Abstract
Epilepsy, a severe neurological disorder impacting approximately 50 million individuals worldwide, is associated with a high prevalence of mental health issues. However, existing research has predominantly examined the relationship between epilepsy and depression or anxiety, neglecting other dimensions of mental health as assessed by factor scores from the general health survey (GHQ), such as the GHQ-12. This study aimed to explore how epilepsy affects both general mental health and specific dimensions of mental health. By employing a factor analysis and a predictive normative modeling approach, the study examined 426 epilepsy patients and 39,171 individuals without epilepsy. The findings revealed that epilepsy patients experienced poorer general mental health and specific aspects of mental health. Consequently, this study highlights the validity of GHQ-12 as a measure of mental health problems in epilepsy patients and emphasizes the importance of considering the impact of epilepsy on various dimensions of mental health, rather than focusing solely on depression or anxiety. Clinicians should incorporate these study results into the development of interventions aimed at enhancing mental well-being in epilepsy patients, ultimately leading to improved outcomes.
Keywords: epilepsy, mental health, GHQ-12
1. Introduction
Epilepsy is a serious neurological condition that affects around 50 million people around the world [1,2]. The incidence range is between 40 and 70 per 100 thousand people per year in high-income countries, with a higher prevalence in children and older adults [3]. Moreover, the incidence rate is even higher in low-income countries, with more than 120 per 100 thousand people per year [4,5]. Nevertheless, in high-income countries, there appears to be a greater occurrence of epilepsy among poor people [4]. The World Health Organization (WHO) states that epilepsy contributes to approximately 0.5 percent of the total annual expenses for all illnesses globally [6]. In the United Kingdom, there are approximately 600,000 people suffering from epilepsy [7].
People with epilepsy have high rates of mental health issues [8], with around 20% of patients experiencing depression or anxiety symptoms, which can lead to adverse outcomes, such as decreased life quality [9,10,11,12,13,14] and poor medical adherence [15,16]. Screening for mental health conditions in epilepsy patients can benefit them from behavioral and/or pharmacological interventions [17,18,19,20,21].
Among mental health issues in epilepsy patients, previous studies extensively focused on depression and anxiety. For instance, a recent meta-analysis of population-based studies found that there is an overall pooled prevalence of 23.1% for depression in epilepsy patients with a significantly increased likelihood of depression in people with epilepsy compared to controls [22]. Additionally, studies on epilepsy patients have also found that co-occurring depression and anxiety disorders are more common in people with epilepsy as compared to the general population [23]. Compared to depression, anxiety is typically seen as the “neglected” psychiatric comorbidity in people with epilepsy [24,25]. Despite the fact that depressive disorders are agreed to be a more common psychiatric comorbidity, recent studies have found that the prevalence of anxiety disorders is comparable to depressive disorders [26] or may even exceed the prevalence of depressive disorders [27]. However, the prevalence of anxiety disorders varies in people with epilepsy, with some recent research estimates from as low as 4.3% [28] to as high as 52.1% [29]. One of the most recent meta-analyses found that the pooled prevalence is 22.9% for depression and 20.2% for anxiety, respectively, in people with epilepsy [30].
The 12-item version of the general health questionnaire (GHQ-12) is a self-administered questionnaire consisting of 12 items, each assessed using a Likert scale. Extensive research in the field has examined the psychometric properties of this questionnaire and has demonstrated its reliability, sensitivity, and specificity as a valid measure of mental health [31,32,33,34,35,36,37,38]. However, there is a debate regarding whether the GHQ-12 should be utilized as a unidimensional scale or as a multidimensional structure. Many studies have provided substantial empirical support for a 3-factor model of the GHQ-12 [39,40,41,42,43,44,45]. This model includes three factors: GHQ-12A, which assesses social dysfunction and anhedonia (6 items); GHQ-12B, which evaluates depression and anxiety (4 items); and GHQ-12C, which measures loss of confidence (2 items). Some proponents of the unidimensional approach argue that the high correlation observed between these factors [31] supports the use of a single overall score. However, recent research utilizing simulated data have demonstrated that imposing a simple structure may artificially inflate correlations between the modeled factors [46]. Therefore, relying solely on these high correlations to establish unidimensionality may result in a self-fulfilling prophecy of oversimplification (i.e., simply using high correlations between factors as justification for using a one-factor solution). Thus, the present study considers both the unitary scale and the 3-factor solution of the GHQ-12.
