Abstract
Introduction
During the COVID-19 pandemic, the workload of healthcare workers managing the disease, increased significantly. The objective of this review is to determine the anxiety and depression prevalence among healthcare workers during the pandemic period.
Methods
We searched systematically the literature in five electronic databases such as PubMed, CINAHL, ScienceDirect, MEDLINE, and Cochrane COVID-19 study register. The last online research was performed in May 2022. We included only cross-sectional studies and performed a meta-analysis of pooled prevalence. Publication bias was assessed with a funnel plot and Egger’s and Begg’s tests. A random effect was applied and heterogenicity I2 was calculated. Quality assessment of included studies was performed using the Joanna Briggs Institute tool.
Results
In this review, we included 14 cross-sectional studies comprising 7780 healthcare workers. Participants were from the whole spectrum of healthcare workers. The pooled prevalence of depression was 33.8% (95% CI: 24.6 – 43.6), heterogenicity I2: 98.69%. The pooled prevalence of anxiety was 41.3% (95% CI: 30.2 – 52.9), heterogenicity I2: 99.01%.
Conclusion
One-third of healthcare workers suffered from depression, and more than one-third suffered from anxiety during the COVID-19 pandemic. Increased measures of surveillance of mental health should have been taken, as well as the support of healthcare workers running a high risk of psychological distress during the COVID-19 pandemic.
Keywords: depression, anxiety, burn-out, emotional distress, fear, health care workers, nurses, resident, doctor, physician, coronavirus, COVID-19, SARS-COV-2
Introduction
The COVID-19 pandemic was a unique challenge, and, as in any disaster, effective communication is of great importance [1]. The risk of COVID-19 infection may cause significant psychosocial stress for medical staff [2]. Furthermore, during critical situations like flu pandemics, Health Care Workers (HCWs) are at risk of developing psychological distress with an impact on their health [3]. Residents stated that COVID-19 influenced their surgical training in 85.2% of responders and only 5% of the residents answered that the COVID-19 pandemic did not affect their surgical training in the operative room (OR). Moreover, residents subjectively received less education and believed they needed an extension of their surgical training [4].
Methods
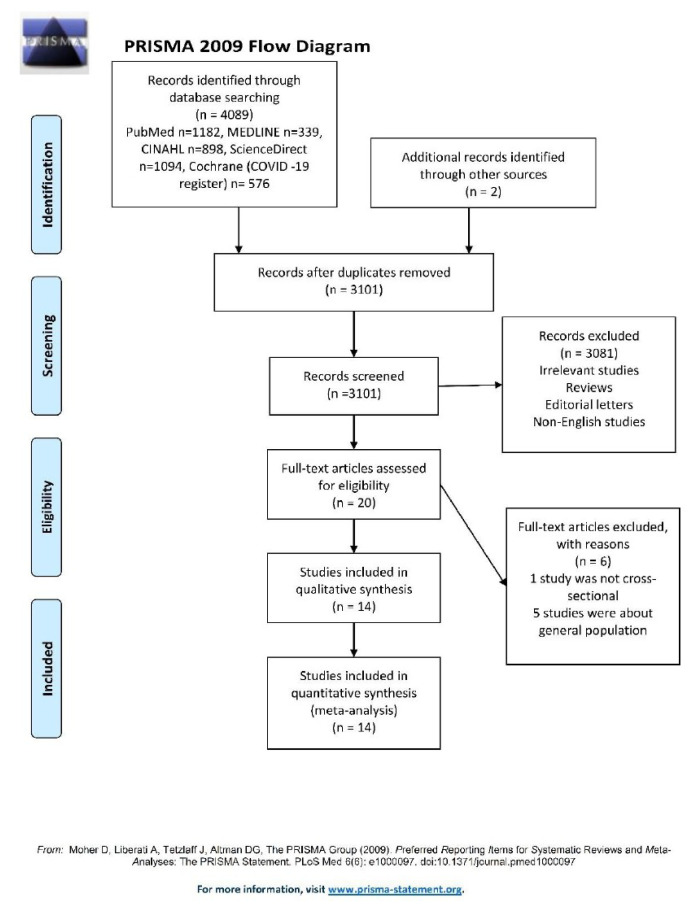
This study adheres to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2009 checklist [5].
