Abstract
Globally, hundreds of millions of outdoor workers are exposed to solar radiation (SR) for most of their work. Such occupational exposure is known to induce various adverse health effects on the eyes, mainly related to its ultraviolet (UV) component. The present work is a call to action to raise awareness of the need for health surveillance to prevent chronic ocular diseases in outdoor workers. Photo-chemical chronic damage can induce pterygium at the eye’s outer layer and cataracts in the lens. Considering carcinogenic effects, rare squamous-cell tumors of the cornea and/or the conjunctiva and ocular melanomas are associated with UV radiation exposure. Solar UV-related eye diseases should be considered “occupational diseases” when workers have sufficient exposure. Still, they are often not recognized and/or frequently not reported to the national compensation authorities. Therefore, to prevent the burden of these work-related eye pathologies, an adequate risk assessment with identification of appropriate preventive measures and a provision of periodic health surveillance to the exposed workers, particularly those at higher risk of exposure or with individual susceptibility, should be urgently implemented.
Keywords: Solar Radiation, Ultraviolet Radiation, Optical Radiation, Occupational Exposure, Cataract, Pterygium, Macular Degeneration, Ocular Melanoma, Eye Tumors, Adverse Eye Effects
1. Introduction
Solar radiation (SR) is essential for human life and is related to various health benefits, such as reducing the risk of rickets, osteoporosis, and possibly other diseases due to its effect on vitamin D activation [1-3]. However, SR exposure is also a well-known health risk for outdoor workers (OW): the components of SR, i.e., ultraviolet (UVR), visible and infrared radiation (IR), defined as ‘optical radiation’ (OR), can have a significant health impact in particular on the eyes and the skin of the workers. Fortunately, the most hazardous UVR bands, i.e., all the UV-C and the majority (about 95%) of the UV-B, are absorbed within the stratospheric ozone layer before reaching the Earth’s surface (Table 1) [4].
Table 1.
Optical radiation bands within solar radiation at the Sun vs. Earth’s surface and ocular exposure [4-5].
| Classification | Sub-class/Wavelength (nanometers) | Emitted by the Sun | Reaches the Earth’s surface | Reaches the outer layers of the eye | Reaches the lens | Reaches the retina |
|---|---|---|---|---|---|---|
| ULTRAVIOLET (UV) | UV-C/100–280 | Yes | No | Yes1 | No | No |
| UV-B/280–315 | Yes | Only 5% | Yes | Yes | No | |
| UV-A/315–400 | Yes | Yes | Yes | Yes | Yes2 | |
| VISIBLE | from violet to red/400-780 | Yes | Yes | Yes | Yes | Yes |
| INFRARED (IR) | IR-A 780–1400 | Yes | Yes | Yes | Yes | Yes |
| IR- B/1400–3000 | Yes | Yes | Yes | Yes | No | |
| IR-C/3000-1000000 | Yes | Yes | Yes | No | No |
1 Only potentially, as there is no ocular exposure to solar UV-C at the Earth’s surface.
2 Only a small percentage, depending on age and on lens transparency, of UV-A with wavelengths around 390-400 nm able to reach the retina.
Occupational exposure to OR may derive from artificial (e.g., welding arcs) and natural sources. However, SR is probably the most widespread occupational exposure in terms of the number of workers exposed worldwide, i.e., all those performing outdoor activities or mixed indoor/outdoor jobs. Moreover, the sun is also the potentially most harmful occupational OR source due to the high exposure levels received by OW, resulting in a significant burden of several SR-related diseases [2, 4].
When SR reaches a human subject, its components can interact with the biological tissues, determining an effect based on the: (a) type of radiation (i.e., the specific classes and sub-classes of OR involved, related to the intrinsic characteristics of the radiation, including its energy), (b) intensity, duration and frequency of the exposure and (c) characteristics of the exposed biological tissue/body part concerning its specific interaction with the radiation [2, 4]. Due to the relatively low penetration ability of OR compared to other types of radiation, these effects mainly involve the skin and the eyes [2, 4].
The purpose of this review is to present a call to action in order to implement health surveillance for OW exposed to SR. We focus on the issue of the prevention of possible adverse ocular effects, considering that many efforts have been made in recent years to raise awareness on the problem of the prevention of skin cancers affecting OW, while SR-related eye diseases of the workers are still under-recognized. Only long-term effects are specifically addressed here, as short-term effects result from acute exposures to high levels of SR, usually representing accidental exposures. These effects cannot be prevented with health surveillance, which can only detect and monitor the phenomena, while for prevention purposes, other technical and organizational measures, as well as workers’ information and training, can be implemented. According to the International Labour Organization (ILO) and the International Commission on Occupational Health (ICOH), health surveillance includes the “…procedures and investigations to assess workers’ health in order to detect and identify any abnormality…” and its objectives must be clearly defined. These procedures have to be implemented and applied in all the working situations where a relevant occupational risk for the health of the exposed workers exists, and the health surveillance program must be tailored to the specific occupational risk considered and consistent with available scientific evidence and good practice [6-7]. According to these premises, the scientifically demonstrated biophysical mechanisms explaining the chronic SR exposure-related ocular damages will be presented in the following sections of this review. This will allow an evidence-based recognition of the long-term non-carcinogenic and carcinogenic effects, recently identified in various systematic reviews, that need to be investigated within a good health surveillance program. Finally, we will also discuss the specific contents of health surveillance for the prevention of long-term adverse eye effects occurring in OW exposed to SR, giving the currently available indications and inserting health surveillance in the context of the other applicable preventive measures to deal with the SR-exposure risk for the eyes at the workplace.
