ASCO and National Comprehensive Cancer Network guidelines recommend all patients with advanced cancer receive early palliative care (PC), within 8 weeks of diagnosis,1,2 on the basis of evidence that concurrent care improves patient symptoms, mood and quality of life (QOL), caregiver distress, and quality of care at the end of life.3 Unfortunately, guidelines ignore the reality that demand for PC outweighs the supply of specialists,4 and the evidence that not all patients have supportive care needs at the time of diagnosis.5 Key opinion leaders have instead advocated for timely PC on the basis of patient needs.6-8 The Symptom Screening with Targeted Early Palliative care (STEP) trial demonstrated proof of concept: using systemic assessment, the research team was able to identify who benefited from timely PC, and who did not demonstrate any PC need.9 Checklists, on the basis of patient symptoms or risk,10 and electronic health record (EHR) prediction models,11 have also successfully triggered timely PC referral. These studies force us to reimagine the current resource-intensive standard of early PC. We propose adoption of precision PC, a pragmatic approach that captures heterogeneous, time-varying, and complex patient/caregiver needs, while considering limited human and system resources.
Deficiencies of the Early PC Model
Consider the cases of Terrell, James, and Rachel.
Terrell is 60 years, exercises 3 days a week, and is asymptomatic from his stage IV slowly growing kidney cancer. He is tolerating single-agent immunotherapy without any side effects.
James is an older adult with an indolent B-cell lymphoma; he is frail, lives alone, and suffers from severe nausea, depression, and existential distress.
Rachel is asymptomatic from her newly diagnosed stage IV metastatic breast cancer, but her caregiver suffers existentially confronting the reality of her never being called grandma.
Randomized trials of early PC referred patients regardless of symptom burden or supportive care need as long as they met predefined, time-based criteria (eg, time from diagnosis and/or prognosis), resulting in universal referral within 3 months of diagnosis.12-17 In our case examples, Terrell and Rachel would be defaulted to early PC,1 while ignoring that James may have the greatest need. The early PC model assumes all patients with advanced cancer require symptom management or specialist PC at diagnosis, which is not true.18,19
Challenges Aligning Early PC Triggers With Workforce Capacity, and Patient and Caregiver Needs
Regrettably, the proportion of patients with advanced cancer outstrip the specialty PC workforce capacity.20 In the United States, there are currently about 1,700-3,300 full-time equivalents of board-certified PC specialists, most of whom are not oncology-specific, and care for patients with other serious illness.21,22 Unfortunately, the current pipeline for future PC physicians is narrow, with approximately 120 fellowship slots available each year, meaning workforce shortages will persist and worsen over time.
Even if capacity was not an issue, generalizing the benefit for early PC from seminal trials is problematic. Although early PC trials between 2002 and 2015 point to benefits in QOL and goal-concordant care,3 there is marked heterogeneity in trial quality and rigor, and weak evidence for these associations.3 In fact, a recent randomized cooperative group study, performed at 18 academic and community sites, did not demonstrate improvement in QOL for early PC.13 Fifteen percent of patients in the early PC intention-to-treat arm were never seen by a PC specialist, reflecting the poor infrastructure for PC delivery.23 Nationally, PC teams are partially constructed,24 dose intensity is variable,25 and equity issues exist: patients seen by PC tend to be White, have higher socioeconomic status, live on the West Coast or Northeast, and receive primary oncologic care in an academic medical center.26 These issues highlight the need to reimagine PC delivery.
