three most common journals in which rehabilitation trials were published included Multiple Sclerosis Journal (n = 36; 14.8%), Clinical Rehabilitation (n = 26; 10.7%), and Archives of Physical Medicine and Rehabilitation (n = 18, 7.4%). There has been a steady increase in the number of MS rehabilitation trials published over time, from 21 between 2002 and 2006, to 126 between 2017 and 2022.
Focus, features, and outcomes of MS rehabilitation trials
Exercise interventions were the most common (n = 132; 54.3%), followed by self-management/behavior change (n = 46, 18.9%), cognitive (re)training (n = 36, 14.8%), neurorehabilitative (n = 21, 8.6%), and mixed (n = 8, 3.35). Sample sizes ranged from 8 to 449, with a mean of 65 (SD = 63), with the average sample size being the largest in the self-management trials (mean = 114, SD = 80) and smallest in the neurorehabilitative trials (mean = 40, SD = 28). Trials were most often conducted in clinical settings (n = 79; 32.5%), offered in an individual format (n = 122; 50.2%), delivered face-to-face (n = 164, 67.5%), and included more than 12 intervention sessions (n = 142, 58.4%). Most studies randomized participants into two groups (n = 206, 84.8%), with the comparator condition most often being an alternative intervention (e.g. different dose, different delivery format) (n = 71, 29.2%) or usual care (n = 66, 27.2%). Across all studies, the primary outcome was most often a measure of impairment (n = 158, 65.0%), as per the ICF. Examples included measures of symptom severity (e.g. fatigue, pain, spasticity), physical assessments (e.g. balance, cardiorespiratory function, spatio-temporal measures of gait), and cognitive tests (e.g. word association, attention, memory). Among activity outcomes (n = 58, 23.9%), measures of walking and mobility were most common (e.g. timed 25-foot walk, 6-minute walk, timed up and go).
Recruitment methods
Twenty-two studies (9.1%) did not report recruitment method. When methods were reported (n = 221), recruitment was most often achieved through a single approach (n = 144; 65.1%), and most often through a MS clinic (122/144; 84.7%), followed by an MS organization (19/144; 13.2%). The most methods used in a study was 5, with only three studies employing this number of methods. The use of single versus multiple methods of recruitment was associated with the setting of the intervention (p < 0.001) but not with the focus of the intervention. Trials conducted in clinical settings were most likely to use a single method of recruitment, whereas those offered in mixed settings were most likely to use two or more methods.
Participant selection criteria
Across all studies, 15,787 people with MS participated. Two studies did not report exclusion criteria (Table 1). For the remaining studies, the most common reasons for exclusion were presence of physical comorbidities (n = 184; 75.7%), disability level (n = 179; 73.7%), age (n = 148; 60.9%), cognitive impairment (n = 100; 41.1%), and mental health comorbidities (n = 97; 40.0%). While less common, participants were also excluded for language, literacy, or education level (n = 54; 22.2%) or lack of access to technology (n = 16; 6.6%). Exclusion criteria were associated with the focus of the intervention (see final column of Table 1), with exercise interventions most likely to exclude for disability level, whereas cognitive interventions were most likely to exclude for age, mental health comorbidities, and language, literacy, or education level. Self-management interventions were most likely to exclude for lack of access to technology.
Table 1.
Explicit exclusion criteria in MS rehabilitation trials since January 2002, by intervention focus.
