Abstract
Aim:
To describe the education and employment transition experience of young adults with spina bifida (YASB) and investigate factors associated with employment.
Method:
We queried education and employment data from the US National Spina Bifida Patient Registry from 2009 to 2019. We applied generalized estimating equations models to analyze sociodemographic and disease-related factors associated with employment.
Results:
A total of 1909 participants (850 males, 1059 females) aged 18 to 26 years contributed 4379 annual visits. Nearly 84% had myelomeningocele and, at last visit, the median age was 21 years (mean 21 years 5 months, SD 2 years 10 months). A total of 41.8% had at least some post-high school education, and 23.9% were employed. In a multivariable regression model, employment was significantly associated with education level, lower extremity functional level, bowel continence, insurance, and history of non-shunt surgery. This large, national sample of YASB demonstrated low rates of post-secondary education attainment and employment and several potentially modifiable factors associated with employment.
Interpretation:
Specific sociodemographic, medical, and functional factors associated with employment are important for clinicians to consider when facilitating transition for YASB into adulthood. Additional research is needed to understand the impact of cognitive functioning and social determinants of health on transition success in YASB.
Most individuals with spina bifida now reach adulthood.1 Achieving developmental milestones of late adolescence and young adulthood is important for all young people, including those with chronic conditions, such as spina bifida. As a complex chronic condition permanently affecting multiple organ systems, spina bifida adds further challenges for individuals as they navigate the increasingly complex roles and responsibilities needed to attain autonomy and interdependence and achieve optimal health as adults. There is growing evidence supporting a planned, structured transition to adult healthcare for adolescents and young adults with chronic conditions, including support for achievement of typical adult milestones.2-4 Although several consensus recommendations for healthcare transition services for young adults with chronic conditions exist,5,6 transition planning for individuals with spina bifida is implemented inconsistently.7 Current healthcare transition services, including formal transition care programs at spina bifida clinics in the USA, show wide variances in their offerings to patients and families.7,8 Educational and employment achievement are important components and outcomes of the process of transition to adulthood and are influenced by clinical, sociocultural, and socioeconomic factors. The Individuals with Disabilities Education Act9 mandates a post-secondary transition process and specific services to support further education, employment, and independent living for all young people who have an individualized education program; however, compared with healthcare transition, less attention has been paid to the steps and processes necessary to promote educational attainment and employment status for young adults with spina bifida (YASB). Post-secondary educational transitions are typically not coordinated with healthcare transition planning, and the impact of specific healthcare transition care programs or services on educational or employment outcomes is unknown.
To better understand the factors that affect the health and quality of life of individuals with spina bifida across the lifespan and inform healthcare transition interventions, it is important to better characterize social, educational, and employment outcomes for young people with spina bifida as they transition from late adolescence into young adulthood.10,11 Previous studies have shown that YASB experience multiple challenges in achieving typical adult milestones,12-15 and are less likely to attend college or to be employed than young adults without spina bifida. However, these conclusions are limited by small sample sizes and limited information on other potentially relevant clinical variables. One study found that employment was not delayed, compared with peers without spina bifida, for those adults with spina bifida who had completed high school by age 19 years.14 Clinical and sociodemographic factors may also affect educational and employment milestones. Previous analyses of adults over 25 years of age enrolled in the National Spina Bifida Patient Registry (NSBPR) found that only employment status, and not educational attainment, was associated with bladder and bowel continence.16,17 Sociodemographic factors, such as race/ethnicity and insurance status, have also been associated with various outcomes tracked in the NSBPR.18
This study of YASB had two aims: (1) to describe educational and employment profiles among individuals aged 18 to 26 years with spina bifida; and (2) to determine how sociodemographic factors, factors related to spina bifida, and specific health outcomes are associated with employment status. We hypothesized that YASB with more severe spina bifida-related factors and less optimal health outcomes would have lower levels of educational attainment and rates of employment.
METHOD
NSBPR
The NSBPR, a large multicenter spina bifida registry funded by the Centers for Disease Control and Prevention, started in 2009 at 10 centers in the USA.19 A total of 37 multidisciplinary spina bifida clinics enrolled patients of all ages between 2009 and 2019. The NSBPR includes a centralized data collection center to facilitate data entry and analysis with established data quality measures including routine monthly data quality checks and interrater reliability reporting. Standardized, de-identified patient data on sociodemographic information, clinical characteristics, and treatment history are collected at enrollment and, thereafter, updated at annual clinic visits. Collection and use of NSBPR data has been approved by each site's Institutional Review Board. For our analyses, we extracted data from NSBPR participants whose ages were 18 to 26 years at time of their visit between 2009 and 2019.
