Abstract
Quantitative sensory testing (QST) is useful when analysing musculoskeletal pain disorders. A handheld algometer is most commonly used for pressure pain threshold (PPT) tests. However, reference intervals for PPTs are not elucidated. We assessed reference intervals of PPTs for QST in 158 healthy adult Japanese with no history of musculoskeletal or neurological problems. A handheld algometer was used to record PPT at five different assessment sites on the body: lumbar paravertebral muscle, musculus gluteus maximus, quadriceps, tibialis anterior muscle, and anterior talofibular ligament. Multiple regression analysis was performed to explore sources of variation of PPT according to sex, age, body mass index, UCLA Activity Level Rating, and Tegner Activity Score. Reference intervals were determined parametrically by Gaussian transformation of PPT values using the two-parameter Box-Cox formula. Results of multiple regression analysis revealed that age was significantly associated with PPT of lumbar paravertebral muscle and musculus gluteus maximus. In females, body mass index showed significant positive correlation with PPT of anterior talofibular ligament, and UCLA Activity Level Rating also showed significant positive association with tibialis anterior muscle and anterior talofibular ligament. Site-specific reference intervals of PPTs for Japanese are of practical relevance in fields of pain research using a handheld algometer.
Subject terms: Musculoskeletal system, Health care, Medical research
Introduction
In recent years, several published articles have shown that quantitative sensory testing (QST) is useful in the analysis of musculoskeletal pain disorders1–6. Based on the evidence from these studies, it is assumed that QST might be a useful tool in the analysis of the pathogenesis, classification, differential diagnosis, and prognosis of musculoskeletal pain1–6.
QST has become a common test in clinical neurophysiology units1–3. QST uses psychophysical tests defined as stimuli with predetermined physical properties based on specific measurement protocols for the analysis of somatosensory aberrations. QST measures responses to sensory stimuli and can be used to assess somatosensory system function, the measurement of altered peripheral and/or central pain sensitivity, and descending pain modulation4,5,7. Low back pain (LBP) is the most common musculoskeletal condition that evolves into chronic problems8,9. LBP patients with lumber disc herniation and/or lumbar spinal stenosis have also lower limbs pain because of the neurological symptoms5. L1 spinal nerve helps to move hip muscles. L2, L3 and L4 spinal nerves provide sensation to the front part of thigh and inner side of lower leg. L5 spinal nerve provides sensation to the outer side of your lower leg, the upper part of your foot and the space between your first and second toe. This nerve also controls foot and toe movements. Sciatic nerve from lumbar spine starts in rear pelvis and runs down the back of leg, ending in foot5,8,9. Therefore, we need to examine QST on the back, buttocks, femur, crus, and ankle in LBP patients (Fig. 1). However, the reference intervals of QST for LBP and lower limb radiculopathy are not available5.
Figure 1.
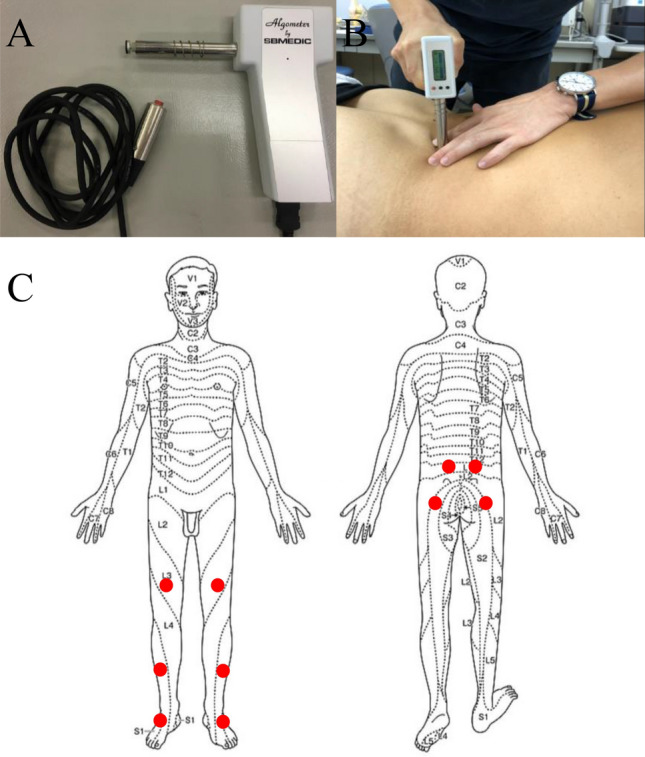
Handheld algometer and assessment of paravertebral muscles. (A) The handheld algometer used to assess pressure pain thresholds (PPTs). (B) Assessment of the paravertebral muscle. (C) Schematic of the body areas used for the analysis of PPTs. The assessment sites marked with red dots are as follows: (Top row) right and left lumbar paravertebral muscle at the level of iliac crest, 4 cm away from the spinal process; (Row 2) right and left musculus gluteus maximus, 5 cm below from iliac crest and 4 cm posterior to the posterior edge of the greater trochanter; (Row 3) right and left quadriceps, 10 cm proximal of the top of the patella; (Row 4) right and left tibialis anterior muscles, 5 cm distal and 3 cm lateral of the tibial tuberosity; (Bottom row) right and left of anterior talofibular ligament.
