Abstract
Background
Advanced radiological stage of knee osteoarthritis (OA) is predictive of poor response to viscosupplementation (VS). To date, the impact of x-ray features on the duration of effectiveness (DE) of VS has not been investigated.
Objectives
To investigate the radiological features associated with DE of VS in patients with knee OA.
Methods
Cross-sectional study in patients with knee OA treated with 1 injection of cross-linked hyaluronic acid (HA). The primary outcome was DE, self-assessed by the patients in weeks of effectiveness. Radiological features (joint space narrowing—JSN topography and Kellgren-Lawrence [K-L] grade) associated with DE were studied.
Results
Fifty-one patients—33 females (76 knees)—were analyzed. The average DE was 52.0 (24.7) weeks (range, 13-155 weeks). In the bivariate analysis, DE was 14 weeks longer in those with K-L grades 1 and 2 (62.6 ± 36.4 weeks) than in those with K-L 3 and 4 (48.9 ± 18.6) (P = 0.03). DE was not significantly different according to the involved compartment(s). It was significantly longer in men than in women (60 ± 31.4 vs. 47 ± 16 weeks; P = 0.035). In multivariate analysis, K-L grade (1-2 vs. 3-4) (P = 0.007), male gender (0.02), and older age (0.04) were independently associated with a longer DE.
Conclusion
DE of a single injection of extended-release HA is longer in K-L 1-2 than in K-L 3-4 OA knees, regardless of the JSN topography. However, even the patients with more advanced OA benefited from HANOX-M-XL injection for an average duration barely less than 1 year.
Keywords: hyaluronic acid, viscosupplementation, knee, osteoarthritis, cross-linking, effectiveness, Kellgren-Lawrence scale, HANOX-M-XL
Introduction
Knee osteoarthritis (OA) is one of the main causes of pain and disability in subjects aged above 50 years, significantly impairing their quality of life. 1 Standard conservative treatments for knee OA include a combination of non-pharmacological and pharmacological modalities,2 -4 as none can be individually classified as highly effective, except total knee replacement. In the early 1990s, E. A. Balazs introduced the concept of viscosupplementation (VS). He hypothesized that intra-articular (IA) injections of high-molecular-weight hyaluronic acid (HA) can alleviate pain and improve joint function by restoring the elastoviscous properties of OA synovial fluid (SF) that are impaired because of quantitative and qualitative alterations in HA. 5 Thirty years later, it has been formally evidenced that HA is not only a lubricating and shock absorber agent but exhibits, through complex mechanisms, many other properties including anti-inflammatory, analgesic, antiapoptotic, and antidegradative effects. 6 VS is recommended by many scientific societies in the clinical management of pain in patients with knee OA not adequately improved by first-line treatments.2,3,7 -10 Despite increasing evidence of a good benefit/risk ratio11-13 and cost-effectiveness, 14 the efficacy of VS remains controversial,15-17 leading to variable recommendations across clinical guidelines. However, there is a gap between these guidelines and clinical daily practice 18 as, despite negative or lukewarm recommendations, more and more practitioners worldwide continue to use VS with satisfying clinical results, 19 allowing a substantial number of patients to delay the need for knee replacement.20 -22 A pragmatic approach has been proposed by several working groups.23 -26 Despite VS being primarily indicated in mild to moderate OA, where it has been shown to be the most effective,27 -29 IA-HA can be useful in advanced disease, especially in patients who cannot or do not want to undergo total knee replacement. Several drug regimens are currently available, depending on the physicians’ and patients’ preference. Repeat injections of linear HA are more and more often replaced by single injections of long-lasting HA. The best validated way to increase the IA residence time of HA is to cross-link HA linear macromolecules using cross-linking agents such as butanediol-diglycidyl ether (BDDE), divinyl sulfone, or ethylene sulfide.30 -32 Adding mannitol, a powerful antioxidant, to HA may reduce reactive oxygen species related to the depolymerization of HA, leading to an increase in HA IA residence time.33-35 HANOX-M-XL is an extended-release viscosupplement combining cross-linking and mannitol, allowing a single-injection regimen, with a high success rate in several indications.36 -40 This is the reason why HANOX-M-XL is the most used HA viscosupplement for treating symptomatic knee OA in our rheumatology department.
As one of the doctor’s duties is to accurately inform patients about the treatment offered to them, it has seemed important to us to try to answer the following question: Is it possible to predict the duration of effectiveness (DE) of VS with HANOX-M-XL, in daily practice conditions, where standard x-rays of the knee are the only available tool for assessing OA anatomical phenotype and severity? Indeed, in the current literature, data assessing both the radiological grade and other anatomical features of OA (i.e., the involved compartment) are lacking.
Hence, the primary goal of the study was to investigate whether radiological features are significantly associated with the DE of a single IA injection of an extended-release hyaluronic acid in patients with knee OA.
