Abstract
Study Design:
Retrospective cohort study.
Objective:
The purpose was to compare rates of postoperative ED visits, readmission, and reoperation between patients with and without preexisting mental illness undergoing outpatient anterior cervical discectomy and fusion (ACDF).
Methods:
A retrospective review of the Mariner Database was conducted on patients who underwent ACDF between 2010 and 2017. Exclusion criteria included same day revision surgery and patients with a history of spine infection, trauma, or neoplasm. Patients were grouped into 3 categories: those with existing history of anxiety and/or depression, those with severe mental illness, and those without any history of mental illness. Severe mental illness was defined as a combination of diagnosis including schizophrenia, bipolar disorder, and/or psychotic disorder. Outcome measures were analyzed by comparing groups using multivariate logistic regression. Significance was set at P < 0.05.
Results:
Patients with anxiety/depression and patients with severe mental illness both had significantly increased risk of ED visits and readmission at 30-day and 90-day intervals. Compared to patients without mental illness, patients with severe mental illness (OR 1.93, P < 0.001) had significantly increased rates of reoperation at 90-days and 1-years postoperatively. Patients with anxiety/depression did not have increased rates of reoperation relative to patients without anxiety/depression at any time interval (P > 0.05).
Conclusion:
Anxiety/depression as well as more severe psychiatric disease such as Schizophrenia and Bipolar disorder were significantly associated with increased healthcare utilization following outpatient ACDF. Patients with preexisting mental illness undergoing outpatient ACDF should be carefully evaluated preoperatively and closely followed postoperatively to reduce risk of adverse events.
Keywords: outpatient, fusion, cervical, depression, mental illness
Introduction
Psychiatric comorbidities have been shown to influence postoperative complications and healthcare utilization following various spine procedures.1-3 With preoperative anxiety and depression being reported in up to a third of patients who undergo spine surgery for back pain, there is clinical value in investigating mental illness as a major driver of postoperative recovery for patients undergoing spine surgery. 4 Preexisting mental illness in surgical patients also carries financial implications, as patients with mental illness have been demonstrated to require increased Medicare bundled payments for various surgeries by at least 13%, compared to patients without mental illness undergoing the same surgeries. 5
In recent years, there has been a trend in performing common spine procedures like anterior cervical discectomy and fusion (ACDF) in the ambulatory setting.6-9 This shift toward outpatient spine surgery is driven by both clinical and financial benefits, as outpatient procedures have been shown to reduce perioperative hospital cost without compromising quality of care.10-12 Since appropriate patient selection is paramount for minimizing risk in outpatient surgery, more comprehensive risk stratification mechanisms for outpatient spine surgery is needed. To this end, several recent studies have examined various preoperative risk factors for complications following outpatient spine procedures such as ACDF and posterior lumbar fusion,2,8 but we are not aware of any which have assessed preexisting psychiatric illness as a predictor of adverse events following ambulatory spine surgery.
Given the increasing prevalence of outpatient spine surgeries, it is important to examine the complication profile of patients with mental illness who undergo outpatient spine surgery. The purpose of this study was to compare rates of postoperative emergency department (ED) visits, readmission, and reoperation in patients undergoing outpatient ACDF with and without preexisting mental illness.
Methods
Data Source
A retrospective database review was performed using the commercially available PearlDiver (PearlDiver Inc., Colorado Springs, Colorado, USA; www.pearldiverinc.com) patient records database. The database contains all Mariner private payer, Medicare, and Medicaid patients records for the years 2011-2017, searchable by International Classification of Diseases (ICD) Ninth and Tenth Edition codes as well as by Current Procedural Terminology (CPT) codes. This study was deemed exempt from institutional review board approval, as all queried data was deidentified and Health Insurance Portability and Accountability Act (HIPAA) compliant.
