Abstract
Purpose The aim of this study was to evaluate the overall and type-specific prevalence of human papillomavirus (HPV) infection among females living in riverside communities in the state of Pará, in the Eastern Brazilian Amazon. These communities are inhabited by low-income people, and are accessible only by small boats. Cervical cytology and risk factors for HPV infection were also assessed.
Methods Cervical samples from 353 women of selected communities were collected both for Papanicolau (Pap) test and HPV detection. Conventional polymerase chain reaction (PCR) and real-time PCR were used to assess the overall and type-specific prevalence of HPV-16 and HPV-18, the main oncogenic types worldwide. Epidemiological questionnaires were used for the assessment of the risk factors for HPV infection.
Results The mean age of the participants was 37 years (standard deviation [SD] ± 13.7). Most were married or with a fixed sexual partner (79%), and had a low educational level (80%) and family monthly income (< U$ 250; 53%). Overall, HPV prevalence was 16.4% (n = 58), with 8 cases of HPV-16 (2.3%) and 5 of HPV-18 (1.4%). Almost 70% of the women surveyed had never undergone the Pap test. Abnormal cytology results were found in 27.5% (n = 97) of the samples, with higher rates of HPV infection according to the severity of the lesions (p = 0.026).
Conclusions The infections by HPV-16 and HPV-18 were not predominant in our study, despite the high prevalence of overall HPV infection. Nevertheless, the oncogenic potential of these types and the low coverage of the Pap test among women from riverside communities demonstrate a potential risk for the development of cervical lesions and their progression to cervical cancer, since the access to these communities is difficult and, in most cases, these women do not have access to primary care and public health services.
Keywords: human papillomavirus 16, human papillomavirus 18, epidemiology, cervical cancer screening, sexually transmitted diseases
Abstract
Resumo
Objetivo O objetivo deste estudo foi avaliar a prevalência global e tipo-específica da infecção pelo papilomavírus humano (HPV) entre mulheres que vivem em comunidades ribeirinhas do estado do Pará, Amazônia oriental, Brasil. Estas comunidades são habitadas por pessoas de baixa renda, e são acessíveis somente por meio de pequenos barcos. A citologia cervical e os fatores de risco para a infecção por HPV também foram avaliados.
Métodos Amostras cervicais de 353 mulheres de comunidades selecionadas foram coletadas para a análise citológica e para a detecção do HPV. A prevalência global e tipo-específica dos HPV-16 e HPV-18, principais tipos oncogênicos no mundo, foram avaliadas por meio de reação em cadeia de polimerase (PCR) convencional e PCR em tempo real. Os fatores de risco para a infecção por HPV foram avaliados a partir de questionários epidemiológicos.
Resultados A idade média das participantes foi de 37 anos (desvio padrão [DP] ± 13,7). A maioria era casada ou tinha um parceiro sexual fixo (79%) e baixo nível de escolaridade (80%) e de renda familiar mensal (< U$ 250; 53%). A prevalência global do HPV foi de 16,4% (n = 58), com 8 casos de HPV-16 (2,3%) e 5 casos de HPV-18 (1,4%). Aproximadamente 70% das mulheres entrevistadas nunca tinha realizado o exame preventivo de Papanicolau. Os resultados citológicos anormais foram encontrados em 27,5% (n = 97) das amostras, com taxas mais altas da infecção por HPV de acordo com a severidade das lesões (p = 0,026).
Conclusões As infecções por HPV-16 e HPV-18 não foram predominantes em nosso estudo, apesar da alta prevalência global da infecção por HPV. No entanto, o potencial oncogênico desses tipos e a baixa cobertura do exame de Papanicolau entre mulheres de comunidades ribeirinhas demonstram um risco potencial para o desenvolvimento de lesões cervicais e sua progressão para o câncer de colo do útero, uma vez que o acesso a essas comunidades é difícil e, na maioria dos casos, estas mulheres não têm acesso aos serviços de atenção primária e de saúde pública.
