Abstract
Extending the benefits of vaccination to everyone who is eligible requires an understanding of which populations current vaccination efforts have struggled to reach. A clear definition of “hard-to-reach” populations – also known as high-risk or marginalized populations, or reaching the last mile – is essential for estimating the size of target groups, sharing lessons learned based on consistent definitions, and allocating resources appropriately. A literature review was conducted to determine what formal definitions of hard-to-reach populations exist and how they are being used, and to propose definitions to consider for future use. Overall, we found that (1) there is a need to distinguish populations that are hard to reach versus hard to vaccinate, and (2) the existing literature poorly defined these populations and clear criteria or thresholds for classifying them were missing. Based on this review, we propose that hard-to-reach populations be defined as those facing supply-side barriers to vaccination due to geography by distance or terrain, transient or nomadic movement, healthcare provider discrimination, lack of healthcare provider recommendations, inadequate vaccination systems, war and conflict, home births or other home-bound mobility limitations, or legal restrictions. Although multiple mechanisms may apply to the same population, supply-side barriers should be distinguished from demand-side barriers. Hard-to-vaccinate populations are defined as those who are reachable but difficult to vaccinate due to distrust, religious beliefs, lack of awareness of vaccine benefits and recommendations, poverty or low socioeconomic status, lack of time to access available vaccination services, or gender-based discrimination. Further work is needed to better define hard-to-reach populations and delineate them from populations that may be hard to vaccinate due to complex refusal reasons, improve measurement of the size and importance of their impact, and examine interventions related to overcoming barriers for each mechanism. This will enable policy makers, governments, donors, and the vaccine community to better plan interventions and allocate necessary resources to remove existing barriers to vaccination.
Keywords: Hard-to-reach, Definition, Vaccination, Immunization, Unvaccinated
1. Introduction
Following the initial success of the Expanded Programme on Immunization, routine immunization coverage in many countries has stalled due to difficulties reaching traditionally under-vaccinated subpopulations [1,2]. The under-vaccination of these subpopulations threatens the attainment of overall vaccination goals. For example, after years of progress, international polio eradication and measles elimination efforts have shown that some populations have been particularly difficult to reach with vaccination [3,4], resulting in unnecessary child deaths and disabilities, persistent polio-endemic areas, and recurring measles outbreaks. Recently, “hard-to-reach” populations (also known as high-risk or marginalized populations, or reaching the last mile) has emerged as a term to describe populations that have never been vaccinated or have not consistently received all recommended doses of the vaccine [5–7].
The public health community has found it difficult to define and describe these hard-to-reach populations. Hard-to-reach populations cannot be defined based on the outcome—individuals not vaccinated—because methods for predicting and implementing interventions prior to the vaccination outcome are needed. Neither can whole population groups (such as those typically defined by place of residence, nationality, or ethnicity) be labeled as hard to reach because they are not innately hard to reach; rather, there may be mechanisms, such as natural or established processes operating in particular social and environmental contexts, that preclude certain individuals from receiving vaccination. Having a clear definition of hard-to-reach populations is important for estimating the size of target populations, identifying strategies, and allocating resources for vaccinating additional individuals. A literature review was conducted to determine what formal definitions of hard-to-reach populations exist, how the term has been used, and the current state of knowledge on this topic, and to propose definitions to consider for future use.
2. Methods
Based on a prior conceptual framework of determinants of vaccination coverage [8] and expert knowledge of the literature, researchers generated a list of mechanisms that could make populations hard to reach for vaccination. A mechanism was defined as the natural or established process by which individuals become difficult to reach for vaccination. For example, rather than labeling specific types of individuals (e.g., migrants) as hard to reach, mechanisms by which a person can become hard to reach (e.g., transient movement) are described. Although special vaccination strategies may be used to reach hard-to-reach populations, this review mainly took into account traditional approaches of health-facility– or school-based vaccination, outreach vaccination, and periodic campaigns as the reference points for considering definitions of populations as hard to reach.
The initial list of mechanisms by which populations become hard to reach was confirmed and modified, based on identified papers and emergent themes from an iterative process consisting of keyword database searches and ad hoc purposive searches. For keyword searches, five databases were searched from 2000 to 2018 (through July 15): PubMed, Embase, Web-of-Science, Scopus, and Google Scholar. Search terms related to “hard to reach” combined with “vaccination” or “immunization” were used. Hard-to-reach search terms incorporated commonly associated terms, such as distant, isolated, remote, inaccessible, disadvantaged, deprived, hidden, vulnerable, marginalized, mobile, displaced, unsettled, or high-risk populations (see the Appendix for full search terms). Recent evidence was synthesized by mechanism to identify gaps in the literature. Recent or seminal papers that describe each mechanism are cited.
3. Identified literature gaps
Although studies that described hard-to-reach populations in terms of determinants of non-vaccination [8–11] were identified, comprehensive definitions of hard-to-reach populations were not found in the literature. For example, studies have examined the reasons for non-vaccination and under-vaccination, identifying factors related to immunization systems, family and caretaker characteristics, attitudes, and knowledge to explain poor vaccination coverage [9,11]. Individuals’ mistrust of health professionals, low literacy, and cultural factors have been used, among others, to characterize populations that are hard to reach for vaccination [12,13]. However, these studies did not provide a clear definition of all hard-to-reach populations. Studies often examined hard-to-reach populations primarily in geographic terms, focusing on populations that are far from health facilities or too remote for vaccination outreach services to access. Most studies simply described basic characteristics of the hard-to-reach groups they targeted, without a comprehensive definition. Not having a clear definition of hard-to-reach populations hampers strategy, planning, and determination of resource needs for extending immunization coverage.
Additionally, hard-to-reach populations were described with low specificity [14–17]; categories used to define these populations were often broad enough to encompass individuals who were vaccinated, under-vaccinated, or unvaccinated. For example, it was common to find imprecise definitions, such as populations “with limited or no geographical access, the urban poor, minorities, and children in conflict situations” [14]. Other studies described entire religious groups, all migrants, and nomadic groups as hard to reach for vaccination [15]. Moreover, existing definitions mostly classified specific population groups as hard to reach rather than describing the mechanisms that made individuals hard to reach. For example, one definition described hard-to-reach populations as “people who do not seek treatment in traditional care settings such as provider offices or clinics” [16] without describing the mechanisms that make care-seeking difficult. Other studies described hard-to-reach individuals as those who feel threatened by acknowledging to belong to a group, as well as group members who are distrustful of nonmembers [17], which ultimately did not define the mechanisms that make these populations avoid the health system in the first place. Labeling entire populations as hard to reach rather than characterizing them based on the mechanisms that make them difficult to reach introduces ambiguity about the population described and tends to lead to over-estimates of the actual numbers of individuals in these populations.
In addition, supply-side and demand-side barriers to vaccination often were not separated in descriptions of hard-to-reach populations. Although policy makers, governments, and donors tend to describe hard-to-reach populations in terms of supply-side barriers to reaching populations for vaccination, descriptions in the literature also included demand-side barriers, such as individuals who did not vaccinate even if vaccines were made available. Not separating the supply-side and demand-side barriers makes it difficult to understand the underlying problem and implement appropriate strategies.