2. Solar Radiation Exposure of the Eyes and Adverse Effects: The Mechanisms Involved
The effects of SR exposure at the eye, similar to what happens to the skin, can be related to photochemical or thermal mechanisms. The former relates to the interactions of OR bands with specific molecules in the eye tissues, determining chemical reactions, possibly resulting in short-term and long-term ocular damage. On the other hand, thermal effects related to SR exposure are mainly acute effects, possibly occurring only after very intense and focused exposures, as a consequence of a significant increase in the temperature of the eye tissues [2, 4, 8-11]. In the case of UVR exposure, the effects are almost exclusively photochemical, while for IR exposure, the mechanisms involved are thermal, and in the case of exposure to visible light, both mechanisms can be crucial. In particular, photochemical effects can be more relevant for visible radiation with wavelengths between 400 and 550 nanometers, while thermal mechanisms are more typical of wavelengths between 600 and 700 nanometers [2, 4, 8-9].
The effects of OR exposure can appear in the eye’s target regions where the specific OR band is absorbed (Table 1, Figure 1). For example, UV-C is absorbed mainly at the ocular surface (however, this UV band does not reach the Earth’s surface within SR), while UV-B and UV-A are absorbed in the ocular surface and the crystalline lens. A small amount of UV-A (approximately 1-2% on average, depending on age, higher during childhood and lower at older ages) is also absorbed in the retina. The retina absorbs visible radiation and IR-A, while IR-B and IR-C mainly interact with the ocular surface, with the remaining IR-B absorbed by the lens (Figure 1) [2, 4, 8-9]. When considering how the different OR bands reach the eyes, it must be noted that various anatomical and physiological protections prevent excessive OR exposure, allowing good vision and decreasing the amount of harmful radiation absorbed by the eyes’ structures. Firstly, the frontal and orbital bones of the skull provide anatomical protection, particularly against overhead OR exposures. Also, eyelashes, eyelids, and eyebrows have a significant protective function.
Figure 1.
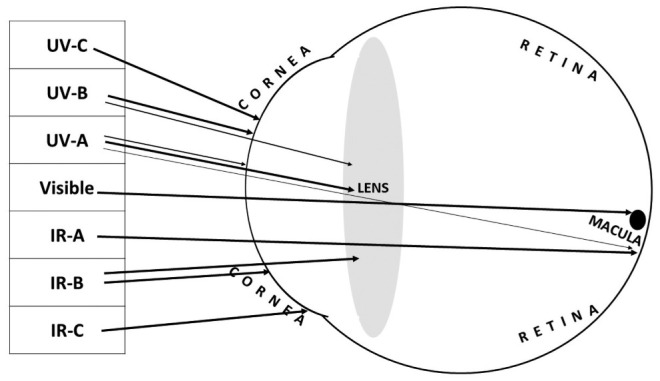
Penetration of the different components of optical radiation into the eye.
Moreover, various involuntary ocular reflexes defend the eyes from intense direct OR exposures, e.g., squinting and aversion responses, occur in a few fractions of a second [2, 4, 8-9]. The pupillary reflex is probably one of the most critical reflexes as, depending on the light intensity, there is the regulation of the pupil’s diameter, increasing the amount of OR reaching the macula when light is scarce (mydriasis) and decreasing it when light is more intense (miosis). This reflex is specifically aimed at providing good vision under different illumination conditions, but it is also a suitable defense mechanism from excessive retina exposure to hazardous OR components [4, 9-10].
As introduced above, the effects of OR can be based on thermal or photochemical mechanisms. Thermal effects are due to an increase in the temperature of the eye, with adverse health effects only occurring if the energy has sufficient power. Otherwise, the tissue dissipates the heat with no health consequences [8]. For these reasons, the thermal effects of OR within the eye are mainly acute and more typical after exposure to artificial sources that can focus high energies on small regions of the eyes, e.g., in case of accidental exposure to LASERs [11]. These exposures can result in ocular thermal burns involving superficial and inner structures, such as the retina [8, 11]. It should be noted that, in the case of SR exposure, thermal retinal damage may occur when people directly look at the Sun for long periods without adequate protection, e.g., during partial solar eclipses [12].