Sociodemographic characteristics
Self-reported sex and race/ethnicity data were collected at the initial encounter. The terms 'race' and 'ethnicity' were used when data were collected/submitted and recorded in NSBPR, so have been retained here. Participants were classified as non-Hispanic White, non-Hispanic Black, Hispanic or Latino, or other (combined Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaskan Native, and multiracial). Educational level at each clinic visit was assigned to one of four categories: less than high school graduates, high school graduates, technical school/some college, and college/advanced degree. Health insurance was reported at each clinic visit as any private (commercial, military, regional, etc.) and non-private (Medicaid, Medicare, charity, etc.). Employment status was characterized as not employed, employed part time, or employed full time.
Clinical characteristics
In this study, spina bifida type was subcategorized into two groups: myelomeningocele and non-myelomeningocele (lipomyelomeningocele, meningocele, fatty filum, terminal myelocystocele, or split cord malformation). Lower extremity functional level was defined as thoracic (no spontaneous movement of legs), lumbar (hip flexion, knee extension, and/or ankle dorsiflexion present), or sacral (ankle plantar flexion present). When the motor function differed between legs, the more severely impaired leg determined the functional level. Ambulation status was documented at each visit as community, household, therapeutic, and non-ambulator.20
Throughout the course of the NSBPR, variable definitions have been refined. For data collected between January 2009 and September 2013, bladder continence was defined as ‘daytime dryness’ and bowel continence as ‘lack of involuntary, daytime stool leakage’. Starting in October 2013, the bladder and bowel continence definitions changed to ‘having episodes of incontinence less than once a month or never’. For this study, individuals with bladder management by urostomy bag, vesicostomy, indwelling catheter, or condom catheter were considered incontinent regardless of their response to the incontinence question. Individuals with bowel management by pouched fecal diversion, ileostomy, or colostomy were considered incontinent regardless of their response as well. Answers with ‘cannot assess’ were treated as missing data.
The placement of shunt, with revisions, replacement, and removal, was documented for each patient upon entry into the registry and updated annually. Non-shunt surgeries occurring since last visit, including other neurological, urological, gastrointestinal, ear/nose/throat, orthopedic, and skin surgeries were documented at each visit. These surgeries are listed in Table S1. Episodes of skin breakdown occurring since the last visit were also recorded at each visit.
Statistical analysis
We examined the association of employment outcomes with covariates using all visits excluding those reported as being a current student with ‘Not employed – child or student’ status. Time-independent variables included sex, race/ ethnicity, and spina bifida type. Time-dependent variables included age, lower extremity functional level, health insurance, educational level, ambulatory status, continence status, history of shunt, non-shunt surgeries since last visit, and episodes of skin breakdown since the last visit. Associations between spina bifida type and all other variables shown in Table 1 were examined using a χ2 test or Fisher's exact test.
TABLE 1.
Patients' characteristics at last visit among individuals living with spina bifida, 18–26 years of age in the NSBPR (2009–2019)
| Spina bifida type | ||||
|---|---|---|---|---|
| Variables | Overall (n = 1909) | Myelomeningocele (n = 1597) | Non-myelomeningocele (n = 312) | p |
| Age at last visit (years) | 0.012 | |||
| 18 | 333 (17.4) | 272 (17.0) | 61 (19.6) | |
| 19 | 301 (15.8) | 244 (15.3) | 57 (18.3) | |
| 20 | 297 (15.6) | 238 (14.9) | 59 (18.9) | |
| 21 | 196 (10.3) | 160 (10.0) | 36 (11.5) | |
| 22 | 146 (7.6) | 124 (7.8) | 22 (7.1) | |
| 23 | 119 (6.2) | 105 (6.6) | 14 (4.5) | |
| 24 | 105 (5.5) | 87 (5.4) | 18 (5.8) | |
| 25 | 171 (9.0) | 146 (9.1) | 25 (8.0) | |
| 26 | 241 (12.6) | 221 (13.8) | 20 (6.4) | |
| Number of visits | 0.004 | |||
| 1 | 782 (41.0) | 632 (39.6) | 150 (48.1) | |
| 2 | 504 (26.4) | 412 (25.8) | 92 (29.5) | |
| 3 | 253 (13.2) | 229 (14.3) | 24 (7.7) | |
| 4 | 177 (9.3) | 151 (9.5) | 26 (8.3) | |
