Abstract
Abnormal uterine bleeding is a frequent condition in Gynecology. It may impact physical, emotional sexual and professional aspects of the lives of women, impairing their quality of life. In cases of acute and severe bleeding, women may need urgent treatment with volumetric replacement and prescription of hemostatic substances. In some specific cases with more intense and prolonged bleeding, surgical treatment may be necessary. The objective of this chapter is to describe the main evidence on the treatment of women with abnormal uterine bleeding, both acute and chronic. Didactically, the treatment options were based on the current International Federation of Gynecology and Obstetrics (FIGO) classification system (PALM-COEIN). The etiologies of PALM-COEIN are: uterine Polyp (P), Adenomyosis (A), Leiomyoma (L), precursor and Malignant lesions of the uterine body (M), Coagulopathies (C), Ovulatory dysfunction (O), Endometrial dysfunction (E), Iatrogenic (I), and Not yet classified (N). The articles were selected according to the recommendation grades of the PubMed, Cochrane and Embase databases, and those in which the main objective was the reduction of uterine menstrual bleeding were included. Only studies written in English were included. All editorial or complete papers that were not consistent with abnormal uterine bleeding, or studies in animal models, were excluded. The main objective of the treatment is the reduction of menstrual flow and morbidity and the improvement of quality of life. It is important to emphasize that the treatment in the acute phase aims to hemodynamically stabilize the patient and stop excessive bleeding, while the treatment in the chronic phase is based on correcting menstrual dysfunction according to its etiology and clinical manifestations. The treatment may be surgical or pharmacological, and the latter is based mainly on hormonal therapy, anti-inflammatory drugs and antifibrinolytics.
Keywords: PALM-COEIN, abnormal uterine bleeding, heavy menstrual bleeding, dysfunctional uterine bleeding, menorrhagia
Resumo
O sangramento uterino anormal é uma afecção frequente que pode afetar negativamente aspectos físicos, emocionais, sexuais e profissionais, piorando a qualidade de vida das mulheres. Nos casos de sangramento intenso e agudo, as mulheres podem necessitar de tratamento de urgência, com reposição volumétrica e substâncias hemostáticas. Há situações que necessitam de tratamento prolongado, e ainda situações em que o tratamento cirúrgico pode ser necessário. O objetivo deste estudo é descrever as principais evidências sobre o tratamento das mulheres com sangramento uterino anormal, tanto na fase aguda quanto na crônica. A apresentação do tratamento foi baseada no sistema de classificação (PALM-COEIN, na sigla em inglês) da Federação Internacional de Ginecologia e Obstetrícia (FIGO). As etiologias do PALM-COEIN são: Pólipo uterino (P), Adenomiose (A), Leiomiomia (L), lesões precursoras e Malignas do corpo uterino (M), Coagulopatias (C), distúrbios da Ovulação (O), disfunção Endometrial (E), Iatrogênicas (I), e não classificadas nos itens anteriores (N). Os artigos foram selecionados conforme os graus de recomendação das bases de dados PubMed, Cochrane e Embase que tivessem como objetivo o tratamento do sangramento uterino anormal em mulheres. Somente artigos escritos em inglês foram incluídos. Todos os editoriais ou papers completos que não tratassem de sangramento uterino anormal, ou estudos baseados em modelos animais, foram excluídos. O tratamento tem como objetivo a redução do fluxo menstrual, reduzindo morbidade e melhorando a qualidade de vida. O tratamento na fase aguda visa estabilizar hemodinamicamente a paciente e estancar o sangramento excessivo, enquanto a terapia da fase crônica é baseada na correção da disfunção menstrual, conforme sua etiologia ou conforme a manifestação clínica. O tratamento pode ser cirúrgico ou medicamentoso, sendo o segundo baseado principalmente em fármacos hormonais, anti-inflamatórios ou antifibrinolíticos.
Palavras-Chave: PALM-COEIN, sangramento uterino anormal, sangramento menstrual excessivo, hemorragia uterina disfuncional, menorragia
Introduction
Abnormal Uterine Bleeding (AUB) is the name currently used for changes in menstruation resulting from increased volume, duration, or frequency. Terms such as dysfunctional uterine bleeding or menorrhagia were abandoned. Abnormal Uterine Bleeding has great importance for its frequency, and because it negatively affects physical, emotional, sexual and professional aspects of the lives of women, worsening their quality of life (Fig. 1).1 (A)– ascending levels of evidence from (A) to (D).
Fig. 1.
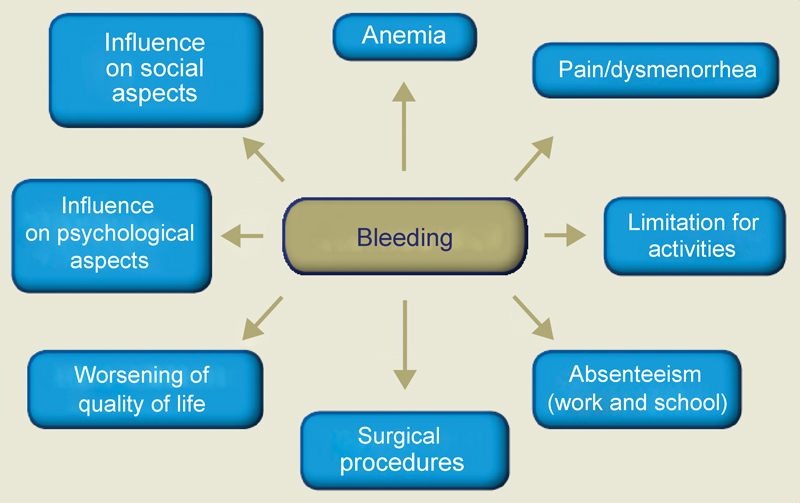
Repercussions of abnormal uterine bleeding on different aspects.
In 2011, a group of experts from the International Federation of Gynecology and Obstetrics (FIGO) proposed a classification for the disorders causing AUB that facilitated the understanding, evaluation and treatment of this condition, and enabled comparisons among the data from the scientific literature. This scheme is known as PALM-COEIN, in which each letter indicates one of the etiologies of bleeding (uterine Polyp [P], Adenomyosis [A], Leiomyoma [L], precursor and Malignant lesions of the uterine body [M], Coagulopathies [C], Ovulatory dysfunction [O], Endometrial dysfunction [E], Iatrogenic [I], and Not yet classified [N]) (Fig. 2). The PALM-COEIN system is applicable after excluding the pregnancy-related causes of bleeding.2 (D)
Fig. 2.
