Abstract
Comorbidity is highly prevalent in people with multiple sclerosis (MS) throughout their disease course. In the last 15 years, our understanding of the association between comorbidity and outcomes such as relapses, disability progressive, health-related quality of life, health care use, and mortality has grown substantially. The broad adverse impacts of comorbidity on these outcomes point to the need to prevent and treat comorbidity effectively in people with MS. This requires having the necessary tools to evaluate comorbidity, an understanding of how MS affects management of comorbidity now, testing of interventions tailored to people with MS, and determining the best models of care to optimize comorbidity management.
Keywords: Multiple sclerosis, epidemiology
Introduction
Multiple sclerosis (MS) is a chronic disease of the central nervous system with protean manifestations. From a clinical perspective, initial presentation and outcomes such as relapse rates and disability progress are heterogeneous. Our understanding of the factors that contribute to that heterogeneity continues to grow, among them genetic factors, social determinants of health, ethnicity, race, and health behaviors (Figure 1).1–3 Comorbidity has received increasing attention because it is common and potentially modifiable.
Figure 1.
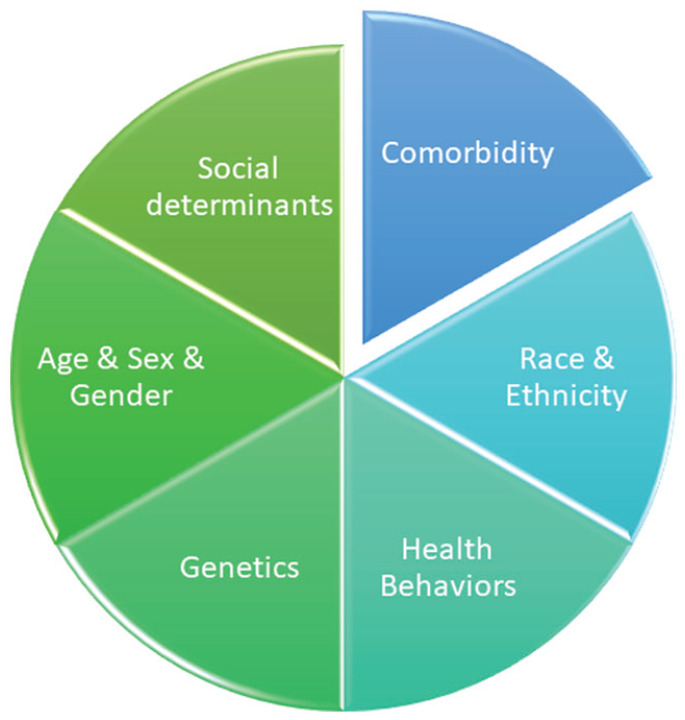
Factors that may account for heterogeneity of clinical presentation and outcomes in multiple sclerosis.
Herein, comorbidity refers to the total burden of illness other than the disease of interest. In the general population, chronic disease is common. The 2016–2019 Medical Expenditure Panel Survey reported that 52.6% of Americans had one or more chronic conditions, 32.9% had two or more, and 20.7% had three or more. 4 The prevalence rose with age such that 88.4% of those aged 65 years and older had multiple chronic conditions. The most common combination was hypertension and hyperlipidemia. In the general population, comorbidity is associated with a broad range of adverse health outcomes including increased physical impairment, reduced functional status, reduced quality of life, increased health care utilization, and increased mortality. A growing body of literature suggests that comorbidity similarly affects people with MS.5–8 Multiple potential benefits may be derived from studying comorbidity including improved understanding of variability in outcomes and better prognostication, novel insights into the etiology and pathophysiology of MS, and identification of novel interventions targeting comorbidity.