| Exclusion criteria reported | All intervention types combined (N = 243) | Exercise a (n = 132) | Self-management b (n = 46) | Cognitive (re) training c (n = 36) | Neuro-rehabilitation d (n = 21) | Mixed (n = 8) | Fisher’s exact test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | Count | % | Count | % | Count | % | p-value | |
| Other physical health conditions | 184 | 75.7% | 105 | 79.5% | 25 | 54.3% | 30 | 83.3% | 18 | 85.7% | 6 | 75.0% | 0.005 |
| Disability level | 179 | 73.7% | 116 | 87.9% | 25 | 54.3% | 14 | 38.9% | 16 | 76.2% | 8 | 100.0% | < 0.001 |
| Age | 148 | 60.9% | 77 | 58.3% | 32 | 69.6% | 27 | 75.0% | 8 | 38.1% | 4 | 50.0% | 0.042 |
| Cognitive impairment | 100 | 41.2% | 47 | 35.6% | 18 | 39.1% | 21 | 58.3% | 9 | 42.9% | 5 | 62.5% | 0.104 |
| Mental health conditions | 97 | 39.9% | 34 | 25.8% | 26 | 56.5% | 30 | 83.3% | 4 | 19.0% | 3 | 37.5% | < 0.001 |
| Other reasons (e.g. BMI, medications, activity level, other interventions received) | 76 | 31.3% | 43 | 32.6% | 12 | 26.1% | 11 | 30.6% | 8 | 38.1% | 2 | 25.0% | 0.873 |
| Language, literacy, or educational level | 54 | 22.2% | 13 | 9.8% | 16 | 34.8% | 21 | 58.3% | 2 | 9.5% | 2 | 25.0% | <0.001 |
| Lack of access to technology (e.g. cell phone, Internet, computer) | 16 | 6.6% | 3 | 2.3% | 9 | 19.6% | 2 | 5.6% | 2 | 9.5% | 0 | 0.0% | 0.003 |
| Distance/geography | 11 | 4.5% | 6 | 4.5% | 4 | 8.7% | 1 | 2.8% | 0 | 0.0% | 0 | 0.0% | 0.638 |
| Exclusion criteria not reported | 2 | 0.8% | 2 | 1.5% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 1.000 |
MS: multiple sclerosis; BMI: body mass index.
Includes general exercise, gait, balance, yoga, and stretching.
Includes behavior change and patient education.
Includes compensatory or remedial training.
Includes transcranial stimulation, functional electrical stimulation, sensory modalities, and task-specific training.
In addition to these explicit exclusion criteria, several trial features may have further restricted the study samples. For example, 200 trials (82.3%) required in-person attendance for assessment or intervention, which may have implicitly excluded some prospective participants. In addition, there was no evidence in 215 (88.5%) of the studies that participants were provided with reimbursement for study costs (e.g. parking, childcare, time off work). In 213 studies (88.0%), there was no evidence that the trial was offered to or accommodated individuals in rural or remote communities.
Participant description
The most common participant descriptors reported across the trials were age (n = 238; 97.9%) and biological sex (n = 226; 93.0%). The next most common characteristics were education (n = 74; 30.5%) and employment status (n = 46, 18.9%). All other SDoH characteristics were reported in less than 10% of studies (Table 2), with no studies reporting on gender identity and only one study reporting on community type. Self-management interventions were most likely to report employment status, race and/or ethnicity, living arrangements, and income, whereas cognitive interventions were most likely to report education (see final column of Table 2).
Table 2.
Participant descriptors reported in MS rehabilitation trials since January 2002, by intervention focus.
| Participant descriptors | All intervention types combined (N = 243) | Exercise a (n = 132) | Self-management b (n = 46) | Cognitive (re) training c (n = 36) | Neuro-rehabilitation d (n = 21) | Mixed (n = 8) | Fisher’s exact test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | Count | % | Count | % | Count | % | p-value | |
| Age | 238 | 97.9% | 129 | 97.7% | 45 | 97.8% | 36 | 100.0% | 20 | 95.2% | 8 | 100.0% | 0.705 |
| Biological sex | 226 | 93.0% | 123 | 93.2% | 44 | 95.7% | 34 | 94.4% | 17 | 81.0% | 8 | 100.0% | 0.306 |
| Education | 74 | 30.5% | 18 | 13.6% | 24 | 52.2% | 30 | 83.3% | 1 | 4.8% | 1 | 12.5% | < 0.001 |
| Employment status | 46 | 18.9% | 12 | 9.1% | 23 | 50.0% | 9 | 25.0% | 1 | 4.8% | 1 | 12.5% | < 0.001 |
| Race and/or ethnicity | 24 | 9.9% | 3 | 2.3% | 15 | 32.6% | 6 | 16.7% | 0 | 0.0% | 0 | 0.0% | < 0.001 |
| Living arrangements | 19 | 7.8% | 1 | 0.8% | 13 | 28.3% | 4 | 11.1% | 1 | 4.8% | 0 | 0.0% | < 0.001 |
| Income | 8 | 3.3% | 1 | 0.8% | 7 | 15.2% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0.001 |
| Type of community (size, or rural/urban) | 1 | 0.4% | 0 | 0.0% | 1 | 2.2% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0.457 |
MS: multiple sclerosis.