On the other hand, photochemical effects are mainly related to the action of the photons, being absorbed by specific target chromophores in the different eye structures (Figure 1). Photochemical effects can result from intense short-term exposures and repeated exposures exerting chronic damage (i.e., inflammation, DNA mutations, formation of reactive oxygen species, protein denaturation, etc.) over many years [2, 4, 9, 13]. The acute effects of UV exposure mainly involve the ocular surface, particularly the cornea and the conjunctiva. Intense exposure to unprotected eyes can induce a photochemical lesion with acute and painful inflammation, redness, and photophobia, called photo keratitis and photo conjunctivitis, often presenting together [2, 4, 9, 13]. In contrast to thermal burns, UV-related injuries involve a latency period before appearance (usually about 30 minutes for the eyes). The reason is that UV rays need sufficient time to interact with the biological tissues and, in particular, with the chromophores inside the corneal and conjunctival cells, inducing the disruption of chemical bonds and the formation of new chemical bonds as a result of the energy released by the photons, therefore initializing the inflammation process [2, 4, 9, 13]. The massive penetration of UV rays in the eyes only happens when the visible component of the OR arising from the same exposure source is not sufficiently intense to cause glare and trigger consequent defense mechanisms of the eye. This can happen, for example, when UV rays are reflected by white or polished surfaces to penetrate the eyes, while direct exposures are shielded [2, 4, 9, 13]. Photo keratitis and photo conjunctivitis are possible on fresh snow surfaces [14] because of their high UV reflectance. Another possibility is using protective equipment such as eyeglasses or masks not explicitly designed for filtering the different UV components. In these cases, even if the equipment blocks a fraction of the OR, some bands of the UVR can reach the ocular surface, potentially causing acute damage.
Nevertheless, it should be noted that, in the case of SR exposure, these events are improbable, as all plastic lens materials block the most energetic UV-B component and some UV-A, and many are treated to extend the blockage to near 400 nm. Meanwhile, glass lenses are less effective in blocking near UV if not adequately integrated with specific filters, and so are rarely used, especially in occupational settings, but even these materials can block most UV-B. Photoretinitis is another possible result of acute ocular exposure to SR. This is a photochemical lesion in the retina induced by UV-A and short-wavelength visible light (“blue light”) [4, 8-9, 13-15]. It is unlikely to occur in OW since it requires affected individuals to stare directly at a very intense source like the Sun (e.g., eclipse retinopathy) for an extended period.
As noted earlier, photochemical effects are also possible due to long-term exposure: this is called the reciprocity rule of photobiology, known as the Bunsen-Roscoe law [16]. This is why OWs exposed to SR, mainly because of its UV component, are not only at risk for acute ocular effects that, according to a medico-legal definition, are occupational injuries but are also more likely to develop long-term adverse eye effects related to SR exposure.
3. Non-Carcinogenic Chronic Adverse Eye Effects Related to Long-Term Occupational Solar Radiation Exposure
The main non-carcinogenic long-term adverse eye effects induced by SR exposure that are preventable include pterygium for the ocular surface, cataracts for the lens, and, possibly, as the evidence level is still considered insufficient, macular degeneration for the retina [2].
The photochemical damage related to cumulative SR exposure, and in particular to its UV component absorbed at the ocular surface (i.e., cornea, conjunctiva), can determine a chronic inflammatory stimulus inducing pathological alterations with abnormal growth of the corneal and conjunctival cells [10, 17]. This may result in various diseases, some more likely to present as aesthetic alterations with no clinical relevancy, such as pinguecula [18]. However, others are more severe and potentially affect visual function if not treated, such as pterygium, abnormal growth of the conjunctiva from the nasal angle of the eye to the center, and finally, covering the cornea [19].
Pterygium prevalence is significantly higher among male subjects, who are more likely to perform outdoor work compared to females. In general, the reported prevalence estimates are highly variable, primarily depending on the latitude of the study’s location. However, it is generally agreed that a higher disease prevalence correlates with lower latitudes, ranging, according to a recent systematic review, from 2.5% to 52% in the adult populations included [20]. Overall, outdoor work was strongly associated with the occurrence of pterygium, with research reporting significantly increased odds ratios in almost all the studies published on this topic [20], reaching values up to a 4-fold increased likelihood of OW developing the disease compared to indoor workers [20-21]. Another possible result of high-level chronic exposure to solar UV is decompensation of the cornea, in which loss of corneal endothelial cells breaks down the mechanism that maintains dehydration of the corneal stroma. These observations were reported for welders and some OW several years ago, while currently, the increased standards for eye protection seem to have significantly reduced the occurrence of these UV-related corneal disorders [22].
Penetrating through the ocular surface, the UV component of SR, mainly UV-A but also a fraction of UV-B [23], can induce long-term photochemical damage of the lens based on photo-oxidative mechanisms resulting in a UV-induced cataract [24]. There is solid mechanistic and experimental evidence suggesting that UVR induces cataracts through photo-oxidation and inflammatory response pathways, as well as through causing DNA damage. Animal studies also support a causal effect of UVR in the development of cataracts. In addition, epidemiological studies have shown strong support for an association between personal solar UVR exposure and the development of cortical cataracts and possibly other forms [23-24]. According to the World Health Organization (WHO), in 2006 the population-attributable fraction of cortical cataracts associated with SR was 25% [2].
Moreover, within its global health estimates of the total disease burden due to SR exposure, the WHO calculated a loss of 529.242 DALYs globally from cataracts attributable to solar UVR, with higher proportions of cortical cataracts at lower latitudes [2]. These estimates only covered cortical cataracts: more recently, new evidence also emerged showing a positive association between the performance of outdoor work with SR exposure and the development of nuclear cataracts [25], while other forms with posterior subcapsular opacities seem more related to lens damage induced by other types of radiation, particularly those which are ionizing in nature [26]. When it is considered that cataract is the leading cause of blindness worldwide, along with the significantly increased risk for OW of developing lens opacities [25], the WHO, together with the ILO, recently included solar UVR-induced cataract as one of the outcomes addressed in their joint project for estimating the work-related burden of various diseases [27].
