Abstract
Objective
The primary aim was to determine and compare the complication rate of different surgical treatment options for osteochondral lesions of the talus (OLTs). The secondary aim was to analyze and compare the severity and types of complications.
Design
A literature search was performed in MEDLINE (PubMed), EMBASE (Ovid), and the Cochrane Library. Methodological quality was assessed using the Methodological Index for Non-Randomized Studies (MINORS). Primary outcome was the complication rate per surgical treatment option. Secondary outcomes included the severity (using the Modified Clavien-Dindo-Sink Complication Classification System for Orthopedic Surgery) and types of complications. The primary outcome, the severity, and the sub-analyses were analyzed using a random effects model. A moderator test for subgroup-analysis was used to determine differences. The types of complications were presented as rates.
Results
In all, 178 articles from the literature search were included for analysis, comprising 6,962 OLTs with a pooled mean age of 35.5 years and follow-up of 46.3 months. Methodological quality was fair. The overall complication rate was 5% (4%-6%; treatment group effect, P = 0.0015). Analysis resulted in rates from 3% (2%-4%) for matrix-assisted bone marrow stimulation to 15% (5%-35%) for metal implants. Nerve injury was the most observed complication.
Conclusions
In 1 out of 20 patients treated surgically for an OLT, a complication occurs. Metal implants have a significantly higher complication rate compared with other treatment modalities. No life-threatening complications were reported.
Keywords: osteochondral defect, osteochondral lesion, surgery, surgical treatment, complication
Introduction
Osteochondral lesions of the talus (OLTs) are lesions that affect the articular cartilage and the subchondral bone. Often, this arises after a traumatic event, such as an ankle sprain or fracture.1,2 Symptomatic OLTs often have a severe impact on the quality of life (QoL) of patients. 3 To improve QoL, patients are treated, either non-operatively or surgically. In a stepped care treatment protocol, non-operative treatment is the first step, which has been shown being somewhat effective.4 -8 However, if this is not successful, then surgical treatment may be considered necessary. The optimal surgical treatment is determined on the patients’ preferences, lesion nature, localization, size, morphology, and fixability of a fragment. 9 A wide variety of surgical treatment options exist, including bone marrow stimulation (BMS) therapies, retrograde drilling, fixation, matrix-assisted BMS, cartilage implantation, osteo(chondral) autograft transplantation therapies, osteo(chondral) allograft transplantation therapies, and metal implants.10 -17 In small lesions (defect size < 10 mm in any of the dimensions), fixation and BMS are the primary treatment options. 9 For larger lesions, retrograde drilling and osteo(chondral) transplantation therapies are more often used. 9
Every different surgical procedure comes with its own risks and complications. Complication characteristics are an important factor in the evidence-based shared decision-making process. 18 Besides complications, the efficacy and costs of a treatment are also of importance. Recent research has shown that no superior treatment for primary and secondary lesions exists.19,20 Increased insight into the occurrence, severity, and types of complications in surgical treatment of OLTs is therefore of importance in future patients’ treatment decisions.
The primary aim of this study is to determine and compare the complication rate per surgical treatment option for OLTs. The secondary purpose is to analyze and compare the severity of complications and to analyze the types of complications per treatment option. The hypothesis of the present study is that surgical treatment of OLTs yields a low complication rate.
Materials and Methods
The protocol of the present study was registered prospectively in the international prospective registry for systematic reviews PROSPERO 21 (registration number CRD42018081490). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was followed as a guideline for this study. 22
Search Strategy
Studies from 1996 until September 2021 from MEDLINE (PubMed), EMBASE (Ovid), and the Cochrane Library were identified. The publication filter from 1996 was applied due to the emerging of arthroscopy in the ankle. The full search strategy can be found in the Supplementary Appendix. Backward citation chaining was performed to find any additional eligible articles.
Eligibility Criteria and Study Selection
All clinical studies that investigated surgical treatment of OLTs were eligible for inclusion. The full text needed to be available in English, French, Spanish, German, or Dutch. No restrictions regarding patient demographics were applied. A study needed to analyze a minimum of 5 OLTs on a minimum follow-up of 6 months. Review, cadaver, and animal studies were excluded. In case there was overlap between studies, the study with the highest number of patients was included. If multiple treatment modalities were used in an eligible study, the authors of the present study needed to be able to extract the data per treatment option to include the study. The title and abstract was screened by two researchers (J.H. and J.D.). This was performed using the Rayyan web-tool, which makes it more convenient for researchers to screen articles. 23
Methodological Quality
Methodological quality was assessed by two independent reviewers (J.H. and J.D.) using the Methodological Index for Non-Randomized Studies (MINORS). 24
Data Extraction
Data extraction was performed by two reviewers (J.H. and J.D.) using a standardized extraction form, specially designed for the present study, and tested before use. Data on study and patient characteristics were collected. Study characteristics include author, title, year of publication, level of evidence, treatments used, and follow-up duration. Patient characteristics are gender, age, laterality, and complications.
The definition of a complication, used in this study, is derived from the definition of Sokol and Wilson, 25 and is as follows: “any undesirable, unintended, and direct result of an operation affecting the patient.” Any complication related to the success rate of the treatment, for example, graft non-union or other graft-related failures, was excluded from the analysis. In addition, secondary surgical procedures were also not scored as a complication. This was done to prevent the double-counting of complications for which subsequent surgical treatment was needed (e.g., complication and subsequent needed surgery counts one complication). 26 Also hardware removal was not considered a complication.27 -29
The severity of the complications was assessed with the help of the Modified Clavien-Dindo-Sink Complication Classification System for Orthopedic Surgery ( Table 1 ). 30 This classification was used to avoid subjective terms as “major” and “minor” and to improve the interrater and intrarater reliability. 30 To compare the different surgical treatment options, treatment groups based on treatment modalities were defined. The treatment modalities are BMS therapies, retrograde drilling, fixation, matrix-assisted BMS, cartilage implantation, osteo(chondral) autograft transplantation therapies, osteo(chondral) allograft transplantation therapies, and metal implants ( Table 2 ). The different types of complications were also extracted, to assess which type of complications occurs per treatment option.
Table 1.
Modified Clavien-Dindo-Sink Complication Classification System for Orthopedic Surgery.
| Grade | Definition |
|---|---|
| I | A complication that does not result in deviation from routine follow-up in the postoperative period and has minimal clinical relevance and requires minimal treatment (e.g., antiemetics, antipyretics, analgesics, diuretics, electrolytes, antibiotics, and physiotherapy) or no treatment. |
| II | A deviation from the normal postoperative course (including unplanned clinic/office visits) that requires outpatient treatment, either pharmacological or close monitoring as an outpatient. |
| III | A complication that is treatable but requires surgical, endoscopic, or interventional radiology procedure(s), or an unplanned hospital readmission. |
| IVa | A complication that is life- or limb-threatening, and/or requires ICU admission, a complication with potential for permanent disability but treatable, a complication that may require organ/joint resection/replacement. No long-term disability. |
| IVb | A complication that is life- or limb-threatening, and/or requires ICU admission, a complication that is not treatable, a complication that requires organ/joint resection/replacement or salvage surgery. With long-term disability. |
| V | Death. |
Adopted from Dodwell et al. 30
ICU = intensive care unit.
Table 2.
Treatment Modalities.
| Treatment Option | Examples |
|---|---|
| Bone marrow stimulation therapies | Bone marrow stimulation, debridement, microfracture |
| Retrograde drilling | Retrograde drilling |
| Fixation | Lift, drill, fill, fix |
| Matrix-assisted bone marrow stimulation | Autologous chondrocyte inducing chondrogenesis, matrix-associated stem cell transplantation, autologous matrix-induced chondrogenesis, bone marrow–derived stem cell transplantation |
| Cartilage implantation | Autologous chondrocyte implantation, matrix-induced autologous chondrocyte implantation, particulated juvenile cartilage allograft transplantation |
| Osteo(chondral) autograft transplantation therapies | Osteochondral autograft transfer system, autologous osteochondral transplantation |
| Osteo(chondral) allograft transplantation therapies | Allogenic osteochondral transplantation |
| Metal implants | Implant therapies |
Statistical Analysis
The primary outcome is the complication rate, which is defined as the proportion of complications to the total number of lesions. This was then pooled per surgical treatment option (i.e., BMS therapies, retrograde drilling, fixation, matrix-assisted BMS, cartilage implantation, osteo(chondral) autograft transplantation therapies, osteo(chondral) allograft transplantation therapies, and metal implants) with a random effects model, weighted by inverse variance. T 2 , a measure of heterogeneity, was determined with the use of the DerSimonian and Laird 31 estimator, and the corresponding confidence interval (CI) was calculated using the Jackson and Bowden 32 method. A logit transformation was applied. The 95% CIs for individual studies were calculated using the Clopper-Pearson 33 interval method. Difference in complication rates within treatment modalities were compared using a moderator test for subgroup-analysis with α = 0.05. 34 If a significant effect among all treatments was found, post hoc moderator tests were used to assess difference between single treatment modalities.
The distribution of grades per treatment option and the types of complications were presented as a rate which is the proportion of the total complications per treatment option. The different types of complications were presented by means of a top 5 per treatment option.
All analyses were performed in STATA 15 (StateCorp LP, College Station, TX) and R version 4.0.2 (RStudio, Boston, MA) with meta package. 35
Results
Article Selection
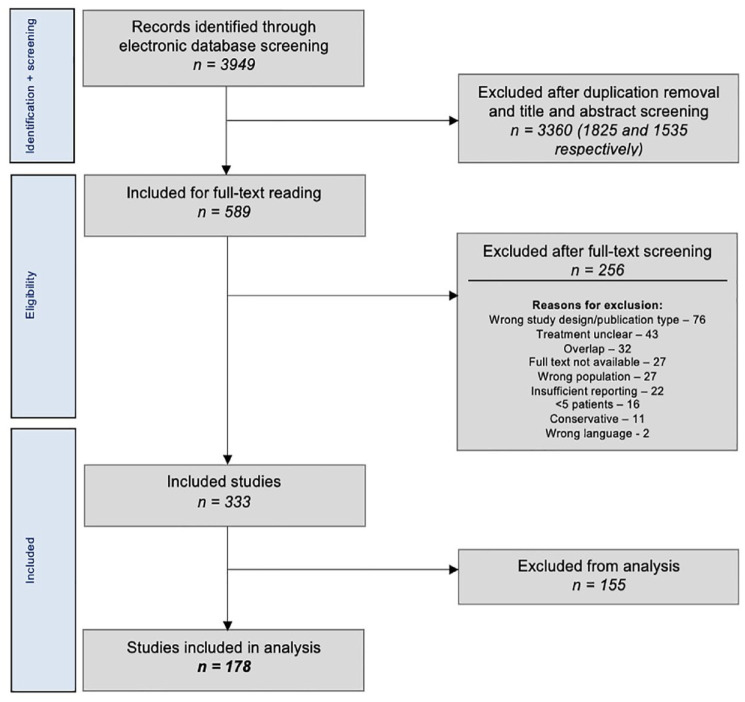
The literature search yielded 3,949 articles, of which 333 met the inclusion criteria ( Fig. 1 ). A total of 155 studies comprising 6,261 lesions could not be included in the analysis as they did not (well) report complications. The distribution of the lesions among the 155 studies can be viewed in Table 3 . In all, 178 studies remained for analysis in the present study.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of study selection.
Table 3.
Characteristics Excluded Studies Due to Underreporting/Unclear Reporting of Complications.
| Treatment Option | Lesions n |
|---|---|
| Overall | 6,261 |
| Bone marrow stimulation therapies | 2,916 |
| Retrograde drilling | 253 |
| Fixation | 181 |
| Matrix-assisted bone marrow stimulation | 1,031 |
| Cartilage implantation | 493 |
| Osteo(chondral) autograft transplantation therapies | 1,068 |
| Osteo(chondral) allograft transplantation therapies | 236 |
| Metal implants | 41 |
| Other | 42 |
Evaluation of the Characteristics of Included Studies
Overall, the 178 studies included 6,921 patients with 6,962 lesions (41 bilateral patients [0.6% of all patients]). The pooled mean age was 35.5 years (range of means: 10.4-58), and the pooled mean follow-up was 46.3 months (range of means: 6-411.6 months).