A handheld algometer (Somedic, Hörby, Sweden) mounted with a 1-cm2 probe is the most common algometer used to evaluate PPT (Fig. 1)3,5,10,11. No statistically-based reference interval (RI) determined from well-defined healthy subjects is available for use in QST assessment in Japanese patients with musculoskeletal pain. For this reason, establishment of an appropriate RI has been in dire need for detecting any pathological changes in QST measurements5. For this reason, reference interval data are needed for QST protocols to assess musculoskeletal pain disorder.
Chronic LBP has a major impact on a patient’s quality of life8,9. In this study, we measured PPTs at points on the back, buttocks, femur, crus, and ankle in healthy Japanese to objectively assess pain intensity for future pain assessment in patients with LBP. The aim of this study was to investigate the reference interval of PPTs, which is defined as the central 95% value of PPTs measured at various assessment sites in healthy individuals. In addition, possible factors causing variation of PPT measurements were investigated, such as sex, body mass index (BMI), daily activity, and sports activity in healthy Japanese. We also discuss the characteristics and the cautions when using Japanese PPT data for widespread use of PPTs in LBP treatment in general clinics.
Results
Factors affecting variation of PPT measurements
Results of multiple regression analysis (MRA) are shown in Table 1 after setting a threshold of practical significance (effect size) as |rp| ≥ 0.3. Age showed a significant association with PPT-PVMin the males and with PPT-PVM and PPT-MGM in the females. In addition, BMI showed a significant correlation with PPT-TLin the females. ALR, which reflects daily activities, also showed significant association with PPT-TA and PPT-TL in the females12.
Table 1.
Sources of variation of PPTs evaluated by multiple regression analysis.
| Exp para | n | R | Age | BMI | ALR | TAS | |
|---|---|---|---|---|---|---|---|
| Males | PPT-PVM | 85 | 0.521 | 0.542 | 0.055 | 0.235 | 0.086 |
| PPT-MGM | 85 | 0.317 | 0.238 | 0.142 | 0.167 | 0.075 | |
| PPT-QC | 85 | 0.465 | 0.268 | 0.290 | 0.027 | 0.192 | |
| PPT-TA | 85 | 0.374 | 0.287 | 0.177 | 0.136 | 0.103 | |
| PPT-TL | 85 | 0.316 | 0.151 | 0.185 | -0.073 | 0.214 | |
| Females | PPT-PVM | 73 | 0.571 | 0.598 | 0.138 | 0.173 | 0.197 |
| PPT-MGM | 73 | 0.402 | 0.440 | 0.114 | 0.020 | 0.275 | |
| PPT-QC | 73 | 0.396 | 0.254 | 0.299 | 0.185 | 0.007 | |
| PPT-TA | 73 | 0.393 | 0.220 | 0.207 | 0.319 | 0.039 | |
| PPT-TL | 73 | 0.454 | 0.017 | 0.388 | 0.361 | -0.133 |
Significant values are in bold.
PPT pressure pain threshold, Exp para experimental parameter, BMI body massindex, ALR UCLA Activity Level Rating, TAS Tegner Activity Score, PVM lumbarparavertebral muscle, MGM musculus gluteus maximus, QC quadriceps, TA tibialisanterior muscle, TL anterior talofibular ligament.
These findings are reflected in Fig. 2, which shows between-sex and between-age changes of PPTs at each assessment site. PPT-TL in the females positively correlated only with BMI (partial correlation coefficient: 0.388). PPT-TA and TL in the females were positively associated with ALR (0.319 and 0.361, respectively). There were no associations with PPTs andTAS, which reflected levels of sports activities13,14.
Figure 2.
Sex and age-related changes in pressure pain thresholds (PPTs) at the five testing sites. Reference values (RVs) of PPTs recorded at the five sites (lumbar paravertebral muscle [PVM], musculus gluteus maximus [MGM], quadriceps [QC], tibialis anterior [TA], and talofibular ligament [TL]) were subgrouped by sex and age at 40 years. The box in the centre of each scattergram indicates the mid 50% range of RVs, and its central vertical bar represents the median. The data size of each subgroup is shown at the right bottom of the group labels. On the top of each graph, the magnitudes of the between-group differences by sex or age are shown as the SD ratio (SDR), SDRsex or SDRage, respectively. SDRs that exceeded the threshold of 0.4 are marked in bold. The background green shading indicates the reference interval determined from all RVs without partition by sex or age. The x-axis range was fixed at 0–1400 kPa for all graphs to show the test site dependency of the PPTs.