Includes general exercise, gait, balance, yoga, and stretching.
Includes behavior change and patient education.
Includes compensatory or remedial training.
Includes transcranial stimulation, functional electrical stimulation, sensory modalities, and task-specific training.
Discussion
The overarching goal of MS rehabilitation is to optimize functioning, considering the contexts in which individuals carry out daily activities. In order for rehabilitation providers to confidently select contextually relevant interventions for their patients using available trial evidence, they must carefully consider how MS rehabilitation trials have recruited, selected, and described their study participants. This scoping review has illustrated that MS rehabilitation trials published over the past 20 years have used limited recruitment methods, restricted samples, and reported very few details about participants that would aid providers in their clinical decision-making. These knowledge gaps have implications for moving evidence into practice, rehabilitation service delivery and outcomes, and opportunities to support the reduction of health inequities through the rehabilitation process. 12 The findings from this review add a rehabilitation dimension to the existing literature regarding the lack of participant diversity and inclusion in MS trials.6,10,13,14
The MS rehabilitation trials included in this review depended heavily on MS Clinics and MS organizations to recruit participants. Using these approaches does increase confidence that the individuals recruited meet necessary diagnostic criteria. Yet, research from the United States has shown that there is not equitable access to MS specialty services and to other supportive care14 –16 across racial and ethnic groups. This means that depending on these recruitment approaches will negatively impact participant diversity. Literature shows that recruiting diverse individuals into clinical trials requires multi-pronged, non-traditional approaches such as geo-marketing, partnerships with non-specialist community providers, community engagement with local agencies, and meaningful involvement of patient partners in the research process.17 –20 There is existing evidence that these strategies are effective, both for the development of MS registries 21 and MS exercise trials. 22
Recently, guidelines for health research recruitment materials targeting African Americans and Latinos were developed and piloted in the United States. 23 Findings indicated the importance of tailored messages that address socio-cultural (e.g. beliefs and values), linguistic preferences, and motivations for participation. Application and evaluation of these guidelines in MS rehabilitation research, and MS trials in general, may enhance participant diversity in MS research. Application of these guidelines may aid researchers in better understanding the perceived culturally safety of various MS rehabilitation interventions, which could lead to important modifications and additional intervention development. Ultimately, going beyond the traditional participant recruitment methods will require researchers and funders to find ways to account for the additional time and costs associated with recruiting diverse participants.
Recruiting diverse participants for MS rehabilitation trials will also require (re)consideration of inclusion and exclusion criteria, both explicitly identified ones and those that are implicit given the practical demands of trial participation (e.g. attendance schedules, reimbursements/incentives). Participation criteria must consider issues of ethics, safety and potential confounders, 24 and where the study falls in the pragmatic-explanatory continuum. 25 The findings from this review suggest that participant criteria—both explicit and implicit—may be restricting diversity of MS rehabilitation trials, yet the lack of description of participants beyond age and sex may be masking important diversity information (e.g. education, income, living situation, language). Therefore, addressing inadequate description of participants and how they are supported to engage in trials is necessary before any critique of inclusion/exclusion criteria can be levied.
Inadequate participant description in rehabilitation trials has been previously identified as a methodological issue that requires attention. 26 The Cochrane Equity Group has published a CONSORT extension for better reporting of health equity in randomized trials, 27 which includes items related to reporting relevant baseline characteristics using the PROGRESS plus framework. 28 To meaningfully use these tools in MS rehabilitation trials, discussions are needed to determine which equity issues are most relevant to support the translation of research into practice. Marrie et al. 10 have proposed that minimal equity descriptors for MS trials should include sex, gender, race and ethnicity, education, and place of residence. MS rehabilitation trialists need to consider if other equity descriptors are needed given our focus on functioning.
Despite the knowledge gained through this scoping review, it is not without limitations. Although a librarian was consulted about the search, the search was conducted by the first author. In addition, only three databases were used, none of which have a focus on social sciences, which could have resulted in missing trials focused on social functioning interventions, and those with a focus on work and educational functioning. Out of necessity, we focused on English language articles, which is a limitation. Nevertheless, the studies included were conducted in 30 different countries, many of which are not English-speaking. Finally, although attempts were made to merge studies in Covidence that were reporting on the same trial, it is possible that some were missed and therefore some double-counting is possible.