Patients and Methods
The PRESAGE study is a cross-sectional, single-center trial, carried out under clinical daily practice settings, aimed to investigate the possible predictive factors of VS DE in 150 knee OA patients (demographics, radiological features, previous and current treatments for OA, comorbidities, number of previous VS or corticosteroid IA injections, HA products, single or repeat injections, etc.). It received the approval of the French “Comité de Protection des Personnes Sud EST III” under ID-CRB N° 2021-A00773-38 (ClinicalTrials.gov Identifier: NCT04988698). The trial was conducted in accordance with good clinical practice and the Declaration of Helsinki (ethical principles for medical research involving human subjects). Due to the limited number of patients, which does not allow the analysis of numerous variables at the same time, this article reports preliminary results specifically focused on the impact of the x-ray characteristics on the DE of VS. The choice to limit the analysis to the results obtained with a single viscosupplement (HANOX-M-XL) was made to avoid the possible confounding factor due to the difference in efficacy between the HA products.
Patient Selection
All the consecutive ambulatory adult patients, female or male, regardless of age, symptomatic or not, who showed up to the rheumatology consultation at the North Franche-Comté Hospital (Belfort, France), more than 2 months and less than 3 years after being treated with a single injection of HANOX-M-XL 2.2 ml (HAPPYCROSS®; LABRHA SAS, Lyon, France) for symptomatic knee OA, evidenced by standard x-rays performed within 12 months prior to injection, were prospectively included in the study. The patients in whom the questionnaire could not be administered reliably (cognitive disorders or language problems) or who were unable to give informed consent were not selected in the trial. The patients treated with IA-HA using another injection protocol (multiple injections or viscosupplement other than HANOX-M-XL) or for a reason other than knee OA, patients in whom VS was performed less than 2 months (i.e., the average onset of action of IA HA) or more than 36 months ago, and patients in whom x-rays prior to IA injection were not available were also excluded.
Study Design
During a routine visit, the investigator handed the patient a document providing information about the study and obtained his or her informed consent for participating in the trial. Next, the investigator collected demographic characteristics (age, gender, weight, height, body mass index [BMI]), collected the x-rays, reported the radiological knee OA location (i.e., medial tibiofemoral [TF] and/or lateral TF and/or patellofemoral [PF]) in the Clinical Report Form, and asked the patient to give his or her self-assessment of the DE of the treatment (DE = number of weeks during which the previous VS was effective). The Felson-modified Kellgren-Lawrence (K-L) score 41 was assessed, by a single experienced observer, on the radiological view (i.e., standing anteroposterior, lateral, Lyon-Schuss, patella skyline views), 42 highlighting the most severe lesions.
Outcomes
The primary criterion was the DE, measured in weeks of effectiveness, of VS, self-assessed by the patients. The question asked to the patients was “How long was the treatment effective?” The potential explanatory variables of DE were K-L score, radiological OA phenotype (medial or lateral TF OA, PF OA, or both), age, BMI, and gender.
Statistics
A descriptive analysis of the collected data was performed. Qualitative variables were described using frequencies. Quantitative variables were described using mean values, standard deviation (SD), and characteristics of their distribution (minimum, maximum, and median). Univariate analysis was performed using the chi-square test, Fischer’s exact test, or the Mann-Whitney test, as appropriate. A multivariate regression analysis has taken into account factors with a significant association at the 0.2 threshold in previous bivariate regressions. All the analyses were carried out under R++© software1.4 (Zebrys SAS, Toulouse, France), with the alpha threshold at 0.05.
Results
Among the 75 patients who had been treated with VS within the last 3 years and who have consulted a physician in the rheumatology department, between October 2021 and February 2022, 51 fulfilled the inclusion criteria and were included in the analysis. The other 24 subjects were unable to reliably answer the questionnaire (n = 8), had no available knee radiograph (n = 4), were treated with another HA product than HANOX-M-XL (n = 11), or had no evidence of knee OA (n = 1). The included 33 female and 18 male patients had a mean age of 66 ± 12 years and a mean BMI of 26.1 (5.6). The patients’ characteristics are provided in Table 1 .
Table 1.
Patients’ Characteristics at Time of Injection.
| Gender: n (%) | |
| Female | 33 (64.7) |
| Male | 18 (35.3) |
| Age (years) | |
| Mean | 65 |
| Standard deviation | 12 |
| Minimum | 22 |
| Maximum | 90 |
| Median | 65 |
| Weight (kg) | |
| Mean | 72.8 |
| Standard deviation | 16.3 |
| Minimum | 45 |
| Maximum | 28 |
| Median | 70 |
| Body mass index (kg/m2) | |
| Mean | 26.1 |
| Standard deviation | 5.6 |
| Minimum | 18.3 |
| Maximum | 42.8 |
| Median | 24.5 |
Seventy-six treated knees were analyzed. Radiologically, the involved compartments were TF in 27 knees, PF in 14, and both TF and PF in the remaining 35.
The K-L score was 1, 2, 3, and 4 in 3 (3.95%), 16 (21%), 36 (47.4%), and 21 (27.6%) of the target knees, respectively. The radiographic data are provided in Table 2 .