Finally, there were few tools or scales identified in the literature that can be used to measure how hard to reach individuals are. Consequently, criteria or thresholds to classify individuals by how hard versus easier it is to reach them were rarely used in the literature, thus making definitions vague and the size of hard-to-reach or hard-to-vaccinate populations unquantifiable. Identifying and utilizing thresholds for clearly defining hard-to-reach and hard-to-vaccinate populations is important for planning, implementing, monitoring, and evaluating interventions to improve vaccination coverage. Identifying where populations exist along the spectrum, from easy to reach to hard to reach, and examining where thresholds are drawn to classify those who are hard to reach and hard to vaccinate can make a sizable difference in terms of the resources required and strategies applied.
4. Proposed definitions of hard-to-reach and hard-to-vaccinate populations
Based on these literature gaps and a list of mechanisms identified from the literature search, two separate definitions are proposed: one for hard-to-reach populations and one for hard-to-vaccinate populations. Specifically, populations that are hard to reach because of supply-side barriers are distinguished from populations who delay or refuse vaccines despite the availability of vaccination services and are therefore hard to vaccinate. This distinction is important because “hard to reach” focuses on vaccine delivery, with health-facility or school-based vaccination, outreach, and periodic campaigns as the reference points, whereas “hard to vaccinate” centers on vaccine uptake and acceptance. Mechanisms that make populations hard to reach or hard to vaccinate are part of a continuum because supply-side barriers can affect demand-side barriers and vice versa. The proposed definitions and mechanisms are classified based on the main demand or supply-side trigger. Moreover, populations are often influenced by multiple mechanisms. The proposed definitions of hard-to-reach populations and hard-to-vaccinate populations as informed by the literature are as follows:
Hard-to-reach populations are those who face supply-side barriers to vaccination due to geography by distance or terrain, transient or nomadic movement, healthcare provider discrimination, lack of healthcare provider recommendations, inadequate vaccination systems, war and conflict, home births or other home-bound mobility limitations, or legal restrictions.
Hard-to-vaccinate populations are those who are reachable but difficult to vaccinate because of demand-side barriers such as distrust, religious beliefs, lack of awareness, poverty or low-socioeconomic status, lack of time, or gender-based discrimination.
The distinction between mechanisms that make populations hard to reach and hard to vaccinate is important because they pose challenges requiring distinct interventions, with supply-side interventions targeting hard-to-reach populations and demand-side interventions targeting hard-to-vaccinate populations. Identifying and describing these populations based on specific mechanisms that make populations hard to reach or hard to vaccinate facilitates targeted interventions, taking into account interactions between supply- and demand-side barriers that simultaneously affect a population. For example, discrimination of certain populations by healthcare providers could reduce the supply of vaccination, but it could also reduce the demand for vaccination based on perceptions and experiences of discrimination among these populations. When both supply- and demand-side barriers exist, supply-side barriers should be addressed first.
Fig. 1 further illustrates the continuum between hard-to-reach and hard-to-vaccinate populations. While current immunization strategies of facility-based vaccination supplemented by outreach campaigns have reached individuals living in catchment areas with high supply and high levels of demand, unvaccinated and under-vaccinated individuals can be categorized into one of three groups. First are hard-to-reach populations that have high levels of demand but face low supply. The second group is hard-to-vaccinate populations who have low levels of demand despite high supply. Finally, there are individuals who are both hard to reach and hard to vaccinate who face both low levels of demand and low supply.
Fig. 1.
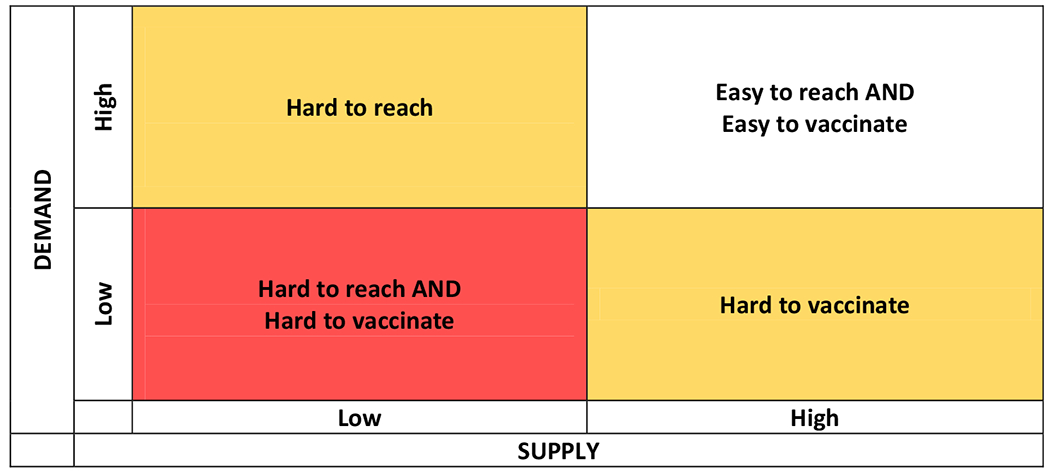
Conceptual framework of hard-to-reach and hard-to-vaccinate populations.
In the following sections, and in Table 1 and Table 2, the mechanisms that make individuals hard to reach or hard to vaccinate are described, and a summary of relevant literature describing each mechanism is presented. Populations may face multiple mechanisms that make them hard to reach, hard to vaccinate, or both. Mechanisms that make individuals hard-to-reach or hard-to-vaccinate are presented in the order of the most to least relevant processes, based partly on how frequently they were discussed in the literature.
Table 1.
Defining hard-to-reach populations for vaccination, based on current literature.
| Hard-to-reach populations | ||
|---|---|---|
|
| ||
| Mechanisms | Descriptions | |
| 1 | Geography by distance | Long distances from health facilities prevent individuals from accessing vaccination services and health providers from reaching individuals during outreach activities. |
|
| ||
| 2 | Geography by terrain | Inaccessible and difficult to traverse terrain, such as mountainous areas, wetlands, and islands, prevents individuals from accessing vaccination services and outreach teams from accessing populations. |
| 3 | Transient or nomadic movement | Movement by transient or nomadic populations, such as migrants, reduces their access to regular health care and complicates tracking of vaccination status, resulting in missed opportunities for vaccination. |
| 4 | Healthcare provider discrimination | Discriminated individuals may be denied services or face ill-treatment, which prevents them from receiving health services and vaccination. |
| 5 | Lack of healthcare provider recommendations | Healthcare providers not recommending or endorsing vaccines results in missed vaccination opportunities. |
| 6 | Inadequate vaccination systems | Inadequate vaccination infrastructure, human resources, and supply chain disruptions can make people living in catchment areas served by these systems hard to reach for vaccination. |
| 7 | War and conflict | In conflict settings, lack of security and destruction of health infrastructure can reduce access to health services and thwart immunization outreach activities. |
| 8 | Home births or other home-bound mobility limitations | Homebound individuals and mothers delivering at home may lack mobility to access vaccination services at health facilities. |
| 9 | Legal restrictions | Onerous paperwork and registration requirements by health facilities can prevent undocumented or migrant populations from accessing health services. In some instances, care is restricted to those with legal status. |
Table 2.