Finally, another non-carcinogenic chronic eye disease should be mentioned here: age-related macular degeneration (AMD), currently the most important cause of vision loss in adults above 50 in high-income countries [28]. A hypothesis states that chronic photo-oxidative retinal damage is one of the main pathogenic pathways inducing degenerative disease [29]. In addition to UVR, as highly energetic blue light can induce photo retinitis, it may be supposed that chronic blue-light-related photochemical damage of the macula may play a role in the development of AMD [30]. Moreover, it should be noted that SR reaching the retina includes a small amount of UV-A in addition to blue light [15, 31]. Although the experimental evidence demonstrating AMD induction after long-term SR exposure is still considered inadequate, several epidemiological studies show AMD associations with outdoor work performance. A recent systematic review found ten studies with significantly increased odds ratios up to a 3-fold increased likelihood of developing AMD due to outdoor work [32].
4. Carcinogenic Eye Effects Related to Long-Term Occupational Solar Radiation Exposure
Eye tumors are rare, with two main groups related to SR exposure considered relevant for prevention purposes: epithelial tumors of the ocular surface and melanoma of the eye [33].
Regarding epithelial tumors, corneal and conjunctival squamous cells can develop carcinomas similar to the skin. Although extremely rare, research has demonstrated that epithelial tumors are associated with cumulative solar UVR exposure [33]. The incidence rates of these cancers (i.e., < 1 case per million people in Europe) are low for sufficient statistical power to perform epidemiologic studies in groups of OW, which are therefore lacking [33-34]. Nevertheless, various reports indicate that squamous cell carcinomas of the cornea and the conjunctiva show an increased incidence in countries at lower latitudes, such as African countries and Australia compared to Europe and the USA [34]. Among the few available epidemiological studies investigating possible risk factors for epithelial eye tumors, Lee et al. found an increased odds ratio of 7.5 (CI 95% 1.8-30.6) for chronic SR exposure, in particular at younger ages for those living 30° or less from the equator [35].
Although melanoma of the eye is rare (incidence <10 cases per million people), it is the most frequent intraocular malignancy among adults. This cancer is more frequent and aggressive than corneal and conjunctival carcinomas, with an increased risk of metastasis [33-34]. Intraocular malignant tumors have been reported as possibly associated with UV exposure, particularly in welders [33, 36]. Still, an increasing number of studies suggest a possible association with excessive SR exposure [33-34]. Nevertheless, as is the case with skin melanoma, which is believed not to be associated with cumulative UVR but only with repeated sunburns, there is still some scientific debate on the association of ocular melanoma with cumulative SR exposure, typical of OW [37].
5. Prevention of the Ocular Damage Related to Occupational Solar Radiation Exposure: A Focus on Health Surveillance
Considering the prevention of ocular damage related to occupational SR exposure, the usual approach includes a risk evaluation and, based on it, the implementation of adequate protective measures and health surveillance of exposed workers.
Risk evaluation of outdoor worker exposure to SR generally consists of estimating or measuring personal SR exposures of workers and comparing these to accepted occupational exposure standards. The standards produced by the ACGIH and ICNIRP provide ‘acceptable’ exposure limits for the prevention of acute and chronic eye conditions [13, 38]. Measurement of personal SR exposure of OW can be undertaken using a variety of techniques, including plastic film dosimeters [39], biological dosimeters [40], and electronic dosimeters [41]. However, these measurements primarily describe skin exposure, whereas there is a range of additional factors influencing ocular SR exposure. As such, ocular SR exposure has been assessed in a series of studies using dosimeters attached to manikins [42], sunglasses of OWs [42-43], and purpose-designed SR dosimeter contact lenses [44]. These studies have assessed SR exposure at the eye’s surface and reported their results in terms of an ‘Ocular Ambient Exposure Ratio’ (OAER, i.e., the proportion of ambient SR which reaches the eye). The reported OAERs have varied dramatically from 4% to 46% [27], with an average annual OAER of 13% considered representative across job categories and seasons [45]. As such, to complete a risk evaluation for ocular SR exposure, the OAER is applied to personal SR exposure measurements, and these are then compared with the occupational exposure standards to determine whether there is an elevated risk of adverse eye conditions. Nevertheless, there is still a lack of data on ocular SR exposures in the occupational setting, and this may limit the possibilities of an adequate risk evaluation and detailed epidemiological research on the associations between work exposures to various OR components and eye damage.
