Abstract
Study Design:
Retrospective cohort study.
Objective:
To determine the prevalence of missed curve progression in patients with adolescent idiopathic scoliosis (AIS) undergoing brace treatment with only in-brace follow-up radiographs, and to provide recommendations on when in-brace and out-of-brace should be obtained during follow-up.
Methods:
133 patients who had documented clinically significant curve progression during brace treatment or only when an out-of-brace radiograph were studied. Of these, 95 patients (71.4%) had curve progression noted on in-brace radiographs while 38 patients (28.6%) showed curve progression only after brace removal. We analyzed differences in age, sex, curve types, Risser stage, months after menarche, standing out-of-brace Cobb angle, correction rate, and flexibility rate between the groups. Multivariate logistic regression was performed to determine factors contributing to curve progression missed during brace treatment.
Results:
There were no differences in initial Cobb angle between out-of-brace and in-brace deterioration groups. However, the correction rate was higher (32.7% vs 25.0%; P = .004) in the in-brace deterioration group as compared to the out-of-brace deterioration group. A lower correction rate was more likely to result in out-of-brace deterioration (OR 0.970; P = .019). For thoracic curves, higher flexibility in the curves was more likely to result in out-of-brace deterioration (OR 1.055; P = .045). For double/triple curves, patients with in-brace deterioration had higher correction rate (OR 0.944; P = .034).
Conclusions:
Patients may develop curve progression despite good correction on in-brace radiographs. Those with higher flexibility and suboptimal brace fitting are at-risk. In-brace and out-of-brace radiographs should be taken alternately for brace treatment follow-up.
Keywords: adolescent idiopathic scoliosis, brace, radiographs, curve progression
Introduction
For adolescent idiopathic scoliosis (AIS), we rely on radiographs obtained at every follow-up to monitor the Cobb angle and alignment, and to determine whether the brace is well-fitted or requires modifications. Two types of radiographs are commonly obtained: out-of-brace and in-brace. Out-of-brace radiographs provide assessment of the actual standing Cobb angle. Any curve progression can be identified using these radiographs through comparison with pre-brace or previous out-of-brace radiographs, which can be used as an indicator of brace adherence or recommendation for surgery if severe progression is noted. However, brace-fitting cannot be assessed with out-of-brace radiographs. In-brace radiographs ensure that the spine is aligned within the brace while assessing whether brace modifications or adjustments are needed for better in-brace correction.
There is no consensus for when in-brace radiographs should be taken. 1 Both types of radiographs should not be obtained at the same setting because of increased radiation exposure. The effect of the brace is also time-dependent, and immediate removal of the brace for an out-of-brace radiograph may not provide adequate information for the actual Cobb angle. Li et al 2 suggested that the brace should be removed for at least 2 hours before out-of-brace radiographs in order to detect possible curve deterioration. Clinically, we observed some patients who, despite having good correction in-brace throughout the brace treatment period, deteriorated once an out-of-brace radiograph is obtained. Hence, this study aims to determine whether patients develop curve progression despite good in-brace correction and to recommend when in-brace and out-of-brace radiographs should be obtained.
Patients and Methods
We retrospectively analyzed patients with AIS who experienced curve progression during their underarm brace (thoracolumbosacral orthosis) treatment. Ethics was approved from the local institutional review board (UW 15-596) and all patients had written informed consent for participation in the study. All patients were followed-up with in-brace radiographs at a single scoliosis referral center. The inclusion criteria were any patients who had documented curve progression (Cobb angle >6°) during the treatment period between 2008 and 2013. The indications for brace treatment were no previous treatment, skeletal immaturity status (Risser stage 0-2), either premenarchal or less than a year post-menarche for females, and standing Cobb angle of 25°-40°. Exclusion criteria included missing data, >1 year postmenarche upon bracing, initial Cobb angle <25° or >40°. Cases were also excluded for curve progression beyond the first follow-up after brace weaning (>7 months after brace weaning) because this could be related to natural history progression. The indication for brace weaning was Risser stage ≥4, no change in body height within 6 months, and 2 years post-menarche for females. 3 After deciding on brace weaning, patients’ next follow-up was approximately 6 months thereafter. These patients gradually weaned their brace over the course of these 6 months. The first 2 months with 8 hours reduction during the day, followed by only night wear in the next 2 months, and finally completely off in the final 2 months. Surgery was indicated for curves >50°.