Defining hard-to-vaccinate populations, based on current literature.
| Hard-to-vaccinate populations | ||
|---|---|---|
|
| ||
| Mechanisms | Descriptions | |
| 1 | Distrust | Lack of trust in vaccines or health institutions, compounded by misinformation, can lead individuals to refuse vaccination. |
| 2 | Religious beliefs | Religious populations can object to immunizations based on religious beliefs, such as prohibitions against taking life, dietary laws, or interference with the natural order. |
| 3 | Lack of awareness | Lack of awareness of vaccine benefits and recommendations can lead to lower vaccination uptake. |
| 4 | Poverty or low socioeconomic status | Low socioeconomic status can preclude individuals from receiving vaccines. Even when vaccines are offered for free, individuals can face other financial barriers. |
| 5 | Lack of time | Inflexible scheduling and long wait times can thwart vaccination, especially among individuals with time constraints. |
| 6 | Gender-based discrimination | Discriminatory norms in the community, such as gender-based discrimination, lead to lack of agency and access to resources, resulting in fewer vaccinations for women and girls. |
5. What makes some individuals hard to reach for vaccination?
5.1. Geography by distance
A population’s remote geographic location is a barrier that can make them hard to reach. The literature discusses how distance from health facilities makes populations hard to reach for vaccination and impacts vaccine uptake [18,19,106]. Most studies did not specify a precise distance threshold for a population to be considered hard to reach; however, two studies used 5 km from a health center as a threshold [19,20]. Distance not only is a barrier from the perspective of individuals’ ability to reach the health facility, but can also impede health providers’ ability to conduct vaccination outreach activities [21].
5.2. Geography by terrain
Inaccessible and difficult-to-traverse terrain can make populations hard to reach. Such terrain is often found in rural settings characterized by a lack of road networks, such as in mountainous regions, wetlands, and islands [21–23]. Some terrain barriers to vaccination are seasonal, with rain, flooding, and other weather patterns causing impassable terrain and presenting barriers for vaccination access and delivery [24–26]. No studies were found that mentioned how long populations were not accessible for vaccination, or how much extra effort it may have taken to reach populations faced with terrain barriers. One study described hard-to-reach areas as having only one way to move, by boat or on foot [27].
5.3. Transient or nomadic movement
Migrants, nomadic groups, and people who are homeless or live on the streets experience settlement-related barriers that can make them hard to reach for vaccination. The literature describes frequent relocation by migrant populations, making tracking vaccination status difficult and reducing adherence to vaccination schedules [22,24,28]. However, no studies were identified that described the frequency of movement or duration per location that could define when populations became hard to reach due to movement. Lack of a fixed physical address among those who are homeless or live on the streets also poses a challenge for vaccination recording and tracking.
Movement makes transient or nomadic populations particularly hard to reach with vaccines that require multiple doses; these groups are often lost to follow-up for subsequent doses [22,29]. Because most vaccination programs are located in designated locations—offered at health centers or schools—movement of individuals can make previous locations distant and inconvenient [30]. When transient or nomadic individuals visit a new health facility, the lack of coordination between immunization information systems makes verification of vaccination status difficult, resulting in missed opportunities to complete doses [31,32].
5.4. Healthcare provider discrimination
Discrimination and marginalization of individuals by healthcare providers can make some populations hard to reach. For example, healthcare providers may discriminate against patients based on historical racial prejudice [33,34], which can prevent vaccination in some population groups. As another example, lesbian, gay, bisexual, and transgender (LGBT) individuals may not disclose their sexual identity, personal history, or medical information or seek healthcare or vaccination because they have previously faced discrimination [35–38]. Female sex workers or LGBT individuals who engage in sex work may be stigmatized and discriminated against by healthcare providers, preventing them from accessing health facilities and receiving vaccinations [39]. Ethnic and religious minorities may also experience discrimination and could be difficult to reach for vaccination. Undocumented and unlawful migrants and homeless persons have also reported that healthcare providers discriminate against them, thus discouraging them from seeking health services and vaccinations [40–42]. Poor people may also face discrimination, be more likely to be ill-treated by healthcare workers, endure long waiting hours, and be denied services, thus dissuading them from seeking vaccination [9]. No studies were identified that measured the level of healthcare provider discrimination or identified individuals who are hard to reach due to such discrimination.
5.5. Lack of healthcare provider recommendations
Individuals whose healthcare providers do not recommend or endorse vaccines can be hard to reach. A review of healthcare providers’ role in vaccination found that providers remain the most trusted advisor and influencer of vaccination decisions [43]. Therefore, when providers fail to recommend vaccines, doctor-patient encounters turn into missed opportunities for vaccination or patients may simply fail to return to the clinic for a visit [44,45]. Although lack of time and cost considerations are often cited as main reasons why providers fail to recommend vaccination [45], absent or weak vaccination information tracking systems can also make it hard for healthcare providers to identify and recommend vaccinations to individuals needing doses [46,47]. Even when such systems exist, healthcare providers sometimes fail to verify vaccination status and recommend vaccination [44,47].
Some subpopulations consistently receive fewer recommendations, thus making them hard to reach. For instance, vaccine uptake for human papillomavirus (HPV) vaccine among adolescents is primarily driven by healthcare provider recommendations, but providers are less likely to recommend the HPV vaccine to boys even when national guidelines indicate that both sexes should be vaccinated [35,48,49]. Language and cultural barriers also affect the ability of migrants to communicate with healthcare providers, which results in fewer vaccination recommendations and lower vaccine uptake [22,23,44]. No studies were found that measured or identified individuals who are hard to reach due to lack of healthcare provider recommendations.
5.6. Inadequate vaccination systems
Living within catchment areas where there are inadequate or dysfunctional vaccination systems can also make individuals hard to reach for vaccination. Supply-side barriers related to weak health systems are key drivers of low vaccination coverage in low- and middle-income countries [50,51]. Inadequacies in vaccination systems include undersupply of vaccines and lack of investment in vaccine infrastructure such as cold chain storage [52], or insufficient numbers of appropriately trained and motivated vaccinators and supervisors, which can amplify the problem of reaching individuals for vaccination, thereby creating hard-to-reach populations [22]. Supply chain disruptions result in vaccine shortages and sporadic availability [37,47] and disproportionately affect transient and low-socioeconomic-status populations that cannot make multiple health facility visits.
Lack of integration of health services in other government-run systems can also render populations hard to reach. For example, prisoners can become a hard-to-reach population because health services may not be integrated in penitentiary systems to provide adequate vaccinations for incarcerated individuals [53–55]. Other factors, such as political commitment to immunizations and local partnerships, have also been shown to be key drivers in vaccination outcomes [56], where individuals living in catchment areas without these attributes are hard to reach for vaccination; however, measures or thresholds for the degree of political commitment or for local partnerships that would render populations hard to reach have not been defined.
5.7. War and conflict
War and conflict create geographic pockets of hard-to-reach populations by displacing populations and physically reducing people’s access to health facilities [57,58]. Reduced access to health facilities and vaccination services can be caused by destruction of health facilities and other infrastructure such as roads and other transport routes [59,60]. Furthermore, conflict often impedes health workers from providing services, and aggressors sometimes view health workers with suspicion and threaten health workers’ personal safety, impeding vaccination services [61]. Professional security assessments are often conducted in areas of conflict to help immunization program personnel understand the risk profiles and receive security guidance [60]. No vaccination studies were found that estimated the number of individuals who are hard to reach due to war and conflict.
