Abstract
We review a comprehensive risk assessment approach for percutaneous coronary interventions in older adults and highlight the relevance of geriatric syndromes within that broader perspective to optimize patient-centered outcomes in interventional cardiology practice. Reflecting the influence of geriatric principles in older adults undergoing percutaneous coronary interventions, we propose a “geriatric” heart team to incorporate the expertise of geriatric specialists in addition to the traditional heart team members, facilitate uptake of the geriatric risk assessment into the preprocedural risk assessment, and address ways to mitigate these geriatric risks. We also address goals of care in older adults, highlighting common priorities that can impact shared decision making among older patients, as well as frequently encountered pharmacotherapeutic considerations in the older adult population. Finally, we clarify gaps in current knowledge and describe crucial areas for future investigation.
Key words: acute coronary syndrome, cardiac catheterization, cardiovascular disease, geriatric assessment, multimorbidity, older adults, percutaneous coronary intervention, polypharmacy
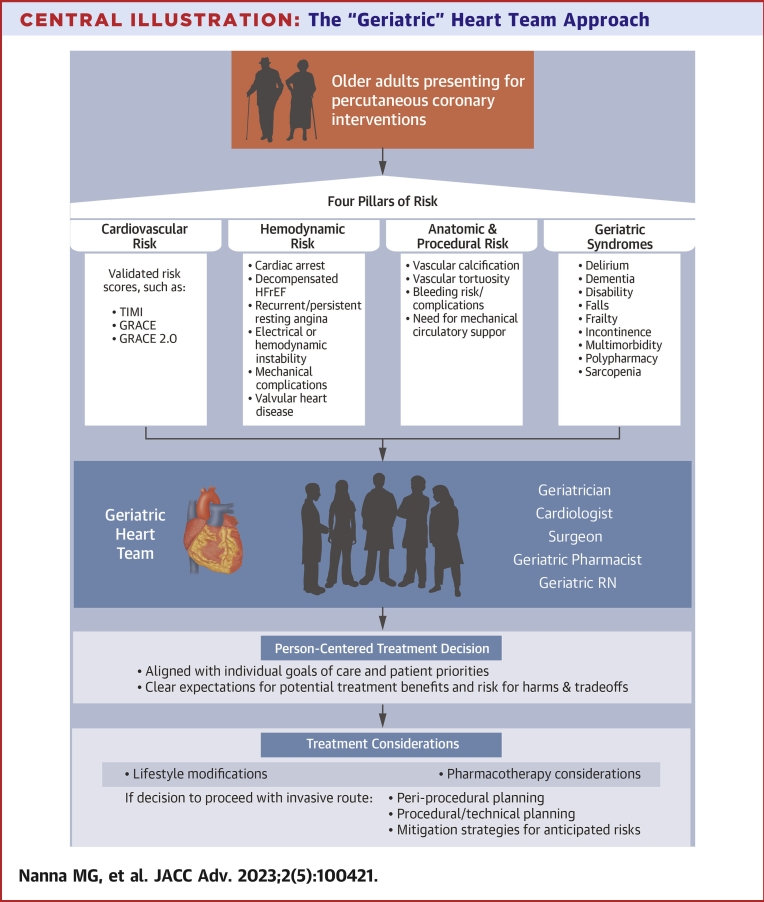
Central Illustration
Highlights
-
•
Geriatric syndromes are a major contributor to periprocedural risk in older adults undergoing PCI.
-
•
A routine geriatric assessment using validated measurement tools should be considered as part of the comprehensive preprocedural evaluation of older adults being considered for PCI.
-
•
A “geriatric” heart team that incorporates the expertise of geriatric specialists, in addition to the traditional heart team members, may provide a more comprehensive and holistic approach to shared decisions in older adults being considered for PCI.
The assessment of geriatric syndromes in older adults is essential and complementary to more traditional cardiovascular risk assessment approaches given the strong association of these risk factors with both short- and long-term morbidity and mortality. In part 1 of percutaneous coronary intervention (PCI) in older adults, we reviewed the 4 pillars of risk in patients presenting for possible PCI, proposing geriatric syndromes as the fourth pillar of risk to consider in older adults. In Part 2, we will review the components of a comprehensive geriatric assessment in older adults being considered for PCI and consider how this information can be used to inform person-centered decisions in collaboration with the “geriatric” heart team. We also review critical periprocedural pharmacotherapeutic considerations in older adults, as well as gaps in current knowledge to guide future areas of investigation.
The geriatric risk assessment
The assessment of geriatric syndromes in older adults is essential and complementary to cardiovascular risk assessment because these age-associated physiologic complexities are risk factors for short- and long-term adverse events. We acknowledge the difficulties inherent in measuring these geriatric conditions and incorporating them into busy clinical workflows, especially in those presenting with acute coronary syndrome (ACS). We present a comprehensive approach for cardiovascular and geriatric assessment prior to invasive treatments in Table 1, as well as a tiered approach to risk assessment in older adults being considered for PCI in Figure 1. While the collection of the complete array of these measures may not be feasible or practical in a busy clinical practice, and there may be collinearity across some measures, this list is meant to provide clinicians with a toolkit for a comprehensive geriatric assessment that may then be tailored to individual patient needs and time constraints. Notably, precedents have already been set in other busy clinical subspecialities for the routine collection of one or more of these geriatric measures.2,3
Table 1.