Inclusion and exclusion criteria
The inclusion criteria were the following: 1. Studies are designed as cross-sectional. 2. The studies must include health care workers (HCW). 3. Studies in the English language. 4. Studies have as objective the impact of the COVID-19 pandemic on HCWs (anxiety, depression) based on appropriate measurement tools. The exclusion criteria were set as follows: 1. Case reports, review studies, intervention studies. 2. Studies that include professions other than health care workers. 3. Studies that are not in the English language. 4. Studies that do not have an emotional impact on HCWs.
Information resources and search strategy
We searched the electronic databases PubMed, ScienceDirect, MEDLINE, CINAHL, and Cochrane Library. The last date of online research was in May 2022.
We used the keywords ‘depression’,’ anxiety, ‘burn-out’, ‘emotional distress’, ‘fear’, ‘health care workers’, ‘nurses’, ‘resident’, ‘doctor’,’ physician’, ‘coronavirus’, ‘COVID-19’, ‘SARS-COV-2’
Selection process and data extraction process
The screening of the studies was performed independently by two authors. First, one author screened the abstracts. Another author screened the abstracts independently.
Any disagreement was resolved by discussion. Data collected were about 1. Study design. 2. Country of the study. 3. Study population characteristics (age, size of study arms, the position of health providers.
Effect measures
In this review, we measured two outcomes. 1. The prevalence of anxiety among healthcare workers caused by COVID-19 and 2. The prevalence of depression among healthcare workers caused by COVID-19. We used the Freeman-Tukey transformation [6] to pool the results.
Evaluation of the quality of the included studies
Two authors worked independently on the quality assessment of the included studies. We used the Joanna Briggs Institute tool [7]. The Joanna Briggs Institute tool consists of 8 items, and it is suitable for a cross-sectional study’s quality assessment. Any disagreement in the assessment process was resolved by discussion.
Statistical methods
In this review, we used the MedCalc [8] statistical software to perform a meta-analysis. Data used from the included studies was about sample size and population of HCWs affected in each study. To pool the prevalence of studies included in the meta-analysis, we used the Freeman-Tukey transformation method [6]. We used a random-effects model (DerSimonian and Laird method) [9] to calculate the pooled prevalence from multiple studies.
Publication bias
For publication bias, we used Begg’s test [10] and Egger’s test [11]. Begg’s test [10] assesses the significant correlation between the ranks of the effect estimates and the ranks of their variances. Egger’s test [11] assesses the relationship between the standardized effect estimates and the standard error (SE) using linear regression. Funnel plots were used also to assess any publication bias [12].
Results
In this review, 14 studies were included (Table I). The flow diagram in figure 1 shows the screening process and the study selection.
Table I.
Characteristics of included studies.