Methodological Quality
Scoring the methodological quality of the 134 non-comparative studies resulted in an average score of 10.1 (range: 5-13) out of 16 points.11,14,15,17,27 -29,36 -162 The 44 comparative studies had an average score of 17.8 (range: 13-22) out of 24 points.163 -206 The MINORS scores per individual study can be found in the Supplementary Appendix.
Primary Outcome
In total, 225 complications were reported. The overall complication rate was 5% (95% CI: 4%-6%; treatment group effect Q = 25.05, P = 0.0015), ranging per treatment option from 3% (95% CI: 2%-4%) for matrix-assisted BMS to 15% (95% CI: 5%-35%) for metal implants. The moderator test for subgroup-analysis between all treatment modalities showed a significant effect of treatment option (Q = 25.05, P = 0.015). Metal implants have a higher complication rate compared with BMS therapies (Q = 5.27, P = 0.0217), compared with retrograde drilling (Q = 3.86, P = 0.0493), compared with fixation (Q = 4.56, P = 0.0328), compared with matrix-assisted BMS (Q = 9.29, P = 0.0023), and compared with cartilage implantation (Q = 3.95, P = 0.0468). In addition, differences between matrix-assisted BMS and osteo(chondral) autograft transplantation therapies (3% [95% CI: 2%-5%] versus 7% [95% CI: 5%-10%], Q = 16.86, P ≤ 0.0001) and between matrix-assisted BMS and osteo(chondral) allograft transplantation therapies (3% [95% CI: 2%-5%] versus 8% [95% CI: 4%-16%], Q = 7.66, P = 0.0056) were found. The overall complication rate and the complication rate per treatment option can be viewed in Table 4 .
Table 4.
Overall Complication Rate per Treatment Option.
| Treatment Option | Studies n |
Lesions n |
Pooled Mean Age (Years) | Pooled Mean Follow-Up (Months) | Complication Rate % (95% Confidence Interval) |
|---|---|---|---|---|---|
| Overall | 178 | 6,962 | 35.5 | 46.3 | 5 (4-6) |
| Bone marrow stimulation therapies a | 67 | 2,926 | 36.7 | 48.7 | 4 (3-6) a |
| Retrograde drilling b | 14 | 289 | 32.6 | 39.2 | 5 (3-8) b |
| Fixation c | 8 | 179 | 22.3 | 35.5 | 3 (1-8) c |
| Matrix-assisted bone marrow stimulation d | 31 | 1,072 | 16.8 | 14.7 | 3 (2-4) d |
| Cartilage implantation e | 22 | 479 | 32.8 | 47.5 | 5 (3-8) e |
| Osteo(chondral) autograft transplantation therapies f | 61 | 1,639 | 34.7 | 54.2 | 8 (6-10) f |
| Osteo(chondral) allograft transplantation therapies g | 15 | 288 | 43.1 | 30.8 | 8 (4-14) g |
| Metal implants h | 3 | 80 | 41.7 | 54.4 | 15 (5-35) h |
| Other i | 1 | 10 | 43.3 | 12 | 5 (0-45) i |
Significantly different from osteo(chondral) autograft transplantation therapies (Q = 7.55, P = 0.0060) and metal implants (Q = 5.27, P = 0.0217).43,52,59,61 -63,66,81,92,93,109,113,117,121,123,125,131,135,141,143,146,149,150,153,158,164,165,167,168,171,173,176,177,179 -183,187,190,192,195 -200,202,204 -206
Significantly different from metal implants (Q = 3.86, P = 0.0493).11,42,53,56,59,116,118,137,170,177,194,196
Significantly different from osteo(chondral) autograft transplantation therapies (Q = 16.86, P < 0.0001), osteo(chondral) allograft transplantation therapies (Q = 7.66, P = 0.0056), and metal implants (Q = 9.29, P = 0.0023).29,38,40,49,58,65,72,77,82,94,98,101,130,139,140,142,144,145,155,157,162,166,169,181,189,192,195,201,204
Significantly different from metal implants (Q = 3.95, P = 0.0468).14,41,45,46,51,64,76,78 -80,86,99,103,107,112,114,115,124,133,147,179
Multiple studies: 15,36,39,47,48,50,60,68,70,71,74,75,83,84,87 -90,95 -97,100,105,106,108,110,120,126,128,129,132,136,138,148,151,152,154,156,159 -161,163,171 -175,178,184,188,191,193,194,197,203.
Study: 127 .
Secondary Outcomes
Severity of complications
No Grade IV and Grade V complications were found. Most of the complications were Grade I complications with an overall rate of 4% (95% CI: 3%-4%; difference between all treatment options, Q = 13.51, P = 0.0955). The rates for Grade II and Grade III are 3% (95% CI: 3%-4%; difference between all treatment options, Q = 12.88, P = 0.1160) and 3% (95% CI: 2%-3%; difference between all treatment options, Q = 8.44, P = 0.3917), respectively. The distribution of the severity of the complications that arise per treatment option can be seen in Table 5 . The proportion of Grade I and Grade II (complications without the need of a hospital readmission or intervention) of all complications is 84%.
Table 5.
Overall Complication Rate Separated in Severity.
| Treatment Option | Grade I a | Grade II a | Grade III a | |||
|---|---|---|---|---|---|---|
| % (95% CI) | Proportion | % (95% CI) | Proportion | % (95% CI) | Proportion | |
| Overall | 4 (3-4) | 51 | 3 (3-4) | 33 | 3 (2-3) | 16 |
| Bone marrow stimulation therapies | 3 (2-4) | 48 | 2 (2-3) | 30 | 2 (2-3) | 22 |
| Retrograde drilling | 4 (2-7) | 50 | 3 (2-7) | 33 | 3 (1-6) | 17 |
| Fixation | 3 (1-7) | 50 | 3 (1-7) | N/A | 3 (1-8) | 50 |
| Matrix-assisted bone marrow stimulation | 2(1-3) | 22 | 2 (1-3) | 67 | 2 (1-3) | 11 |
| Cartilage implantation | 4 (2-6) | 44 | 3 (2-6) | 44 | 3 (1-5) | 11 |
| Osteo(chondral) autograft transplantation therapies | 6 (4-8) | 62 | 4 (3-5) | 28 | 3 (2-4) | 10 |
| Osteo(chondral) allograft transplantation therapies | 3 (2-7) | 13 | 6 (3-11) | 47 | 5 (3-9) | 40 |
| Metal implants | 7 (2-28) | 50 | 7 (3-15) | 42 | 3 (1-13) | 8 |
| Other | 5 (0-45) | N/A | 5 (0-45) | N/A | 5 (0-45) | N/A |
CI = confidence interval; N/A = not applicable.
Severity based on the grades of Modified Clavien-Dindo-Sink Complication Classification System for Orthopedic Surgery. Rates presented as percentage of the overall complication rate of the respective treatment option, and the proportion of the grade of all complications overall and per treatment option. No significant differences were found.
Type of complications
The proportions of all complications for the most occurring complications per treatment option can be viewed in Table 6 . In 5 treatment modalities (i.e., BMS therapies, retrograde drilling, fixation, cartilage implantation, and metal implants), nerve injury, either temporary or duration unknown, was the most frequently reported complication (range of the proportions of the total complications per treatment option: 22%-50%). For matrix-assisted BMS, superficial infection was the most occurring type of complication (56%), for osteochondral autograft transplantation therapies, it is donor site morbidity (41%), and deep venous thrombosis (DVT) for osteo(chondral) allograft transfer (27%).
Table 6.
Most Occurring Complications per Treatment Option.
| Treatment Option | Most Occurring | Second Most Occurring | Third Most Occurring | Fourth Most Occurring | Fifth Most Occurring | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Complication | % | Complication | % | Complication | % | Complication | % | Complication | % | |
| Bone marrow stimulation therapies | Nerve injury (dur. unk.) | 22 | Superficial infection | 12 | DVT | 12 | Nerve injury (temporary) | 10 | Hematoma | 7 |
| Retrograde drilling | Nerve injury (dur. unk.) | 50 | Arterial bleeding | 17 | Delayed wound healing | 17 | Extensor hallucis longus weakness | 17 | N/A | |
| Fixation | Nerve injury (temporary) | 50 | Screw loosening | 50 | N/A | N/A | N/A | |||
| Matrix-assisted bone marrow stimulation | Superficial infection | 56 | Arthrofibrosis | 11 | Delayed union of osteotomy site | 11 | Nerve injury (temporary) | 11 | Donor site morbidity | 11 |
| Cartilage implantation | Nerve injury (temporary) | 44 | Delayed union of osteotomy site | 22 | Non-union of osteotomy site | 11 | Skin necrosis | 11 | Superficial infection | 11 |
| Osteo(chondral) autograft transplantation therapies | Donor site morbidity | 41 | Superficial infection | 13 | Nerve injury (temporary) | 6 | Nerve injury (dur. unk.) | 3 | Delayed union of osteotomy site | 3 |
| Osteo(chondral) allograft transplantation therapies a | DVT | 27 | Delayed union of osteotomy site | 20 | Plantar fasciitis | 13 | Arthrofibrosis | 7 | Cellulitis | 7 |
| Metal implants | Nerve injury (dur. unk.) | 50 | Wound dehiscence | 25 | Superficial infection | 17 | DVT | 8 | N/A | |
| Other | N/A | N/A | N/A | N/A | N/A | |||||
Rates are the proportions from the total amount complications per treatment option. DVT = deep venous thrombosis; N/A = not applicable; dur. unk. = duration unknown.
Nerve injury (duration unknown) and non-union both also have rates of 7% in this treatment option.
Discussion
The main finding of the present study is that there is a 5% risk of a complication with surgical treatment of an OLT. Significant differences between treatment modalities exist, with metal implants having a significantly higher complication rate than BMS therapies, retrograde drilling, fixation, matrix-assisted BMS, and cartilage implantation. BMS therapies have a significantly lower complication than osteo(chondral) autograft transplantation therapies, and it has also been shown that matrix-assisted BMS results in significantly lower complication rates than osteo(chondral) autograft- and allograft transplantation therapies.
Primary Outcome
There are multiple factors reported in the literature that affect the complication rate of OLT surgeries, such as operative time and the experience of the surgeon.207,208 The latter is of interest in the context of the present study as ankle arthroscopy is regarded as a challenging procedure. 209 Accordingly, this is of importance regarding the possible complications, considering damaging the peroneal nerve near the lateral portal in anterior ankle arthroscopy.210,211
Metal implants have a significantly higher complication rate compared with retrograde drilling, fixation, matrix-assisted BMS, and cartilage implantation. This may be due to several reasons. First, for the implantation of a metal implant, an open procedure with an osteotomy is often needed. This primarily, already, introduces a higher risk for potential infections, nerve injury, and other types of complications. This is because a longer incision is often needed which could damage nerve branches and introduce a greater porte d’entrée. This clarifies why in the analysis of the type of complications, the present study also found nerve damage and superficial infections to be more frequent in metal implants. Second, implantation of a metal resurfacing inlay implant may cause degenerative changes to the distal tibia. 27 The literature has found rates from 10% to 60%.16,69 Third, the learning curve of this procedure is fairly long.69,212 This is due in part to the fact that the depth of the implantation is of importance, due to the deformity of the talar cartilage during load.213,214 As mentioned above, the experience of a surgeon is of vast importance for the complication rate. Given the potential limited experience with these implants, may cause higher complication rates. In addition, it must be noted that metal implantation often is used as a salvage procedure and that may influence the complication rate. There is, however, an intrinsic relationship between the indication and the treatment technique and the other treatment groups also include a subset of secondary patients.
Secondary Outcomes
The severity of the complications was assessed with the use of the Modified Clavien-Dindo-Sink Complication Classification System for Orthopedic Surgery. 30 No Grade IV (a and b) and V complications were found. Grade I, II, and III complications have overall rates of 4%, 3%, and 3%, respectively. No significant difference was found for either grade.
In 5 treatment modalities (i.e., BMS therapies, retrograde drilling, fixation, cartilage implantation, and metal implants), nerve injury (temporary and duration unknown) was the most occurring complication. In the other treatment modalities, superficial infection (matrix-assisted BMS), donor site morbidity (osteo(chondral) autograft transplantation therapies) and DVT (osteo(chondral) allograft transplantation therapies) occurred the most times. All types of complications found in the present study are treatable and not life-threatening. It should be mentioned that the term nerve injury comprises complications from dysesthesia, neuralgia, paraesthesia, and altered sensation.