Moving From Early PC to Precision PC
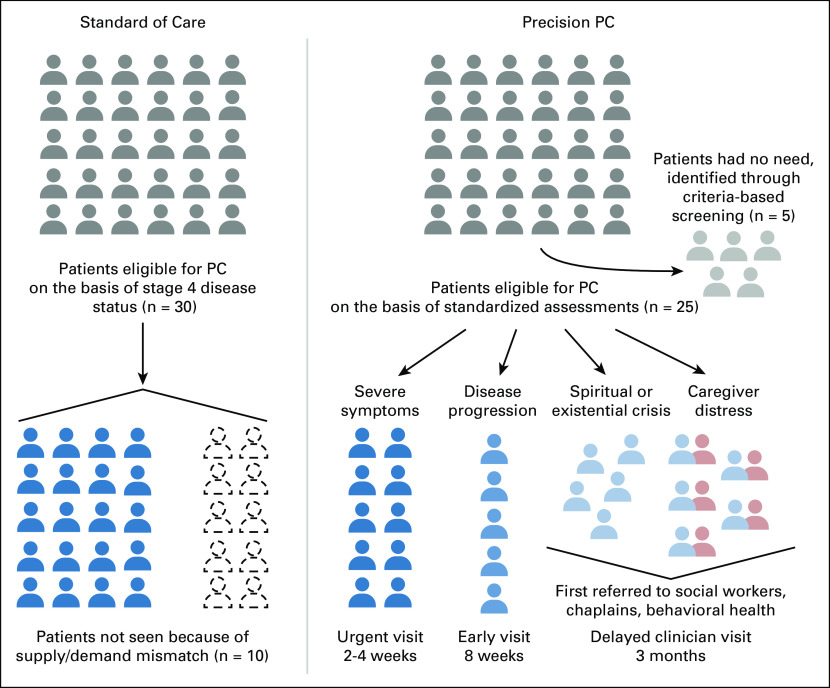
The model for PC delivery should transition from early PC as the standard of care to precision PC (Fig 1). With the current standard of care, a cohort of 30 patients with stage IV gastric cancer are appropriate to refer to specialty PC on the basis of disease characteristics as outlined in guidelines. Owing to capacity constraints, only 20 of those patients are scheduled an appointment with a specialty PC clinician within 2 months. Importantly, these appointments are agnostic to patient or caregiver need.
FIG 1.
Standard early PC versus precision PC delivery. PC, palliative care.
In a precision PC framework, supply and capacity are met when referral is personalized on the basis of patient and/or caregiver needs. This requires (1) routine systematic screening of supportive care needs, (2) consensus referral criteria that considers local resources, (3) timely triage and targeted services, and (4) adherence to behavioral economic principles.27
The first element of precision is establishing consensual criteria and having a system in place to trigger referral when appropriate. PC need (Fig 1) can be identified using consensus criteria validated in outpatient settings.28 This includes severe physical or emotional symptoms, request for hastened death, spiritual or existential crisis, assistance with decision making or care planning, patient request, delirium, brain or leptomeningeal disease, spinal cord compression or cauda equine, within 3 months of advanced or incurable cancer for patients with a median survival of 1 year or less, or progressive disease despite second-line systemic therapy for an incurable cancer. These factors could be assessed by structured EHR data, patient-reported outcome (PROs), and machine learning.
The next element of precision is timely triage. In our precision PC example, 25 patients meet criteria for PC need on the basis of Delphi criteria. Five patients with low levels of PC need are deferred from PC referral until they or their caregivers desire it, or when the level of PC need increases. In fact, ongoing is a randomized trial of stepped PC versus early PC (ClinicalTrials.gov identifier: NCT03337399). In this noninferiority trial, patients participate in outpatient PC visits at key points in their illness trajectory (including at the time of diagnosis, after changes in their cancer therapy, and after a hospitalization), with routine monitoring of QOL to ensure that those whose QOL deteriorates step up to more frequent PC visits. This will be compared with the established model of monthly PC visits, offering a more accessible, scalable, and patient-centered approach to ambulatory PC.
The third element of precision is targeted services. One fundamental aspect of PC is its interdisciplinary nature. In our cohort of patients with stage IV gastric cancer, 10 patients are flagged due to severe symptoms and are offered an urgent visit. Five patients meet criteria because of brain metastasis and progression on second-line therapy, and are offered an early visit within 8 weeks, understanding they will also see neurosurgery, radiation oncology, and the phase I team for trial evaluation. Five patients are noted to suffer from existential and/or spiritual crisis. An additional five are flagged as appropriate for PC because ofcaregiver distress. These 10 patients are offered a delayed PC clinician visit, within 3 months, and are meanwhile scheduled to see other members of the PC team, such as chaplaincy, social work, or behavioral health. Targeted services match the supply of patients needing an urgent visit (15 patients) to available new patient appointment slots. In fact, five new patient appointments remain open for urgent needs that may develop in subsequent weeks.