| Author/Year | Country | Study Design/Participants | Sample size | Male (%) | Mean age | Depression % (n) | Anxiety % (n) |
|---|---|---|---|---|---|---|---|
| Barua et al., 2020 [13] | Bangladesh | Cross-sectional/Frontline doctors | 370 | 60.3% | 30.5 | 38.3% (142) | 36.4% (135) |
| Chatterjee et al., 2020 [14] | India | Cross-sectional/Medical doctors | 152 | 78.3% | 42.05 | 34.8% (53) | 39.4% (60) |
| Dal’Bosco et al., 2020 [15] | South America | Cross-sectional/Nurse | 88 | 10.2% | 21–30 (42%) 31–40 (36.4%) > 40 (21.6%) |
25% (22) | 48.8% (43) |
| Holton et al., 2020 [16] | Australia. | Cross-sectional/Nurses n=391; Doctors, n=138, AH staff n=139 | 668 | 14% | 40 | 20.6% (138) | 20.6% (138) |
| Khanal et al., 2020 [17] | Nepal | Cross-sectional/Doctor n = 161, Nurses n = 167, Other n = 147 | 475 | 47.4% | 28.2 | 37.4% (178) | 41.8% (199) |
| Mathur et al., 2020 [18] | India | Cross-sectional/Doctors = 174, Nurses=26 | 200 | 69% | 42.1 | 17% (34) | 19.5% (39) |
| Nasrullah et al., 2021 [19] | Indonesia | Cross-sectional/Not specified | 644 | 24.8% | 20–29 (32.3%) 30–39 (39.1%) 40–49 (23.9%) >50 (4.7%) |
23.4% (151) | 65.6% (423) |
| Ning et al., 2020 [20] | China | Cross-sectional/Doctors n = 317, Nurses n = 295 | 612 | 27.1% | > 40 (20.1%) <40 (79.9%) |
25% (153) | 16.3% (100) |
| Pan et al., 2020 [21] | China | Cross-sectional/Doctor n = 42, Nurses n = 148, Other n=4 | 194 | 18.6% | < 30 (44.8%) >30 (33.3%) >50 (21.9%) |
37.6% (73) | 32.4% (63) |
| Pouralizadeh et al., 2020 [22] | Iran | Cross-sectional/Nurses | 441 | 4.8% | 36.34 | 70.9% (313) | 73.4% (324) |
| Prasad et al., 2020 [23] | USA | Cross-sectional/Nurses=248, administrative staff=63, practice providers=36 | 347 | 9.2% | 26–30 (34.3%) 31–35 (21.3%) 36–40 (9.5%) >40 (34.9%) |
22.7% (79) | 69.4% (241) |
| Que et al., 2020 [24] | China | Cross-sectional/Physicians n=860, Medical residents n=913, Nurses n=208, Other n=304 | 2285 | 30.9% | 31.06 | 44.3% (1014) | 46.3% (1052) |
| Si et al., 2020 [25] | China | Cross-sectional/Doctor=377, Nurse=211, Other=275 | 863 | 29.3% | ≤ 29 (32.1%) 30–39 (45.2%) 40–49 (16.8%) ≥ 50 (5.9%) |
13.5% (117) | 13.9% (120) |
| Wankowicz et al., 2020 [26] | Poland | Cross-sectional/Not otherwise specified | 441 | Frontline HCWs: 43.69% Second-line HCWs: 51.49% |
Frontline HCWs:40.47 Second-line HCWs:40.05 |
70.7% (312) | 64.3% (284) |
AH: Allied health; HCW: Health Care Workers.
Figure 1.
PRISMA Flow Diagram.
Risk of bias assessment (Table II)
Table II.
Risk of bias assessment of included studies according to Joanna Briggs Institute tool [7].
| Were the criteria for inclusion in the sample clearly defined? | Were the study subjects and the setting described in detail? | Was the exposure measured in a valid and reliable way? | Were objective standard criteria used for the measurement of the condition? | Were confounding factors identified? | Were strategies to deal with confounding factors stated? | Were the outcomes measured in a validating reliable way? | Was appropriate statistical analysis used? | |
|---|---|---|---|---|---|---|---|---|
| Barua et al., 2020 [13] | Y | Y | Y | Y | Y | N | Y | Y |
| Chatterjee et al., 2020 [14] | Y | Y | Y | Y | N | N | Y | Y |
| Dal’Bosco et al., 2020 [15] | Y | Y | Y | Y | N | N | Y | Y |
| Holton et al., 2021 [16] | Y | Y | Y | Y | N | N | Y | Y |
| Khanal et al., 2020 [17] | Y | Y | Y | Y | Y | N | Y | Y |
| Mathur et al., 2020 [18] | Y | Y | Y | Y | N | N | Y | Y |
| Nasrullah et al., 2021 [19] | Y | Y | Y | Y | Y | N | Y | Y |
| Ning et al., 2020 [20] | Y | Y | Y | Y | N | N | Y | Y |
| Pan et al., 2020 [21] | Y | Y | Y | Y | Y | N | Y | Y |
| Pouralizad et al., 2020 [22] | Y | Y | Y | Y | Y | N | Y | Y |
| Prasad et al., 2020 [23] | Y | Y | Y | Y | Y | N | Y | Y |
| Que et al., 2020 [24] | Y | Y | Y | Y | Y | N | Y | Y |
| Si et al., 2020 [25] | Y | Y | Y | Y | N | N | Y | Y |
| Wankowicz et al., 2020 [26] | Y | Y | Y | Y | Y | N | Y | Y |
Y: Yes; N: No
Meta-Analysis
Depression (Table III)
Table III.