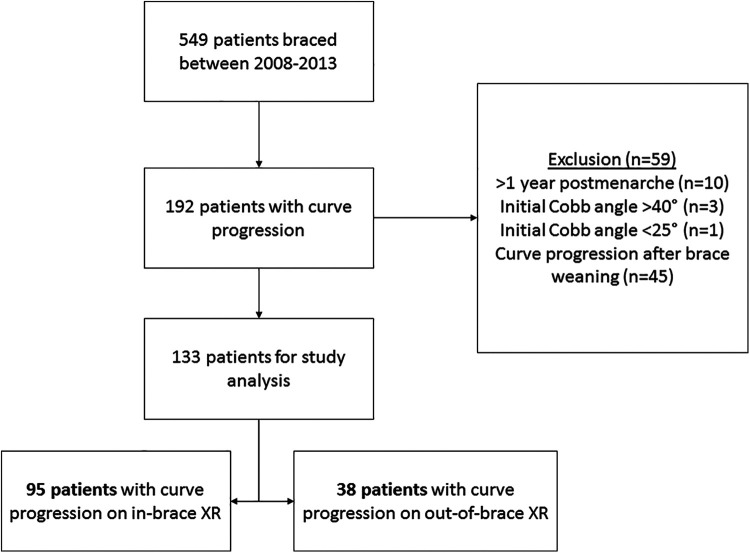
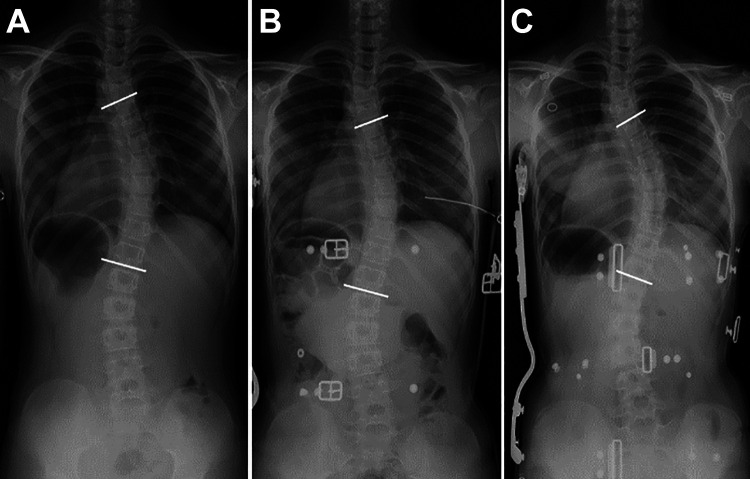
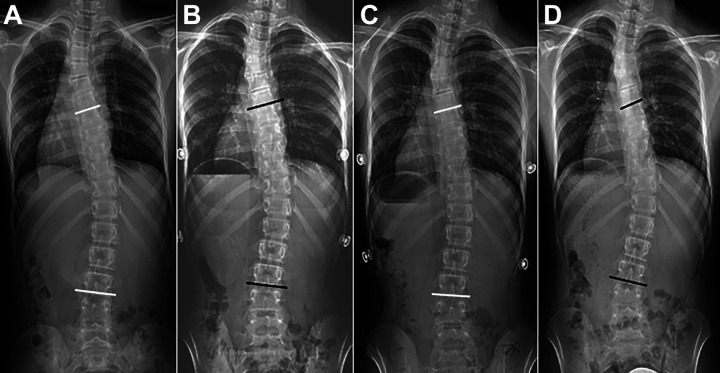
From 549 patients screened in the study period, 192 patients (35.0%) deteriorated despite our protocol for brace treatment (≥16 hours of brace-wearing daily via self-reporting). Of the remaining 133 patients (69.3%) after exclusion (Figure 1), 95 patients (71.4%) had curve progression during brace treatment, with Cobb angle progression noted on in-brace radiographs (Figure 2) while 38 patients (28.6%) showed no deterioration during in-brace assessment, and curve progression was only identified on out-of-brace radiographs (Figure 3). Some patients only had their first out-of-brace radiographs at the next immediate follow-up after brace weaning which was ≤7 months.
Figure 1.
Flowchart of patients included in the study.
Figure 2.
A representative radiograph of a patient with in-brace deterioration (main curve: T5-12) showing the deterioration during brace treatment: (A) Pre-brace standing radiograph Cobb angle of 35°; (B) Initial inbrace radiograph Cobb angle of 29°; and (C) In-brace radiograph showing deterioration to Cobb angle of 44°.
Figure 3.
A representative radiograph of a patient with deterioration only when out-of-brace (main curve: T7-L3) showing deterioration after brace treatment: (A) Pre-brace standing radiograph Cobb angle of 35°; (B) Initial in-brace radiograph Cobb angle of 24°; (C) In-brace radiograph at brace-weaning with Cobb angle of 22.6°; and (D) After-brace treatment standing radiograph showing deterioration to Cobb angle of 42.5°.
Study Parameters
Prior to brace treatment, the pre-brace standing and supine radiographs 4 were studied for baseline major Cobb angle measurement and supine flexibility. 5 Supine radiographs were utilized for assessing spinal flexibility for brace fitting. These images are obtained without patient effort and are thus most reliable. They are also in the identical posture to standing which is the posture patients are in with the brace. They are obtained on the day of brace casting and within 1 month of the pre-brace radiograph. All patients undergo negative casting in the supine position with traction and counter-traction in the long axis of the curve. We utilize a molded cast to manufacture these underarm braces. Patients wear the brace for 2 weeks before the first in-brace radiograph is obtained. Patients are advised for 20 hours of brace-wear per day and followed-up in our clinic every 3-6 months. Thereafter, standing in-brace radiographs immediately after the first brace fitting (initial in-brace radiographs) and standing in-brace radiographs during the course of brace treatment were studied for follow-up Cobb angle measurements. In this population, all patients obtained in-brace radiographs at every visit unless curve progression was noted in the in-brace radiographs, in which case they were asked to return to the clinic for another radiograph with the brace removed for at least 2 hours. 2 Two hours is adequate for accommodating the curves’ viscoelastic properties and is adequate for assessment of the brace fitting after donning the brace and for assessment of the real Cobb angle after doffing the brace. Radiographic parameters included major curve Cobb angles, correction rate, 6 and flexibility rate. 7 The correction rate was (standing Cobb angle—initial in-brace Cobb angle / standing Cobb angle) × 100%, and the flexibility rate was (standing Cobb angle—initial supine Cobb angle / standing Cobb angle) × 100%. 5 , 8 Other parameters included chronological age, sex, major curve type, Risser stage, months after menarche for females, duration of brace treatment, and time from brace initiation to when curve progression was noted.