Studying comorbidity requires a means of measuring it. Potential data sources include administrative (health claims) databases, medical records, and self-report. Notably, the validity of the data sources varies depending on the comorbidity being evaluated. For example, administrative data are often population-based in universal health systems, are accessible, and highly cost-efficient as compared to primary data collection. However, they are not collected for research purposes, and data elements need to be validated. Several studies, particularly in Canada, have developed and tested case definitions for various comorbidities that perform well in the MS population, but there are comorbidities for which high-performing case definitions are not available.9,10 Although the optimal case definition for a condition may vary across health systems, these findings demonstrate that it is feasible to use administrative data to study comorbidity in MS. Medical records data may provide more clinical information to support the accuracy of diagnosis of a comorbidity, as well as treatment information, but data extraction may be costly and labor-intensive. Self-report data are more accessible and less costly than medical records data, but the validity of self-reported comorbidities varies by comorbidity; 11 well-defined chronic conditions that require ongoing care, such as diabetes, are accurately reported. In people with MS there is moderate to high agreement between self-report and medical records for hypertension, diabetes, hyperlipidemia, heart disease, thyroid disease, and chronic lung disease. 12 Depending on the question being answered, the optimal measurement approach for comorbidity will vary.
There are several key areas to consider related to comorbidity in people with MS, including which comorbidities occur, how often they occur, who is most at risk of those comorbidities (i.e., risk factors), and how those comorbidities affect outcomes in MS.
Which comorbidities affect people with MS and how often do they occur?
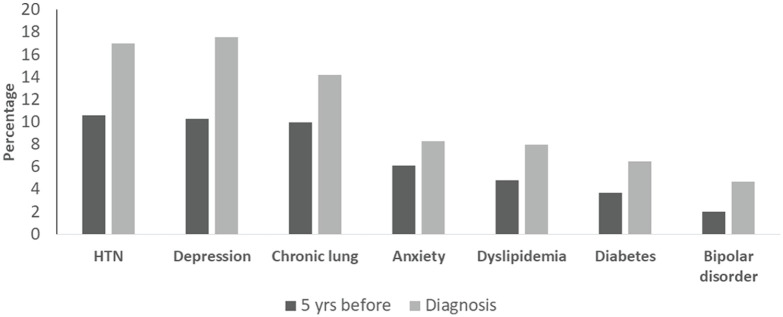
In 2015, a systematic review of the world literature concluded that the most prevalent comorbidities among people with MS were depression (23.7%), anxiety (21.9%), hypertension (18.6%), hyperlipidemia (10.9%), and chronic lung disease (10.0%), although wide variability in estimates between studies was observed. 13 In a Canadian population-based study, hypertension, hyperlipidemia, chronic lung disease, depression, and anxiety were the most common comorbidities at the time of MS diagnosis (Figure 2). 14 Before the diagnosis of MS, people with MS are more likely to have uveitis, inflammatory bowel disease, bullous pemphigoid, as well as depression, anxiety, bipolar disorder, schizophrenia, hypertension, hyperlipidemia, diabetes, ischemic heart disease, fibromyalgia, chronic lung disease, and epilepsy.14,15
Figure 2.
Percentage of people with MS who have comorbidity at the time of diagnosis and 5 years earlier*.
*Adapted from Ref. 14
HTN = hypertension; MS = multiple sclerosis.
Who is at risk?
Several factors are associated with an increased incidence or prevalence of comorbidity among people with MS, including sociodemographic characteristics, adverse childhood experiences, and genetic factors, among others. For example, the incidence and prevalence of many comorbidities, including hypertension, hyperlipidemia, diabetes, heart disease, stroke, chronic lung disease, and psoriasis increase with age.16–18 In contrast, the incidence and prevalence of depression and anxiety disorders have less consistent associations with age. 19 As compared to men, women with MS have an increased incidence of depression, anxiety and bipolar disorder. 19 Women also have an increased incidence of cardiovascular disease, cerebrovascular disease and psoriasis.8,16
As compared to long-term residents, immigrants to Ontario, Canada have an increased prevalence of comorbidity at the time MS is diagnosed, including mood/anxiety disorders, schizophrenia, diabetes, hypertension, ischemic heart disease, chronic lung disease, migraine, epilepsy, inflammatory bowel disease, and rheumatoid arthritis. 20
Lower socioeconomic status is associated with an increased incidence and prevalence of psychiatric comorbidities including depression, anxiety, bipolar disorder, and schizophrenia. 21 It is also associated with an increased incidence and prevalence of physical comorbidities. Similarly, urban rather than rural residence is associated with an increased incidence of psychiatric and physical comorbidities. 21 Childhood maltreatment, specifically emotional abuse, is associated with increased odds of having a comorbid psychiatric disorder as identified based on structured psychiatric interview (odds ratio (OR) 2.24; 1.58–3.16). 22 Health behaviors, such as smoking, are associated with increased odds of depression and anxiety. 23
Findings regarding the association of genetic factors and comorbidity are also emerging. A Mendelian randomization study reported that obesity is a causal risk factor for depression in MS; obesity also confers an increased risk of MS. 24 In a cohort of individuals with MS, inflammatory bowel disease and rheumatoid arthritis, a polygenic score for obesity was associated with increased odds of having persistently elevated symptoms of depression for 3 years. 25 Understanding who is at risk for depression and other comorbidities provides the opportunity to target specific individuals for preventive interventions. 26
Notably, bidirectional relationships exist between psychiatric and physical comorbidities. In the North American Research Committee on Multiple Sclerosis (NARCOMS) registry after accounting for age, sex, race, income, region, and marital status, reporting any physical comorbidity was associated with a two-fold increased risk of being diagnosed with depression (hazard ratio (HR) 2.20; 2.04–2.38) after MS onset. 27 Using population-based administrative (health claims) data, an increasing number of physical comorbidities is associated with an increased incidence of depression, anxiety disorder, and bipolar disorder in a dose-response relationship. 28
How do comorbidities affect outcomes in MS?