Adequate preventive measures, including those aimed at the collective and the individual implementing these measures, should be coordinated through a Sun Safety Program, part of a workplace’s Occupational Health and Safety Management System [46]. Considering SR exposure as an occupational risk factor, collective prevention can be provided with engineering and administrative controls. A fundamental collective measure for prevention is the adequate information and training of the workers on the risks and their reduction. Technical interventions include the coverage and shading of the outdoor workplaces to reduce the amount of harmful OR directly reaching the skin and the eyes of the workers. All the artificial and natural surfaces in the work environment must also be evaluated based on the albedo properties of the specific materials: as anticipated, the eyes are naturally protected from overhead exposure. At the same time, reflections are a relevant issue that must be prevented [46-48]. Considering organizational measures, these usually consist of the provision of (i) work breaks to be spent indoors or at least under well-shaded areas; (ii) modification of the working hours according to the season of the year (e.g., in summer, starting earlier in the morning and avoiding, or at least significantly reducing, the work activities during the central hours of the day when the UV index is ≥3); and (c) rotation of the exposed personnel. Individual protection mainly includes using personal protective equipment (PPE) [46-48]. Regarding ocular SR exposure, appropriate PPE includes eye protection and hats [49-50]. Sunglasses adequate for use at the workplace should comply with the requirements of standards for PPE [51-52], both in terms of the ability of the lens to properly filter all the harmful OR bands included in the SR spectrum, especially UVR (with appropriate labeling on the PPE), and of the shape of the sunglasses. Good sunglasses must have ample and properly shaped lenses that can be worn close to the eyes to enhance their protective function and prevent SR exposure from overhead or the side, and wide temples to protect the skin close to the eye. Moreover, the lenses must be appropriate for the specific type of activity performed: e.g., able to resist chemical or physical agents if needed, break and scratch resistant, anti-glare, etc. [46-48].
The choice of appropriate head covering depends on the type of occupational outdoor activity. In agriculture and fishing sectors, for example, broad-brimmed or legionnaire hats can shield the forehead and eyes appropriately. In the construction sector, workers must wear safety helmets that, for better protection against the risk of excessive SR exposure, can be larger on the front to shield the forehead and supplied with brim attachments to protect the ears and neck [46-48].
Moreover, as introduced above, to improve prevention, in case of residual risk after the assessment process and the implementation of other preventive measures, a specific health surveillance program should be set up for the exposed workers. It is uncommon to see health surveillance programs addressing OW to prevent SR-induced adverse eye effects [46]. In many countries, recent increased awareness of the need to protect OW from harmful SR exposure has been reported. However, the focus of these health surveillance activities is generally related to preventing possible adverse skin effects [48]. One of the main challenges in fully recognizing SR as an occupational risk factor is the unavailability, in the vast majority of the countries of the world, of regulations that identify an occupational exposure limit for SR, with this providing different considerations for ocular and skin exposures [27].
Another fundamental element for preventing SR-related adverse eye effects is the need to identify workers belonging to susceptible groups, which may be more susceptible to developing ocular and skin diseases, and therefore deserving of focused attention during preventive health surveillance activities [46-47]. Considering adverse ocular effects, a non-exhaustive list of possible conditions increasing susceptibility includes workers with alterations of the iris (e.g., coloboma or aniridia), with conditions determining chronic dilation of the pupil or with the absence of the lens (aphakia) or surgical removal of the lens (pseudophakia). In these cases, the alterations of the ocular structures result in possibly different levels of penetration of blue light and UV radiation into the eye. Other conditions to be potentially evaluated during health surveillance include those related to possible indications of early damage, e.g., the identification of drusen for macular degeneration or small opacities for cataracts. In such cases, the workers should be followed closely, as long-term exposure to SR may worsen the condition. Finally, other individuals who should be included among the group of susceptible workers are those with monocular vision, as in this case, the induction of disease in the healthy eye can lead to vision loss [46-47].
We argue, therefore, that a specific health surveillance program should be established for all workers exposed to potentially harmful solar UVR levels and, in particular, for those with a potentially increased susceptibility. Considering SR-associated adverse eye effects, the objective of this health surveillance would be the primary prevention, or at least (if the damage has already developed in its initial phase) early diagnosis of these diseases and their precursory ocular changes. Health surveillance programs usually include pre-employment and periodic medical examinations by trained occupational physicians, who may require, on an individual basis, supplementary assessments and management by ophthalmologists and optometrists for the specific problems detected [46-47]. As UVR is a carcinogenic agent, even if eye tumors are rare, the additional carcinogenic risk for the eyes of the exposed workers also has to be considered [33]. Finally, SR-related eye diseases occurring in OW should be reported to national compensation authorities so that they can be recognized as occupational diseases, thus raising awareness of the problem among the general public and exposed workers, as well as among employers, occupational health and safety professionals, and policymakers, who are often not fully aware of the problem [46-48]. Currently, these diseases are underreported, if not totally neglected, in countries that include such diseases in the available lists of occupational diseases and in countries that do not consider them. Accordingly, it is vitally essential that SR-related eye diseases be included in the official lists of occupational diseases in all countries. Such an approach is considered one of the first steps to fully recognize these pathologies as being related to outdoor work and therefore notified and compensated appropriately.
6. Conclusions
Epidemiological studies consistently report increased eye diseases among workers with long-term exposure to SR, including pterygium, cataracts, eye tumors, and, possibly, macular degeneration. These diseases should be recognized as “occupational diseases”, but they are frequently not reported to the national compensation authorities. To prevent the burden of these work-related eye diseases, an adequate risk evaluation with the identification of appropriate preventive measures (e.g., eye protection) and the provision of health surveillance programs for exposed workers (and in particular for those with increased susceptibility) should be implemented as a matter of urgency.