Meta-analysis of depression prevalence among HCWs.
| Study | Sample size | Proportion (%) | 95% CI | Weight (%) | |
|---|---|---|---|---|---|
| Fixed | Random | ||||
| Barua et al., 2020 [13] | 370 | 38.378 | 33.399 to 43.546 | 4.76 | 7.17 |
| Chatterjee et al., 2020 [14] | 152 | 34.868 | 27.328 to 43.012 | 1.96 | 6.99 |
| Dal’ Bosco et al., 2020 [15] | 88 | 25.000 | 16.378 to 35.368 | 1.14 | 6.78 |
| Holton et al., 2021 [16] | 668 | 20.659 | 17.649 to 23.930 | 8.58 | 7.23 |
| Khanal et al., 2020 [17] | 475 | 37.474 | 33.105 to 41.999 | 6.11 | 7.20 |
| Mathur et al., 2020 [18] | 200 | 17.000 | 12.070 to 22.937 | 2.58 | 7.06 |
| Nasrullah et al., 2021 [19] | 644 | 23.447 | 20.225 to 26.915 | 8.28 | 7.23 |
| Ning et al., 2020 [20] | 612 | 25.000 | 21.615 to 28.628 | 7.87 | 7.22 |
| Pan et al., 2020 [21] | 194 | 37.629 | 30.791 to 44.851 | 2.50 | 7.05 |
| Pouralizadeh et al., 2020 [22] | 441 | 70.975 | 66.495 to 75.172 | 5.67 | 7.19 |
| Prasad et al., 2020 [23] | 347 | 22.767 | 18.459 to 27.545 | 4.46 | 7.16 |
| Que et al., 2020 [24] | 2285 | 44.376 | 42.326 to 46.441 | 29.33 | 7.28 |
| Si et al., 2020 [25] | 863 | 13.557 | 11.343 to 16.024 | 11.09 | 7.25 |
| Wankowicz et al., 2020 [26] | 441 | 70.748 | 66.260 to 74.956 | 5.67 | 7.19 |
| Total (fixed effects) | 7780 | 35.003 | 33.943 to 36.074 | 100.00 | 100.00 |
| Total (random effects) | 7780 | 33.820 | 24.660 to 43.637 | 100.00 | 100.00 |
| Test for heterogeneity | |||||
| Q | 993,0064 | ||||
| DF | 13 | ||||
| Significance level | P < 0,0001 | ||||
| I2 (inconsistency) | 98.69% | ||||
| 95% CI for I2 | 98.38 to 98.94 | ||||
| Publication bias | |||||
| Egger’s test | |||||
| Intercept | −2,2943 | ||||
| 95% CI | −16,0003 to 11,4118 | ||||
| Significance level | P = 0.7217 | ||||
| Begg’s test | |||||
| Kendall’s Tau | 0,1547 | ||||
| Significance level | P = 0.4409 | ||||
The vertical line represents the pooled prevalence. The Egger’s test is P = 0.7217 and Begg’s test is P = 0.4409 indicating no publication bias. Heterogeneity I2 was 98.69% (Figure 2).
Figure 2.
Funnel plot of HCWs depression prevalence.