Palavras-chave: papilomavírus humano 16, papilomavírus humano 18, epidemiologia, rastreamento de câncer do colo do útero, doenças sexualmente transmissíveis
Introduction
The human papillomavirus (HPV) is capable of inducing skin or mucosa lesions in various regions of the body, both malignant and benign.1 Human papillomavirus infection is the most common sexually transmitted infection (STI) in the world, since most of the sexually active population is exposed to the virus at some moment in their lives.2
The infection caused by HPV is usually asymptomatic, having a limited evolution and often regressing spontaneously in up to 18 months in immunocompetent women.3 However, persistent infections by high-risk oncogenic types, mainly HPV-16 and HPV-18, which cause ∼ 70% of all cervical cancers (CC) in the world, can progress with the integration of viral DNA into the genome of the target cell, this process being the main carcinogenic factor for the development of premalignant lesions and, consequently, the evolution to a CC.4
The Brazilian Amazon is home to countless riverside communities, which are, for the most part, lacking in primary care and public health, sanitation and education. This situation occurs basically due to the difficult to access to these communities, usually made only by small boats, and for cultural reasons, like their fear of exams and lack of knowledge on the importance of screening. In the state of Pará, which is located in the Eastern Brazilian Amazon, there are several of these communities; however, little is known about HPV infection and CC among this population.
The official estimates indicate that the crude incidence rate of CC in Pará is of 20.52 per 100,000 women, the second most frequent cancer among women in the state, excluding nonmelanoma skin cancer.5 This high rate can be linked to the low coverage of the Papanicolau (Pap) test offered by the public health system, as well as to the high prevalence of HPV infection in the region.6 7 Therefore, the identification of indicators that can contribute to the development of healthcare actions for these communities is essential for the prevention of HPV infection and to reduce CC mortality rates.
The objective of this study was to estimate the overall and type-specific (HPV-16 and HPV-18) prevalence of HPV infection and correlate it with cervical intraepithelial lesions and other risk factors for CC among women from riverside communities of several municipalities located in the state of Pará, Brazil.
Methods
Study Site and Participants
In this cross-sectional study, we conducted an investigation of HPV infection and cervical screening in a spontaneous demand of women who have permanent residence in riverside communities in the state of Pará. Sixteen communities in 7 municipalities were visited between February and December 2008. Including all villages, 353 women were enrolled. All of them provided viable samples for the Pap and HPV tests.
Despite the recommendation of the Brazilian National Cancer Institute for the screening of women aged 25–648, we included women of all ages in the present study due to the difficult access to these communities and to the unusually high mortality rates of CC in our region. Thus, the inclusion criteria were sexually active women of all ages who signed the informed consent form (ICF) and who were not pregnant or menstruating.
The participants were instructed about the importance of the study, and were invited to participate in the research. Informed consent was obtained from all participants. The research protocol was approved by the Human Research Ethics Committee of the Center for Tropical Medicine (NMT from Portuguese) – Universidade Federal do Pará (UFPA) (protocol no. 050/2007). All samples were coded to ensure the privacy of the participants.
Socioeconomic, demographic, behavioral, sexual and reproductive history were collected through interviews and by filling out standardized epidemiological questionnaires. The people who performed the interviews were oriented about the study protocols and trained by the physician responsible for the collection of the cervical specimens.
Specimen Collection
Conventional cytological smears were obtained with an Ayres spatula (ectocervical sample) and endocervical brush (endocervical sample), extended in a glass slide, fixed with polyethylene glycol, and stained using the Pap technique. The samples were examined in the Laboratory of Pathology and Cytopathology, and the results were classified according to the 3rd edition of the Brazilian nomenclature for cervical cytological reports.8 A second endocervical brush was washed into microtubes containing 0.5 mL of saline that were stored at -20°C until the molecular analysis. The viral DNA was extracted using the standard phenol-chloroform protocol, and purified by ethanol precipitation.
General HPV Detection
The HPV polymerase chain reaction (PCR) was conducted using degenerate MY09/11 primers (Invitrogen, Carlsbad, California, US), which amplify a fragment of 449–458 nucleotides of a highly conserved region of the L1 viral gene.9 Each assay included positive and negative controls, and the suitability of the samples was assessed through amplification of a 268-bp fragment of the β-globin gene.10
Detection of HPV-16 and HPV-18
Human papillomavirus typing was performed using reagents from the Platinum qPCR SuperMix-UDG (Invitrogen, Carlsbad, California, US). Each reaction was prepared with a total volume of 15 μL (1 μL of DNA, 7.30 μL of mix, 0.375 μL of each probe, 0.15 μL of ROX Dye, 0.15 μL of magnesium, and 6.07 μL of ultrapure water). The amplification reaction consisted of 40 cycles of denaturation at 95°C for 30 seconds, hybridization at 60°C for 30 seconds, and extension at 72°C for 30 seconds. The results were analyzed using the StepOne software, version 2.0 (Applied Biosystems, Foster City, California, US). Each assay included positive and negative controls. The PCR real-time analyses for the detection of HPV-16 and -18 were conducted in the Immunopathology Laboratory of our institution.