Statistical Analyses
Data is presented as mean ± standard deviation. Demographics and imaging data were compared between the in-brace and out-of-brace deterioration groups. Normality testing was performed. Baseline characteristics of sex, curve type, Risser staging, menarche status and whether surgery was performed were compared between groups with chi-square test and Fisher’s exact test. The age at bracing, period after menarche, pre-brace Cobb angle, supine Cobb angle, initial in-brace Cobb angle, correction rate, flexibility rate, total number of months braced and duration of bracing before deterioration noted were compared between groups with Mann-Whitney U test.
The curve type was divided into subgroups of thoracic major curves, double/triple curves, and thoracolumbar/lumbar major curves. Between group analyses were performed for whether in-brace or out-of-brace deterioration occurred. Parameters compared included age at bracing, Risser staging, sex, period after menarche, pre-brace Cobb angle, supine Cobb angle, initial in-brace Cobb angle, correction rate, and flexibility rate with Mann-Whitney U test. Associations of parameters with outcome of out-of-brace deterioration between curve types were compared via univariate logistic regression. Those with factors with P < .20 were selected for the multivariate logistic regression model.
Statistical analysis was performed using SPSS Statistics version 25.0 (IBM Corp., Armonk, NY, USA), with P value less than 0.05 were considered statistically significant. Post-hoc power analyses were performed using G*Power. Levene’s tests were also performed to assess whether there was equal variance across groups (confirmed to be via Dunn-Bonferonni tests as listed in the tables) and P-value adjustment using Bonferroni correction. Unequal group size was accounted by z-test assessing column proportions.
Results
Of the 133 patients in the study, 95 patients (71.4%) had in-brace deterioration and 38 patients (28.6%) had out-of-brace deterioration. The Cobb angle outcomes were 50.5 ± 10.3° for the in-brace deterioration group and 45.9 ± 9.2° for the out-of-brace deterioration group (P < .05). There were no differences in sex, curve type, menarche status or whether surgery was performed between the 2 groups (Table 1). There was a slightly larger proportion of Risser stage 2 for the out-of-brace deterioration group (P = .023) but this lacked sufficient power. Higher correction rate was observed in the in-brace deterioration group (32.7% vs 25.0%; P = .004) which reached acceptable power (Table 2). After adjusting for age and sex, the multivariate model (X 2 (5) = 14.076, P = .015, Nagelkerke R 2 = 14.4%, % Predicted correctly by model: 74.4%) observed lower correction rate to be the main significant factor for out-of-brace deterioration (P = .019; OR 0.97 095% CI: 0.946-0.995).
Table 1.
Baseline Characteristics.
| Parameter count (Column %) | In-brace deterioration | Out-of-brace deterioration | P value^ | Power |
|---|---|---|---|---|
| Cases (Count, %) | 95 (71.4) | 38 (28.6) | ||
| Sex | .999 | 0.05 | ||
| Female | 80 (84.2) | 32 (84.2) | ||
| Male | 15 (15.8) | 6 (15.8) | ||
| Curve type | .264 | 0.92 | ||
| Thoracic | 48 (50.5) | 14 (36.8) | ||
| Double/ triple curves | 27 (28.4) | 16 (42.1) | ||
| Thoracolumbar | 20 (21.1) | 8 (21.1) | ||
| Risser stage | 0.023*# | 0.13 | ||
| 0 | 72 (75.8) | 26 (68.4) | ||
| 1 | 19 (20.0) | 5 (13.2) | ||
| 2 | 4 (4.2)□ | 7 (18.4) | ||
| Menarche | .191 | 0.88 | ||
| Pre | 46 (57.5) | 22 (71.0) | ||
| Post | 34 (42.5) | 9 (29.0) | ||
| Operation | .079 | 0.96 | ||
| Yes | 35 | 8 | ||
| No | 60 | 30 | ||
| Bracing success rate | 63.2% | 78.9% |
^Chi-square test unless stated otherwise.
#Fisher’s exact test.
*Statistical significance.
□z-test for independent proportions were run throughout all parameters in the table. Within each row, each possible pair of percentages is compared using a z-test and there was no significant difference at the level of 0.05 level—except for the proportion of Risser stage 2 patients, counts and proportions of in-brace-deterioration group [4.2% (n = 4)] is significantly different from 18.4% (n = 7) of out-of-brace deterioration group.
Table 2.
Comparison of In-Brace and Out-of-Brace Deterioration Groups at Commencement of Bracing and Number of Months Bracing.
| Parameter (Median, mean ± SD) | In-brace deterioration | Out-of-brace deterioration | P value^ | Power |
|---|---|---|---|---|
| Age at bracing (Months) | 144.0 145.8 ± 12.9 |
147.0 148.8 ± 11.7 |
.171 | 0.33 |
| Period after menarche (months) for those post-menarche | 5.5 5.6 ± 3.6 |
4.0 4.9 ± 3.3 |
.620 | 0.24 |
| Pre-brace Cobb angle (°) | 32.0 32.0 ± 4.3 |
31.3 31.5 ± 3.7 |
.603 | 0.12 |
| Supine Cobb angle (°) | 25.6 24.8 ± 6.1 |
25.3 24.9 ± 5.3 |
.962 | 0.05 |
| Initial in-brace Cobb angle (°) | 21.2 21.1 ± 6.3 |
22.9 23.5 ± 6.5 |
.033* | 0.64 |
| Correction rate (%) | 32.7 34.2 ± 16.5 |
25.0 25.3 ± 17.6 |
.004* | 0.89 |
| Flexibility rate (%) | 18.7 22.5 ± 15.2 |
18.9 20.9 ± 13.3 |
.733 | 0.11 |
| Total number of months braced | 22.0 22.3 ± 9.8 |
16.0 16.9 ± 8.4 |
.004* | 0.95 |
| Time starting deterioration since first initiated brace (Months) | 13.0 14.6 ± 8.4 |
20.5 22.0 ± 8.7 |
<.001* | > 0.99 |
^Mann-Whitney U test.