Table 2.
Radiographic Features at the Date of Injection.
| Knee Compartment(s) Involved | Number (%) of Knees |
|---|---|
| Tibiofemoral | 27 (35.5) |
| Patellofemoral | 14 (18.5) |
| Tibiofemoral + patellofemoral | 35 (46) |
| Kellgren-Lawrence Grade | Number (%) of Knees |
| I | 3 (3.95) |
| II | 16 (21.05) |
| III | 36 (47.4) |
| IV | 21 (27.6) |
The average time between VS and the present visit was 56 ± 26 weeks. At the time of the visit, 65 patients (85.5%) were still satisfied with the treatment. The average DE was 52.0 ± 24.7 weeks (range, 13-155 weeks). In the bivariate analysis, despite a trend for a shorter DE in the most advanced stages, DE was not significantly associated with K-L grade (P = 0.12) (Figure 1). When K-L grades were pooled into 2 groups (K-L 1 + 2 vs. 3 + 4), the mean DE was 14 weeks longer in knees with K-L 1 + 2 (62.6 ± 36.4 weeks) than in those with K-L 3 + 4 (48.9 ± 18.6) (P = 0.03) despite the small sample sizes and the wide range of results (13-155 weeks) (Figure 2). DE was not significantly different in accordance with the involved compartment(s), ranging from 55.6 ± 28.0 weeks for TF OA to 48.5 ± 19.3 weeks for isolated PF OA (P = 0.63). Among patients with KL 1 and 2, DE was much longer in those with medial (81 weeks) than in those with lateral TF OA or PF involvement 37 and 47 weeks, respectively ( Table 3 ). However, the very small number of patients with lateral TF and PF OA does not allow relevant conclusions to be drawn. Surprisingly, DE was significantly longer in men than in women (60 ± 31.4 vs. 47 ± 16 weeks; P = 0.035). There was a trend for an inverse correlation between DE and BMI, which was not statistically significant (F = −0.59; 50%; confidence interval [CI] [−1.41 to 0.22]; P = 0.15). Unsurprisingly, DE was significantly positively correlated with the time between the last VS and the present visit (P < 0.0001). DE was not statistically different between unilateral and bilateral knee OA (P = 0.56). There was a significant relationship between age and K-L score (P = 0.001) but only a trend between age and DE (P = 0.16).
Figure 1.
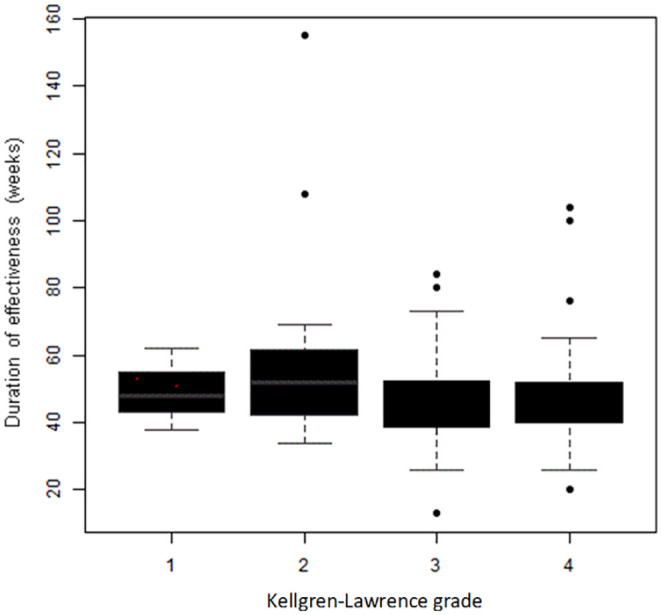
Duration of effectiveness (weeks) of 1 injection of HANOX-M-XL according to the Kellgren-Lawrence radiological grading scale (1-4).
Figure 2.