Statistical Analysis
For the descriptive statistics, data were transferred from the questionnaires to Microsoft Excel (Microsoft Corporation, Redmond, WA, US) spreadsheets, in which graphs and tables were generated, as well as measures of central tendency and dispersion. The Chi-squared test was used to assess the association between the variables investigated in the project and the overall prevalence of HPV, and the G test was used to ascertain the association between the same variables and the prevalence of specific virus types (p < 0.05 were considered statistically significant for all data analyses conducted), both at a 95% confidence interval (95%CI). Women who did not respond on a given variable were excluded from the analyses. The analyses were performed using the BioEstat software, version 5.3 (Instituto Mamirauá, Tefé, AM, Brazil).11
Results
Total 353 women living in riverside communities from 7 municipalities in the state of Pará participated voluntarily in the present study. Among this sample, 16 (4.5%) women were from the city Belém (the capital of the state), 82 (23.3%) were from the region of Marajó Island (from the municipalities of Soure, Salvaterra and Cachoeira do Arari), 177 (50.1%) were from Northeastern Pará (from the towns of Cametá and Abaetetuba) and 78 (22.1%) were from Midwest Pará (from the town of Itaituba) (Fig. 1).
Fig. 1.
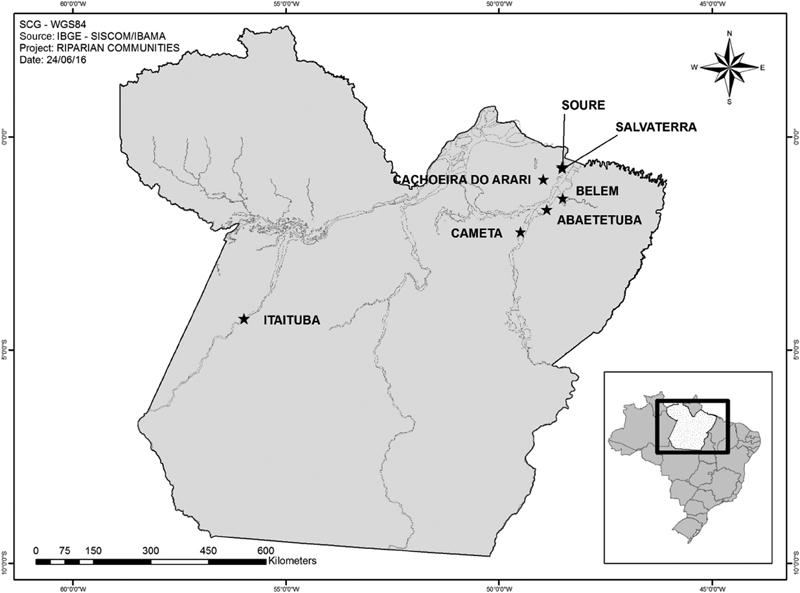
Map of the state of Pará, Northern Brazil.
The age of the participants ranged from 16 to 81 years (mean age 37 ± 13.7 years). They presented low schooling (68.8% only studied until elementary school or just know how to read and write, and 11.6% were illiterate), and their monthly incomes were lower than the Brazilian minimum wage (approximately U$ 250) (53%). The majority (79%) was married or with a fixed sexual partner, with the first intercourse after 15 years of age (58.9%), and more than half (56.1%) reported having had only 1 sexual partner their whole lives. Additionally, 91.8% reported 1 or more pregnancies, and 22.1% described at least 1 spontaneous or induced abortion. Most also reported they did not smoke (88.4%) drink alcohol (69.7%), or use contraceptive methods (73.7%) (Table 1). Almost 70% of the women surveyed had never undergone the Pap test.