Need for partitioning PPT reference values by sex and age
The above source-of-variation analysis by MRA revealed that there were significant sex and age differences in PPT depending on the assessment sites. To determine the need for partitioning reference values by sex and/or age, two-level ANOVA was performed. The magnitudes of between-sex and between-age variation were each calculated as a standard deviation ratio (SDR), SDRsex and SDRage, respectively52. By adopting 0.4 as a threshold for SDR, SDRsex50 was significant at the site of PPT-QC (0.520) and at that of PPT-TA (0.503), whereas SDRage was significant at the site of PPT-PVM (0.669) as shown in Table 2.
Table 2.
Reference intervals of PPTs.
| Item | Sex | Age | n | 90% CI of LL | Reference interval | 90% CI of LL | Variations of PPTs by sex and age | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | LL | Me | UL | Low | High | SDRsex | SDRage | ||||
| PPT-PVM | M/F | All | 158 | 229 | 273 | 250 | 539 | 1057 | 990 | 1107 | 0.000 | 0.669 |
| M/F | < 40 | 100 | 216 | 264 | 238 | 475 | 928 | 845 | 1032 | |||
| M/F | ≥ 40 | 58 | 296 | 385 | 324 | 665 | 1138 | 1033 | 1245 | |||
| M | All | 85 | 235 | 302 | 268 | 548 | 1037 | 968 | 1118 | |||
| F | All | 73 | 201 | 281 | 240 | 526 | 1101 | 963 | 1218 | |||
| PPT-MGM | M/F | All | 158 | 205 | 250 | 222 | 519 | 1095 | 1024 | 1185 | 0.119 | 0.357 |
| M/F | < 40 | 100 | 235 | 264 | 249 | 472 | 1090 | 945 | 1268 | |||
| MF | ≥ 40 | 58 | 115 | 250 | 155 | 614 | 1051 | 958 | 1134 | |||
| M | All | 85 | 189 | 265 | 225 | 564 | 1115 | 1000 | 1227 | |||
| F | All | 73 | 226 | 253 | 238 | 462 | 1087 | 966 | 1204 | |||
| PPT-QC | M/F | All | 158 | 160 | 191 | 174 | 366 | 682 | 643 | 716 | 0.520 | 0.322 |
| M/F | < 40 | 100 | 162 | 199 | 179 | 337 | 632 | 557 | 686 | |||
| M/F | ≥ 40 | 58 | 37 | 200 | 83 | 441 | 681 | 634 | 726 | |||
| M | All | 85 | 193 | 236 | 212 | 415 | 700 | 663 | 744 | |||
| F | All | 73 | 154 | 178 | 163 | 310 | 626 | 564 | 676 | |||
| PPT-TA | M/F | All | 158 | 166 | 214 | 204 | 455 | 900 | 849 | 943 | 0.503 | 0.336 |
| M/F | < 40 | 100 | 181 | 263 | 243 | 420 | 860 | 731 | 944 | |||
| M/F | ≥ 40 | 58 | 84 | 216 | 103 | 532 | 898 | 839 | 980 | |||
| M | All | 85 | 277 | 298 | 279 | 514 | 932 | 865 | 1000 | |||
| F | All | 73 | 141 | 202 | 169 | 379 | 831 | 719 | 907 | |||
| PPT-TL | M/F | All | 158 | 126 | 169 | 147 | 368 | 664 | 627 | 740 | 0.313 | 0.328 |
| M/F | < 40 | 100 | 145 | 199 | 164 | 343 | 616 | 577 | 732 | |||
| M/F | ≥ 40 | 58 | 66 | 175 | 126 | 416 | 715 | 620 | 780 | |||
| M | All | 85 | 196 | 235 | 216 | 390 | 743 | 657 | 826 | |||
| F | All | 73 | 71 | 147 | 115 | 336 | 620 | 553 | 687 | |||
PPT pressure pain threshold, CI confidence interval, LL lower level, UL upper level, Me medium, SDR standard deviation rate, PVM lumbar paravertebral muscle, M/F male and female, M male, F female, MGM musculus gluteus maximus, QC quadriceps, TA tibialis anterior muscle, TL anterior talofibular ligament.
*SDR threshold = 0.40, Unit; kPa.
Derivation of assessment site-specific reference intervals for PPT
The reference interval of PPTs at each assessment site was calculated as the lower limit (LL: 2.5% point), median (Me: 50% point), and upper limit (UL: 97.5% point) as listed in Table 2. For partitioning of reference values by age, we arbitrarily set 40 years as a mid-age range for boundary. When SDRsex or SDRage exceeded the threshold of 0.4049, corresponding reference intervals (LL ~ Me ~ UL) were marked in bold. Otherwise, reference intervals without partitioning were shown in italics as the default. Notably, the range of reference intervals was generally low for PPT-QC, PPT-TA, and PPT-TL, implying that between-individual variations of PPTs are narrow. In contrast, the range was wider for PPT-PVM and PPT-MGM. These site-specific differences in the variability of PPT measurements are also apparent from Fig. 2.
