Abstract
Objective
The standard path of health education is a standardised health education method formulated according to the characteristics of the disease in question. This study aimed to explore the effect of traditional Chinese medicine (TCM) nursing combined with the health education standard path in terms of acute myeloid leukaemia (AML).
Methods
Sixty patients with AML at Shijiazhuang Ping'an Hospital were recruited and divided into the control group (n = 30) and the intervention group (n = 30). Both groups received the same chemotherapy treatment, while the control group received routine nursing and the intervention group received a combined TCM–health education standard path intervention. The scores for the self-rating anxiety scale (SAS), Spitzer quality of life index (QLI), self-rating depression scale (SDS), awareness of TCM health education standard path content and nursing satisfaction were then compared.
Results
The SAS and SDS scores of the patients decreased following the intervention, while the QLI score increased, with the intervention group significantly improved compared to the control group (P < 0.05). The awareness of TCM health education standard path content was significantly higher in the intervention group than in the control group (P < 0.05), and the nursing satisfaction was also higher in the former than in the latter (P < 0.05). Furthermore, the hospitalisation cost and length of stay were lower in the intervention group than in the control group (P < 0.05). There were no statistical differences in the median survival time between the intervention group and the control group (P > 0.05).
Conclusion
The application of TCM combined with the health education standard path has an effect in terms of reducing patients' anxiety and depression, improving their awareness of health education content and enhancing their nursing satisfaction.
Keywords: Acute myeloid leukaemia, Health education, Traditional Chinese medicine nursing
This study has been registered on the ClinicalTrials.gov website (https://clinicaltrials.gov/) (NCT05563207).
1. Introduction
Acute myeloid leukaemia (AML) is a common clinical haematological disease, with fever, haemorrhage and anaemia the main clinical manifestations. The attendant aetiology and pathogenesis are complex and have not yet been fully elucidated [1,2]. While chemotherapy can control the progression of AML to a certain extent, the procedure involves major adverse reactions and poor patient acceptance [3,4]. In fact, AML can cause strong psychological and physical stress reactions in patients, resulting in a decline in compliance with the treatment [5]. The negative emotions and reduced quality of life of AML patients are mostly related to the lack of disease-related knowledge, meaning health education plays an important role in improving the prognosis of such patients. Routine health education is largely completed between diagnosis and treatment and involves a lack of standardisation and an effect of publicity and education that is far from ideal. The standard path of health education is a standardised health education method formulated according to the characteristics of the specific disease, and it has played an effective auxiliary role in the treatment of various diseases [6,7]. The aim of this study was to observe the effect of the health education standard path combined with traditional Chinese medicine (TCM) in patients with AML, and to explore effective means for improving the life quality of patients.
2. Materials and methods
2.1. General information
All patients with AML who were treated at Shijiazhuang Ping'an Hospital from March 2021 to May 2022 were selected using a random sampling method. A final total of 60 patients were included. The patients were then divided into the intervention group (n = 30) and the control group (n = 30). The inclusion criteria were as follows: (1) patients admitted to the hospital for the first time; (2) patients diagnosed with AML [8]; (3) patients with a stable disease, clear consciousness, fluent speech and normal communication; (4) patients who were willing to participate in this study. The exclusion criteria included the following: (1) patients who were repeatedly admitted to hospital during the investigation period; (2) patients with a hospitalisation time of <3 days; (3) patients whose condition changed after admission and could not continue to cooperate with the study; and (4) patients who asked to withdraw during the intervention period. This study was approved by The Ethics Committee of Shijiazhuang Ping'an Hospital (ethics number: 202003). All patients and family members were informed about the study and signed a consent form. Ethics date:November 20, 2020.
2.2. Intervention methods
Both groups were given routine treatment administered by the same group of nursing staff.
2.2.1. Control group
The patients were provided with routine nursing content for health education, were closely observed during chemotherapy, were listened to regarding their chief complaints, with any questions raised answered, and were guided to follow the doctor's advice, while the nurses ensured that any complications, such as infection or bleeding, were prevented.