Table 1. Sample characterization.
| Risk factors | Total | HPV+ (n) | HPV+ (%) | p |
|---|---|---|---|---|
| Age (years) | 0.003 | |||
| ≤ 20 | 26 | 9 | 34.6 | |
| 21–35 | 164 | 22 | 13.4 | |
| 36–51 | 110 | 15 | 13.6 | |
| 52–66 | 41 | 10 | 24.4 | |
| ≥ 67 | 12 | 2 | 16.6 | |
| Fixed sexual partner | < 0.001 | |||
| Present | 278 | 33 | 11.9 | |
| Absent | 75 | 25 | 33.3 | |
| Educational level | 0.622 | |||
| Illiterate | 41 | 8 | 19.5 | |
| Only reads and writes | 129 | 19 | 14.7 | |
| 9 years of basic education | 114 | 21 | 18.4 | |
| 12 years of basic education | 46 | 9 | 19.6 | |
| College graduated | 7 | 0 | 0 | |
| Family income (Brazilian minimum wage)* | 0.683 | |||
| < 1 | 187 | 33 | 17.6 | |
| ≥ 1 and ≤ 2 | 132 | 21 | 15.9 | |
| > 2 and ≤ 3 | 22 | 2 | 9.1 | |
| > 3 | 8 | 2 | 25 | |
| Sexual partners during lifetime | 0.117 | |||
| 1 | 198 | 26 | 13.1 | |
| 2 to 3 | 110 | 24 | 21.8 | |
| 4 to 5 | 20 | 2 | 10 | |
| ≥ 6 | 10 | 3 | 30 | |
| Number of pregnancies | 0.144 | |||
| None | 29 | 6 | 20.7 | |
| 1 to 2 | 88 | 18 | 20.5 | |
| 3 to 4 | 105 | 10 | 9.5 | |
| ≥ 5 | 131 | 24 | 18.3 | |
| Cytological diagnosis | 0.026 | |||
| Normal or inflammatory | 256 | 34 | 13.3 | |
| ASCUS | 28 | 4 | 14.3 | |
| AGUS | 12 | 5 | 41.6 | |
| ASCH | 3 | 0 | 0 | |
| LSIL | 48 | 14 | 29.2 | |
| HSIL | 6 | 2 | 33.3 | |
Abbreviations: AGUS, atypical glandular cell of undetermined significance; ASCH, atypical squamous cell, cannot exclude HSIL; ASCUS, atypical squamous cell of undetermined significance; HPV, human papillomavirus; HSIL, high-grade squamous intraepithelial lesion; LSIL, low-grade intraepithelial lesion.
Note: *The Brazilian minimum wage is equivalent to approximately U$ 250 per month.
There was no evidence of invasive carcinoma in any of the samples. Abnormal cytology results were found in a total of 97 samples (27.5%). High-grade squamous intraepithelial lesions (HSIL) were found in 6 (1.7%) participants, low-grade intraepithelial lesions (LSIL) in 48 (13.6%), atypical squamous cells of undetermined significance (ASCUS) in 28 (7.9%), atypical glandular cells of undetermined significance (AGUS) in 12 (3.4%), and atypical squamous cells, cannot exclude HSIL (ASCH) were found in 3 (0.9%) participants. Furthermore, an elevated number of inflammatory cases without the identification of the agent (70.5%) was observed. Only 7 samples (2%) presented normal cytology.
The overall prevalence of HPV infection was of 16.4% (58/353), whereas the prevalence of types 16 and 18 was of 2.3% (8/353) and 1.4% (5/353) respectively (including 1 case of co-infection by HPV-16 and HPV-18) (Table 2). Human papillomavirus infection was most common among women aged 20 years or younger (34.6%), and among women aged 52 to 66 years (24.4%) (p = 0.003). A statistically significant association between the presence of HPV and the cytological results, with higher rates of infection in samples with intraepithelial lesions than in normal cytology results (p = 0.026), was evidenced (Table 1).
Table 2. Status of HPV infection and viral type.
| Viral type | Age (years) | |||||
|---|---|---|---|---|---|---|
| ≤ 20 | 21–35 | 36–51 | 52–66 | ≥ 67 | Total | |
| HPV negative | 17 | 142 | 95 | 31 | 10 | 295 |
| HPV overall | 9 | 22 | 15 | 10 | 2 | 58 |
| HPV-16 | 1 | 5 | 1 | 1 | – | 8 |
| HPV-18 | 2 | 2 | 1 | – | – | 5 |
| HPV-16 and HPV-18 | – | 1 | – | – | – | 1 |
Abbreviations: HPV, human papillomavirus; HPV-16, human papillomavirus type 16; HPV-18, human papillomavirus type 18.
The sociodemographic and behavioral variables, as well as the reproductive history surveyed, showed no statistically significant association with HPV infection, except among the women who did not have a steady sexual partner, for whom the infection rates were 3 times higher than among women with a fixed sexual partner (33.3% versus 11% respectively) (p < 0.01) (Table 1). No association was found between infection by HPV-16 and HPV-18 and the variables investigated in the study (Table 3).