5.8. Home births or other home-bound mobility limitations
Populations with mobility limitations and women who deliver babies at home can also be hard to reach, where infants of mothers who deliver at home are less likely to be vaccinated [62]. Home births can make populations difficult to reach, especially for pediatric vaccines that should be given soon after birth [63,64]. Home-bound individuals and elders living alone, sometimes described as elderly shut-ins, are also reported to be difficult to reach [65]. No vaccination studies were found that examined individuals who are hard to reach due to home births or mobility limitations.
5.9. Legal restrictions
Laws can also make some individuals hard to reach by placing restrictions on how people can access the health system. For example, undocumented populations and unlawful immigrants face legal barriers that can make them hard to reach for vaccination [66,67]. Onerous paperwork and registration requirements by health facilities can prevent undocumented and unlawful migrants from accessing health services and receiving vaccinations [23,40,67]. Also, fear of detention and deportation deters many individuals from seeking healthcare, thus preventing vaccination [40]. No vaccination studies were found that focused on individuals who are hard to reach due to legal restrictions.
6. What makes some individuals reachable but hard to vaccinate?
6.1. Distrust
Some individuals lack trust in the scientific benefits of vaccines and the legitimacy of health institutions and authorities, making them physically reachable but hard to vaccinate [68]. Distrust in vaccines and resulting vaccine hesitancy has been observed globally spanning socio-economic strata, with contextual influences varying within and across countries [69]. Distrust in vaccines tends to affect pockets of the population who perceive the risk of vaccines to be greater than their benefits. This is most common in areas where vaccination has been successful in reducing the incidence of vaccine-preventable diseases, so that parents and providers become less familiar with the diseases vaccines prevent [70]. Belief in the benefits of acquiring natural immunity from vaccine-preventable illnesses rather than through vaccines has been shown to be correlated with less trust in health institutions and less willingness to vaccinate [71]. This mechanism was one of the few identified in the review for which measures, such as the Health Care System Distrust Scale [72] and the vaccine hesitancy survey, [73] have been developed. However, these measures have not been applied to identify individuals who are hard-to-vaccinate due to distrust of vaccines.
Distrust could also arise due to misinformation, such as the discredited link between the measles, mumps, and rubella vaccine and autism, [74] which can profoundly threaten vaccination programs. Rumors and community suspicions about profits of vaccine manufacturers or motives behind immunization promotion, such as fear of sterilization, have reduced vaccination coverage, spurred vaccine boycotts, and paused immunization programs [75,76]. Individuals may also distrust healthcare providers, which also limits vaccination opportunities. For example, homeless people living in shelters report concerns about privacy and confidentiality of information shared with healthcare providers, resulting in less use of health services and vaccination [41,42]. Another example is the fear of discrimination and the resulting distrust of health providers among LGBT individuals that can result in lower demand for vaccination, thus making them hard to vaccinate [38].
6.2. Religious beliefs
Some religious group members are hard to vaccinate because they object to immunizations based on their beliefs [9,77], such as their objection to 1) taking life, 2) violation of dietary laws, or 3) interference with the natural order by not letting events take their course [78]. For example, groups such as the Christian Scientists and apostolic faith sects founded in Zimbabwe decline some or all medical help for disease [79,80], so individual believers often forego immunization. Dutch Reformed congregations have also chosen to forego immunization to avoid interference with divine providence [81,82]. Some Muslims may have concerns about vaccines containing porcine-derived products such as gelatin, although numerous Islamic religious leaders and legal scholars have determined such products to be permissible [78]. Although there are relatively few objections that are theological in nature, with varying interpretations of religious texts, some religious leaders—who often act as gatekeepers to communities—have discouraged their followers from receiving vaccinations [81,83]. Preferences for limited contact with religious community outsiders can impede vaccination and other public health interventions [84]. Few vaccination studies were found that estimated the number of individuals who are hard to vaccinate due to religious beliefs through religious exemptions filed or granted [85].
6.3. Lack of awareness
Lack of awareness of vaccine benefits and recommendations is a communication barrier that can make some populations hard to vaccinate [29,44,45]. Lack of awareness about vaccinations disproportionately affects minority, immigrant, and low-socioeconomic-status populations. Individuals living in poverty are more likely to have low health literacy and education levels, which has been associated with low immunization uptake [86,87]. Undocumented and unlawful populations, even in instances where they are guaranteed certain health services, are often unaware of their entitlements and rights [40,67]. Moreover, women who are poorly educated are less aware of vaccine benefits [88] and are less likely to seek vaccination. Although these individuals may be within physical reach, they can be hard to identify and target because they do not actively seek immunizations. Other individuals may be easy to reach at one age but become hard to reach at a different age due to lack of awareness. For example, a child may be easy to reach as an infant because parents are familiar with the infant vaccination schedule, but children may become harder to reach when they are 2 years old or older due to lack of parental awareness of recommended vaccinations for older children [89]. No vaccination studies were found that estimated the extent of individuals who are hard to vaccinate due to lack of awareness of vaccine benefits and recommendations.
6.4. Poverty or low socioeconomic status
Poverty and low socioeconomic status can make some populations hard to vaccinate [90,91]. Poor people, for example, are less likely to have health insurance, which could cover vaccination costs [92]. Charging user fees can be a significant barrier to vaccination, especially for people of low socioeconomic status [9,10,47]. Even when free vaccinations are provided, poor people still face other financial barriers, such as not being able to afford transport to health facilities to be vaccinated [90,93]. Undocumented and unlawful populations as well as those who are homeless or live on the street often have limited resources to access health services, resulting in low vaccine uptake [21,40,67]. Poverty may also preclude people from being reached during special vaccination outreach initiatives such as school-based vaccination, because poor children may not be enrolled in schools [22]. The World Bank defines poverty as making less than $1.90 per person per day [94], but we did not identify any study that conducted poverty assessments to identify hard-to-vaccinate populations.
6.5. Lack of time
In addition to lack of financial resources, time constraints can impede vaccination uptake by making it difficult for people to use available vaccination services. At health facilities, inefficient procedures such as inflexible scheduling and long wait times preclude people with time constraints from accessing services, making them hard to vaccinate [37,95]. Moreover, individuals living in poverty face particular difficulty taking time away from work, and they may have financial insecurities and other competing priorities that can delay or prevent vaccination [9,91]. No vaccination studies were found that measured and targeted individuals who are hard to vaccinate due to limited time availability.
6.6. Gender-based discrimination
Gender-based discriminatory norms can make girls and women hard to vaccinate in some settings [9,88,96]. A preference for sons in some societies leads to less access to immunization for girls [88,96]. In some instances, men refuse permission for women to go or take children for immunization [9]. Such permission is more likely to be refused if children have had previous side effects from vaccination or when women need a chaperone to leave the house [9,88]. Lack of control over household finances can also impede women’s ability to obtain vaccination for themselves and their children [88,97]. Although widely used measures of discrimination such as the Everyday Discrimination Scale have been adapted to medical settings [98], such measures were not used to define and identify individuals who are hard to vaccinate due to discrimination.
7. Considerations
Based on the review of current literature, there is a clear need to more accurately define hard-to-reach and hard-to-vaccinate populations. Specifically, consideration should be given to the following:
To enable better targeting of interventions, hard-to-reach populations facing supply-side barriers should be described separately from hard-to-vaccinate populations facing demand-side barriers.