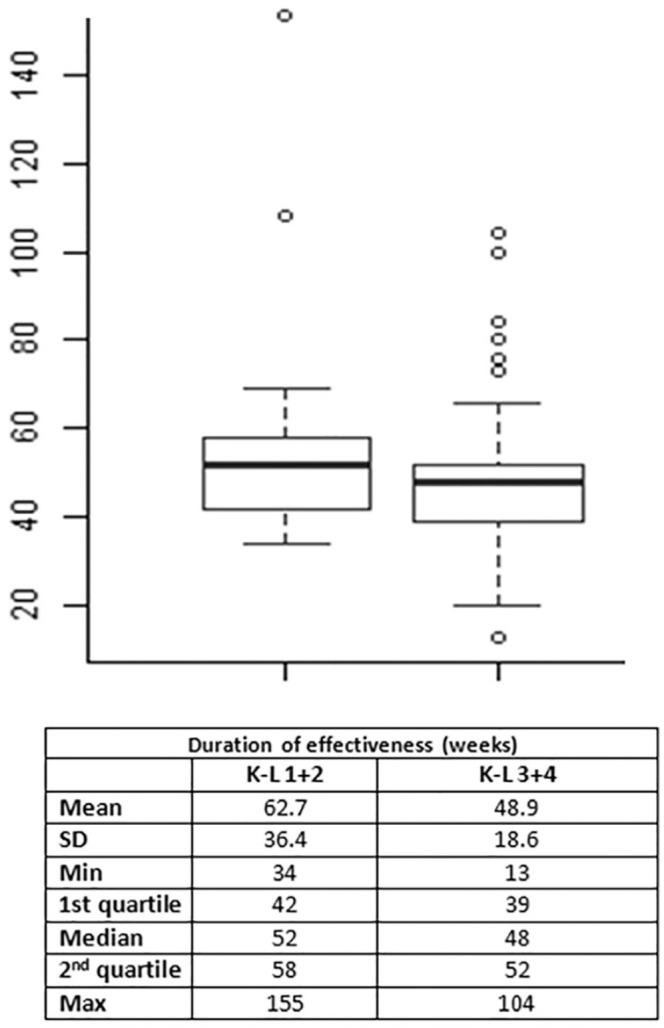
Duration of effectiveness (weeks) of 1 injection of HANOX-M-XL according to the Kellgren-Lawrence radiological grading scale (1 + 2 vs. 3 + 4). K-L = Kellgren-Lawrence.
Table 3.
Duration of Efficacy (Weeks) According to Radiological Grade and Location of Joint Space Narrowing in Patients with Knee Treated with HANOX-M-XL Intra-Articular Injection.
| K-L 1 + 2 | K-L 3 + 4 | |
|---|---|---|
| Medial tibiofemoral | ||
| Mean | 81 | 51.1 |
| SD | 57.7 | 13.9 |
| Lateral tibiofemoral | ||
| Mean | 37.0 | 49.8 |
| SD | 0 | 10.6 |
| Patellofemoral | ||
| Mean | 47.2 | 49.4 |
| SD | 10.8 | 18.9 |
| Medial tibiofemoral and patellofemoral | ||
| Mean | 76.0 | 51.6 |
| SD | 45.3 | 23.3 |
| Lateral tibiofemoral and patellofemoral | ||
| Mean | 52.0 | 42.7 |
| SD | 0 | 4.6 |
K-L = Kellgren and Lawrence modified by Felson.
In the multivariate analysis, including all variables whose level of significance was <0.2 in bivariate analysis (K-L grade, gender, age, and BMI), a longer DE was associated (R2= 0.17, P = 0.009) with K-L grade 1-2 (vs. 3-4) (P = 0.007), with male gender (P = 0.02), and with older age (P = 0.04) ( Table 4 ).
Table 4.
Multivariate Analysis Assessing Factors Associated with the Duration of Effectiveness of 1 Injection of a Sustained-Release Hyaluronic Acid (HANOX-M-XL) in Knee Osteoarthritis (R2 = 0.17, F = 3.64, P = 0.009).
| Variables | Duration of Effectiveness | ||
|---|---|---|---|
| Coefficient | 95% CI | P Value | |
| K-L grade | −18.07 | −31.01 to −5.14 | 0.0068 |
| Gender: male vs. female | 13.25 | 2.05 to 24.4 | 0.02 |
| Age | 0.528 | 0.03 to 1.02 | 0.038 |
| BMI | −0.29 | −1.19 to 0.59 | 0.51 |
K-L = Kellgren-Lawrence grade (1 + 2) versus (3 + 4); CI = confidence interval; BMI = body mass index.
P values with statisically significance are written in bold.
Discussion
This study, carried out under real-life conditions, provides additional information to the data available to date, which comes mostly from prospective controlled or observational studies. We have previously shown that the radiological grade seriously impacted the chances of being a responder to VS. 28 This new trial focused on the duration of efficacy, perceived by the patients themselves. Indeed, in current practice, it is customary to ask the patient how long he felt relieved, and if the pain has returned, for how long. In this study, the influence of the radiological severity did not appear so clearly. Indeed, although our results suggested a more sustainable effect in patients with mild knee OA compared with those with moderate to severe radiographic OA, the difference was only obtained in the multivariate analysis, after adjustment for gender, age, and BMI. These findings corroborate those of Altman et al., 29 who found significantly greater positive responses in all outcomes for the patient subgroup classified as K-L grade 2, when compared with K-L grade 3 patients. However, although the difference in DE between mild and moderate/severe OA was approximately 3 months, one can wonder about the clinical relevance of such results at the level of a given individual. Indeed, DE, as perceived by the patients themselves, was about 1 year at all x-ray stages, data that match with the expected duration of such a mannitol-combined highly cross-linked HA. On the other hand, the very large interindividual variations, with DE ranging from a few months to several years in all anatomical stages, make it difficult to accurately predict DE in a particular individual, based solely on plain x-ray data. Another interesting point to underline is the absence of DE difference between K-L grades 3 and 4. This may seem surprising, K-L 4 being often considered as a contraindication to VS, except in patients who cannot undergo surgery. The explanation is probably that very symptomatic patients with severe radiological knee OA are usually not treated with VS and are referred to orthopedic surgeons for total knee arthroplasty. It is likely that subjects with K-L grade 4, included in the present study, were moderately symptomatic and did not require short-term surgery. Furthermore, it has been suggested that patients with more advanced K-L grade had a better response with repeated series of IA-HA injections, 29 and most of our patients had already received one or more HA injections before entering the study. Another surprising result is the shorter DE in women than in men, which was found in both bivariate and multivariate analyses. One might have assumed that this difference was due to the higher frequency of TF and lateral PF involvement in women than in men. However, we did not find any difference in DE related to the damaged compartment(s). Previous studies did not show such a gender difference and we do not have any explanation for this. As previously mentioned, PF involvement, isolated or combined with TF damage, was not found to be a risk factor of a shorter efficacy duration, contrary to what we had observed in an earlier study. 43 Contrary to what we have shown in a previous study pooling 2 non-cross-linked viscosupplements, 28 BMI and obesity were not associated with a poorer outcome. This may be due to a fairly low BMI (average, 26 kg/m2) and a small number of obese subjects (12 out of 51). A weak but significant correlation between age and DE, that was still present in the multivariate analysis, was highlighted. The most likely reason for this is lower physical activity in the elderly, with less strain on the knees.