Study Population
The study population included all patients less than 85 years of age who underwent elective single level ACDF (CPT-22 551, CPT-22 554) between the years of 2011 and 2017. Patients undergoing same day revision, multilevel fusion and those with a history of trauma, infection, or malignancy were excluded from the population using ICD-9-CM and ICD-10-CM diagnosis codes (SDC 1). ICD-9 and ICD-10 codes were used to identify preexisting mental illness diagnoses, including anxiety, depression, bipolar disorder, schizophrenia, and psychotic disorders (SDC 1). Preexisting mental illness was defined as a diagnosis in the year preceding the index of operation. Patients were grouped into 3 categories: those with existing history of anxiety and/or depression, those with severe mental illness, and those with no history of mental illness. Severe mental illness was defined as a combination of any of the following diagnoses including schizophrenia, bipolar disorder, and other psychotic disorders based on prior literature that suggested these disorders predispose patients to greater risk of adverse events following spine surgery.2,13-18
Outcomes Measures
Outcomes of interest included emergency department (ED) visits, readmission, and reoperation at 30-day and 90-day postoperative intervals. Reoperation was also assessed at 1-year intervals. For all outcomes of interest, patients without diagnosis of mental illness were compared with patients with anxiety/depression and those with severe mental illness.
Statistical Analysis
Multivariate logistic regression was used to determine the independent effect of mental illness on the postoperative outcomes, after adjusting for demographic factors and pertinent comorbidities. Odds ratio (OR) and 95% confidence interval (95% CI) were reported for all comparisons. Kaplan-Meier survivorship curves were generated for the outcomes of interest using the log-rank test. R software embedded within the PearlDiver database (R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analysis, with statistical significance was set at P < 0.05 for appropriate tests.
Results
We identified 18 339 patients undergoing outpatient ACDF, of whom 7.9% had anxiety and/or depression diagnosed a year prior to their surgery and 2.8% had severe mental illness diagnosed within a year of their surgery (Table 1). There were more women (56.2% No history, 66.5%, Anxiety-depression, 65.8% Severe) than men in all 3 cohorts and most patients in all 3 cohorts were between the ages of 50 and 64 (Table 1). Detailed patient demographics are shown in Table 1.
Table 1.
Demographics.
| Outpatient ACDF No history N = 16 375 | Outpatient ACDF Anxiety/depression N = 1455 | Outpatient ACDF Severe mental illness N = 509 | |||||
|---|---|---|---|---|---|---|---|
| Age | 18-49 | 6890 | 42.1% | 603 | 41.4% | 227 | 44.6% |
| 50-64 | 7816 | 47.7% | 741 | 50.9% | 250 | 49.1% | |
| 65-79 | 1669 | 10.2% | 111 | 7.6% | 32 | 6.3% | |
| Gender (Female) | 9195 | 56.2% | 967 | 66.5% | 335 | 65.8% | |
| CCI | 0.91 ± 1.49 | 1.15 ± 1.75 | 1.57 ± 1.96 | ||||
| Comorbidities | |||||||
| Obese | 2881 | 17.6% | 431 | 29.6% | 126 | 24.8% | |
| Chronic Kidney Disease | 527 | 3.2% | 64 | 4.4% | 25 | 4.9% | |
| COPD | 1208 | 7.4% | 302 | 20.8% | 81 | 15.9% | |
| Diabetes Mellitus | 3112 | 19.0% | 330 | 22.7% | 130 | 25.5% | |
| Congestive Heart Failure | 445 | 2.7% | 51 | 3.5% | 35 | 6.9% | |
| Coronary Artery Disease | 1904 | 11.6% | 205 | 14.1% | 78 | 15.3% | |
| Hypertension | 7855 | 48.0% | 804 | 55.3% | 290 | 57.0% | |
| Hyperlipidemia | 6951 | 42.2% | 772 | 53.1% | 258 | 50.7% | |
| Substance Use | |||||||
| Tobacco | 4410 | 26.9% | 576 | 39.6% | 255 | 50.1% | |
Abbreviations: CCI, Charlson Comorbidity Index; COPD, Chronic Obstructive Pulmonary Disease.