The squares indicate the event rate of each study. The diamond indicates the pooled prevalence and 95% confidence intervals. The pooled prevalence of depression among healthcare workers was 33.82% (95% CI: 24.66 to 43.63) applying random effects DerSimonian-Laird method [9] (Figure 3).
Figure 3.
Forest plot of HCWs depression prevalence.
Anxiety (Table IV)
Table IV.
Meta-analysis of anxiety prevalence among HCWs.
| Study | Sample size | Proportion (%) | 95% CI | Weight (%) | |
|---|---|---|---|---|---|
| Fixed | Random | ||||
| Barua et al., 2020 [13] | 370 | 36.486 | 31.572 to 41.619 | 4.76 | 7.16 |
| Chatterjee et al., 2020 [14] | 152 | 39.474 | 31.650 to 47.716 | 1.96 | 7.03 |
| Dal’Bosco et al., 2020 [15] | 88 | 48.864 | 38.052 to 59.754 | 1.14 | 6.86 |
| Holton et al., 2021 [16] | 668 | 20.659 | 17.649 to 23.930 | 8.58 | 7.21 |
| Khanal et al., 2020 [17] | 475 | 41.895 | 37.415 to 46.476 | 6.11 | 7.19 |
| Mathur et al., 2020 [18] | 200 | 19.500 | 14.249 to 25.679 | 2.58 | 7.08 |
| Nasrullah et al., 2021 [19] | 644 | 65.683 | 61.873 to 69.349 | 8.28 | 7.21 |
| Ning et al., 2020 [20] | 612 | 16.340 | 13.497 to 19.512 | 7.87 | 7.20 |
| Pan et al., 2020 [21] | 194 | 32.474 | 25.941 to 39.552 | 2.50 | 7.08 |
| Pouralizadeh et al., 2020 [22] | 441 | 73.469 | 69.087 to 77.534 | 5.67 | 7.18 |
| Prasad et al., 2020 [23] | 347 | 69.452 | 64.311 to 74.259 | 4.46 | 7.16 |
| Que et al., 2020 [24] | 2285 | 46.039 | 43.980 to 48.109 | 29.33 | 7.25 |
| Si et al., 2020 [25] | 863 | 13.905 | 11.665 to 16.395 | 11.09 | 7.22 |
| Wankowicz et al., 2020 [26] | 441 | 64.399 | 59.732 to 68.872 | 5.67 | 7.18 |
| Total (fixed effects) | 7780 | 40.608 | 39.515 to 41.709 | 100.00 | 100.00 |
| Total (random effects) | 7780 | 41.359 | 30.272 to 52.908 | 100.00 | 100.00 |
| Test for heterogeneity | |||||
| Q | 1312,1849 | ||||
| DF | 13 | ||||
| Significance level | P < 0.0001 | ||||
| I2 (inconsistency) | 99.01% | ||||
| 95% CI for I2 | 98.80 to 99.19 | ||||
| Publication bias | |||||
| Egger’s test | |||||
| Intercept | 0.8572 | ||||
| 95% CI | −14.9762 to 16.6907 | ||||
| Significance level | P = 0.9081 | ||||
| Begg’s test | |||||
| Kendall’s Tau | 0.1105 | ||||
| Significance level | P = 0.5820 | ||||
The vertical line represents the pooled prevalence. The Egger’s test is P = 0.9081 and Begg’s test is P = 0.5820 indicating no publication bias. Heterogeneity I2 was 99.01% (Figure 4).
Figure 4.
Funnel plot of HCWs anxiety prevalence.
The squares indicate the event rate of each study. The diamond indicates the pooled prevalence and 95% confidence intervals. The pooled prevalence of anxiety among healthcare workers was 41,35% (95% CI: 30.27 to 52.90) applying random effects DerSimonian-Laird method [9] (Figure 5).
Figure 5.
Forest plot of HCWs anxiety prevalence.