Although nascent, there are examples of precision PC in real-world practice. In one study at our institution, patients at high risk of death within 6 months were flagged by a machine learning mortality prediction model, and their oncologists nudged to consider early serious illness conversations while awaiting specialty referral to better understand patient and caregiver needs.29 An analogous mortality prediction model–based intervention at Stanford demonstrated improvement in advance care planning and documentation of prognosis.30 At Princess Margaret, in the STEP trial, targeted PC referral was implemented according to an algorithm based on symptom severity.9 Forty percent of patients never screened positive and QOL, symptom control, and mood remained stable over time demonstrating early PC was not necessary for those with mild symptoms.9
Precision PC Is What Patients and Caregivers Want
Qualitative research with patients and caregivers who have received PC unveil several key insights: they prefer care that is flexible in timing, steered by needs rather than clinician intuition, and focused on the family unit of care.31,32 Caregivers report improved satisfaction with care when PC is involved.33 Improvement in satisfaction is unrelated to the number of PC visits attended by the caregiver, as it is mediated by an observation of better care for the patient.34
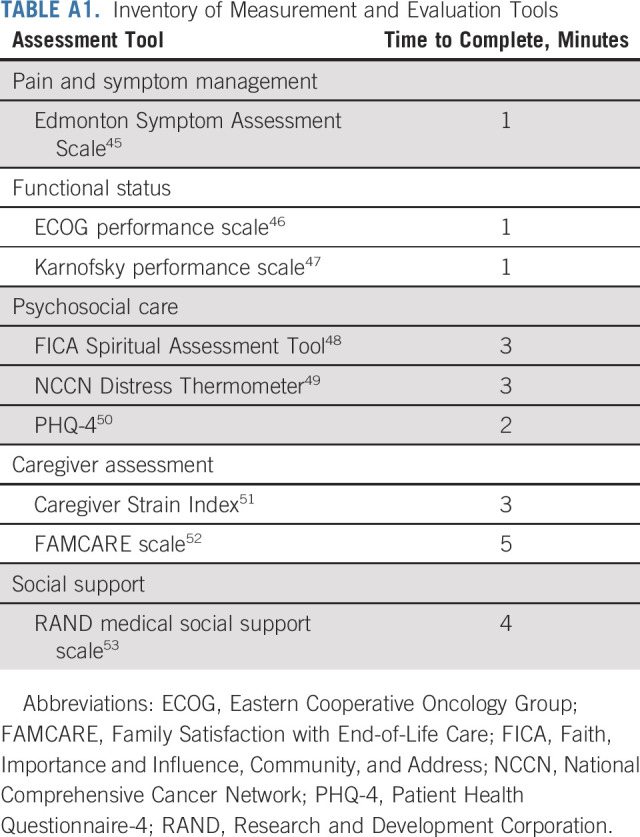
There are several steps necessary to meet patient and caregiver needs. First, automated assessments using PROs should be embedded into the EHR. Several randomized controlled trials have found that routine symptom monitoring is not only associated with improved QOL, but also longer survival.35,36 PROs enable not only real-time identification of PC need, but targeted referral to specific PC services. An inventory of suggested tools that assess multiple domains at risk is included in Appendix Table A1 (online only). Ideally, these assessments should be (1) available beyond the clinical encounter to allow timely upstream intervention, (2) embedded into the EHR as structured searchable data, and (3) integrated into clinical workflow with personnel dedicated to follow-up and triage. To use PRO data to identify patients' needs and direct care, we need to solidify computational methods to interpret large PRO data sets and clear mechanisms to flag missing information to capture unmet needs.37
Second, a common system barrier to timely PC referral is limited PC program infrastructure. Only 40% of non–National Cancer Institute–designated cancer centers report having PC services available.38 Where available, community PC teams are less likely to be interdisciplinary, a key element for success.39 Multidisciplinary PC teams, as opposed to single clinician services, are necessary for precision PC. Payers should consider value-based alternative payment models that provide bundled payments for PC-eligible individuals, to incentivize targeted referrals to behavioral health, social work, chaplaincy, physical therapy, and other services that address various aspects of PC need without the pressure to demonstrate financial viability of clinician-billed services. Extension of telehealth waivers, which began in response to the COVID-19 pandemic, may also increase access for patients and caregivers, and encourage innovation in PC delivery with regards to the supply/demand problem.
Third, medical oncologists who remain in power to influence change must own their responsibility to both deliver excellent primary PC, and support implementation of PC initiatives. Good leaders know the ripple effect of institutional culture. To this extent, oncology leaders should endorse the WHO view of PC as a core component of health systems.40 Outpatient PC programs would do better if they shared resources and budgets with oncology practices to build together.37 What if, oncologists insisted PC integration, implementation of PROs,35,36 and expansion of their multidisciplinary care team to include social work, chaplains, mental health providers, and care navigators was essential to their work, instead of it being an added benefit.