Conclusion
Unfavorable SDoH contribute to health inequities by restricting health-related choices, access to health care, and making it more difficult to engage in the rehabilitation process. 12 The findings of this scoping review indicate that, moving forward, there are multiple opportunities to improve participant diversity and inclusion in MS rehabilitation trials over the past 20 years. Trialists need to explicitly leverage what is already known about recruiting diverse participants into rehabilitation trials, and publish what is learned about which strategies work and which do not for different intervention types and in different settings. Trialists also need to report on known equity-relevant characteristics of study participants, and to the extent possible, leverage these data to inform strategies to facilitate equitable access to research participation and, ultimately, to evidence-based rehabilitation services for all people with MS.
Supplemental Material
Supplemental material, sj-docx-1-msj-10.1177_13524585231189670 for Participant diversity in clinical trials of rehabilitation interventions for people with multiple sclerosis: A scoping review by Marcia Finlayson, Leyan Al-Mashita and Rebekah Sandhu in Multiple Sclerosis Journal
Acknowledgments
The authors extend thanks to The International Advisory Committee on Clinical Trials in Multiple Sclerosis and the International Conference on Innovations in Clinical Trial Design & Enhancing Inclusivity of Clinical Trial Populations for the invitation to present this work. The Committee and the Conference were supported by the National Multiple Sclerosis Society and the European Committee for Treatment and Research in Multiple Sclerosis. There was no involvement of the meeting sponsors in the design, collection, analysis, or interpretation of contents of this paper.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.F. is an investigator on projects funded by Multiple Sclerosis Canada, the Patient-Centered Outcomes Research Institute, the University Hospitals Kingston Foundation, and the National Multiple Sclerosis Society. She has received consulting or teaching honoraria from Novartis and Biogen. L.A.-M. and R.S. have no disclosures.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Open access was made possible by the participation of Queen’s University in the Canadian Research Knowledge Network.
ORCID iD: Marcia Finlayson  https://orcid.org/0000-0002-1774-4810
https://orcid.org/0000-0002-1774-4810
Supplemental Material: Supplemental material for this article is available online.
Contributor Information
Marcia Finlayson, School of Rehabilitation Therapy, Faculty of Health Sciences, Queen’s University, Kingston, ON, Canada.
Leyan Al-Mashita, Health Sciences Program, Faculty of Health Sciences, Queen’s University, Kingston, ON, Canada.
Rebekah Sandhu, Aging and Health Program, School of Rehabilitation Therapy, Faculty of Health Sciences, Queen’s University, Kingston, ON, Canada.
References
- 1. National Institute of Health and Care Excellence. Multiple sclerosis in adults: Management. NICE guideline 220. London: National Institute of Health and Care Excellence, 2022. [PubMed] [Google Scholar]
- 2. Gimigliano F, Negrini S. The World Health Organization “rehabilitation 2030: A call to action.” Eur J Phys Rehab Med 2017; 53: 155–168. [DOI] [PubMed] [Google Scholar]
- 3. Negrini S, Selb M, Kiekens C, et al. Rehabilitation definition for research purposes. A global stakeholders’ initiative by Cochrane rehabilitation. Eur J Phys Rehabil Med 2022; 58: 333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stucki G, Bickenbach J. Functioning: The third health indicator in the health system and the key indicator for rehabilitation. Eur J Phys Rehabil Med 2017; 53(1): 134–138. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. Towards a common language for functioning, disability and health (ICF), 2002, https://www.who.int/publications/m/item/icf-beginner-s-guide-towards-a-common-language-for-functioning-disability-and-health
- 6. Dobson R, Rice DR, D’hooghe M, et al. Social determinants of health in multiple sclerosis. Nat Rev Neurol 2022; 18: 723–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Novak I, Te Velde A, Hines A, et al. Rehabilitation evidence-based decision-making: The READ model. Front Rehabil Sci 2021; 2: 726410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murad MH, Katabi A, Benkhadra R, et al. External validity, generalisability, applicability and directness: A brief primer. BMJ Evid Based Med 2018; 23(1): 17–19. [DOI] [PubMed] [Google Scholar]