The main strength of this study is that it was carried out under conditions of daily practice, and therefore testifies to what happens in real life. Patients were not influenced by the fact that they were participating in a study. All ages and all x-ray stages were admitted and patients with numerous comorbidities were not excluded. The decision to include “self-assessment of DE by the patient” as a main criterion was a pragmatic decision. Although the notion of efficacy is subjective and varies from one subject to another, depending on their expectations, it corresponds to clinical practice where scores (i.e., Western Ontario and McMaster Universities Arthritis score [WOMAC], Knee Injury and Osteoarthritis Outcome [KOOS]) 44 are rarely used in routine consultation. On the other hand, efficacy is well correlated with patient satisfaction and a decrease in the patient’s global assessment and WOMAC score. 36 The radiological criterion (K-L score) is simple, easy, and quick to perform, with a good intraobserver reproducibility. 45 The fact that the study was monocentric made it possible not to introduce any confounding factors, by the use of a single product (HANOX-M-XL), injected according to the same injection protocol (single intra-articular injection) and the same technique of injection via a lateral mid-patellar route. Furthermore, the use of the same radiographic views (standing anteroposterior view, Lyon-Schuss view, profile view, and skyline view of the patella) and a centralized single-observer reading of the x-rays ensured good homogeneity of the scoring.
The study also suffers from several limitations. The exclusive use of HANOX-M-XL makes it impossible to extrapolate our results to other products/protocols, especially with non-cross-linked HA and/or using repeat injections. However, as HA products cannot be considered as a class, but as medical devices that widely differ in terms of rheological properties, molecular weight, concentration, volume, and half-life, 24 it seemed more appropriate to us to study only one HA product, the one most often used in our department. A specific study will have to be carried out to compare different products/dosing regimen/injection protocols.
In fact it is not so surprising that plain radiographs failed to predict the outcome of VS. The standard radiographs, especially the Lyon-Schuss view, allows a good assessment of the TF compartments 46 but frequently underestimates the severity of knee OA, 47 particularly in the case of PF involvement, even if radiographic skylines of the patellae were systematically performed. Furthermore, K-L score is a fairly crude means for assessing the anatomical severity of knee OA. It has been shown to be positively associated with age and disease duration but not with pain and function scores. 48 Not very sensitive to change, it has the advantages of being simple, reproducible, and quick to perform in routine consultation.
The main weakness of our study is the relatively small sample size that limits the power of the analysis. The recruitment stage is still in progress, with an objective of 300 knees to be analyzed. The second limitation is the method of recruitment. In most cases, patients are advised to come back as soon as they start to suffer from their knee again. For those who remain asymptomatic, an appointment is systematically scheduled 1 year after the injection. Finally, patients at high risk of progression or very symptomatic at the time of the injection are called back 6 months after VS. Therefore, there is a risk of underestimation of DE in subjects who were seen before pain returned. Finally, patients who did not benefit from the treatment probably did not come back and chose another therapeutic option, like surgery or platelet-rich plasma. On the other hand, some fully asymptomatic patients probably did not return either and it is not possible for us to count these 2 populations. To limit this bias, we are in the habit, after each VS, of systematically calling patients back 9 to 12 months after the injections and advising them to come back sooner if pain reappears.
In conclusion, this study shows that, in patients with knee OA who are not amenable to knee arthroplasty, a single IA injection of a cross-linked sustained-release HA viscosupplement can provide relief from knee pain for about a year (or longer), regardless of the radiographic features. Patients with K-L grades 1 and 2, men, and elderly patients may benefit from treatment the longest, while the involved knee compartments do not impact the clinical outcome. This knowledge should encourage recommending VS, even in certain patients with radiologically advanced knee OA, as the treatment may provide them a long period of improvement. These preliminary data need to be confirmed on a larger sample of patients.