| 5 | 98 (5.1) | 86 (5.4) | 12 (3.8) | |
| 6 | 48 (2.5) | 43 (2.7) | ≤5 | |
| 7 | 32 (1.7) | 30 (1.9) | ≤5 | |
| 8 | 15 (0.8) | 14 (0.9) | ≤5 | |
| Sex | 0.49 | |||
| Male | 850 (44.5) | 717 (44.9) | 133 (42.6) | |
| Female | 1059 (55.5) | 880 (55.1) | 179 (57.4) | |
| Race/ethnicity (n = 1907) | <0.001 | |||
| Non-Hispanic White | 1273 (66.8) | 1062 (66.6) | 211 (67.6) | |
| Non-Hispanic Black | 167 (8.8) | 152 (9.5) | 15 (4.8) | |
| Hispanic or Latino | 370 (19.4) | 312 (19.6) | 58 (18.6) | |
| Other | 97 (5.1) | 69 (4.3) | 28 (9.0) | |
| Ambulation status | <0.001 | |||
| Community ambulators | 893 (46.8) | 625 (39.1) | 268 (85.9) | |
| Household ambulators | 136 (7.1) | 123 (7.7) | 13 (4.2) | |
| Therapeutic ambulators | 80 (4.2) | 74 (4.6) | 6 (1.9) | |
| Non-ambulators | 800 (41.9) | 775 (48.5) | 25 (8.0) | |
| Lower extremity functional level | <0.001 | |||
| Sacral | 451 (23.6) | 260 (16.3) | 191 (61.2) | |
| Lumbar | 979 (51.3) | 870 (54.5) | 109 (34.9) | |
| Thoracic | 479 (25.1) | 467 (29.2) | 12 (3.8) | |
| Educational level (n = 1871) | <0.001 | |||
| Less than high school | 131 (7.0) | 104 (6.7) | 27 (8.7) | |
| High school graduate | 957 (51.1) | 855 (54.7) | 102 (33.0) | |
| Technical school/some college | 638 (34.1) | 502 (32.1) | 136 (44.0) | |
| College/advanced degree | 145 (7.7) | 101 (6.5) | 44 (14.2) | |
| Employment status | <0.001 | |||
| Not employed | 1452 (76.1) | 1247 (78.1) | 205 (65.7) | |
| Part-time | 276 (14.5) | 233 (14.6) | 43 (13.8) | |
| Full-time | 181 (9.5) | 117 (7.3) | 64 (20.5) | |
| Bladder continence (n = 1861) | <0.001 | |||
| Yes | 932 (50.1) | 721 (46.5) | 211 (68.3) | |
| No | 929 (49.9) | 831 (53.5) | 98 (31.7) | |
| Bowel continence (n = 1847) | <0.001 | |||
| Yes | 1153 (62.4) | 921 (59.5) | 232 (77.3) | |
| No | 929 (49.9) | 831 (53.5) | 98 (31.7) | |
| History of skin breakdown | <0.001 | |||
| Yes | 519 (27.2) | 470 (29.4) | 49 (15.7) | |
| No | 1390 (72.8) | 1127 (70.6) | 263 (84.3) | |
| History of non-shunt surgery | 0.49 | |||
| Yes | 1160 (60.8) | 976 (61.1) | 184 (59.0) | |
| No | 749 (39.2) | 621 (38.9) | 128 (41.0) | |
| History of shunt surgery | <0.001 | |||
| Yes | 1413 (74.0) | 1387 (86.9) | 26 (8.3) | |
| No | 496 (26.0) | 210 (13.1) | 286 (91.7) | |
| Health insurance | <0.001 | |||
| Any private | 904 (47.4) | 725 (45.4) | 179 (57.4) | |
| Non-private | 1005 (52.6) | 872 (54.6) | 133 (42.6) | |
Data are n (%) unless otherwise indicated. Abbreviation: NSBPR, National Spina Bifida Patient Registry.
To account for the effect of repeated observations of employment status and other time-dependent variables from the same person, we used generalized estimating equations (GEE) models with logit link function.21 The outcome of the main analysis was any employment. An outcome of sub-analysis was full-time employment among all visits at which participants reported being employed. GEE regression models estimated the odds ratios of these outcomes. The GEE regression models also accounted for correlated data from participants clustered by clinic. Multiple GEE regression models were conducted to test the independent association between outcome and covariates; an independent correlation structure was specified. Multiple collinearity was checked for both multiple regression models by examining the estimated correlation matrix. Any p-values less than 0.05 were considered significant; 95% confidence intervals (CIs) were calculated for odds ratio point estimates. Association between medical characteristics and health outcomes was also tested and is presented in Table S2. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). All analyses were replicated by a second analyst.
RESULTS
From 2009 to 2019, 1909 NSBPR participants between 18 years and 26 years of age contributed 4379 annual clinic visit records. Sociodemographic and clinic characteristics at the last visit are summarized in Table 1. At last visit, the participants' median age was 21 years. Most study participants were female (55.5%), non-Hispanic White (66.8%), and covered by non-private insurance (52.6%). At their most recent visit, 41.9% of participants were non-ambulatory, 50.1% were continent of bladder and 62.4% were continent of bowel, 41.8% had at least some post-high school education, and 23.9% were employed. Except for sex, all characteristics were significantly different between myelomeningocele and non-myelomeningocele spina bifida type.
