Abstract
Global developmental delay (GDD) is a complex disorder that requires multimodal treatment involving different developmental skills. The objective of this single-blind, randomized, controlled pilot study is to evaluate the feasibility and effectiveness of conventional rehabilitation programs integrated with the BTs-Nirvana virtual reality system. Patients with GDD aged 12 to 66 months were enrolled and treated for a 48-session cycle. Patients were randomized into two groups, (1) conventional treatment and (2) conventional treatment supplemented with the use of BTs-Nirvana, in a 1:1 ratio. Before and after treatments, areas of global development were tested with the Griffiths-III Mental Developmental Scale and the clinical indicator of global improvement were measured with the Clinical Global Impressions-Improvement (CGI-I). Feasibility was confirmed by the high retention rate. The experimental group presented a significantly improvement in General Quotient (GQ) after treatment (GQ, p = 0.02), and the effect of the two treatments was significantly different in both the GQ (t =2.44; p = 0.02) and the Foundations of Learning subscale (t =3.66; p < 0.01). The overall improvement was also confirmed by the CGI-I (p = 0.03). According to these preliminary data, virtual reality can be considered a useful complementary tool to boost the effectiveness of conventional therapy in children with GDD.
Keywords: neurodevelopmental disorders, virtual reality exposure therapy, child, preschool, randomized controlled trial, early intervention, educational
1. Introduction
Global Developmental Delay (GDD) is a common neurodevelopmental disorder which affects 1–3% of children aged 5 years or younger [1]. It is characterized by deficits in developmental milestones in several areas of intellectual functioning [2]. GDDs are usually identified by caregivers, by teachers at school who raise concerns, or during routine clinical evaluations by the pediatrician [3]. It can be caused by specific conditions which are not always easy to identify. Chromosomal abnormalities, perinatal asphyxia, preterm birth, cerebral dysgenesis, psychosocial deprivation, and toxin exposure are some of the possible causes [4].
Recent data from the literature have underlined the importance of early diagnosis followed by appropriate therapeutic management. In fact, GDD could evolve into different neurodevelopmental disorders, especially if associated with other risk factors, such as intra-uterine growth retardation, nutrient deficiencies, breastfeeding and maternal education, scarce social and economic conditions, poor learning opportunities, inadequate quality of caregiver–child interactions [5]. The recognition of risk factors and early treatments can significantly influence the long-term outcome of developmental disability [6]. The importance of continuously stimulating children is well known, especially during the earliest stages of development. In fact, the young nervous system is capable of producing numerous new behaviors to interact with the environment and adapting to it [7].
For patients affected by GDD, the Italian National Health Service provides “speech therapy” and “neuropsychomotor therapy”. “Neuropsychomotor therapy” is a typical Italian rehabilitation approach for patients from birth until 18 years old, affected from neurodevelopmental disorders. It is similar to “play therapy” and “developmental therapy” practiced in other countries [8]. This therapy aims to strengthen motor, functional, affective, relational, and cognitive areas by trying to stimulate active learning through toys and interactive games; therefore, the ultimate goal of this kind of therapy is the harmonious integration of all functional areas during the growth process through a comprehensive approach [9]. Speech and neuropsychomotor therapy are usually prescribed to child and adolescent by psychiatrists or neurologists and delivered by community child neuropsychiatry services.
In recent decades, the use of virtual reality (VR) in rehabilitation has become more and more popular for its possible implementation in innovative treatments in cognitive-motor domain. Many studies suggest that VR can constitute a motivating and fun rehabilitation approach, being more engaging than conventional therapy or educational programs, both for adults and children [10,11]. This system allows naturalistic behaviors to be enacted in a controlled environment and permits therapists to adjust multimodal stimulus according to patients’ characteristics and needs [12]. VR-based rehabilitation promotes implicit learning, offering repetitive and intensive tasks with immediate sensorimotor feedback. Virtual reality, being associated with the idea of playing, allows the children an unconscious learning process [13].
In recent literature, several studies have been conducted to test the effectiveness and feasibility of virtual reality system for rehabilitative treatment in various neurodevelopmental disorders. Among these, probably one of the disorders in which this hypothesis has been most tested is infant cerebral palsy, in which gross motor function appears to improve significantly, although the effect on the daily living ability remains controversial [14]. Several reviews on autism spectrum disorder described the usefulness of VR tools for children affected by this heterogeneous neurodevelopmental disorder, particularly on social and emotional skills training [15,16], and as support for social situations that can be generalized in real-world [17]. Moreover, 83% of the articles reviewed by Goharinejad et colleagues [18] described the benefits of virtual, augmented, and mixed reality technologies to ameliorate symptoms of attention deficit hyperactivity disorder.