Rather than labeling entire populations as hard to reach, they should be characterized based on mechanisms that make them difficult to reach. This is important because individuals may enter and exit from different hard-to-reach and hard-to-vaccinate populations over time (e.g., at different ages over the life course). Focusing on mechanisms allows the definitions of “hard to reach” and “hard to vaccinate” to be used in a consistent way when characterizing these populations, permitting the composition of individuals within each population to vary over time. This is necessary to better estimate the size of these populations.
All mechanisms that make populations hard to reach or hard to vaccinate should be evaluated for each target population in need of vaccination because multiple mechanisms may apply, and supply- and demand-side factors may intersect in reinforcing cycles. This will facilitate consideration of multiple intervention strategies for each target population.
Standard measurements of each mechanism that makes populations hard to reach or hard to vaccinate should be developed and consistently used. Accurate and validated measures can be used in surveys and surveillance activities to identify these populations.
To inform strategy and planning, benefit-cost tradeoffs of different criteria or thresholds for defining hard-to-reach and hard-to-vaccinate populations should be examined. Without clear thresholds, these definitions cannot be operationalized for policy use.
Hard-to-reach populations should be targeted with supply-side interventions, and hard-to-vaccinate populations should be targeted with demand-side interventions. If the population faces both low supply and low demand levels, a mix of interventions should be considered, although ensuring sufficient supply should be addressed first to avoid the potential frustration and disengagement that may arise from increasing demand for vaccination services that the health system is not yet equipped to provide.
Based on contextual factors of target populations, evidence of costs and effectiveness of interventions should be examined to overcome barriers that characterize each mechanism of hard-to-reach and hard-to-vaccinate populations. Cost-effectiveness evidence is important for allocating resources efficiently and selecting appropriate interventions.
The most relevant and cost-effective interventions should be implemented for each mechanism to reach and vaccinate hard-to-reach and hard-to-vaccinate populations.
Beyond interventions within the health sector, cross-sector collaborations and non-health interventions should also be considered to reduce barriers that make populations hard-to-reach or hard-to-vaccinate. For example, infrastructure improvements such as better roads and bridges can mitigate barriers related to distance or terrain that make individuals hard-to-reach.
8. Conclusions
By summarizing the state of knowledge on the topic of defining hard-to-reach populations based on identified gaps in the literature, we propose definitions of hard-to-reach and hard-to-vaccinate populations that separate supply-side and demand-side factors. While we note that the mechanisms that can make individuals hard-to-reach or hard-to-vaccinate presented here may not be exhaustive, we highlight those that have been commonly identified from the literature. Defining these populations clearly is essential for policy makers, governments, donors, and the vaccine community to inform strategy, planning, and resource determinations for target interventions to remove existing barriers to vaccination.
There are other frameworks that exist to help identify determinants of individuals who may be difficult to vaccinate. For example, a matrix of determinants of vaccine hesitancy has been developed by the World Health Organization Strategic Advisory Group of Experts (SAGE) working group [99] and applied to classify reasons for vaccine hesitancy across countries [100]. While this matrix includes some of the hard-to-reach and hard-to-vaccinate mechanisms identified in this paper, such as geographical barriers and health provider factors, they may be less focused on supply side factors that make individuals hard-to-reach.
Further work is needed to examine the benefit-cost trade-offs of different thresholds for defining hard-to-reach populations, as well as developing validated measures of hard-to-reach populations to better estimate target populations. For each mechanism of hard-to-reach and hard-to-vaccinate populations, evidence of costs and effectiveness of interventions should be examined, within the country context, to select the best intervention for reaching and vaccinating these populations.
By defining mechanisms that make individuals hard to reach or hard to vaccinate, it is easier for vaccine community stakeholders to use common language when describing these populations, enhancing sharing of lessons across contexts. We show the current imprecise use of the hard-to-reach term across a heterogeneous mix of supply and demand mechanisms, and propose separating the term into hard-to-reach and hard-to-vaccinate to better describe the populations requiring different interventions. Furthermore, better describing these populations allows for better targeting of these populations, which in turn enable better advocacy for resources to implement necessary interventions.
By focusing on the mechanisms that make individuals hard to reach or hard to vaccinate, interventions can be better tailored to reduce or remove underlying barriers to vaccination, rather than broadly targeting whole sub-populations. For example, using new modes of transportation, such as drones, could potentially help reach populations that are hard to reach due to geography by distance or terrain, war, or conflict [101]. More nationally or regionally integrated vaccine information tracking systems could improve immunization coverage for hard-to-reach populations due to transient movement, or for hard-to-vaccinate individuals currently lacking healthcare provider recommendations [102]. Laws could be modified to remove restrictions to accommodate vaccination or reduce discriminatory practices. Incentives can be deployed to increase the use of vaccination among individuals with socioeconomic hardship or debilitating time constraints preventing vaccination [103]. Healthcare workers could be trained to reduce discriminatory practices and improve immunization recommendations. Community-based education programs may be carried out to raise awareness, reduce distrust, or involve religious leaders to accommodate vaccination [104]. Because each mechanism involves different challenges to reach and vaccinate populations, clearly defining these populations is essential for averting vaccine-preventable illnesses and deaths.
During the current “Decade of Vaccines” (2011–2020), the Global Vaccine Action Plan aims to prevent illnesses and deaths by promoting equitable access to existing vaccines for people in all communities [105]. The goal of the Global Vaccine Action Plan is to reach 90% national vaccination coverage and at least 80% vaccination coverage in every district or equivalent administrative unit for all vaccines in the national immunization programs by 2020 [105]. To reach such goals and beyond, better defining and characterizing hard-to-reach populations and hard-to-vaccinate populations who are either not vaccinated or under-vaccinated is essential. Better defining thresholds to identify and target these populations could aid policy makers, governments, donors, and the vaccine community improve immunization coverage.
Supplementary Material
Acknowledgements
Research reported in this publication was supported by the Centers for Disease Control and Prevention (CDC) via contract NU2GGH002000-02-00, the International Society for Infectious Diseases (ISID) and Pfizer via the SIGMA grant and the Agency for Healthcare Research and Quality (AHRQ) via grant R01HS023317, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Office of Behavioral and Social Sciences Research (OBSSR) and the Global Obesity Prevention Center (GOPC) via grant U54HD070725, NICHD via grant U01HD086861, and the National Institute for General Medical Science (NIGMS) via the MIDAS 5U24GM110707 grant. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Declaration of Competing Interest
None
Appendix A. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2019.06.081.
