Abstract
Labial varices are commonly seen in women with varicose veins of the pelvis. Initial management is conservative management since labial varies typically resolve, particularly in pregnant patients following delivery. Varices can be seen also in association with pelvic varices in the pelvic venous disease spectrum. Sclerotherapy is often the management. This article reviews the presentation and treatment of patients with labial varices, with a focus on interventional radiologic management.
Keywords: interventional radiology, varices, labial, vulvar, sclerotherapy, pelvic venous disorder
Labial varices are seen in up to 34% of women with varicose veins of the pelvis, mostly secondary to pregnancy, due to increased levels of estrogen and progesterone. 1 The incidence of labial varices may be underestimated due to lack of reporting from patients and the fact that in some cases it can present without clinical symptoms. 2 Conservative management is the most common approach, as most patients are asymptomatic and labial varies often self-resolve in the months after delivery, when hormone levels begin to decrease. However, in a subset of patients, symptoms persist and/or labial varices recur after subsequent pregnancies and can be seen also in association with pelvic varices in the pelvic venous disease (PeVD) spectrum. Interventions may vary depending on the size, location of varices, and severity of symptoms. While surgical resection with phlebectomy can be an option, sclerotherapy is often preferred as it is less invasive and very effective on thin-walled varices such as those seen in the vulva. Sclerotherapy is also preferred when there is concomitant PeVD. In this review, we provide an overview of interventional procedures, as well as the approach on patients presenting with symptomatic labial varices.
Clinical Presentation and Evaluation of Patients
Labial varices are present in up to 22% of women during pregnancy. 1 Common, more minor symptoms include dyspareunia, pruritus, pelvic pain, and pain with ambulation. Patients with minor symptoms or asymptomatic patients are managed conservatively if no complications occur. 1 However, if more serious complications, such as progression to PeVD, development of significant pain with superficial dyspareunia and vulvodynia, or thromboembolic events occur, intervention is indicated. While most cases of labial varices resolve in the months following delivery, 8% of patients have persistence and enlargement of varices after the postpartum period. These patients typically require intervention. 3 4 Though most cases of labial varices occur in pregnant patients, nonpregnant patients, especially those with high-estrogen states, such as in a case report of a morbidly obese adolescent female, or with vascular abnormalities, such as left iliac vein stenosis, can develop the condition in the absence of pregnancy. 5 6
Due to the extensive collateralization of the pelvic veins with superficial and deep vasculature in the external genitalia and lower extremities, patients may also have pain, tenderness, itching, bleeding, or superficial venous thrombosis in collateral areas. 7 Lower extremity varices are subcutaneous, dilated veins greater than or equal to 4 mm in diameter with reflux in the upright position and involve the saphenous and accessory saphenous trunks as well as their tributaries and nonsaphenous superficial veins of the leg. 8 They typically occur along the posteromedial thigh following the distribution of the perineal, vulvovaginal, and gluteal varices. 9 10 Furthermore, nonsaphenous varicosities in the vulva are not uncommon, and can occur in estimated 24 to 40% of patients with lower extremity varicose veins. 11 12 Sciatic or tibial nerve varices have also been reported in the setting of inferior gluteal vein reflux, resulting in radiating pain from the buttock to the lateral leg which increases with sitting. 13 Previous data have shown that a proportion (16.6%) of patients treated with stenting for pelvic venous disease and iliac vein stenosis have labial varices that required adjunctive procedures, including embolization, for treatment. 14
Anatomy and Pathophysiology
The pelvic venous drainage includes the inferior vena cava, internal iliac veins, and femoral veins. These pelvic veins typically are extensively collateralized—pelvic veins are often interconnected with the superficial veins of the genitalia and the lower extremities, which can result in extrapelvic symptoms. In the context of PeVD, these are referred to as escape points, which arise when venous obstruction in the common iliac vein results in secondary reflux into the left internal iliac vein lower extremity or labial (vulvar) veins. These cause extrapelvic varices from retrograde flow arising from reflux exiting the pelvis through these escape points ( Table 1 ). 7 15 16
Table 1. Common escape points in pelvic venous disease.