ED Visits and Readmissions
Compared to patients without mental illness, patients with anxiety/depression or severe mental illness had significantly increased rates of emergency department visits at the 30-day (Anxiety-depression: OR 1.69, CI 1.30-2.19, P-value < 0.001; Severe: OR 1.55, CI 1.19-2.01, P-value < 0.001; Table 2, Figures 1 and 2) and 90-day (Anxiety-depression: OR 1.44, CI 1.24-1.67, P-value < 0.001; Severe: OR 2.08, CI 1.68-2.55, P-value < 0.001; Table 2) postoperative intervals. Compared to patients without mental illness, patients with anxiety/depression or severe mental illness also had significantly increased rates of readmission at the 30-day (Anxiety-depression: OR 1.66, CI 1.24-2.19, P-value < 0.001; Severe: OR 1.92, CI 1.24-2.86, P-value = 0.002; Table 2) and 90-day (Anxiety-depression: OR 1.51, CI 1.20-1.87, P-value < 0.001; Severe: OR 1.94, CI 1.41-2.63, P-value < 0.001; Table 2) postoperative intervals.
Table 2.
Postoperative Outcomes.a
| Outpatient ACDF No history N = 16 375 |
Outpatient ACDF Anxiety/depression N = 1455 |
Outpatient ACDF Severe mental illness N = 509 |
|||
|---|---|---|---|---|---|
| 30 Day | |||||
| ED Visit | 1157 (7.1%) | 157 (10.8%) | *1.69 [1.30-2.19] | 74 (14.5%) | *1.55 [1.19-2.01] |
| Readmission | 430 (2.6%) | 62 (4.3%) | *1.66 [1.24-2.19] | 26 (5.1%) | #1.92 [1.24-2.86] |
| Reoperation | 153 (0.9%) | 13 (0.9%) | 0.73 [0.37-1.31] | - | 1.58 [0.70-3.09] |
| 90 Day | |||||
| ED-Visit | 2026 (12.4%) | 282 (19.4%) | *1.44 [1.24-1.67] | 140 (27.5%) | *2.08 [1.68-2.55] |
| Readmission | 801 (4.9%) | 109 (7.5%) | *1.51 [1.20-1.87] | 49 (9.6%) | *1.94 [1.41-2.63] |
| Reoperation | 206 (1.26%) | 17 (1.17%) | 0.72 [0.40-1.20] | 15 (2.95%) | #2.38 [1.31-3.99] |
| 1 Year | |||||
| Reoperation | 449 (2.7%) | 44 (3.0%) | 0.83 [0.58-1.15] | 30 (5.9%) | *1.93 [1.28-2.81] |
a Groups were compared to patients without history of mental illness, reported as OR [95% CI].
Significance was held at P < 0.05.
Outcomes with <11 patients were not reported (-) to protect patient privacy.
* Denotes P < 0.001, #Denotes P < 0.01, *Denotes P < 0.05.
Figure 1.
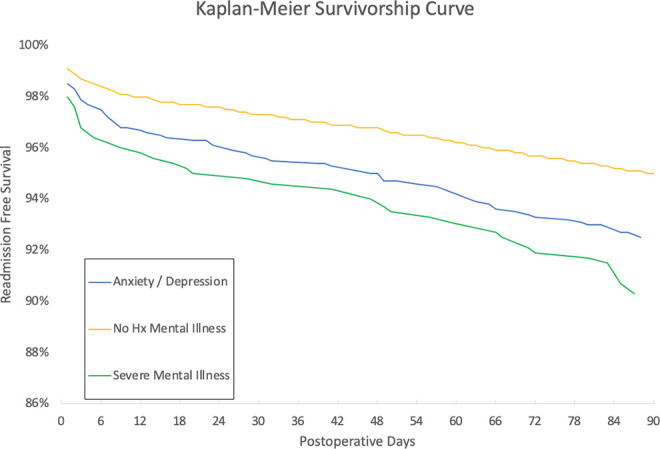
90 day readmission free survival.
Figure 2.
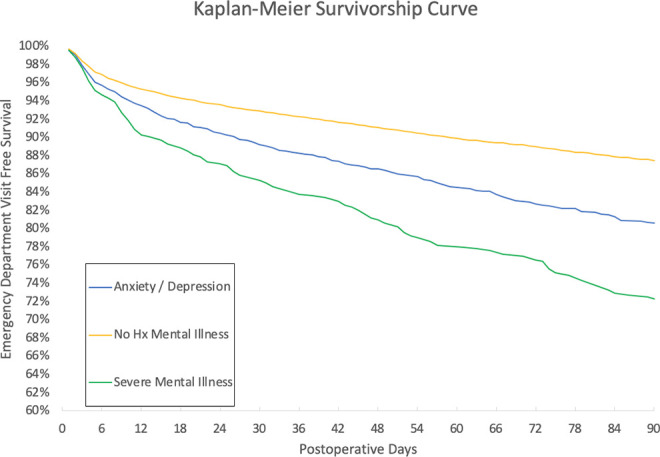
90 day emergency department visit free survival.