*P < .05.
There were larger pre-brace Cobb angles (P = .004), supine Cobb angles (P < .001), and initial in-brace Cobb angles (P < .001) for thoracic and double/triple curves as compared to thoracolumbar/lumbar curves. Thoracolumbar/lumbar curves have higher correction rates (P < .001) and flexibility rates (P < .001) than thoracic and double/triple curves (Table 3). For thoracolumbar/lumbar curves, patients with in-brace deterioration had smaller initial in-brace Cobb angles (15.4° vs 18.8°; P = .033) and higher correction rates (47.8% vs 33.5%, P = .049) than the out-of-brace deterioration group (Table 4). However, these results lacked sufficient power. After adjusting for other parameters, the higher flexibility rate in the thoracic curve subgroup had 1.055 higher odds (P = .045; 95% CI: 1.001-1.111) of out-of-brace deterioration (Table 5). For double/triple curves, more mature patients (Risser 1; OR 0.046; P = .032; 95% CI: 0.003-0.765) and higher correction rate (OR 0.944; P = .034; 95% CI: 0.894-0.996) was associated with in-brace deterioration (Table 5). The model for thoracolumbar curves did not reach statistical significance (P = .060) and no model had adequate power.
Table 3.
Comparison Between Curve Types for Various Baseline Parameters.
| Parameters Median Mean ± SD | Curve types | Post-hoc analysis# | |||||
|---|---|---|---|---|---|---|---|
| Thoracic | Double/triple | Thoracolumbar | P-value | Pairwise comparison | Mean difference (95% CI) | Adjusted P-value | |
| Number (%) | 62 (46.6) | 43 (32.3) | 28 (21.1) | ||||
| Age at bracing (months)+ | 145.0 146.1 ± 13.2 | 147.0 148.1 ± 12.9 |
146.0 145.5 ± 11.0 |
||||
| Risser stage—count (Column%)# | .174 | ||||||
| 0 | 50 (80.6) | 27 (62.8) | 21 (75.0) | ||||
| 1 | 9 (14.5) | 9 (20.9) | 6 (21.4) | ||||
| 2 | 3 (4.8) | 7 (16.3) | 1 (3.6) | ||||
| Sex—count (%)# | .474 | ||||||
| Males | 9 (14.5) | 9 (20.9) | 3 (10.7) | ||||
| Females | 53 (85.5) | 34 (79.1) | 25 (89.3) | ||||
| Period after menarche (Months)+ for those post-menarche |
4.0 | 6.5 | 5.0 | .166 | |||
| 5.3 ± 3.9 | 6.9 ± 3.1 | 4.3 ± 3.1 | |||||
| Pre-brace Cobb angle (°)+ | 32.6 | 32.4 | 29.3 | .004* | Thoracic vs double/triple | 0.6 (−1.4 to 2.6) | .999 |
| 32.7 ± 4.1 | 32.1 ± 4.2 | 29.7 ± 3.5 | Thoracic vs thoracolumbar | 3.0 (1.0 to 5.0) | .003▴ | ||
| Double/triple vs thoracolumbar | 2.4 (0.2 to 4.5) | .043▴ | |||||
| Supine Cobb angle (°)+ | 26.0 | 26.9 | 18.1 | <.001* | Thoracic vs double/triple | −1.2 (−3.7 to 1.2) | .844 |
| 25.8 ± 5.0 | 27.0 ± 5.4 | 19.6 ± 5.3 | Thoracic vs thoracolumbar | 6.2 (3.3 to 9.0) | <0.001▴ | ||
| Double/triple vs thoracolumbar | 7.4 (4.3 to 10.5) | <.001▴ | |||||
| Initial in-brace Cobb angle (°)+ | 22.4 | 24.3 | 16.4 | <.001* | Thoracic vs double/triple | −3.6 (−6.5 to −0.8) | .058 |
| 21.4 ± 6.2 | 25.0 ± 5.9 | 17.6 ± 4.7 | Thoracic vs thoracolumbar | 3.8 (1.0 to 6.7) | .005▴ | ||
| Double/triple vs thoracolumbar | 7.4 (4.4 to 10.5) | <.001▴ | |||||
| Correction rate (%)+ | 32.2 | 24.0 | 41.2 | <.001* | Thoracic vs double/triple | 12.3 (5.1-19.6) | .003▴ |
| 34.4 ± 17.1 | 22.1 ± 14.1 | 40.3 ± 15.5 | Thoracic vs thoracolumbar | −5.9 (−14.7 to 2.9) | .195 | ||
| Double/triple vs thoracolumbar | −18.3 (−27.1 to −9.5) | <.001▴ | |||||
| Flexibility rate (%)+ | 18.3 | 14.3 | 39.0 | <.001* | Thoracic vs Double/triple | 5.0 (−0.7 to 10.7) | .175 |
| 20.9 ± 12.6 | 16.0 ± 11.6 | 33.8 ± 16.8 | Thoracic vs thoracolumbar | −12.8 (−21.4 to −4.2) | .004▴ | ||
| Double/triple vs thoracolumbar | −17.8 (−26.6 to −9.0) | <.001▴ | |||||
| Operation—count (%)^ | .147 | ||||||
| Yes | 24 | 14 | 5 | ||||
| No | 38 | 29 | 23 | ||||
| Bracing successful rate (%) | 61.3% | 67.4% | 82.1% | ||||
#Fisher’s exact test.