| Escape point | Venous connection | Location of varices |
|---|---|---|
| Perineal | Internal to external pudendal veins | Perineum, posterior labia |
| Inguinal | Recanalized round ligament vein | Groin, labia |
| Gluteal | Inferior gluteal vein and femoral circumflex | Lower extremity |
| Obturator | Deep veins of medial thigh and obturator | Lower extremity |
In compensated physiology of PeVD, increased intrapelvic venous pressure is transmitted to the distal venous reservoir in the pelvis and decompressed through reflux via collaterals, resulting in pelvic-derived labial and lower extremity varices. The common pathways include reflux of the perineal vein via internal and external pudendal veins causing inner thigh and posterior labial varicose veins; reflux of the inguinal vein via recanalized round ligament vein causing groin and labial varicose veins; reflux of the superior gluteal point causing posterolateral varices of the thigh; and reflux of the inferior gluteal point causing sciatic nerve varicose veins. 17 If collateral varices are present, additional clinical and radiologic examinations are recommended prior to deciding on a treatment method.
The American Vein and Lymphatic Society recognized the need for a classification instrument and created the Symptoms-Varices-Pathophysiology (SVP) classification in 2021 to improve clinical decision making and can be used in conjunction with the Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification. 18 19 Further, the goal of the development of the SVP classification system is to help create patient population groups to help increase the robustness of literature and future clinical trials. The development of this system reflects the increasingly nuanced understanding of PeVD, as these disorders are defined by a heterogeneous mix of pathologic mechanisms that impact the vasculature of the pelvis, genitalia, and lower extremities, manifesting in overlapping and sometimes vague symptoms. The SVP classification includes three domains: symptoms (S), varices (V), and a composite anatomic-pathophysiologic domain (P). Symptoms (S) and varices (V) are considered to occur in four anatomic zones in a descending fashion. 18 Zone 4 is classified with CEAP and is not included in the SVP instrument. Symptoms are defined as S 0 –S 3 and varices as V 0 –V 3 . Patients with lower extremity symptoms arising in the pelvis should be described using both SVP and CEAP classifications.
Diagnostic Imaging
In the case of labial varices, ultrasound may be the first-line imaging modality used for diagnosis, as it is noninvasive and can provide valuable information about the location, size, shape, and extent of involvement of the varices. Ultrasound should also be considered in patients with persistent symptoms after treatment for chronic venous disorders. A 2020 study of 227 patients with pelvic venous insufficiency by Scotti et al found that at least 50% of patients also have associated lower extremity reflux. 20 Cross-sectional diagnostic imaging may be used in cases where more detailed information is needed or if there is suspicion of associated conditions or complications. Cross-sectional imaging can also be useful for surgical or interventional planning. Catheter venography is advantageous in that it allows radiologists not only to diagnose, but also treat PeVD at the same time. Data supporting factors that should be treated are lacking, but studies have reported that findings associated with inclination to treat were pelvic contrast retention of more than 20 seconds, gonadal vein diameter of 6 mm or more, reflux into the iliac vein, or contrast flow via escape points into perineal, labial, or lower extremity varicosities. 21
Interventional Treatments
There are different interventional pathways in how to treat labial varicosities. Interventional treatments are usually performed in an outpatient basis, under conscious sedation. There is significant debate on whether to treat labial varices with pelvic embolization (typically branches of internal iliac and/or ovarian veins), the so-called top-down approach, or to directly puncture these varices if accessible percutaneously with ultrasound, the “bottom-up approach.” 22 There are a few case reports and in the absence of prospective randomized study comparing different treatment options, it has been recommended that pelvic embolization should be performed in PeVD patients who are symptomatic due to ovarian or pelvic vein reflux with or without labial varices. 23 However, in patients with pelvic insufficiency, without pelvic pain, but with vulvodynia and evidence of visible varices, embolization from a top-down approach is not indicated, given that foam sclerotherapy with direct puncture results in good clinical outcomes in patients with labial varices. The bottom-up approach with direct sclerotherapy to labial varices is the preferred treatment in patients with isolate vulvar symptoms. Sclerotherapy alone may not be a sufficient standalone treatment if there is concomitant significant saphenofemoral, ovarian, or iliac venous insufficiency that is not also treated as this increases risk of recurrence. 12 Therefore, many patient factors are important to consider when deciding which interventional approach is most appropriate for the patient. Below we describe indications and techniques for both approaches.