Education and employment transition patterns
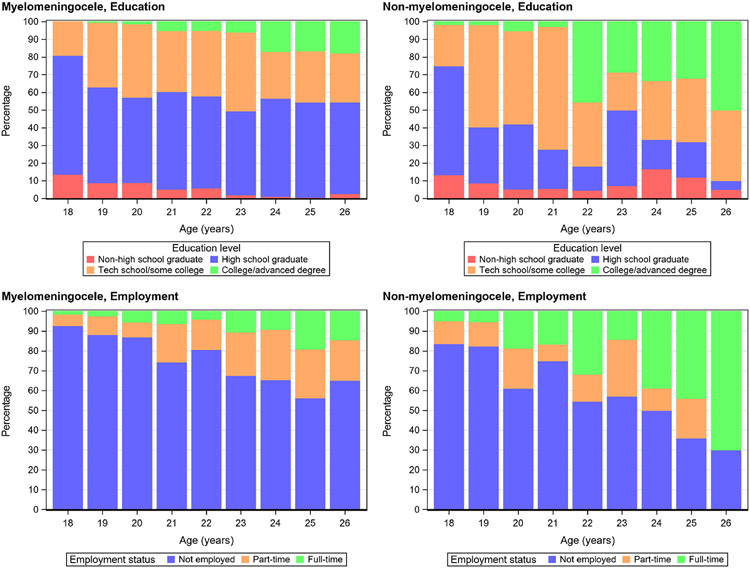
The summarized age-specific education and employment status data are presented for both myelomeningocele and non-myelomeningocele spina bifida type in Figure 1. During the transitional period, a larger proportion of participants pursued higher education and were employed as age increased. Participants with non-myelomeningocele showed higher education attainment and increased rate of employment than participants with myelomeningocele.
FIGURE 1.
Age-specific education and employment status for myelomeningocele (MMC) and non-myelomeningocele (NMMC) spina bifida type
Among all participants in this study, 7.6% of less than high school graduates, 18.6% of high school graduates, 25.7% of technical school/some college, and 66.9% of college/advanced degree were employed. About two-thirds of 18-year-olds and half of 19- to 26-year-olds were high school graduates only. About 40% of those aged 18 to 24 years and 49% aged 25 years and 26 years had at least some post-high school education. Only 1% to 2% of YASB aged 20 years and 21 years both received a college or advanced degree and were employed; this number was about 6% for those aged 22 years and 23 years, 13% for aged 24 years, and 15% for 25- and 26-year-olds.
Characteristics associated with employment status
Among 1182 participants with 2440 visits, excluding reports of being a current student with ‘Not employed – child or student’ status, factors associated with any employment versus none were assessed in a multivariable regression model (Table 2). In this main analysis, any employment was independently and significantly associated with higher education level, sacral lower extremity functional level, being continent of bowel, a history of non-shunt surgery since last visit, and having private health insurance. In the subsample of visits with any employment (949 visits in 545 participants), the multivariable regression model showed full-time employment was independently and significantly associated with older age, higher education level, non-myelomeningocele spina bifida type, being a community ambulator, and without skin breakdown since last visit. Multiple collinearity check for both models showed no significant findings (all estimated correlation coefficients were less than 0.8).
TABLE 2.
Estimated odds ratios from multivariable GEE models on any employment and full-time job among participants aged 18 to 26 years, NSBPR 2009 to 2019a
| Any employment vs none (among 2440 visits in 1182 participants) |
Full-time vs part-time employment (among 949 visits in 545 participants with any employment) |
|||
|---|---|---|---|---|
| Variables | Odds ratio (95% CI) | p | Odds ratio (95% CI) | p |
| Age at visit | ||||
| 1-year increase | 1.01 (0.97–1.06) | 0.62 | 1.20 (1.11–1.29) | <0.001 |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 0.99 (0.77–1.27) | 0.93 | 1.18 (0.79–1.76) | 0.43 |
| Race/ethnicity | 0.22b | 1.0b | ||
| Non-Hispanic White | 1.56 (1.00–2.42) | 0.048 | 0.99 (0.46–2.09) | 0.97 |
| Non-Hispanic Black | 1.51 (0.86–2.45) | 0.153 | 0.94 (0.38–2.36) | 0.90 |
| Hispanic or Latino | Ref | Ref | ||
| Other | 1.33 (0.75–2.36) | 0.33 | 1.00 (0.37–2.68) | 1.0 |
| Education level | <0.001b | <0.001b | ||
| Less than high school | 0.39 (0.21–0.71) | 0.003 | 0.54 (0.11–2.75) | 0.46 |
| High school graduate | Ref | Ref | ||
| Technical school/some college | 2.49 (1.90–3.25) | <0.001 | 0.73 (0.46–1.17) | 0.188 |
| College/advanced degree | 4.27 (2.69–6.77) | <0.001 | 2.88 (1.60–5.17) | <0.001 |
| Spina bifida type | ||||
| Myelomeningocele | Ref | Ref | ||
| Non-myelomeningocele | 1.24 (0.75–2.05) | 0.40 | 2.37 (1.21–4.65) | 0.012 |
| Ambulation status | 0.172b | 0.010b | ||
| Community ambulators | 1.41 (0.99–1.99) | 0.054 | 2.24 (1.27–3.96) | 0.005 |
| Household ambulators | 0.96 (0.57–1.62) | 0.89 | 1.03 (0.32–3.32) | 0.95 |
| Therapeutic ambulators | 1.16 (0.59–2.28) | 0.58 | 0.58 (0.20–1.69) | 0.32 |
| Non-ambulators | Ref | Ref | ||
| Lower extremity functional level | 0.009b | 0.85b | ||
| Thoracic | Ref | Ref | ||
| Lumbar | 1.29 (0.91–1.83) | 0.154 | 0.88 (0.46–1.70) | 0.71 |
| Sacral | 2.02 (1.27–3.21) | 0.003 | 0.80 (0.37–1.73) | 0.58 |
| Bladder continence | ||||
| Yes | 0.94 (0.75–1.18) | 0.60 | 1.16 (0.79–1.73) | 0.45 |
| No | Ref | Ref | ||
| Bowel continence | ||||
| Yes | 1.40 (1.11–1.76) | 0.004 | 1.14 (0.76–1.70) | 0.53 |
| No | Ref | Ref | ||
| Skin breakdown since last visit | ||||
| Yes | Ref | Ref | ||
| No | 0.79 (0.59–1.06) | 0.120 | 2.42 (1.35–4.35) | 0.003 |
| Non-shunt surgery since last visit | ||||