Previous research has primarily examined the relationship between epilepsy and mental health, specifically focusing on depression and anxiety; however, much less is known about how epilepsy is related to general and dimensions of mental health. The objective is to explore how epilepsy impacts overall mental health and its various dimensions. There are two main hypotheses: First, there are three factors in the GHQ-12 scale, including GHQ-12A, GHQ-12B, and GHQ-12C. Second, the study anticipates that individuals with epilepsy will experience poorer general mental health and various aspects of mental health.
2. Methods
2.1. Data
This research utilized data from Understanding Society: the United Kingdom Household Longitudinal Study (UKHLS), a study that has been gathering yearly data from a representative sample of UK households since 1991, previously known as The British Household Panel Study (BHPS). The data analyzed in this study were obtained from Wave 1, conducted from 2009 to 2010 [47]. Among the participants included in the analysis after removing missing values, 426 individuals reported having epilepsy, while 39,597 participants reported not being clinically diagnosed with epilepsy. Detailed descriptive statistics can be found in Table 1.
Table 1.
The demographic characteristics of the studied sample. The demographic characteristics of these groups of participants are similar.
| Healthy Controls | Epilepsy Patients | |||
|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | |
| Age | 45.85 (15–99) | 17.99 | 43.31 (16–84) | 15.84 |
| Monthly net income | 1248.77 | 1351.45 | 1046.10 | 835.41 |
| N | % | N | % | |
| Sex | ||||
| Male | 21,974 | 56.10 | 178 | 41.78 |
| Female | 17,197 | 43.90 | 248 | 58.22 |
| Highest educational qualification | ||||
| College | 11,296 | 28.84 | 83 | 19.48 |
| Below college | 27,875 | 71.16 | 27,875 | 80.52 |
| Legal marital status | ||||
| Single | 19,171 | 48.94 | 238 | 55.87 |
| Married | 20,000 | 51.06 | 188 | 44.13 |
| Residence | ||||
| Urban | 30,597 | 78.11 | 326 | 76.53 |
| Rural | 8574 | 21.89 | 100 | 23.47 |
2.2. Measures
2.2.1. Epilepsy
Utilizing self-reported epilepsy proves to be a reliable method for identifying epilepsy (e.g., [48]). Participants were asked whether a doctor or other health professional had ever diagnosed them with epilepsy, and they responded with a simple “Yes” or “No” to indicate their condition.
2.2.2. Mental Health
Mental health was assessed using the GHQ-12, a 12-item questionnaire often used to screen for general (non-psychiatric) mental health problems in primary care settings. The Likert method of scoring was employed, with response options ranging from 0 (“Not at all”) to 3 (“Much more than usual”) [49]. To capture overall mental health, a summary score was calculated by summing the responses across all 12 items. A higher score indicated poorer mental health. However, for the factor analysis conducted in this study, the GHQ-12 items were scored on a scale of 1 (“Not at all”) to 4 (“Much more than usual”) before the factor analysis.
2.2.3. Demographic Controls
Demographic controls in the model include age, sex, monthly net income, highest educational qualification, legal marital status, and residence.
2.3. Analysis
2.3.1. Factor Model
A factor analysis was conducted using MATLAB 2018a software to examine the factor structure of the GHQ-12 questionnaire in this study, which is a statistical technique used in research and data analysis to test and validate the underlying structure of a set of observed variables. The analysis involved an oblique rotation technique with a pre-specified factor 3. The GHQ-12 questionnaire was expected to have three factors: GHQ-12A, GHQ-12B, and GHQ-12C. A higher score indicates a greater presence of mental health issues.
2.3.2. Linear Model
Initially, four general linear models were trained using demographic variables from health controls as predictors and GHQ-12, GHQ-12A, GHQ-12B, and GHQ-12C as the variables to be predicted. Residuals from these models were normally distributed. In the next stage, the four trained models were applied to data from individuals diagnosed with epilepsy in order to estimate the scores they would have obtained if they did not have epilepsy. Lastly, one-sample t-tests were conducted to compare the actual scores of participants with epilepsy to the predicted scores.
3. Results
Consistent with previous studies, the three factors obtained from the factor analysis (chi-squared = 2344.61, p < 0.001) included GHQ-12A (social dysfunction and anhedonia; 6 items), GHQ-12B (depression and anxiety; 4 items), and GHQ-12C (loss of confidence; 2 items). The loadings of these items can be found in Table 2.
Table 2.