Among the high-tech tools used in recent years for neuropsychomotor rehabilitation, the BTs-Nirvana system (BTsN) is a medical markerless device that uses semi-immersive VR to rehabilitate patients with neurological disorders associated with motor and cognitive difficulties, even in childhood. BTsN is based on infrared optoelectronic sensors, through which the patient can interact with a virtual scenario. The system is connected to a wall or floor projector, reproducing an interactive series of exercises, using an infrared camera that analyzes the patient’s movements [11]. The previous literature on adult patients affirm the utility of this tool to enhance the functional recovery of cognition dysfunctions. In De Luca et al. [19], the use of BTsN seems to be useful in post-stroke rehabilitation, leading to improved cognitive and motor impairment with particular regard to trunk control, and visuo-spatial. Several other studies have demonstrated the usefulness of semi-immersive VR-BTsN, showing promising results regarding functional recovery and perception of quality of life in patients with various neurological diseases, including multiple sclerosis [20], traumatic brain injury [21] and Parkinson disease [22].
Thanks to its characteristic of interactive and game-like tool, active explorations are encouraged in patients and a major involvement provides motivation and enjoyment, allowing longer training sessions and improving treatment adherence. Furthermore, BTs-N has emerged as a valuable tool in the treatment of different disorders, even in pediatric age. In patients with autism spectrum disorder, for example, it was used to improve attention processes and visuospatial cognition [23]; moreover, this rehabilitation device also was used to improve balance and motor skills in children and adolescents with cerebral palsy [24].
The primary goal of this single-blind, randomized-controlled pilot study was to evaluate the feasibility of an integrated rehabilitation program with BTs-Nirvana Intervention (BTsN-I) in patients with GDD with regard to patient acceptability and sustainability along the months. The secondary aim was to evaluate the effectiveness of semi-immersive VR compared to treatment as usual (TAU).
2. Materials and Methods
2.1. Study Design
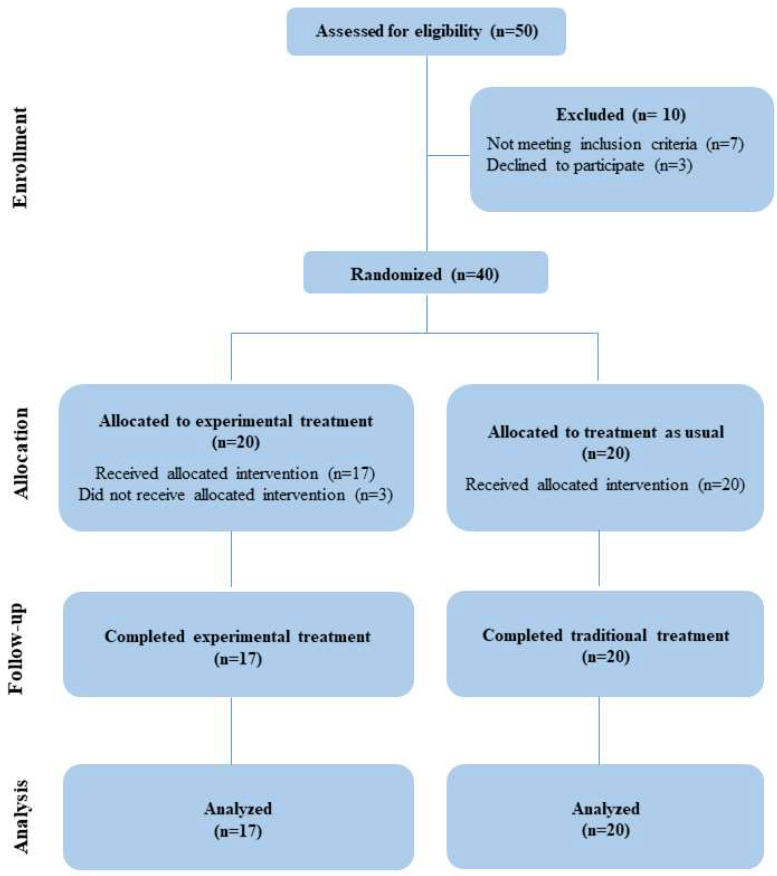
A single-blind, randomized, controlled pilot study was performed at the Child Neuropsychiatry service of the IRCCS Centro Neurolesi “Bonino Pulejo” in Messina, Italy. This study was carried out in accordance with the Declaration of Helsinki; furthermore, it was examined and approved by the Ethical Committee IRCCS Sicilia Centro Neurolesi “Bonino-Pulejo”; this clinical trial adheres to CONSORT guidelines [25], and has been registered in http://www.clinicaltrials.com (accessed on 5 June 2023) (identifier: NCT05879952). See detailed information about the CONSORT flow-chart of the study in Figure 1. Written informed consent was obtained from both caregivers or a legally authorized patient representative.
Figure 1.
The CONSORT flow-chart with detailed information about participants in the study.
2.2. Inclusion Criteria and Participants
After viewing the information relating to the experimental treatment, parents remained interested in the study; a total of 50 children with GDD were screened for eligibility between December 2020 and September 2022. Inclusion criteria were (a) diagnosis of GDD, (b) age between 12 and 66 months, and (c) consistent attendance in the therapy program for the total number of sessions scheduled. Children who had other major medical conditions such as epilepsy, severe visual and auditory sensory deficits, traumatic brain injury, or other significant genetic disorders, were excluded. A total of N. 40 patients fulfilled inclusion criteria and were enrolled. The distribution of participants into experimental or control group was randomly made by a computer-generated list of arbitrary numbers, used to assign participants. Allocation was conducted by a blind researcher who did not participate in the trial.