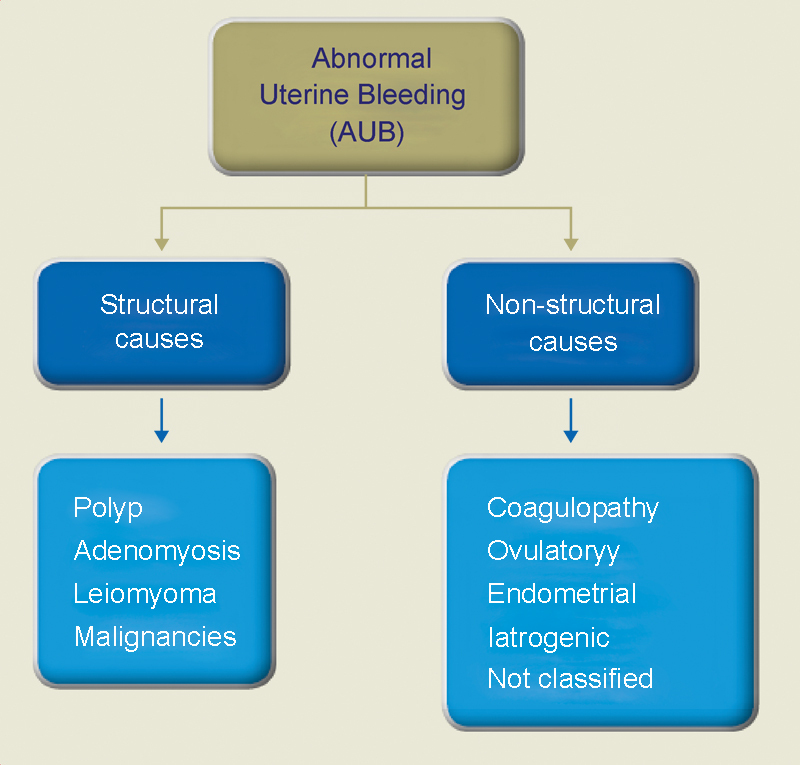
Classification of abnormal uterine bleeding according to the International Federation of Gynecology and Obstetrics (FIGO).
After excluding pregnancy, the initial evolution includes a detailed history of bleeding and medical history focusing on risk factors for endometrial cancer, coagulopathies, medications in use, concomitant diseases, as well a complete physical examination focusing on signs of polycystic ovarian syndrome, insulin resistance, thyroid diseases, petechiae, bruises, vagina or cervix lesions, and uterine size. To further the investigation, blood counts, ferritin dosage and pelvic ultrasonography may be performed.
In women with low risk for endometrial cancer and normal ultrasonography, excluding structural causes such as polyps, fibroids, endometrial thickening or other malignancies (classified in the PALM-COEIN system), the treatment can be pharmacological, through the use of drugs, or surgical. Structural lesions classified in the PALM-COEIN system have specific treatments according to the diagnosis.
The goal of the treatment is the reduction of the menstrual flow, thereby reducing morbidity and improving quality of life. Treatment by drug or pharmacological therapy is considered the first line whenever possible. The effectiveness and adherence to this alternative is strongly linked to the medical care and excellency of the doctor-patient relationship. The provision of information about therapeutic resources, their mechanism of action, their benefits, risks, information on the expected outcomes, and guidance on the long-term use may be crucial for treatment continuity.
This review covers the hormonal and non-hormonal therapeutic resources and the surgical treatment using the system proposed by FIGO, which are of the gynecologist's competence.
Propedeutics in Abnormal Uterine Bleeding
The etiologic diagnosis guides the therapy in AUB, and is directly associated with the success of the treatment. Only in acute and severe bleeding situations it is acceptable to establish treatment with the sole aim of staunching the bleeding and stabilizing the patient's hemodynamics, postponing the investigation for as soon as the bleeding is controlled.
In the initial clinical propedeutics, discard vaginal, cervical, and uterine lesions. The first two can be diagnosed already in the speculum exam, and deserve specific treatment that will not be the object of this article. The most complementary test that provides data for the conduction of AUB cases is the pelvic region ultrasound. It has excellent sensitivity (96%), but low specificity (13.8%) for endometrial injuries in general.3 (B)
In intracavitary injuries without diagnostic conclusion, hysterosonography or hysteroscopy are indicated, both with similar sensitivity4 (B), but the latter enables the guided biopsy of the lesion. The identification of benign injuries of the endometrium improves the accuracy in the therapeutic indication, and the differential diagnosis of endometrial neoplasia performed soon after the installation of the clinical picture directly interferes with the prognosis. These lesions are more frequent after menopause. The definitive diagnosis is made by biopsy of diffuse or focal lesions. In the latter, biopsy guided by hysteroscopy has greater sensitivity (94.4%) and specificity (99.6%).5 (C)
These tests are usually sufficient for the diagnosis of polyps, myomas, and malignant or pre-malignant lesions. Adenomyosis has a more imprecise diagnosis, with confirmation by an anatomopathological study after the hysterectomy. Nonetheless, the standardization of diagnostic criteria has advanced both by conventional and three-dimensional ultrasonography, and magnetic resonance imaging (MRI).6 (B)
Methods
A literature review was performed based on the PICOS structured method: P (patient: women with abnormal uterine bleeding), I (intervention: pharmacological treatment), C (control: surgical treatment), O (outcomes: bleeding control outcomes), S (systematic reviews, meta-analyzes and randomized clinical trials). The search was performed in the PubMed, Embase and Cochrane databases using the following terms: heavy menstrual bleeding OR menorrhagia OR abnormal menstrual bleeding AND medical treatment AND surgical treatment, by selecting systematic reviews, meta-analyzes, randomized controlled trials and reviews, and articles in English.
We describe the findings using some of these studies separated by the following outcomes: surgical treatment and drug or pharmacological treatment according to the etiologies classified in the PALM-COEIN system proposed by FIGO.
Results and Discussion
The treatments indicated for the different etiologies of AUB will be presented initially for AUB in the presence of structural lesions (PALM), then in the absence of lesions (COEIN). The evidence for the treatment of acute bleeding will be presented afterwards.
Treatment of Abnormal Uterine Bleeding of Structural Cause (PALM)
Neoplastic and pre-neoplastic alterations of the endometrium are greatly important for the differential diagnosis, but have a particularized behavior that will not be addressed in this section.
Polyp
In the presence of an endometrial polyp causing AUB, hysteroscopic polypectomy is an effective and safe option for the diagnosis and treatment, with rapid recovery and early return to activities.
Small polyps (< 0.5 cm) can be removed in the ambulatory setting using 5-Fr mechanical instruments (sharp scissors and/or grasping forceps) primarily for cost reasons. Larger polyps (> 0.5 cm) can be removed en bloc (by resection of the base of the implantation injury with a monopolar or bipolar electrode) or, alternatively, sectioned into fragments.7 (D)
Myoma
About 30% of the patients with leiomyomas will require treatment because of the presence of symptoms, including AUB. Pharmacological treatment can be used in the presence of symptoms, and it has as alternatives the same drugs available for the reduction of non-structural bleeding (which will be discussed later in this article). Surgical approach should be considered if there is no response to the clinical treatment. The path and type of approach will depend on the number, location, and size of the leiomyoma, as well as on the future desire of conception.8 (B)
Submucosal leiomyomas are more often associated with AUB. The best surgical approach is defined according to the proportion of submucosal or intramural components. When the majority of the lesion is intracavitary, the excision may be exclusively hysteroscopic, while lesions with a large intramural component should be approached by laparoscopy or, if not possible, laparotomically.