Table 3. G test of the association between selected risk factors and specific HPV types (16 and 18).
| Risk factors | HPV + | HPV-16 + | % | p | HPV-18 + | % | p |
|---|---|---|---|---|---|---|---|
| Age (years) | 0.59 | 0.35 | |||||
| ≤ 20 | 9 | 1 | 11.1 | 2 | 22.2 | ||
| 21–35 | 22 | 5 | 22.7 | 2 | 9.1 | ||
| 36–51 | 15 | 1 | 6.7 | 1 | 6.7 | ||
| 52–66 | 10 | 1 | 10 | 0 | 0 | ||
| ≥ 67 | 2 | 0 | 0 | 0 | 0 | ||
| Fixed sexual partner | 0.73 | ||||||
| Present | 33 | 5 | 15 | 4 | 12 | ||
| Absent | 25 | 3 | 12 | 1 | 4 | ||
| Cytological Results | 0.82 | 0.77 | |||||
| Normal or inflammatory | 33 | 3 | 9.1 | 2 | 6 | ||
| Atypical cells | 9 | 3 | 33.3 | 1 | 11.1 | ||
| LSIL | 14 | 2 | 14.3 | 2 | 14.3 | ||
| HSIL | 2 | 0 | 0 | 0 | 0 | ||
| Age at first sexual intercourse (years) | 0.68 | 0.07 | |||||
| ≤ 15 | 24 | 3 | 12.5 | 4 | 16.6 | ||
| 16–20 | 26 | 4 | 15.4 | 1 | 3.8 | ||
| ≥ 21 | 3 | 1 | 33.3 | 0 | 0 | ||
Abbreviations: HPV, human papillomavirus; HPV-16, human papillomavirus type 16; HPV-18, human papillomavirus type 18; HSIL, high-grade squamous intraepithelial lesion; LSIL, low-grade intraepithelial lesion.
Discussion
The present study was conducted among women from riverside communities in the Brazilian Amazon that are only accessible by river through small boats. Therefore, it is difficult for the inhabitants of these communities to access basic services such as health and education. Almost 70% of the women surveyed had never undergone the screening test for CC. Although geographically isolated, an elevated HPV prevalence was observed (16.4%), which included HPV-16 and HPV-18, which are associated with 70% of the CC cases worldwide.12
The prevalence of HPV infection demonstrated was similar to the data found in other studies with regional communities with similar characteristics, such as those who live in the towns of Tucuruí (14.2%)6 and Abaetetuba (11.4%),13 both in the state of Pará. However, the prevalence was lower than that of the indigenous tribes of the Amazon region belonging to Brazil (22.4% to 39.7%)14 15 and Paraguay (23.2%).16 Little is known about the prevalence of the high-risk HPVs -16 and -18 in these isolated communities in the Amazon, which makes it difficult to compare our results. In fact, to our knowledge, this is the first local study to assess the prevalence of these specific viral types among riverside populations.
It is important to point out that most of the researches reported in the literature identify the rates of infection and HPV types in a referenced demand of women who have lesions in the cervix, invasive or not, or women who seek healthcare services in order to undergo the Pap test, where there is a tendency to have higher rates of HPV infection and lesions of the uterine cervix associated with viral infection. The overall and specific prevalence of HPV demonstrated in this study was obtained from a spontaneous demand of women who received in their homes healthcare professionals and agreed to perform the Pap test. In Spain, a study with sampling features similar to the present one found a prevalence of HPV lower than 3%.17
The bimodal distribution of HPV infection found in this investigation is in agreement with several studies in the literature.6 18 19 The first peak between women aged 20 years or younger may be explained by the greater quantity and turnover of sexual partners, the irregularity in the use of a contraceptive barrier, and the fragility of the uterine cervix, which is still in maturation in young women.2 The elevated rates of infection in older women (aged between 52 and 66 years) is possibly associated with the gradual loss of immunity after menopause, which would facilitate the persistence of viral infection, or with new infections related to new sexual partners.20
The results also demonstrated that women who reported a fixed sexual partner had rates of infection 3 times smaller than women without a fixed sexual partner (p < 0.001). Similar data were found in a study conducted by Foliaki et al21, and they may be explained by limiting the primary route of viral transmission. Moreover, the association between HPV infection and the occurrence of multiple sexual partners is well established, mainly in women who reported having multiple sexual partners over the previous year.22 Additionally, the Pap test revealed an elevated number of inflammatory cases that can possibly be associated with concurrent sexually transmitted infections, like infections by Chlamydia trachomatis and Neisseria gonorrhoeae. As previously described, the inflammation caused by these pathogens can facilitate the infection by HPV.16 23 Unfortunately, it was not possible to perform molecular tests for the detection of these pathogens in the analyzed samples.