Insights from behavioral economics dictate that normative appeals to leadership endorsed standards can modify clinician behavior.41,42 What does it say when clinicians receive monthly e-mails detailing their relative value unit reports and not the frequency of their panels unmet needs? It signals that volume trumps quality. What we measure and incentivize matters. The EHR offers a unique opportunity to change behavior and facilitate best practice. The EHR can (1) administer PROs for screening, (2) display supportive care needs for the multidisciplinary care team, (3) offer best practice alerts and/or nudges for referral, (4) default a referral order, and (5) provide a dashboard to track key metrics.6,43 Successful work in behavioral science has already incentivized earlier referral to specialty PC,11 hospice use,41 and better conversations for seriously ill patients.29,30,44
In conclusion, specialty PC has a major role in cancer care delivery, although it must be deployed in a staged and sustainable fashion, targeted to individual and caregiver needs. As it now stands, current clinical guidelines for specialty PC referral apply a one-size-fits-all framework to often nuanced levels of PC need. Even 10 years after the seminal New England Journal of Medicine trial,12 what qualifies an advanced cancer prognosis has changed dramatically. As precision oncology has taken hold in the care of our patients with cancer, PC delivery models must too adopt a precision framework.
APPENDIX
TABLE A1.
Inventory of Measurement and Evaluation Tools
Lawrence N. Shulman
Consulting or Advisory Role: Genentech
Research Funding: Celgene (Inst), Independence Blue Cross (Inst)
Ravi B. Parikh
Stock and Other Ownership Interests: Merck, Google, GNS Healthcare, Onc.AI, Thyme Care
Consulting or Advisory Role: Thyme Care, Humana, NanOlogy, Merck
Research Funding: Humana
Patents, Royalties, Other Intellectual Property: Technology to integrate patient-reported outcomes into electronic health record algorithms
Travel, Accommodations, Expenses: The Oncology Institute of Hope and Innovation
Open Payments Link: https://openpaymentsdata.cms.gov/physician/701967
No other potential conflicts of interest were reported.
AUTHOR CONTRIBUTIONS
Financial support: Ravi B. Parikh
Administrative support: Ramy Sedhom, Ravi B. Parikh
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Precision Palliative Care as a Pragmatic Solution for a Care Delivery Problem
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Lawrence N. Shulman
Consulting or Advisory Role: Genentech
Research Funding: Celgene (Inst), Independence Blue Cross (Inst)
Ravi B. Parikh
Stock and Other Ownership Interests: Merck, Google, GNS Healthcare, Onc.AI, Thyme Care
Consulting or Advisory Role: Thyme Care, Humana, NanOlogy, Merck
Research Funding: Humana
Patents, Royalties, Other Intellectual Property: Technology to integrate patient-reported outcomes into electronic health record algorithms
Travel, Accommodations, Expenses: The Oncology Institute of Hope and Innovation
Open Payments Link: https://openpaymentsdata.cms.gov/physician/701967
No other potential conflicts of interest were reported.