For hysteroscopic myomectomy, some criteria may increase the safety and success of surgery, considering the size of the leiomyoma, the penetration of the nodule into the myometrium, the extension of the base of the nodule, and the topography of the nodule in the uterus (Table 1).9 (D)
Table 1. Score to guide the course for myomectomy.
| Score | Penetration | Size | Base | Topography | Lateral wall |
|---|---|---|---|---|---|
| 0 | 0 | = 2 cm | = 1/3 | Low | + 1 |
| 1 | = 50% | > 2 to 5 cm | > 1/3 to 2/3 | Middle | + 1 |
| 2 | > 50% | > 5 cm | > 2/3 | Upper | + 1 |
| Score | + | + | + | + | = |
| Score | Group | Suggested conduct | |||
| 0 to 4 | I | Low complexity hysteroscopic myomectomy | |||
| 5 to 6 | II | Complex myomectomy. Consider the use of gonadotropin-releasing hormone or two-step surgery | |||
| 7 to 9 | III | Consider alternatives to the hysteroscopic technique | |||
Source: Lasmar RB, Barrozo PR, Dias R, Oiveira MA. Submucous fibroids: a new presurgical classification (STEP-w). J Minim Invasive Gynecol. 2005; 12(4):308–11.9 (D)
Advances in instrumental and surgical techniques have made hysteroscopic myomectomy the treatment of choice for leiomyomas with a submucosal component, especially when there is a desire to preserve fertility.10 (D) Depending on the patient's clinical condition, small leiomyomas (< 2 cm) may be removed in the ambulatory setting.11 12 (C, D) Leiomyomas larger than 3 cm are at an increased risk for operative complications and damage to the surrounding myometrium. In such cases, an alternative is to perform myomectomy in two-step surgeries (leiomyomas types 1–3, according to the FIGO classification).13 (D)
When the AUB is caused by intramural leiomyomas, myomectomy can be performed laparoscopically or laparotomically, depending on the location of the leiomyoma, the availability of materials, and the training of the surgeon. In very large leiomyomas, a gonadotropin-releasing hormone (GnRH) analogue may be used prior to surgery to reduce their volume. The GnRH analogue is recommended for three months, and surgery should be performed prior to the return of menstruation.14 (D) However, the patient should be alerted to the intraoperative need for conversion from surgery to hysterectomy. When it is impossible to perform a myomectomy, or when there is no desire to preserve fertility, hysterectomy is indicated for AUB control motivated by leiomyoma or endometrial polyp. It can be performed vaginally, laparoscopically or laparotomically.
In some cases of leiomyomas in which the patient desires to preserve fertility, and also in cases of severe adenomyosis, a new technique that may be employed is uterine arterial embolization (UAE), with the catheterization of the leiomyoma nourishing arteries by a vascular surgeon and injecting Gelfoam (Pfizer, New York City, NY, US) or polypropylene beads, thereby ceasing the blood flow of the myomas or the organ, and eliminating the myomas or reducing the adenomyosis.15 (C)
Although UAE is highly effective in reducing bleeding and the size of the myoma, it may be necessary to repeat the procedure in 15–20% of cases after successful embolization, and in up to 50% of cases of incomplete ischemia.16 17 (C,D) There are also concerns about the impact of UAE on the ovarian reserve.18 (C) The desire for future gestation is still recognized as a relative contraindication because there are not enough studies in the literature to guarantee good results. However, a randomized study presented favorable results for UAE regarding myomectomy in terms of gestation rate, childbirth and abortion.19 (A)
Adenomyosis
Often associated with bleeding and dysmenorrhea, adenomyosis is usually treated with a hysterectomy. However, studies show that symptoms can be controlled with suppressive therapies similar to those used for AUB without structural change, such as combined contraceptives, progestogens, and the levonorgestrel-releasing intrauterine system (LNG-IUS), especially when there is a desire to maintain the reproductive capacity.20 (C) Therefore, the therapies for bleedings of non-structural cause that could also apply to adenomyosis are described below.
Treatment of Abnormal Uterine Bleeding of Non-structural Cause (COEIN)
All causes of uterine bleeding in which it is not possible to identify a structural or anatomical change are included here. This is the case of coagulopathies, chronic anovulation, endometrial dysfunctions, bleedings secondary to the use of drugs or other drugs (iatrogenic), whether hormonal or not, and a group of other unclassified causes. In these cases, the principle of the therapy is to act on endometrial stability or the on the control of the factors leading to desquamation and endometrial healing. If this treatment fails, the available surgical options will also be presented.
Pharmacological or drug treatment
The drug treatment for AUB is based on the action of hormones and other inflammatory mediators on the endometrium, in addition to the hemostatic control of the bleeding (Table 2).21 22 The available options are:
Table 2. Pharmacological options for the treatment of acute and chronic abnormal uterine bleeding.