2.2.2. Observation group
The patients were given TCM nursing combined with health education path intervention. In terms of the TCM nursing, the observation group had increased TCM nursing based on routine nursing, with the following steps. (1) Bleeding nursing: bleeding may occur during AML treatment, and peppermint oil was used to deal with and stop any nasal bleeding. Gastrointestinal bleeding was appropriately dealt with according to the syndrome type, with an enema with Qingkailing used for patients with heat toxicity and fresh Rehmannia juice taken to cool the blood and to detoxify. Patients with stasis and toxin stagnation were treated with Sihuang Shuimi Powder for external application of lumps, taking Tufuling Huoxue Jiedu. (2) Diet intervention: the patients were advised to eat more light and nutritious food, as well as to consume hot foods, such as cattle, sheep and dogs, according to the dietary norms of TCM, to eat more foods such as fungi, red beans, poria cocos and jujube to nourish the qi and blood, and to avoid eating turtles and ginseng soup to prevent the proliferation of leukaemia clonal cells and to improve their prognosis. (3) Sleep care: once a day, the patient's Shen men, kidney and three sympathetic acupoints were selected, with 75% alcohol used to disinfect the auricle locally and the most sensitive point selected to insert the needle. In addition, pressure was applied to the acupoint using Vaccaria seed to promote the patient's sleep, with each acupoint pressed for around 0.5–1 min (4) Complications nursing: a massage was given to promote blood circulation and muscle growth and to prevent anaemia, with patients with anaemia guided to use blood-activating and blood-tonifying foods. In terms of patients experiencing gastrointestinal discomfort, the family members were instructed to massage the Zusanli, Sanyinjiao, Tianshu and other acupoints to improve gastrointestinal disorders and promote food digestion.
The contents of the health education path intervention included the following aspects. (1) Graphic and text education: the responsible nurse gained a comprehensive understanding of the patient's disease cognition and psychological state, and based on this, an individualised intervention plan was formulated. With the help of publicity boards, brochures and other forms of pictures and texts, the knowledge and precautions pertaining to disease treatment were disseminated. (2) Language education: a one-to-one method was adopted to inform the patients of the principles, effects and precautions of chemotherapy and to eliminate any misunderstandings, with the language education repeated a number of times during the treatment process to strengthen the patient's memory. (3) Psychological education: the patients were encouraged to express their emotions based on their specific personality and cultural background. After discussing the details with family members, the patient's actual condition was communicated. (4) Dietary education: the patients were advised to follow the principles of light, easy to digest and balanced nutrition. (5) Complication education: the patients were informed about the complications in advance, with guidance provided regarding the prevention methods, which include increasing water intake and avoiding activities involving the affected limbs following chemotherapy. In terms of any negative emotions, such as anxiety and depression, emerging in the patients alongside adverse reactions, such as vomiting and alopecia, corresponding measures were taken in a timely manner and the patient was comforted by being informed that this was a normal phenomenon, encouraging them to maintain a good attitude. The details of the treatment are presented in Fig. 1.
Fig. 1.
Flowchart of traditional chinese medicine health education standard path.
Nursing staff must actively learn and master the commonly used TCM nursing methods, especially the attendant decoction methods, acupuncture treatment methods, TCM massage techniques and the different TCM nursing methods. This should be done according to the patient's condition and treatment needs, with a traditional TCM diet and other methods adopted to ensure that the patient effectively cooperates with the clinical treatment. All patients were followed up until May 2022, and the survival of the patients was recorded.
2.3. Observation indicators and evaluation criteria
The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used to evaluate the anxiety and depression across all the patient groups [9]. An SAS score of >50 indicates that the patient is experiencing anxiety, and the scores are positively correlated with the degree of anxiety. An SDS score of >53 indicates that the patient is experiencing depression, with the scores positively correlated with the degree of depression.