A Comprehensive Risk Assessment Prior to Invasive Treatments in Older Adults Considered for PCI
| Risk Assessment | Identify High Risk Groups | Perform a Complete Cardiovascular Risk Assessment | Assess Frailty Phenotypea | Complete a Timed Up and Go Testb | Perform the Montreal Cognitive Assessmentc | Perform Short Physical Performance Battery (SPPB)d | Ensure Adequate Social Support | Review Multimorbidity and Polypharmacy | Review Health Care Utilization |
|---|---|---|---|---|---|---|---|---|---|
| Risk category | Cardiogenic shock, cardiac arrest, decompensated HFrEF, recurrent or persistent resting angina with electrical or hemodynamic instability, mechanical complications | Overall geriatric cardiology, hs-cTN, CK/CK-MB, BNP or NT-proBNP plasma concentration, GRACE Score, CRUSADE Bleeding Score | Length of stay, discharge location, postprocedure morbidity and mortality, postprocedure functional recovery potential, incident disability risk, rehospitalization, health care utilization | Functional mobility and falls, with performance correlating with functional status/decline, readmission, and 6-mo mortality | Delirium, ability to understand and adhere to complex postprocedure care plans, critical medication adherence (eg, DAPT) | Postprocedure recovery | Postprocedure care, medication adherence, compliance, and recovery, short, and long-term cardiovascular outcomes | Morbidity and mortality, risk for adverse drug reactions | Rehospitalization |
| Excellent | No high-risk features, stable | Biomarkers are within normal limits. TIMI/GRACE/Crusade: low risk |
Not frail (PFP) | Preserved mobility, ≤15 s to complete | 26+ (out of 30) | 10+ | Yes | None or well-controlled | No ED visits or hospitalization in past year |
| Good | At risk for complications because of recent symptoms | Above average Likely to survive intervention, but some pre-and postcardiovascular procedure risk reduction suggestions are offered; adequate social support |
Pre-frail (PFP: 1-2/5 criteria) | Mild impairment, >15 to ≤25 s to complete | 22-25 | 7-9 | Yes | Yes, generally well-controlled | 1 ED visit or hospitalization in past year |
| Fair | +1 high risk category | Significantly increased. Significant concerns about procedural success; but may be able to optimize over time with intervention |
Frail (PFP: 3/5 criteria) | Moderate impairment, >25 s to complete | <22 | 4-6 | No | Poorly controlled | 2+ ED or hospitalization in past year |
| Poor | +2 high risk categories |
High Deficits unlikely to be remediable, would not recommend procedure |
Frail (PFP: 4-5/5 criteria) | Severe impairment, unable to complete | <22 | 0-3 | No | Poorly controlled | 2+ ED visits or hospitalization in past year |
The cardiovascular risk assessment is performed by cardiovascular clinician and the geriatric risk assessment can be performed by a geriatrician or specialist in geriatric cardiology.
BNP = brain natriuretic peptide; CK = creatine kinase; CK-MB = creatine kinase-myoglobin binding; Crusade = Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines; DAPT = dual antiplatelet therapy; dHFrEF = decompensated Heart Failure with Reduced Ejection Fraction; ED = emergency department visits; GRACE = Global Registry of Acute Coronary Events; hs-cTN = high sensitivity cardiac troponin; NT-proBNP = N-terminal pro-B-type natriuretic peptide; PCI = percutaneous coronary intervention; PFP = Physical Frailty Phenotype; TIMI = Thrombolysis In Myocardial Infarction.
Fried LP, et al. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156.
Montreal Cognitive Assessment (MoCA). https://www.parkinsons.va.gov/resources/MOCA-Test-English.pdf.
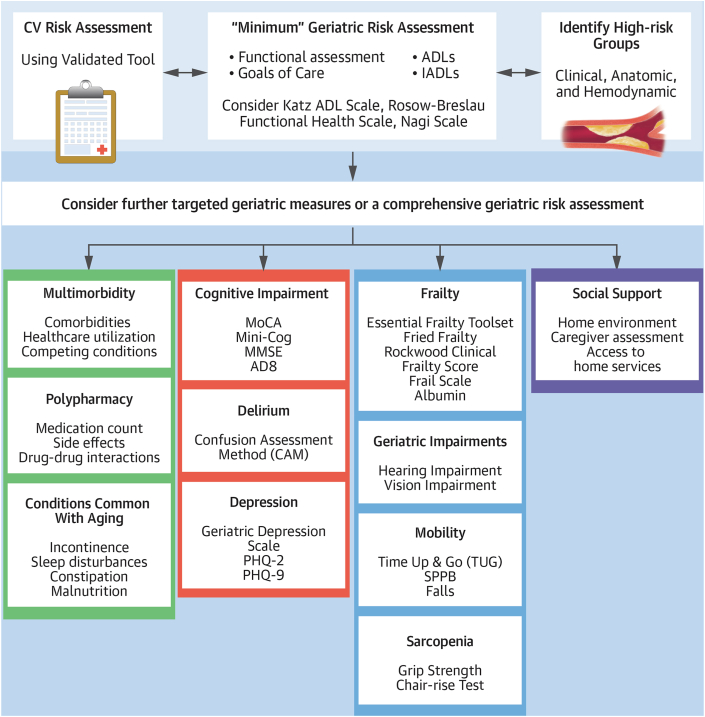
Figure 1.