| Yes | 1.33 (1.09–1.62) | 0.004 | 1.17 (0.83–1.67) | 0.37 |
| No | Ref | Ref | ||
| History of shunt surgery | ||||
| Yes | 1.26 (0.83–1.93) | 0.28 | 1.34 (0.72–2.50) | 0.36 |
| No | Ref | Ref | ||
| Health insurance | ||||
| Any private | 1.81 (1.39–2.37) | <0.001 | 1.05 (0.65–1.68) | 0.85 |
| Non-private | Ref | Ref | ||
Abbreviations: GEE, generalized estimating equations; NSBPR, National Spina Bifida Patient Registry.
Excluded visits reporting current students with ‘Not employed – child or student’ status.
Overall p-value.
To address concerns about defining all patients as incontinent, regardless of their self-reported continence, if they had management strategies commonly considered incontinent as described in the Method section, we performed a secondary analysis on the main outcome using multiple regression modelling after excluding 37 patients using these management techniques. The association of employment with bladder and bowel continence and the other covariates did not change (data not shown).
DISCUSSION
Our analysis of data from 1182 YASB enrolled in the NSBPR between 2009 and 2019 and a subsample of 545 YASB reported being employed found that both sociodemographic factors and clinical factors were associated with employment status during their transition period from late adolescence to early adulthood. In multivariable regression, education level, lower extremity functional level, bowel continence, non-shunt surgery since last visit, and health insurance were significantly associated with any employment; age, education level, spina bifida type, and skin breakdown since last visit were significantly associated with full-time employment. Some of these factors are modifiable and may be instructive to guide care before and during transition to adulthood in patients with spina bifida.
About 40% of our cohort aged 18 to 24 years pursued post-high school education compared with 54.3% of the general US population in the same age range in 2019.22 The estimated employment rate among people aged 20 to 24 years in the US population was 68.2% in 2019,23 compared with 36.8% in the YASB of the same ages in our cohort (data not shown). These findings are consistent with previous studies showing that individuals with spina bifida face transition challenges.14,15
YASB and their caregivers have identified multiple barriers in the transition from school to work,13 and the presence of chronic physical illness related to spina bifida in adolescence has been associated with lower rates of employment in adulthood.12 Among YASB, our findings demonstrated that thoracic lower extremity functional level and bowel incontinence were negatively associated with employment. Among employed YASB, myelomeningocele type, non-community ambulatory status, and skin breakdown were negatively associated with full-time employment. These findings are consistent with a previous study that identified higher lesion level with lower odds of employment in spina bifida.24 These results support the importance of addressing school to work concerns previously identified by YASB, including lack of accessibility and accommodation, difficulty with management of their condition at school or work, unreliable transportation, and stigma and discrimination based on disability.13
Bladder and bowel management, with a goal of independent performance of necessary tasks to achieve continence, is potentially attainable in this population with appropriate family, medical, and, in some cases, surgical support. Consistent with previous studies,16 our findings indicated a positive association of bowel continence with employment in YASB. This highlights the importance of encouraging bowel management throughout childhood, not just in late adolescence, to ease the transition toward independence and promote better continence outcomes for adults. Self-management is considered an essential component of successful transition to adulthood for adolescents and young adults with complex conditions such as spina bifida,16,17,25 and supports for developing independence with bladder and bowel management are an important component in a healthcare transition program.15,26,27 The impact of incontinence on employment and potential interventions to promote continence should be an area of future study. This could include identifying opportunities for collaboration between healthcare professionals and educational and/or vocational professionals during transition planning to better address goals such as independence with bowel self-management and improve outcomes such as bowel continence and employment.