Before and after the intervention, the Spitzer quality of life index (QLI) was used to evaluate the life quality of the patients [10]. The QLI comprises five dimensions and a total score of 10 points, with the scores positively correlated with the quality of life.
Self-made questionnaires were used to assess the awareness of TCM and the health education standard path content in view of evaluating the health guidance of medical staff and their grasping of the relevant knowledge of the patients. With reference to the relevant literature [11], the patient awareness scale for promotion and education content was compiled, which included five items: promotion and education content, a promotion and education form, professional level of promotion and education, nurses' professional attitude and the promotion and education effect. Here, 1 point was given for ‘awareness’ and 5 points for ‘awareness’, and the total score range was 5–25 points. The awareness survey was conducted when the patients were discharged from the hospital. The higher the overall mean score, the higher the patients' level of awareness.
Self-made questionnaires were used to assess the level of nursing satisfaction, which was evaluated in terms of nursing attitude, nursing skills and the explanations provided by medical staff. Here, a five-point Likert scale was used, with 1 point denoting ‘dissatisfied’ and 5 points denoting ‘satisfied’, for a total score range of 5–25 points. The patient satisfaction survey was conducted at the time of discharge and the overall mean score was positively correlated with the overall patient satisfaction.
2.4. Statistical methods
The data were analyzed using SPSS software (vers. 25.0). The count data (n [%]) were compared using a chi-square test, the measurement data ( ±s) following normal distribution and homogenous variance were compared using a t-test, with survival curves drawn according to the Kaplan–Meier method. A log-rank test was used for inter-group comparisons, with a P-value of <0.05 considered to be statistically significant. The SAS, SDS and QLI scores were expressed as mean ± SD ( ±s), with a t-test performed for comparisons.
3. Results
3.1. Comparison of basic information between the two groups
In the control group, there were 15 (50%) male and 15 (50%) female patients. The mean age was 49.73 ± 18.37 years, while the education level included six cases of junior high school and below, 10 cases of high school and 14 cases of junior college and above. In terms of marital status, one patient was unmarried, 27 were married and two were divorced. The mean course of the disease was 10.52 ± 3.42 days. Meanwhile, there were 18 (60%) males and 12 (40%) females in the intervention group. The mean age was 49.6 ± 19.09 years, while the education level included seven cases of junior high school and below, 10 cases of high school and 13 cases of junior college and above. In terms of marital status, two patients were unmarried, 26 were married and two were divorced. The mean course of the disease was 9.68 ± 3.52 days. There was no significant difference in the basic information between the two groups (P > 0.05), with the two groups deemed as comparable (Table 1).
Table 1.
Comparison of general data between the two groups.
| Variable | Control group | Observation Group | x2/t value | P value | |
|---|---|---|---|---|---|
| Sex | Male | 15 (50%) | 18 (60%) | 0.612 | 0.430 |
| Female | 15 (50%) | 12 (40%) | |||
| Age | 49.73 ± 18.37 | 49.6 ± 19.09 | 0.031 | 0.671 | |
| Course of disease | 10.52 ± 3.42 | 9.68 ± 3.52 | 0.849 | 0.398 | |
| Education level | Junior Secondary and below | 6 | 7 | 0.288 | 0.774 |
| High School | 10 | 10 | |||
| Junior College and above | 14 | 13 | |||
| Family situation | Unmarried | 1 | 2 | 0.771 | 0.856 |
| Married | 27 | 26 | |||
| Divorced | 2 | 2 | |||
| Widowed | 0 | 0 |
3.2. Comparison of anxiety and depression scores
There was no significant difference in SAS score (83.97 ± 6.33 vs 82.4 ± 6.33) or SDS score (81.5 ± 6.31 vs 81.43 ± 6.48) between the two groups before the intervention (P > 0.05). After three months of intervention, the SAS score (67.3 ± 8.33 vs 78.6 ± 6.11) and SDS score (62.83 ± 7.56 vs 75.67 ± 6.82) were significantly lower in the observation group than in the control group (P < 0.05). This indicated that the anxiety of the patients in the observation group had been effectively alleviated. In fact, the SAS score (83.97 ± 6.33 vs 67.3 ± 8.33) and SDS score (81.5 ± 6.31 vs 62.83 ± 7.56) of the intervention group decreased significantly, and the difference was statistically significant (P < 0.05) (Table 2). This indicated that the patients’ depression has been effectively alleviated.