Risk Assessment in Older Adults Presenting for PCI
This figure presents a proposed risk assessment strategy for older adults presenting for percutaneous coronary intervention including a “minimum” geriatric assessment as well as further targeted geriatric measures as part of a more comprehensive geriatric risk assessment that can be considered. The outlined geriatric measures are grouped according to the 4-domain framework proposed in other cardiovascular populations that include medical (green), mind and emotion (red), physical function (blue), and social environment (purple) domains to address the multidimensional needs of older adults.1 AD8 = The Eight-item Informant Interview to Differentiate Aging and Dementia; ADLs = activities of daily living; CV = cardiovascular; IADLs = instrumental activities of daily living; MMSE = Mini-Mental State Examination; MoCA = Montreal Cognitive Assessment; PCI = percutaneous coronary intervention; PHQ-2 = the patient Health Questionnaire-2; PHQ-9 = the Patient Health Questionnaire-9; SPPB = short physical performance battery.
At a minimum, we recommend an assessment of activities of daily living (ADLs) and instrumental activities of daily living for all older adults undergoing PCI to provide a broad baseline assessment of physical and cognitive function. Examples of useful tools for the assessment of ADLs, instrumental activities of daily living (IADLs), and physical function include the modified Katz Activities of Daily Living Scale,4 the Rosow-Breslau Functional Health Scale,5 and the Nagi Scale.6 For every older adult undergoing invasive assessment, documentation of multimorbidity and polypharmacy is essential as part of geriatric risk assessment, particularly prior to invasive cardiovascular procedures. For those interested in an assessment of lower extremity functioning to inform post procedural recovery, the short physical performance battery can provide valuable information, particularly for those requiring large bore access. An alternative option is the Timed Up and Go test, which provides a simple way to assess functional mobility and fall risk in older adults and represents one of the strongest predictors of functional decline, 180-day readmission, and 6-month mortality among older adults with acute myocardial infarction.7, 8, 9
There are several instruments to capture frailty in practice including the Fried physical frailty phenotype, the Rockwood Clinical Frailty Score and the Frail Scale.10, 11, 12 The essential frailty toolset correlates well with other more complex instruments and may be preferred as it demonstrated superior performance for predicting worsening disability and mortality compared with other commonly used frailty measures and has been validated in patients after revascularization procedures.13, 14, 15 The essential frailty toolset provides objective information and is easy to administer in clinical practice, including 4 components: chair-rise test, cognitive function assessment using the Mini-Mental State Examination or Mini-Cog, hemoglobin, and serum albumin. Albumin is a frequently collected and common element of many of the available frailty measures which reflects nutritional frailty. Nutritional frailty can also be captured with simple measures such as body mass index and inquiries regarding unintentional weight loss.15 Handgrip strength is another straightforward bedside test that has been included in prior frailty measures. Whichever frailty tool is selected should be predictive of adverse outcomes and quick and relatively easy to perform to promote adoption in routine clinical practice.16
Screening tools for cognitive impairment include the Mini-Mental State Examination,17 Mini-Cog,18 Montreal Cognitive Assessment,19 and AD8,20 which is followed by a comprehensive geriatric assessment by a geriatrician if a high burden of cognitive impairment or dementia is detected (though not necessarily prior to the procedure). If cognitive impairment is suspected and confirmed, the cardiovascular team should become familiar with cognitive assessment tools, such as the simple Reisberg Functional Assessment Staging scale for dementia (also known as the Functional Assessment Staging Tool scale). Utilization of this scale, rather than an eyeball test, should lead to better shared decision-making discussions of the benefits and harms of the intervention for the patient and caregiver(s).21
Delirium prevention is key and early identification of patients at risk for delirium can lead to the application of proven delirium prevention interventions including orientation, sleep enhancement, early mobilization, hearing and vision aids, maintaining nutrition and hydration, and minimizing social isolation and psychoactive medications.22,23 Once delirium develops, it can be detected using the confusion assessment method on a daily basis for older patients admitted with ACS, particularly those with chronic comorbidities or polypharmacy.24,25
Finally, assessment for social support is essential to improve postprocedural transitioning, medication adherence, compliance, and patient-centered outcomes. Ultimately the complexity of multimorbidity must be appreciated, where coordination of different clinical priorities and outcomes across subspecialities can be incredibly challenging for patient with multiple chronic conditions.