^Chi-square test with z-test of column proportions.
+Kruskal Wallis test.
#By Dunn-Bonferroni post hoc test, accounting for unequal group size with equal variance among groups (As per results of Levene’s tests performed).
▴Adjusted P-value by Bonferroni correction for multiple tests.
*Statistical significance, CI: confidence interval.
Table 4.
Comparison of Baseline Parameters Between In-Brace Deterioration and Out-of-Brace Deterioration Groups.
| Parameters | Outcome | P-value^ | Power | |
|---|---|---|---|---|
| In-brace deterioration | Out-of-brace deterioration | |||
| Thoracic curves (n = 62) | ||||
| Count—n (%) | 48 (77.4) | 14 (22.6) | - | |
| Age at bracing (Months) | 141.0 | 153.0 | .049* | 0.49 |
| 144.9 ± 14.4 | 150.6 ± 6.1 | |||
| Risser stage—count # (%) | .711 | 0.51 | ||
| 0 | 38 (79.2) | 12 (85.7) | ||
| 1 | 8 (16.7) | 1 (7.1) | ||
| 2 | 2 (4.2) | 1 (7.1) | ||
| Sex—count # (%) | .409 | 0.61 | ||
| Males | 6 (12.5) | 3 (21.4) | ||
| Females | 42 (87.5) | 11 (78.6) | ||
| Period after menarche (Months) for those post-menarche |
4.5 | 2.5 | .267 | 0.94 |
| 5.6 ± 4.0 | 2.5 ± 2.1 | |||
| Pre-brace Cobb angle (°) | 32.6 | 32.5 | .705 | 0.06 |
| 32.7 ± 4.4 | 32.4 ± 2.6 | |||
| Supine Cobb angle (°) | 26.2 | 24.9 | .249 | 0.39 |
| 26.2 ± 5.0 | 24.1 ± 4.5 | |||
| Initial in-brace Cobb angle (°) + | 22.3 | 22.7 | .692 | 0.05 |
| 21.4 ± 6.2 | 21.5 ± 6.4 | |||
| Correction rate (%) | 32.5 | 31.8 | .556 | 0.06 |
| 34.8 ± 16.2 | 33.1 ± 20.7 | |||
| Flexibility rate (%) | 17.3 | 21.9 | .132 | 0.45 |
| 19.6 ± 12.3 | 25.7 ± 12.8 | |||
| Double/triple curves (n = 43) | ||||
| Count—n (%) | 27 (62.8) | 16 (37.2) | - | |
| Age at bracing (Months) | 147.0 | 142.5 | .697 | 0.05 |
| 148.1 ± 11.4 | 148.2 ± 15.5 | |||
| Risser stage—count # (%) | .046* | > 0.99 | ||
| 0 | 17 (63.0) | 10 (62.5) | ||
| 1 | 8 (29.6) | 1 (6.3) | ||
| 2 | 2 (7.4) □ | 5 (31.3) | ||
| Sex—count # (%) | .999 | 0.08 | ||
| Males | 6 (22.2) | 3 (18.8) | ||
| Females | 21 (77.8) | 13 (81.3) | ||
| Period after menarche (Months) | 6.5 6.8 ± 3.4 |
7.0 7.0 ± 2.6 |
.945 | 0.06 |
| Pre-brace Cobb angle (°) | 32.4 | 32.3 | .821 | 0.07 |
| 32.2 ± 4.4 | 31.7 ± 4.0 | |||
| Supine Cobb angle (°) | 26.4 | 28.0 | .474 | 0.12 |
| 26.6 ± 5.8 | 27.7 ± 4.9 | |||
| Initial in-brace Cobb angle (°) | 22.8 23.9 ± 5.6 |
25.7 27.0 ± 6.2 |
.102 | 0.47 |
| Correction rate (%) | 29.6 | 14.0 | .019* | 0.79 |
| 25.9 ± 13.9 | 15.6 ± 12.3 | |||
| Flexibility rate (%) | 15.2 | 10.0 | .218 | 0.32 |
| 17.7 ± 12.6 | 13.1 ± 9.4 | |||
| Thoracolumbar curves (n = 28) | ||||
| Count—n (%) | 20 (71.4%) | 8 (28.6%) | - | |
| Age at bracing (Months) | 144.5 | 147.5 | .746 | 0.65 |
| 145.0 ± 11.3 | 146.9 ± 11.1 | |||
| Risser stage—count # (%) | .114 | 0.01 | ||
| 0 | 17 (85.0) | 4 (50.0) | ||
| 1 | 3 (15.0) | 3 (37.5) | ||
| 2 | 0 | 1 (12.5) | ||
| Sex—count # (%) | .536 | 0.10 | ||
| Males | 3 (15.0) | 0 | ||
| Females | 17 (85.0) | 8 (100) | ||
| Period after menarche (Months) | 1.0 | 0 | .374 | 0.19 |
| 2.6 ± 3.2 | 1.4 ± 2.8 | |||
| Pre-brace Cobb angle (°) | 29.8 | 28.7 | .469 | 0.08 |
| 29.9 ± 3.3 | 29.2 ± 4.0 | |||
| Supine Cobb angle (°) | 17.5 | 20.3 | .281 | 0.16 |
| 19.1 ± 5.6 | 20.9 ± 4.5 | |||
| Initial in-brace Cobb angle (°) | 15.4 | 18.8 | .033* | 0.54 |
| 16.6 ± 4.8 | 20.1 ± 3.7 | |||
| Correction rate (%) | 47.8 | 33.5 | .049* | 0.65 |
| 44.1 ± 15.4 | 31.0 ± 12.3 | |||
| Flexibility rate (%) | 40.8 | 28.0 | .237 | 0.24 |
| 35.9 ± 17.7 | 28.4 ± 13.8 | |||
^Mann-Whitney U test unless stated otherwise.