Recent non-shunt surgery was also associated with employment. This finding is contrary to our expectation that greater recent surgical burden would negatively affect employment. Most of the non-shunt surgeries that occurred between 18 years and 26 years of age were performed to optimize patient functional independence in areas such as continence or ambulation, which could make it easier for YASB to gain or retain employment. Further investigation of the association between recent surgeries and employment is warranted.
Because studies have shown controversial results on the association between shunting and cognitive/neurocognitive function,28,29 we included history of shunt surgery in the analysis. Our final models did not show significant association between history of shunt surgery and employment outcome.
The size of the NSBPR and repeated measures allowed longitudinal analysis in a large sample of YASB. Longitudinal analysis of data from multiple clinic visits offers a more complete assessment of employment status and its association with covariates. The use of GEE models enabled us to examine the associations between covariates and employment status while simultaneously capturing the influence of between- and within-subject variation. Another strength of our study was using prospective data collection, which systematically captured sociodemographic, condition-related, and management data in a more extensive and consistent manner than comparable retrospective studies.
In the USA, employers are the major payers of private insurance. Using last clinic visit records, our data found that 71.3% of full-time employed NSBPR participants had private insurance, compared with 55.4% and 42.8% for part-time employees and those not employed respectively (data not shown). Our final multiple regression model showed that, as expected, the odds of having higher employment status was 1.62 times greater for participants with private health insurance than those without. However, the NSBPR does not capture whether participants have private insurance through their employers or through close relatives (i.e. parents) and the large majority of the included YASB population was younger than 26 years, the age at which they might no longer be on their parents' insurance.
There were several limitations to this study. First, more than 40% of the individuals in it had only one visit, and although the GEE model is designed to accommodate single and multiple visits, the model was not able to examine the within-subject trajectory of employment over time for participants with a single visit. Second, the participants in this study received care at NSBPR clinic sites and may not be representative of the larger YASB population in the USA. Third, the definitions used in the NSBPR for bladder and bowel continence and other functional outcomes changed over time, and functional outcomes studied are dependent on patient (or proxy) report, which can be missing, subjective, and vary over time. The definition of employment may also be subjective depending on consistency of hours worked and remuneration, and our analysis does not address type of employment, which limits our understanding of employment as an outcome in this study. An individual's decisions about employment status may also be affected by the restrictive eligibility requirements of other support programs and a potential loss of those benefits. Also, the NSBPR did not collect cognitive function data, such as IQ and executive functioning, and other factors including social skills, mental health indicators, quality of life, and family functioning, which may be important predictors of education and employment status. Lastly, employment is only one factor that may influence health-related and overall quality of life. The NSBPR started collecting cognitive and IQ data in 2020, and quality of life data in 2021, which will allow a better understanding of the relationships between education, employment, and quality of life, and enable future study of targeted interventions in spina bifida transition.
In conclusion, our study showed low rates of post-secondary educational attainment and employment in YASB within a large, national sample as they transitioned from adolescence to young adulthood in comparison with the US general population in the same age range. Specific sociodemographic, medical, and functional factors were associated with a higher likelihood of attaining employment in early adult life. By considering the educational and employment goals of their patients with spina bifida, clinicians could focus their care interventions on factors that facilitate the transition process of YASB. The use of already available resources and new strategies to modify the impact of these factors on transition patterns are necessary to maximize the potential of YASB. Additional research could help us understand how cognitive functioning and social determinants of health such as health insurance, access to health services, family supports, and health status influence YASB's employment, quality of life, and transition into adulthood.
Supplementary Material
Table S1: List of non-shunt surgeries.
Table S2: Medical characteristics and health outcomes among individuals aged 18 to 26 years at last visit, NSBPR 2009 to 2019.
What this paper adds.
There were low education attainment and employment rates in a large sample of young adults with spina bifida.
Specific sociodemographic, medical, and functional factors are associated with employment.
Some employment-associated factors, such as continence and self-management skills, are modifiable.