Reoperations
The presence of anxiety/depression did not increase risk of reoperation within 1 year of surgery (OR 0.83, CI 0.58-1.15, P-value = 0.274; Table 2, Figure 3). However, the presence of severe mental illness did significantly increase risk of 1 year reoperation (OR 1.93, CI 1.28-2.81, P-value < 0.001; Table 2).
Figure 3.
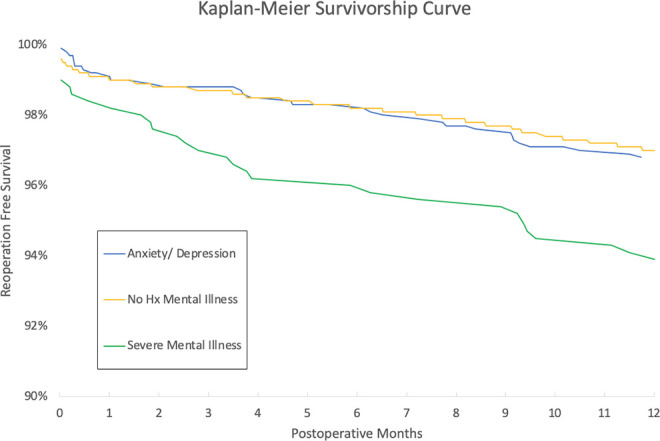
One year reoperation free survival.
Discussion
With a growing trend toward ambulatory spine procedures, understanding the effects of mental illness on patients undergoing outpatient 1-level ACDF is important for surgical decision-making in patients with concomitant psychiatric illness and cervical spine pathology. The present study found increased rates of readmission for patients with anxiety/depression and severe mental illness at the 30-day, and 90-day postoperative intervals, as well as increased rates of ED visits at the 30-day and 90-day postoperative intervals. For patients with severe mental illness, reoperation rates were also higher at the 90-day and 1-year intervals, though this pattern was not seen for patients with anxiety/depression.
For patients suffering from psychiatric conditions who require any type of surgery, both the presence and severity of their mental illness should be important considerations. Within the field of Orthopedic Surgery, depression has been shown to negatively affect postoperative outcomes following total joint arthroplasty, rotator cuff repair, lumbar decompression, ACDF, and several other surgeries.14,18-23 More severe psychiatric disorders, such as Schizophrenia, can further increase risk of medical complications, implant-related complications, and mental status changes following both total hip arthroplasty and total knee arthroplasty.14,19 Even with the clear influence of mental health on surgical outcomes, there is evidence to suggest that anxiety/depression is underreported in orthopedic surgery patients. 24
In spine surgery specifically, mental health has been documented as a risk factor for postoperative complications, adverse outcomes, and increased health utilization following several common procedures, including ACDF and lumbar decompression.2,18 Specifically, Harris et al found patients with anxiety/depression to be at increased risk for multi-day hospitalization, 90-day readmission, revision surgery within 2 years, chronic postoperative opioid use, and increased hospital payments following ACDF. 2 In a single-center retrospective review, Merrill et al found that patients with depression had worse outcomes following lumbar decompression compared to non-depressed patients, in terms of postoperative physical function, depression, pain, and Oswestry Disability Index (ODI). 18 However, depressed patients actually exhibited greater magnitudes of improvement in postoperative outcomes scores relative to preoperative scores compared to non-depressed patients, indicating that spine surgery for appropriately selected patients with mental illness can substantially improve quality of life postoperatively. 18 Jackson et al performed a systematic review to show that patients with psychological disorders are associated with higher rates of spinal pain complaints and worsened functional outcomes following surgery. 25 Although these previous studies were all conducted using data from both inpatient and outpatient procedures, our findings using solely outpatient surgical data are consistent with this prior research, suggesting that patients with mental illness undergoing outpatient ACDF also have increased complications and healthcare utilization relative to patients without mental illness. At present, we are not aware of any other previous studies investigating healthcare utilization following spine surgery specifically in the outpatient setting.