The factor loadings for the three-factor structure of the GHQ-12. Bold values represent that the item in that row loads the heaviest on the corresponding factor in the column.
| GHQ-12 Items | GHQ-12A (Social Dysfunction and Anhedonia; 6 Items) | GHQ-12B (Depression and Anxiety; 4 Items) | GHQ-12C (Loss of Confidence; 2 Items) |
|---|---|---|---|
| Concentration | 0.57 | 0.19 | −0.11 |
| Loss of sleep | 0.01 | 0.68 | 0.012 |
| Playing a useful role | 0.61 | −0.17 | 0.13 |
| Constantly under strain | 0.74 | −0.13 | −0.02 |
| Problem overcoming difficulties | −0.03 | 0.86 | −0.08 |
| Unhappy or depressed | 0.08 | 0.50 | 0.20 |
| Losing confidence | 0.57 | 0.23 | −0.12 |
| Believe worthless | 0.69 | −0.05 | 0.04 |
| General happiness | 0.01 | 0.53 | 0.34 |
| Capable of making decisions | 0.01 | 0.17 | 0.72 |
| Ability to face problems | 0.10 | −0.01 | 0.73 |
| Enjoy day-to-day activities | 0.49 | 0.12 | 0.12 |
Training general linear models on healthy controls revealed a main effect of age (F(1, 39,164) = 14.59, p < 0.001), sex (F(1, 39,164) = 245.89, p < 0.001), monthly income (F(1, 39,164) = 23.21, p < 0.001), highest educational qualification (F(1, 39,164) = 22.08, p < 0.001), legal marital status (F(1, 39,164) = 23.21, p < 0.001), and residence (F(1, 39164) = 35.39, p < 0.001) on GHQ-12 summary score. Similarly, there was a main effect of age (F(1, 39,164) = 562.28, p < 0.001), sex (F(1, 39,164) = 105.25, p < 0.001), monthly income (F(1, 39,164) = 23.58, p < 0.001), highest educational qualification (F(1, 39,164) = 82.68, p < 0.001), legal marital status (F(1, 39,164) = 23.21, p < 0.001), and residence (F(1, 39,164) = 9.87, p < 0.01) on GHQ-12A (social dysfunction and anhedonia). Moreover, there was a main effect of age (F(1, 39,164) = 147.07, p < 0.001), sex (F(1, 39,164) = 257.62, p < 0.001), legal marital status (F(1, 39,164) = 40.92, p < 0.001), and residence (F(1, 39,164) = 47.5, p < 0.001) on GHQ-12B (depression and anxiety). However, the main effect of monthly income and highest educational qualification was not significant. Finally, there was a main effect of sex (F(1, 39,164) = 152.03, p < 0.001), monthly income (F(1, 39,164) = 108.89, p < 0.001), highest educational qualification (F(1, 39,164) = 55.20, p < 0.001), legal marital status (F(1, 39,164) = 234.8, p < 0.001), and residence (F(1, 39,164) = 14.21, p < 0.001) on GHQ-12C (loss of confidence). However, the main effect of age was not significant.
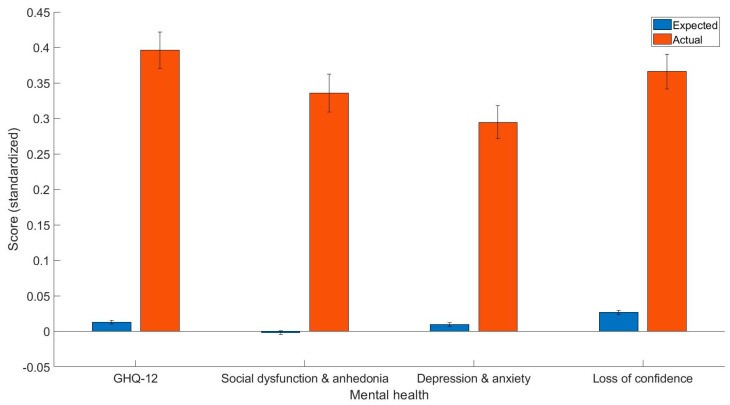
Most importantly, the current study found that epilepsy patients have worse overall mental health as indicated by the GHQ-12 summary score (t(425) = 6.63, p < 0.001, Cohen’s d = 0.38, 95% C.I. [0.27, 0.50]), GHQ-12A (t(425) = 5.62, p < 0.001, Cohen’s d = 0.34, 95% C.I. [0.22, 0.46]), GHQ-12B (t(425) = 5.41, p < 0.001, Cohen’s d = 0.29, 95% C.I. [0.18, 0.39]), GHQ-12C (t(425) = 6.12, p < 0.001, Cohen’s d = 0.34, 95% C.I. [0.23, 0.45]). The mean and standard error of predicted and actual standardized scores can be found in Figure 1.