The ‘geriatric’ heart team
When considering the optimal treatment strategy for older patients at high-risk for complications and adverse outcomes, contemporary guidelines recommend a heart team approach (involving interventional cardiology, cardiac surgery, and clinical cardiology) to craft a revascularization strategy that is patient-centered.26,27 Given the influence of geriatric syndromes on risk, the heart team may also benefit from the inclusion of a geriatrician or a geriatric cardiology specialist to provide expertise on the risk conferred by geriatric syndromes and a more holistic view of how the procedure fits into the broader care of the patient, assessing multiple domains for comprehensive integration by the “geriatric” heart team (Central Illustration). Inclusion of geriatrics specialists may also facilitate the incorporation of geriatric risk assessment into the preprocedural risk in older patients undergoing PCI and address ways to mitigate these risks. The integration of geriatrics experts into the heart team to guide potential geriatric-centered risk mitigation strategies holds great potential value for both patients and their care teams: improving the overall care of this vulnerable population while specifically targeting the prevention of adverse geriatric outcomes such as delirium and falls. In many cases, this may be accomplished by nonphysician care partners including nurses, nurse practitioners, physician assistants, and pharmacists. Optimal management of complex older patients with geriatric syndromes referred for PCI requires a systematic approach, integrating geriatrics expertise into the heart team to enhance communication, shared decision-making, and adherence to best practices.28
Central Illustration.
The “Geriatric” Heart Team Approach
CK-MB = creatine kinase-myoglobin binding; Grace = Global Registry of Acute Coronary Events; HFrEF = heart failure with reduced ejection fraction; RN = registered nurse.
Person-centered goals of care
While the implementation of the comprehensive geriatric risk assessment into a heart team approach for complex decisions around PCI is a priority, the incorporation of that information into the broader context of individual patient priorities, preferences, and risk tolerance in older individuals is another challenge.29 Clinicians are faced with the task of eliciting individual health goals of the patient and advising the patient and caregivers on the best course of action to meet those goals. As noted above, an added layer of complexity is the fact that some of the geriatric syndromes that increase the risk of PCI are also associated with the greatest potential cardiovascular benefit gained from the procedure.
While major adverse cardiovascular events remain the standard reported outcomes for patients admitted with ACS, many of these traditional metrics become less important to individual patients as they reach an advanced age. Parallel to improvement in survival and reduction in cardiovascular outcomes during follow-up, older people may be more likely to prioritize health status and wellbeing compared with younger people.30 Recent randomized clinical trials in cardiology have recognized the importance of outcomes beyond major adverse cardiovascular events, with more person-centered outcomes such as days alive and out of hospital and disability-free survival being highlighted in multiple recent large randomized trials.31, 32, 33, 34, 35, 36
Assessing what matters most to patients is foundational in shared decision-making. Aspects that are particularly important to older patients may include: 1) improvement in ischemic symptom burden; 2) functional independence; 3) remaining at home; 4) improvement in quality-of-life and wellbeing; 5) avoidance of rehospitalization; 6) avoidance of loneliness, isolation, and malnutrition; 7) avoidance of falls, physical disability, and frailty; 8) access to health care and social services; and 9) establishment of end of life goals of care.30,37
Pharmacotherapy considerations
Appropriate pharmacologic treatment for older adult patients undergoing cardiac procedures can be challenging, as this population is at high risk for both ischemic and bleeding events. Indeed, advanced chronological age is a risk factor for both increased risk of stent thrombosis and increased bleeding risk in the current American College of Cardiology/American Heart Association (AHA) guidelines on duration of dual antiplatelet therapy in patients with coronary artery disease. In this section, we will review the use of antiplatelet therapy and sedating medications in geriatric patients undergoing PCI (Table 2).
Table 2.
Pharmacotherapy Considerations for Antiplatelet Therapy and Sedating Medications in Geriatric Patients Undergoing PCI
| Medication Class | Risks Specific to Older Patients | Key Considerations in Older Adults |
|---|---|---|
| Dual antiplatelet therapy | ||
| Concurrent increased risk of ischemic events and bleeding events Particularly high bleeding risk with more potent agents |
|
|
| Sedatives | ||
| Increased burden of comorbidities (cardiac, pulmonary, renal, hepatic, etc) Age-related changes in pharmacokinetics and pharmacodynamics Paradoxical agitation with benzodiazepines |
|
|
PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Dual antiplatelet therapy
The increased risk of ischemic events among older adults is thought to occur secondary to several processes, including increased blood stasis, decreased fibrinolysis, increased endothelialization and platelet reactivity, increased clotting factors, and increased vessel inflammation.38 However, there are concomitant processes that place older adults at greater risk of bleeding events, including increased amyloid and collagen deposits in the arterial walls.
There have been several key subgroup analyses performed in geriatric patients from pivotal ACS trials of P2Y12 inhibitors. Among older adults from TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel–Thrombolysis In Myocardial Infarction 38), there was demonstrated a 19% relative risk reduction in the primary efficacy outcome with the use of prasugrel over clopidogrel with a significant increased risk of bleeding (32% relative increased risk of bleeding).39 As a result of these findings, there is a black box warning against the use of standard dosing of prasugrel (10 mg) in older adults with a chronological age cutoff of >75 years.