Declaration of Interest:
The authors declare no conflict of interest.
References
- Cherrie JW, Cherrie MPC. Workplace exposure to UV radiation and strategies to minimize cancer risk. Br Med Bull. 2022;144(1):45–56. doi: 10.1093/bmb/ldac019. Doi: 10.1093/bmb/ldac019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Environmental Burden of Disease Series, No. 13. Solar ultraviolet radiation: Global burden of disease from solar ultraviolet radiation. Available online: https://www.who.int/publications/i/item/9241594403. (Last Accessed on 30 June 2023) [Google Scholar]
- Razzaque MS. Sunlight exposure: Do health benefits outweigh harm? J Steroid Biochem Mol Biol. 2018;175:44–48. doi: 10.1016/j.jsbmb.2016.09.004. Doi: 10.1016/j.jsbmb.2016.09.004. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection; International Labour Organization; World Health Organization. Protecting, ICNIRP 14/2007. Protecting Workers from Ultraviolet Radiation. Available online: https://www.icnirp.org/cms/upload/publications/ICNIRPUVWorkers.pdf. (Last Accessed on 30 June 2023) [Google Scholar]
- Internationals Standard Organization and Commision Internationale d’Eclairage ISO 17166:1999(E) CIE S 007/E-1998. Erythema reference action spectrum and standard erythema dose. Spectre d’action érythémale de référence et dose érythémale normalisée. Available online: https://www.iso.org/obp/ui/#iso:std:iso:17166:ed-1:v2:en. (Last Accessed on 30 June 2023) [Google Scholar]
- International Labour Office. Occupational Safety and Health Series n° 72. Technical and Ethical Guidelines for Workers’ Health Surveillance. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/normativeinstrument/wcms_177384.pdf. (accessed on 27 April 2023) [Google Scholar]
- International Commission on Occupational Health. International Code of Ethics for Occupational Health Professionals. Available online: https://www.icohweb.org/site/code-of-ethics.asp. (Last Accessed on 30 June 2023) [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP) ICNIRP Guidelines on Limits of Exposure to Incoherent Visible and Infrared Radiation. Health Phys. 2013;105(1):74–96. doi: 10.1097/HP.0b013e318289a611. Doi: 10.1097/HP.0b013e318289a611. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP) ICNIRP statement--Protection of workers against ultraviolet radiation. Health Phys. 2010;99(1):66–87. doi: 10.1097/HP.0b013e3181d85908. Doi: 10.1097/HP.0b013e3181d85908. [DOI] [PubMed] [Google Scholar]
- Coroneo M. Ultraviolet radiation and the anterior eye. Eye Contact Lens. 2011;37(4):214–224. doi: 10.1097/ICL.0b013e318223394e. Doi: 10.1097/ICL.0b013e318223394e. [DOI] [PubMed] [Google Scholar]
- Hohberger B, Bergua A. Selbst verursachte laserinduzierte Makulopathie im Jugendalter [Self-inflicted laser-induced maculopathy in adolescence] Ophthalmologe. 2017;114(3):259–261. doi: 10.1007/s00347-016-0293-x. Doi: 10.1007/s00347-016-0293-x. [DOI] [PubMed] [Google Scholar]
- Bachmeier I, Helbig H, Greslechner R. Retinopathia solaris: Eine Fallserie nach der Sonnenfinsternis am 20.3.2015 [Eclipse retinopathy: A case series after the partial solar eclipse on 20 March 2015] Ophthalmologe. 2017;114(1):44–48. doi: 10.1007/s00347-016-0286-9. Doi: 10.1007/s00347-016-0286-9. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP) Guidelines on limits of exposure to ultraviolet radiation of wavelengths between 180 nm and 400 nm (incoherent optical radiation) Health Phys. 2004;87(2):171–186. doi: 10.1097/00004032-200408000-00006. Doi: 10.1097/00004032-200408000-00006. [DOI] [PubMed] [Google Scholar]
- Guly HR. Snow blindness and other eye problems during the heroic age of Antarctic exploration. Wilderness Environ Med. 2012;23(1):77–82. doi: 10.1016/j.wem.2011.10.006. Doi: 10.1016/j.wem.2011.10.006. [DOI] [PubMed] [Google Scholar]
- Sliney DH. Exposure geometry and spectral environment determine photobiological effects on the human eye. Photochem Photobiol. 2005;81(3):483–489. doi: 10.1562/2005-02-14-RA-439. Doi: 10.1562/2005-02-14-RA-439. [DOI] [PubMed] [Google Scholar]
- Bunsen RW, Roscoe HE. Photochemical researches – Part V. On the measurement of the chemical action of direct and diffuse sunlight. Proceedings of the Royal Society. 1862;12:306. [Google Scholar]
- Sengillo JD, Kunkler AL, Medert C, et al. UV-Photokeratitis Associated with Germicidal Lamps Purchased during the COVID-19 Pandemic. Ocul Immunol Inflamm. 2021;29(1):76–80. doi: 10.1080/09273948.2020.1834587. [DOI] [PubMed] [Google Scholar]