Figure 1.
The expected and predicted GHQ-12 summary scores, GHQ-12A (social dysfunction and anhedonia), GHQ-12B (depression and anxiety), and GHQ-12C (loss of confidence). Y axis = standardized scores.
4. Discussion
The primary objective of this study was to examine and contrast the disparities in overall mental well-being and specific aspects of mental health between individuals diagnosed with epilepsy and those without epilepsy. To achieve this, a predictive normative modeling approach was employed, which effectively controlled for demographic variables. The main findings were that epilepsy patients are characterized by more general health issues, social dysfunction, and anhedonia as well as depression and anxiety and loss of confidence.
In this study, the factor analysis resulted in the identification of three factors, namely GHQ-12A, GHQ-12B, and GHQ-12C. This three-factor structure observed in our study aligns closely with previous research that also identified three factors within the GHQ-12 measure [39,40,41,42,43,44,45]. Furthermore, as indicated in Table 2, the factor loadings obtained in our study were notably high.
Importantly, the main findings in the current study were that epilepsy patients have poorer general mental health when compared to the scores that would be expected given their demographics, which is largely consistent with the literature regarding the general mental health problems in epilepsy patients [23,50,51,52,53]. The finding that epilepsy patients have social dysfunction and anhedonia problems is also consistent with previous studies that found that epilepsy is related to anhedonia via pathophysiological pathways [54,55,56] and in adolescents [57]. Moreover, the finding that epilepsy patients have worse depression and anxiety problems is largely consistent with previous research [23,24,25,26,27,28,29,30]. Finally, the finding regarding loss of confidence is quite novel, although previous studies have only looked at the confidence of epilepsy knowledge [58,59] and management [60].
There are several possible pathophysiological pathways that can possibly explain the association between epilepsy and mental health [61]. Particularly, the amygdala plays an important role in this relationship because it is part of the corticolimbic circuit for producing fear and anxiety symptoms [62]. In patients with temporal lobe epilepsy, ictal fear is typically associated with epileptic discharges from the mesial temporal lobe area [10]. Evidence from magnetic resonance imaging has also found the link between amygdala atrophy and seizure focus on people with ictal fear [63]. Studies on mouse models of temporal lobe epilepsy also revealed an anhedonic phenotype and inhibiting the glutamine synthetase in the central nucleus of the amygdala induces anhedonic behavior and recurrent seizures [55]. Furthermore, there is a suggestion that the neurotransmitter gamma-aminobutyric acid (GABA) might be involved in both epilepsy and depression and anxiety. This connection is demonstrated by the shared properties of GABAergic antiepileptic drugs, which exhibit both anticonvulsant effects and anxiolytic properties [64]. Consequently, GABA could have a significant role in the underlying mechanisms of epilepsy, depression, and anxiety.
The results from the current study suggest that mental health problems can represent a complicating clinical factor in improving the health of epilepsy patients. Comorbid mental health problems can cause adverse clinical outcomes, which may in turn translate to higher health care use and cost. Patients with mental health problems are more likely to encounter epilepsy-specific hospitalizations, epilepsy-specific ED visits, and epilepsy-specific outpatient visits, which may indicate that comorbid psychiatric conditions may be a contributing factor to epilepsy. As a result, the identification and management of epilepsy patients with mental health are important. Comorbid mental health problems can sometimes be overlooked, particularly when they are less severe (i.e., do not cause marked disability). Furthermore, if epilepsy patients with mental health issues go undetected and untreated, it can lead to consequences specific to epilepsy and psychiatric conditions [21]. These outcomes may arise due to neurologists’ lack of awareness regarding suitable screening tools and effective medications for treating mental health conditions. To address this, a more comprehensive approach to care is recommended, involving a multidisciplinary team within epilepsy clinics [8,21].
While this study possesses notable strengths, there are several limitations that need to be acknowledged. First, the reliance on self-reported measures in this study introduces the possibility of self-reporting bias. To address this concern, future research should incorporate more objective measures, such as clinical assessments. Second, the cross-sectional design employed in this study is inadequate for establishing causality, particularly considering the bidirectional association between epilepsy and mental health (e.g., [65]). Therefore, it is recommended that future longitudinal investigations be conducted to further explore the bi-directional association between epilepsy and mental health. Finally, the focus of this study was limited to individuals with epilepsy within the United Kingdom, thus potentially restricting the generalizability of the findings to people living in other countries.