Footnotes
Author Contributions: SP: performed the statistical analysis and wrote the first draft of the manuscript.
J-CB, CR, CB, AL: participated in the acquisition and inclusion of data.
TC: participated in the design of the study, contributed to the interpretation and discussion of the results, and coordinated the manuscript writing.
All authors read, commented, made changes, and then approved the final manuscript.
Acknowledgments and Funding: The authors acknowledge Elodie Bouvier, the HNFC Clinical Research Unit, as well as ALPHATRAD for linguistic assistance.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: TC received fees from LABRHA, SANOFI, MEDAC, and FIDIA for scientific and board member services. CB, SP, CR, CG, J-CB: None; AL received fees from VIVACY for consultant services.
Declarations: Data from the PRESAGE study are accessible at the Clinical Research Unit, North Franche-Comté Hospital, France (elodie.bouvier@hnfc.fr).
Ethical Approval: The PRESAGE study received the approval of the French “Comité de Protection des Personnes Sud EST III” under ID-CRB N° 2021-A00773-38 and have been registered under ClinicalTrials.gov Identifier: NCT04988698). The trial was conducted in accordance with good clinical practice and the Declaration of Helsinki (ethical principles for medical research involving human subjects).
ORCID iD: Thierry Conrozier  https://orcid.org/0000-0003-0353-6292
https://orcid.org/0000-0003-0353-6292
References
- 1. Jackson J, Iyer R, Mellor J, Wei W. The burden of pain associated with osteoarthritis in the hip or knee from the patient’s perspective: a multinational cross-sectional study. Adv Ther. 2020;37(9):3985-99. doi: 10.1007/s12325-020-01445-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bruyère O, Honvo G, Veronese N, Arden NK, Branco J, Curtis EM, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49(3):337-50. doi: 10.1016/j.semarthrit.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 3. Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62:1145-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578-89. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 5. Balazs EA, Denlinger JL. Viscosupplementation: a new concept in the treatment of osteoarthritis. J Rheumatol. 1993;39:3-9. [PubMed] [Google Scholar]
- 6. Altman RD, Manjoo A, Fierlinger A, Niazi F, Nicholls M. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review. BMC Musculoskelet Disord. 2015;16:321. doi: 10.1186/s12891-015-0775-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rillo O, Riera H, Acosta C, Liendo V, Bolaños J, Monterola L, et al. PANLAR consensus recommendations for the management in osteoarthritis of hand, hip, and knee. J Clin Rheumatol. 2016;22:345-54. [DOI] [PubMed] [Google Scholar]
- 8. Trojian TH, Concoff AL, Joy SM, Hatzenbuehler JR, Saulsberry WJ, Coleman CI. AMSSM scientific statement concerning viscosupplementation injections for knee osteoarthritis: importance for individual patient outcomes. Br J Sports Med. 2016;50(2):84-92. doi: 10.1136/bjsports-2015-095683. [DOI] [PubMed] [Google Scholar]
- 9. Abdulla A, Adams N, Bone M, Elliott AM, Gaffin J, Jones D, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42(Suppl 1):i1-57. doi: 10.1093/ageing/afs200. [DOI] [PubMed] [Google Scholar]
- 10. Sellam J, Courties A, Eymard F, Ferrero S, Latourte A, Ornetti P, et al. French Society of Rheumatology. Recommendations of the French Society of Rheumatology on pharmacological treatment of knee osteoarthritis. Joint Bone Spine. 2020;87(6):548-55. doi: 10.1016/j.jbspin.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 11. Maheu E, Rannou F, Reginster JY. Efficacy and safety of hyaluronic acid in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(Suppl 4):S28-33. doi: 10.1016/j.semarthrit.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 12. Strand V, McIntyre LF, Beach WR, Miller LE, Block JE. Safety and efficacy of US-approved viscosupplements for knee osteoarthritis: a systematic review and meta-analysis of randomized, saline-controlled trials. J Pain Res. 2015;8:217-28. doi: 10.2147/JPR.S83076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maheu E, Bannuru RR, Herrero-Beaumont G, Allali F, Bard H, Migliore A. Why we should definitely include intra-articular hyaluronic acid as a therapeutic option in the management of knee osteoarthritis: results of an extensive critical literature review. Semin Arthritis Rheum. 2019;48(4):563-72. doi: 10.1016/j.semarthrit.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 14. Rosen J, Niazi F, Dysart S. Cost-effectiveness of treating early to moderate stage knee osteoarthritis with intra-articular hyaluronic acid compared to conservative interventions. Adv Ther. 2020;37(1):344-52. doi: 10.1007/s12325-019-01142-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21:571-6. [DOI] [PubMed] [Google Scholar]