Discussion
QST is a formal variant of a time-honoured clinical examination technique in neurology. Currently, none of the neuropathic pain medications on the market have been developed based on prediction of treatment efficacy by QST. However, such an approach to the development of medicines has been encouraged by the European Medicines Agency15,16.
In the assessment of musculoskeletal conditions, clinicians often identify points of tenderness in superficial tissue15,16. The handheld algometer we used calculates PPT on superficial tissue that equate to one point of skin tenderness as found clinically when assessing a painful area16–20. It also includes measures of temporal summation by wind-up and documentation of dynamic mechanical allodynia18–23. When appropriate standards are applied, PPT can provide important and unique information about the functional status of the somatosensory system, which would complement already existing clinical methods20–22. Unfortunately, to our knowledge, reference intervals for the Japanese have never been reported using the handheld algometer for PPTs even though this measurement system is the most popular in the fields of pain research3,5,18–22. In addition, detection of PPT at the site of the most severe pain in patients with LBP was reported to be the most useful test in the assessment of hypersensitivity24.
Several studies of PPTs were reported previously in the study of LBP in western countries1,5,15,17–22,24–40. All of the studies used healthy control data to compare with the data of the patients with LBP15,23–37. PPT data using manual/electronic pressure algometry and cross-friction algometry in healthy control subjects from the lower back and QC or hip, gluteus maximus, or femur were reported. However, it was difficult to compare these studies’ results directly with our results because the algometry system itself was different from the instrument we used5,25–27.
In western countries, the data from healthy control subjects was reported at lumbar sites5,28. Lumbar PPT ranged from 299 to 628 kPa in the back area in these healthy control subjects5. However, the sample size was statistically too small to use the range as a reference interval for the PPT5. In the present study, we determined the reference intervals and sources of variation of the PPT for quantitative sensory testing by enrolling a larger number of healthy individuals, as shown in Table 2, which exceeded the minimum sample size of 120 recommended for determining reference intervals in the field of laboratory medicine29. The average values for all ages were as follows: PVM PPT-PVM, 539 kPa; PPT-MGM, 519 kPa; PPT-QC, 366 kPa; PPT-TA, 455 kPa; and PPT-TL, 368 kPa. We reviewed the previously published data in healthy control subjects measured by the instrument: The range of PPT at the lumbar area was 299–628 kPa, that at the gluteal areas was 535.9–863.97 kPa, and that at the lower leg was 321.8–771.5 kPa5,15,23–38. There were some differences between the articles depending on the volunteers’ backgrounds. However, these data may suggest differences in PPT in each race37: but more studies should be performed to confirm it.
The present study revealed the PPT at the PVM, MGM, QC, TA, and TL in healthy Japanese ranging in age from 19 to 59 years for the first time, to our knowledge (Table 2). It also revealed that the PPT at the PVM, MGM, QC, TA, and TL in healthy Japanese differed at each site, and these differences were influenced by sex, age, BMI, and ALR (Table 2). We show the characteristics of the PPT data for each site in Fig. 2. The variability of PPT-PVM and PPT-MGM was comparatively large, whereas that of PPT-QC, PPT-TA, and PPT-TL was small (Fig. 2, Table 2). These reference intervals should be used clinically with caution for patients with LBP.
Female participants showed higher pain thresholds for PPT-QC and PPT-TA compared to the male participants (Table 2). Females showed more tolerance than males for QST parameters, consistent with prior studies1,39–42. These sex differences in pain thresholds are unlikely to be due to peripheral factors such as innervation density and different central processing1,41,42.
In previous reports, obese individuals were more sensitive to pressure pain than individuals within a normal range of BMI43. Pain response varied according to subcutaneous body fat at different body sites43. However, PPT-TL in the females correlated only with BMI in the present study. Most of our participants were within the standard range of BMI, and therefore, we thought that our data showed a weak correlation between PPT and BMI only in the females.
PPT-TA and TL in the females were associated with ALR (correlation coefficients: 0.319 and 0.361, respectively). This result indicates that Japanese females with higher daily activity are more tolerant of lower leg pain. In addition, there was no association between PPT and the TAS, which reflects sports activities. We did not detect any correlation of PPT with sports and daily activity level in the healthy Japanese male volunteers. Previous articles revealed that exercise-induced hypoalgesia occurred following exercise. In addition, endocannabinoid levels were found to be elevated following exercise44–46. Our results showed a correlation between PPT and the questionnaire on activities only in the females of our study. We could not directly compare people with low activity to those with moderate or high activity because the participants basically all participated in moderate to slightly high activity levels of sports and daily activities, and no people with low activity were included.
The limitation of this study was relatively small sample size of healthy individuals recruited: n = 158. It was regarded as acceptable for determining the RIs without partitioning by sex and age. However, despite statistically significant between-sex and between-age differences in PPT, we could not reliably determine the RIs specific for each subgroup. It is certainly necessary to expand the scale of the study for better clinical usage of the RIs. The other limitation was that inter-rater reliability was not examined in this study. Therefore, we could only show the reference intervals for PPT in this study.