Discussion
In this review, we included 14 cross-sectional studies comprising 7780 healthcare workers. The population of participants covers the whole spectrum of healthcare professionals (medical doctors, trainees, nurses, administrative staff). Among the studies included, 10 were from Asia, 1 from USA, 1 from Europe, 1 from Australia and 1 from South America. A comprehensive search strategy was applied in five electronic databases such as PubMed, Cochrane COVID-19 study register, CINAHL, MEDLINE, and ScienceDirect. After the selection of relevant studies, we proceeded to quality and risk of bias assessment using the Johana-Biggs [7] tool. We did not observe a serious risk of bias in the included studies. We proceeded to statistical analysis to pool the results. MedCalc statistical software [8] was used to perform prevalence pooling. Our results are comparable to other published reviews. Anxiety was higher, with a prevalence of 41.3% (95% CI: 30.2 – 52.9) and depression of 33.8% (95% CI: 24.6 – 43.6). We used the random effect DerSimonian-Laird method [9] in our results due to high heterogeneity to extract a generalized conclusion.
Heterogenicity was high in our review, like in other meta-analyses. Possible explanations are the different characteristics of participants, work environment, and screening tools.
Our results are comparable to other reviews. In the meta-analysis of Ching et al [27], the prevalence of healthcare workers affected by depression was 37.5% (95% CI: 33.8–41.3) and anxiety was 39.7 (95% CI: 34.3–45.1). Furthermore, in the same study [27] the prevalence of stress was 36.4% (95% CI: 23.2–49.7), fear was 71.3% (95% CI: 54.6–88.0), and burnout was 68.3% (95% CI: 54.0–82.5). The authors recommend urgent actions to support healthcare workers to reduce the psychological distress during the COVID-19 pandemic. In another meta-analysis, by Saragih et al [28], the prevalence of anxiety was 40% (95% CI: 29–52%) and the prevalence of depression was 37% (95% CI: 29–45%). The prevalence of post-traumatic stress was 49% (95% CI: 22–75%), and distress was 37% (95% CI: 25–50%). The authors recommend to all relevant policymakers and stakeholders act to reduce the psychological impact on healthcare workers’ mental health. In the meta-analysis of Li et al [29] overall prevalence depression was 21.7% (95% CI, 18.3%–25.2%), of anxiety 22.1% (95% CI, 18.2%–26.3%) and of post-traumatic distress 21.5% (95% CI, 10.5%–34.9%). The authors recommend urgent measures to support the psychological well-being of health care workers.
There are many factors that can explain anxiety and depression. According to Saragih et al [28], several factors related to anxiety, such as the fear of becoming infected by COVID-19 and spreading the virus to their relatives, and the lack of confidence to cope with stress. Moreover, the possibility to be stigmatized by society, change work duties, and overtime work exacerbated the risk of anxiety.
Furthermore, factors related to depression were working in a high-risk environment and again the possibility to get infected and spreading the infection.
It is important to consider that healthcare providers are under constant pressure to provide high-quality healthcare services, and this becomes another challenge for all healthcare workers [30].
Limitations of evidence included and the review process
In this review, we faced several limitations. First, although we performed a meta-analysis about psychological stress on healthcare workers, included studies were not specific to nurses, physicians, residents, or other personnel. We did not perform analysis specifically for any working group, rather we included all working groups of health care workers in a united statistical analysis. Second, confounding factors may have an unspecified impact on the psychological stress percentage measured in included studies. Third, high heterogenicity was observed among included studies.
Three of the studies had a population of more than a thousand participants, in contrast to seven studies that included less than five hundred participants. Fourth, even if we performed a research with a comprehensive search strategy on five electronic databases, we may have missed several relevant studies. Fifth, most of the studies included were performed in Asia, thus it is difficult to generalize the results.
Implications of the results for practice, policy, and future research
Our review shows that COVID 19 had a significant psychological impact on healthcare workers. The analysis of the situation indicates that healthcare workers are under psychological stress that reduces the quality of their life. The increased workload, the critical care of the patients as well as the increased number of night shifts, are major factors that caused burn-out, anxiety, depression, and post-traumatic distress to the healthcare workers. Furthermore, the fear of infection was another factor of stress, not only for the frontline but also for all healthcare workers.