The adverse effects of comorbidity on MS are broad and include effects on relapse rates, progression of physical and cognitive impairments, imaging findings, health care utilization, health-related quality of life and mortality.3,8,29–31 The presence of multiple comorbidities is associated with an increased relapse rate. 29 Hyperlipidemia, in particular, has been associated with increased relapse rates. 29 In an analysis of the CombiRx clinical trial, dyslipidemia was associated with a 32% increase in relapse rate. 29 In that analysis, anxiety was also associated with an increased relapse rate of 25%.
In a cross-sectional study of 111 participants with MS, diabetes was associated with lower performance on tests of visual member and verbal fluency, while anxiety was associated with lower performance on tests of processing speed. 30 Similarly, a retrospective study found that having two or more vascular comorbidities (any of hypertension, diabetes, hyperlipidemia) was associated with lower performance on an IPAD-based test of processing speed. 6 In a 3-year longitudinal study, elevations of depressive symptoms within an individual participant over time were associated with declines in performance on a measure of processing speed, the Symbol Digit Modalities Test. 32 It remains uncertain whether the effects of comorbidities on cognition in MS differ from those observed in the general population, or whether effectively managing comorbidities could improve cognitive performance in MS.
A dose–response relationship exists between the number of physical comorbidities and the rate of disability progression. 31 In a Canadian study using linked clinical and administrative data for 3166 individuals with MS, each additional physical comorbidity was associated with a 0.18 increase in the Expanded Disability Status Scale (EDSS) score annually. 31 A similarly designed study using data for 2312 individuals with MS, found that having a mood/anxiety disorder was associated with a 0.28 increase in the EDSS score annually, after accounting for physical comorbidity. 7 Studies in other regions have also found that comorbidities are associated with greater disability progression. 33
Comorbidity is associated with higher rates of hospitalization, annual physician visits, and prescription drug use.34,35 For example, having a mood or anxiety disorder is associated with an increased prevalence of opioid use (prevalence ratio 1.22; 1.17–1.27) and longer duration of use, 36 than not having a mood or anxiety disorder. The presence of comorbidity is also associated with a lower likelihood of initiating disease-modifying therapy, and lower persistence on therapy.37,38 The influence of comorbidity on the effectiveness of disease-modifying therapy is not well-understood.
Comorbidity is also associated with increased mortality. Notably, the effects of depression and MS are synergistic, such that 14% of deaths may be attributed to the joint effects of these conditions. 8
Collectively, these findings indicate that comorbidity has a clinically meaningful adverse impact on multiple outcomes in MS. The question that follows this observation is whether preventing or treating comorbidity more effectively can improve outcomes.
“Would you tell me, please, which way I ought to go from here?”