- 16. National Institute for Health and Care Excellence. Osteoarthritis: care and management (NICE clinical guideline no. 177). London (UK): National Institute for Health and Care Excellence; 2014. [cited 2017 Jun 6]. Available from: https://www.nice.org. [Google Scholar]
- 17. Kaulback K, Jones S, Wells C, Felipe E. Viscosupplementation for knee osteoarthritis: a review of clinical and cost-effectiveness and guidelines. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2017. [PubMed] [Google Scholar]
- 18. Migliore A, Bizzi E, Herrero-Beaumont J, Petrella RJ, Raman R, Chevalier X. The discrepancy between recommendations and clinical practice for viscosupplementation in osteoarthritis: mind the gap! Eur Rev Med Pharmacol Sci. 2015;19(7):1124-9. [PubMed] [Google Scholar]
- 19. Rosen J, Avram V, Fierlinger A, Niazi F, Sancheti P, Bedi A. Clinicians’ perspectives on the use of intra-articular hyaluronic acid as a treatment for knee osteoarthritis: a North American, multidisciplinary survey. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:21-7. doi: 10.4137/CMAMD.S34496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Delbarre A, Amor B, Bardoulat I, Tetafort A, Pelletier—Fleury N. Do intra—articular hyaluronic acid injections delay total knee replacement in patients with osteoarthritis—a Cox model analysis. PLoS ONE. 2017;12(11):e0187227. doi: 10.1371/journal.pone.0187227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Altman R, Fredericson M, Bhattacharyya SK, Bisson B, Abbott T, Yadalam S, et al. Association between hyaluronic acid injections and time-to-total knee replacement surgery. J Knee Surg. 2016;29(7):564-70. doi: 10.1055/s-0035-1568992. [DOI] [PubMed] [Google Scholar]
- 22. Altman R, Lim S, Steen RG, Dasa V. Hyaluronic acid injections are associated with delay of total knee replacement surgery in patients with knee osteoarthritis: evidence from a large U.S. health claims database. PLoS ONE. 2015;10(12):e0145776. doi: 10.1371/journal.pone.0145776. Erratum in: PLoS ONE. 2016;11(1):e0148591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bhadra AK, Altman R, Dasa V, Myrick K, Rosen J, Vad V, et al. Appropriate use criteria for hyaluronic acid in the treatment of knee osteoarthritis in the United States. Cartilage. 2017;8(3):234-54. doi: 10.1177/1947603516662503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Henrotin Y, Raman R, Richette P, Bard H, Jerosch J, Conrozier T, et al. Consensus statement on viscosupplementation with hyaluronic acid for the management of osteoarthritis. Semin Arthritis Rheum. 2015;45(2):140-9. doi: 10.1016/j.semarthrit.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 25. Conrozier T, Monfort J, Chevalier X, Raman R, Richette P, Diraçoglù D, et al. EUROVISCO recommendations for optimizing the clinical results of viscosupplementation in osteoarthritis. Cartilage. 2020;11(1):47-59. doi: 10.1177/1947603518783455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Migliore A, Gigliucci G, Alekseeva L, Bannuru RR, Blicharski T, Diracoglu D. Systematic literature review and expert opinion for the use of viscosupplementation with hyaluronic acid in different localizations of osteoarthritis. Orthop Res Rev. 2021;13:255-73. doi: 10.2147/ORR.S336185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Toh EM, Prasad PS, Teanby D. Correlating the efficacy of knee viscosupplementation with osteoarthritic changes on roentgenological examination. Knee. 2002;9(4):321-30. [DOI] [PubMed] [Google Scholar]
- 28. Eymard F, Chevalier X, Conrozier T. Obesity and radiological severity are associated with viscosupplementation failure in patients with knee osteoarthritis. J Orthop Res. 2017;35:2269-74. doi: 10.1002/jor.23529. [DOI] [PubMed] [Google Scholar]
- 29. Altman RD, Farrokhyar F, Fierlinger A, Niazi F, Rosen J. Analysis for prognostic factors from a database for the intra-articular hyaluronic acid (Euflexxa) treatment for osteoarthritis of the knee. Cartilage. 2016;7(3):229-37. doi: 10.1177/1947603515620890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lindqvist U, Tolmachev V, Kairemo K, Aström G, Jonsson E, Lundqvist H. Elimination of stabilised hyaluronan from the knee joint in healthy men. Clin Pharmacokinet. 2002;4:603-13. [DOI] [PubMed] [Google Scholar]
- 31. Larsen NE, Dursema HD, Pollak CT, Skrabut EM. Clearance kinetics of a hylan-based viscosupplement after intra-articular and intravenous administration in animal models. J Biomed Mater Res B Appl Biomater. 2012;100(2):457-62. doi: 10.1002/jbm.b.3197. [DOI] [PubMed] [Google Scholar]