Table 2.
Comparison of SAS and SDS scores before and after intervention ( ±s).
| Index | Time | Observation Group (n = 30) | Control Group (n = 30) |
|---|---|---|---|
| SAS Score | Before intervention | 83.97 ± 6.33 | 82.4 ± 6.33 |
| Three months after the intervention | 67.3 ± 8.33ab | 78.6 ± 6.11a | |
| SDS Score | Before intervention | 81.5 ± 6.31 | 81.43 ± 6.48 |
| Three months after the intervention | 62.83 ± 7.56ab | 75.67 ± 6.82a |
Note: A compared with the pre-intervention group, P < 0.05; B compared with the control group after 3 months of intervention, P < 0.05. SAS: self-rating anxiety scale; SDS: self-rating depression scale.
3.3. Evaluation of quality of life
Prior to the intervention, the neurological appearance score (0.56 ± 0.12 vs 0.58 ± 0.09), health status score (0.81 ± 0.07 vs 0.78 ± 0.11), support and help score (0.45 ± 0.11 vs 0.41 ± 0.13), psychological status score (0.24 ± 0.07 vs 0.25 ± 0.06) and activity ability score (0.54 ± 0.09 vs 0.52 ± 0.11) between the two groups were not significantly different (P > 0.05). After three months of intervention, the scores of both groups were higher than before the intervention, with the difference in neurological score (1.62 ± 0.22 vs 1.14 ± 0.26), health status score (1.58 ± 0.19 vs 1.23 ± 0.27), support and help score (1.26 ± 0.17 vs 0.96 ± 0.14), psychological status score (1.32 ± 0.26 vs 0.93 ± 0.17) and activity ability score (1.48 ± 0.21 vs 1.02 ± 0.24) of both groups statistically significant (P < 0.05) (Table 3). Overall, the implication is that the application of TCM nursing combined with the health education standard path can improve the quality of life of AML patients.
Table 3.
Quality of life ( ± s) of the two groups.
| Group | Time | The nerve face | Health status | Support help | Mental Health | Ability to move |
|---|---|---|---|---|---|---|
| Control Group (n = 30) | Before intervention | 0.58 ± 0.09 | 0.78 ± 0.11 | 0.41 ± 0.13 | 0.25 ± 0.06 | 0.52 ± 0.11 |
| After intervention | 1.14 ± 0.26 | 1.23 ± 0.27a | 0.96 ± 0.14a | 0.93 ± 0.17a | 1.02 ± 0.24a | |
| Observation Group (n = 30) | Before intervention | 0.56 ± 0.12 | 0.81 ± 0.07 | 0.45 ± 0.11 | 0.24 ± 0.07 | 0.54 ± 0.09 |
| After intervention | 1.62 ± 0.22ab | 1.58 ± 0.19ab | 1.26 ± 0.17ab | 1.32 ± 0.26ab | 1.48 ± 0.21ab |
Note: aP < 0.05 before intervention and bP < 0.05 after intervention.
3.4. Comparison of traditional Chinese medicine–health education standard path content awareness and nursing satisfaction
Among the 25 patients who had no awareness of health education content, 20 (80%) were in the control group and five (20%) were in the observation group. Among the patients who did have some awareness of the content of health education (n = 35), 10 (28.6%) were in the control group and 25 (71.4%) were in the observation group. The difference was statistically significant (χ2 = 15.43, P < 0.05) (Table 4).
Table 4.