“That depends a good deal on where you want to get to”
Lewis Caroll, Alice in Wonderland
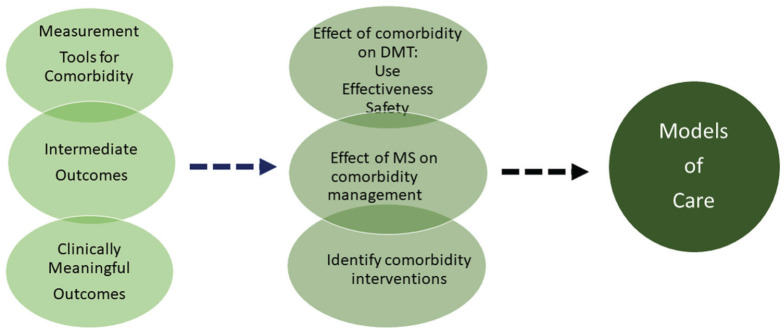
Realizing comorbidity as a viable treatment target
Several steps will be needed to realize comorbidity as a viable treatment target to improve outcomes in MS (Figure 3). First, we need appropriate tools to detect or risk-stratify comorbidity. Second, we need to understand how MS may influence the diagnosis and management of comorbidity so that we know where to start. Third, we need to identify appropriate intermediate and clinically meaningful outcomes for clinical trials. Fourth, we need to consider delivery of the comorbidity interventions—who, how, where—will they be delivered? Finally, we need to determine what the interventions should be.
Figure 3.
Realizing comorbidity-related interventions as viable targets for multiple sclerosis.
Tools
Identifying easy to use, valid, and reliable screening tools is needed to support the implementation of screening depression and anxiety in appropriate at-risk groups. Theoretically, screening tools developed in the general population may not perform well in people with MS due to overlap between somatic symptoms of depression such as fatigue, which is a common symptom of MS; the situation is similar for anxiety. However, as compared to a semi-structured psychiatric interview, multiple scales have good psychometric properties in MS, and these properties do not differ substantially between scales (Table 1). 39 For the busy clinician, single items “I felt depressed,” and “I felt like I needed help for my anxiety” perform nearly as well as scales with multiple items. 40
Table 1.
Test characteristics for previously defined cut-points for depression and anxiety screening measures.
| Instrument | Cutpoint⩾ | Sens | Spec | PPV | NPV | Internal consistency (Cronbach’s alpha) | Test–retest Intraclass correlation coefficient |
|---|---|---|---|---|---|---|---|
| Depression | |||||||
| PHQ-2 | 3 | 0.68 | 0.86 | 0.35 | 0.96 | 0.80 | 0.86 |
| PHQ-9 | 10 | 0.84 | 0.76 | 0.29 | 0.97 | 0.87 | 0.85 |
| PHQ-9 | 12 | 0.80 | 0.84 | 0.36 | 0.97 | – | – |
| PHQ-9 | 7 | 0.76 | 0.76 | 0.27 | 0.96 | – | – |
| HADS-D | 8 | 0.69 | 0.81 | 0.30 | 0.96 | 0.82 | 0.83 |
| HADS-D | 11 | 0.31 | 0.95 | 0.40 | 0.92 | – | – |
| PROMIS-D | T score 57.7 | 0.85 | 0.78 | 0.31 | 0.98 | 0.95 | 0.85 |
| PROMIS-D D | T score 60 | 0.69 | 0.85 | 0.35 | 0.96 | – | – |
| Kessler-6 | 15 | 0.81 | 0.80 | 0.32 | 0.97 | ||
| Kessler-6 | 19 | 0.31 | 0.94 | 0.36 | 0.92 | 0.87 | 0.87 |
| Anxiety | |||||||
| GAD-7 | 7 | 0.91 | 0.72 | 0.13 | 0.99 | ||
| GAD-7 | 10 | 0.54 | 0.83 | 0.13 | 0.97 | 0.92 | 0.76 |
| OASIS | 8 | 0.73 | 0.81 | 0.15 | 0.98 | 0.90 | 0.73 |
| HADS-A | 8 | 0.82 | 0.68 | 0.10 | 0.99 | 0.86 | 0.83 |
| HADS-A | 9 | 0.82 | 0.59 | 0.08 | 0.99 | – | – |
| HADS-A | 11 | 0.64 | 0.86 | 0.18 | 0.98 | – | – |
| PROMIS Anxiety | T score 60 | 0.73 | 0.83 | 0.16 | 0.98 | 0.95 | 0.79 |
| PROMIS Anxiety | T score 54.3 | 0.82 | 0.62 | 0.09 | 0.99 | – | – |
Sens: sensitivity; spec: specificity; PPV: positive predictive value; NPV: negative predictive value; PHQ-2: Patient Health Questionnaire-2; PHQ-9: Patient Health Questionnaire-9; GAD-7: Generalized Anxiety Disorder-7; OASIS: Overall Anxiety and Severity Impairment Scale; HADS-D: Hospital Anxiety and Depression Scale—depression score; HADS-A: Hospital Anxiety and Depression Scale—anxiety score; PROMIS-D: Patient Reported Outcomes Measurement Information System- Depression 8a; PROMIS-A: PROMIS-Anxiety 8a.