The combination of cytology and HPV screening used in the present study was effective in the identification of women with increased risk of developing CC. The use of primary high-risk HPV screening alone has been evaluated as an alternative to cytology-based CC screening methods in several countries, showing equivalent or superior effectiveness.24 However, the use of primary high-risk HPV screening needs to be better evaluated in populations such as riverside communities, and the complementary screening through the Pap test is still essential due to the elevated number of abnormal cytology results and inflammatory cases.
Additionally, the main carcinogenic types -16 and -18 were found only in 24% of the positive cases, and the 2 cytological results of HSIL were not associated with these genotypes, which may reflect in possible limitations to HPV vaccination in this population. Moreover, ∼ 70% of the participants underwent a Pap screening for the first time; the lack of access to these tests contributes to the high CC mortality rates found in Northern Brazil, and demonstrates the necessity of active search in this population.
A limitation of this study is related to the use of questionnaires to collect information on the risk factors of HPV infection. The statistical analyses were composed exclusively of information provided by the participants of the study, which may contain inaccuracies, omissions or lies for various reasons such as shame, fear or forgetfulness. In addition, the cross-sectional design precluded the use of time as a factor of cause of viral infection, since the risk factors and outcomes were collected at the same time, and the bias of reverse causality could not be extinguished.
Conclusion
Human papillomavirus infections were more frequent among women with multiple sexual partners and those with an abnormal Pap test. A bimodal distribution of the infection according to the age of the participants, with a first peak of infection among participants aged 20 years or younger, and a second peak among those aged between 52 and 66 years. There was no association between HPV-16 and HPV-18 and the risk factors evaluated in this study.
Despite the isolation of the study population from urban centers, a high prevalence of HPV infection was demonstrated. Infections by HPV-16 and HPV-18 were not predominant. However, due to the oncogenic potential of these types and the elevated percentage of abnormal cytology results, there is an increased risk of CC development among riverside women. These observations highlight the importance of specific actions aimed at preventing transmission, as well as actions to promote the screening of cervical lesions among the riverside communities of the Amazon region.
Acknowledgments
We wish to thank the healthcare professionals and women who participated in the study.
Conflicts of Interest The authors have no conflicts of interest to declare.
Authors' Contributions
DD performed the molecular identification of general and specific HPV, being primarily responsible for the analysis, interpretation of data, literature review and production of the manuscript. RV contributed to the draft of the manuscript, data interpretation, and the revision of the final version of the manuscript, providing suggestions. EB performed the cytological analysis of the samples and participated in the collection of the questionnaires. MP coordinated the collection of the samples and the application of the questionnaires. JM performed the molecular analysis of general and specific HPV, and helped in the interpretation of the data. MV was responsible for the statistical analysis of the research, and for the preparation of figures and tables. EI contributed to the analyses, data interpretation and critical review of the manuscript. HF contributed to the analyses, data interpretation and detection of HPV-16 and -18. MS was responsible for the study design, interpretation of data, and critical revision of the intellectual content of the manuscript. All authors read and approved the final draft of the manuscript.