Defining the Term “Complication”
It is of critical importance in the analysis of complications to determine the definition of the term “complication.” Unfortunately, there is currently no widely accepted uniform definition for this term available, resulting in high heterogeneity in the reporting of complications in the literature. Factors related to the treatment failure were explicitly not considered as complications by the authors. This includes graft-related complications, such as failure to incorporate and reject a graft, as well as issues like persistent pain and no improvement of function. The removal of possible implanted hardware was also not included. Many studies removed screws from an osteotomy (reported rates of 17%-48% in 9 studies) which could also be for reasons other than, for example, irritation over the screw head.15,27 -29,83,87,122,133,179 As a result of the high heterogeneity in the definition of a complication, some studies report possible purely radiological findings, such as bone marrow edema and subchondral cyst formation, as a complication.112,176 These findings were not counted as a complication in the present study, as they may not have any clinical consequences.
To improve this troublesome situation, the present study recommends that a proper definition should be established for complications in the treatment of OLTs. A definition could be drafted on a consensus meeting.
Methodological Considerations
The methodological quality of the included articles can be considered fair, as shown by the MINORS score. Many studies were of a non-comparative design and only 7 randomized controlled trials (RCTs) were included. This may be of influence for the results, as a higher methodological quality is possibly closer to the actual complication rate of procedure. Although it was our intention to perform a sub-analysis on the complication rate and severity of primary OLTs versus non-primary OLTs, it must be stated that this was not possible due to the heterogeneous patient groups and limited reporting.
In the literature search, only articles from 1996 were searched. This filter was applied because the technique of ankle arthroscopy only really emerged since this year. It became more and more normal to use this surgical technique. This is due to technological advances and increased clarity about (the applicability of) the technique.215 -217
In the methodology of the present study, it was decided not to contact authors of articles in case of any doubt. There are, however, a high number of articles included, and therefore, the authors expect that this will have little impact on the results. In all, 137 studies (46% of the included articles) were excluded for the analysis because the complications were not (clearly) described.
Among the included studies, some were of retrospective nature, which may affect the complication rates. In effect, there may be underreporting due to selection, detection, and recall biases. Therefore, the complication rates found in the present study may be in reality higher. A 2-fold difference has been found in the literature. 218
Clinical Relevance and Future Perspectives
This study presents the complication rate per treatment option for OLTs and significant differences between treatment modalities. The complication rate and severity, in combination with the clinical efficacy and the costs, are one of the most important factors in the treatment selection. The clinical efficacy has already been recently reviewed, finding no clearly superior treatment for either primary or secondary lesions.19,20 Thus, to justify the treatment choice, mere complication and cost factors remain. The insight of this study that surgical treatment of OLTs can be considered safe and that there are differences between treatment modalities may be of importance in the consulting room. It can, thus, help clinicians and patients in the evidence-based shared decision-making process and can also manage postoperative expectations of clinicians and patients.
The present study was not able to analyze the surgery duration. This was often not reported and in the case of reporting, then it was not clear. For example, it was often not known to which treatment group it applied and what the start and end points of the measurement were. Surgery duration, however, has been identified as an independent risk factor for postoperative complications in orthopedic surgery.219 -226 Further research on risk factors, specific for this type of surgery, needs to be done in the future.
Conclusion
In 1 out of 20 patients treated surgically for an OLT, a complication occurs. Metal implants have a significantly higher complication rate than BMS therapies, retrograde drilling, fixation, matrix-assisted BMS, and cartilage implantation. BMS and matrix-assisted BMS have significantly lower complication rates compared with osteo(chondral) autograft transplantation therapies. In addition, matrix-assisted BMS is also significantly lower than osteo(chondral) allograft transplantation therapies. No life-threatening complications were reported. Nerve injuries were the most frequently observed type of complications for BMS therapies, retrograde drilling, fixation, cartilage implantation, and metal implants.
Supplemental Material
Supplemental material, sj-docx-1-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-2-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-3-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-4-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-5-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Footnotes
Supplementary material for this article is available on the Cartilage website at http://cart.sagepub.com/supplemental.
Author Contributions: J.J. Hollander, J. Dahmen, and K.S. Emanuel have made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data, and have been involved in drafting the manuscript. J.J. Hollander, J. Dahmen, K.S. Emanuel, S.A.S. Stufkens, J.G. Kennedy, and G.M.M.J. Kerkhoffs have been involved in revising the manuscript, critically for important intellectual content, and have given final approval of the version to be published.
Acknowledgments and Funding: The authors would like to thank F. van Etten-Jamaludin of the AMC Medical Library for her help with the literature search. The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable.
Informed Consent: Not applicable.
ORCID iDs: Julian J. Hollander  https://orcid.org/0000-0001-8345-1648
https://orcid.org/0000-0001-8345-1648
Jari Dahmen  https://orcid.org/0000-0002-6849-1008
https://orcid.org/0000-0002-6849-1008
References
- 1. Blom RP, Mol D, van Ruijven LJ, Kerkhoffs G, Smit TH. A single axial impact load causes articular damage that is not visible with micro-computed tomography: an ex vivo study on caprine tibiotalar joints. Cartilage. 2021. Sep 20;13:1490S-1500S. doi: 10.1177/1947603519876353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Martijn HA, Lambers KTA, Dahmen J, Stufkens SAS, Kerkhoffs G. High incidence of (osteo)chondral lesions in ankle fractures. Knee Surg Sports Traumatol Arthrosc. 2021. May;29(5):1523-34. doi: 10.1007/s00167-020-06187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. D’Ambrosi R, Maccario C, Serra N, Ursino C, Usuelli FG. Relationship between symptomatic osteochondral lesions of the talus and quality of life, body mass index, age, size and anatomic location. Foot Ankle Surg. 2018. Aug;24(4):365-72. doi: 10.1016/j.fas.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 4. Seo SG, Kim JS, Seo DK, Kim YK, Lee SH, Lee HS. Osteochondral lesions of the talus. Acta Orthop. 2018. Aug;89(4):462-7. doi: 10.1080/17453674.2018.1460777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Akpancar S, Gül D. Comparison of platelet rich plasma and prolotherapy in the management of osteochondral lesions of the talus: a retrospective cohort study. Med Sci Monit. 2019. Jul 30;25:5640-7. doi: 10.12659/msm.914111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Klammer G, Maquieira GJ, Spahn S, Vigfusson V, Zanetti M, Espinosa N. Natural history of nonoperatively treated osteochondral lesions of the talus. Foot Ankle Int. 2015. Jan;36(1):24-31. doi: 10.1177/1071100714552480. [DOI] [PubMed] [Google Scholar]
- 7. Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, Nyska M. Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med. 2012. Mar;40(3):534-41. doi: 10.1177/0363546511431238. [DOI] [PubMed] [Google Scholar]
- 8. Shearer C, Loomer R, Clement D. Nonoperatively managed stage 5 osteochondral talar lesions. Foot Ankle Int. 2002. Jul;23(7):651-4. doi: 10.1177/107110070202300712. [DOI] [PubMed] [Google Scholar]
- 9. Rikken QGH, Kerkhoffs G. Osteochondral lesions of the talus: an individualized treatment paradigm from the Amsterdam perspective. Foot Ankle Clin. 2021. Mar;26(1):121-36. doi: 10.1016/j.fcl.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 10. Yasui Y, Ramponi L, Seow D, Hurley ET, Miyamoto W, Shimozono Y, et al. Systematic review of bone marrow stimulation for osteochondral lesion of talus—evaluation for level and quality of clinical studies. World J Orthop. 2017. Dec 18;8(12):956-63. doi: 10.5312/wjo.v8.i12.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hyer CF, Berlet GC, Philbin TM, Lee TH. Retrograde drilling of osteochondral lesions of the talus. Foot Ankle Spec. 2008. Aug;1(4):207-9. doi: 10.1177/1938640008321653. [DOI] [PubMed] [Google Scholar]
- 12. Kerkhoffs GMMJ, Reilingh ML, Gerards RM, de Leeuw PA. Lift, drill, fill and fix (LDFF): a new arthroscopic treatment for talar osteochondral defects. Knee Surg Sports Traumatol Arthrosc. 2016. Apr;24(4):1265-71. doi: 10.1007/s00167-014-3057-7. [DOI] [PubMed] [Google Scholar]
- 13. D'Ambrosi R, Villafañe JH, Indino C, Liuni FM, Berjano P, Usuelli FG. Return to sport after arthroscopic autologous matrix-induced chondrogenesis for patients with osteochondral lesion of the talus. Clin J Sport Med. 2019. Nov;29(6):470-5. doi: 10.1097/jsm.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 14. Giannini S, Buda R, Ruffilli A, Cavallo M, Pagliazzi G, Bulzamini MC, et al. Arthroscopic autologous chondrocyte implantation in the ankle joint. Knee Surg Sports Traumatol Arthrosc. 2014. Jun;22(6):1311-9. doi: 10.1007/s00167-013-2640-7. [DOI] [PubMed] [Google Scholar]
- 15. Kerkhoffs GMMJ, Altink JN, Stufkens SAS, Dahmen J. Osteoperiostale Beckenkammtransplantation (TOPIC) für große Defekte der medialen Talusrolle: Operationstechnik [Talar OsteoPeriostic grafting from the Iliac Crest (TOPIC) for large medial talar osteochondral defects: operative technique]. Oper Orthop Traumatol. 2021. Apr;33(2):160-9. doi: 10.1007/s00064-020-00673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Bergen CJ, van Eekeren IC, Reilingh ML, Sierevelt IN, van Dijk CN. Treatment of osteochondral defects of the talus with a metal resurfacing inlay implant after failed previous surgery: a prospective study. Bone Joint J. 2013. Dec;95-b(12):1650-5. doi: 10.1302/0301-620x.95b12.32455. [DOI] [PubMed] [Google Scholar]
- 17. Adams SB, Jr, Viens NA, Easley ME, Stinnett SS, Nunley JA, II. Midterm results of osteochondral lesions of the talar shoulder treated with fresh osteochondral allograft transplantation. J Bone Joint Surg Am. 2011. Apr 6;93(7):648-54. doi: 10.2106/jbjs.J.00141. [DOI] [PubMed] [Google Scholar]