#Fisher’s exact test with z-test (any significant difference between column proportions will be signified by □), n: number, -: not applicable.
*Statistical significance.
Table 5.
Multivariate Logistic Regression Model for the Outcome of Out-of-Brace Deterioration.
| Baseline parameter | Regression coefficient (B) | Wald X2 | P-value | Odds ratio | 95% CI | Power |
|---|---|---|---|---|---|---|
| For thoracic curves | X2(2) = 6.298, P = .043*, Nagelkerke R2 = 0.147, correct prediction = 79.0% | 0.10 | ||||
| Constant | −9.970 | 4.365 | .022* | |||
| Age at bracing (Months) | 0.051 | 3.537 | .060 | 1.052 | 0.998-1.110 | |
| Flexibility rate (%) | 0.053 | 4.010 | .045* | 1.055 | 1.001-1.111 | |
| For double/triple curves | X 2 (3) = 11.625, P = .009, Nagelkerke R 2 = 0.323, correct prediction = 69.8% | 0.10 | ||||
| Constant | 2.181 | 4.041 | .044 | |||
| Risser sign (Reference: Risser 2) | 4.794 | .091 | ||||
| Risser 0 | −1.537 | 2.446 | .118 | 0.215 | 0.031-1.476 | |
| Risser 1 | −3.087 | 4.606 | .032* | 0.046 | 0.003-0.765 | |
| Correction rate (%) | −0.058 | 4.475 | .034* | 0.944 | 0.894-0.996 | |
Abbreviation: CI, confidence interval.
*Significance at P-value < .05.
Discussion
During brace treatment for patients with AIS, radiographs are crucial for assessing brace fitting and curve progression. Although there is no consensus for when in-brace and out-of-brace radiographs should be taken, a consensus statement from the International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) 1 revealed some insight into what radiographs should be obtained, suggesting that in-brace radiographs should be used to ensure proper curve correction. Some clinicians may view brace fitting as the most important factor for brace success and obtain in-brace radiographs at every follow-up, whereas others may only obtain out-of-brace radiographs to check the Cobb angle. Possibly, a balance between in-brace and out-of-brace radiographs is needed since both measure important parameters. 1 Some individuals may opt to undergo both in-brace and out-of-brace radiographs at every visit. However, we need to be vigilant about radiation exposure in children. 9 Furthermore, it has not been determined which radiograph is optimal for early determination of deterioration.
Approximately 70% of patients with curve progression relative to the initial in-brace Cobb angle were identified during brace treatment with in-brace radiographs. While 28.6% (38/133) of patients deteriorated during bracing but was only identified soon after brace weaning when out-of-brace radiographs were obtained. This suggests that only using in-brace radiographs to monitor patients undergoing brace treatment is inadequate. The in-brace radiographs masked the curve deterioration during the brace treatment and may be insufficient to evaluate the curve progression. Although Shi et al 10 reported that 43.5% of patients with AIS deteriorated after brace weaning and of these, deterioration was recognized in the first 6 months in 57% of the patients, the degree of deterioration was reported to be small and not reaching the average 15° observed in our patients. Furthermore, there are no reports indicating whether the patients showing deterioration were identified while the patients were wearing a brace or while being weaned from it. This group of patients poses a possible awkward consultation as parents may associate this deterioration to premature brace weaning despite our use of standardized brace weaning criteria. In addition, there are implications of offering earlier surgical intervention for those who have significant deterioration during brace treatment and can avoid unnecessary brace treatment. Hence, consistent monitoring of the real Cobb angle is warranted even with good in-brace correction.