In summary, the present study determined the reference intervals of PPTs for the first time in healthy Japanese. In addition, we revealed that the PPTs at the PVM, MGM, QC, TA, and TL in healthy Japanese differed at each site and that these differences were influenced by sex, age, BMI, and ALR. Therefore, the above key points need to be taken into consideration when PPTs are measured in the assessment of patients with LBP. We hope that these data may become the reference intervals for the assessment of Japanese patients with LBP.
Conclusions
In this study, we determined test site-specific reference intervals for pressure pain thresholds in quantitative sensory testing in a healthy Japanese population. In addition, we showed that sex- and age-related differences in pressure pain thresholds also depend on the site of assessment. Consequently, in the clinical assessment of patients with low back pain, it is necessary to take into considerations that reference intervals of pressure pain thresholds differ according to the site of assessment and that the levels of pressure pain thresholds are influenced by sex, age, body mass index, and UCLA activity level rating. These findings may be of practical relevance in the fields of pain research using pressure pain thresholds measured by the handheld algometer in Japan.
Methods
Subjects
Participants in this study included 158 healthy Japanese subjects (73 females, 85 males; age, 35.2 ± 12.7 years [mean ± SD]; BMI, 22.3 ± 3.03 kg/m2) with no history of musculoskeletal or neurological problems. Participants were medical staff, medical doctors, rehabilitation staff, medical students and their families in our institution. None of the participants had (1) ongoing pain problems, (2) circulatory disorders, (3) a history of metabolic disease or neuropathy, (4) current use of prescription medications, including analgesics, tranquilizers, antidepressants, or other centrally acting agents, (5) diagnosed mental health disorders, (6) current pregnancy, (7) liver or kidney disease, and (8) disorders involving the neuroendocrine system. The subjects were given a detailed written and verbal explanation of the procedures for measuring PPT, and all signed an informed consent form. This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Boards of Yamaguchi University (H2020-169) in May 2020.
Experimental protocol
As the QST, the PPT was recorded 5 times at each of five pressure points (see below), and the average of the middle 3 scores, excluding the top and bottom score, was used for the data of pressure thresholds measured at each point (Fig. 1). A handheld algometer (Somedic, Hörby) mounted with a 1-cm2 probe (covered by a disposable latex sheath) was used to record the PPTs at 10 different locations on the body (Fig. 1). The investigator placed the handheld algometer on a site to be inspected and pressed against the tester in a vertical direction (Fig. 1). The investigator instructed the subjects to push the button by themselves when they felt slight pain. An interval of at least 20 s was kept between each assessment of a PPT. The PPT was defined for the subjects as “the time point at which the pressure sensation changed into pain.” Pressure was increased gradually at a rate of 30 kPa/s until the pain threshold was reached and the subject pressed a button3,10,11,47.
The assessment sites were as follows: (1) right and left lumbar paravertebral muscle (PVM) at the level of iliac crest, 4 cm away from the lateral side of spinal process; (2) right and left musculus gluteus maximus (MGM), 5 cm below from iliac crest and 4 cm posterior to the posterior edge of the greater trochanter; (3) right and left quadriceps (QC), 10 cm proximal of the top of the patella; (4) right and left tibialis anterior (TA), 5 cm distal and 3 cm lateral of the tibial tuberosity; and (5) right and left anterior talofibular ligament (TL). (1) and (2) assessments were in a prone position. (3), (4) and (5) assessments were in the supine position.
Questionnaires
We evaluated daily activity with the UCLA ALR12, which is a single-item 10-level scale, ranging from level 10, representing a highly physically active person, to level 1, a person who is dependent on others and unable to leave home.
We evaluated sports activity with the TAS, which was developed by Tegner and Lysholm in 198513. An activity level of 10–6 corresponds to participation in competitive and/or recreational sports, 5–1 corresponds to participation in recreational sports and heavy/moderate/light labour, and 0 is recorded for a person on sick leave or with a disability pension13,14.
Statistical analyses
Summary values for numerical parameters are presented as the mean and standard deviation (SD). To explore sources of variation of PPTs, MRA was performed, separately for each sex. The PPT at each location was set as an objective variable and age, BMI, ALR, and TAS as the explanatory variables. The contribution of each variable to prediction of the level of PPT was expressed by the standardized partial regression coefficient (rp), which corresponds to a partial correlation coefficient and takes a value between − 1.0 and 1.0. The practical significance was set to |rp| ≥ 0.30 guided by the medium effect size of Cohen for correlation coefficients (0.3)48. To evaluate the need for partitioning PPT values by sex and/or age, two-level nested ANOVA was performed, in which age was partitioned at 40 years. Variations of PPT by sex and age were computed as SDs, SDsex and SDage, respectively. The SDR was computed by dividing each by between-individual (residual) SD (SDind) as SDRsex = SDsex/SDind and SDRage = SDage/SDind, respectively. The threshold for SDR was set to 0.447. Reference intervals were determined parametrically after Gaussian transformation of the PPT by use of the two-parameter Box-Cox formula49,50:
where x and X denote a PPT value before and after transformation, and the parameters λ and α represent power and shift (or a start), respectively, of data distribution. Details of the computation are as described elsewhere51,52. All data were analysed using StatFlex Ver. 7 for Windows (Artec, Osaka, Japan; https://www.statflex.net/)51,52.