“Top-Down” Approach
Catheterization of the internal iliac veins can be performed from a femoral or internal jugular approach. At our institution, we perform access from the internal jugular vein (IJV) as it results in a less tortuous pathway to the gonadal veins. After accessing the IJV with a micropuncture set, a 6-Fr-long vascular sheath is placed. Next, a 4- to 5-Fr multipurpose catheter is advanced over the wire into internal iliac veins and hand injection of contrast venography is performed to confirm positioning of the catheter and confirm venous reflux ( Fig. 1a ). Using a combination of a 4- to 5-Fr catheter and 0.035-inch hydrophilic guidewire, selective catheterization into the distal branches of the internal iliac veins is then performed. However, even when venography is performed with Valsalva maneuver, it may be difficult to visualize the escape points into the labial regions, due to persistent antegrade flow into the internal iliac veins. 2 In these situations, the use of a compliant balloon-occlusion catheter may be needed ( Fig. 1b ). In selected cases, a 2.8-Fr microcatheter can be used to obtain distal access into the labial veins ( Fig. 2a, b ), for a more controlled delivery of sclerosants into these distal branches of vulvar region ( Fig. 2c ).
Fig. 1.
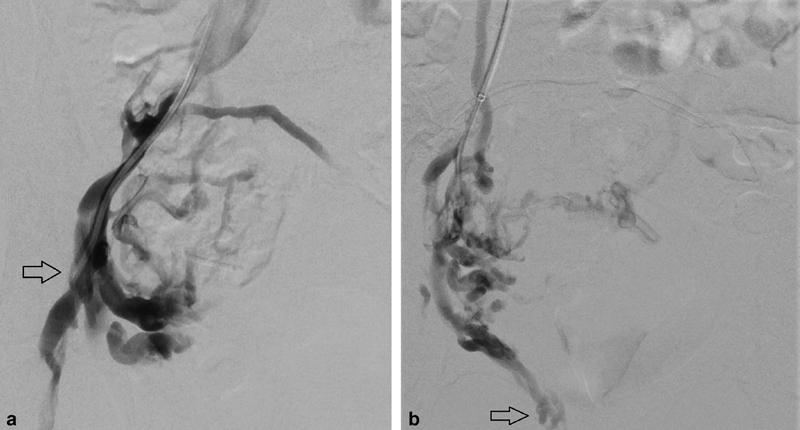
Pelvic venography at the right internal iliac vein level (arrow) with a 5-Fr Kumpe catheter (Cook Medical, Inc., Bloomington, IN) ( a ) and with a 5.5-Fr balloon-occlusion catheter ( b ). Distal pelvic venous branches and vulvar varices (arrow) are opacified after placement of a compliant balloon catheter ( b ).
Fig. 2.
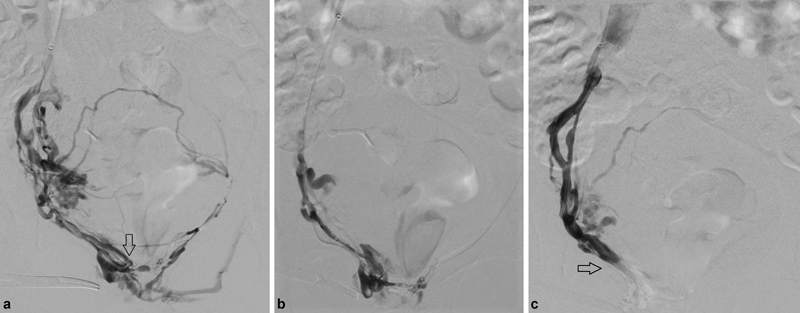
“Top-down” approach to labial varices: catheterization with a 5-Fr Kumpe catheter (arrow, a ) and with a 2.8-Fr microcatheter ( b ) for delivery of foam sclerotherapy into the right labial varices. Post-sclerotherapy venography of right labial varices demonstrated occlusion of veins distally into the right genital area (arrow, c ).