Data are somewhat contradictory in the literature regarding the use of ticagrelor vs clopidogrel in older adults. A recent subanalysis from the SWEDEHEART (Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) Registry examined the use of clopidogrel vs ticagrelor in older patients (age >80 years) with ACS demonstrated no significant difference in the primary composite ischemic endpoint,40 but a 20% lower risk of myocardial infarction and 28% lower risk of stroke with ticagrelor countered against a 17% higher risk of death and 48% increased risk of hospitalization for bleeding compared with clopidogrel. The POPular Age (Randomized Comparison of Clopidogrel vs Ticagrelor or Prasugrel in Patients of 70 years or Older With Non–ST-Elevation Acute Coronary Syndrome) did demonstrate a 29% lower bleeding risk with clopidogrel vs ticagrelor.41 A recent AHA Scientific Statement on the management of ACS in the older adult population suggests that the use of ticagrelor may be reasonable in patients with ST-segment elevation myocardial infarction or those with complex anatomy, but recommend clopidogrel as the preferred P2Y12 inhibitor in most older patients with ACS because of a significantly lower bleeding profile than ticagrelor or prasugrel.42 Currently, there are recommendations from both the European Society of Cardiology and the American College of Cardiology/AHA generally against the use of prasugrel in geriatric patients (>75 years of age), unless the patient has a high ischemic risk.
Sedation before and during cardiac catheterization
As an increasing proportion of patients undergoing procedures in the catheterization laboratory are of a higher chronological age and greater procedural complexity, there are important considerations for procedural sedation. In 2017, the Society for Coronary Angiography and Interventions published a document outlining pertinent considerations for moderate sedation in patients undergoing coronary angiography.43 In older adults in particular, it is critical to assess preprocedural comorbidities, such as cardiac function and underlying lung disease, as well as renal and liver function, as these comorbidities may impact the ability of the patient to metabolize sedative agents.44 In older patients and patients with significant obstructive lung disease or hypotension, consideration should be given to administering “half doses” and titrating sedation to achieve a safe balance between patient comfort and hemodynamic compromise. Additionally, several agents used for sedation or preprocedural treatment have a prolonged half-life in older patients due to age-related changes in pharmacokinetics, which along with changes in pharmacodynamics, can lead to unpredictable properties.42 These agents include diphenhydramine, which has a normal half-life of 7 to 18 hours but can be prolonged in older patients, and benzodiazepines which can have a prolonged half-life and cause paradoxical agitation in older patients. For older patients with a history of poor tolerance of moderate sedation, consideration should be given to engage an anesthesia clinician, if possible, to administer sedation.
Gaps in knowledge and future directions
Uptake of risk tools in the cardiac catheterization laboratory
As identified above, the care of geriatric patients in the cardiac catheterization laboratory often requires individually nuanced preprocedural, intraprocedural, and postprocedural risk assessment and decision making. While there has been increasing focus on including gero-centric variables in risk models for patients undergoing PCI, risk models remain inconsistently utilized, which may relate to a perceived lack of importance, complexity of scores requiring specialized calculators for use, and lack of awareness of available risk scores.45,46 Standardized implementation of electronic health record-based risk-score calculators may, in the future, negate some of these factors but would be restricted to variables that are readily available with the electronic health record.
Collection of geriatric risk markers and risk modifying approaches
It remains to be seen whether geriatric risk markers can be reliably collected and integrated into care decisions. Studies piloting the incorporation of a geriatric assessment into routine clinical care of patients being considered for PCI are required to assess the feasibility of such an approach. Successful implementation of the suggested comprehensive geriatric risk assessment or a streamlined point-of-care version also involves demonstrating an improvement in not just the geriatric measures themselves, but improvement in clinical outcomes, including patient centered outcomes. Certain measures of frailty and nutritional status, such as serum albumin and body mass index, are already routinely collected in most patients and provide incremental information on risk. Implementation of a standardized frailty assessment and targeted interventions surrounding surgical procedures have been shown to reduce postoperative complications and mortality.47,48 Prior studies in older patients undergoing aortic valve replacement have similarly demonstrated the feasibility of implementing a frailty assessment and shown that it can be used mortality.49, 50, 51 In a similar manner, one can imagine implementing a peri-procedural assessment and targeted interventions in patients undergoing PCI to improve outcomes in this particularly vulnerable population of patients. This is a critical area for future investigation.
Decision support tools
Unfortunately, previously developed decision support tools for younger populations with coronary artery disease fail to include the more holistic approach necessary in older adults.52,53 Other decision aids focused on older adults with multiple chronic conditions, such as the patient priorities care approach,54 carry more promise but have not been tested in the older adult population referred to the cardiac catheterization laboratory. The prioritization of both traditional outcomes and more person-centered outcomes focused on quality of life and function in clinical decision-making in interventional cardiology and the dedicated evaluation of treatment effects of cardiovascular procedures on these particular endpoints are key areas for future emphasis and study.