2.3. Outcome Measures
Changes from pre (T0) to post (T1) interventions were evaluated by independent assessors, blind to treatment conditions. Each patient was evaluated pre- and post-treatment by the same assessor. Feasibility was assessed through service utilization analysis, which consists of engagement and the rate of participation in rehabilitation programs. To evaluate preliminary efficacy of experimental interventions, we take into account two main measures. (1) Griffiths-III Mental Development Scale (GMDS-III [26]), to track change among all developmental areas. The GMDS-III is an assessment tool for children from 0 to 72 months, that provides a General Quotient (GQ) and five different scales: Learning Bases, Language and Communication, Eye-hand Coordination, Personal-Social Emotional, and Gross-motor. For each of these areas, a score is obtained which indicates an extremely low GQ if ≤69, borderline 70–79, below average 80–89, average 90–109, above average 110–119, high 120–129, and very high > 130. (2) Clinical Global Impressions-Improvement (CGI-I [27]), to quantify and monitor patients’ progress and response to treatment, providing a clinical judgment on global improvement. In detail, the scores of the Severity section (CGI-S), ranging from 1 (normal, no disease) to 6 (seriously ill), were considered to assess the severity at baseline (T0). Moreover, the scores relating to the improvement section ranging from 1 (very improved condition) to 6 (moderately worsened).
2.4. Intervention
All patients underwent a cycle of 48 treatments, each lasting 45 min, in 1:1 ratio. The control group was treated with TAU twice a week, while the patients of the experimental group underwent one session of TAU and one session of BTsN per week. Therapies were carried out by qualified therapists who were randomly assigned. Each child was treated by the same therapist for the entire cycle. Both professional teams (TAU and BTsN-I teams) had similar backgrounds and professional training.
Participants assigned to control group (TAU) underwent standard neuro-psychomotor training, representatives of the existing services nationwide. During TAU sessions, patients performed exercises to promote better organization of global motor skills, improve hand-eye coordination, promote the development of language as communication, enriching representation and symbolization skills and improve the acquisition of age-appropriate developmental milestones. The treatment was tailored according to each child’s goals and preferences.
In the experimental group (BTsN-I) the conventional therapy program was integrated with the use of BTsN pediatric modules in a 1:1 ratio. BTsN treatment session included exercises designed to identify, find, chase, or move objects, with the aim of improving the perceptual-cognitive skills of each patient, through audio–visual stimuli and feedback implementing visuo-spatial skills and spatial cognition, allowing, at the same time, motor coordination and balance improvement. All the exercises had been customized according to the therapists to the individual’s treatment needs, adapting the level of difficulty to the patient’s abilities. These exercises made it possible, in a more captivating and engaging environment for the child, to work simultaneously on different cognitive and motor domains: visual perception, spatial organization, attention, memory, language, balance, posture, and coordination (See description of the games adopted during VR-based intervention in Table 1 and images in Figure 2).
Table 1.
Description of the main games used during session with BTsN by type of system projection and neuropsychological domain involved in each activity.
| Scenario | Projection | Game | Neuropsychological Domain |
|---|---|---|---|
| Balloons | floor | To reach the balloons flying upwards and pop them with foot | Visual–motor integration, Motor coordination, Impulse control |
| Tap Mole * | floor | To capture the mole that appears randomly | Visual–spatial cognition, Motor coordination, Impulse control |
| Balls * | wall | To play with the ball to bounce it off the walls of the screen | Visual–spatial cognition, Visual–motor integration, Executive functions—planning |
| Trumpets | wall | To play the trumpets by touching them | Auditory discrimination and working memory, Visual discrimination, Executive functions—planning |
| Guitar | wall | To play the single guitar chords by hands movement | Auditory discrimination and working memory, Visual discrimination, Executive functions—planning |
| Cooking | wall | To grasp the ingredients indicated on the board and move them to the pot | Executive functions—self monitoring, organization, planning |
* The scenarios of Tap Mole and Balls games of BTS-Nirvana are shown in Figure 2.
Figure 2.
Example of two games used during BTsN intervention. Panel (A) Game 2—Tap Mole: the exercise is projected onto the floor and the child has to catch the moles that suddenly appear from the holes. Panel (B) Game 3—Balls: the exercise is projected onto the wall and the child has to bounce the balls.
2.5. Statistical Analysis
Data were analyzed using the R software, version 4.0.5, considering p-value < 0.05 as statistically significant. Due to the small sample size, a non-parametric approach was used. Thus, the Mann–Whitney U test was used to compare the two groups at baseline, whereas the Wilcoxon signed-rank test was used to compare each group between baseline and the end of the study. The Chi-squared test was used to compare proportions. Using the car package of R, for any dimension of the Griffiths III scale, an analysis of covariance (ANCOVA) was performed after testing of assumptions. The model had the test score at T1 as dependent variable, the categorical variable ‘Group’ (1 = experimental; 0 = control) as independent variable, and the outcome score at baseline (T0) as covariate. We also performed ANOVA to verify whether the model was significantly different when we fitted it including the interaction term effect “outcome score at baseline * categorical variable”.