If performed from a right femoral vein approach, access is obtained via a 6-Fr short sheath, and the contralateral internal iliac vein is selected with a Cobra catheter. A 5.5-Fr Fogarty balloon is exchanged over a 0.035-inch Rosen wire and is placed just above the true pelvis where the tributaries and gonadal vein join. Access can be repeated on the contralateral side to select both internal iliac veins and bilateral injections can be performed. If necessary, a catheter can be advanced further into tributaries off the internal iliac vein and subselective balloon occluded venograms can be performed to identify residual varices in the pelvis, vulvar, or thigh regions.
The volume of the pelvic varices venous plexus can be estimated by inflating the balloon and injecting contrast until normal veins are opacified or when contrast refluxes into the contralateral internal iliac vein. The volume of sclerosing agent should be 75% of the measured volume. Different agents can be used for sclerosant, but our practice utilizes a 3% sodium tetradecyl sulfate (STS) solution mixed with air in a 1:4 ratio to create a sclerosant foam. Once delivered into the varices, the balloons remain inflated for 5 to 10 minutes to prevent nontarget sclerosis. The embolization can be repeated on the contralateral side if necessary or simultaneous bilateral treatment can be performed. Endovascular stenting has also been historically used to treat left iliac vein stenosis and resultant vulvar varices; however, a small study of 12 patients found that 83.4% of patients who underwent stenting also required adjunctive embolization due to persistent pelvic pain after treatment. 14 While there are different approaches, depending on the patients' symptoms, these procedures can be performed with balloon-occlusion catheters into the internal iliac veins and then visualizing the escape points into the lower extremities ( Fig. 1b ) if patients have associated pelvic pain symptoms. If patients present with localized pain into the perineum, vulvar areas, and the upper thighs, without significant pelvic pain, our preference is to perform direct puncture of varices as described later.
“Bottom-up” Approach
In our clinical practice, fluoroscopic and/or ultrasound guidance is used to directly access these veins, perform venography, and proceed with foam sclerotherapy. Fluoroscopic guidance is advantageous in that it is more amenable to close drug dose titration and control of the injection to the level of the normal pelvic veins, which reduces the risk of nontarget sclerotherapy. Injection can be manipulated manually by compression and guiding sclerosant to desired target. Our preferred sclerosant is a mixture of 1 to 3% sodium STS mixed with air at a 1:5 ratio, to produce a foam mixture using the Tessari technique. 24 Our preference is to have maximum volume of 10 mL of foam mixture injected per procedure. 25 Others have described using alternative liquid sclerosing agents such as Aethoxysklerol 1% (Kreussler Pharma, Wiesbaden, Germany) or Fibrovein 0.5% (STD Pharmaceutical products, Hereford, UK). Approximately 1.5 to 2 mL of sclerosing agent is injected into patients while in the supine position and manual compression of the injection site is held for 5 to 7 minutes. 3
Using sterile technique and ultrasound guidance in the “bottom-up” approach, a 21-G butterfly needle is used to directly access labial varices and/or the tributaries and veins connecting with the labial varices in the medial aspect of the thigh ( Fig. 3 ). After venous blood return is confirmed, a small injection of contrast is then injected under fluoroscopic guidance ( Fig. 3 ) to confirm connection with labial varices and to determine the volume needed to fill the veins. At this point, injection of sclerotherapy is then performed with fluoroscopic evaluation with the same volume of sclerosants. In a single-institution review of cases of vulvar varices over 14 years by Gavrilov, almost 20% (12/61) of nonpregnant patients with varicose veins of the pelvis and enlarged vulvar veins were treated with direct sclerotherapy. 3 These patients were selected for sclerotherapy if there was no evidence of connection between vulvar varices and the internal iliac vein and if varices were <6 mm in diameter. No patients had complications after receiving sclerotherapy, and 16.7% (2/12) of patients receiving sclerotherapy as primary treatment for vulvar varices had recurrence of disease 2 to 3 months after treatment; however, both patients with recurrence had also become pregnant shortly after sclerotherapy. 3 A 2022 review of 70 cases of fluoroscopically guided sclerotherapy for vulvoperineal varices by Abd El Tawab et al had a technical success rate of 100% with clinical improvement in all patients' symptoms. 26 If the appropriate patient is selected, direct sclerotherapy is an excellent and effective minimally invasive technique to reduce vulvar varices and associated symptoms, with minimal risk of complications. There has yet to be a randomized control trial formally assessing outcomes of treatment of uncomplicated vulvar varices with sclerotherapy.