In addition to the presence of a preexisting diagnosis of mental illness, our findings also suggest that severity of psychiatric disease may be an important predictor of adverse events following 1-level ACDF. In our study, patients with severe psychiatric illness—defined as schizophrenia, bipolar disorder, and other psychotic disorders—exhibited significantly increased risks of reoperation within 90-days and 1-year following outpatient ACDF, whereas patients with anxiety/depression did not have increased rates of reoperation at any time interval. Based on these results, it may be important for surgeons to consider not only the presence of psychiatric disease, but also disease severity when determining whether a patient is suitable for outpatient ACDF and which patients might require pretreatment. Adogwa et al and Elsamadicy et al showed that pretreatment of anxiety and depression improves clinical outcomes and patients’ perceptions of postoperative health status.26,27 As such, patients with severe mental illnesses may require preoperative psychiatric evaluation and optimization to improve patient safety.
Although the use of an insurance claims database prevents us from specifying the cause of an ED visit or readmission, pain is likely a primary reason for the increased rate of ED visits and readmissions seen in patients with mental illness undergoing outpatient ACDF. The correlation between anxiety/depression and chronic pain has been well established in prior literature, and spine surgery would only further exacerbate preexisting pain in this patient population.1,28-30 Increased pain in patients with mental illness relative to patients without mental illness is a thus potential explanation of the increased rates of readmission and ED visits found in our study. In outpatient ACDF, pain management should be an important consideration in this patient population to prevent additional healthcare utilization.
The results of our study should be interpreted in the context of a few limitations. First, we did not make a direct comparison between patients with mental illness undergoing inpatient vs. outpatient surgery, so we are unable to draw any conclusions on whether outpatient surgery is safe for this patient population relative to inpatient surgery. However, we contribute to the literature a robust assessment of the risk profile of patients with mental illness undergoing outpatient ACDF, which has not been previously reported. Second, we did not assess preoperative treatment of psychiatric disease, so we are unable to stratify our results by how well a patient’s psychiatric disease was controlled. Even so, our study finds that the presence of medical illness is in itself a risk factor for complications following outpatient ACDF. Finally, as our analysis was performed using an administrative claims database, our study is subject to inaccuracies deriving from coding errors within the database, but previous literature has shown that this occurs less than 1.1%. 31 Despite these limitations, this study adds to the growing literature surrounding outpatient spine surgery to help surgeons evaluate and appropriately choose patients to optimize their safety.
Conclusion
Anxiety/depression as well as more severe psychiatric disease such as Schizophrenia and Bipolar disorder were significantly associated with increased healthcare utilization following outpatient ACDF. Patients with preexisting mental illness undergoing outpatient ACDF should be carefully evaluated preoperatively and closely followed postoperatively to reduce risk of adverse events.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_21925682211026913 for Presence and Severity of Mental Illness Is Associated With Increased Risk of Postoperative Emergency Visits, Readmission, and Reoperation Following Outpatient ACDF: A National Database Analysis by Pramod N. Kamalapathy, Kevin Y. Wang, Varun Puvanesarajah, Micheal Raad and Hamid Hassanzadeh in Global Spine Journal
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hamid Hassanzadeh, MD  https://orcid.org/0000-0002-8224-9517
https://orcid.org/0000-0002-8224-9517