- 18. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997. Mar;44(5):681-92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 19. Dahmen J, Lambers KTA, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs G. No superior treatment for primary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2018. Jul;26(7):2142-57. doi: 10.1007/s00167-017-4616-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lambers KTA, Dahmen J, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs G. No superior surgical treatment for secondary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2018. Jul;26(7):2158-70. doi: 10.1007/s00167-017-4629-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chien PF, Khan KS, Siassakos D. Registration of systematic reviews: PROSPERO. Bjog. 2012. Jul;119(8):903-5. doi: 10.1111/j.1471-0528.2011.03242.x. [DOI] [PubMed] [Google Scholar]
- 22. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009. Jul 21;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003. Sep;73(9):712-6. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 25. Sokol DK, Wilson J. What is a surgical complication? World J Surg. 2008. Jun;32(6):942-4. doi: 10.1007/s00268-008-9471-6. [DOI] [PubMed] [Google Scholar]
- 26. Looney AM, Fackler NP, Pianka MA, Bodendorfer BM, Fryar CM, Conroy CM, et al. No difference in complications between elbow ulnar collateral ligament reconstruction with the docking and modified Jobe techniques: a systematic review and meta-analysis. Am J Sports Med. 2022. Sep 7;50:2324-38. doi: 10.1177/03635465211023952. [DOI] [PubMed] [Google Scholar]
- 27. Ebskov LB, Hegnet Andersen K, Bro Rasmussen P, Johansen JK, Benyahia M. Mid-term results after treatment of complex talus osteochondral defects with HemiCAP implantation. Foot Ankle Surg. 2020. Jun;26(4):384-90. doi: 10.1016/j.fas.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 28. Vuurberg G, Reilingh ML, van Bergen CJA, van Eekeren ICM, Gerards RM, van Dijk CN. Metal resurfacing inlay implant for osteochondral talar defects after failed previous surgery: a midterm prospective follow-up study. Am J Sports Med. 2018. Jun;46(7):1685-92. doi: 10.1177/0363546518764916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Weigelt L, Hartmann R, Pfirrmann C, Espinosa N, Wirth SH. Autologous matrix-induced chondrogenesis for osteochondral lesions of the talus: a clinical and radiological 2- to 8-year follow-up study. Am J Sports Med. 2019. Jun;47(7):1679-86. doi: 10.1177/0363546519841574. [DOI] [PubMed] [Google Scholar]
- 30. Dodwell ER, Pathy R, Widmann RF, Green DW, Scher DM, Blanco JS, et al. Reliability of the modified Clavien-Dindo-sink complication classification system in pediatric orthopaedic surgery. JB JS Open Access. 2018. Dec 20;3(4):e0020. doi: 10.2106/jbjs.Oa.18.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32. Jackson D, Bowden J. Confidence intervals for the between-study variance in random-effects meta-analysis using generalised heterogeneity statistics: should we use unequal tails? BMC Med Res Methodol. 2016;16(1):118. doi: 10.1186/s12874-016-0219-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26(4):404-13. doi: 10.1093/biomet/26.4.404. [DOI] [Google Scholar]
- 34. Li X, Dusseldorp E, Su X, Meulman JJ. Multiple moderator meta-analysis using the R-package meta-CART. Behav Res Methods. 2020. Dec;52(6):2657-73. doi: 10.3758/s13428-020-01360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019. Nov;22(4):153-60. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Assenmacher JA, Kelikian AS, Gottlob C, Kodros S. Arthroscopically assisted autologous osteochondral transplantation for osteochondral lesions of the talar dome: an MRI and clinical follow-up study. Foot Ankle Int. 2001. Jul;22(7):544-51. doi: 10.1177/107110070102200703. [DOI] [PubMed] [Google Scholar]
- 37. Ahmad J, Maltenfort M. Arthroscopic treatment of osteochondral lesions of the talus with allograft cartilage matrix. Foot Ankle Int. 2017. Aug;38(8):855-62. doi: 10.1177/1071100717709571. [DOI] [PubMed] [Google Scholar]
- 38. Akmeşe R, Ertan MB, Kocaoğlu H. Comparison of chitosan-based liquid scaffold and hyaluronic acid-based soft scaffold for treatment of talus osteochondral lesions. Foot Ankle Int. 2020. Oct;41(10):1240-8. doi: 10.1177/1071100720937662. [DOI] [PubMed] [Google Scholar]
- 39. Al-Shaikh RA, Chou LB, Mann JA, Dreeben SM, Prieskorn D. Autologous osteochondral grafting for talar cartilage defects. Foot Ankle Int. 2002. May;23(5):381-9. doi: 10.1177/107110070202300502. [DOI] [PubMed] [Google Scholar]
- 40. Albano D, Martinelli N, Bianchi A, Messina C, Malerba F, Sconfienza LM. Clinical and imaging outcome of osteochondral lesions of the talus treated using autologous matrix-induced chondrogenesis technique with a biomimetic scaffold. BMC Musculoskelet Disord. 2017. Jul 18;18(1):306. doi: 10.1186/s12891-017-1679-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Anders S, Goetz J, Schubert T, Grifka J, Schaumburger J. Treatment of deep articular talus lesions by matrix associated autologous chondrocyte implantation—results at five years. Int Orthop. 2012. Nov;36(11):2279-85. doi: 10.1007/s00264-012-1635-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Anders S, Lechler P, Rackl W, Grifka J, Schaumburger J. Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. Int Orthop. 2012. Aug;36(8):1635-40. doi: 10.1007/s00264-012-1530-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Angthong C, Yoshimura I, Kanazawa K, Takeyama A, Hagio T, Ida T, et al. Critical three-dimensional factors affecting outcome in osteochondral lesion of the talus. Knee Surg Sports Traumatol Arthrosc. 2013. Jun;21(6):1418-26. doi: 10.1007/s00167-013-2364-8. [DOI] [PubMed] [Google Scholar]
- 44. Arauz JMY, Del Vecchio JJ, Bilbao F, Raimondi N. Osteochondral lesions of the talus treatment with fresh frozen allograft. Foot Ankle Surg. 2017. Dec;23(4):296-301. doi: 10.1016/j.fas.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 45. Aurich M, Bedi HS, Smith PJ, Rolauffs B, Mückley T, Clayton J, et al. Arthroscopic treatment of osteochondral lesions of the ankle with matrix-associated chondrocyte implantation: early clinical and magnetic resonance imaging results. Am J Sports Med. 2011. Feb;39(2):311-9. doi: 10.1177/0363546510381575. [DOI] [PubMed] [Google Scholar]
- 46. Bai L, Guan S, Liu S, You T, Xie X, Chen P, et al. Clinical outcomes of osteochondral lesions of the talus with large subchondral cysts treated with osteotomy and autologous chondral grafts: minimum 2-year follow-up and second-look evaluation. Orthop J Sports Med. 2020. Jul;8(7):2325967120937798. doi: 10.1177/2325967120937798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Basal O, Aslan TT. A triplanar osteotomy technique in arthroscopy-assisted ankle mosaicplasty. J Orthop Surg (Hong Kong). 2020. Jan-Apr;28(1):2309499020905054. doi: 10.1177/2309499020905054. [DOI] [PubMed] [Google Scholar]
- 48. Battaglia M, Rimondi E, Monti C, Guaraldi F, Sant’Andrea A, Buda R, et al. Validity of T2 mapping in characterization of the regeneration tissue by bone marrow derived cell transplantation in osteochondral lesions of the ankle. Eur J Radiol. 2011. Nov;80(2):e132-9. doi: 10.1016/j.ejrad.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 49. Baumfeld T, Baumfeld D, Prado M, Nery C. All-arthroscopic AMIC(®) (AT-AMIC) for the treatment of talar osteochondral defects: a short follow-up case series. Foot (Edinb). 2018. Dec;37:23-7. doi: 10.1016/j.foot.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 50. Baumgartner M, Wagner T, Bösch P. Therapie der Osteochondrosis dissecans tali mittels Mosaikplastik. Fuss. 2006;4(4):247-55. doi: 10.1007/s10302-006-0168-6. [DOI] [Google Scholar]
- 51. Baums MH, Heidrich G, Schultz W, Steckel H, Kahl E, Klinger HM. Autologous chondrocyte transplantation for treating cartilage defects of the talus. J Bone Joint Surg Am. 2006. Feb;88(2):303-8. doi: 10.2106/jbjs.E.00033. [DOI] [PubMed] [Google Scholar]
- 52. Becher C, Thermann H. Results of microfracture in the treatment of articular cartilage defects of the talus. Foot Ankle Int. 2005. Aug;26(8):583-9. doi: 10.1177/107110070502600801. [DOI] [PubMed] [Google Scholar]
- 53. Beck S, Claßen T, Haversath M, Jäger M, Landgraeber S. Operative technique and clinical outcome in endoscopic core decompression of osteochondral lesions of the talus: a pilot study. Med Sci Monit. 2016. Jun 30;22:2278-83. doi: 10.12659/msm.896522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Berlet GC, Hyer CF, Philbin TM, Hartman JF, Wright ML. Does fresh osteochondral allograft transplantation of talar osteochondral defects improve function? Clin Orthop Relat Res. 2011. Aug;469(8):2356-66. doi: 10.1007/s11999-011-1813-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bleazey S, Brigido SA. Reconstruction of complex osteochondral lesions of the talus with cylindrical sponge allograft and particulate juvenile cartilage graft: provisional results with a short-term follow-up. Foot Ankle Spec. 2012. Oct;5(5):300-5. doi: 10.1177/1938640012457937. [DOI] [PubMed] [Google Scholar]
- 56. Bohnsack M, Fischer J, Lipka W, Schmolke S, Börner C, Wirth CJ, et al. The influence of limited postoperative weight-bearing on the outcome of drilling in osteochondritis dissecans tali. Arch Orthop Trauma Surg. 2003. Nov;123(9):447-50. doi: 10.1007/s00402-003-0550-8. [DOI] [PubMed] [Google Scholar]
- 57. Brigido SA, Protzman NM, Galli MM, Bleazey ST. The role of demineralized allograft subchondral bone in the treatment of talar cystic OCD lesions that have failed microfracture. Foot Ankle Spec. 2014. Oct;7(5):377-86. doi: 10.1177/1938640014531984. [DOI] [PubMed] [Google Scholar]
- 58. Buda R, Vannini F, Cavallo M, Baldassarri M, Natali S, Castagnini F, et al. One-step bone marrow-derived cell transplantation in talar osteochondral lesions: mid-term results. Joints. 2013. Jul-Sep;1(3):102-7. [PMC free article] [PubMed] [Google Scholar]
- 59. Carlson MJ, Antkowiak TT, Larsen NJ, Applegate GR, Ferkel RD. Arthroscopic treatment of osteochondral lesions of the talus in a pediatric population: a minimum 2-year follow-up. Am J Sports Med. 2020. Jul;48(8):1989-98. doi: 10.1177/0363546520924800. [DOI] [PubMed] [Google Scholar]
- 60. Chen W, Tang K, Yuan C, Zhou Y, Tao X. Intermediate results of large cystic medial osteochondral lesions of the talus treated with osteoperiosteal cylinder autografts from the medial tibia. Arthroscopy. 2015. Aug;31(8):1557-64. doi: 10.1016/j.arthro.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 61. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008. Jan;24(1):106-12. doi: 10.1016/j.arthro.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 62. Cuttica DJ, Smith WB, Hyer CF, Philbin TM, Berlet GC. Osteochondral lesions of the talus: predictors of clinical outcome. Foot Ankle Int. 2011. Nov;32(11):1045-51. doi: 10.3113/fai.2011.1045. [DOI] [PubMed] [Google Scholar]
- 63. de Lima E, de Queiroz F, Lopes OV, Jr, Spinelli LDF. Treatment of osteochondral lesions of the talus by means of thearthroscopy-assisted microperforation technique. Rev Bras Ortop. 2011. Nov-Dec;46(6):702-8. doi: 10.1016/s2255-4971(15)30328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. DeSandis BA, Haleem AM, Sofka CM, O’Malley MJ, Drakos MC. Arthroscopic treatment of osteochondral lesions of the talus using juvenile articular cartilage allograft and autologous bone marrow aspirate concentration. J Foot Ankle Surg. 2018. Mar-Apr;57(2):273-80. doi: 10.1053/j.jfas.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 65. Di Cave E, Versari P, Sciarretta F, Luzon D, Marcellini L. Biphasic bioresorbable scaffold (TruFit Plug(®)) for the treatment of osteochondral lesions of talus: 6- to 8-year follow-up. Foot (Edinb). 2017. Dec;33:48-52. doi: 10.1016/j.foot.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 66. Doral MN, Bilge O, Batmaz G, Donmez G, Turhan E, Demirel M, et al. Treatment of osteochondral lesions of the talus with microfracture technique and postoperative hyaluronan injection. Knee Surg Sports Traumatol Arthrosc. 2012. Jul;20(7):1398-403. doi: 10.1007/s00167-011-1856-7. [DOI] [PubMed] [Google Scholar]