Comparison of patients' awareness of health education contents.
| Group | Without informed consent (25) | Informed consent (35) | x2 value | P value |
|---|---|---|---|---|
| Control Group | 20 (80%) | 10 (28.6%) | 15.43 | <0.01 |
| Observation Group | 5 (20%) | 25 (71.4%) |
The number of dissatisfied people in the control group was 16 (53.3%), while the number in the intervention group was seven (23.3%). The number of satisfied people in the control group was 14 (46.7%), while the number in the intervention group was 23 (76.7%). The difference was statistically significant (χ2 = 5.71, P < 0.05) (Table 5). This indicates that the AML patients were satisfied with the treatment provided and that TCM nursing combined with the health education standard path helps to improve patient satisfaction.
Table 5.
Comparison of nursing satisfaction scores between the two groups.
| Group | Not satisfied | Satisfied | x2 value | P value |
|---|---|---|---|---|
| Control Group | 16 (53.3%) | 14 (46.7%) | 5.71 | 0.02 |
| Observation Group | 7 (23.3%) | 23 (76.7%) |
3.5. Comparison of hospitalisation costs and length of stay
The hospitalisation cost of the two groups was compared. The hospitalisation cost of the observation group (18,491.84 ± 7074.59 yuan) was significantly lower than that of the control group (21,886.14 ± 5669.18 yuan), with the difference statistically significant (t = 2.05, P < 0.05). The hospitalisation stay of the two groups was also compared and was found to be significantly lower in the observation group (18.67 ± 6.54 days) than in the control group (22.17 ± 6.20 days), with the difference statistically significant (t = 2.13, P < 0.05) (Table 6).
Table 6.
Comparison of hospital costs and number of days in hospital between the two groups.
| Variable | Control Group | Observation Group | t value | P value |
|---|---|---|---|---|
| Hospital costs (yuan) | 21886.14 ± 5669.18 | 18491.84 ± 7074.59 | 2.05 | 0.05 |
| Number of days in hospital | 22.17 ± 6.20 | 18.67 ± 6.54 | 2.13 | 0.04 |
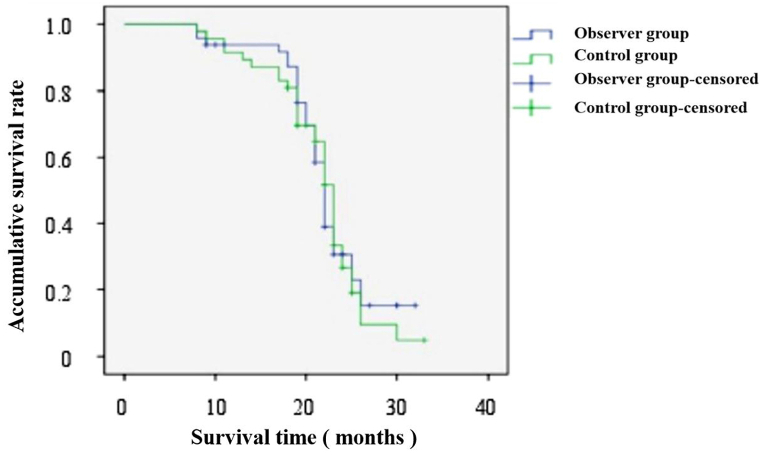
3.6. Comparison of survival conditions
As of May 2022, the median survival time of the patients in the intervention group and control group was 22 months (95% confidence [CI]: 21.25–22.75) and 23 months (95%CI: 22.02–23.98), respectively, with the difference not significant (χ2 = 0.039, P > 0.05) (Fig. 2). This suggests that TCM nursing combined with the health education standard path has no significant effect on the prognosis of AML patients, and more in-depth studies with a larger sample size are needed to further investigate the survival time.
Fig. 2.
Survival curves of acute myeloid leukaemia patients in intervention group and control group.