ACKNOWLEDGMENTS
We thank the many individuals with spina bifida and their family members who participated in this research, without whom the NSBPR would not be possible. The NSBPR has also been successful because of the contributions of the Centers for Disease Control and Prevention, the Spina Bifida Association, and all members of the NSBPR Coordinating Committee. Members of this Committee during the collection of the data reported are listed in alphabetical order and were Richard Adams, Texas Scottish Rite Hospital for Children, Dallas; Pat Beierwaltes, Children's Hospital of Michigan, Detroit; Timothy Brei, Riley Hospital for Children, Indianapolis; Robin Bowman, Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago; Heidi Castillo, Cincinnati Children's Hospital Medical Center, Cincinnati and Texas Children's Hospital, Houston; James Chinarian, Children's Hospital of Michigan, Detroit; Mark Dias, Hershey Medical Center, Hershey; Brad Dicianno, University of Pittsburgh Medical Center, Pittsburgh; Nienke Dosa, Upstate Golisano Children's Hospital, Syracuse; Carlos Estrada, Boston Children's Hospital, Boston; Kurt Freeman, Oregon Health and Science University, Portland; Greg Heuer, Children's Hospital of Philadelphia, Philadelphia; David Joseph, Children's Hospital of Alabama, Birmingham; Lynne Logan, Upstate Medical University, Syracuse; Pamela Murphy, District Medical Group Children's Rehabilitative Services, Phoenix; Jacob Neufeld, Children's Hospital and Research Center at Oakland, Oakland, University of California at San Francisco Benioff Children's Hospital, San Francisco, and St. Luke's Boise Medical Center, Boise; Joseph O'Neil, Riley Hospital for Children, Indianapolis; Michael Partington, Gillette Children's Specialty Healthcare, St. Paul; Paula Peterson, Primary Children's Medical Center, Salt Lake City; Elaine Pico, Children's Hospital and Research Center at Oakland, Oakland and University of California at San Francisco Benioff Children's Hospital, San Francisco; Karen Ratliff-Schaub, Nationwide Children's Hospital, Columbus; Kathleen Sawin, Children's Hospital of Wisconsin, Milwaukee; Kathryn Smith, Children's Hospital Los Angeles, Los Angeles; Katherine Steingass, Nationwide Children's Hospital, Columbus; Stacy Tanaka, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville; Jeffrey Thomson, Connecticut Children's Medical Center, Hartford and Shriners Hospitals for Children Springfield, Springfield; David Vandersteen, Gillette Specialty Clinics, St. Paul; William Walker, Seattle Children's Hospital, Seattle; John Wiener, Duke University Medical Center, Durham; Pamela Wilson, Children's Hospital Colorado, Denver; and Hadley Wood, Cleveland Clinic, Cleveland.
FUNDING INFORMATION
The National Spina Bifida Patient Registry is funded by the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, by Grants DD000738, DD000740, DD000743, DD000774, DD001057, DD001062, DD001065, DD001093, DD001235, DD001237, DD001240, DD001262, DD001265, DD001266, DD001268, DD001270, DD001272, DD001274, DD001275, DD001278, DD001279, and DD001280.
Abbreviations:
- GEE
generalized estimating equations
- NSBPR
National Spina Bifida Patient Registry
- YASB
young adults with spina bifida
Footnotes
CONFLICT OF INTEREST
The authors have stated that they had no interests that might be perceived as posing a conflict or bias.
SUPPORTING INFORMATION
The following additional material may be found online.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are accessed through the sites contributing their data. Restrictions apply to the availability of these data. Interested researchers can contact cdcinfo@cdc.gov.
REFERENCES
- 1.Bowman RM, McLone DG, Grant JA, et al. Spina bifida outcome: A 25-year prospective. Pediatr Neurosurg. 2001;34(3): 114–120. [DOI] [PubMed] [Google Scholar]
- 2.Fremion E, Morrison-Jacobus M, Castillo J, et al. A chronic care model for spina bifida transition. J Pediatr Rehabil Med. 2017;10(3–4):243–247. doi: 10.3233/PRM-170451. [DOI] [PubMed] [Google Scholar]
- 3.Gabriel P, McManus M, Rogers K, et al. Outcome Evidence for Structured Pediatric to Adult Health Care Transition Interventions: A Systematic Review. J Pediatr. 2017; 188:263–269 .e15. [DOI] [PubMed] [Google Scholar]
- 4.Suris JC and Akre C. Key Elements for, and Indicators of, a Successful Transition: An International Delphi Study. Journal of Adolescent Health. 2015; 56 (6):612–618. [DOI] [PubMed] [Google Scholar]
- 5.Fremion EJ, Dosa NP. Spina bifida transition to adult healthcare guidelines. J Pediatr Rehabil Med. 2019;12(4):423–429. doi: 10.3233/PRM-190633. [DOI] [PubMed] [Google Scholar]
- 6.White PH, Cooley WC, Transitions Clinical Report Authoring Group, et al. Supporting the Health Care Transition from Adolescence to Adulthood in the Medical Home. Pediatrics. 2018;142(5) e20182587; DOI: https://doi.org/ 10.1542/peds.2018-2587. [DOI] [PubMed] [Google Scholar]
- 7.Kelly MS, Thibadeau J, Struwe S, et al. Evaluation of spina bifida transitional care practices in the United States. J Pediatr Rehabil Med. 2017;10(3-4):275–281. doi: 10.3233/PRM-170455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Kort LMO. Transition from childhood to adolescence: steps to be taken. Curr Opin Urol. 2020;30(4):491–495. [DOI] [PubMed] [Google Scholar]