- 67. El-Rashidy H, Villacis D, Omar I, Kelikian AS. Fresh osteochondral allograft for the treatment of cartilage defects of the talus: a retrospective review. J Bone Joint Surg Am. 2011. Sep 7;93(17):1634-40. doi: 10.2106/jbjs.J.00900. [DOI] [PubMed] [Google Scholar]
- 68. Emre TY, Ege T, Cift HT, Demircioğlu DT, Seyhan B, Uzun M. Open mosaicplasty in osteochondral lesions of the talus: a prospective study. J Foot Ankle Surg. 2012. Sep-Oct;51(5):556-60. doi: 10.1053/j.jfas.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 69. Ettinger S, Stukenborg-Colsman C, Waizy H, Becher C, Yao D, Claassen L, et al. Results of HemiCAP(®) implantation as a salvage procedure for osteochondral lesions of the talus. J Foot Ankle Surg. 2017. Jul-Aug;56(4):788-92. doi: 10.1053/j.jfas.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 70. Flynn S, Ross KA, Hannon CP, Yasui Y, Newman H, Murawski CD, et al. Autologous osteochondral transplantation for osteochondral lesions of the talus. Foot Ankle Int. 2016. Apr;37(4):363-72. doi: 10.1177/1071100715620423. [DOI] [PubMed] [Google Scholar]
- 71. Fraser EJ, Harris MC, Prado MP, Kennedy JG. Autologous osteochondral transplantation for osteochondral lesions of the talus in an athletic population. Knee Surg Sports Traumatol Arthrosc. 2016. Apr;24(4):1272-9. doi: 10.1007/s00167-015-3606-8. [DOI] [PubMed] [Google Scholar]
- 72. Galla M, Duensing I, Kahn TL, Barg A. Open reconstruction with autologous spongiosa grafts and matrix-induced chondrogenesis for osteochondral lesions of the talus can be performed without medial malleolar osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019. Sep;27(9):2789-95. doi: 10.1007/s00167-018-5063-7. [DOI] [PubMed] [Google Scholar]
- 73. Galli MM, Protzman NM, Bleazey ST, Brigido SA. Role of demineralized allograft subchondral bone in the treatment of shoulder lesions of the talus: clinical results with two-year follow-up. J Foot Ankle Surg. 2015. Jul-Aug;54(4):717-22. doi: 10.1053/j.jfas.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 74. Gautier E, Kolker D, Jakob RP. Treatment of cartilage defects of the talus by autologous osteochondral grafts. J Bone Joint Surg Br. 2002. Mar;84(2):237-44. doi: 10.1302/0301-620x.84b2.11735. [DOI] [PubMed] [Google Scholar]
- 75. Georgiannos D, Bisbinas I, Badekas A. Osteochondral transplantation of autologous graft for the treatment of osteochondral lesions of talus: 5- to 7-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2016. Dec;24(12):3722-9. doi: 10.1007/s00167-014-3389-3. [DOI] [PubMed] [Google Scholar]
- 76. Giannini S, Battaglia M, Buda R, Cavallo M, Ruffilli A, Vannini F. Surgical treatment of osteochondral lesions of the talus by open-field autologous chondrocyte implantation: a 10-year follow-up clinical and magnetic resonance imaging T2-mapping evaluation. Am J Sports Med. 2009. Nov;37(Suppl 1):112S-118S. doi: 10.1177/0363546509349928. [DOI] [PubMed] [Google Scholar]
- 77. Giannini S, Buda R, Battaglia M, Cavallo M, Ruffilli A, Ramponi L, et al. One-step repair in talar osteochondral lesions: 4-year clinical results and T2-mapping capability in outcome prediction. Am J Sports Med. 2013. Mar;41(3):511-8. doi: 10.1177/0363546512467622. [DOI] [PubMed] [Google Scholar]
- 78. Giannini S, Buda R, Grigolo B, Vannini F. Autologous chondrocyte transplantation in osteochondral lesions of the ankle joint. Foot Ankle Int. 2001. Jun;22(6):513-7. doi: 10.1177/107110070102200612. [DOI] [PubMed] [Google Scholar]
- 79. Giannini S, Buda R, Grigolo B, Vannini F, De Franceschi L, Facchini A. The detached osteochondral fragment as a source of cells for autologous chondrocyte implantation (ACI) in the ankle joint. Osteoarthritis Cartilage. 2005. Jul;13(7):601-7. doi: 10.1016/j.joca.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 80. Giannini S, Buda R, Vannini F, Di Caprio F, Grigolo B. Arthroscopic autologous chondrocyte implantation in osteochondral lesions of the talus: surgical technique and results. Am J Sports Med. 2008. May;36(5):873-80. doi: 10.1177/0363546507312644. [DOI] [PubMed] [Google Scholar]
- 81. Goh GS, Bin Abd, Razak HR, Mitra AK. Outcomes are favorable after arthroscopic treatment of osteochondritis dissecans of the talus. J Foot Ankle Surg. 2015. Jan-Feb;54(1):57-60. doi: 10.1053/j.jfas.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 82. Gu W, Li T, Shi Z, Mei G, Xue J, Zou J, et al. Management of Hepple stage v osteochondral lesion of the talus with a platelet-rich plasma scaffold. Biomed Res Int. 2017;2017:6525373. doi: 10.1155/2017/6525373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gül M, Yavuz U, Çetinkaya E, Aykut ÜS, Özkul B, Kabukçuoğlu YS. Chevron osteotomy in patients with scheduled osteotomy of the medial malleolus. Acta Orthop Traumatol Turc. 2015;49(4):399-404. doi: 10.3944/aott.2015.14.0186. [DOI] [PubMed] [Google Scholar]
- 84. Hangody L, Kish G, Módis L, Szerb I, Gáspár L, Diószegi Z, et al. Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int. 2001. Jul;22(7):552-8. doi: 10.1177/107110070102200704. [DOI] [PubMed] [Google Scholar]
- 85. Haraguchi N, Shiratsuchi T, Ota K, Ozeki T, Gibu M, Niki H. Fixation of the osteochondral talar fragment yields good results regardless of lesion size or chronicity. Knee Surg Sports Traumatol Arthrosc. 2020. Jan;28(1):291-7. doi: 10.1007/s00167-019-05716-8. [DOI] [PubMed] [Google Scholar]
- 86. Heida KA, Jr, Tihista MC, Kusnezov NA, Dunn JC, Orr JD. Outcomes and predictors of postoperative pain improvement following particulated juvenile cartilage allograft transplant for osteochondral lesions of the talus. Foot Ankle Int. 2020. May;41(5):572-81. doi: 10.1177/1071100720903721. [DOI] [PubMed] [Google Scholar]
- 87. Hintermann B, Wagener J, Knupp M, Schweizer C J, Schaefer D. Treatment of extended osteochondral lesions of the talus with a free vascularised bone graft from the medial condyle of the femur. Bone Joint J. 2015. Sep;97-B(9):1242-9. doi: 10.1302/0301-620x.97b9.35292. [DOI] [PubMed] [Google Scholar]
- 88. Hu Y, Guo Q, Jiao C, Mei Y, Jiang D, Wang J, et al. Treatment of large cystic medial osteochondral lesions of the talus with autologous osteoperiosteal cylinder grafts. Arthroscopy. 2013. Aug;29(8):1372-9. doi: 10.1016/j.arthro.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 89. Hu Y, Yue C, Li X, Li Z, Zhou D, Xu H, et al. A novel medial malleolar osteotomy technique for the treatment of osteochondral lesions of the talus. Orthop J Sports Med. 2021. Mar;9(3):2325967121989988. doi: 10.1177/2325967121989988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Imhoff AB, Paul J, Ottinger B, Wörtler K, Lämmle L, Spang J, et al. Osteochondral transplantation of the talus: long-term clinical and magnetic resonance imaging evaluation. Am J Sports Med. 2011. Jul;39(7):1487-93. doi: 10.1177/0363546510397726. [DOI] [PubMed] [Google Scholar]
- 91. Jackson AT, Drayer NJ, Samona J, Dukes CA, Chen CS, Arrington EA, et al. Osteochondral allograft transplantation surgery for osteochondral lesions of the talus in athletes. J Foot Ankle Surg. 2019. Jul;58(4):623-7. doi: 10.1053/j.jfas.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 92. Jung HG, Carag JA, Park JY, Kim TH, Moon SG. Role of arthroscopic microfracture for cystic type osteochondral lesions of the talus with radiographic enhanced MRI support. Knee Surg Sports Traumatol Arthrosc. 2011. May;19(5):858-62. doi: 10.1007/s00167-011-1411-6. [DOI] [PubMed] [Google Scholar]
- 93. Jurina A, Dimnjaković D, Mustapić M, Smoljanović T, Bojanić I. Clinical and MRI outcomes after surgical treatment of osteochondral lesions of the talus in skeletally immature children. J Pediatr Orthop. 2018. Feb;38(2):122-7. doi: 10.1097/bpo.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 94. Kanatlı U, Eren A, Eren TK, Vural A, Geylan DE, Öner AY. Single-step arthroscopic repair with cell-free polymer-based scaffold in osteochondral lesions of the talus: clinical and radiological results. Arthroscopy. 2017. Sep;33(9):1718-26. doi: 10.1016/j.arthro.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 95. Kennedy JG, Murawski CD. The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate: surgical technique. Cartilage. 2011. Oct;2(4):327-36. doi: 10.1177/1947603511400726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kim T, Haskell A. Patient-reported outcomes after structural autograft for large or cystic talar dome osteochondral lesions. Foot Ankle Int. 2020. May;41(5):549-55. doi: 10.1177/1071100720907313. [DOI] [PubMed] [Google Scholar]
- 97. Kolker D, Murray M, Wilson M. Osteochondral defects of the talus treated with autologous bone grafting. J Bone Joint Surg Br. 2004. May;86(4):521-6. [PubMed] [Google Scholar]
- 98. Körner D, Gonser CE, Döbele S, Konrads C, Springer F, Keller G. Matrix-associated autologous chondrocyte implantation with autologous bone grafting of osteochondral lesions of the talus in adolescents: patient-reported outcomes with a median follow-up of 6 years. J Orthop Surg Res. 2021. Apr 8;16(1):243. doi: 10.1186/s13018-021-02384-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Koulalis D, Schultz W, Heyden M. Autologous chondrocyte transplantation for osteochondritis dissecans of the talus. Clin Orthop Relat Res. 2002. Feb;395:186-92. doi: 10.1097/00003086-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 100. Kreuz PC, Steinwachs M, Edlich M, Kaiser T, Mika J, Lahm A, et al. The anterior approach for the treatment of posterior osteochondral lesions of the talus: comparison of different surgical techniques. Arch Orthop Trauma Surg. 2006. May;126(4):241-6. doi: 10.1007/s00402-005-0058-5. [DOI] [PubMed] [Google Scholar]
- 101. Kubosch EJ, Erdle B, Izadpanah K, Kubosch D, Uhl M, Südkamp NP, et al. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop. 2016. Jan;40(1):65-71. doi: 10.1007/s00264-015-2988-z. [DOI] [PubMed] [Google Scholar]
- 102. Kumai T, Takakura Y, Kitada C, Tanaka Y, Hayashi K. Fixation of osteochondral lesions of the talus using cortical bone pegs. J Bone Joint Surg Br. 2002. Apr;84(3):369-74. doi: 10.1302/0301-620x.84b3.12373. [DOI] [PubMed] [Google Scholar]
- 103. Kwak SK, Kern BS, Ferkel RD, Chan KW, Kasraeian S, Applegate GR. Autologous chondrocyte implantation of the ankle: 2- to 10-year results. Am J Sports Med. 2014. Sep;42(9):2156-64. doi: 10.1177/0363546514540587. [DOI] [PubMed] [Google Scholar]
- 104. Lambers KTA, Dahmen J, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs G. Arthroscopic lift, drill, fill and fix (LDFF) is an effective treatment option for primary talar osteochondral defects. Knee Surg Sports Traumatol Arthrosc. 2020. Jan;28(1):141-7. doi: 10.1007/s00167-019-05687-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Largey A, Faure P, Hebrard W, Hamoui M, Canovas F. Osteochondral transfer using a transmalleolar approach for arthroscopic management of talus posteromedial lesions. Orthop Traumatol Surg Res. 2009. Nov;95(7):537-42. doi: 10.1016/j.otsr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 106. Lee KB, Yang HK, Moon ES, Song EK. Modified step-cut medial malleolar osteotomy for osteochondral grafting of the talus. Foot Ankle Int. 2008. Nov;29(11):1107-10. doi: 10.3113/fai.2008.1107. [DOI] [PubMed] [Google Scholar]