Treating the whole patient: moving from a lesion-centered to a person-centered model
Even with routine measurement of geriatric risk markers, percutaneous procedures do not cure most older patients presenting to the catheterization laboratory. Rather, all procedures must be seen as important but limited components of the broader therapeutic construct for older adults presenting with cardiovascular conditions. Thus, improving the uptake of interventions targeting prevalent geriatric conditions to improve quality of life and function are a crucial component of these cardiovascular encounters. Interventions to reduce frailty in patients with cardiovascular disease was the focus of a recent comprehensive review, demonstrating that frailty is a dynamic process that can potentially be reversible with multicomponent approaches including physical therapy and rehabilitation, and pharmacologic, cognitive, nutritional, and psychosocial interventions.15 Cardiac rehabilitation is grossly underutilized in patients following PCI compared with postsurgical patients despite the older, multimorbid demographic of many patients undergoing PCI.55 Potential treatments of sarcopenia include physical exercise (especially strength training), nutrition, hormone therapy, and medications including angiotensin-converting enzyme inhibitor and angiotensin receptor blockers which have benefits for muscle tissue.56 Routine implementation of strategies for the prevention57 of falls is a critical component of in-hospital care and postdischarge care.58,59 These include the use of bed alarms, physical therapy, occupational therapy, durable medical equipment for gait assistance, and skilled nursing resources whenever appropriate.58,59 Importantly, a third to nearly half of delirium episodes can be prevented using early intervention and avoidance strategies targeted at avoiding psychoactive medications wherever possible.60, 61, 62
Conclusions
Given the importance of geriatric syndromes in the preprocedural assessment of older adults undergoing cardiac procedures, we propose the components of a comprehensive geriatric risk assessment, including periprocedural pharmacotherapy considerations, to provide a toolkit that can be implemented to help guide care decisions. We highlight key areas for ongoing investigation that will improve the decision-making process around invasive cardiovascular procedures for older adults in the near future.
Funding support and author disclosures
Dr Nanna consults for HeartFlow, Inc. Dr Rymer has relationships with Chiesi, Abiomed, Pfizer, and Idorsia. Dr Lowenstern is a consultant for Edwards Lifesciences. Dr Bortnick is site PI for CSL-Behring; is the recipient of an unrestricted educational grant to the institution from Zoll, Inc; and has received honoraria from ClearView Healthcare, LLC. Dr Damluji receives mentored patient-oriented research career development award from the National Heart, Lung, and Blood Institute K23-HL153771-01. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Gorodeski E.Z., Goyal P., Hummel S.L., et al. Domain management approach to heart failure in the geriatric patient: present and future. J Am Coll Cardiol. 2018;71:1921–1936. doi: 10.1016/j.jacc.2018.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amini S., Crowley S., Hizel L., et al. Feasibility and rationale for incorporating frailty and cognitive screening protocols in a preoperative anesthesia clinic. Anesth Analg. 2019;129:830. doi: 10.1213/ANE.0000000000004190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birkelbach O., Mörgeli R., Spies C., et al. Routine frailty assessment predicts postoperative complications in elderly patients across surgical disciplines–a retrospective observational study. BMC Anesthesiol. 2019;19:1–10. doi: 10.1186/s12871-019-0880-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz S., Akpom C.A. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 5.Rosow I., Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 6.Nagi S.Z. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54:439–467. [PubMed] [Google Scholar]
- 7.Dodson J.A., Hajduk A.M., Murphy T.E., et al. 180-day readmission risk model for older adults with acute myocardial infarction: the SILVER-AMI study. Open Heart. 2021;8 doi: 10.1136/openhrt-2020-001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodson J.A., Hajduk A.M., Geda M., et al. Predicting 6-month mortality for older adults hospitalized with acute myocardial infarction: a cohort study. Ann Intern Med. 2020;172:12–21. doi: 10.7326/M19-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hajduk A.M., Murphy T.E., Geda M.E., et al. Association between mobility measured during hospitalization and functional outcomes in older adults with acute myocardial infarction in the SILVER-AMI study. JAMA Intern Med. 2019;179:1669–1677. doi: 10.1001/jamainternmed.2019.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 11.Dalhousie University. Clinical Frailty Scale. Accessed June 28, 2023. https://www.bgs.org.uk/sites/default/files/content/attachment/2018-07-05/rockwood_cfs.pdf
- 12.Frail Scale. Accessed June 28, 2023. https://www.mass.gov/doc/frail-scale-screening-tool/download