- 9.Individuals with Disabilities Education Act (IDEA). https://sites.ed.gov/idea/topic-areas/#Secondary-Transition (accessed 9/23/2022). [Google Scholar]
- 10.Davis BE, Shurtleff DB, Walker WO, et al. Acquisition of autonomy skills in adolescents with myelomeningocele. Developmental Medicine & Child Neurology. 2006;48: 253–258. [DOI] [PubMed] [Google Scholar]
- 11.Thibadeau JK, Alriksson-Schmidt AI, Zabel TA. The National Spina Bifida Program transition initiative: the people, the plan, and the process. Pediatric clinics of North America. 2010;57(4):903–910. [DOI] [PubMed] [Google Scholar]
- 12.Pinquart M Achievement of developmental milestones in emerging and young adults with and without pediatric chronic illness – a meta-analysis. J Pediatr Psychol. 2014;39(6):577–587. [DOI] [PubMed] [Google Scholar]
- 13.Lindsay S, McPherson AC, Maxwell J. Perspectives of school-work transitions among youth with spina bifida, their parents and health care providers. Disabil Rehabil. 2017;39(7):641–652. [DOI] [PubMed] [Google Scholar]
- 14.Zukerman JM, Devine KA, Holmbeck GN. Adolescent predictors of emerging adulthood milestones in youth with spina bifida. J Pediatr Psychol. 2011;36(3):265–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holbein CE, Zebracki K, Bechtel CF, et al. Milestone achievement in emerging adulthood in spina bifida: a longitudinal investigation of parental expectations. Developmental Medicine & Child Neurology. 2017;59(3), 311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiener JS, Suson KD, Castillo J, et al. Bowel management and continence in adults with spina bifida: Results from the National Spina Bifida Patient Registry 2009–15. Journal of pediatric rehabilitation medicine. 2017;10(3–4), 335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiener JS, Suson KD, Castillo J, et al. Bladder management and continence outcomes in adults with spina bifida: Results from the National Spina Bifida Patient Registry 2009–15. The Journal of Urology. 2018;200(1), 187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schechter MS, Liu T, Soe M, et al. Sociodemographic attributes and spina bifida outcomes. Pediatrics 2015; 135 (4): e957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thibadeau J, Ward E, Soe MM, et al. Testing the feasibility of the of a National Spina Bifida Patient Registry. Birth Defects Research (Part A). 2013;97:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffer MM, Feiwell E, Perry R, et al. Functional ambulation in patients with myelomeningocele. The Journal of Bone & Joint Surgery. 1973;55(1), 137–148. [PubMed] [Google Scholar]
- 21.Lipsitz SR, Kim K, Zhao L. Analysis of Repeated Categorical Data Using Generalized Estimating Equations. Statistics in Medicine. 1994;13:1149–1163. [DOI] [PubMed] [Google Scholar]
- 22.Educational Attainment in the United States: 2019. https://www.census.gov/data/tables/2019/demo/educational-attainment/cps-detailed-tables.html (accessed 9/11/2020). [Google Scholar]
- 23.United States Census Bureau. Employment Status. Washington: American Community Survey, 2019. https://data.census.gov/cedsci/table?q=employment&tid=ACSST1Y2019.S2301&hidePreview=false (accessed 9/21/2020). [Google Scholar]
- 24.Bellin MH, Dicianno BE, Levey E, et al. Interrelationships of sex, level of lesion, and transition outcomes among young adults with myelomeningocele. Dev Med Child Neurol 2011; 53 (7): 647–652. [DOI] [PubMed] [Google Scholar]
- 25.Liu T, Ouyang L, Thibadeau J, et al. Longitudinal study of bladder continence in patients with spina bifida in the National Spina Bifida Patient Registry. J Urol. 2018;199(3), 837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liptak GS, Kennedy JA, Dosa NP. Youth with spina bifida and transitions: health and social participation in a nationally represented sample. J Pediatr. 2010;157(4):584–588. [DOI] [PubMed] [Google Scholar]
- 27.Hale DR, Bevilacqua L, Viner RM. Adolescent health and adult education and employment: a systematic review. Pediatrics. 2015;136(1), 128–140. [DOI] [PubMed] [Google Scholar]
- 28.Warf B, Ondoma S, Kulkarni A, et al. Neurocognitive outcome and ventricular volume in children with myelomeningocele treated for hydrocephalus in Uganda. J Neurosurg Pediatr. 2009; 4: 564–70. [DOI] [PubMed] [Google Scholar]
- 29.Lindquist B, Persson EK, Fernell E, Uvebrant P. Very long-term follow-up of cognitive function in adults treated in infancy for hydrocephalus. Childs Nerv Syst. 2011; 27: 597–601. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: List of non-shunt surgeries.
Table S2: Medical characteristics and health outcomes among individuals aged 18 to 26 years at last visit, NSBPR 2009 to 2019.
Data Availability Statement
The data that support the findings of this study are accessed through the sites contributing their data. Restrictions apply to the availability of these data. Interested researchers can contact cdcinfo@cdc.gov.