5. Conclusions
Taken together, the current study found that both general mental health and the dimensions of mental health are negatively affected by epilepsy. This study implies that there is a need to consider how dimensions of mental health are affected by epilepsy rather than solely focusing on depression or anxiety problems in patients with epilepsy. Factors with the GHQ-12 may indicate sub-areas for interventions. Clinicians should utilize findings from the current study to develop interventions that improve mental health in epilepsy patients, which can then lead to better outcomes.
Institutional Review Board Statement
Ethics approval was received from the University of Essex Ethics Committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Publicly available datasets were analyzed in this study. These data can be found here: https://www.understandingsociety.ac.uk.
Conflicts of Interest
The author declares no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.de Boer H.M., Mula M., Sander J.W. The global burden and stigma of epilepsy. Epilepsy Behav. 2008;12:540–546. doi: 10.1016/j.yebeh.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Epilepsy: A Public Health Imperative. WHO; 2019. [(accessed on 1 July 2022)]. Available online: http://www.who.int/mental_health/neurology/epilepsy/report_2019/en/ [Google Scholar]
- 3.MacDonald B.K., Cockerell O.C., Sander J.W., Shorvon S.D. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain. 2000;123:665–676. doi: 10.1093/brain/123.4.665. [DOI] [PubMed] [Google Scholar]
- 4.Ngugi A.K., Kariuki S.M., Bottomley C., Kleinschmidt I., Sander J.W., Newton C.R. Incidence of epilepsy: A systematic review and meta-analysis. Neurology. 2011;77:1005–1012. doi: 10.1212/WNL.0b013e31822cfc90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ngugi A.K., Bottomley C., Kleinschmidt I., Wagner R.G., Kakooza-Mwesige A., Ae-Ngibise K., Newton C.R. Prevalence of active convulsive epilepsy in sub-Saharan Africa and associated risk factors: Cross-sectional and case-control studies. Lancet Neurol. 2013;12:253–263. doi: 10.1016/S1474-4422(13)70003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mula M., Kaufman K.R. Double stigma in mental health: Epilepsy and mental illness. BJPsych Open. 2020;6:e72. doi: 10.1192/bjo.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epilepsy Action About Epilepsy. 2018. [(accessed on 9 July 2020)]. Available online: https://www.epilepsy.org.uk/info/about.
- 8.Petrilla A.A., Sutton B.S., Leinwand B.I., Parente A., Ferrari L., Wade C.T. Incremental burden of mental health conditions in adult patients with focal seizures. Epilepsy Behav. 2020;112:107426. doi: 10.1016/j.yebeh.2020.107426. [DOI] [PubMed] [Google Scholar]
- 9.Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 10.Pham T., Sauro K.M., Patten S.B., Wiebe S., Fiest K.M., Bulloch A.G.M., Jetté N. The prevalence of anxiety and associated factors in persons with epilepsy. Epilepsia. 2017;58:e107. doi: 10.1111/epi.13817. [DOI] [PubMed] [Google Scholar]
- 11.Baca C.B., Vickrey B.G., Caplan R., Vassar S.D., Berg A.T. Psychiatric and medical comorbidity and quality of life outcomes in childhood-onset epilepsy. Pediatrics. 2011;128:e1532–e1543. doi: 10.1542/peds.2011-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gur-Ozmen S., Leibetseder A., Cock H.R., Agrawal N., von Oertzen T.J. Screening of anxiety and quality of life in people with epilepsy. Seizure. 2017;4:107–113. doi: 10.1016/j.seizure.2016.11.026. [DOI] [PubMed] [Google Scholar]
- 13.Banerjee P.N., Filippi D., Allen Hauser W. The descriptive epidemiology of epilepsy—A review. Epilepsy Res. 2009;85:31–45. doi: 10.1016/j.eplepsyres.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kwan P., Brodie M.J. Early identification of refractory epilepsy. N. Engl. J. Med. 2000;342:314–319. doi: 10.1056/NEJM200002033420503. [DOI] [PubMed] [Google Scholar]
- 15.Dowd F.J., Johnson B.S., Mariotti A.J. Pharmacology and Therapeutics for Dentistry. 7th ed. Elsevier; St. Louis, MO, USA: 2017. [Google Scholar]
- 16.Chen Z., Brodie M.J., Liew D., Kwan P. Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: A 30-year longitudinal cohort study. JAMA Neurol. 2018;75:279–286. doi: 10.1001/jamaneurol.2017.3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel A.D., Baca C., Franklin G., Herman S.T., Hughes I., Meunier L., Josephson S.A. Quality improvement in neurology: Epilepsy quality measurement set 2017 update. Neurology. 2018;91:829–836. doi: 10.1212/WNL.0000000000006425. [DOI] [PubMed] [Google Scholar]
- 18.Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br. J. Clin. Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 19.Gilliam F.G., Barry J.J., Hermann B.P., Meador K.J., Vahle V., Kanner A.M. Rapid detection of major depression in epilepsy: A multicentre study. Lancet Neurol. 2006;5:399–405. doi: 10.1016/S1474-4422(06)70415-X. [DOI] [PubMed] [Google Scholar]
- 20.Mula M. Depression in epilepsy. Curr. Opin. Neurol. 2017;30:180–186. doi: 10.1097/WCO.0000000000000431. [DOI] [PubMed] [Google Scholar]
- 21.Mula M. The neglected diagnosis: Mood disorders in patients with epilepsy. Neurol. Times. 2017. [(accessed on 11 July 2022)]. Available online: https://www.neurologytimes.com/epilepsy-and-seizure/neglected-diagnosis-mood-disorders-patients-epilepsy.