References
- 1.Ferenczy A, Franco E. Persistent human papillomavirus infection and cervical neoplasia. Lancet Oncol. 2002;3(01):11–16. doi: 10.1016/s1470-2045(01)00617-9. [DOI] [PubMed] [Google Scholar]
- 2.de Sanjosé S, Diaz M, Castellsagué X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis Lancet Infect Dis 2007707453–459. [DOI] [PubMed] [Google Scholar]
- 3.Winer R L, Hughes J P, Feng Q, et al. Early natural history of incident, type-specific human papillomavirus infections in newly sexually active young women Cancer Epidemiol Biomarkers Prev 20112004699–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore M A, Tajima K. Cervical cancer in the asian pacific-epidemiology, screening and treatment. Asian Pac J Cancer Prev. 2004;5(04):349–361. [PubMed] [Google Scholar]
- 5.Brasil. Ministério da Saúde. Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2016: incidência do câncer no Brasil Rio de Janeiro: INCA; 2016 [Google Scholar]
- 6.Pinto DdaS, Fuzii H T, Quaresma J AS. Prevalence of genital HPV infection in urban and rural women in the Eastern Brazilian Amazon. Cad Saude Publica. 2011;27(04):769–778. doi: 10.1590/s0102-311x2011000400016. [DOI] [PubMed] [Google Scholar]
- 7.Vieira R C, Monteiro JdoS, Manso E P, et al. Prevalence of type-specific HPV among female university students from northern Brazil Infect Agent Cancer 20151021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Instituto Nacional de Câncer. Nomenclatura brasileira para laudos cervicais e condutas preconizadas. 3a ed Rio de Janeiro: INCA; 2012 [Google Scholar]
- 9.Manos M M, Ting Y, Wright D K, Lewis A J, Broker T R, Wolinsky S M. The use of polymerase chain reaction amplification for the detection of genital human papillomaviruses. Cancer Cells. 1989;7:209–214. [Google Scholar]
- 10.Gage J C, Partridge E E, Rausa A, et al. Comparative performance of human papillomavirus DNA testing using novel sample collection methods J Clin Microbiol 201149124185–4189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ayres M, Ayres Júnior M, Ayres D L, dos Santos A SS.BioEstat 5.3 [Internet] Tefé: Instituto de Desenvolvimento Sustentável Mamirauá; 2011 [cited 2016 Mar 22]. Available at: http://www.mamiraua.org.br/pt-br/downloads/programas/bioestat-versao-53/
- 12.Muñoz N, Bosch F X, Castellsagué X, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective Int J Cancer 200411102278–285. [DOI] [PubMed] [Google Scholar]
- 13.Duarte D V, Brito E B, Canto A SS, et al. Frequência e genotipagem do Papilomavírus humano em mulheres de comunidades ribeirinhas do Município de Abaetetuba, Pará, Brasil Rev Pan-Amaz Saúde 201010375–82. [Google Scholar]
- 14.Brito E B, Silva I D, Stávale J N, Taromaru E, Menezess R C, Martins S J. Amerindian women of the Brazilian Amazon and STD. Eur J Gynaecol Oncol. 2006;27(03):279–281. [PubMed] [Google Scholar]
- 15.Fonseca A J, Taeko D, Chaves T A, et al. HPV infection and cervical screening in socially isolated indigenous women inhabitants of the Amazonian rainforest PLoS One 20151007e0133635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendoza L, Mongelos P, Paez M, et al. Human papillomavirus and other genital infections in indigenous women from Paraguay: a cross-sectional analytical study BMC Infect Dis 201313531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Sanjose S, Almirall R, Lloveras B, et al. Cervical human papillomavirus infection in the female population in Barcelona, Spain Sex Transm Dis 20033010788–793. [DOI] [PubMed] [Google Scholar]
- 18.Dursun P, Senger S S, Arslan H, Kuşçu E, Ayhan A. Human papillomavirus (HPV) prevalence and types among Turkish women at a gynecology outpatient unit. BMC Infect Dis. 2009;9:191. doi: 10.1186/1471-2334-9-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lazcano-Ponce E, Herrero R, Muñoz N, et al. Epidemiology of HPV infection among Mexican women with normal cervical cytology Int J Cancer 20019103412–420. [DOI] [PubMed] [Google Scholar]
- 20.Molano M, Posso H, Weiderpass E, et al; HPV Study Group HPV Study. Prevalence and determinants of HPV infection among Colombian women with normal cytology Br J Cancer 20028703324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foliaki S, Brewer N, Pearce N, et al. Prevalence of HPV infection and other risk factors in a Fijian population Infect Agent Cancer 2014914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunne E F, Unger E R, Sternberg M, et al. Prevalence of HPV infection among females in the United States JAMA 200729708813–819. [DOI] [PubMed] [Google Scholar]
- 23.Shew M L, Fortenberry J D, Tu W, et al. Association of condom use, sexual behaviors, and sexually transmitted infections with the duration of genital human papillomavirus infection among adolescent women Arch Pediatr Adolesc Med 200616002151–156. [DOI] [PubMed] [Google Scholar]
- 24.Huh W K, Ault K A, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance Obstet Gynecol 201512502330–337. [DOI] [PubMed] [Google Scholar]