Some tools that guide clinical decision-making and initiation of interventions may need to be modified for use in people with MS. For example, the Fracture Risk Assessment Tool estimates 10-year risk of osteoporotic fracture. It underestimates the risk in people with MS, 41 potentially leading to underuse of interventions for osteoporosis. However, it can be readily recalibrated by treating MS as a secondary cause of osteoporosis, as is done for rheumatoid arthritis. 41 These issues may apply to other commonly used clinical tools for comorbidity.
Comorbidity management
In the general population, comorbidity has inconsistent effects on the management of other chronic conditions. 42 The presence of concordant (related) conditions can lead to better management of the comorbidity, whereas the presence of discordant (unrelated) conditions can have the opposite effect. Although the problem of underdiagnosis of depression appears to be improving, undertreatment remains an ongoing concern. 43 The evidence regarding the management of comorbidity, other than depression and anxiety, in people with MS is relatively limited. One study using electronic medical records data from the Canadian Primary Care Sentinel Surveillance Network found that people with MS had a similar likelihood of achieving guideline-indicated treatment targets for hypertension and diabetes as people without MS. 44 However, findings have differed for other comorbidities. Acute myocardial infarction (AMI) is an acute condition for which most affected individuals will present to hospital for care, and for which there are specific, detailed guidelines regarding investigations and management. A matched retrospective cohort study conducted in two Canadian provinces compared management of incident AMI in people with and without MS of the same, age, region and with onset of the AMI in the same calendar year. Notably, people with MS were less likely to undergo cardiac catheterization within 30 days of hospitalization (OR 0.61; 0.49–0.77) and had a longer time to revascularization (HR 0.78; 0.69–0.88). They were less likely to fill a prescription for beta-blockers, high dose statins, an ace inhibitor/angiotensin receptor blocker, or dual anti-platelet therapy, 45 although persistence to therapy at 1 year and adherence among treated individuals were similar in people with and without MS. Unfortunately, people with MS were more likely to die 30 days after myocardial infarction (OR 1.46; 1.01–2.08). Similarly, mortality rates after breast and colorectal cancer are higher in people with MS than without MS.46,47 The differences in the association between MS and the care and outcomes of diabetes, hypertension, AMI, and two cancers highlight the need to examine this association in every comorbidity of interest.
Outcomes
Identification of appropriate intermediate outcomes has the potential to facilitate shorter, smaller trials of interventions for comorbidity. One recent study suggested that approximately one-third of the effect of vascular comorbidity on cognitive function in MS was mediated by changes in brain structure (thalamic and hippocampal volume, mean diffusivity of normal appearing white matter, and of gray matter). 48 Further work regarding intermediate outcomes is needed. As discussed earlier, comorbidity adversely affects relapse rates, as well as progression of physical and cognitive impairment. These are the typical outcomes used in clinical trials of disease-modifying therapies for MS. However, outcomes that are related to activities and participation may be more meaningful from the perspectives of people with MS and society. Quality of life can be conceptualized as encompassing abnormalities in body function (such as physical impairment) as well as activities and participation. Among people with MS, those with elevated symptoms of depression and anxiety, along with pain and fatigue, have greater presenteeism and absenteeism, as well as greater impairments in overall activity than those without elevated symptoms. 49 Physical and psychiatric comorbidities are associated with lower health-related quality of life (HRQoL). In one study, the magnitude of effect of depression on HRQoL was similar in magnitude to the effect of disability as measured by the EDSS. 5 Thus inclusion of a broader range of outcomes may be useful.