3. Results
3.1. Baseline Characteristics of Participants
A total of N. 40 patients fulfilled inclusion criteria and were enrolled. Despite the initial agreement, n. 3 patients randomly assigned to the BTsN-I group did not start the study for personal reasons. Final sample were constituted by n. 20 subjects (13 males and 7 females, mean age 42.5 ± 13.9 months) randomly assigned to TAU and n. 17 subjects (13 males and 4 females, mean age 35.1 ± 9.8 months) to BTsN-I. A more detailed description of the two groups is in Table 2. No significant difference either for age (p = 0.06) or gender (p = 0.69) were found between experimental and control group.
Table 2.
Demographic characteristics of participants.
| TAU | BTsN-I | Total Sample | ||||
|---|---|---|---|---|---|---|
| N | Mean ± SD or % |
N | Mean ± SD or % |
N | Mean ± SD or % |
|
| Enrolled patients | 20 | 20 | 40 | |||
| Final Sample | 20 | 17 | 37 | |||
| Age in months | 35.1 ± 9.8 | 42.5 ± 13.9 | 39.1 ± 12.6 | |||
| Gender | ||||||
| Male | 13 | 65.0% | 13 | 76.5% | 26 | 70.3% |
| Female | 7 | 35.0% | 4 | 23.5% | 11 | 29.7% |
| M:F Ratio | 2:1 | 3:1 | 2:1 | |||
| CGI Severity (T0) | 4.1 ± 1 | 3.8 ± 1.1 | 4 ± 1.1 | |||
Mean ± standard deviation was used to describe continuous variables; proportions (numbers and percentages) were used to describe categorical variables.
3.2. Feasibility and Efficacy
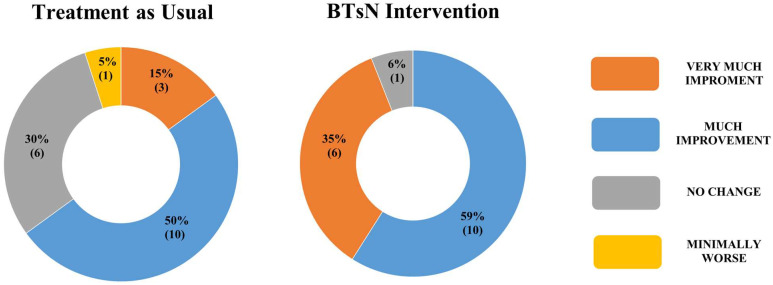
Among the final sample, the retention rate of children who started the study and completed all the 48 sessions was 100% in both groups. The use of a semi-immersive VR instrument was well accepted by patients; there were no episodes of fear or requests to leave the room of BTsN. Moreover, no considerable alternations or side effects were observed among the BTsN-I group. Clinically, there were no significant differences between the GQ at T0. Quite the opposite, there was a statistically significant difference between the two groups at T1 regarding the GQ (t = 2.44; p = 0.02). As showed in Table 3, the experimental patients had significant T0–T1 differences in General Quotient Griffiths III score (p = 0.04), whereas emerged significant T0-T1 changes in Eye and hand coordination scale for controls (p < 0.01). ANCOVA results are reported in Table 4 for GQ, Foundations of Learning, Language and Communication and Eye and Hand Coordination. Assumption of homogeneity of variance was not met for Personal–Social Emotional and Gross Motor. Such results confirmed that the effect of the two treatments was significantly different in GQ (t = 2.44; p = 0.02), but also in Foundations of Learning (t = 3.66; p < 0.01), and ANOVA results showed a significance of the interaction term “outcome score at baseline * categorical variable” in these two models, (t = 2.49; p = 0.02) and (t = 3.73; p < 0.01), respectively. As concerning the CGI-I scale, we found a significant difference between the two groups at T1 (χ2 (3) = 9.16; p = 0.03). The distribution of raw scores related to CGI-Improvement is detailed in Figure 3.
Table 3.
Statistical comparisons of clinical scores between baseline (T0) and follow-up (T1).
| Intervention | Griffiths III | BASELINE—T0 | FOLLOW-UP—T1 | p-Value |
|---|---|---|---|---|
| BTsN-I | General Quotient | 69.0 (65.0–76.0) | 75.0 (61.0–87.0) | 0.04 |
| Foundations of Learning | 78.0 (72.0–85.0) | 80.0 (74.0–87.0) | 0.49 | |
| Language and Communication | 64.0 (53.0–77.0) | 58.0 (50.0–78.0) | 0.83 | |
| Eye and Hand Coordination | 83.0 (70.0–89.0) | 80.0 (73.0–91.0) | 0.28 | |
| Personal–Social–Emotional | 75.0 (69.0–88.0) | 81.0 (69.0–90.0) | 0.28 | |
| Gross Motor | 84.0 (69.0–96.0) | 91.0 (83.0–93.0) | 0.59 | |
| TAU | General Quotient | 58.0 (49.0–77.2) | 62.0 (49.0–89.0) | 0.13 |
| Foundations of Learning | 70.0 (61.5–82.0) | 75.5 (60.7–91.2) | 0.08 | |
| Language and Communication | 51.0 (49.0–73.2) | 52.5 (49.0–83.0) | 0.25 | |
| Eye and Hand Coordination | 68.5 (56.5–80.0) | 76.0 (67.5–89.2) | <0.01 | |
| Personal–Social–Emotional | 72.5 (49.0–86.5) | 70.0 (49.7–97.2) | 0.21 | |
| Gross Motor | 73.0 (60.5–85.0) | 75.0 (55.5–91.2) | 0.48 |
Scores are in median (first-third quartile); significant differences are in bold. Legend: BTsN-I = BTs-Nirvana system Intervention; TAU = Treatment as usual.