- 22.Fiest K.M., Dykeman J., Patten S.B., Wiebe S., Kaplan G.G., Maxwell C.J. Depression in epilepsy: A systematic review and meta-analysis. Neurology. 2013;80:590–599. doi: 10.1212/WNL.0b013e31827b1ae0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tellez-Zenteno J.F., Patten S.B., Jette N., Williams J., Wiebe S. Psychiatric comorbidity in epilepsy: A population-based analysis. Epilepsia. 2007;48:2336–2344. doi: 10.1111/j.1528-1167.2007.01222.x. [DOI] [PubMed] [Google Scholar]
- 24.Kanner A.M. Anxiety disorders in epilepsy: The forgotten psychiatric comorbidity. Epilepsy Curr. 2011;11:90–91. doi: 10.5698/1535-7511-11.3.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gandy M., Sharpe L., Perry K.N., Miller L., Thayer Z., Boserio J., Mohamed A. Anxiety in epilepsy: A neglected disorder. J. Psychosom. Res. 2015;78:149–155. doi: 10.1016/j.jpsychores.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Gandy M., Sharpe L., Perry K.N., Miller L., Thayer Z., Boserio J., Mohamed A. Rates of DSM-IV mood, anxiety disorders, and suicidality in Australian adult epilepsy outpatients: A comparison of well-controlled versus refractory epilepsy. Epilepsy Behav. 2013;26:29–35. doi: 10.1016/j.yebeh.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 27.Suda T., Tatsuzawa Y., Mogi T., Yoshino A. Interictal dysphoric disorder in patients with localization-related epilepsy: Diagnostic relationships with DSM-IV psychiatric disorders and the impact of psychosocial burden. Epilepsy Behav. 2016;54:142–147. doi: 10.1016/j.yebeh.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 28.Dalmagro C.L., Velasco T.R., Bianchin M.M., Martins A.P.P., Guarnieri R., Cescato M.P., Sakamoto A.C. Psychiatric comorbidity in refractory focal epilepsy: A study of 490 patients. Epilepsy Behav. 2012;25:593–597. doi: 10.1016/j.yebeh.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 29.Jones J.E., Hermann B.P., Barry J.J., Gilliam F., Kanner A.M., Meador K.J. Clinical assessment of Axis I psychiatric morbidity in chronic epilepsy: A multicenter investigation. J. Neuropsychiatry Clin. Neurosci. 2005;17:172–179. doi: 10.1176/jnp.17.2.172. [DOI] [PubMed] [Google Scholar]
- 30.Scott A.J., Sharpe L., Hunt C., Gandy M. Anxiety and depressive disorders in people with epilepsy: A meta-analysis. Epilepsia. 2017;58:973–982. doi: 10.1111/epi.13769. [DOI] [PubMed] [Google Scholar]
- 31.El-Metwally A., Javed S., Razzak H.A., Aldossari K.K., Aldiab A., Al-Ghamdi S.H., Al-Zahrani J.M. The factor structure of the general health questionnaire (GHQ12) in Saudi Arabia. BMC Health Serv. Res. 2018;18:595. doi: 10.1186/s12913-018-3381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandes H.M., Vasconcelos-Raposo J. Factorial validity and invariance of the GHQ-12 among clinical and nonclinical samples. Assessment. 2012;20:219–229. doi: 10.1177/1073191112465768. [DOI] [PubMed] [Google Scholar]
- 33.Hankins M. The factor structure of the twelve-item general health questionnaire (GHQ-12): The result of negative phrasing? Clin. Pract. Epidemiol. Ment. Health. 2008;4:10. doi: 10.1186/1745-0179-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.López M.P.S., Dresch V. The 12-item general health questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema. 2008;20:839–843. [PubMed] [Google Scholar]