| Medication | Regime | Efficiency |
|---|---|---|
| Combined oral contraceptives |
Acute bleeding
Contraceptives with ethinyl estradiol 30 mcg or 35 mcg 1 tablet/day, every 8 hours, for 7 days, followed by 1 tablet/day for 3 weeks. Chronic bleeding Combined oral, combined transdermal contraceptives or combined vaginal ring - all according to the package insert. |
High |
| Oral progestogen |
Acute bleeding
Medroxyprogesterone acetate 20 mg, every 8 hours, for 7 days. Chronic bleeding Oral medroxyprogesterone acetate (2.5–10 mg), or norethisterone acetate (2.5–5 mg), or megestrol acetate (40-320 mg) at the dose recommended in the package insert, or micronized progesterone (200–400 mg), dydrogesterone (10 mg). No ovulatory dysfunction: 1 tablet/day from the 5th to 26th day of the cycle or continuously. With ovulatory dysfunction: adjust dose/day, use for 2 weeks every 4 weeks. |
High |
| Levonorgestrel-releasing intrauterine system |
Chronic bleeding
Insert the levonorgestrel-releasing intrauterine system every 5 years, with release of 20 mcg/day. |
High |
| Depot medroxyprogesterone acetate |
Chronic bleeding
150 mg intramuscularly injected every 12 weeks. |
Low/Moderate |
| Gonadotropin-releasing hormone analog |
Chronic bleeding
Leuprolide acetate (3.75 mg monthly or 11.25 mg quarterly) intramuscularly, or goserelin (3.6 mg monthly or 10.8 mg quarterly), or subdermal. |
High |
| Non-steroidal anti-inflammatory drugs |
Chronic bleeding
Ibuprofen 600 to 800 mg, every 8 hours, or mefenamic acid 500 mg every 8 hours. |
Moderate |
| Tranexamic acid |
Chronic bleeding
• Swedish Medical Products Agency (MPA): 1–1.5 g, 3 to 4 times a day orally, for 3 to 4 days (the dose may be increased for up to 1 g, 6 times a day). • European Medicines Agency (EMA): 1 g, 3 times a day, for 4 days (the dose may be increased, but respecting the maximum dose of 4 g per day). • US Food and Drug Administration (FDA): 1.3 g, 3 times a day, for up to 5 days, or 10 mg/kg intravenously (at a maximum dose of 600 mg/dose, every 8 hours, for 5 days [in cases of bleeding without structural lesion]). |
High |
Source: Bradley LD, Gueye NA. The medical management of abnormal uterine bleeding in reproductive-aged women. Am J Obstet Gynecol. 2016; 214(1):31–44;21 Karakus S, Kiran G, Ciralik H. Efficacy of micronized vaginal progesterone versus oral dydrogesterone in the treatment of irregular dysfunctional uterine bleeding: A pilot randomized controled trial. Aust N Z J Obstet Gynaecol. 2009; 49(6):685–8;30 American College of Obstetricians and Gynecologists. ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013; 121(4):891–6.22
-
Hormonal
Combined estrogen and progestogen;
Cyclic or continuous oral progestogen;
Injectable progestogen;
LNG-IUS;
Other options.
-
Non-hormonal
Non-steroidal anti-inflammatory drugs (NSAIDs);
Antifibrinolytics.
Hormone treatment
Combined estrogen and progestogen
Combined contraceptives (CCs) containing estrogen and progestogen reduce menstrual blood loss by 35 to 72%, and are a therapeutic option for most causes of AUB without structural change.23 24 25 (D, A, A) Combined monophasic contraceptives are generally used in cyclic schedules with pauses, but can also be administered continuously, and reduce the number of menstruation episodes. Literature studies are more frequent with formulations containing 30 mcg of ethinyl estradiol associated with levonorgestrel, but theoretically various formulations may be used.
In the literature, there are studies with different combinations in different regimens through oral route or vaginal ring proving the reduction of bleeding. Given the diversity of the associations, the comparison between them is difficult, but studies have shown more efficacy in monophasic oral regimens compared with mefenamic acid, naproxen, or danazol. Continuous regimens were also superior to the cyclic use of combined formulations.23 26 (D, B)
Recently, a formulation containing dienogest associated with estradiol valerate showed reduction of menstrual bleeding; hence, its indication for this purpose was approved by the Food and Drug Administration (FDA) of the United States in 2012. In Brazil, the indication for menstrual flow reduction is in the package insert.27 (C)
An important limitation to the use of Dienogest associated with estradiol valerate is the immediate reproductive desire, because these regimens have an anovulatory action. In the treatment of AUB, the use of CCs is also guided by the World Health Organization's (WHO) eligibility criteria for contraceptive methods, respecting the contraindications for estrogen use, such as hypertension, migraine with aura, smoking habits after 35 years, thrombophilia, among others.
Isolated systemic progestogen
Progesterone is a hormone produced in the female organism during the luteal phase of the menstrual cycle, and is responsible for the secretory transformation of the endometrium. When there is no fertilization, estrogen and progesterone levels fall, and menstruation occurs. There are several synthetic derivatives of progesterone in the market. Although its denomination is not standardized in Brazil, we will use the term progestogen.
Progestogens promote endometrial atrophy by various mechanisms, and have anti-inflammatory action, but there are still gaps in the knowledge of how they promote bleeding reduction. Although they may be indicated for most women, their use is particularly relevant for those with contraindications for estrogen, or who do not tolerate its use. There are different progestogens used by different routes and doses, namely, continuous use, cyclical, oral route, injected or intrauterine. The main limitation to the continuous use of progestogen alone is the unexpected bleeding resulting from endometrial atrophy.
Cyclic or continuous oral progestogen
Cyclic use: perhaps the most controversial of hormonal treatments is the cyclic use of progestogens, and this seems not to be the best therapeutic option for the control of uterine bleeding.21 (C) In the scientific literature, there are studies showing a 20% increase in menstrual bleeding with the cyclic use (oral administration for 7 to 10 days a month) of norethisterone.28 (B) An extensive review of the literature has concluded that the LNG-IUS, CCs, and antifibrinolytics are all superior to the cyclic use of progestogens.29 (A) These results show it is probably better to restrict this indication to AUB caused by ovulatory dysfunction, that is, in anovulatory women who do not want to get pregnant and cannot use other hormonal options. For these patients, there would be a benefit with the use of an oral progestogen for 12 to 14 days per month, mimicking the luteal phase of the menstrual cycle.
Dydrogesterone has a molecular structure similar to natural progesterone. The effect of 10 mg of dydrogesterone is comparable to the effect of 10 mg of medroxyprogesterone acetate. A study evaluated its use in women with excessive bleeding by comparing the use of 20 mg of oral dydrogesterone from the 15th day of the menstrual cycle for 10 days with the use of a 90-mg dose of vaginal micronized progesterone from days 17 to 27 of the menstrual cycle. It showed both treatments were similar in reducing the menstrual flow and regarding the presence of secretory endometrium at the end of the treatment. Satisfaction with the treatment and the presence of regular cycles after three months were also similar between the groups.30 (A)
Continuous use: continuous use of oral progestogen has proven effective in reducing the volume of the bleeding, and it may block menstruation periods, promoting amenorrhea in a percentage of women. Its use is based on the intention of producing endometrial atrophy, consequently reducing the estrogenic action on endometrial proliferation. It may be indicated for both anovulatory and ovulatory women with endometrial bleeding. The formulations cited in the literature are oral medroxyprogesterone acetate (2.5 to 10 mg daily), norethisterone (2.5 mg and 5 mg daily), megestrol acetate (40 mg and 320 mg daily), or micronized progesterone (200 mg and 400 mg daily), used from day 5 to 26 of the cycle or continuously. Norethisterone is well studied and prescribed at a dose of 5 mg 3 times a day, from days 5 to 26 of the menstrual cycle. It has frequent side effects related to the action of progestogens that may limit its use31 (A), such as irregular bleeding, mastalgia, headache, edema and acne.
Injectable progestogen
There is no conclusive evidence for the use of depot injectable progestogen (medroxyprogesterone acetate 150 mg for IM use every 3 months) in AUB. However, there are studies that show it can promote amenorrhea in up to 24% of women, suggesting it is a good option for women with increased bleeding. The side effects often lead to discontinuation of the use, mainly due to irregular bleeding, weight gain, and headache.32 (A)
Subdermal etonogestrel implant
There are not enough studies to point out the use of the etonogestrel implant in AUB.