Table 4.
ANCOVA results for each covariance model.
| Griffiths III | Group Coefficient | Adjusted R2 | |||
|---|---|---|---|---|---|
| Estimate | Std. Error | t Value | p Value | ||
| General Quotient | 35.87 | 14.70 | 2.44 | 0.02 | 0.56 |
| Foundations of Learning | 55.61 | 15.21 | 3.66 | <0.01 | 0.56 |
| Language and Communication | −2.95 | 3.31 | −0.89 | 0.38 | 0.45 |
| Personal–Social–Emotional | −1.36 | 3.17 | −0.43 | 0.67 | 0.46 |
Significant differences between treatment effects are in bold.
Figure 3.
Graphic distribution of raw scores related to CGI-Improvement in children who have completed training with BTsN compared to children who have completed treatment as usual.
4. Discussion
This single-blind, randomized-controlled pilot study investigated the feasibility and usefulness of neuro-psychomotor therapy integrated with semi-immersive VR in GDD patients, using an innovative tool, namely BTS-Nirvana. Specifically, it evaluated the engagement and the participation rate in rehabilitation programs and the effectiveness on global development improvement of semi-immersive VR compared with treatment as usual. To our knowledge, this is the first study addressing cognitive and motor rehabilitation integrated with a semi-immersive virtual reality system in children with GDD.
Few studies in the literature involve a group of GDD patients similar to ours in age distribution [28], as well as our results support the fair acceptability and feasibility of a semi-immersive virtual game in pre-school children, documented by high participant retention rates in the experimental treatment programs and the absence of adverse events. Furthermore, the results in terms of effectiveness can be interpreted as hinting at a possible utility of semi-immersive virtual reality for the rehabilitation of children with GDD. Indeed, the clinical global improvement underlined by CGI-I scale between TAU and BTsN-I groups. This finding seems well supported by significant T0-T1 differences in the General Quotient score of BTsN-I groups, with a confirmed probability of significant difference between groups (t = 2.44; p = 0.02), also found in the Foundations of Learning subscale (t = 3.66; p < 0.01).
This last specific subscale refers to a child’s ability to learn, involving different skills, such as attention and curiosity, problem solving, and processing-speed abilities. Foundations of Learning subscale also explores the ability to understand the relationships between objects or elements and the approach needed to facilitate the learning process. In early childhood, learning means exploring, recognizing similarities and differences, and understanding cause-and-effect connections. Overall, it assesses those aspects that during early childhood are the prerequisites of learning skills and that promote academic success.
Therefore, VR technology applied to neurorehabilitation treatment at preschool age can be a very valuable tool. Some reasons that would make this system advantageous could be related to the intrinsic potential of virtual reality systems. VR can offer an immersive experience to stimulate different senses at the same time; the use of auditory and visual feedback simultaneously enhances different perceptual channels, increasing awareness of one’s body actions and movements; furthermore, the presence of body shadows during VR play may improve children to a better body consciousness, too [29]. Visual observation of one’s own movements will activate the “mirror neuron system”, and the systematic exercise based on observation and imitation may improve the development of different skills in children, as shown by the studies inherent stroke rehabilitation and cerebral palsy [30,31,32]. Nonetheless, through a computer-generated virtual world, therapeutic exercises can be transformed into engaging and fun games, increasing patient compliance with treatment. Unlike other kinds of neurorehabilitation treatments, this system involves scenarios and activities that stimulate imagination and creativity within controlled and secure environments, keeping high levels of motivation and attention during the whole session [33]. Individual motivation would facilitate neuroplasticity mechanisms [34], and is important to achieve adequate compliance with therapists.
Finally, VR-based treatments give to therapists the possibility of customized settings and interventions [35]. The possibility of personalized intervention enables the transformation of each proposed scenario in a new and different environment to explore, adapting the treatment to the child, according to clinical features and personal preferences, to better targeted treatments, fostering more targeted treatments and effective interventions [36]. It is also possible to use the same scenario to work on acquiring or upgrading different skills. Specifically, BTs-N is a versatile tool capable of adapting images, sounds, and activity to the different goals of treatment.