4. Discussion
Acute myeloid leukaemia is a high-incidence type of adult leukaemia, and the disease treatment cycle is long, with patients requiring long-term intermittent treatment [12]. Chemotherapy remains the main treatment for AML, but the prognosis is poor [13,14]. Serious adverse reactions during chemotherapy can directly lead to anxiety, depression and other emotions in patients, and the lack of knowledge regarding both the disease and the chemotherapy process will reduce the quality of life of the patients [15].
As a planned, purposeful and evaluative educational activity, health education can help patients better grasp disease-related knowledge and could promote healthier behaviour [16,17]. The conventional nursing method neglects the repeated promotion and education of the attendant information, with most patients having a low understanding of the disease and a lack of understanding of how to better protect themselves, resulting in a poor nursing effect. To explore better nursing methods, the hospital's TCM nursing health path provides nursing care, evaluates the patients' SAS and SDS scores and determines their awareness of health education and their satisfaction with the nursing. Better results are thus achieved.
The results indicated that following the intervention, compared to the control group, the SAS and SDS scores of the intervention group were lower (P < 0.05), indicating that the TCM– health education standard path could reduce the anxiety and depression of patients. Furthermore, the QLI was higher in the intervention group than in the control group (P < 0.05) following the intervention, suggesting that the TCM–health education standard path could improve the quality of life of patients. The health awareness and nursing satisfaction levels were also higher in the intervention group than in the control group (P < 0.05), which indicates that the TCM–health education standard path could improve the patients' trust in the nursing process. The hospitalisation cost and length of stay were both lower in the intervention group than in control group (P < 0.05), indicating that the TCM–health education standard path could reduce the costs and the length of stay. However, the results revealed that the median survival time of the intervention group and the control group were 22 months and 23 months, respectively (P > 0.05), which indicates that the TCM–health education standard path has no significant effect on the prognosis of patients with AML and has no advantage in terms of prolonging the survival time.
The TCM–health education standard path can help improve the anxiety, depression and life quality of patients with AML. This approach largely strengthens the patients' cognition of disease-related knowledge through text education, language education and other methods, such that the patients can master the correct knowledge to avoid unnecessary panic, alleviate any negative emotions and enhance the treatment cooperation. At the same time, it can also enable patients to master relevant self-care knowledge, such as diet and personal hygiene, as well as enhance their confidence in fighting the disease and obtaining a better quality of life.
This research involved a number of limitations and further studies need to be conducted to verify the results. Regarding the participants, only patients with a three-month admission were selected, meaning the sample was too small and was not fully representative. Furthermore, the patients’ educational level and attitude towards the disease may be confounding factors in this study. Finally, in terms of emotional assessment, simply using the SAS/SDS scores to assess the patients' emotions may not be sufficient enough for a comprehensive evaluation.
5. Conclusion
The combined TCM–health education standard path can help relieve the anxiety and depression of patients, improve their awareness regarding health education content and increase their satisfaction with the nursing, as well as reduce the cost and the length of the hospitalisation.
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Shijiazhuang Pingan Hospital (ethics number: 202003). Written informed consent was obtained from all participants.
Funding
This research did not receive any funding support.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
The mansuscript is not submitted for publication or consideration elsewhere.
Author contribution statement
(I) Conceived and designed the experiments: Jianhua Zhang. (II) Performed the experiments: Jing Ma, Qingqing Xie and Jianmei Li. (III) Contributed reagents, materials, analysis tools or data: Qingqing Xie, Linkang Zheng and Jianmei Li. (IV) Analyzed and interpreted the data: Jing Ma, Jianhua Zhang. (VI) Wrote the paper: All authors.
Data availability statement
No data was used for the research described in the article.