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Strøm J, Bjerrum MB, Nielsen CV, et al. Anxiety and depression in spine surgery—a systematic integrative review. Spine J. 2018;18(7):1272–1285. doi:10.1016/j.spinee.2018.03.017 [DOI] [PubMed] [Google Scholar]
- 2.Harris AB, Marrache M, Puvanesarajah V, et al. Are preoperative depression and anxiety associated with patient-reported outcomes, health care payments, and opioid use after anterior discectomy and fusion? Spine J. 2020;20(8):1167–1175. doi:10.1016/j.spinee.2020.03.004 [DOI] [PubMed] [Google Scholar]
- 3.Menendez ME, Neuhaus V, Bot AGJ, Ring D, Cha TD. Psychiatric disorders and major spine surgery: epidemiology and perioperative outcomes. Spine (Phila Pa 1976). 2014;39(2):E111–E122. doi:10.1097/BRS.0000000000000064 [DOI] [PubMed] [Google Scholar]
- 4.Moore JE. Chronic low back pain and psychosocial issues. Phys Med Rehabil Clin N Am. 2010;21(4):801–815. doi:10.1016/j.pmr.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 5.Courtney PM, Bohl DD, Lau EC, Ong KL, Jacobs JJ, Della Valle CJ. Risk adjustment is necessary in Medicare bundled payment models for total hip and knee arthroplasty. J Arthroplasty. 2018;33(8):2368–2375. doi:10.1016/j.arth.2018.02.095 [DOI] [PubMed] [Google Scholar]
- 6.McClelland S, Passias PG, Errico TJ, Bess RS, Protopsaltis TS. Inpatient versus outpatient anterior cervical discectomy and fusion: a perioperative complication analysis of 259,414 patients from the healthcare cost and utilization project databases. Int J Spine Surg. 2017;11(2):11. doi:10.14444/4011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin CT, D’Oro A, Buser Z, et al. Trends and costs of anterior cervical discectomy and fusion: a comparison of inpatient and outpatient procedures. Iowa Orthop J. 2018;38:167–176. [PMC free article] [PubMed] [Google Scholar]
- 8.Arshi A, Park HY, Blumstein GW, et al. Outpatient posterior lumbar fusion: a population-based analysis of trends and complication rates. Spine (Phila Pa 1976). 2018;43(22):1559–1565. doi:10.1097/BRS.0000000000002664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segal DN, Wilson JM, Staley C, Yoon ST. Outpatient and inpatient single-level cervical total disc replacement: a comparison of 30-day outcomes. Spine (Phila Pa 1976). 2019;44(1):79–83. doi:10.1097/BRS.0000000000002739 [DOI] [PubMed] [Google Scholar]
- 10.Khanna R, Kim RB, Lam SK, Cybulski GR, Smith ZA, Dahdaleh NS. Comparing short-term complications of inpatient versus outpatient single-level anterior cervical discectomy and fusion: an analysis of 6940 patients using the ACS-NSQIP database. Clin Spine Surg. 2018;31(1):43–47. doi:10.1097/BSD.0000000000000499 [DOI] [PubMed] [Google Scholar]
- 11.McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015;39(6):E9. doi:10.3171/2015.9.FOCUS15335 [DOI] [PubMed] [Google Scholar]
- 12.Fu MC, Gruskay JA, Samuel AM, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one- and two-level cases: a propensity-adjusted analysis. Spine (Phila Pa 1976). 2017;42(14):1044–1049. doi:10.1097/BRS.0000000000001988 [DOI] [PubMed] [Google Scholar]
- 13.Kheir MM, Kheir YNP, Tan TL, Ackerman CT, Rondon AJ, Chen AF. Increased complications for schizophrenia and bipolar disorder patients undergoing total joint arthroplasty. J Arthroplasty. 2018;33(5):1462–1466. doi:10.1016/j.arth.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 14.Gholson JJ, Bedard NA, Dowdle SB, Brown TS, Gao Y, Callaghan JJ. Total joint arthroplasty in patients with schizophrenia: how much does it increase the risk of complications? J Arthroplasty. 2018;33(7):2082–2086. doi:10.1016/j.arth.2018.01.074 [DOI] [PubMed] [Google Scholar]
- 15.Poon SH, Sim K, Baldessarini RJ. Pharmacological approaches for treatment-resistant bipolar disorder. Curr Neuropharmacol. 2015;13(5):592–604. doi:10.2174/1570159X13666150630171954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jørgensen CC, Knop J, Nordentoft M, Kehlet H; Lundbeck Foundation Centre for Fast-Track Hip and Knee Replacement Collaborative Group. Psychiatric disorders and psychopharmacologic treatment as risk factors in elective fast-track total hip and knee arthroplasty. Anesthesiology. 2015;123(6):1281–1291. doi:10.1097/ALN.0000000000000632 [DOI] [PubMed] [Google Scholar]