GDD encompasses a wide range of impairments in distinct areas, such as gross and fine motor skills, speech ability, and critical aspects of learning [37]. The studies and guidelines related to treatment in GDD are still few, but the goals of therapy are very broad, encompassing all areas of development and children’s acquisition of awareness of self and others, the knowledge of strategies to copy with novelty and difficulties, the ability to plan their own behaviors and manage the possible consequences. Moreover, it is known that early and intensive interventions can improve outcomes and developmental trajectories [38,39]. Several factors have been identified to explain the greater effectiveness of early intervention: the immaturity and brain plasticity of the young child, the possibility of improving family functioning by acting on maladaptive parent–child interactions, and, lastly, the opportunity to prevent secondary complications [40]. Child development is related to learning and plasticity mechanisms generated by experience, which lead to changes in brain network and behavior. A child exposed to attractive stimuli acquires new skills, so direct experience in a challenging environment is an important source of learning [41].
Our study showed that the VR system, combined with the usual treatment, could be helpful in enhancing cognitive and learning processes, probably due to their potential for personalization, global stimulation, and engagement. Patients with GDD have complex needs, and the aim of treatment was indeed to strengthen all the areas of neurodevelopment, allowing the acquisition of praxic and perceptive, communicative-relational, symbolic, linguistic, logical-cognitive, and motor skills. Those preliminary results demonstrated that, although there were no significant changes in individual areas, the use of semi-immersive VR can be considered a valid context for global stimulation. As this is a pilot study, the sample size is limited; however, this limitation may be overcome in a future RCT. Another limitation of our study is the heterogeneity inherent in the definition of global developmental delay; GDD is a general descriptor of a broad phenotype and can result from a variety of etiological factors. However, strict exclusion criteria for serious medical conditions have been implemented to reduce this potential bias. Finally, the large age range could constitute a limit to the interpretation of the data; for this reason, we tried to keep a non-significant difference between the groups, in order to better compare the results. Nevertheless, preliminary studies allow us to test hypotheses in the investigated issue and guide future studies, and to our knowledge, this is the first study to test and confirm the feasibility and effectiveness of cognitive and motor rehabilitation integrated with a semi-immersive VR system in children with GDD.
5. Conclusions
Our results suggest a possible utility of VR for the rehabilitation of children with GDD, both in terms of feasibility and effectiveness. In addition, VR has been shown to be more effective than TAU in improving global perceptual-cognitive skills, probably by encouraging implicit learning through exposure to a series of fun games and targeted concrete tasks. Further studies should be promoted on larger samples to confirm these results, focusing on GDD patient with long-term follow-up.
Acknowledgments
The authors gratefully acknowledge all the families who participated in this study.
Author Contributions
C.S., R.M. and E.P. participated in the study design and coordination, provided clinical oversight for data collection and interpretation, and drafted the manuscript; A.Q. and F.C. conceptualized the study and supervised the manuscript; C.D.D., M.L.F., M.T. and F.M.G. participated in data collection and processing, contributed to the literature review, and helped draft the manuscript; M.C.D.C. performed statistical analysis of the data; E.T., C.I. and A.A. contributed to the literature review and helped draft the manuscript; F.C. supervised the coordination of the study. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethical Committee IRCCS Sicilia Centro Neurolesi “Bonino-Pulejo” (protocol code 15/2019 and date of approval 5 June 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Funding Statement
This study was supported by Ministry of Health, Italy, Current Research Funds 2022.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Vasudevan P., Suri M. A clinical approach to developmental delay and intellectual disability. Clin. Med. 2017;17:558–561. doi: 10.7861/clinmedicine.17-6-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders—(DSM-V) American Psychiatric Association; Washington, DC, USA: 2014. [Google Scholar]
- 3.McDonald L., Rennie A., Tolmie J., Galloway P., McWilliam R. Investigation of global developmental delay. Arch. Dis. Child. 2006;91:701–705. doi: 10.1136/adc.2005.078147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Srour M., Mazer B., Shevell M. Analysis of Clinical Features Predicting Etiologic Yield in the Assessment of Global Developmental Delay. Pediatrics. 2006;118:139–145. doi: 10.1542/peds.2005-2702. [DOI] [PubMed] [Google Scholar]