- 13.Solomon J., Moss E., Morin J.F., et al. The essential frailty toolset in older adults undergoing coronary artery bypass surgery. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.020219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Afilalo J., Lauck S., Kim D.H., et al. Frailty in older adults undergoing aortic valve replacement. J Am Coll Cardiol. 2017;70:689–700. doi: 10.1016/j.jacc.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 15.Ijaz N., Buta B., Xue Q.L., et al. Interventions for frailty among older adults with cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79:482–503. doi: 10.1016/j.jacc.2021.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yanagawa B., Graham M.M., Afilalo J., Hassan A., Arora R.C. Frailty as a risk predictor in cardiac surgery: beyond the eyeball test. J Thorac Cardiovasc Surg. 2019;157:1905–1909. doi: 10.1016/j.jtcvs.2018.08.054. [DOI] [PubMed] [Google Scholar]
- 17.TENG MINI-MENTAL STATE EXAMINATION (3MS). Accessed June 28, 2023. https://healthabc.nia.nih.gov/sites/default/files/mmse_0.pdf
- 18.Mini-Cog©. Quick Screening for Early Dementia Detection. Accessed June 28, 2023. https://mini-cog.com
- 19.MONTREAL COGNITIVE ASSESSMENT (MOCA). Accessed June 28, 2023. https://www.parkinsons.va.gov/resources/MOCA-Test-English.pdf
- 20.Galvin J.E., Roe C.M., Coats M.A., Morris J.C. Patient's rating of cognitive ability: using the AD8, a brief informant interview, as a self-rating tool to detect dementia. Arch Neurol. 2007;64:725–730. doi: 10.1001/archneur.64.5.725. [DOI] [PubMed] [Google Scholar]
- 21.Reisberg B. Functional assessment staging (FAST) Psychopharmacol Bull. 1988;24:653–659. [PubMed] [Google Scholar]
- 22.Inouye S.K. The importance of delirium and delirium prevention in older adults during lockdowns. JAMA. 2021;325:1779–1780. doi: 10.1001/jama.2021.2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdullah A., Eigbire G., Salama A., et al. Impact of delirium on patients hospitalized for myocardial infarction: a propensity score analysis of the national inpatient sample. Clin Cardiol. 2018;41:910–915. doi: 10.1002/clc.22972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wei L.A., Fearing M.A., Sternberg E.J., Inouye S.K. The confusion assessment method: a systematic review of current usage. J Am Geriatr Soc. 2008;56:823–830. doi: 10.1111/j.1532-5415.2008.01674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inouye S.K., van Dyck C.H., Alessi C.A., Balkin S., Siegal A.P., Horwitz R.I. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 26.Lawton J.S., Tamis-Holland J.E., Bangalore S., et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e21–e129. doi: 10.1016/j.jacc.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Krishnaswami A., Bernacki G.M., Bhatt D.L. Geriatric and palliative care specialists as valued members of the multidisciplinary heart team. Am J Med. 2022;135:810–812. doi: 10.1016/j.amjmed.2022.01.020. [DOI] [PubMed] [Google Scholar]
- 28.Batchelor W., Anwaruddin S., Wang D., et al. The multidisciplinary heart team in cardiovascular medicine: current role and future challenges. JACC: Adv. 2022;2 [Google Scholar]
- 29.Nanna M.G., Peterson E.D., Wu A., et al. Age, knowledge, preferences, and risk tolerance for invasive cardiac care. Am Heart J. 2020;219:99–108. doi: 10.1016/j.ahj.2019.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akpan A., Roberts C., Bandeen-Roche K., et al. Standard set of health outcome measures for older persons. BMC Geriatr. 2018;18:36. doi: 10.1186/s12877-017-0701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McNeil J.J., Woods R.L., Nelson M.R., et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379:1499–1508. doi: 10.1056/NEJMoa1800722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou Z., Ofori-Asenso R., Curtis A.J., et al. Association of statin use with disability-free survival and cardiovascular disease among healthy older adults. J Am Coll Cardiol. 2020;76:17–27. doi: 10.1016/j.jacc.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McNeil J. Rationale for aspree disability-free survival primary outcome and overview of primary outcome results. Innov Aging. 2019;3(Suppl 1) doi: 10.1093/geroni/igz038.2357. [DOI] [Google Scholar]
- 34.Fanaroff A.C., Cyr D., Neely M.L., et al. Days alive and out of hospital: exploring a patient-centered, pragmatic outcome in a clinical trial of patients with acute coronary syndromes. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.118.004755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jerath A., Austin P.C., Wijeysundera D.N. Days alive and out of hospital: validation of a patient-centered outcome for perioperative medicine. Anesthesiology. 2019;131:84–93. doi: 10.1097/ALN.0000000000002701. [DOI] [PubMed] [Google Scholar]
- 36.White H.D., O'Brien S.M., Alexander K.P., et al. Comparison of days alive out of hospital with initial invasive vs conservative management: a prespecified analysis of the ISCHEMIA trial. JAMA Cardiol. 2021;6:1023–1031. doi: 10.1001/jamacardio.2021.1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goyal P., Kwak Min J., Al Malouf C., et al. Geriatric cardiology: coming of age. JACC: Adv. 2022;1:1–14. doi: 10.1016/j.jacadv.2022.100070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Capranzano P., Angiolillo D.J. Antithrombotic management of elderly patients with coronary artery disease. J Am Coll Cardiol Intv. 2021;14:723–738. doi: 10.1016/j.jcin.2021.01.040. [DOI] [PubMed] [Google Scholar]