Levonorgestrel-releasing intrauterine system
Most studies on the use of continuous progestogen refer to the use of LNG-IUS. The LNG-IUS releases 20 mcg of levonorgestrel daily, resulting, through several mechanisms, in endometrial atrophy with reduced bleeding. It is considered more effective than the oral treatments for AUB control.
In addition to the large reduction (71–96%) in bleeding volume33 (A) and consequent improvement in quality of life, the LNG-IUS seems to have better acceptance considering the prolonged treatment with less incidence of adverse effects.34 (A) This method should not be used when the uterine cavity is not regular, given the increased risk of expulsion. The most commonly reported adverse effect is the occurrence of unexpected bleeding, which is more frequent within the first months of use. In this situation, the use of tranexamic acid or anti-inflammatory drugs can bring benefits.35 (A)
In the comparison between the LNG-IUS and endometrial ablation, the rates of satisfaction and improvement in quality of life were similar, with fewer side effects and lower cost for the LNG-IUS. Regarding hysterectomy, even considering irregular bleedings with the LNG-IUS, the literature shows similar satisfaction rates for these treatments.36 (A)
All treatments containing progestogen alone may have the adverse effect of irregular bleeding, especially in the first three months of use. Although the initial goal is amenorrhea, it occurs in only 10–15% of users of oral progestogen alone, in 20% of users of subdermal progestogen-only implants, and more frequently in users of quarterly injectable (medroxyprogesterone acetate) and the LNG-IUS.37 (C) A systematic review by Abdel-Aleem and colleagues (2013) confirmed the difficulty in managing this type of bleeding. After extensive evaluation of the current literature, they concluded no therapy can be recommended with confirmed efficacy based on high-quality scientific evidence.38 (C) In this review, the use of estrogen, progestogen (combination or dose increase), combined contraceptives, non-steroidal anti-inflammatory drugs, antioxidants, antifibrinolytics, progesterone receptor modulators (mifepristone), selective estrogen receptor modulators (SERMs), antiangiogenic agents, and inhibitors of the metalloproteinases matrix (doxycycline) was evaluated. At the end of the study, compared with the placebo, they found a reduction in the time the bleeding stopped with the combination of tranexamic acid, and mifepristone combined with estrogen and doxycycline, even though it was weak evidence based on three small studies.38 (C)
Non-hormonal treatment
The non-hormonal treatment of AUB includes the use of antifibrinolytics or non-steroidal anti-inflammatory drugs (NSAIDs). It is particularly indicated for women who do not wish to use hormones or who have contraindications to use them, and those who want to get pregnant.
Antifibrinolytics
Studies have shown women with increased menstrual flow may have the fibrinolytic system activated during menstruation with accelerated degradation of the fibrin clot formed to contain the bleeding.
Medications acting by reducing fibrinolysis may reduce bleeding. Tranexamic acid medication is often indicated in these cases. Since its market launch, it has been prescribed for women with hemophilia, Von Willebrand disease, Glanzmann's thrombasthenia, and AUB with good results. However, there are still questions regarding the dose and the contraindications.
Tranexamic acid is an antifibrinolytic with a short half-life, and according to different literature sources, it should be used 3 to 4 times a day with a variable recommended dose:39 (D)
Swedish Medical Products Agency (MPA): 1 to 1.5 g, 3 to 4 times a day, orally, for 3 to 4 days (the dose may be increased when the volume is too great for up to 1 g, 6 times a day);
European Medicines Agency (EMA): 1 g, 3 times a day, for 4 days (the dose may be increased, but respecting the maximum dose of 4 g a day).
U.S. Food and Drug Administration (FDA): 1.3 g, 3 times a day, for up to 5 days.
All of these recommendations are for use in days of bulky bleeding. The side effects are few and related to gastrointestinal symptoms. History of thromboembolism or renal failure are contraindications to tranexamic acid. A reduction of up to 50% in bleeding volume can be expected.40 41 42 (C, B, A)
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs act by inhibiting cyclooxygenase, the catalysis enzyme of the transformation of arachidonic acid into prostaglandin and thromboxane. Studies comparing normal and increased bleeding have shown that increased inflammation in the endometrium is associated with increased blood loss during menstruation, serving as basis for the indication of NSAIDs in the treatment of AUB, since they limit the production of inflammatory mediators. They can also be used alone or as an adjunctive therapy for the hormonal treatment.
Perhaps the most studied NSAID for this purpose is mefenamic acid, which provides 25 to 50% reduction in bleeding volume. It should be used during menstruation, and has the benefit of reducing dysmenorrhea. The most common side effects are related to gastrointestinal symptoms, so it should be avoided in women with a history of ulcer.28 43 (B, C)
A recent literature review44 (A) compared anti-inflammatory drugs with placebos, and found that the real drug caused menstrual flow reduction, but tranexamic acid and LNG-IUS cause greater reduction. Anti-inflammatories were also compared with Danazol, which causes greater bleeding reduction, but has more obvious side effects. The same review compared mefenamic acid with naproxen, and found no difference between the two.
Some authors suggest the reassessment of bleeding reduction after 3months of use, but ∼ 52% of women will still experience bleeding above normal (80 mL) despite the use of NSAIDs. If the control is adequate, the use can be maintained.
Other therapeutic options
Gonadotropin-releasing hormone analogs may be considered prior to surgery, in myomas, for example, particularly to enable the recovery of the organism and a reduction in volume. They are used when other hormonal methods are contraindicated, for a short period of time until the conditions for surgery are adequate. It is necessary to consider the costs and frequent side effects. Evidences for the use of desmopressin in AUB are scarce and still inconclusive for its recommendation.45 (B)
Surgical treatment of abnormal uterine bleeding without structural lesion
Surgical treatment in AUB with non-structural cause is indicated when the clinical treatment fails. Among the forms of surgical treatment, there are endometrial ablation and hysterectomy.
Endometrial ablation
The development of hysteroscopic techniques for endometrial ablation inaugurated the phase of the conservative treatment of AUBs without structural lesion, constituting a less invasive alternative to hysterectomy. The purpose of this technique is to promote the destruction of the endometrium with damage in its basal layer, hence preventing its regeneration. Endometrial ablation shows good results when the uterus hysterometry is < 10 cm. Several endometrial destruction techniques may be employed, all with relatively similar success, leading to significant improvement in bleeding, and to an amenorrhea rate of around 40 to 50% after 1 year.