Models of care
A key question is what the optimal models are for managing comorbidity in people with MS. Most health care systems have a single disease focus that can lead to inefficient and fragmented care. 42 Treatment guidelines are not tailored to comorbidity. Initial steps may include examining the current state of MS teams and how comorbidity is currently addressed. For example, Canadian health care providers within MS Clinics indicate they lack insufficient personnel to address mental health issues. 50 This is concordant with the perspectives of people with MS, who report that they have insufficient access to such care. 51 Although mental health is recognized as an important comorbidity for the MS care team to address, management of other comorbidities is not. Novel approaches may better integrate underused providers such as advanced practice pharmacists into care teams, and use digital technologies to enhance communications.
All of these issues need to be better understood and addressed to support the implementation of any interventions targeting comorbidity in people with MS and should proceed in parallel with testing such interventions.
Conclusion
Comorbidity is common in people with MS, throughout the disease course, and adversely affects a broad range of outcomes. Attention is needed regarding prevention and treatment of comorbidity. This requires a better understanding of how MS affects comorbidity management, and determining optimal models of care.
Acknowledgments
Ruth Ann Marrie is supported by the Waugh Family Chair in Multiple Sclerosis. The author thanks the Charles and Margery Barancik Foundation and National Multiple Sclerosis Society.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Ruth Ann Marrie receives research funding from: CIHR, Research Manitoba, Multiple Sclerosis Society of Canada, Multiple Sclerosis Scientific Foundation, Crohn’s and Colitis Canada, National Multiple Sclerosis Society, CMSC, the Arthritis Society and the US Department of Defense, and is a co-investigator on studies receiving funding from Biogen Idec and Roche Canada.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ruth Ann Marrie  https://orcid.org/0000-0002-1855-5595
https://orcid.org/0000-0002-1855-5595
References
- 1. Graves JS, Barcellos LF, Simpson S, et al. The multiple sclerosis risk allele within the AHI1 gene is associated with relapses in children and adults. Mult Scler Relat Disord 2018; 19: 161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amezcua L, Rivera VM, Vazquez TC, et al. Health disparities, inequities, and social determinants of health in multiple sclerosis and related disorders in the US: A review. JAMA Neurol 2021; 78: 1515–1524. [DOI] [PubMed] [Google Scholar]
- 3. Rotstein D, Maxwell C, Tu K, et al. Risk of mortality in immigrants with multiple sclerosis in Ontario, Canada. Neuroepidemiology 2020; 54(2): 148–156. [DOI] [PubMed] [Google Scholar]
- 4. Schiltz NK. Prevalence of multimorbidity combinations and their association with medical costs and poor health: A population-based study of U.S. Front Public Health 2022; 10: 953886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berrigan LI, Fisk JD, Patten SB, et al. Health-related quality of life in multiple sclerosis: Direct and indirect effects of comorbidity. Neurology 2016; 86: 1417–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fitzgerald KC, Damian A, Conway D, et al. Vascular comorbidity is associated with lower brain volumes and lower neuroperformance in a large multiple sclerosis cohort. Mult Scler 2021; 27(12): 1914–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McKay KA, Tremlett H, Fisk JD, et al. Psychiatric comorbidity is associated with disability progression in multiple sclerosis. Neurology 2018; 90: e1316–e1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Palladino R, Chataway J, Majeed A, et al. Interface of multiple sclerosis, depression, vascular disease, and mortality: A population-based matched cohort study. Neurology 2021; 97: e1322–e1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marrie RA, Fisk JD, Stadnyk KJ, et al. Performance of administrative case definitions for comorbidity in multiple sclerosis in Manitoba and Nova Scotia. Chronic Dis Inj Can 2014; 34(2–3): 145–153. [PubMed] [Google Scholar]