From the intergroup comparisons, we found that the main determinants of curve deterioration in or out of brace were flexibility and correction rates. With similar initial Cobb angles, patients with higher correction rate equating to the fitting of the brace and Cobb reduction on in-brace radiographs were more likely to experience in-brace deterioration. On the contrary, for thoracic curves, higher flexibility rates were more likely for out-of-brace deterioration. Previous studies reported several factors which related to curve progression despite bracing including younger age, larger initial Cobb angle, and less skeletal maturity.11-13 Males may also fare worse prognosis with bracing. 14
Our findings raise 2 important concepts. Firstly, curve progression is not easily identified in more flexible curves especially in the thoracic spine if only in-brace radiographs are obtained. Without an out-of-brace radiograph, any curve progression may go unnoticed. A larger curve may still be corrected well with the brace due to its high inherent curve flexibility. It is well-established that thoracic curves are at greater risk for brace failure than lumbar curves due to its inherently less flexible nature. 15 Higher flexibility is often linked with good bracing results.4,5 Despite the advantages of flexible curves, it is important to be vigilant during follow-up of these patients to not miss a silent curve progression. A simple out-of-brace radiograph is sufficient. Secondly, a higher or better correction rate was associated with a greater chance for in-brace deterioration. This means that curve progression may also be missed in patients with suboptimal brace fitting. In contrast, patients with closely fit braces, should not miss cases of curve progression even with in-brace radiographs. In-brace deterioration may indicate stiffer curves that are less amenable to correction by the brace despite an initial good in-brace correction. This relationship raises an important role of the orthotist to be in close communication with the clinician and we advise for a 3-monthly orthotist assessment for close monitoring and adjustment of the braces especially during the growth spurt. Despite the likelihood of brace success in flexible curves, the results may be hindered without good brace fabrication and patient fitting. The correction rate is a good measure of the brace fitting and should be matched closely to the pre-brace flexibility measure. 4 It is also a good parameter for determining success in preventing curve progression or even resulting in curve regression. 16 Clinicians should study the similarities of the curve corrected on pre-brace flexibility assessments and in-brace radiographs to determine whether the brace fitting is adequate. Any deviations from the expected correction pre-determined by the flexibility rate should be consulted with the orthotist to improve the fitting.
The average Cobb angle after bracing was larger for the in-brace deterioration group as compared to the out-of-brace deterioration group. These patients reached the threshold of 50° in about half of cases. Although the out-of-brace deterioration group mostly reached the 40° threshold for adult progression, there is a greater likelihood of surgical intervention for the in-brace deterioration group at the end of brace treatment. It is likely that these patients are more prone to rapid progression than other curves. Several features should be analyzed in future study of these rapid deteriorating curves such as the severity of vertebral wedging and rotation which has been shown to increase the likelihood of curve progression. 17 Prognosis even with good brace compliance is likely poor and may require alternative interventions in case the brace fails to control the deformity such as tethering or early fusion surgery. Our in-brace deterioration group experienced curve progression by nearly more than 6 months earlier and was also braced for nearly 6 months longer. Considering ultimately a poor outcome for these individuals, it may not be worthwhile to continue brace treatment. Prolonged brace treatment for these individuals was not effective in preventing the surgical threshold and the ineffective brace period may lead to complications of prolonged immobilization such as reduced muscle and bone mass, and poor mental health.18-22
Some limitations should be acknowledged. Some factors did not reach significant power such as the multivariate model for curve types. It is expected the sample size may not be adequate for a subgroup analysis regarding curve types and should be revisited in a larger scale study. Nevertheless, the main outcome related to the study theme was correction rate which reached adequate power, and our discussion is well supported by this. As this was a retrospective study, we are unable to provide objective data on brace compliance. Self-reported data was provided and is inferior to data from objective measures like pressure or thermal sensors. In addition, other features like 3-dimensional correction by the brace or degree of brace fitting were not studied. For the out-of-brace deterioration group, as patients had in-brace radiographs on the day of weaning decision, we do not have out-of-brace radiographic assessment until the following follow-up less than 7 months later. We cannot verify whether the curve progression occurred within the 7 months between the day of weaning to the follow-up or even if the curve has regressed with brace treatment. 16 Although we used standardized brace weaning criteria with Risser stage ≥4, no change in body height within 6 months, and 2 years post-menarche for females, these criteria has been shown to be flawed. 3 Nevertheless, the mean deterioration was nearly 15°. This figure is too large to be considered a likely result of stopping brace treatment early in this final stage of follow-up with minimal growth remaining and no previous deterioration while in-brace. Hence, the influence of these 7 months on the results is unlikely to be significant.
Based on our findings, we do not recommend both in-brace and out-of-brace radiographs at the same consultation but to obtain these alternately at each subsequent follow-up. Both in and out-of-brace radiographs taken at the same visit is not practical as rebound in the curvature takes at least 2 hours after donning or doffing the brace. 23 Patients will need to wait for 2 additional hours either in or out of the brace to get both radiographs. This poses an increased radiation risk to patients 9 and increased cost both in terms of clinic time for clinicians, and time away from school for patients and time away from work for their caretakers. Alternate in-brace and out-of-brace radiographs at each subsequent follow-up balances the need for assessment of brace fitting and Cobb angles to reduce the likelihood of missing cases with masked curve progression while avoiding increased radiation exposure with additional radiographs. Per annum, we should expect to obtain at least one in-brace and one out-of-brace radiograph considering a 3-6 monthly follow-up. Patients at higher risk of masked curve progression are those with higher curve flexibility and suboptimal brace fitting.