There are several methods of endometrial destruction (laser, vaporization, thermal balloon, cryoablation, microwave ablation, bipolar radiofrequency). Currently, endometrial ablation is classified as first generation (hysteroscopic route) or second generation (non-hysteroscopic route) performed with thermal balloons. Although newer techniques are easier to perform than traditional techniques based on hysteroscopy, they all have similar results. However, some require special equipment and specific training, making their routine performance difficult.46 47 48 49 (A, B, B, A) In addition, hysteroscopic ablation enables the anatomopathological examination with the resected material.
Both endometrial ablation and hysterectomy are effective procedures in the treatment of AUB, with high satisfaction rates. Although hysterectomy is associated with a longer surgical time, longer recovery period and higher rates of postoperative complications, it offers better and more definitive results for the treatment of AUB. In turn, the cost of endometrial ablation is significantly lower than that of hysterectomy, but repetition of the surgical procedure is often necessary, and, therefore, the difference in cost narrows over time.49 (A)
Hysterectomy
Hysterectomy is an exception treatment for AUB of non-structured cause, and has a high index of patient satisfaction because it is curative. In randomized studies comparing hysterectomy with endometrial ablation, higher satisfaction rates among women undergoing hysterectomy were found.50 51 (D, D) The comparison of hysterectomy with the LNG-IUS showed no difference in satisfaction rates. However, the analysis of the high costs of the surgical treatment, the prolonged time away from daily activities, the risk of infection, and the surgical complications results in the recommendation of this method uniquely for cases in which all therapeutic alternatives have failed, and when the patient no longer wants children.36 52 53 54 (A, C, A, C) In some exceptional cases, if the patient does not accept the conservative treatment or has a contraindication to other available treatments, she may decide for hysterectomy together with the physician.55 (D)
Treatment of Acute Abnormal Uterine Bleeding
When the blood loss is acute and significant, and the patient is anemic and hypovolemic, the first step is to reestablish the hemodynamic balance using crystalloid and colloid solutions. In some cases, blood transfusion may be necessary. At the same time, it is essential to stop the bleeding. In the literature, there are different schemes with this indication. The following medications should be considered:
Intravenous estrogen;
Multidose monophasic combined oral contraceptive;
Multidose oral progestogen; and
Tranexamic acid.
Using high doses of intravenous estrogen causes rapid growth of the endometrium, stimulates the contraction of the uterine arteries, and promotes platelet aggregation and coagulation. A study in the literature showed control of bleeding in 72% of women treated with intravenous conjugated estrogen (CE).56 (A) The use of 25 mg intravenous CE every 4 to 6 hours for 24 hours is suggested, followed by the use of estrogen combined with progestogen, or by the use of progestogen alone after initial bleeding control. Unfortunately, currently there is no estrogen available for intravenous use in Brazil. Thus, we use the other hormonal options, as explained below.
Theoretically, all combined oral contraceptives can be used to treat the acute form of AUB, but the amount of evidence in the literature is relatively restricted. A study evaluated the use of ethinyl estradiol 35 mcg associated with monophasic norethisterone 1 mg at a dose of 1 tablet 3 times a day for 1 week, followed by 1 tablet a day for another 3 weeks, with bleeding control in 88% of women.57 (A) Another therapeutic option in women with acute AUB is the use of multiple doses of progestogen, especially indicated in cases when the use of estrogens is contraindicated. Medroxyprogesterone acetate 20 mg may be used 3 times a day for a week followed by a daily dose for 3 weeks.57 (A) The use of high hormonal doses can bring side effects such as nausea and vomiting.
After controlling bleeding and maintaining the therapy at smaller doses for a time similar to that of a menstrual cycle, discuss the need to maintain control of the cycle with medication for three consecutive months, and proceed with the etiological investigation.
Other options suggested in the literature are the use of a GnRH antagonist associated with an aromatase inhibitor or a GnRH antagonist (to prevent initial stimulation by the release of estrogen). Intrauterine tamponade can also be considered, using the Foley probe with an inflated balloon with 3–10 mL. The use of antifibrinolytic substances, such as tranexamic acid, may greatly aid in the control of bulky bleeding, usually used adjunctively and associated with other alternatives.
Final Considerations
The International Federation of Gynecology and Obstetrics recommends basing the classification of the etiologies of AUB on the PALM-COEIN system, which comprises the structural and non-structural causes of uterine bleeding, excluding gestational causes.
If there is acute bleeding with impairment of the patient's general condition, her hemodynamic stabilization should be prioritized, followed by the immediate start of treatment, whether clinical or surgical, even if the bleeding cause is not completely established, ruling out only vaginal and cervical lesions and pregnancy.
In cases of AUB without systemic repercussion, identifying the cause of the bleeding is mandatory before the start of treatment. Considering the main diagnosis of this clinical manifestation, pregnancy and the presence of vaginal and cervical lesions should be excluded by physical examination. Afterwards, an evaluation of the uterine cavity by imaging exams should be performed to identify the presence of organic lesions in the endometrial cavity.
In the presence of endometrial lesions such as endometrial polyps and submucosal leiomyomas, surgical treatment may be indicated. The only definitive treatment for adenomyosis is hysterectomy, but the control of symptoms by medical drug treatment is not rare.
In cases of intramural myomas, with an increase of uterine bleeding, the first therapeutic option is pharmacological, and there may be an improvement in the bleeding in some cases, avoiding an unnecessary surgical procedure. If there is no response to the clinical treatment, surgical treatment should be recommended. The surgical access route and type of surgery will depend on the number, location and size of the myoma, and the patient's desire for pregnancy.
If there is an AUB of non-structural cause, clinical treatment is always the first option. The main therapeutic options are described in Table 2
If there is no response to the clinical treatment in bleedings of non-structural cause, there are also surgical therapeutic options, such as endometrial ablation (by thermal balloon or hysteroscopy), or even hysterectomy.
The various therapeutic options available for the treatment of AUB should be used rationally to allow their control, leaving surgical procedures for specific situations and avoiding unnecessary surgical procedures.
Conflicts of Interest The authors have no conflicts of interest to declare.
This revision is part of the Series, Guidelines and Recommendations of the Federação Brasileira das Associações de Ginecologia e Obstetrícia – FEBRASGO, elaborated by the Specialized National Committees in Endocrine Gynecology.