- Asokan R, Venkatasubbu RS, Velumuri L, Lingam V, George R. Prevalence and associated factors for pterygium and pinguecula in a South Indian population. Ophthalmic Physiol Opt. 2012;32(1):39–44. doi: 10.1111/j.1475-1313.2011.00882.x. Doi: 10.1111/j.1475-1313.2011.00882.x. [DOI] [PubMed] [Google Scholar]
- Chui J, Di Girolamo N, Wakefield D, Coroneo MT. The pathogenesis of pterygium: current concepts and their therapeutic implications. Ocul Surf. 2008;6(1):24–43. doi: 10.1016/s1542-0124(12)70103-9. Doi: 10.1016/s1542-0124(12)70103-9. [DOI] [PubMed] [Google Scholar]
- Modenese A, Gobba F. Occupational Exposure to Solar Radiation at Different Latitudes and Pterygium: A Systematic Review of the Last 10 Years of Scientific Literature. Int J Environ Res Public Health. 2017;15(1):37. doi: 10.3390/ijerph15010037. Doi: 10.3390/ijerph15010037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malekifar P, Esfandiari H, Behnaz N, et al. Risk Factors for Pterygium in Ilam Province, Iran. J Ophthalmic Vis Res. 2017;12(3):270–274. doi: 10.4103/jovr.jovr_85_16. Doi: 10.4103/jovr.jovr_85_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen AP, Chou BR, Hall MG, Jany SE. Ultraviolet-B damages corneal endothelium. Am J Optom Physiol Opt. 1984;61(7):473–478. doi: 10.1097/00006324-198407000-00009. Doi: 10.1097/00006324-198407000-00009. [DOI] [PubMed] [Google Scholar]
- Taylor HR. Ocular effects of UV-B exposure. Doc Ophthalmol. 1994;88(3-4):285–293. doi: 10.1007/BF01203682. Doi: 10.1007/BF01203682. [DOI] [PubMed] [Google Scholar]
- Löfgren S. Solar ultraviolet radiation cataract. Exp Eye Res. 2017;156:112–116. doi: 10.1016/j.exer.2016.05.026. Doi: 10.1016/j.exer.2016.05.026. [DOI] [PubMed] [Google Scholar]
- Modenese A, Gobba F. Cataract frequency and subtypes involved in workers assessed for their solar radiation exposure: a systematic review. Acta Ophthalmol. 2018;96(8):779–788. doi: 10.1111/aos.13734. Doi: 10.1111/aos.13734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della Vecchia E, Modenese A, Loney T, et al. Risk of cataract in health care workers exposed to ionizing radiation: a systematic review. Med Lav. 2020;111(4):269–284. doi: 10.23749/mdl.v111i4.9045. Doi: 10.23749/mdl.v111i4.9045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenkate T, Adam B, Al-Rifai RH, et al. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of occupational exposure to solar ultraviolet radiation and of the effect of occupational exposure to solar ultraviolet radiation on cataract. Environ Int. 2019;125:542–553. doi: 10.1016/j.envint.2018.10.001. Doi: 10.1016/j.envint.2018.10.001. [DOI] [PubMed] [Google Scholar]
- Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. Doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- Nowak JZ. Age-related macular degeneration (AMD): pathogenesis and therapy. Pharmacol Rep. 2006;58(3):353–363. [PubMed] [Google Scholar]
- Fletcher AE, Bentham GC, Agnew M, et al. Sunlight exposure, antioxidants, and age-related macular degeneration. Arch Ophthalmol. 2008;126(10):1396–1403. doi: 10.1001/archopht.126.10.1396. Doi:10.1001/archopht.126.10.1396. [DOI] [PubMed] [Google Scholar]
- Sliney DH. How light reaches the eye and its components. Int J Toxicol. 2002;21(6):501–509. doi: 10.1080/10915810290169927. Doi:10.1080/10915810290169927. [DOI] [PubMed] [Google Scholar]
- Modenese A, Gobba F. Macular degeneration and occupational risk factors: a systematic review. Int Arch Occup Environ Health. 2019;92(1):1–11. doi: 10.1007/s00420-018-1355-y. Doi:10.1007/s00420-018-1355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) Radiation Volume 100 D. A review of human carcinogens. Lyon, WHO press 2012. Available online: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic-Hazards-To-Humans/Radiation-2012. (Last Accessed on 30 June 2023) [Google Scholar]
- Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2014;34(2):383–400. doi: 10.1007/s10792-013-9791-x. Doi: 10.1007/s10792-013-9791-x. [DOI] [PubMed] [Google Scholar]
- Lee GA, Williams G, Hirst LW, Green AC. Risk factors in the development of ocular surface epithelial dysplasia. Ophthalmology. 1994;101(2):360–364. doi: 10.1016/s0161-6420(94)31328-5. Doi: 10.1016/s0161-6420(94)31328-5. [DOI] [PubMed] [Google Scholar]
- Guha N, Loomis D, Guyton KZ, et al. Carcinogenicity of welding, molybdenum trioxide, and indium tin oxide. Lancet Oncol. 2017;18(5):581–582. doi: 10.1016/S1470-2045(17)30255-3. Doi: 10.1016/S1470-2045(17)30255-3. [DOI] [PubMed] [Google Scholar]