REFERENCES
- 1.Ferrell BR, Temel JS, Temin S, et al. : Integration of palliative care into standard oncology care: ASCO Clinical Practice Guideline update summary. JCO Oncol Pract 13:119-121, 2017 [DOI] [PubMed] [Google Scholar]
- 2.Dans M, Kutner JS, Agarwal R, et al. : NCCN Guidelines® Insights: Palliative care, version 2.2021: Featured updates to the NCCN Guidelines. J Natl Compr Canc Netw 19:780-788, 2021. 34340208 [Google Scholar]
- 3.Kavalieratos D, Corbelli J, Zhang D, et al. : Association between palliative care and patient and caregiver outcomes: A systematic review and meta-analysis. JAMA 316:2104-2114, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sedhom R, Kamal AH: Is improving the penetration rate of palliative care the right measure? JCO Oncol Pract 18:e1388-e1391, 2022 [DOI] [PubMed] [Google Scholar]
- 5.Rodin R, Swami N, Pope A, et al. : Impact of early palliative care according to baseline symptom severity: Secondary analysis of a cluster-randomized controlled trial in patients with advanced cancer. Cancer Med 11:1869-1878, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hui D, Heung Y, Bruera E: Timely palliative care: Personalizing the process of referral. Cancers (Basel) 14:1047, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hui D, Hannon BL, Zimmermann C, et al. : Improving patient and caregiver outcomes in oncology: Team-based, timely, and targeted palliative care. CA Cancer J Clin 68:356-376, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathews J, Hannon B, Zimmermann C: Models of integration of specialized palliative care with oncology. Curr Treat Options Oncol 22:44, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmermann C, Pope A, Hannon B, et al. : Phase II trial of symptom screening with targeted early palliative care for patients with advanced cancer. J Natl Compr Canc Netw 20:361-370.e3, 2022 [DOI] [PubMed] [Google Scholar]
- 10.Paiva CE, Paiva BSR, Menezes D, et al. : Development of a screening tool to improve the referral of patients with breast and gynecological cancer to outpatient palliative care. Gynecol Oncol 158:153-157, 2020 [DOI] [PubMed] [Google Scholar]
- 11.Courtright KR, Chivers C, Becker M, et al. : Electronic health record mortality prediction model for targeted palliative care among hospitalized medical patients: A pilot quasi-experimental study. J Gen Intern Med 34:1841-1847, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Temel JS, Greer JA, Muzikansky A, et al. : Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733-742, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Temel JS, Sloan J, Zemla T, et al. : Multisite, randomized trial of early integrated palliative and oncology care in patients with advanced lung and gastrointestinal cancer: Alliance A221303. J Palliat Med 23:922-929, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakitas M, Lyons KD, Hegel MT, et al. : The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: Baseline findings, methodological challenges, and solutions. Palliat Support Care 7:75-86, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrell B, Sun V, Hurria A, et al. : Interdisciplinary palliative care for patients with lung cancer. J Pain Symptom Manage 50:758-767, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bakitas M, Lyons KD, Hegel MT, et al. : Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized controlled trial. JAMA 302:741-749, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Temel JS, Greer JA, El-Jawahri A, et al. : Effects of early integrated palliative care in patients with lung and GI cancer: A randomized clinical trial. J Clin Oncol 35:834-841, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quill TE, Abernethy AP: Generalist plus specialist palliative care—Creating a more sustainable model. N Engl J Med 368:1173-1175, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Block SD, Billings JA: A need for scalable outpatient palliative care interventions. Lancet 383:1699-1700, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Schenker Y, Arnold R: Toward palliative care for all patients with advanced cancer. JAMA Oncol 3:1459-1460, 2017 [DOI] [PubMed] [Google Scholar]
- 21.Active physician summary, AAHPM. http://aahpm.org/uploads/Profile_of_Active_HPM_Physicians_Executive_Summary_September_2017.pdf
- 22.Lupu D; American Academy of Hospice and Palliative Medicine Workforce Task Force : Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symptom Manage 40:899-911, 2010 [DOI] [PubMed] [Google Scholar]
- 23.Kamal AH, Bull JH, Swetz KM, et al. : Future of the palliative care workforce: Preview to an impending crisis. Am J Med 130:113-114, 2017 [DOI] [PubMed] [Google Scholar]
- 24.Aldridge MD, Hasselaar J, Garralda E, et al. : Education, implementation, and policy barriers to greater integration of palliative care: A literature review. Palliat Med 30:224-239, 2016 [DOI] [PubMed] [Google Scholar]
- 25.Sedhom R, Gupta A, MacNabb L, et al. : The impact of palliative care dose intensity on outcomes for patients with cancer. Oncologist 25:913-915, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Griggs JJ: Disparities in palliative care in patients with cancer. J Clin Oncol 38:974-979, 2020 [DOI] [PubMed] [Google Scholar]