- 35.Salama-Younes M., Montazeri A., Ismaïl A., Roncin C. Factor structure and internal consistency of the 12-item general health questionnaire (GHQ-12) and the subjective vitality scale (VS), and the relationship between them: A study from France. Health Qual. Life Outcomes. 2009;7:1. doi: 10.1186/1477-7525-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith A.B., Fallowfield L.J., Stark D.P., Velikova G., Jenkins V.A. Rasch and confirmatory factor analysis of the general health questionnaire (GHQ)-12. Health Qual. Life Outcomes. 2010;8:45. doi: 10.1186/1477-7525-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daradkeh T.K., Ghubash R., ElRufaie O.E.F. Reliability, validity, and factor structure of the Arabic version of the 12-item general health questionnaire. Psychol. Rep. 2001;89:85–94. doi: 10.2466/pr0.2001.89.1.85. [DOI] [PubMed] [Google Scholar]
- 38.Endsley P., Weobong B., Nadkarni A. The psychometric properties of GHQ for detecting common mental disorder among community dwelling men in Goa, India. Asian J. Psychiatr. 2017;28:106–110. doi: 10.1016/j.ajp.2017.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Campbell A., Knowles S. A confirmatory factor analysis of the GHQ12 using a large Australian sample. Eur. J. Psychol. Assess. 2007;23:2–8. doi: 10.1027/1015-5759.23.1.2. [DOI] [Google Scholar]
- 40.Gao W., Stark D., Bennett M.I., Siegert R.J., Murray S., Higginson I.J. Using the 12-item general health questionnaire to screen psychological distress from survivorship to end-of-life care: Dimensionality and item quality. Psycho-Oncology. 2012;21:954–961. doi: 10.1002/pon.1989. [DOI] [PubMed] [Google Scholar]
- 41.Graetz B. Multidimensional properties of the general health questionnaire. Soc. Psychiatry Psychiatr. Epidemiol. 1991;26:132–138. doi: 10.1007/BF00782952. [DOI] [PubMed] [Google Scholar]
- 42.Martin L.M., Leff M., Calonge N., Garrett C., Nelson D.E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med. 2000;18:215–218. doi: 10.1016/S0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 43.Padrón A., Galán I., Durbán M., Gandarillas A. Confirmatory factor analysis of the general health questionnaire (GHQ-12) in Spanish adolescents. Qual. Life Res. 2012;21:1291–1298. doi: 10.1007/s11136-011-0038-x. [DOI] [PubMed] [Google Scholar]
- 44.Penninkilampi-Kerola V., Miettunen J., Ebeling H. Health and disability: A comparative assessment of the factor structures and psychometric properties of the GHQ-12 and the GHQ-20 based on data from a Finnish population-based sample. Scand J. Psychol. 2006;47:431–440. doi: 10.1111/j.1467-9450.2006.00551.x. [DOI] [PubMed] [Google Scholar]
- 45.Rajabi G., Sheykhshabani S.H. Factor structure of the 12-item general health questionnaire. J. Educ. Psychol. 2009;3:81–94. [Google Scholar]
- 46.Marsh H.W., Morin A.J., Parker P.D., Kaur G. Exploratory structural equation modeling: An integration of the best features of exploratory and confirmatory factor analysis. Annu. Rev. Clin. Psychol. 2014;10:85–110. doi: 10.1146/annurev-clinpsy-032813-153700. [DOI] [PubMed] [Google Scholar]
- 47.University of Essex, Institute for Social and Economic Research . Understanding Society: Waves 1–11, 2009–2020 and Harmonised BHPS: Waves 1–18, 1991–2009. [Data Collection] 15th ed. UK Data Service; Essex, UK: 2022. SN: 6614. [DOI] [Google Scholar]
- 48.Brooks D.R., Avetisyan R., Jarrett K.M., Hanchate A., Shapiro G.D., Pugh M.J., Kazis L.E. Validation of self-reported epilepsy for purposes of community surveillance. Epilepsy Behav. 2012;23:57–63. doi: 10.1016/j.yebeh.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 49.Goldberg D., Williams P. A User’s Guide to the General Health Questionnaire. NFER-NELSON; London, UK: 1988. [Google Scholar]
- 50.Beletsky V., Mirsattari S.M. Epilepsy, mental health disorder, or both? Epilepsy Res. Treat. 2012;2012:163731. doi: 10.1155/2012/163731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davies S., Heyman I., Goodman R. A population survey of mental health problems in children with epilepsy. Dev. Med. Child Neurol. 2003;45:292–295. doi: 10.1111/j.1469-8749.2003.tb00398.x. [DOI] [PubMed] [Google Scholar]