Acknowledgements
An appropriate use of up-to-date statistical methods was the key for successful derivation of reference interval in this study. In this regard, we are very grateful to Emeritus Prof. Kiyoshi Ichihara (the 11h coauthor) of Yamaguchi University Graduate School of Medicine, for his dedicated support in performing statistical data analyses as a biostatistician and a clinician who has been leading the international research on the topic of reference interval in general.
Abbreviations
- QST
Quantitative sensory testing
- PPT
Pressure pain threshold
- PVM
Pressure pain threshold
- MGM
Musculus gluteus maximus
- QC
Quadriceps
- TA
Tibialis anterior muscle
- TL
Anterior talofibular ligament
- MRA
Multiple regression analysis
- BMI
Body mass index
- ALR
UCLA activity level rating
- TAS
Tegner Activity Score
- LBP
Low back pain
- PPT-PVM
Pressure pain threshold at the area of lumbar paravertebral muscle
- MGM
Pressure pain threshold at the area of musculus gluteus maximus
- PPT-TL
Pressure pain threshold at the area of anterior talofibular ligament
- PPT-QC
Pressure pain threshold at the area of quadriceps
- PPT-TA
Pressure pain threshold at the area of quadriceps
- PPT-TL
Pressure pain threshold at the area of anterior talofibular ligament
Author contributions
H.S., S.T., K.U., and M.M. designed the study and collected the data; H.S., M.F., K.F., H.I., H.I., K.Y., K.S., and N.N. drafted the manuscript; K.I., and H.S. performed statistical analysis in this study. N.N. and T.S. critically reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministry of Health, Labour and Welfare FG Program Grant Number JPMH22FG2001.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rolke R, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): Standardized protocol and reference values. Pain. 2006;123:231–243. doi: 10.1016/j.pain.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 2.Courtney CA, Kavchak AE, Lowry CD, O'Hearn MA. Interpreting joint pain: Quantitative sensory testing in musculoskeletal management. J. Orthop. Sports Phys. Ther. 2010;40:818–825. doi: 10.2519/jospt.2010.3314. [DOI] [PubMed] [Google Scholar]
- 3.Arendt-Nielsen L, Yarnitsky D. Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J. Pain. 2010;10:556–572. doi: 10.2519/jospt.2010.3314. [DOI] [PubMed] [Google Scholar]
- 4.Timmerman H, Wilder-Smith OH, Steegers MA, Vissers KC, Wolff AP. The added value of bedside examination and screening QST to improve neuropathic pain identification in patients with chronic pain. J. Pain Res. 2018;11:1307–1318. doi: 10.2147/JPR.S154698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suzuki H, et al. Current concept of quantitative sensory testing and pressure pain threshold in neck/shoulder and low back pain. Healthcare. 2022;10:1485. doi: 10.3390/healthcare10081485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Georgopoulos, V. et al. Quantitative sensory testing and predicting outcomes for musculoskeletal pain, disability, and negative affect: A systematic review and meta-analysis. Pain160, 1920–1932. 10.1097/j.pain.0000000000001590 (2019). [DOI] [PMC free article] [PubMed]
- 7.Cruz-Almeida, Y. & Fillingim, R. B. Can quantitative sensory testing move us closer to mechanism based pain management? Pain Med.15, 61–72. 10.1111/pme.12230 (2014). [DOI] [PMC free article] [PubMed]
- 8.Matsudaira, K. et al. Potential risk factors of persistent low back pain developing from mild low back pain in urban Japanese workers. PLoS One 9, e93924. 10.1371/journal.pone.0093924 (2014). [DOI] [PMC free article] [PubMed]
- 9.Walker BF, Muller R, Grant WD. Low back pain in Australian adults: Prevalence and associated disability. J. Manip. Physiol. Ther. 2004;27:238–244. doi: 10.1016/j.jmpt.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Izumi, M. et al. Facilitated temporal summation of pain correlates with clinical pain intensity after hip arthroplasty. Pain158, 323–332. 10.1097/j.pain.0000000000000764 (2017). [DOI] [PubMed]