Fig. 3.

“Bottom-up approach” to labial varices: treatment of labial varices with access to tributaries in the medial aspect of thigh with a 21-G butterfly needle (arrow).
Conclusions
Labial varices typically affect women during pregnancy; however, a subset of patients will have persistent symptoms necessitating treatment. Interventional treatments are minimally invasive and can be performed in conjunction with management of PeVD in selected patients (“top-down approach”). The majority of patients can be treated with direct puncture of varices using fluoroscopic and ultrasonographic guidance (“bottom-up approach”) with up to a 100% technical success rate and good clinical outcomes with proper patient selection.
Footnotes
Conflict of Interest None declared.
References
- 1.Fassiadis N. Treatment for pelvic congestion syndrome causing pelvic and vulvar varices. Int Angiol. 2006;25(01):1–3. [PubMed] [Google Scholar]
- 2.Antignani P L, Lazarashvili Z, Monedero J L et al. Diagnosis and treatment of pelvic congestion syndrome: UIP consensus document. Int Angiol. 2019;38(04):265–283. doi: 10.23736/S0392-9590.19.04237-8. [DOI] [PubMed] [Google Scholar]
- 3.Gavrilov S G. Vulvar varicosities: diagnosis, treatment, and prevention. Int J Womens Health. 2017;9:463–475. doi: 10.2147/IJWH.S126165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell D, Kane P B, Liang S, Conway C, Tornos C. Vulvar varices: an uncommon entity in surgical pathology. Int J Gynecol Pathol. 2007;26(01):99–101. doi: 10.1097/01.pgp.0000215304.62771.19. [DOI] [PubMed] [Google Scholar]
- 5.Giannouli A, Tsinopoulou V R, Tsitsika A, Deligeoroglou E, Bacopoulou F. Vulvar varicosities in an adolescent girl with morbid obesity: a case report. Children (Basel) 2021;8(03):202. doi: 10.3390/children8030202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan T A, Rudolph K P, Huber T S, Fatima J. May-Thurner syndrome presenting as pelvic congestion syndrome and vulvar varicosities in a nonpregnant adolescent. J Vasc Surg Cases Innov Tech. 2019;5(03):252–254. doi: 10.1016/j.jvscit.2019.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kachlik D, Pechacek V, Musil V, Baca V. The venous system of the pelvis: new nomenclature. Phlebology. 2010;25(04):162–173. doi: 10.1258/phleb.2010.010006. [DOI] [PubMed] [Google Scholar]
- 8.American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification . Eklöf B, Rutherford R B, Bergan J J et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(06):1248–1252. doi: 10.1016/j.jvs.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 9.Labropoulos N, Tassiopoulos A K, Gasparis A P, Phillips B, Pappas P J. Veins along the course of the sciatic nerve. J Vasc Surg. 2009;49(03):690–696. doi: 10.1016/j.jvs.2008.09.061. [DOI] [PubMed] [Google Scholar]
- 10.Ricci S, Georgiev M, Jawien A, Zamboni P. Sciatic nerve varices. Eur J Vasc Endovasc Surg. 2005;29(01):83–87. doi: 10.1016/j.ejvs.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Gavrilov S G, Moskalenko Y P, Karalkin A V. Effectiveness and safety of micronized purified flavonoid fraction for the treatment of concomitant varicose veins of the pelvis and lower extremities. Curr Med Res Opin. 2019;35(06):1019–1026. doi: 10.1080/03007995.2018.1552043. [DOI] [PubMed] [Google Scholar]
- 12.Kim A S, Greyling L A, Davis L S. Vulvar varicosities: a review. Dermatol Surg. 2017;43(03):351–356. doi: 10.1097/DSS.0000000000001008. [DOI] [PubMed] [Google Scholar]