- 9. Paci M, Faedda G, Ugolini A, et al. Barriers to evidence-based practice implementation in physiotherapy: A systematic review and meta-analysis. Int J Qual Health Care 2021; 33: mzab093. [DOI] [PubMed] [Google Scholar]
- 10. Marrie R, Chataway J, Amezcua L, et al. Enhancing diversity of clinical trial populations in multiple sclerosis. Mult Scler J 2023; 29(9): 1174–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 12. Frier A, Barnett F, Devine S. The relationship between social determinants of health, and rehabilitation of neurological conditions: A systematic literature review. Disabil Rehabil 2017; 39(10): 941–948. [DOI] [PubMed] [Google Scholar]
- 13. Onuorah H-M, Charron O, Meltzer E, et al. Enrollment of non-white participants and reporting of race and ethnicity in phase III trials of multiple sclerosis DMTs: A systematic review. Neurology 2022; 98: e880–e892. [DOI] [PubMed] [Google Scholar]
- 14. Amezcua L, Rivera VM, Vazquez TC, et al. Health disparities, inequities, and social determinants of health in multiple sclerosis and related disorders in the US. JAMA Neurol 2021; 78: 1515. [DOI] [PubMed] [Google Scholar]
- 15. Saadi A, Himmelstein DU, Woolhandler S, et al. Racial disparities in neurologic health care access and utilization in the United States. Neurology 2017; 88: 2268–2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fabius CD, Thomas KS, Zhang T, et al. Racial disparities in Medicaid home and community-based service utilization and expenditures among persons with multiple sclerosis. BMC Health Serv Res 2018; 18: 773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dobkin RD, Amondikar N, Kopil C, et al. Innovative recruitment strategies to increase diversity of participation in Parkinson’s disease research: The fox insight cohort experience. J Parkinsons Dis 2020; 10(2): 665–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gorelick PB. Community engagement: Lessons learned from the AAASPS and SDBA. Stroke 2022; 53(3): 654–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reuland M, Sloan D, Antonsdottir IM, et al. Recruitment of a diverse research cohort in a large metropolitan area for dementia intervention studies. Contemp Clin Trials 2022; 112: 106622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vaswani PA, Tropea TF, Dahodwala N. Overcoming barriers to Parkinson disease trial participation: Increasing diversity and novel designs for recruitment and retention. Neurotherapeutics 2020; 17(4): 1724–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Puhan MA, Steinemann N, Kamm CP, et al. A digitally facilitated citizen-science driven approach accelerates participant recruitment and increases study population diversity. Swiss Med Wkly 2018; 148: w14623. [DOI] [PubMed] [Google Scholar]
- 22. Tracy TF, Young H-J, Lai B, et al. Supporting successful recruitment in a randomized control trial comparing clinic and home-based exercise among adults with multiple sclerosis. Res Involv Engagem 2022; 8: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cunningham-Erves J, Kusnoor SV, Villalta-Gil V, et al. Development and pilot implementation of guidelines for culturally tailored research recruitment materials for African Americans and Latinos. BMC Med Res Methodol 2022; 22: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Portney LG. Foundations of clinical research: Applications to evidence-based practice. 4th ed. New York: F. A. Davis Company, 2020. [Google Scholar]
- 25. Loudon K, Treweek S, Sullivan F, et al. The PRECIS-2 tool: Designing trials that are fit for purpose. BMJ 2015; 350: h2147. [DOI] [PubMed] [Google Scholar]
- 26. Arienti C, Armijo-Olivo S, Minozzi S, et al. Methodological issues in rehabilitation research: A scoping review. Arch Phys Med Rehabil 2021; 102(8): 1614–1622.e14. [DOI] [PubMed] [Google Scholar]
- 27. Welch VA, Norheim OF, Jull J, et al. CONSORT-Equity 2017 extension and elaboration for better reporting of health equity in randomised trials. BMJ (Clin Res Ed) 2018; 359: j5085. [DOI] [PubMed] [Google Scholar]
- 28. O’Neill J, Tabish H, Welch V, et al. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014; 67(1): 56–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-msj-10.1177_13524585231189670 for Participant diversity in clinical trials of rehabilitation interventions for people with multiple sclerosis: A scoping review by Marcia Finlayson, Leyan Al-Mashita and Rebekah Sandhu in Multiple Sclerosis Journal