- 107. Lee KT, Kim JS, Young KW, Lee YK, Park YU, Kim YH, et al. The use of fibrin matrix-mixed gel-type autologous chondrocyte implantation in the treatment for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2013. Jun;21(6):1251-60. doi: 10.1007/s00167-012-2096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Leumann A, Valderrabano V, Wiewiorski M, Barg A, Hintermann B, Pagenstert G. Bony periosteum-covered iliac crest plug transplantation for severe osteochondral lesions of the talus: a modified mosaicplasty procedure. Knee Surg Sports Traumatol Arthrosc. 2014. Jun;22(6):1304-10. doi: 10.1007/s00167-013-2604-y. [DOI] [PubMed] [Google Scholar]
- 109. Li S, Li H, Liu Y, Qu F, Wang J, Liu C. Clinical outcomes of early weight-bearing after arthroscopic microfracture during the treatment of osteochondral lesions of the talus. Chin Med J (Engl). 2014;127(13):2470-4. [PubMed] [Google Scholar]
- 110. Li S, Lu R, Zhang J, Tao H, Hua Y. Outcomes of arthroscopic bone graft transplantation for Hepple stage V osteochondral lesions of the talus. Ann Transl Med. 2021. May;9(10):884. doi: 10.21037/atm-21-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Lin JS, Andersen LB, Juliano PJ. Effectiveness of composite bone graft substitute plugs in the treatment of chondral and osteochondral lesions of the talus. J Foot Ankle Surg. 2010. May-Jun;49(3):224-31. doi: 10.1053/j.jfas.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 112. López-Alcorocho JM, Guillén-Vicente I, Rodríguez-Iñigo E, Navarro R, Caballero-Santos R, Guillén-Vicente M, et al. High-density autologous chondrocyte implantation as treatment for ankle osteochondral defects. Cartilage. 2021. Jul;12(3):307-19. doi: 10.1177/1947603519835898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Lundeen GA, Dunaway LJ. Immediate unrestricted postoperative weightbearing and mobilization after bone marrow stimulation of large osteochondral lesions of the talus. Cartilage. 2017. Jan;8(1):73-9. doi: 10.1177/1947603516657639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Magnan B, Samaila E, Bondi M, Vecchini E, Micheloni GM, Bartolozzi P. Three-dimensional matrix-induced autologous chondrocytes implantation for osteochondral lesions of the talus: midterm results. Adv Orthop. 2012;2012:942174. doi: 10.1155/2012/942174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Manzi J, Arzani A, Hamula MJ, Manchanda K, Dhanaraj D, Chapman CB. Long-term patient-reported outcome measures following particulated juvenile allograft cartilage implantation for treatment of difficult osteochondral lesions of the talus. Foot Ankle Int. 2021. Jun 11;42:1399-409. doi: 10.1177/10711007211014173. [DOI] [PubMed] [Google Scholar]
- 116. Masquijo JJ, Ferreyra A, Baroni E. Arthroscopic retrograde drilling in juvenile osteochondritis dissecans of the talus. J Pediatr Orthop. 2016. Sep;36(6):589-93. doi: 10.1097/bpo.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 117. Ming SH, Tay Keng Jin D, Amit Kanta M. Arthroscopic treatment of osteochondritis dissecans of the talus. Foot and Ankle Surgery. 2004;10(4):181-6. doi: 10.1016/j.fas.2004.07.009. [DOI] [Google Scholar]
- 118. Minokawa S, Yoshimura I, Kanazawa K, Hagio T, Nagatomo M, Sugino Y, et al. Retrograde drilling for osteochondral lesions of the talus in skeletally immature children. Foot Ankle Int. 2020. Jul;41(7):827-33. doi: 10.1177/1071100720920847. [DOI] [PubMed] [Google Scholar]
- 119. Nakasa T, Ikuta Y, Ota Y, Kanemitsu M, Adachi N. Clinical results of bioabsorbable pin fixation relative to the bone condition for osteochondral lesion of the talus. Foot Ankle Int. 2019. Dec;40(12):1388-96. doi: 10.1177/1071100719868726. [DOI] [PubMed] [Google Scholar]
- 120. Nguyen A, Ramasamy A, Walsh M, McMenemy L, Calder JDF. Autologous osteochondral transplantation for large osteochondral lesions of the talus is a viable option in an athletic population. Am J Sports Med. 2019. Dec;47(14):3429-35. doi: 10.1177/0363546519881420. [DOI] [PubMed] [Google Scholar]
- 121. Ogilvie-Harris DJ, Sarrosa EA. Arthroscopic treatment of osteochondritis dissecans of the talus. Arthroscopy. 1999. Nov-Dec;15(8):805-8. doi: 10.1053/ar.1999.v15.0150801. [DOI] [PubMed] [Google Scholar]
- 122. Orr JD, Dunn JC, Heida KA, Jr, Kusnezov NA, Waterman BR, Belmont PJ, Jr. Results and functional outcomes of structural fresh osteochondral allograft transfer for treatment of osteochondral lesions of the talus in a highly active population. Foot Ankle Spec. 2017. Apr;10(2):125-32. doi: 10.1177/1938640016666924. [DOI] [PubMed] [Google Scholar]
- 123. Pagliazzi G, Baldassarri M, Perazzo L, Vannini F, Castagnini F, Buda R. Tissue bioengineering in the treatment of osteochondritis dissecans of the talus in children with open physis: preliminary results. J Pediatr Orthop. 2018. Aug;38(7):375-81. doi: 10.1097/bpo.0000000000000827. [DOI] [PubMed] [Google Scholar]
- 124. Pagliazzi G, Vannini F, Battaglia M, Ramponi L, Buda R. Autologous chondrocyte implantation for talar osteochondral lesions: comparison between 5-year follow-up magnetic resonance imaging findings and 7-year follow-up clinical results. J Foot Ankle Surg. 2018. Mar-Apr;57(2):221-5. doi: 10.1053/j.jfas.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 125. Park JH, Park KH, Cho JY, Han SH, Lee JW. Bone marrow stimulation for osteochondral lesions of the talus: are clinical outcomes maintained 10 years later? Am J Sports Med. 2021. Apr;49(5):1220-6. doi: 10.1177/0363546521992471. [DOI] [PubMed] [Google Scholar]
- 126. Paul J, Sagstetter A, Kriner M, Imhoff AB, Spang J, Hinterwimmer S. Donor-site morbidity after osteochondral autologous transplantation for lesions of the talus. J Bone Joint Surg Am. 2009. Jul;91(7):1683-8. doi: 10.2106/jbjs.H.00429. [DOI] [PubMed] [Google Scholar]
- 127. Penner M, Younger A, Wing K, Cresswell M, Veljkovic A. Arthroscopic repair of talar osteochondral defects with umbilical cord allograft: a prospective, single-center, pilot study. Foot Ankle Spec. 2021. Jun;14(3):193-200. doi: 10.1177/1938640020910953. [DOI] [PubMed] [Google Scholar]
- 128. Petersen W, Taheri P, Schliemann B, Achtnich A, Winter C, Forkel P. Osteochondral transplantation for the treatment of osteochondral defects at the talus with the Diamond twin system(®) and graft harvesting from the posterior femoral condyles. Arch Orthop Trauma Surg. 2014. Jun;134(6):843-52. doi: 10.1007/s00402-014-1991-y. [DOI] [PubMed] [Google Scholar]
- 129. Sabaghzadeh A, Mirzaee F, Shahriari Rad H, Bahramian F, Alidousti A, Aslani H. Osteochondral autograft transfer (mosaicplasty) for treatment of patients with osteochondral lesions of talus. Chin J Traumatol. 2020. Feb;23(1):60-2. doi: 10.1016/j.cjtee.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Sadlik B, Blasiak A, Barg A, Valderrabano V, Wiewiorski M. Dry arthroscopy with a retraction system for matrix-aided cartilage repair of osteochondral lesions of the talus. Foot Ankle Int. 2015. Mar;36(3):339-43. doi: 10.1177/1071100714557521. [DOI] [PubMed] [Google Scholar]
- 131. El Sallakh S. Arthroscopic debridement and microfracture for osteochondral lesions of the talus. Curr Orthop Pract. 2012;23(2):116-21. doi: 10.1097/BCO.0b013e318247c2fb. [DOI] [Google Scholar]
- 132. Sammarco GJ, Makwana NK. Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int. 2002. Aug;23(8):693-8. doi: 10.1177/107110070202300803. [DOI] [PubMed] [Google Scholar]
- 133. Schneider TE, Karaikudi S. Matrix-induced autologous chondrocyte implantation (MACI) grafting for osteochondral lesions of the talus. Foot Ankle Int. 2009. Sep;30(9):810-4. doi: 10.3113/fai.2009.0810. [DOI] [PubMed] [Google Scholar]
- 134. Schuh A, Salminen S, Zeiler G, Schraml A. Ergebnisse der Refixation der Osteochondrosis Dissecans des Talus mit Kirschnerdrähten [Results of fixation of osteochondral lesions of the talus using K-wires]. Zentralbl Chir. 2004. Dec;129(6):470-5. doi: 10.1055/s-2004-832393. [DOI] [PubMed] [Google Scholar]
- 135. Schuman L, Struijs PA, van Dijk CN. Arthroscopic treatment for osteochondral defects of the talus. Results at follow-up at 2 to 11 years. J Bone Joint Surg Br. 2002. Apr;84(3):364-8. doi: 10.1302/0301-620x.84b3.11723. [DOI] [PubMed] [Google Scholar]
- 136. Scranton PE, Jr, Frey CC, Feder KS. Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br. 2006. May;88(5):614-9. doi: 10.1302/0301-620x.88b5.17306. [DOI] [PubMed] [Google Scholar]
- 137. Taranow WS, Bisignani GA, Towers JD, Conti SF. Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int. 1999. Aug;20(8):474-80. doi: 10.1177/107110079902000802. [DOI] [PubMed] [Google Scholar]
- 138. Tosun B. Posteromedial approach for osteochondral lesions of the talus. Foot Ankle Int. 2021. Jan;42(1):17-22. doi: 10.1177/1071100720948842. [DOI] [PubMed] [Google Scholar]
- 139. Usuelli FG, D’Ambrosi R, Maccario C, Boga M, de Girolamo L. All-arthroscopic AMIC(®) (AT-AMIC(®)) technique with autologous bone graft for talar osteochondral defects: clinical and radiological results. Knee Surg Sports Traumatol Arthrosc. 2018. Mar;26(3):875-81. doi: 10.1007/s00167-016-4318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Valderrabano V, Miska M, Leumann A, Wiewiorski M. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am J Sports Med. 2013. Mar;41(3):519-27. doi: 10.1177/0363546513476671. [DOI] [PubMed] [Google Scholar]
- 141. van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 2013. Mar 20;95(6):519-25. doi: 10.2106/jbjs.L.00675. [DOI] [PubMed] [Google Scholar]
- 142. Vannini F, Cavallo M, Ramponi L, Castagnini F, Massimi S, Giannini S, et al. Return to sports after bone marrow-derived cell transplantation for osteochondral lesions of the talus. Cartilage. 2017. Jan;8(1):80-7. doi: 10.1177/1947603516642574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Ventura A, Terzaghi C, Legnani C, Borgo E. Treatment of post-traumatic osteochondral lesions of the talus: a four-step approach. Knee Surg Sports Traumatol Arthrosc. 2013. Jun;21(6):1245-50. doi: 10.1007/s00167-012-2028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Volpi P, Bait C, Quaglia A, Redaelli A, Prospero E, Cervellin M, et al. Autologous collagen-induced chondrogenesis technique (ACIC) for the treatment of chondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2014. Jun;22(6):1320-6. doi: 10.1007/s00167-013-2830-3. [DOI] [PubMed] [Google Scholar]
- 145. Walther M, Altenberger S, Kriegelstein S, Volkering C, Röser A. Reconstruction of focal cartilage defects in the talus with miniarthrotomy and collagen matrix. Oper Orthop Traumatol. 2014. Dec;26(6):603-10. doi: 10.1007/s00064-012-0229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Wang C, Kang MW, Kim HN. Arthroscopic treatment of osteochondral lesions of the talus in a suspended position with the patient in a prone position. Foot Ankle Int. 2019. Jul;40(7):811-7. doi: 10.1177/1071100719839697. [DOI] [PubMed] [Google Scholar]
- 147. Whittaker JP, Smith G, Makwana N, Roberts S, Harrison PE, Laing P, et al. Early results of autologous chondrocyte implantation in the talus. J Bone Joint Surg Br. 2005. Feb;87(2):179-83. doi: 10.1302/0301-620x.87b2.15376. [DOI] [PubMed] [Google Scholar]
- 148. Woelfle JV, Reichel H, Javaheripour-Otto K, Nelitz M. Clinical outcome and magnetic resonance imaging after osteochondral autologous transplantation in osteochondritis dissecans of the talus. Foot Ankle Int. 2013. Feb;34(2):173-9. doi: 10.1177/1071100712467433. [DOI] [PubMed] [Google Scholar]