Declaration of interest's statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Clinical Trial: NCT05563207.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
References
- 1.Tachibana Takayoshi. Allogeneic hematopoietic cell transplantation in patients with acute myeloid leukemia that is not in remission. Rinsho Ketsueki. 2021;62(5):496–504. doi: 10.11406/rinketsu.62.496. [DOI] [PubMed] [Google Scholar]
- 2.Poor E., Chan Y.N., Iadonisi K., Tan K., Leak Bryant A. Exploring experiences of bereaved caregivers of older adult patients with acute myeloid leukemia. Clin. J. Oncol. Nurs. 2022;26(2):135–139. doi: 10.1188/22.CJON.135-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen F. Nursing care of a case of acute myeloid leukemia with frequent Aspen syndrome. Contemp. Nurse. 2021;(1):126–128. [Google Scholar]
- 4.Thol F., Ganser A. Treatment of relapsed acute myeloid leukemia. Curr. Treat. Options Oncol. 2020;21(8):66. doi: 10.1007/s11864-020-00765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valizadeh N. Treatment of refractory hemorrhagic cystitisafter hematopoietic stem cell transplantation in a case of acute myeloid leukemia with mesenchymal stem cell infu-sion. J. Appl. Hematol. 2018;(9):79–80. [Google Scholar]
- 6.Yin D. Effect of staged health education combined with follow-up on chemotherapy patients with acute leukemia. Nurs. Res. Pract. 2019;16(18):49–50. [Google Scholar]
- 7.Zhang K., Wang Y., Gui R., Yan X. Effects of cognitive behavioral intervention during the induction treatment for patients first diagnosed with acute leukemia. J. Nurs. 2019;34(13):82–84. [Google Scholar]
- 8.Ji N. Effects of nursing intervention on anxiety, depression and quality of life in patients with acute leukemia undergoing chemotherapy. Journal of Modern Integrative Medicine. 2016;25(18):2044–2046. [Google Scholar]
- 9.Yue T., Li Q., Wang R., Liu Z., Guo M., Bai F., et al. Comparison of hospital anxiety and depression scale (HADS) and zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236(2):170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 10.Rencz F., Szabo Á., Brodszky V. Questionnaire modifications and alternative scoring methods of the dermatology life quality index: a systematic review. Value Health. 2021;24(8):1158–1171. doi: 10.1016/j.jval.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Chen W., Gu J., Lai Y. Study on the effect of short animation in health education of ectopic pregnancy patients. Zhejiang Medical Education. 2021;20(5):48–51. [Google Scholar]
- 12.Luo R., Xie W., Liu Y., Zhang X., Liu Y. Development of evaluation index system for health education among adult acute leukemia patients with chemotherapy. Chin. J. Nurs. 2019;54(10):1482–1487. [Google Scholar]
- 13.Signorelli J., Luk S., Tavares E., Hobbs G.S. Antiemetic prophylaxis for induction chemotherapy in patients with acute myeloid leukemia. J. Oncol. Pharm. Pract. 2020;26(5):1213–1215. doi: 10.1177/1078155220918017. [DOI] [PubMed] [Google Scholar]
- 14.Lachowiez C., DiNardo C.D., Konopleva M. Venetoclax in acute myeloid leukemia - current and future directions. Leuk. Lymphoma. 2020;61(6):1313–1322. doi: 10.1080/10428194.2020.1719098. [DOI] [PubMed] [Google Scholar]
- 15.Vergara-Lluri M., Chan R.Y. Acute megakaryoblastic leukemia presenting as hemophagocytic lymphohistiocytosis. J. Pediatr. Hematol. Oncol. 2020;42(1):61–62. doi: 10.1097/MPH.0000000000001660. [DOI] [PubMed] [Google Scholar]
- 16.Zhu Z. Application value of health education standard path in nursing care of patients with acute leukemia during chemotherapy. China Primary Medicine. 2018;25(13):1745–1748. [Google Scholar]
- 17.Du W., Chen H., Qu J., Fu S. Influence of tertiary nursing quality control based on intelligent health management system on improving the will to survive and cooperation in diagnosis and treatment of leukemia patients. Int. J. Nurs. 2020;39(9):1535–1538. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
No data was used for the research described in the article.