References
- 1.Liu Z, Doan Q V, Blumenthal P, Dubois R W. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(03):183–194. doi: 10.1111/j.1524-4733.2007.00168.x. [DOI] [PubMed] [Google Scholar]
- 2.Munro M G, Critchley H O, Fraser I S; FIGO Menstrual Disorders Working Group. The FIGO classification of causes of abnormal uterine bleeding in the reproductive years Fertil Steril 201195072204–2208., 2208.e1–2208.e3 [DOI] [PubMed] [Google Scholar]
- 3.Babacan A, Gun I, Kizilaslan C, et al. Comparison of transvaginal ultrasonography and hysteroscopy in the diagnosis of uterine pathologies Int J Clin Exp Med 2014703764–769. [PMC free article] [PubMed] [Google Scholar]
- 4.Farquhar C, Ekeroma A, Furness S, Arroll B. A systematic review of transvaginal ultrasonography, sonohysterography and hysteroscopy for the investigation of abnormal uterine bleeding in premenopausal women. Acta Obstet Gynecol Scand. 2003;82(06):493–504. doi: 10.1034/j.1600-0412.2003.00191.x. [DOI] [PubMed] [Google Scholar]
- 5.Ribeiro C T, Rosa-E-Silva J C, Silva-de-Sá M F, et al. Hysteroscopy as a standard procedure for assessing endometrial lesions among postmenopausal women Sao Paulo Med J 200712506338–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbott J A. Adenomyosis and abnormal uterine bleeding (AUB-A)-pathogenesis, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2017;40:68–81. doi: 10.1016/j.bpobgyn.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Di Spiezio Sardo A, Calagna G, Guida M, Perino A, Nappi C. Hysteroscopy and treatment of uterine polyps. Best Pract Res Clin Obstet Gynaecol. 2015;29(07):908–919. doi: 10.1016/j.bpobgyn.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Donnez J, Dolmans M M. Uterine fibroid management: from the present to the future. Hum Reprod Update. 2016;22(06):665–686. doi: 10.1093/humupd/dmw023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lasmar R B, Barrozo P R, Dias R, Oiveira M A. Submucous myomas: a new presurgical classification to evaluate the viability of hysteroscopic surgical treatment--preliminary report. J Minim Invasive Gynecol. 2005;12(04):308–311. doi: 10.1016/j.jmig.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Emanuel M H. Hysteroscopy and the treatment of uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2015;29(07):920–929. doi: 10.1016/j.bpobgyn.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Bettocchi S, Ceci O, Nappi L, et al. Operative office hysteroscopy without anesthesia: analysis of 4863 cases performed with mechanical instruments J Am Assoc Gynecol Laparosc 2004110159–61. [DOI] [PubMed] [Google Scholar]
- 12.Vilos G A, Allaire C, Laberge P Y, Leyland N; SPECIAL CONTRIBUTORS. The management of uterine leiomyomas J Obstet Gynaecol Can 20153702157–178. [DOI] [PubMed] [Google Scholar]
- 13.Munro M G, Critchley H O, Broder M S, Fraser I S; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age Int J Gynaecol Obstet 2011113013–13. [DOI] [PubMed] [Google Scholar]
- 14.Moghissi K S. A clinician's guide to the use of gonadotropin-releasing hormone analogues in women. Medscape Womens Health. 2000;5(01):5. [PubMed] [Google Scholar]
- 15.Ravina J H, Herbreteau D, Ciraru-Vigneron N, et al. Arterial embolisation to treat uterine myomata Lancet 1995346(8976):671–672. [DOI] [PubMed] [Google Scholar]
- 16.Mara M, Kubinova K. Embolization of uterine fibroids from the point of view of the gynecologist: pros and cons. Int J Womens Health. 2014;6:623–629. doi: 10.2147/IJWH.S43591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spies J B. Current role of uterine artery embolization in the management of uterine fibroids. Clin Obstet Gynecol. 2016;59(01):93–102. doi: 10.1097/GRF.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 18.Kaump G R, Spies J B. The impact of uterine artery embolization on ovarian function. J Vasc Interv Radiol. 2013;24(04):459–467. doi: 10.1016/j.jvir.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Mara M, Maskova J, Fucikova Z, Kuzel D, Belsan T, Sosna O. Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Cardiovasc Intervent Radiol. 2008;31(01):73–85. doi: 10.1007/s00270-007-9195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pontis A, D'Alterio M N, Pirarba S, de Angelis C, Tinelli R, Angioni S. Adenomyosis: a systematic review of medical treatment. Gynecol Endocrinol. 2016;32(09):696–700. doi: 10.1080/09513590.2016.1197200. [DOI] [PubMed] [Google Scholar]
- 21.Bradley L D, Gueye N A. The medical management of abnormal uterine bleeding in reproductive-aged women. Am J Obstet Gynecol. 2016;214(01):31–44. doi: 10.1016/j.ajog.2015.07.044. [DOI] [PubMed] [Google Scholar]
- 22.American College of Obstetricians and Gynecologists. ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women Obstet Gynecol 201312104891–896. [DOI] [PubMed] [Google Scholar]
- 23.Fraser I S, Kovacs G T. The efficacy of non-contraceptive uses for hormonal contraceptives. Med J Aust. 2003;178(12):621–623. doi: 10.5694/j.1326-5377.2003.tb05387.x. [DOI] [PubMed] [Google Scholar]
- 24.Uhm S, Perriera L. Hormonal contraception as treatment for heavy menstrual bleeding: a systematic review. Clin Obstet Gynecol. 2014;57(04):694–717. doi: 10.1097/GRF.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 25.Iyer V, Farquhar C, Jepson R. Oral contraceptive pills for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000;(02):CD000154. doi: 10.1002/14651858.CD000154. [DOI] [PubMed] [Google Scholar]
- 26.Kaunitz A M, Portman D J, Hait H, Reape K Z. Adding low-dose estrogen to the hormone-free interval: impact on bleeding patterns in users of a 91-day extended regimen oral contraceptive. Contraception. 2009;79(05):350–355. doi: 10.1016/j.contraception.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 27.Braunstein J B, Hausfeld J, Hausfeld J, London A. Economics of reducing menstruation with trimonthly-cycle oral contraceptive therapy: comparison with standard-cycle regimens. Obstet Gynecol. 2003;102(04):699–708. doi: 10.1016/s0029-7844(03)00738-5. [DOI] [PubMed] [Google Scholar]
- 28.Cameron I T, Haining R, Lumsden M A, Thomas V R, Smith S K. The effects of mefenamic acid and norethisterone on measured menstrual blood loss. Obstet Gynecol. 1990;76(01):85–88. [PubMed] [Google Scholar]
- 29.Matteson K A, Rahn D D, Wheeler T L, II, et al; Society of Gynecologic Surgeons Systematic Review Group. Nonsurgical management of heavy menstrual bleeding: a systematic review Obstet Gynecol 201312103632–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karakus S, Kiran G, Ciralik H. Efficacy of micronised vaginal progesterone versus oral dydrogestrone in the treatment of irregular dysfunctional uterine bleeding: a pilot randomised controlled trial. Aust N Z J Obstet Gynaecol. 2009;49(06):685–688. doi: 10.1111/j.1479-828X.2009.01093.x. [DOI] [PubMed] [Google Scholar]