- Chalada M, Ramlogan-Steel CA, Dhungel BP, Layton CJ, Steel JC. The Impact of Ultraviolet Radiation on the Aetiology and Development of Uveal Melanoma. Cancers (Basel) 2021;13(7):1700. doi: 10.3390/cancers13071700. Doi: 10.3390/cancers13071700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Conference of Governmental Industrial Hygienists. Documentation of the Threshold Limit Values and Biological Exposure Indices. 7th ed. Cincinnati, US: American Conference of Governmental Industrial Hygienists; 2001. [Google Scholar]
- Peters CE, Pasko E, Strahlendorf P, Holness DL, Tenkate T. Solar Ultraviolet Radiation Exposure among Outdoor Workers in Three Canadian Provinces. Ann Work Expo Health. 2019;63(6):679–688. doi: 10.1093/annweh/wxz044. Doi: 10.1093/annweh/wxz044. [DOI] [PubMed] [Google Scholar]
- Moehrle M, Dennenmoser B, Garbe C. Continuous long-term monitoring of UV radiation in professional mountain guides reveals extremely high exposure. Int J Cancer. 2003;103(6):775–778. doi: 10.1002/ijc.10884. Doi: 10.1002/ijc.10884. [DOI] [PubMed] [Google Scholar]
- Wittlich M, John SM, Tiplica GS, et al. Personal solar ultraviolet radiation dosimetry in an occupational setting across Europe. J Eur Acad Dermatol Venereol. 2020;34(8):1835–1841. doi: 10.1111/jdv.16303. Doi: 10.1111/jdv.16303. [DOI] [PubMed] [Google Scholar]
- Rosenthal FS, Phoon C, Bakalian AE, Taylor HR. The ocular dose of ultraviolet radiation to outdoor workers. Invest Ophthalmol Vis Sci. 1988;29(4):649–656. [PubMed] [Google Scholar]
- Duncan DD, Schneider W, West KJ, Kirkpatrick SJ, West SK. The development of personal dosimeters for use in the visible and ultraviolet wavelengths regions. The Salisbury Eye Evaluation Team. Photochem Photobiol. 1995;62(1):94–100. doi: 10.1111/j.1751-1097.1995.tb05244.x. Doi: 10.1111/j.1751-1097.1995.tb05244.x. [DOI] [PubMed] [Google Scholar]
- Sydenham MM, Collins MJ, Hirst LW. Measurement of ultraviolet radiation at the surface of the eye. Invest Ophthalmol Vis Sci. 1997;38(8):1485–1492. [PubMed] [Google Scholar]
- Duncan DD, Muñoz B, Bandeen-Roche K, West SK. Visible and ultraviolet-B ocular-ambient exposure ratios for a general population. Salisbury Eye Evaluation Project Team. Invest Ophthalmol Vis Sci. 1997;38(5):1003–1011. [PubMed] [Google Scholar]
- Tenkate T, Strahlendorf P. Sun Safety at Work: A Management Systems Approach to Occupational Sun Safety. 2020 Available online: https://sunsafetyatwork.ca/sites/default/files/ssp_guide_final-e-version.pdf. (Last Accessed on 30 June 2023) [Google Scholar]
- European Commission. Non-binding guide to good practice for implementing Directive 2006/25/EC “artificial optical radiation”. Available online: https://osha.europa.eu/en/legislation/guidelines/non-binding-guide-good-practice-implementing-directive-200625ec-artificial-optical-radiation. (Last Accessed on 30 June 2023) [Google Scholar]
- Alfonso JH, Bauer A, Bensefa-Colas L, et al. Minimum standards on prevention, diagnosis and treatment of occupational and work-related skin diseases in Europe - position paper of the COST Action StanDerm (TD 1206) J Eur Acad Dermatol Venereol. 2017;31(Suppl 4):31–43. doi: 10.1111/jdv.14319. Doi: 10.1111/jdv.14319. [DOI] [PubMed] [Google Scholar]
- Backes C, Religi A, Moccozet L, Vuilleumier L, Vernez D, Bulliard JL. Facial exposure to ultraviolet radiation: Predicted sun protection effectiveness of various hat styles. Photodermatol Photoimmunol Photomed. 2018;34(5):330–337. doi: 10.1111/phpp.12388. doi: 10.1111/phpp.12388. [DOI] [PubMed] [Google Scholar]
- Backes C, Religi A, Moccozet L, et al. Sun exposure to the eyes: predicted UV protection effectiveness of various sunglasses. J Expo Sci Environ Epidemiol. 2019;29(6):753–764. doi: 10.1038/s41370-018-0087-0. doi: 10.1038/s41370-018-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Organization for Standardization. ISO 16321-1: 2021 Eye and face protection for occupational use - Part 1: General requirements. Geneva, 2021. Available online: https://www.iso.org/standard/62527.html. (Last Accessed on 30 June 2023) [Google Scholar]
- American National Standards Institute. ANSI/ISEA Z87.1: 2020 American National Standard for Occupational and Educational Personal Eye and Face Protection Devices. Washington, 2020. Available online: https://blog.ansi.org/2020/04/ansi-isea-z87-1-2020-safety-glasses-eye-face/#gref. (Last Accessed on 30 June 2023) [Google Scholar]