References
- [1].Sodha SV, Dietz V. Strengthening routine immunization systems to improve global vaccination coverage. Br Med Bull 2015;113:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Oyo-Ita A, Wiysonge CS, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database Systematic Rev 2016;7:Cd008145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cutts FT, Lessler J, Metcalf CJ. Measles elimination: progress, challenges and implications for rubella control. Expert Rev Vacc 2013;12:917–32. [DOI] [PubMed] [Google Scholar]
- [4].Thompson KM, Duintjer Tebbens RJ. Lessons from the polio endgame: overcoming the failure to vaccinate and the role of subpopulations in maintaining transmission. J Infect Dis 2017;216:S176–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].World Health Organization. Microplanning for immunization service delivery using the Reaching Every District (RED) strategy. Geneva, Switzerland: World Health Organization, 2009. http://apps.who.int/iris/bitstream/handle/10665/70450/WHO_IVB_09.11_eng.pdf;jsessionid=1DBEF506458FC15D0B48429BBAE5BA7B?sequence=1. [Google Scholar]
- [6].World Health Organization. REACHING EVERY DISTRICT (RED) 2017 Edition: A guide to increasing coverage and equity in all communities in the African Region. Geneva, Switzerland: World Health Organization, 2017. http://www.afro.who.int/sites/default/files/2018-02/Feb%202018_Reaching%20Every%20District%20%28RED%29%20English%20F%20web%20v3.pdf. [Google Scholar]
- [7].World Health Organization. The Guide to Tailoring Immunization Programmes (TIP): Increasing coverage of infant and child vaccination in the WHO European Region. Geneva, Switzerland: World Health Organization, 2013. http://www.euro.who.int/__data/assets/pdf_file/0003/187347/The-Guide-to-Tailoring-Immunization-Programmes-TIP.pdf. [Google Scholar]
- [8].Phillips DE, Dieleman JL, Lim SS, Shearer J. Determinants of effective vaccine coverage in low and middle-income countries: a systematic review and interpretive synthesis. BMC Health Serv Res 2017;17:681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Favin M, Steinglass R, Fields R, Banerjee K, Sawhney M. Why children are not vaccinated: a review of the grey literature. Int Health 2012;4:229–38. [DOI] [PubMed] [Google Scholar]
- [10].Phillips DE, Dieleman JL, Shearer JC, Lim SS. Childhood vaccines in Uganda and Zambia: Determinants and barriers to vaccine coverage. Vaccine 2018;36:4236–44. [DOI] [PubMed] [Google Scholar]
- [11].Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999–2009. Vaccine 2011;29:8215–21. [DOI] [PubMed] [Google Scholar]
- [12].Print F. Accessing hard to reach groups, travelers and looked after children. Hum Vacc Immunotherapeut 2013;9:1372–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bryant WK, Ompad DC, Sisco S, Blaney S, Glidden K, Phillips E, et al. Determinants of influenza vaccination in hard-to-reach urban populations. Prev Med 2006;43:60–70. [DOI] [PubMed] [Google Scholar]
- [14].Toikilik S, Tuges G, Lagani J, Wafiware E, Posanai E, Coghlan B, et al. Are hard-to-reach populations being reached with immunization services? Findings from the 2005 Papua New Guinea national immunization coverage survey. Vaccine 2010;28:4673–9. [DOI] [PubMed] [Google Scholar]
- [15].European Centre for Disease Prevention and Control. Review of outbreaks and barriers to MMR vaccination coverage among hard-to-reach populations in Europe. Stockholm, Sweden:ECDC, 2013. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/MMR-vaccination-hard-to-reach-population-review-2013.pdf. [Google Scholar]
- [16].Cassady D, Castaneda X, Ruelas MR, Vostrejs MM, Andrews T, Osorio L. Pandemics and vaccines: perceptions, reactions, and lessons learned from hard-to-reach latinos and the H1N1 campaign. J Health Care Poor Underserved 2012;23:1106–22. [DOI] [PubMed] [Google Scholar]
- [17].Benoit C, Jansson M, Millar A, Phillips R. Community-academic research on hard-to-reach populations: benefits and challenges. Qual Health Res. 2005;15:263–82. [DOI] [PubMed] [Google Scholar]
- [18].Blanford JI, Kumar S, Luo W, MacEachren AM. It’s a long, long walk: accessibility to hospitals, maternity and integrated health centers in Niger. Int J Health Geographics 2012;11:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jacobs B, Lindelow M, Xayyavong P, Sackett P. Building on community outreach for childhood vaccination to deliver maternal and child health services in Laos: a feasibility assessment. Reprod Health Matters 2012;20:112–21. [DOI] [PubMed] [Google Scholar]
- [20].World Health Organization. Immunization in Practice: A practical guide for health staff – 2015 Update. Geneva, Switzerland: World Health Organization, 2015. http://apps.who.int/iris/bitstream/handle/10665/193412/9789241549097_eng.pdf;jsessionid=B4EF6546AE5A1D397DA1713B1EE92B16?sequence=1. [Google Scholar]
- [21].Uddin MJ, Shamsuzzaman M, Horng L, Labrique A, Vasudevan L, Zeller K, et al. Use of mobile phones for improving vaccination coverage among children living in rural hard-to-reach areas and urban streets of Bangladesh. Vaccine 2016;34:276–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kaji A, Parker DM, Chu CS, Thayatkawin W, Suelaor J, Charatrueangrongkun R, et al. Immunization coverage in migrant school children along the thailand-myanmar border. J Immigr Minor Health 2016;18:1038–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kaewkungwal J, Apidechkul T, Jandee K, Khamsiriwatchara A, Lawpoolsri S, Sawang S, et al. Application of mobile technology for improving expanded program on immunization among highland minority and stateless populations in northern Thailand border. JMIR mHealth and uHealth. 2015;3:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Watson-Jones D, Mugo N, Lees S, Mathai M, Vusha S, Ndirangu G, et al. Access and attitudes to HPV vaccination amongst Hard-To-Reach populations in Kenya. PLoS ONE 2015;10:e0123701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Redzwan Habib K. Evaluating Immunisation Dropout Rates in Eight Hard to Reach Unions of Maulvibazar District, Bangladesh, Intl J Immunology 5, 2017, 5–10. [Google Scholar]
- [26].Sally ET, Kenu E. Evaluation of access and utilization of EPI services amongst children 12–23 months in Kwahu Afram Plains, Eastern region, Ghana. Pan African Med J 2017;28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Uddin MJ, Koehlmoos TP, Saha NC, Khan IA, Shamsuzzaman. Child immunization coverage in rural hard-to-reach areas of Bangladesh. Vaccine 2010;28:1221–5. [DOI] [PubMed] [Google Scholar]
- [28].Holzmann H, Hengel H, Tenbusch M, Doerr HW. Eradication of measles: remaining challenges. Med Microbiol Immunol 2016;205:201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Froehlich H, West DJ. Compliance with hepatitis B virus vaccination in a high-risk population. Ethn Dis 2001;11:548–53. [PubMed] [Google Scholar]
- [30].Bonner K, Banura C, Basta NE. HPV vaccination strategies targeting hard-to-reach populations: Out-of-school girls in LMICs. Vaccine 2018;36:191–3. [DOI] [PubMed] [Google Scholar]