- 5.Alderman H., Behrman J.R., Glewwe P., Fernald L., Walker S. Child and Adolescent Health and Development. 3rd ed. The International Bank for Reconstruction and Development/The World Bank; Washington, DC, USA: 2017. Evidence of Impact of Interventions on Growth and Development during Early and Middle Childhood. Chapter 7. [PubMed] [Google Scholar]
- 6.Thomaidis L., Zantopoulos G.Z., Fouzas S., Mantagou L., Bakoula C., Konstantopoulos A. Predictors of severity and outcome of global developmental delay without definitive etiologic yield: A prospective observational study. BMC Pediatr. 2014;14:40. doi: 10.1186/1471-2431-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cioni C., Sgandurra G. Normal psychomotor development. In: Dulac O., Lassonde M., Sarnat H.B., editors. Handbook of Clinical Neurology. 3rd ed. Volume 111. Elsevier B.V.; Amsterdam, The Netherlands: 2013. Pediatric Neurology Part I. [DOI] [PubMed] [Google Scholar]
- 8.Giangiacomo E., Visaggi M.C., Aceti F., Giacchetti N., Martucci M., Giovannone F., Valente D., Galeoto G., Tofani M., Sogos C. Early Neuro-Psychomotor Therapy Intervention for Theory of Mind and Emotion Recognition in Neurodevelopmental Disorders: A Pilot Study. Children. 2022;9:1142. doi: 10.3390/children9081142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caliendo M., Di Sessa A., D’Alterio E., Frolli A., Verde D., Iacono D., Romano P., Vetri L., Carotenuto M. Efficacy of Neuro-Psychomotor Approach in Children Affected by Autism Spectrum Disorders: A Multicenter Study in Italian Pediatric Population. Brain Sci. 2021;11:1210. doi: 10.3390/brainsci11091210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pournajaf S., Morone G., Goffredo M., Bonaiuti D., Franceschini M. Realtà virtuale applicata alla riabilitazione: Evidenze cliniche e prospettive future. G. Ital. Di Med. Riabil. 2021;35:30–42. [Google Scholar]
- 11.Lorusso M.L., Travellini S., Giorgetti M., Negrini P., Reni G., Biffi E. Semi-Immersive Virtual Reality as a Tool to Improve Cognitive and Social Abilities in Preschool Children. Appl. Sci. 2020;10:2948. doi: 10.3390/app10082948. [DOI] [Google Scholar]
- 12.Bohil C.J., Alicea B., Biocca F.A. Virtual reality in neuroscience research and therapy. Nature reviews. Neuroscience. 2011;12:752–762. doi: 10.1038/nrn3122. [DOI] [PubMed] [Google Scholar]
- 13.Choi J.Y., Yi S.H., Ao L., Tang X., Xu X., Shim D., Yoo B., Park E.S., Rha D.W. Virtual reality rehabilitation in children with brain injury: A randomized controlled trial. Dev. Med. Child. Neurol. 2021;63:480–487. doi: 10.1111/dmcn.14762. [DOI] [PubMed] [Google Scholar]
- 14.Liu C., Wang X., Chen R., Zhang J. The Effects of Virtual Reality Training on Balance, Gross Motor Function, and Daily Living Ability in Children with Cerebral Palsy: Systematic Review and Meta-analysis. JMIR Serious Games. 2022;10:e38972. doi: 10.2196/38972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mesa-Gresa P., Gil-Gómez H., Lozano-Quilis J., Gil-Gómez J.A. Efectiveness of virtual reality for children and adolescents with autism spectrum disorder: An evidence-based systematic review. Sensors. 2018;18:2486. doi: 10.3390/s18082486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dechsling A., Orm S., Kalandadze T., Sütterlin S., Øien R.A., Shic F., Nordahl-Hansen A. Virtual and Augmented Reality in Social Skills Interventions for Individuals with Autism Spectrum Disorder: A Scoping Review. J. Autism Dev. Disord. 2022;52:4692–4707. doi: 10.1007/s10803-021-05338-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lorenzo G., Lledó A., Arráez-Vera G., Lorenzo-Lledó A. The application of immersive virtual reality for students with ASD: A review between 1990–2017. Educ. Inf. Technol. 2018;24:127–151. doi: 10.1007/s10639-018-9766-7. [DOI] [Google Scholar]
- 18.Goharinejad S., Goharinejad S., Hajesmaeel-Gohari S., Bahaadinbeigy K. The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: An overview of relevant studies. BMC Psychiatry. 2018;22:4. doi: 10.1186/s12888-021-03632-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Luca R., Russo M., Naro A., Tomasello P., Leonardi S., Santamaria F., Latella D., Bramanti A., Silvestri G., Bramanti P., et al. Effects of virtual reality-based training with BTs-Nirvana on functional recovery in stroke patients: Preliminary considerations. Int. J. Neurosci. 2018;128:791–796. doi: 10.1080/00207454.2017.1403915. [DOI] [PubMed] [Google Scholar]
- 20.Manuli A., Maggio M.G., Tripoli D., Gullì M., Cannavò A., La Rosa G., Sciarrone F., Avena G., Calabrò R.S. Patients’ perspective and usability of innovation technology in a new rehabilitation pathway: An exploratory study in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2020;44:102312. doi: 10.1016/j.msard.2020.102312. [DOI] [PubMed] [Google Scholar]
- 21.De Luca R., Maggio M.G., Maresca G., Latella D., Cannavò A., Sciarrone F., Voi E.L., Accorinti M., Bramanti P., Calabrò R.S. Improving Cognitive Function after Traumatic Brain Injury: A Clinical Trial on the Potential Use of the Semi-Immersive Virtual Reality. Behav. Neurol. 2019;2019:9268179. doi: 10.1155/2019/9268179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maggio M.G., De Cola M.C., Latella D., Maresca G., Finocchiaro C., La Rosa G., Cimino V., Sorbera C., Bramanti P., De Luca R., et al. What About the Role of Virtual Reality in Parkinson Disease’s Cognitive Rehabilitation? Preliminary Findings From a Randomized Clinical Trial. J. Geriatr. Psychiatry Neurol. 2018;31:312–318. doi: 10.1177/0891988718807973. [DOI] [PubMed] [Google Scholar]