- 149. Yang HY, Lee KB. Arthroscopic microfracture for osteochondral lesions of the talus: second-look arthroscopic and magnetic resonance analysis of cartilage repair tissue outcomes. J Bone Joint Surg Am. 2020. Jan 2;102(1):10-20. doi: 10.2106/jbjs.19.00208. [DOI] [PubMed] [Google Scholar]
- 150. Younger A, Wing K, Penner M, Cresswell M. A study to evaluate the safety of platelet-derived growth factor for treatment of osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2016. Apr;24(4):1250-8. doi: 10.1007/s00167-015-3549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Zhang L, Luo Y, Zhou X, Fu S, Wang G. Outcomes from osteochondral autograft transplant or mosaicplasty in 26 patients with type V osteochondral lesions of the talus. Med Sci Monit. 2021. May 25;27:e930527. doi: 10.12659/msm.930527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Zhu X, Yang L, Duan X. Arthroscopically assisted anterior treatment of symptomatic large talar bone cyst. J Foot Ankle Surg. 2019. Jan;58(1):151-5. doi: 10.1053/j.jfas.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 153. Batista JP, Duarte Pereira HM, van Dijk CN, Del Vecchio JJ. Posterior arthroscopic treatment of ankle osteochondral lesions: technical note. J ISAKOS. 2020;5(2):104-8. doi: 10.1136/jisakos-2019-000375. [DOI] [Google Scholar]
- 154. de l’Escalopier N, Amouyel T, Mainard D, Lopes R, Cordier G, Baudrier N, et al. Long-term outcome for repair of osteochondral lesions of the talus by osteochondral autograft: a series of 56 Mosaicplasties®. Orthop Traumatol Surg Res. 2021. Dec;107(Suppl. 8):103075. doi: 10.1016/j.otsr.2021.103075. [DOI] [PubMed] [Google Scholar]
- 155. Geyer S, Mattes J, Petersen W, Imhoff AB, Achtnich AE. Arthroskopische einzeitige matrixunterstützte Knochenmarkstimulation zur Behandlung osteochondraler Defekte des Talus [Arthroscopic one-step matrix-assisted bone marrow stimulation for the treatment of osteochondral defects of the talus]. Oper Orthop Traumatol. 2022. Aug;34(4):295-302. doi: 10.1007/s00064-021-00737-4. [DOI] [PubMed] [Google Scholar]
- 156. Örs Ç Sarpel Y. Autologous osteochondral transplantation provides successful recovery in patients with simultaneous medial and lateral talus osteochondral lesions. Acta Orthop Traumatol Turc. 2021. Dec;55(6):535-40. doi: 10.5152/j.aott.2021.21204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Richter M, Zech S, Meissner S, Naef I. Autologous matrix induced chondrogenesis plus peripheral blood concentrate (AMIC+PBC) in chondral lesions at the ankle as part of a complex surgical approach—5-year follow-up. Foot Ankle Surg. 2022. Jul 3;28:1321-6. doi: 10.1016/j.fas.2022.06.015. [DOI] [PubMed] [Google Scholar]
- 158. Schafer KA, Cusworth BM, Kazarian GS, Backus JD, Klein SE, Johnson JE, et al. Outcomes following repeat ankle arthroscopy and microfracture for osteochondral lesions of the talus. Foot Ankle Spec. Epub 2022. Mar 6. doi: 10.1177/19386400221079203. [DOI] [PubMed] [Google Scholar]
- 159. Wan DD, Huang H, Hu MZ, Dong QY. Results of the osteochondral autologous transplantation for treatment of osteochondral lesions of the talus with harvesting from the ipsilateral talar articular facets. Int Orthop. 2022. Jul;46(7):1547-55. doi: 10.1007/s00264-022-05380-7. [DOI] [PubMed] [Google Scholar]
- 160. Wang X, Zhang D, Zhang F, Jin L, Shi D, Hou Z. Effect analysis of iliac bone autografting for Hepple V osteochondral lesions of the talus. J Orthop Surg Res. 2022. Jan 15;17(1):33. doi: 10.1186/s13018-022-02924-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Windhofer CM, Orthner E, Bürger HK. Vascularized osteochondral free flaps from the femoral trochlea as versatile procedure for reconstruction of osteochondral lesions of the talus. Foot Ankle Surg. 2022. Jan 14;28:935-43. doi: 10.1016/j.fas.2022.01.002. [DOI] [PubMed] [Google Scholar]
- 162. Yontar NS, Aslan L, Öğüt T. Functional outcomes of autologous matrix-related chondrogenesis to treat large osteochondral lesions of the talus. Foot Ankle Int. 2022. Jun;43(6):783-9. doi: 10.1177/10711007221078021. [DOI] [PubMed] [Google Scholar]
- 163. Ahmad J, Jones K. Comparison of osteochondral autografts and allografts for treatment of recurrent or large talar osteochondral lesions. Foot Ankle Int. 2016. Jan;37(1):40-50. doi: 10.1177/1071100715603191. [DOI] [PubMed] [Google Scholar]
- 164. Allahabadi S, Johnson B, Whitney M, Oji D, Chou L, Lau BC. Short-term outcomes following dehydrated micronized allogenic cartilage versus isolated microfracture for treatment of medial talar osteochondral lesions. Foot Ankle Surg. 2022;28:642-9. doi: 10.1016/j.fas.2021.07.012. [DOI] [PubMed] [Google Scholar]
- 165. Arıcan M, Degirmenci E. Improved clinical outcomes after arthroscopic microfracture in isolated medial talar osteochondral lesions with a single injection of high molecular weight hyaluronic acid. Konuralp Tip Derg. 2019;11:460-7. [Google Scholar]
- 166. Cadossi M, Buda RE, Ramponi L, Sambri A, Natali S, Giannini S. Bone marrow-derived cells and biophysical stimulation for talar osteochondral lesions: a randomized controlled study. Foot Ankle Int. 2014. Oct;35(10):981-7. doi: 10.1177/1071100714539660. [DOI] [PubMed] [Google Scholar]
- 167. Camurcu Y, Ucpunar H, Yapici F, Karakose R, Ozcan S, Cobden A, et al. Clinical and magnetic resonance imaging outcomes of microfracture plus chitosan/blood implant vs microfracture for osteochondral lesions of the talus. Foot Ankle Int. 2020. Nov;41(11):1368-75. doi: 10.1177/1071100720942173. [DOI] [PubMed] [Google Scholar]
- 168. Choi WJ, Choi GW, Kim JS, Lee JW. Prognostic significance of the containment and location of osteochondral lesions of the talus: independent adverse outcomes associated with uncontained lesions of the talar shoulder. Am J Sports Med. 2013. Jan;41(1):126-33. doi: 10.1177/0363546512453302. [DOI] [PubMed] [Google Scholar]
- 169. D’Ambrosi R, Maccario C, Serra N, Liuni F, Usuelli FG. Osteochondral lesions of the talus and autologous matrix-induced chondrogenesis: is age a negative predictor outcome? Arthroscopy. 2017. Feb;33(2):428-35. doi: 10.1016/j.arthro.2016.09.030. [DOI] [PubMed] [Google Scholar]
- 170. Gao F, Chen N, Sun W, Wang B, Shi Z, Cheng L, et al. Combined therapy with shock wave and retrograde bone marrow-derived cell transplantation for osteochondral lesions of the talus. Sci Rep. 2017. May 18;7(1):2106. doi: 10.1038/s41598-017-02378-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006. Oct;22(10):1085-92. doi: 10.1016/j.arthro.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 172. Gül M, Çetinkaya E, Aykut ÜS, Özkul B, Saygılı MS, Akman YE, et al. Effect of the presence of subchondral cysts on treatment results of autologous osteochondral graft transfer in osteochondral lesions of the talus. J Foot Ankle Surg. 2016. Sep-Oct;55(5):1003-6. doi: 10.1053/j.jfas.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 173. Guney A, Yurdakul E, Karaman I, Bilal O, Kafadar IH, Oner M. Medium-term outcomes of mosaicplasty versus arthroscopic microfracture with or without platelet-rich plasma in the treatment of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016. Apr;24(4):1293-8. doi: 10.1007/s00167-015-3834-y. [DOI] [PubMed] [Google Scholar]
- 174. Haasper C, Zelle BA, Knobloch K, Jagodzinski M, Citak M, Lotz J, et al. No mid-term difference in mosaicplasty in previously treated versus previously untreated patients with osteochondral lesions of the talus. Arch Orthop Trauma Surg. 2008. May;128(5):499-504. doi: 10.1007/s00402-007-0513-6. [DOI] [PubMed] [Google Scholar]
- 175. Haleem AM, Ross KA, Smyth NA, Duke GL, Deyer TW, Do HT, et al. Double-plug autologous osteochondral transplantation shows equal functional outcomes compared with single-plug procedures in lesions of the talar dome: a minimum 5-year clinical follow-up. Am J Sports Med. 2014. Aug;42(8):1888-95. doi: 10.1177/0363546514535068. [DOI] [PubMed] [Google Scholar]
- 176. Hannon CP, Ross KA, Murawski CD, Deyer TW, Smyth NA, Hogan MV, et al. Arthroscopic bone marrow stimulation and concentrated bone marrow aspirate for osteochondral lesions of the talus: a case-control study of functional and magnetic resonance observation of cartilage repair tissue outcomes. Arthroscopy. 2016. Feb;32(2):339-47. doi: 10.1016/j.arthro.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 177. Kono M, Takao M, Naito K, Uchio Y, Ochi M. Retrograde drilling for osteochondral lesions of the talar dome. Am J Sports Med. 2006. Sep;34(9):1450-6. doi: 10.1177/0363546506287300. [DOI] [PubMed] [Google Scholar]
- 178. Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Henle P, Niemeyer P. Mosaicplasty with autogenous talar autograft for osteochondral lesions of the talus after failed primary arthroscopic management: a prospective study with a 4-year follow-up. Am J Sports Med. 2006. Jan;34(1):55-63. doi: 10.1177/0363546505278299. [DOI] [PubMed] [Google Scholar]
- 179. Lanham NS, Carroll JJ, Cooper MT, Perumal V, Park JS. A comparison of outcomes of particulated juvenile articular cartilage and bone marrow aspirate concentrate for articular cartilage lesions of the talus. Foot Ankle Spec. 2017. Aug;10(4):315-21. doi: 10.1177/1938640016679697. [DOI] [PubMed] [Google Scholar]
- 180. Lee KB, Park HW, Cho HJ, Seon JK. Comparison of arthroscopic microfracture for osteochondral lesions of the talus with and without subchondral cyst. Am J Sports Med. 2015. Aug;43(8):1951-6. doi: 10.1177/0363546515584755. [DOI] [PubMed] [Google Scholar]
- 181. Lee YK, Young KW, Kim JS, Lee HS, Cho WJ, Kim HN. Arthroscopic microfracture with atelocollagen augmentation for osteochondral lesion of the talus: a multicenter randomized controlled trial. BMC Musculoskelet Disord. 2020. Nov 3;21(1):716. doi: 10.1186/s12891-020-03730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Murphy EP, McGoldrick NP, Curtin M, Kearns SR. A prospective evaluation of bone marrow aspirate concentrate and microfracture in the treatment of osteochondral lesions of the talus. Foot Ankle Surg. 2019. Aug;25(4):441-8. doi: 10.1016/j.fas.2018.02.011. [DOI] [PubMed] [Google Scholar]
- 183. Park HW, Lee KB. Comparison of chondral versus osteochondral lesions of the talus after arthroscopic microfracture. Knee Surg Sports Traumatol Arthrosc. 2015. Mar;23(3):860-7. doi: 10.1007/s00167-014-3061-y. [DOI] [PubMed] [Google Scholar]
- 184. Park KH, Hwang Y, Han SH, Park YJ, Shim DW, Choi WJ, et al. Primary versus secondary osteochondral autograft transplantation for the treatment of large osteochondral lesions of the talus. Am J Sports Med. 2018. May;46(6):1389-96. doi: 10.1177/0363546518758014. [DOI] [PubMed] [Google Scholar]
- 185. Rak Choi Y, Soo Kim B, Kim YM, Park JY, Cho JH, Cho YT, et al. Internal fixation of osteochondral lesion of the talus involving a large bone fragment. Am J Sports Med. 2021. Mar;49(4):1031-9. doi: 10.1177/0363546520988739. [DOI] [PubMed] [Google Scholar]
- 186. Reilingh ML, Lambers KTA, Dahmen J, Opdam KTM, Kerkhoffs G. The subchondral bone healing after fixation of an osteochondral talar defect is superior in comparison with microfracture. Knee Surg Sports Traumatol Arthrosc. 2018. Jul;26(7):2177-82. doi: 10.1007/s00167-017-4654-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Reilingh ML, van Bergen CJ, Gerards RM, van Eekeren IC, de Haan RJ, Sierevelt IN, et al. Effects of pulsed electromagnetic fields on return to sports after arthroscopic debridement and microfracture of osteochondral talar defects: a randomized, double-blind, placebo-controlled, multicenter trial. Am J Sports Med. 2016. May;44(5):1292-300. doi: 10.1177/0363546515626544. [DOI] [PubMed] [Google Scholar]