- 39.Wiviott S.D., Braunwald E., McCabe C.H., et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 40.Szummer K., Montez-Rath M.E., Alfredsson J., et al. Comparison between ticagrelor and clopidogrel in elderly patients with an acute coronary syndrome. Circulation. 2020;142:1700–1708. doi: 10.1161/CIRCULATIONAHA.120.050645. [DOI] [PubMed] [Google Scholar]
- 41.Gimbel M., Qaderdan K., Willemsen L., et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-ST-elevation acute coronary syndrome (POPular AGE): the randomised, open-label, non-inferiority trial. Lancet. 2020;395:1374–1381. doi: 10.1016/S0140-6736(20)30325-1. [DOI] [PubMed] [Google Scholar]
- 42.Damluji A.A., Forman D.E., Wang T.Y., et al. Management of acute coronary syndrome in the older adult population: a scientific statement from the American Heart Association. Circulation. 2023;147(3):e32–e62. doi: 10.1161/CIR.0000000000001112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bagai J., Beavers C.J. 2017. Moderate Sedation Practices for Adult Patients in the Cardiac Catheterization Laboratory (CCL)https://scai.org/moderate-sedation-practices-adult-patients-cardiac-catheterization-laboratoryccl SCAI.org. [Google Scholar]
- 44.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–1017. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 45.Fanaroff A.C., Wang T.Y. Risk prediction in percutaneous coronary intervention: solving the last mile problem. Circ Cardiovasc Interv. 2022;15(7) doi: 10.1161/CIRCINTERVENTIONS.122.012262. [DOI] [PubMed] [Google Scholar]
- 46.Engel J., Heeren M.-J., van der Wulp I., de Bruijne M.C., Wagner C. Understanding factors that influence the use of risk scoring instruments in the management of patients with unstable angina or non-ST-elevation myocardial infarction in the Netherlands: a qualitative study of health care practitioners’ perceptions. BMC Health Serv Res. 2014;14:418. doi: 10.1186/1472-6963-14-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilson S., Sutherland E., Razak A., et al. Implementation of a frailty assessment and targeted care interventions and its association with reduced postoperative complications in elderly surgical patients. J Am Coll Surg. 2021;233:764–775.e1. doi: 10.1016/j.jamcollsurg.2021.08.677. [DOI] [PubMed] [Google Scholar]
- 48.Hall D.E., Arya S., Schmid K.K., et al. Association of a frailty screening initiative with postoperative survival at 30, 180, and 365 days. JAMA Surg. 2017;152:233–240. doi: 10.1001/jamasurg.2016.4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Afilalo J. The clinical frailty scale: upgrade your eyeball test. Circulation. 2017;135:2025–2027. doi: 10.1161/CIRCULATIONAHA.116.025958. [DOI] [PubMed] [Google Scholar]
- 50.Rockwood K., Song X., MacKnight C., et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shimura T., Yamamoto M., Kano S., et al. Impact of the clinical frailty scale on outcomes after transcatheter aortic valve replacement. Circulation. 2017;135:2013–2024. doi: 10.1161/CIRCULATIONAHA.116.025630. [DOI] [PubMed] [Google Scholar]
- 52.Coylewright M., Dick S., Zmolek B., et al. PCI choice decision aid for stable coronary artery disease: a randomized trial. Circ Cardiovasc Qual Outcomes. 2016;9:767–776. doi: 10.1161/CIRCOUTCOMES.116.002641. [DOI] [PubMed] [Google Scholar]
- 53.Coylewright M., Shepel K., Leblanc A., et al. Shared decision making in patients with stable coronary artery disease: PCI choice. PLoS One. 2012;7 doi: 10.1371/journal.pone.0049827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tinetti M.E., Naik A.D., Dindo L., et al. Association of patient priorities–aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med. 2019;179:1688–1697. doi: 10.1001/jamainternmed.2019.4235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beatty A.L., Bradley S.M., Maynard C., McCabe J.M. Referral to cardiac rehabilitation after percutaneous coronary intervention, coronary artery bypass surgery, and valve surgery. Circ Cardiovasc Qual Outcomes. 2017;10 doi: 10.1161/CIRCOUTCOMES.116.003364. [DOI] [PubMed] [Google Scholar]
- 56.He N., Zhang Y., Zhang L., Zhang S., Ye H. Relationship between sarcopenia and cardiovascular diseases in the elderly: an overview. Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.743710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Damluji A.A., Alfaraidhy M., AlHajri N., et al. Sarcopenia and cardiovascular diseases. Circulation. 2023;147:1534–1553. doi: 10.1161/CIRCULATIONAHA.123.064071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.LeLaurin J.H., Shorr R.I. Preventing falls in hospitalized patients: state of the science. Clin Geriatr Med. 2019;35:273–283. doi: 10.1016/j.cger.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morris R., O'Riordan S. Prevention of falls in hospital. Clin Med. 2017;17:360–362. doi: 10.7861/clinmedicine.17-4-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fong T.G., Tulebaev S.R., Inouye S.K. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5:210–220. doi: 10.1038/nrneurol.2009.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Siddiqi N., House A.O., Holmes J.D. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35:350–364. doi: 10.1093/ageing/afl005. [DOI] [PubMed] [Google Scholar]
- 62.Oh E.S., Fong T.G., Hshieh T.T., Inouye S.K. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318:1161–1174. doi: 10.1001/jama.2017.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]