- 31.Hickey M, Higham J M, Fraser I. Progestogens with or without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Rev. 2012;(09):CD001895. doi: 10.1002/14651858.CD001895.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Multinational comparative clinical trial of long-acting injectable contraceptives: norethisterone enanthate given in two dosage regimens and depot-medroxyprogesterone acetate. Final report. Contraception. 1983;28(01):1–20. doi: 10.1016/s0010-7824(83)80002-x. [DOI] [PubMed] [Google Scholar]
- 33.Stewart A, Cummins C, Gold L, Jordan R, Phillips W. The effectiveness of the levonorgestrel-releasing intrauterine system in menorrhagia: a systematic review. BJOG. 2001;108(01):74–86. doi: 10.1111/j.1471-0528.2001.00020.x. [DOI] [PubMed] [Google Scholar]
- 34.Lethaby A, Hussain M, Rishworth J R, Rees M C. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2015;(04):CD002126. doi: 10.1002/14651858.CD002126.pub3. [DOI] [PubMed] [Google Scholar]
- 35.Andersson K, Odlind V, Rybo G. Levonorgestrel-releasing and copper-releasing (Nova T) IUDs during five years of use: a randomized comparative trial. Contraception. 1994;49(01):56–72. doi: 10.1016/0010-7824(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 36.Marjoribanks J, Lethaby A, Farquhar C. Surgery versus medical therapy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2016;(01):CD003855. doi: 10.1002/14651858.CD003855. [DOI] [PubMed] [Google Scholar]
- 37.Royal College of Obstetricians and Gynaecologists. Faculty of Sexual & Reproductive Healthcare Clinical Guidance. Management of unscheduled bleeding in women using hormonal contraception London: Faculty of Sexual and Reproductive Healthcare; 2009. [Internet]. [cited 2017 Feb 2]. Available from: https://www.rcog.org.uk/globalassets/documents/guidelines/unscheduledbleeding23092009.pdf
- 38.Abdel-Aleem H, d'Arcangues C, Vogelsong K M, Gaffield M L, Gülmezoglu A M. Treatment of vaginal bleeding irregularities induced by progestin only contraceptives. Cochrane Database Syst Rev. 2013;(10):CD003449. doi: 10.1002/14651858.CD003449.pub4. [DOI] [PubMed] [Google Scholar]
- 39.Tengborn L, Blombäck M, Berntorp E. Tranexamic acid--an old drug still going strong and making a revival. Thromb Res. 2015;135(02):231–242. doi: 10.1016/j.thromres.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 40.Andersch B, Milsom I, Rybo G. An objective evaluation of flurbiprofen and tranexamic acid in the treatment of idiopathic menorrhagia. Acta Obstet Gynecol Scand. 1988;67(07):645–648. doi: 10.3109/00016348809004279. [DOI] [PubMed] [Google Scholar]
- 41.Gleeson N C, Buggy F, Sheppard B L, Bonnar J. The effect of tranexamic acid on measured menstrual loss and endometrial fibrinolytic enzymes in dysfunctional uterine bleeding. Acta Obstet Gynecol Scand. 1994;73(03):274–277. doi: 10.3109/00016349409023453. [DOI] [PubMed] [Google Scholar]
- 42.Lukes A S, Moore K A, Muse K N, et al. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial Obstet Gynecol 201011604865–875. [DOI] [PubMed] [Google Scholar]
- 43.Maybin J A, Critchley H O. Medical management of heavy menstrual bleeding. Womens Health (Lond) 2016;12(01):27–34. doi: 10.2217/whe.15.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lethaby A, Duckitt K, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2013;(01):CD000400. doi: 10.1002/14651858.CD000400.pub3. [DOI] [PubMed] [Google Scholar]
- 45.Ray S, Ray A. Non-surgical interventions for treating heavy menstrual bleeding (menorrhagia) in women with bleeding disorders. Cochrane Database Syst Rev. 2016;11:CD010338. doi: 10.1002/14651858.CD010338.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fergusson R J, Lethaby A, Shepperd S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2013;(11):CD000329. doi: 10.1002/14651858.CD000329.pub2. [DOI] [PubMed] [Google Scholar]
- 47.Gupta B, Mittal S, Misra R, Deka D, Dadhwal V. Levonorgestrel-releasing intrauterine system vs. transcervical endometrial resection for dysfunctional uterine bleeding. Int J Gynaecol Obstet. 2006;95(03):261–266. doi: 10.1016/j.ijgo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 48.Vilos G A, Fortin C A, Sanders B, Pendley L, Stabinsky S A. Clinical trial of the uterine thermal balloon for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 1997;4(05):559–565. doi: 10.1016/s1074-3804(05)80089-1. [DOI] [PubMed] [Google Scholar]
- 49.Lethaby A, Penninx J, Hickey M, Garry R, Marjoribanks J. Endometrial resection and ablation techniques for heavy menstrual bleeding. Cochrane Database Syst Rev. 2013;(08):CD001501. doi: 10.1002/14651858.CD001501.pub4. [DOI] [PubMed] [Google Scholar]
- 50.Moore A A. Heavy menstrual bleeding. Adv NPs PAs. 2013;4(01):21–23. [PubMed] [Google Scholar]
- 51.Livingstone M, Fraser I S. Mechanisms of abnormal uterine bleeding. Hum Reprod Update. 2002;8(01):60–67. doi: 10.1093/humupd/8.1.60. [DOI] [PubMed] [Google Scholar]
- 52.Clegg J P, Guest J F, Hurskainen R. Cost-utility of levonorgestrel intrauterine system compared with hysterectomy and second generation endometrial ablative techniques in managing patients with menorrhagia in the UK. Curr Med Res Opin. 2007;23(07):1637–1648. doi: 10.1185/030079907x199709. [DOI] [PubMed] [Google Scholar]
- 53.Bhattacharya S, Middleton L J, Tsourapas A, et al; International Heavy Menstrual Bleeding Individual Patient Data Meta-analysis Collaborative Group. Hysterectomy, endometrial ablation and Mirena® for heavy menstrual bleeding: a systematic review of clinical effectiveness and cost-effectiveness analysis Health Technol Assess 20111519iii–xvi., 1–252 Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Unger J B, Meeks G R.Hysterectomy after endometrial ablation Am J Obstet Gynecol 1996175061432–1436., discussion 1436–1437 [DOI] [PubMed] [Google Scholar]
- 55.Mayor S.NICE says hysterectomy must be last option for heavy menstrual bleeding BMJ 2007334(7586):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DeVore G R, Owens O, Kase N. Use of intravenous Premarin in the treatment of dysfunctional uterine bleeding--a double-blind randomized control study. Obstet Gynecol. 1982;59(03):285–291. [PubMed] [Google Scholar]
- 57.Munro M G, Mainor N, Basu R, Brisinger M, Barreda L. Oral medroxyprogesterone acetate and combination oral contraceptives for acute uterine bleeding: a randomized controlled trial. Obstet Gynecol. 2006;108(04):924–929. doi: 10.1097/01.AOG.0000238343.62063.22. [DOI] [PubMed] [Google Scholar]