- [31].Mipatrini D, Stefanelli P, Severoni S. Rezza G. Vaccinations in migrants and refugees: a challenge for European health systems. A systematic review of current scientific evidence. Pathogens Global Health 2017;111:59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kpozehouen E, Heywood AE, Kay M, Smith M, Paudel P, Sheikh M, et al. Improving access to immunisation for migrants and refugees: recommendations from a stakeholder workshop. Aust N Z J Public Health 2017;41:118–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Sanders Thompson VL, Arnold LD, Notaro SR. African American Parents’ HPV vaccination intent and concerns. J Health Care Poor Underserved 2012;23:290–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Quinn S, Jamison A, Musa D, Hilyard K, Freimuth V. Exploring the continuum of vaccine hesitancy between african american and white adults: results of a qualitative study. PLoS currents 2016;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Bednarczyk RA, Whitehead JL, Stephenson R. Moving beyond sex: Assessing the impact of gender identity on human papillomavirus vaccine recommendations and uptake among a national sample of rural-residing LGBT young adults. Papillomavirus Res 2017;3:121–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Reiter PL, McRee A-L, Katz ML, Paskett ED. Human papillomavirus vaccination among young adult gay and bisexual men in the United States. Am J Publ Health 2015;105:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Anderson EL. Recommended solutions to the barriers to immunization in children and adults. Mo Med 2014;111:344–8. [PMC free article] [PubMed] [Google Scholar]
- [38].Whitehead J, Shaver J, Stephenson R. Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS ONE 2016;11:e0146139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Scorgie F, Nakato D, Harper E, Richter M, Maseko S, Nare P, et al. ‘We are despised in the hospitals’: sex workers’ experiences of accessing health care in four African countries. Cult, Health Sex 2013;15:450–65. [DOI] [PubMed] [Google Scholar]
- [40].Hacker K, Anies M, Folb BL, Zallman L. Barriers to health care for undocumented immigrants: a literature review. Risk Manage Healthcare Policy 2015;8:175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Doroshenko A, Hatchette J, Halperin SA, MacDonald NE, Graham JE. Challenges to immunization: the experiences of homeless youth. BMC Publ Health 2012;12:338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Metcalfe SE, Sexton EH. An academic-community partnership to address the flu vaccination rates of the homeless. Publ Health Nurs (Boston, Mass) 2014;31:175–82. [DOI] [PubMed] [Google Scholar]
- [43].Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine 2016;34:6700–6. [DOI] [PubMed] [Google Scholar]
- [44].Greenfield LS, Page LC, Kay M, Li-Vollmer M, Breuner CC, Duchin JS. Strategies for increasing adolescent immunizations in diverse ethnic communities. J Adolescent Health: Off Publ Soc Adolescent Med 2015;56:S47–53. [DOI] [PubMed] [Google Scholar]
- [45].Bruno DM, Wilson TE, Gany F, Aragones A. Identifying human papillomavirus vaccination practices among primary care providers of minority, low-income and immigrant patient populations. Vaccine 2014;32:4149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Esposito S, Principi N, Cornaglia G. Barriers to the vaccination of children and adolescents and possible solutions. Clin Microbiol Infect 2014;20:25–31. [DOI] [PubMed] [Google Scholar]
- [47].Olorunsaiye CZ, Langhamer MS, Wallace AS, Watkins ML. Missed opportunities and barriers for vaccination: a descriptive analysis of private and public health facilities in four African countries. Pan African Med J 2017;27:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Krakow M, Beavis A, Cosides O, Rositch AF. Characteristics of adolescents lacking provider-recommended human papillomavirus vaccination. J Adolesc Health: Off Publ Soc Adolesc Med 2017;60:619–22. [DOI] [PubMed] [Google Scholar]
- [49].Vadaparampil ST, Malo TL, Sutton SK, Ali KN, Kahn JA, Casler A, et al. Missing the target for routine human papillomavirus vaccination: consistent and strong physician recommendations are lacking for 11- to 12-year-old males. Cancer Epidemiol Biomark Prev 2016;25:1435–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Nelson KN, Wallace AS, Sodha SV, Daniels D, Dietz V. Assessing strategies for increasing urban routine immunization coverage of childhood vaccines in low and middle-income countries: A systematic review of peer-reviewed literature. Vaccine 2016;34:5495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Haq Z, Shaikh BT, Tran N, Hafeez A, Ghaffar A. System within systems: challenges and opportunities for the Expanded Programme on Immunisation in Pakistan. Health Res Policy Syst 2019;17:51-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Ashok A, Brison M, LeTallec Y. Improving cold chain systems: Challenges and solutions. Vaccine 2017;35:2217–23. [DOI] [PubMed] [Google Scholar]
- [53].Sequera V-G, Valencia S, García-Basteiro AL, Marco A, Bayas JM. Vaccinations in prisons: A shot in the arm for community health. Hum Vacc Immunotherapeut 2015;11:2615–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Niveau G. Prevention of infectious disease transmission in correctional settings: A review. Publ Health 2006;120:33–41. [DOI] [PubMed] [Google Scholar]
- [55].Devine A, Karvelas M, Sundararajan V. Evaluation of a prison-based hepatitis B immunisation pilot project. Aust N Z J Public Health 2007;31:127–30. [DOI] [PubMed] [Google Scholar]
- [56].LaFond A, Kanagat N, Steinglass R, Fields R, Sequeira J, Mookherji S. Drivers of routine immunization coverage improvement in Africa: findings from district-level case studies. Health Policy Plann 2015;30:298–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Obradovic Z, Balta S, Obradovic A, Mesic S. The impact of war on vaccine preventable diseases. Materia Socio-Medica 2014;26:382–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Raslan R, El Sayegh S, Chams S, Chams N, Leone A, Hajj Hussein I. Re-emerging vaccine-preventable diseases in war-affected peoples of the eastern mediterranean region—An update. Front Publ Health 2017;5:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Duttine A, Hottentot E. Landmines and explosive remnants of war: a health threat not to be ignored. Bull World Health Organ 2013;91:160–A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Nnadi C, Etsano A, Uba B, Ohuabunwo C, Melton M, wa Nganda G, et al. Approaches to vaccination among populations in areas of conflict. J Infect Dis 2017;216:S368–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Silwal RC, Jimba M, Poudyal AK, Poudel KC, Wakai S. Improving immunization services under the armed conflict in rural Nepal. Public Health 2006;120:805–8. [DOI] [PubMed] [Google Scholar]
- [62].Moyer CA, Tadesse L, Fisseha S. The relationship between facility delivery and infant immunization in Ethiopia. Int J Gynaecol Obstet: Off Organ Int Federation Gynaecol Obstet 2013;123:217–20. [DOI] [PubMed] [Google Scholar]
- [63].Muranjan M, Mehta C, Pakhare A. An observational, health service based survey for missed opportunities for immunization. Indian Pediatr 2011;48:633–6. [DOI] [PubMed] [Google Scholar]
- [64].Creati M, Saleh A, Ruff TA, Stewart T, Otto B, Sutanto A, et al. Implementing the birth dose of hepatitis B vaccine in rural Indonesia. Vaccine 2007;25:5985–93. [DOI] [PubMed] [Google Scholar]
- [65].Coady MH, Galea S, Blaney S, Ompad DC, Sisco S, Vlahov D. Project VIVA: a multilevel community-based intervention to increase influenza vaccination rates among hard-to-reach populations in New York City. Am J Publ Health 2008;98:1314–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Aragones A, Genoff M, Gonzalez C, Shuk E, Gany F. HPV vaccine and latino immigrant parents: if they offer it, we will get it. J Immigr Minor Health 2016;18:1060–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Woodward A, Howard N, Wolffers I. Health and access to care for undocumented migrants living in the European Union: a scoping review. Health Policy Plann 2014;29:818–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med 2014;112:1–11. [DOI] [PubMed] [Google Scholar]