- 10. Marrie RA, Yu BN, Leung S, et al. The utility of administrative data for surveillance of comorbidity in multiple sclerosis: A validation study. Neuroepidemiology 2013; 40(2): 85–92. [DOI] [PubMed] [Google Scholar]
- 11. Okura Y, Urban LH, Mahoney DW, et al. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 2004; 57: 1096–1103. [DOI] [PubMed] [Google Scholar]
- 12. Horton M, Rudick RA, Hara-Cleaver C, et al. Validation of a self-report comorbidity questionnaire for multiple sclerosis. Neuroepidemiology 2010; 35(2): 83–90. [DOI] [PubMed] [Google Scholar]
- 13. Marrie RA, Cohen J, Stuve O, et al. A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: Overview. Mult Scler 2015; 21(3): 263–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marrie RA, Patten SB, Tremlett H, et al. Sex differences in comorbidity at diagnosis of multiple sclerosis: A population-based study. Neurology 2016; 86: 1279–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Langer-Gould A, Albers KB, Van Den Eeden SK, et al. Autoimmune diseases prior to the diagnosis of multiple sclerosis: A population-based case-control study. Mult Scler 2010; 16(7): 855–861. [DOI] [PubMed] [Google Scholar]
- 16. Marrie RA, Patten SB, Tremlett H, et al. Increased incidence and prevalence of psoriasis in multiple sclerosis. Mult Scler Relat Disord 2017; 13: 81–86. [DOI] [PubMed] [Google Scholar]
- 17. Marrie RA, Patten S, Tremlett H, et al. Chronic lung disease and multiple sclerosis: Incidence, prevalence, and temporal trends. Mult Scler Relat Disord 2016; 8: 86–92. [DOI] [PubMed] [Google Scholar]
- 18. Marrie RA, Fisk J, Tremlett H, et al. Differing trends in the incidence of vascular comorbidity in MS and the general population. Neurology 2016; 6: 120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marrie RA, Fisk JD, Tremlett H, et al. Differences in the burden of psychiatric comorbidity in MS vs the general population. Neurology 2015; 85: 1972–1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rotstein D, Maxwell C, Tu K, et al. High prevalence of comorbidities at diagnosis in immigrants with multiple sclerosis. Mult Scler 2021; 27(12): 1902–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marrie RA, Walld R, Bolton JM, et al. Increased incidence of psychiatric disorders in immune-mediated inflammatory disease. J Psychosom Res 2017; 101: 17–23. [DOI] [PubMed] [Google Scholar]
- 22. Wan A, Bernstein CN, Graff LA, et al. Childhood maltreatment and psychiatric comorbidity in immune-mediated inflammatory disorders. Psychosom Med 2022; 84: 10–19. [DOI] [PubMed] [Google Scholar]
- 23. Vong V, Simpson-Yap S, Phaiju S, et al. The association between tobacco smoking and depression and anxiety in people with multiple sclerosis: A systematic review. Mult Scler Relat Disord 2023; 70: 104501. [DOI] [PubMed] [Google Scholar]
- 24. Harroud A, Marrie RA, Fitzgerald KC, et al. Mendelian randomization provides no evidence for a causal role in the bidirectional relationship between depression and multiple sclerosis. Mult Scler 2021; 27(13): 2077–2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kowalec K, Salter A, Fitzgerald KC, et al. Depressive symptom trajectories and polygenic risk scores in individuals with an immune-mediated inflammatory disease. Gen Hosp Psychiatry 2022; 77: 21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cuijpers P, Pineda BS, Quero S, et al. Psychological interventions to prevent the onset of depressive disorders: A meta-analysis of randomized controlled trials. Clin Psychol Rev 2021; 83: 101955. [DOI] [PubMed] [Google Scholar]
- 27. Marrie RA, Cutter G, Tyry T, et al. Effect of physical comorbidities on risk of depression in multiple sclerosis. Int J MS Care 2009; 11: 161–165. [Google Scholar]
- 28. Marrie RA, Walld R, Bolton JM, et al. Physical comorbidities increase the risk of psychiatric comorbidity in immune-mediated inflammatory disease. Gen Hosp Psychiatry 2018; 51: 71–78. [DOI] [PubMed] [Google Scholar]
- 29. Salter A, Kowalec K, Fitzgerald KC, et al. Comorbidity is associated with disease activity in MS: Findings from the CombiRx trial. Neurology 2020; 95: e446–e456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Marrie RA, Patel R, Figley CR, et al. Diabetes and anxiety adversely affect cognition in multiple sclerosis. Mult Scler Relat Disord 2019; 27: 164–170. [DOI] [PubMed] [Google Scholar]