- 11.Izumi, M., Petersen, K. K., Arendt-Nielsen, L. & Graven-Nielsen, T. Pain referral and regional deep tissue hyperalgesia in experimental human hip pain models. Pain155, 792–800. 10.1016/j.pain.2014.01.008 (2014). [DOI] [PubMed]
- 12.Mørup-Petersen A, et al. Measurement properties of UCLA Activity Scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop. 2021;17:1–8. doi: 10.1080/17453674.2021.1977533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985;198:43–49. doi: 10.1080/17453674.2021.1977533. [DOI] [PubMed] [Google Scholar]
- 14.Briggs KK, Kocher MS, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J. Bone Joint Surg. Am. 2006;88:698–705. doi: 10.2106/JBJS.E.00339. [DOI] [PubMed] [Google Scholar]
- 15.Treede RD. The role of quantitative sensory testing in the prediction of chronic pain. Pain. 2019;160:S66–S69. doi: 10.1097/j.pain.0000000000001544. [DOI] [PubMed] [Google Scholar]
- 16.Lewis C, Souvlis T, Sterling M. Sensory characteristics of tender points in the lower back. Man. Ther. 2010;15:451–456. doi: 10.1016/j.math.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Andersen KG, Duriaud HM, Kehlet H, Aasvang EK. The relationship between sensory loss and persistent pain 1 year after breast cancer surgery. J. Pain. 2017;18:1129–1138. doi: 10.1016/j.jpain.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Arendt-Nielsen L, Egsgaard LL, Petersen KK. Evidence for a central mode of action for etoricoxib (COX-2 inhibitor) in patients with painful knee osteoarthritis. Pain. 2016;157:1634–1644. doi: 10.1097/j.pain.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 19.Arendt-Nielsen L, et al. A mechanism-based pain sensitivity index to characterize knee osteoarthritis patients with different disease stages and pain levels. Eur. J. Pain. 2015;19:1406–1417. doi: 10.1002/ejp.651. [DOI] [PubMed] [Google Scholar]
- 20.Arendt-Nielsen L, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur. J. Pain. 2018;22:216–241. doi: 10.1002/ejp.1140. [DOI] [PubMed] [Google Scholar]
- 21.Rolke R, et al. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain. 2006;10:77–88. doi: 10.1016/j.ejpain.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 22.González-Duarte, A., Lem-Carrillo, M. & Guerrero-Torres, L. Normative values of quantitative sensory testing in Hispanic Latino population. Brain Behav.6, e00466. 10.1002/brb3.466 (2016). [DOI] [PMC free article] [PubMed]
- 23.Seto T, et al. Three-dimensional analysis of the characteristics of joint motion and gait pattern in a rodent model following spinal nerve ligation. Biomed. Eng. Online. 2021;20:55. doi: 10.1186/s12938-021-00892-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neziri AY, et al. Ranking of parameters of pain hypersensitivity according to their discriminative ability in chronic low back pain. Pain. 2012;153:2083–2091. doi: 10.1016/j.pain.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 25.Marcuzzi A, Dean CM, Wrigley PJ, Chakiath RJ, Hush JM. Prognostic value of quantitative sensory testing in low back pain: A systematic review of the literature. J. Pain Res. 2016;9:599–607. doi: 10.2147/JPR.S115659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goubert D, Danneels L, Graven-Nielsen T, Descheemaeker F, Meeus M. Differences in pain processing between patients with chronic low back pain, recurrent low back pain, and fibromyalgia. Pain Physician. 2017;20:307–318. [PubMed] [Google Scholar]
- 27.Farasyn A, Lassat B. Cross friction algometry (CFA): Comparison of pressure pain thresholds between patients with chronic non-specific low back pain and healthy subjects. J. Bodyw. Mov. Ther. 2016;20:224–234. doi: 10.1016/j.jbmt.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Giesbrecht RJ, Battié MC. A comparison of pressure pain detection thresholds in people with chronic low back pain and volunteers without pain. Phys. Ther. 2005;85:1085–1092. doi: 10.1093/ptj/85.10.1085. [DOI] [PubMed] [Google Scholar]
- 29.IFCC and CLSI. C28-A3 Document. Defining, Establishing and Verifying Reference Intervals in the Clinical Laboratory: Approved Guideline, 3rd ed. Vol. 28 No. 30 (2008).