- 188. Ross AW, Murawski CD, Fraser EJ, Ross KA, Do HT, Deyer TW, et al. Autologous osteochondral transplantation for osteochondral lesions of the talus: does previous bone marrow stimulation negatively affect clinical outcome? Arthroscopy. 2016. Jul;32(7):1377-83. doi: 10.1016/j.arthro.2016.01.036. [DOI] [PubMed] [Google Scholar]
- 189. Sadlik B, Kolodziej L, Puszkarz M, Laprus H, Mojzesz M, Whyte GP. Surgical repair of osteochondral lesions of the talus using biologic inlay osteochondral reconstruction: clinical outcomes after treatment using a medial malleolar osteotomy approach compared to an arthroscopically-assisted approach. Foot Ankle Surg. 2019. Aug;25(4):449-56. doi: 10.1016/j.fas.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 190. Shang XL, Tao HY, Chen SY, Li YX, Hua YH. Clinical and MRI outcomes of HA injection following arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016. Apr;24(4):1243-9. doi: 10.1007/s00167-015-3575-y. [DOI] [PubMed] [Google Scholar]
- 191. Shimozono Y, Hurley ET, Nguyen JT, Deyer TW, Kennedy JG. Allograft compared with autograft in osteochondral transplantation for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2018. Nov 7;100(21):1838-44. doi: 10.2106/jbjs.17.01508. [DOI] [PubMed] [Google Scholar]
- 192. Shimozono Y, Williamson ERC, Mercer NP, Hurley ET, Huang H, Deyer TW, et al. Use of extracellular matrix cartilage allograft may improve infill of the defects in bone marrow stimulation for osteochondral lesions of the talus. Arthroscopy. 2021. Jul;37(7):2262-9. doi: 10.1016/j.arthro.2021.03.032. [DOI] [PubMed] [Google Scholar]
- 193. Shimozono Y, Yasui Y, Hurley ET, Paugh RA, Deyer TW, Kennedy JG. Concentrated bone marrow aspirate may decrease postoperative cyst occurrence rate in autologous osteochondral transplantation for osteochondral lesions of the talus. Arthroscopy. 2019. Jan;35(1):99-105. doi: 10.1016/j.arthro.2018.06.047. [DOI] [PubMed] [Google Scholar]
- 194. Struckmann VF, Harhaus L, Simon R, von Recum J, Woelfl C, Kneser U, et al. Vascularized medial femoral condyle autografts for osteochondral lesions of the talus: a preliminary prospective randomized controlled trial. J Foot Ankle Surg. 2020. Mar-Apr;59(2):307-13. doi: 10.1053/j.jfas.2019.03.025. [DOI] [PubMed] [Google Scholar]
- 195. Tahta M, Akkaya M, Gursoy S, Isik C, Bozkurt M. Arthroscopic treatment of osteochondral lesions of the talus: nanofracture versus hyaluronic acid-based cell-free scaffold with concentration of autologous bone marrow aspirate. J Orthop Surg (Hong Kong). 2017. May-Aug;25(2):2309499017717870. doi: 10.1177/2309499017717870. [DOI] [PubMed] [Google Scholar]
- 196. Takao M, Uchio Y, Kakimaru H, Kumahashi N, Ochi M. Arthroscopic drilling with debridement of remaining cartilage for osteochondral lesions of the talar dome in unstable ankles. Am J Sports Med. 2004. Mar;32(2):332-6. doi: 10.1177/0363546503261718. [DOI] [PubMed] [Google Scholar]
- 197. Yoon HS, Park YJ, Lee M, Choi WJ, Lee JW. Osteochondral autologous transplantation is superior to repeat arthroscopy for the treatment of osteochondral lesions of the talus after failed primary arthroscopic treatment. Am J Sports Med. 2014. Aug;42(8):1896-903. doi: 10.1177/0363546514535186. [DOI] [PubMed] [Google Scholar]
- 198. Yoshimura I, Kanazawa K, Takeyama A, Angthong C, Ida T, Hagio T, et al. Arthroscopic bone marrow stimulation techniques for osteochondral lesions of the talus: prognostic factors for small lesions. Am J Sports Med. 2013. Mar;41(3):528-34. doi: 10.1177/0363546512472979. [DOI] [PubMed] [Google Scholar]
- 199. Danilkowicz RM, Grimm NL, Zhang GX, Lefebvre TA, Lau B, Adams SB, et al. Impact of early weightbearing after ankle arthroscopy and bone marrow stimulation for osteochondral lesions of the talus. Orthop J Sports Med. 2021. Sep;9(9):23259671211029883. doi: 10.1177/23259671211029883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Gianakos AL, Williamson ERC, Mercer N, Kerkhoffs GM, Kennedy JG. Gender differences may exist in the presentation, mechanism of injury and outcomes following bone marrow stimulation for osteochondral lesions of the talus. J Foot Ankle Surg. 2023. Apr 29;62:75-9. doi: 10.1053/j.jfas.2022.04.010. [DOI] [PubMed] [Google Scholar]
- 201. Kim BS, Na Y, Jang DS. Outcomes of bone marrow aspirate concentrate and matrix-induced chondrogenesis (BMIC) for treatment of osteochondral lesions of the talus. Foot Ankle Surg. 2022;28:944-9. doi: 10.1016/j.fas.2022.01.005. [DOI] [PubMed] [Google Scholar]
- 202. Koh DTS, Tan MWP, Zhan X, Li Z, Tay KS, Tan SM, et al. Association of elevated body mass index and outcomes of arthroscopic treatment for osteochondral lesions of the talus. Foot Ankle Orthop. 2022. Apr;7(2):24730114221103263. doi: 10.1177/24730114221103263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Mercer NP, Samsonov AP, Dankert JF, Kennedy JG. Outcomes of autologous osteochondral transplantation with and without extracellular matrix cartilage allograft augmentation for osteochondral lesions of the talus. Am J Sports Med. 2022. Jan;50(1):162-9. doi: 10.1177/03635465211057117. [DOI] [PubMed] [Google Scholar]
- 204. Tan MWP, Tay KS, Yeo EMN. Atelocollagen-induced chondrogenesis versus microfracture alone for osteochondral lesions of the talus: surgical technique and a 1-year clinical outcome study. Foot Ankle Spec. Epub 2022. Jul 11. doi: 10.1177/19386400221107003. [DOI] [PubMed] [Google Scholar]
- 205. Wei Y, Song J, Yun X, Zhang Z, Qi W, Wei M. Outcomes of single-stage versus staged treatment of osteochondral lesions in patients with chronic lateral ankle instability: a prospective randomized study. Orthop J Sports Med. 2022. Feb;10(2):23259671211069909. doi: 10.1177/23259671211069909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Zhao Z, Li J, Yu X, Liu G, Zhao F, Li R. Effect of mosaic allograft osteochondral transplantation combined with corrective osteotomy in treating osteochondral lesions of the talus on ankle and knee joint function and lower limb alignment. Comput Math Methods Med. 2022;2022:9688098. doi: 10.1155/2022/9688098. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 207. Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, et al. Surgical skill and complication rates after bariatric surgery. N Engl J Med. 2013. Oct 10;369(15):1434-42. doi: 10.1056/NEJMsa1300625. [DOI] [PubMed] [Google Scholar]
- 208. Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt). 2017. Aug/Sep;18(6):722-35. doi: 10.1089/sur.2017.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Gasparetto F, Collo G, Pisanu G, Villella D, Drocco L, Cerlon R, et al. Posterior ankle and subtalar arthroscopy: indications, technique, and results. Curr Rev Musculoskelet Med. 2012. Jun;5(2):164-70. doi: 10.1007/s12178-012-9118-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Vega J, Dalmau-Pastor M, Malagelada F, Fargues-Polo B, Peña F. Ankle arthroscopy: an update. J Bone Joint Surg Am. 2017. Aug 16;99(16):1395-407. doi: 10.2106/jbjs.16.00046. [DOI] [PubMed] [Google Scholar]
- 211. Ferkel RD, Heath DD, Guhl JF. Neurological complications of ankle arthroscopy. Arthroscopy. 1996;12(2):200-8. doi: 10.1016/S0749-8063(96)90011-0. [DOI] [PubMed] [Google Scholar]
- 212. Schimmel JJ, Walschot LH, Louwerens JW. Comparison of the short-term results of the first and last 50 Scandinavian total ankle replacements: assessment of the learning curve in a consecutive series. Foot Ankle Int. 2014. Apr;35(4):326-33. doi: 10.1177/1071100713518187. [DOI] [PubMed] [Google Scholar]
- 213. van Bergen CJ, Zengerink M, Blankevoort L, van Sterkenburg MN, van Oldenrijk J, van Dijk CN. Novel metallic implantation technique for osteochondral defects of the medial talar dome. A cadaver study. Acta Orthop. 2010. Aug;81(4):495-502. doi: 10.3109/17453674.2010.492764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. van Bergen CJA, Reilingh ML, van Dijk CN. Novel metal implantation technique for secondary osteochondral defects of the medial talar dome—one-year results of a prospective study. Fuss. 2012;10(2):130-7. doi: 10.1016/j.fuspru.2012.03.004. [DOI] [Google Scholar]
- 215. Stetson WB, Ferkel RD. Ankle arthroscopy: I. Technique and complications. J Am Acad Orthop Surg. 1996. Jan;4(1):17-23. doi: 10.5435/00124635-199601000-00003. [DOI] [PubMed] [Google Scholar]
- 216. Chaytor ER, Conti SF. Arthroscopy of the foot and ankle: current concepts review. Foot Ankle Int. 1998. Mar;19(3):184-92. doi: 10.1177/107110079801900315. [DOI] [PubMed] [Google Scholar]
- 217. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000. Nov;16(8):871-6. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 218. Kelly MP, Lenke LG, Godzik J, Pellise F, Shaffrey CI, Smith JS, et al. Retrospective analysis underestimates neurological deficits in complex spinal deformity surgery: a Scoli-RISK-1 Study. J Neurosurg Spine. 2017. Jul;27(1):68-73. doi: 10.3171/2016.12.Spine161068. [DOI] [PubMed] [Google Scholar]
- 219. Boddapati V, Fu MC, Schairer WW, Ranawat AS, Dines DM, Taylor SA, et al. Increased shoulder arthroscopy time is associated with overnight hospital stay and surgical site infection. Arthroscopy. 2018. Feb;34(2):363-8. doi: 10.1016/j.arthro.2017.08.243. [DOI] [PubMed] [Google Scholar]
- 220. Carvalho RLR, Campos CC, Franco LMC, Rocha AM, Ercole FF. Incidence and risk factors for surgical site infection in general surgeries. Rev Lat Am Enfermagem. 2017;25:e2848. doi: 10.1590/1518-8345.1502.2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Held MB, Boddapati V, Sarpong NO, Cooper HJ, Shah RP, Geller JA. Operative duration and short-term postoperative complications after unicompartmental knee arthroplasty. J Arthroplasty. 2021. Mar;36(3):905-9. doi: 10.1016/j.arth.2020.09.007. [DOI] [PubMed] [Google Scholar]
- 222. Naranje S, Lendway L, Mehle S, Gioe TJ. Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop Relat Res. 2015. Jan;473(1):64-9. doi: 10.1007/s11999-014-3628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J. 2006. Feb;2(1):70-2. doi: 10.1007/s11420-005-0130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Swindell HW, Alrabaa RG, Boddapati V, Trofa DP, Jobin CM, Levine WN. Is surgical duration associated with postoperative complications in primary shoulder arthroplasty? J Shoulder Elbow Surg. 2020. Apr;29(4):807-13. doi: 10.1016/j.jse.2019.08.015. [DOI] [PubMed] [Google Scholar]
- 225. Young SW, Mutu-Grigg J, Frampton CM, Cullen J. Does speed matter? Revision rates and functional outcomes in TKA in relation to duration of surgery. J Arthroplasty. 2014. Jul;29(7):1473-7.e1. doi: 10.1016/j.arth.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 226. Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018. Sep;229:134-44. doi: 10.1016/j.jss.2018.03.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-2-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-3-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-4-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE
Supplemental material, sj-jpg-5-car-10.1177_19476035231154746 for The Frequency and Severity of Complications in Surgical Treatment of Osteochondral Lesions of the Talus: A Systematic Review and Meta-Analysis of 6,962 Lesions by Julian J. Hollander, Jari Dahmen, Kaj S. Emanuel, Sjoerd A.S. Stufkens, John G. Kennedy and Gino M.M.J. Kerkhoffs in CARTILAGE