- [69].Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy-country-specific characteristics of a global phenomenon. Vaccine 2014;32:6649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Ozawa S, Stack ML. Public trust and vaccine acceptance–international perspectives. Hum Vaccin Immunother 2013;9:1774–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Baumgaertner B, Carlisle JE, Justwan F. The influence of political ideology and trust on willingness to vaccinate. PLoS ONE 2018;13:e0191728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Rose A, Peters N, Shea JA, Armstrong K. Development and testing of the health care system distrust scale. J Gen Intern Med 2004;19:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Sarathchandra D, Navin MC, Largent MA, McCright AM. A survey instrument for measuring vaccine acceptance. Prev Med 2018;109:1–7. [DOI] [PubMed] [Google Scholar]
- [74].Mrozek-Budzyn D, Kieltyka A, Majewska R. Lack of association between measles-mumps-rubella vaccination and autism in children: a case-control study. Pediatr Infect Dis J 2010;29:397–400. [DOI] [PubMed] [Google Scholar]
- [75].Nasiru SG, Aliyu GG, Gasasira A, Aliyu MH, Zubair M, Mandawari SU, et al. Breaking community barriers to polio vaccination in Northern Nigeria: the impact of a grass roots mobilization campaign (Majigi). Pathog Glob Health 2012;106:166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Renne E. Perspectives on polio and immunization in Northern Nigeria. Soc Sci Med 2006;63:1857–69. [DOI] [PubMed] [Google Scholar]
- [77].Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: An overview. Human Vacc Immunotherapeut 2013;9:1763–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Grabenstein JD. What the world’s religions teach, applied to vaccines and immune globulins. Vaccine 2013;31:2011–23. [DOI] [PubMed] [Google Scholar]
- [79].Kriss JL, Goodson J, Machekanyanga Z, Shibeshi ME, Daniel F, Masresha B, et al. Vaccine receipt and vaccine card availability among children of the apostolic faith: analysis from the 2010–2011 Zimbabwe demographic and health survey. Pan African Med J 2016;24:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Gerede R, Machekanyanga Z, Ndiaye S, Chindedza K, Chigodo C, Shibeshi ME, et al. How to Increase Vaccination Acceptance Among Apostolic Communities: Quantitative Results from an Assessment in Three Provinces in Zimbabwe. J Relig Health 2017;56:1692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Ruijs WL, Hautvast JL, van Ijzendoorn G, van Ansem WJ, van der Velden K, Hulscher ME. How orthodox protestant parents decide on the vaccination of their children: a qualitative study. BMC Publ Health 2012;12:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Spaan DH, Ruijs WLM, Hautvast JLA, Tostmann A. Increase in vaccination coverage between subsequent generations of orthodox Protestants in The Netherlands. Eur J Pub Health 2017;27:524–30. [DOI] [PubMed] [Google Scholar]
- [83].Pelčić G, Karačić S, Mikirtichan GL, Kubar OI, Leavitt FJ, Cheng-tek Tai M, et al. Religious exception for vaccination or religious excuses for avoiding vaccination. Croatian Med J 2016;57:516–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Stein-Zamir C, Zentner G, Abramson N, Shoob H, Aboudy Y, Shulman L, et al. Measles outbreaks affecting children in Jewish ultra-orthodox communities in Jerusalem. Epidemiol Infect 2008;136:207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties. PLoS Med 2018;15:e1002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Devasenapathy N, Ghosh Jerath S, Sharma S, Allen E, Shankar AH, Zodpey S. Determinants of childhood immunisation coverage in urban poor settlements of Delhi, India: a cross-sectional study. BMJ Open. 2016;6:e013015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Castro-Sánchez E, Chang PWS, Vila-Candel R, Escobedo AA, Holmes AH. Health literacy and infectious diseases: why does it matter? Int J Infect Dis 2016;43:103–10. [DOI] [PubMed] [Google Scholar]
- [88].Gavi (The Vaccine Alliance). Gender and immunisation. Geneva, Switzerland: Gavi, 2018. Retrieved from https://www.gavi.org/about/mission/gender/. [Google Scholar]
- [89].World Health Organization. Establishing and strengthening immunization in the second year of life: practices for vaccination beyond infancy. Geneva, Switzerland: World Health Organization, 2018. http://apps.who.int/iris/bitstream/handle/10665/260556/9789241513678-eng.pdf?ua=1. [Google Scholar]
- [90].Cushon JA, Neudorf CO, Kershaw TM, Dunlop TG, Muhajarine N. Coverage for the entire population: tackling immunization rates and disparities in Saskatoon Health Region. Can J Publ Health 2012;103:eS37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Guthmann JP, Chauvin P, Le Strat Y, Soler M, Fonteneau L, Lévy-Bruhl D. Moindre couverture vaccinale par le vaccin anti-pneumococcique conjugue dans les menages aux revenus faibles : une étude en île-de-France. Archives de Pédiatrie 2014;21:584–92. [DOI] [PubMed] [Google Scholar]
- [92].Fiscella K. Tackling disparities in influenza vaccination in primary care: it takes a team. J Gen Intern Med 2014;29:1579–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Egondi T, Oyolola M, Mutua MK, Elung’ata P. Determinants of immunization inequality among urban poor children: evidence from Nairobi’s informal settlements. Int J Equity Health 2015;14:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Ferreira FHG, Jolliffe DM, Prydz EB. The international poverty line has just been raised to $1.90 a day, but global poverty is basically unchanged. How is that even possible? Let’s talk development. Washington, DC: The World Bank; 2015. [Google Scholar]
- [95].McKnight J, Holt DB. Designing the Expanded Programme on Immunisation (EPI) as a service: Prioritising patients over administrative logic. Global Publ Health 2014;9:1152–66. [DOI] [PubMed] [Google Scholar]
- [96].Corsi DJ, Bassani DG, Kumar R, Awasthi S, Jotkar R, Kaur N, et al. Gender inequity and age-appropriate immunization coverage in India from 1992 to 2006. BMC Int Health Hum Rights 2009;9:S3–S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Topuzoglu A, Ay P, Hidiroglu S, Gurbuz Y. The barriers against childhood immunizations: a qualitative research among socio-economically disadvantaged mothers. Eur J Publ Health 2007;17:348–52. [DOI] [PubMed] [Google Scholar]
- [98].Williams DR, Yan Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol 1997;2:335–51. [DOI] [PubMed] [Google Scholar]
- [99].SAGE Vaccine Hesitancy Working Group. Report of the SAGE working group on vaccine hesitancy. Geneva, Switzerland: World Health Organization, 2014. https://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf. [Google Scholar]
- [100].Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015-2017. Vaccine 2018;36:3861–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Balasingam M. Drones in medicine-The rise of the machines. Int J Clin Pract 2017;71. [DOI] [PubMed] [Google Scholar]
- [102].Stockwell MS, Fiks AG. Utilizing health information technology to improve vaccine communication and coverage. Hum Vacc Immunotherapeut 2013;9:1802–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Jacob V, Chattopadhyay SK, Hopkins DP, Morgan JM, Pitan AA, Clymer J. Increasing coverage of appropriate vaccinations: a community guide systematic economic review. Am J Prev Med 2016;50:797–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].McArthur-Lloyd A, McKenzie A, Findley SE, Green C, Adamu F. Community engagement, routine immunization, and the polio legacy in Northern Nigeria. Global Health Commun 2016;2:1–10. [Google Scholar]
- [105].World Health Organization. Global Vaccine Action Plan 2011–2020. Geneva, Switzerland: World Health Organization, 2013. https://www.unicef.org/immunization/files/GVAP.pdf. [Google Scholar]
- [106].Lee B, Brown S, Haidari L, Clark S, Abimbola T, Pallas S, et al. Economic value of vaccinating geographically hard-to-reach populations with measles vaccine: A modeling application in Kenya. Vaccine 2019;37:2377–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