- 30.Corrêa JB, Costa LO, de Oliveira NT, Sluka KA, Liebano RE. Central sensitization and changes in conditioned pain modulation in people with chronic nonspecific low back pain: A case-control study. Exp. Brain Res. 2015;233:2391–2399. doi: 10.1007/s00221-015-4309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.den Bandt HL, et al. Pain mechanisms in low back pain: A systematic review with meta-analysis of mechanical quantitative sensory testing outcomes in people with nonspecific low back pain. J. Orthop. Sports Phys. Ther. 2019;49:698–715. doi: 10.2519/jospt.2019.8876. [DOI] [PubMed] [Google Scholar]
- 32.Blumenstiel K, et al. Quantitative sensory testing profiles in chronic back pain are distinct from those in fibromyalgia. Clin. J. Pain. 2011;27:682–690. doi: 10.1097/AJP.0b013e3182177654. [DOI] [PubMed] [Google Scholar]
- 33.Farasyn A, Meeusen R. The influence of non-specific low back pain on pressure pain thresholds and disability. Eur. J. Pain. 2005;9:375–381. doi: 10.1016/j.ejpain.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 34.Laursen BS, Bajaj P, Olesen AS, Delmar C, Arendt-Nielsen L. Health related quality of life and quantitative pain measurement in females with chronic non-malignant pain. Eur. J. Pain. 2005;9:267–275. doi: 10.1016/j.ejpain.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 35.O'Neill S, Manniche C, Graven-Nielsen T, Arendt-Nielsen L. Generalized deep-tissue hyperalgesia in patients with chronic low-back pain. Eur. J. Pain. 2007;11:415–420. doi: 10.1016/j.ejpain.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 36.O'Sullivan P, et al. Sensory characteristics of chronic non-specific low back pain: A subgroup investigation. Man. Ther. 2014;19:311–318. doi: 10.1016/j.math.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 37.Marcuzzi A, Wrigley PJ, Dean CM, Graham PL, Hush JM. From acute to persistent low back pain: A longitudinal investigation of somatosensory changes using quantitative sensory testing an exploratory study. Pain Rep. 2018;3:e641. doi: 10.1097/PR9.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mlekusch S, et al. Conditioned pain modulation in patients with acute and chronic low back pain. Clin. J. Pain. 2016;32:116–121. doi: 10.1097/AJP.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 39.Meints SM, Wang V, Edwards RR. Sex and race differences in pain sensitization among patients with chronic low back pain. J. Pain. 2018;19:1461–1470. doi: 10.1016/j.jpain.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tschugg A, et al. Gender differences after lumbar sequestrectomy: A prospective clinical trial using quantitative sensory testing. Eur. Spine J. 2017;26:857–864. doi: 10.1007/s00586-016-4891-8. [DOI] [PubMed] [Google Scholar]
- 41.Castro-Sánchez AM, et al. Gender differences in pain severity, disability, depression, and widespread pressure pain sensitivity in patients with fibromyalgia syndrome without comorbid conditions. Pain Med. 2012;13:1639–1647. doi: 10.1111/j.1526-4637.2012.01523.x. [DOI] [PubMed] [Google Scholar]
- 42.Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin. J. Pain. 2001;17:20–24. doi: 10.1097/00002508-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Tashani OA, Astita R, Sharp D, Johnson MI. Body mass index and distribution of body fat can influence sensory detection and pain sensitivity. Eur. J. Pain. 2017;21:1186–1196. doi: 10.1002/ejp.1019. [DOI] [PubMed] [Google Scholar]
- 44.Koltyn KF, Brellenthin AG, Cook DB, Sehgal N, Hillard C. Mechanisms of exercise-induced hypoalgesia. J. Pain. 2014;15:1294–1304. doi: 10.1016/j.jpain.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koltyn KF. Analgesia following exercise: A review. Sports Med. 2000;29:85–98. doi: 10.2165/00007256-200029020-00002. [DOI] [PubMed] [Google Scholar]
- 46.Koltyn KF. Exercise-induced hypoalgesia and intensity of exercise. Sports Med. 2002;32:477–487. doi: 10.2165/00007256-200232080-00001. [DOI] [PubMed] [Google Scholar]
- 47.Alahmari, K., Silvian, S. P., Ahmad, I., Reddy, R. S. & Kakaraparthi, V. N. Subjective and objective evaluation of pain for older adults with knee osteoarthritis in Saudi Arabia: A reliability study. Niger. J. Clin. Pract.7, 934–943. 10.4103/njcp.njcp_270_19(2020). [DOI] [PubMed]
- 48.Cohen, J. (1992). A power primer. Psychol. Bull.112, 155–159. [DOI] [PubMed]
- 49.Ichihara K. Statistical considerations for harmonization of the global multicenter study on reference values. Clin. Chim. Acta. 2014;432:108–118. doi: 10.1016/j.cca.2014.01.025;2014. [DOI] [PubMed] [Google Scholar]
- 50.Box GEP, Cox DR. An analysis of transformations. J. R. Stat. Soc. Ser. B. 1964;26:211–243. [Google Scholar]
- 51.Ichihara K, Kawai T. Determination of reference intervals for 13 plasma proteins based on IFCC international reference preparation (CRM470) and NCCLS proposed guideline (C28-P 1992: Trial to select reference individuals by results of screening tests and application of maximal likelihood method. J. Clin. Lab. Anal. 1996;10:110–117. doi: 10.1002/(SICI)1098-2825(1996)10:2<110::AID-JCLA9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 52.Ichihara K, Boyd J, IFCC Committee on Reference Intervals and Decision Limits (C-RIDL) An appraisal of statistical procedures used in derivation of reference intervals. Clin. Chem. Lab. Med. 2010;48:1537–1551. doi: 10.1515/CCLM.2010.319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.