- 17.Paredes AZ, Hyer JM, Diaz A, Tsilimigras DI, Pawlik TM. The impact of mental illness on postoperative outcomes among Medicare beneficiaries: a missed opportunity to help surgical patients? Ann Surg. 2020;272(3):419-425. doi:10.1097/SLA.0000000000004118 [DOI] [PubMed] [Google Scholar]
- 18.Merrill RK, Zebala LP, Peters C, Qureshi SA, McAnany SJ. Impact of depression on patient-reported outcome measures after lumbar spine decompression. Spine (Phila Pa 1976). 2018;43(6):434–439. doi:10.1097/BRS.0000000000002329 [DOI] [PubMed] [Google Scholar]
- 19.Vakharia RM, Sabeh KG, Sodhi N, Mont MA, Roche MW, Hernandez VH. A nationwide analysis on the impact of schizophrenia following primary total knee arthroplasty: a matched-control analysis of 49,176 Medicare patients. J Arthroplasty. 2020;35(2):417–421. doi:10.1016/j.arth.2019.09.034 [DOI] [PubMed] [Google Scholar]
- 20.Werner BC, Wong AC, Chang B, et al. Depression and patient-reported outcomes following total shoulder arthroplasty. J Bone Joint Surg Am. 2017;99(8):688–695. doi:10.2106/JBJS.16.00541 [DOI] [PubMed] [Google Scholar]
- 21.Wilson JM, Farley KX, Erens GA, Bradbury TL, Guild GN. Preoperative depression is associated with increased risk following revision total joint arthroplasty. J Arthroplasty. 2020;35(4):1048–1053. doi:10.1016/j.arth.2019.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gold HT, Slover JD, Joo L, Bosco J, Iorio R, Oh C. Association of depression with 90-day hospital readmission after total joint arthroplasty. J Arthroplasty. 2016;31(11):2385–2388. doi:10.1016/j.arth.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 23.Kuo LT, Chen HM, Yu PA, et al. Depression increases the risk of rotator cuff tear and rotator cuff repair surgery: a nationwide population-based study. PLoS One. 2019;14(11):e0225778. doi:10.1371/journal.pone.0225778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haupt E, Vincent HK, Harris A, et al. Pre-injury depression and anxiety in patients with orthopedic trauma and their treatment. Injury. 2018;49(6):1079–1084. doi:10.1016/j.injury.2018.03.024 [DOI] [PubMed] [Google Scholar]
- 25.Jackson KL, Rumley J, Griffith M, Agochukwu U, DeVine J. Correlating psychological comorbidities and outcomes after spine surgery. Global Spine J. 2020;10(7):929–939. doi:10.1177/2192568219886595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adogwa O, Elsamadicy AA, Cheng J, Bagley C.Pretreatment of anxiety before cervical spine surgery improves clinical outcomes: a prospective, single-institution experience. World Neurosurg. 2016;88:625–630. doi:10.1016/j.wneu.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 27.Elsamadicy AA, Adogwa O, Cheng J, Bagley C.Pretreatment of depression before cervical spine surgery improves patients’ perception of postoperative health status: a retrospective, single institutional experience. World Neurosurg. 2016;87:214–219. doi:10.1016/j.wneu.2015.11.067 [DOI] [PubMed] [Google Scholar]
- 28.Michaelides A, Zis P. Depression, anxiety and acute pain: links and management challenges. Postgrad Med. 2019;131(7):438–444. doi:10.1080/00325481.2019.1663705 [DOI] [PubMed] [Google Scholar]
- 29.IsHak WW, Wen RY, Naghdechi L, et al. Pain and depression: a systematic review. Harv Rev Psychiatry. 2018;26(6):352–363. doi:10.1097/HRP.0000000000000198 [DOI] [PubMed] [Google Scholar]
- 30.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi:10.1001/archinte.163.20.2433 [DOI] [PubMed] [Google Scholar]
- 31.Centers for Medicare & Medicaid Services (CMS). Executive summary. The Medicare Fee-For-Service Improper Payments Report. Medicare Fee-For-Service 2016 Improper Payments Report. CMS; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_21925682211026913 for Presence and Severity of Mental Illness Is Associated With Increased Risk of Postoperative Emergency Visits, Readmission, and Reoperation Following Outpatient ACDF: A National Database Analysis by Pramod N. Kamalapathy, Kevin Y. Wang, Varun Puvanesarajah, Micheal Raad and Hamid Hassanzadeh in Global Spine Journal