- 13.Choudur H N, Joshi R, Munk P L. Inferior gluteal vein varicosities: a rare cause of sciatica. J Clin Rheumatol. 2009;15(08):387–388. doi: 10.1097/RHU.0b013e3181c427ff. [DOI] [PubMed] [Google Scholar]
- 14.Gavrilov S G, Vasilyev A V, Krasavin G V, Moskalenko Y P, Mishakina N Y. Endovascular interventions in the treatment of pelvic congestion syndrome caused by May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord. 2020;8(06):1049–1057. doi: 10.1016/j.jvsv.2020.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Francheschi C, Bahnini A. Treatment of lower extremity venous insufficiency due to pelvic leak points in women. Ann Vasc Surg. 2005;19(02):284–288. doi: 10.1007/s10016-004-0180-9. [DOI] [PubMed] [Google Scholar]
- 16.Greiner M, Dadon M, Lemasle P, Cluzel P. How does the patho-physiology influence the treatment of pelvic congestion syndrome and is the result long-lasting? Phlebology. 2012;27 01:58–64. doi: 10.1258/phleb.2011.012s07. [DOI] [PubMed] [Google Scholar]
- 17.Marcelin C, Le Bras Y, Molina Andreo I, Jambon E, Grenier N. Diagnosis and management of pelvic venous disorders in females. Diagnostics (Basel) 2022;12(10):2337. doi: 10.3390/diagnostics12102337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meissner M H, Khilnani N M, Labropoulos N et al. The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: a report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. J Vasc Surg Venous Lymphat Disord. 2021;9(03):568–584. doi: 10.1016/j.jvsv.2020.12.084. [DOI] [PubMed] [Google Scholar]
- 19.Lurie F, Passman M, Meisner M et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. 2020;8(03):342–352. doi: 10.1016/j.jvsv.2019.12.075. [DOI] [PubMed] [Google Scholar]
- 20.Scotti N, Pappas K, Lakhanpal S, Gunnarsson C, Pappas P J. Incidence and distribution of lower extremity reflux in patients with pelvic venous insufficiency. Phlebology. 2020;35(01):10–17. doi: 10.1177/0268355519840846. [DOI] [PubMed] [Google Scholar]
- 21.Maratto S, Khilnani N M, Winokur R S. Clinical presentation, patient assessment, anatomy, pathophysiology, and imaging of pelvic venous disease. Semin Intervent Radiol. 2021;38(02):233–238. doi: 10.1055/s-0041-1729745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartung O.Embolization is essential in the treatment of leg varicosities due to pelvic venous insufficiency Phlebology 201530(1, Suppl):81–85. [DOI] [PubMed] [Google Scholar]
- 23.Rabe E, Pannier F.Embolization is not essential in the treatment of leg varices due to pelvic venous insufficiency Phlebology 201530(1, Suppl):86–88. [DOI] [PubMed] [Google Scholar]
- 24.Xu J, Wang Y F, Chen A W, Wang T, Liu S H. A modified Tessari method for producing more foam. Springerplus. 2016;5:129. doi: 10.1186/s40064-016-1769-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanaka M E, Kutsenko O, Salazar G. Choosing the most appropriate treatment option for pelvic venous disease: stenting versus embolization. Semin Intervent Radiol. 2021;38(02):182–188. doi: 10.1055/s-0041-1727104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abd El Tawab K A, Hagag M AA, Khafagy R TM. Direct fluoroscopic-guided sclerotherapy for vulvoperineal varices: an experience in 70 patients. Arab Journal of Interventional Radiology. 2022;6(01):25–32. [Google Scholar]