- 52.Kuroda N. Mental health considerations for patients with epilepsy during COVID-19 crisis. Epilepsy Behav. 2020;111:107198. doi: 10.1016/j.yebeh.2020.107198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lu B., Elliott J.O. Beyond seizures and medications: Normal activity limitations, social support, and mental health in epilepsy. Epilepsia. 2012;53:e25–e28. doi: 10.1111/j.1528-1167.2011.03331.x. [DOI] [PubMed] [Google Scholar]
- 54.Gruenbaum S.E., Wang H., Zaveri H.P., Tang A.B., Lee T.S.W., Eid T., Dhaher R. Inhibition of glutamine synthetase in the central nucleus of the amygdala induces anhedonic behavior and recurrent seizures in a rat model of mesial temporal lobe epilepsy. Epilepsy Behav. 2015;51:96–103. doi: 10.1016/j.yebeh.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mula M. Anhedonia: A Comprehensive Handbook Volume II. Springer; Dordrecht, The Netherlands: 2014. Anhedonia and Epilepsy; pp. 257–264. [Google Scholar]
- 56.Zeidler Z., Brandt-Fontaine M., Leintz C., Krook-Magnuson C., Netoff T., Krook-Magnuson E. Targeting the mouse ventral hippocampus in the intrahippocampal kainic acid model of temporal lobe epilepsy. Eneuro. 2018;5 doi: 10.1523/ENEURO.0158-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baker G.A., Spector S., McGrath Y., Soteriou H. Impact of epilepsy in adolescence: A UK controlled study. Epilepsy Behav. 2005;6:556–562. doi: 10.1016/j.yebeh.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 58.Mott J., Shellhaas R.A., Joshi S.M. Knowledge of epilepsy and preferred sources of information among elementary school teachers. J. Child Neurol. 2013;28:740–744. doi: 10.1177/0883073812451775. [DOI] [PubMed] [Google Scholar]
- 59.Wodrich D.L., Jarrar R., Buchhalter J., Levy R., Gay C. Knowledge about epilepsy and confidence in instructing students with epilepsy: Teachers’ responses to a new scale. Epilepsy Behav. 2011;20:360–365. doi: 10.1016/j.yebeh.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 60.Ridsdale L., Charlton J., Ashworth M., Richardson M.P., Gulliford M.C. Epilepsy mortality and risk factors for death in epilepsy: A population-based study. Br. J. Gen. Pract. 2011;61:e271–e278. doi: 10.3399/bjgp11X572463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beyenburg S., Mitchell A.J., Schmidt D., Elger C.E., Reuber M. Anxiety in patients with epilepsy: Systematic review and suggestions for clinical management. Epilepsy Behav. 2005;7:161–171. doi: 10.1016/j.yebeh.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 62.Satishchandra P., Krishnamoorthy E.S., van Elst L.T., Lemieux L., Koepp M., Brown R.J., Trimble M.R. Mesial temporal structures and comorbid anxiety in refractory partial epilepsy. J. Neuropsychiatry Clin. Neurosci. 2003;15:450–452. doi: 10.1176/jnp.15.4.450. [DOI] [PubMed] [Google Scholar]
- 63.Van Paesschen W., King M.D., Duncan J.S., Connelly A. The amygdala and temporal lobe simple partial seizures: A prospective and quantitative MRI study. Epilepsia. 2001;42:857–862. doi: 10.1046/j.1528-1157.2001.042007857.x. [DOI] [PubMed] [Google Scholar]
- 64.Mohler H. GABAA receptors in central nervous system disease: Anxiety, epilepsy, and insomnia. J. Recept. Signal Transduct. Res. 2006;26:731–740. doi: 10.1080/10799890600920035. [DOI] [PubMed] [Google Scholar]
- 65.Kanner A.M. Depression and epilepsy: A bidirectional relation? Epilepsia. 2011;52:21–27. doi: 10.1111/j.1528-1167.2010.02907.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available datasets were analyzed in this study. These data can be found here: https://www.understandingsociety.ac.uk.