- 23.De Luca R., Naro A., Colucci P.V., Pranio F., Tardiolo G., Billeri L., Le Cause M., De Domenico C., Portaro S., Rao G., et al. Improvement of brain functional connectivity in autism spectrum disorder: An exploratory study on the potential use of virtual reality. J. Neural Transm. 2021;128:371–380. doi: 10.1007/s00702-021-02321-3. [DOI] [PubMed] [Google Scholar]
- 24.Ravi D.K., Kumar N., Singhi P. Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: An updated evidence-based systematic review. Physiotherapy. 2017;103:245–258. doi: 10.1016/j.physio.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Eldridge S.M., Chan C.L., Campbell M.J., Bond C.M., Hopewell S., Thabane L., Lancaster G.A. PAFS consensus group, CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239. doi: 10.1136/bmj.i5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Green E., Stroud L., O’Connell R., Bloomfield S., Cronje J., Foxcroft C., Hurter K., Lane H., Marais R., Marx C., et al. Griffiths Scales of Child Development. 3rd ed. Hogrefe Ltd.; Oxford, UK: 2017. Manual Griffiths III—Part II: Administration and Scoring. [Google Scholar]
- 27.Busner J., Targum S.D. The clinical global impressions scale: Applying a research tool in clinical practice. Psychiatry. 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 28.Hsieh R.L., Lee W.C., Lin J.H. The Impact of Short-Term Video Games on Performance among Children with Developmental Delays: A Randomized Controlled Trial. PLoS ONE. 2016;11:e0149714. doi: 10.1371/journal.pone.0149714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Russo M., De Luca R., Naro A., Sciarrone F., Aragona B., Silvestri G., Manuli A., Bramanti A., Casella C., Bramanti P., et al. Does body shadow improve the efficacy of virtual reality-based training with BTS NIRVANA?: A pilot study. Medicine. 2017;96:e8096. doi: 10.1097/MD.0000000000008096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buccino G., Solodkin A., Small S.L. Functions of the mirror neuron system: Implications for neurorehabilitation. Cogn. Behav. Neurol. 2006;19:55–63. doi: 10.1097/00146965-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Kommalapati R., Michmizos K.P. Virtual reality for pediatric neuro-rehabilitation: Adaptive visual feedback of movement to engage the mirror neuron system. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016;2016:5849–5852. doi: 10.1109/EMBC.2016.7592058. [DOI] [PubMed] [Google Scholar]
- 32.Shaffer J. Neuroplasticity and Clinical Practice: Building Brain Power for Health. Front. Psychol. 2016;7:1118. doi: 10.3389/fpsyg.2016.01118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montana J.I., Tuena C., Serino S., Cipresso P., Riva G. Neurorehabilitation of Spatial Memory Using Virtual Environments: A Systematic Review. J. Clin. Med. 2019;8:1516. doi: 10.3390/jcm8101516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coco-Martin M.B., Piñero D.P., Leal-Vega L., Hernández-Rodríguez C.J., Adiego J., Molina-Martín A., de Fez D., Arenillas J.F. The Potential of Virtual Reality for Inducing Neuroplasticity in Children with Amblyopia. J. Ophthalmol. 2020;2020:7067846. doi: 10.1155/2020/7067846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiss P.L., Katz N. The potential of virtual reality for rehabilitation. J. Rehabil. Res. Dev. 2004;41:7–10. [PubMed] [Google Scholar]
- 36.Cucinotta F., Ricciardello A., Turriziani L., Calabrese G., Briguglio M., Boncoddo M., Bellomo F., Tomaiuolo P., Martines S., Bruschetta M., et al. FARP-1 deletion is associated with lack of response to autism treatment by early start denver model in a multiplex family. Mol. Genet. Genom. Med. 2020;8:e1373. doi: 10.1002/mgg3.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan I., Leventhal B.L. StatPearls. StatPearls Publishing; St. Petersburg, FL, USA: 2023. Developmental Delay. [PubMed] [Google Scholar]
- 38.Shevell M., Majnemer A., Platt R.W., Webster R., Birnbaum R. Developmental and functional outcomes in children with global developmental delay or developmental language impairment. Dev. Med. Child Neurol. 2005;47:678–683. doi: 10.1017/S0012162205001386. [DOI] [PubMed] [Google Scholar]
- 39.Dobos A.E., Jr., Dworkin P.H., Bernstein B.A. Pediatricians’ approaches to developmental problems: Has the gap been narrowed? J. Dev. Behav. Pediatr. 1994;15:34–38. doi: 10.1097/00004703-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Dworkin P.H. Promoting development through child health services. Introduction to the Help Me Grow roundtable. J. Dev. Behav. Pediatr. 2006;27((Suppl. 1)):S2–S52. doi: 10.1097/00004703-200602001-00002. [DOI] [PubMed] [Google Scholar]
- 41.Fandakova Y., Hartley C.A. Mechanisms of learning and plasticity in childhood and adolescence. Dev. Cogn. Neurosci. 2020;42:100764. doi: 10.1016/j.dcn.2020.100764. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.