- 31. Zhang T, Tremlett H, Zhu F, et al. Effects of physical comorbidities on disability progression in multiple sclerosis. Neurology 2018; 90: e419–e427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Marrie RA, Patel R, Bernstein CN, et al. Anxiety and depression affect performance on the symbol digit modalities test over time in MS and other immune disorders. Mult Scler 2021; 27(8): 1284–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Binzer S, McKay KA, Brenner P, et al. Disability worsening among persons with multiple sclerosis and depression: A Swedish cohort study. Neurology 2019; 93: e2216–e2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Al-Sakran L, Marrie RA, Blackburn D, et al. Impact of comorbidity on hospitalizations in individuals newly diagnosed with multiple sclerosis: A longitudinal population-based study. Mult Scler Relat Disord 2020; 40: 101955. [DOI] [PubMed] [Google Scholar]
- 35. Marrie RA, Walld R, Bolton JM, et al. Effect of mood and anxiety disorders on health care utilization in multiple sclerosis. Mult Scler 2021; 27(9): 1411–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Marrie RA, Fisk JD, Walld R, et al. Prescription opioid use in multiple sclerosis. J Neurol Neurosurg Psychiatry 2023; 94(2): 167–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Laroni A, Signori A, Maniscalco GT, et al. Assessing association of comorbidities with treatment choice and persistence in MS: A real-life multicenter study. Neurology 2017; 89: 2222–2229. [DOI] [PubMed] [Google Scholar]
- 38. Zhang T, Tremlett H, Leung S, et al. Examining the effects of comorbidities on disease-modifying therapy use in multiple sclerosis. Neurology 2016; 86: 1287–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Marrie RA, Zhang L, Lix LM, et al. The validity and reliability of screening measures for depression and anxiety disorders in multiple sclerosis. Mult Scler Relat Disord 2017; 20: 9–15. [DOI] [PubMed] [Google Scholar]
- 40. Tennenhouse LG, Marrie RA, Bernstein CN, et al. Machine-learning models for depression and anxiety in individuals with immune-mediated inflammatory disease. J Psychosom Res 2020; 134: 110126. [DOI] [PubMed] [Google Scholar]
- 41. Bisson EJ, Finlayson ML, Ekuma O, et al. Accuracy of FRAX® in people with multiple sclerosis. J Bone Miner Res 2019; 34(6): 1095–1100. [DOI] [PubMed] [Google Scholar]
- 42. Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers 2022; 8: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Raissi A, Bulloch AG, Fiest KM, et al. Exploration of undertreatment and patterns of treatment of depression in multiple sclerosis. Int J MS Care 2015; 17(6): 292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marrie RA, Kosowan L, Singer A. Management of diabetes and hypertension in people with multiple sclerosis. Mult Scler Relat Disord 2020; 40: 101987. [DOI] [PubMed] [Google Scholar]
- 45. Marrie RA, Tremlett H, Kingwell E, et al. Disparities in management and outcomes of myocardial infarction in multiple sclerosis: A matched cohort study. Mult Scler 2020; 26(12): 1560–1568. [DOI] [PubMed] [Google Scholar]
- 46. Marrie RA, Maxwell C, Mahar A, et al. Breast cancer survival in multiple sclerosis: A matched cohort study. Neurology 2021; 97: e13–e22. [DOI] [PubMed] [Google Scholar]
- 47. Marrie RA, Maxwell C, Mahar A, et al. Colorectal cancer survival in multiple sclerosis: A matched cohort study. Neurology 2021; 97: e1447–e1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Marrie RA, Patel R, Figley CR, et al. Effects of vascular comorbidity on cognition in multiple sclerosis are partially mediated by changes in brain structure. Front Neurol 2022; 13: 910014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Enns MW, Bernstein CN, Kroeker K, et al. The association of fatigue, pain, depression and anxiety with work and activity impairment in immune mediated inflammatory diseases. PLoS ONE 2018; 13(6): e0198975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Marrie RA, Donkers SJ, Jichici D, et al. Models of care in multiple sclerosis: A survey of Canadian health providers. Front Neurol 2022; 13: 904757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pétrin J, McColl MA, Donnelly C, et al. Prioritizing the healthcare access concerns of Canadians with MS. Mult Scler J Exp Transl Clin 2021; 7: 20552173211029672. [DOI] [PMC free article] [PubMed] [Google Scholar]