Footnotes
Authors’ Note: Sachiko Kawasaki and Prudence Wing Hang Cheung contributed equally to this article. Ethics approval from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 15-596).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Prudence Wing Hang Cheung, BDSc  https://orcid.org/0000-0002-3213-7373
https://orcid.org/0000-0002-3213-7373
Yuma Suga, MD  https://orcid.org/0000-0003-0029-2464
https://orcid.org/0000-0003-0029-2464
Jason Pui Yin Cheung, MBBS, MMedSc, MS, PDipMDPath, MD, FHKCOS, FHKAM  https://orcid.org/0000-0002-7052-0875
https://orcid.org/0000-0002-7052-0875
References
- 1.Knott P, Pappo E, Cameron M, et al. SOSORT 2012 consensus paper: reducing x-ray exposure in pediatric patients with scoliosis. Scoliosis. 2014;9(4):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li M, Wong MS, Luk KD, Wong KW, Cheung KM. Time-dependent response of scoliotic curvature to orthotic intervention: when should a radiograph be obtained after putting on or taking off a spinal orthosis? Spine (Phila Pa 1976). 2014;39(17):1408–1416. doi:10.1097/BRS.0000000000000423 [DOI] [PubMed] [Google Scholar]
- 3.Cheung JPY, Cheung PWH, Luk KD. When should we wean bracing for adolescent idiopathic scoliosis? Clin Orthop Relat Res. 2019;477(9):2145–2157. doi:10.1097/CORR.0000000000000781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheung JPY, Yiu KKL, Vidyadhara S, Chan PPY, Cheung PWH, Mak KC. Predictability of supine radiographs for determining in-brace correction for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2018;43(14):971–976. doi:10.1097/BRS.0000000000002503 [DOI] [PubMed] [Google Scholar]
- 5.Cheung JPY, Cheung PWH. Supine flexibility predicts curve progression for patients with adolescent idiopathic scoliosis undergoing underarm bracing. Bone Joint J. 2020;102-B(2):254–260. doi:10.1302/0301-620X.102B2.BJJ-2019-0916.R1 [DOI] [PubMed] [Google Scholar]
- 6.Schmid EC, Aubin CE, Moreau A, Sarwark J, Parent S. A novel fusionless vertebral physeal device inducing spinal growth modulation for the correction of spinal deformities. Eur Spine J. 2008;17(10):1329–1335. doi:10.1007/s00586-008-0723-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohrt-Nissen S, Hallager DW, Gehrchen M, Dahl B. Flexibility predicts curve progression in providence nighttime bracing of patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2016;41(22):1724–1730. doi:10.1097/BRS.0000000000001634 [DOI] [PubMed] [Google Scholar]
- 8.Cheung JPY, Chong CHW, Cheung PWH. Underarm bracing for adolescent idiopathic scoliosis leads to flatback deformity: the role of sagittal spinopelvic parameters. Bone Joint J. 2019;101-B(11):1370–1378. doi:10.1302/0301-620X.101B11.BJJ-2019-0515.R1 [DOI] [PubMed] [Google Scholar]
- 9.Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174(1):83–90. doi:10.1667/RR2022.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi B, Guo J, Mao S, et al. Curve progression in adolescent idiopathic scoliosis with a minimum of 2 years’ follow-up after completed brace weaning with reference to the SRS standardized criteria. Spine Deform. 2016;4(3):200–205. doi:10.1016/j.jspd.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 11.Bettany-Saltikov J, Turnbull D, Ng SY, Webb R. Management of spinal deformities and evidence of treatment effectiveness. Open Orthop J. 2017;11:1521–1547. doi:10.2174/1874325001711011521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung JPY, Cheung PWH, Samartzis D, Luk KD. Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res. 2018;476(2):429–436. doi:10.1007/s11999.0000000000000027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y, Yang Y, Dang X, et al. Factors relating to curve progression in female patients with adolescent idiopathic scoliosis treated with a brace. Eur Spine J. 2015;24(2):244–248. doi:10.1007/s00586-014-3674-3 [DOI] [PubMed] [Google Scholar]
- 14.Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2001;26(18):2001–2005. [DOI] [PubMed] [Google Scholar]
- 15.Thompson RM, Hubbard EW, Jo CH, Virostek D, Karol LA. Brace success is related to curve type in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2017;99(11):923–928. doi:10.2106/JBJS.16.01050 [DOI] [PubMed] [Google Scholar]
- 16.Cheung JPY, Cheung PWH, Yeng WC, Chan LCK. Does curve regression occur during underarm bracing in patients with adolescent idiopathic scoliosis? Clin Orthop Relat Res. 2020;478(2):334–345. doi:10.1097/CORR.0000000000000989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nault ML, Mac-Thiong JM, Roy-Beaudry M, et al. Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine (Phila Pa 1976). 2014;39(10):E601–E606. doi:10.1097/BRS.0000000000000284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheung PWH, Wong CKH, Cheung JPY. An insight into the health-related quality of life of adolescent idiopathic scoliosis patients who are braced, observed, and previously braced. Spine (Phila Pa 1976). 2019;44(10):E596–E605. doi:10.1097/BRS.0000000000002918 [DOI] [PubMed] [Google Scholar]
- 19.Vasiliadis E, Grivas TB, Savvidou O, Triantafyllopoulos G. The influence of brace on quality of life of adolescents with idiopathic scoliosis. Stud Health Technol Inform. 2006;123:352–356. [PubMed] [Google Scholar]
- 20.Ugwonali OF, Lomas G, Choe JC, et al. Effect of bracing on the quality of life of adolescents with idiopathic scoliosis. Spine J. 2004;4(3):254–260. doi:10.1016/j.spinee.2003.12.001 [DOI] [PubMed] [Google Scholar]
- 21.Odermatt D, Mathieu PA, Beausejour M, Labelle H, Aubin CE. Electromyography of scoliotic patients treated with a brace. J Orthopaedic Res. 2003;21(5):931–936. doi:10.lOlS/S0736-0266(03)00038-X [DOI] [PubMed] [Google Scholar]
- 22.Noonan KJ, Dolan LA, Jacobson WC, Weinstein SL. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J Pediatr Orthop. 1997;17(6):712–717. [PubMed] [Google Scholar]
- 23.Lenssinck ML, Frijlink AC, Berger MY, Bierman-Zeinstra SM, Verkerk K, Verhagen AP. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther. 2005;85(12):1329–1339. [PubMed] [Google Scholar]