- 27.Hui D, Bruera E: Integrating palliative care into the trajectory of cancer care. Nat Rev Clin Oncol 13:159-171, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hui D, Mori M, Watanabe SM, et al. : Referral criteria for outpatient specialty palliative cancer care: An international consensus. Lancet Oncol 17:e552-e559, 2016 [DOI] [PubMed] [Google Scholar]
- 29.Manz CR, Parikh RB, Small DS, et al. : Effect of integrating machine learning mortality estimates with behavioral nudges to clinicians on serious illness conversations among patients with cancer: A stepped-wedge cluster randomized clinical trial. JAMA Oncol 6:e204759, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gensheimer MF, Gupta D, Patel MI, et al. : Use of machine learning and lay care coaches to increase advance care planning conversations for patients with metastatic cancer. JCO Oncol Pract 19:e176-e184, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimmermann C, Ryan S, Hannon B, et al. : Team-based outpatient early palliative care: A complex cancer intervention. BMJ Support Palliat Care 10.1136/bmjspcare-2019-001903 [epub ahead of print August 12, 2019] [DOI] [PubMed] [Google Scholar]
- 32.Hannon B, Swami N, Pope A, et al. : Early palliative care and its role in oncology: A qualitative study. Oncologist 21:1387-1395, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McDonald J, Swami N, Hannon B, et al. : Impact of early palliative care on caregivers of patients with advanced cancer: Cluster randomised trial. Ann Oncol 28:163-168, 2017 [DOI] [PubMed] [Google Scholar]
- 34.Wadhwa D, Burman D, Swami N, et al. : Quality of life and mental health in caregivers of outpatients with advanced cancer. Psychooncology 22:403-410, 2013 [DOI] [PubMed] [Google Scholar]
- 35.Basch E, Deal AM, Dueck AC, et al. : Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 318:197-198, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Basch E, Deal AM, Kris MG, et al. : Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol 34:557-565, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaufmann TL, Kamal AH: Oncology and palliative care integration: Cocreating quality and value in the era of health care reform. JCO Oncol Pract 13:580-588, 2017 [DOI] [PubMed] [Google Scholar]
- 38.Hui D, De La Rosa A, Bruera E: State of integration of palliative care at National Cancer Institute-designated and nondesignated cancer centers. JAMA Oncol 6:1292-1295, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hui D, De La Rosa A, Chen J, et al. : State of palliative care services at US cancer centers: An updated national survey. Cancer 126:2013-2023, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Assembly : Resolution: Strengthening of palliative care as a component of comprehensive care throughout the life course, 2014. http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R19-en.pdf
- 41.Sedhom R, Blackford AL, Gupta A, et al. : Oncologist peer comparisons as a behavioral science strategy to improve hospice utilization. JCO Oncol Pract 18:e1122-e1131, 2022 [DOI] [PubMed] [Google Scholar]
- 42.Albertini JG, Wang P, Fahim C, et al. : Evaluation of a peer-to-peer data transparency intervention for Mohs micrographic surgery overuse. JAMA Dermatol 155:906-913, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mooney K, Berry DL, Whisenant M, et al. : Improving cancer care through the patient experience: How to use patient-reported outcomes in clinical practice. Am Soc Clin Oncol Ed Book 37:695-704, 2017 [DOI] [PubMed] [Google Scholar]
- 44.Takvorian SU, Bekelman J, Beidas RS, et al. : Behavioral economic implementation strategies to improve serious illness communication between clinicians and high-risk patients with cancer: Protocol for a cluster randomized pragmatic trial. Implement Sci 16:90, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Watanabe SM, Nekolaichuk C, Beaumont C, et al. : A multicenter study comparing two numerical versions of the Edmonton Symptom Assessment System in palliative care patients. J Pain Symptom Manage 41:456-468, 2011 [DOI] [PubMed] [Google Scholar]
- 46.Oken MM, Creech RH, Tormey DC, et al. : Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649-656, 1982 [PubMed] [Google Scholar]
- 47.Schag CC, Heinrich RL, Ganz PA: Karnofsky performance status revisited: Reliability, validity, and guidelines. J Clin Oncol 2:187-193, 1984 [DOI] [PubMed] [Google Scholar]
- 48.Puchalski CM: The FICA spiritual history tool #274. J Palliat Med 17:105-106, 2014 [DOI] [PubMed] [Google Scholar]
- 49.Riba MB, Donovan KA, Andersen B, et al. : Distress management, version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 17:1229-1249, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kroenke K, Spitzer RL, Williams JB, et al. : An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 50:613-621, 2009 [DOI] [PubMed] [Google Scholar]
- 51.Robinson BC: Validation of a Caregiver Strain Index. J Gerontol 38:344-348, 1983 [DOI] [PubMed] [Google Scholar]
- 52.Ringdal GI, Jordhoy MS, Kaasa S: Measuring quality of palliative care: Psychometric properties of the FAMCARE Scale. Qual Life Res 12:167-176, 2003 [DOI] [PubMed] [Google Scholar]
- 53.Sherbourne CD, Stewart AL: The MOS social support survey. Soc Sci Med 32:705-714, 1991 [DOI] [PubMed] [Google Scholar]