- 32. Fallacara A, Baldini E, Manfredini S, Vertuani S. Hyaluronic acid in the third millennium. Polymers (Basel). 2018;10(7):701. doi: 10.3390/polym10070701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mendoza G, Alvarez AI, Pulido MM, Molina AJ, Merino G, Real R, et al. Inhibitory effects of different antioxidants on hyaluronan depolymerization. Carbohydr Res. 2007;342(1):96-102. doi: 10.1016/j.carres.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 34. Conrozier T. Is the addition of a polyol to hyaluronic acid a significant advance in the treatment of osteoarthritis? Curr Rheumatol Rev. 2018;14(3):226-30. doi: 10.2174/1573397113666170710115558. [DOI] [PubMed] [Google Scholar]
- 35. Rinaudo M, Lardy B, Grange L, Conrozier T. Effect of mannitol on hyaluronic acid stability in two in vitro models of oxidative stress. Polymers. 2014;6:1948-57. doi: 10.3390/polym6071948Esp. [DOI] [Google Scholar]
- 36. Conrozier T, Monet M, Lohse A, Raman R. Getting better or getting well? The patient acceptable symptom state (PASS) better predicts patient’s satisfaction than the decrease of pain, in knee osteoarthritis subjects treated with viscosupplementation. Cartilage. 2018;9(4):370-7. doi: 10.1177/1947603517723072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Eymard F, Maillet B, Lellouche H, Mellac-Ducamp S, Brocq O, Loeuille D, et al. Predictors of response to viscosupplementation in patients with hip osteoarthritis: results of a prospective, observational, multicentre, open-label, pilot study. BMC Musculoskelet Disord. 2017;18(1):3. doi: 10.1186/s12891-016-1359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bossert M, Boublil D, Parisaux JM, Bozgan AM, Richelme E, Conrozier T. Imaging guidance improves the results of viscosupplementation with HANOX-M-XL in patients with ankle osteoarthritis: results of a clinical survey in 50 patients treated in daily practice. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dauvissat J, Rizzo C, Lellouche H, Porterie J, Melac-Ducamp S, Locquet V, et al. Safety and predictive factors of short-term efficacy of a single injection of mannitol-modified cross-linked hyaluronic acid in patients with trapeziometacarpal osteoarthritis. results of a multicentre prospective open-label pilot study (INSTINCT trial). Clin Med Insights Arthritis Musculoskelet Disord. 2018;11:1179544118782901. doi: 10.1177/1179544118782901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Galois L, Coillard JY, Porterie J, Melac-Ducamp S, Conrozier T. Open-label pilot study of a single intra-articular injection of mannitol-modified cross-linked hyaluronic acid (HANOX-M-XL) for the treatment of the first metatarsophalangeal osteoarthritis (hallux rigidus): the REPAR trial. Clin Med Insights Arthritis Musculoskelet Disord. 2022;15:11795441211055882. doi: 10.1177/11795441211055882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P. Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis. 2011;70(11):1884-6. doi: 10.1136/ard.2011.155119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brandt KD, Mazzuca SA, Conrozier T, Dacre JE, Peterfy CG, Provvedini D, et al. Which is the best radiographic protocol for a clinical trial of a structure modifying drug in patients with knee osteoarthritis? J Rheumatol. 2002;29(6):1308-20. [PubMed] [Google Scholar]
- 43. Conrozier T, Mathieu P, Schott A-M, Laurent I, Hajri T, Crozes P, et al. Factors predicting long-term efficacy of Hylan GF-20 viscosupplementation in knee osteoarthritis. Joint Bone Spine. 2003;70:128-33. [DOI] [PubMed] [Google Scholar]
- 44. Wang D, Jones MH, Khair MM, Miniaci A. Patient-reported outcome measures for the knee. J Knee Surg. 2010;23(3):137-51. doi: 10.1055/s-0030-1268691. [DOI] [PubMed] [Google Scholar]
- 45. Eckersley T, Faulkner J, Al-Dadah O. Inter- and intra-observer reliability of radiological grading systems for knee osteoarthritis. Skeletal Radiol. 2021;50(10):2069-78. doi: 10.1007/s00256-021-03767-y. [DOI] [PubMed] [Google Scholar]
- 46. Merle-Vincent F, Vignon E, Brandt K, Piperno M, Coury-Lucas F, Conrozier T, et al. Superiority of the Lyon schuss view over the standing anteroposterior view for detecting joint space narrowing, especially in the lateral tibiofemoral compartment, in early knee osteoarthritis. Ann Rheum Dis. 2007;66(6):747-53. doi: 10.1136/ard.2006.056481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Abdelaziz H, Balde OM, Citak M, Gehrke T, Magan A, Haasper C. Kellgren-Lawrence scoring system underestimates cartilage damage when indicating TKA: preoperative radiograph versus intraoperative photograph. Arch Orthop Trauma Surg. 2019;139(9):1287-92. doi: 10.1007/s00402-019-03223-6. [DOI] [PubMed] [Google Scholar]
- 48. Cubucku D, Sarsan A, Alkan H. Relationships between pain, function and radiographic findings in osteoarthritis of the knee: a cross-sectional study. Arthritis. 2012;2012:984060. doi: 10.1155/2012/904060. [DOI] [PMC free article] [PubMed] [Google Scholar]