Healthcare workers must be protected from psychological stress and its impact on their working efficiency and the quality of their life. We suggest continuous monitoring, especially of those working in the critical care of patients. Monitoring should be concentrated on the assessment of the psychological wellness of healthcare workers at regular time points and the early recognition of signs of exhaustion, burn-out, depression, anxiety, and post-traumatic distress. Dialogue and consulting between healthcare workers and supervisors should be established discretely, to achieve psychological wellness and psychological stress reduction.
Future research should concentrate on integrated tools creation of mental surveillance during periods of increased psychological stress, such as the COVID 19 era. Regular questionnaires for psychological assessment, personal or group dialogue, and psychological support, should be part of an integrated tool in the future.
Conclusion
We conclude that the COVID-19 pandemic affected the mental health of healthcare workers. The prevalence of anxiety was higher, with more than one-third of healthcare workers affected, and one-third affected by depression. We strongly suggest continuous mental health surveillance of healthcare workers during the COVID-19 pandemic to take the necessary measures to protect and support them. Interventions from all policy makers are needed in this direction.
References
- 1.Holtzclaw T, Newman SD, Dwyer M, Simpson J, Goodwin T. Coronavirus Disease 2019 in the Emergency Department: Establishing an Interprofessional Incident Command System. J Emerg Nurs. 2022;48:477–483. doi: 10.1016/j.jen.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang L, Lin G, Tang L, Yu L, Zhou Z. Special attention to nurses’ protection during the COVID-19 epidemic. Crit Care. 2020;24:120. doi: 10.1186/s13054-020-2841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barello S, Falcó-Pegueroles A, Rosa D, Tolotti A, Graffigna G, Bonetti L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: a rapid review. Int J Public Health. 2020;65:1205–1216. doi: 10.1007/s00038-020-01463-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poelmann FB, Koëter T, Steinkamp PJ, Vriens MR, Verhoeven B, Kruijff S. The immediate impact of the coronavirus disease 2019 (COVID-19) pandemic on burn-out, work-engagement, and surgical training in the Netherlands. Surgery. 2021;170:719–726. doi: 10.1016/j.surg.2021.02.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman MF, Tukey JW. Transformations Related to the Angular and the Square Root. Ann Math Stat. 1950;21:607–611. [Google Scholar]
- 7.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetc R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI. 2020. [Google Scholar]
- 8.Schoonjans F. MedCalc. MedCalc Software; 2022. Meta-analysis: proportion. [Google Scholar]
- 9.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 10.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 11.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J. Clin. Epidemiol. 2001;54:1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 13.Barua L, Zaman MS, Omi FR, Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Res. 2020;9:1304. doi: 10.12688/f1000research.27189.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chatterjee SS, Bhattacharyya R, Bhattacharyya S, Gupta S, Das S, Banerjee BB. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J Psychiatry. 2020;62:257–265. doi: 10.4103/psychiatry.IndianJPsychiatry_333_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dal’Bosco EB, Floriano LSM, Skupien SV, Arcaro G, Martins AR, Anselmo ACC. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev Bras Enferm. 2020;73(Suppl 2):e20200434. doi: 10.1590/0034-7167-2020-0434. [DOI] [PubMed] [Google Scholar]
- 16.Holton S, Wynter K, Trueman M, Bruce S, Sweeney S, Crowe S, et al. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust Health Rev. 2021;45:297–305. doi: 10.1071/AH20203. [DOI] [PubMed] [Google Scholar]
- 17.Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health. 2020;16:89. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathur S, Sharma D, Solanki RK, Goyal MK. Stress-related disorders in health-care workers in COVID-19 pandemic: A cross-sectional study from India. Ind J Med Spec. 2020;11:180–184. [Google Scholar]
- 19.Nasrullah D, Natsir M, Twistiandayani R, Rohayani L, Siswanto S, Sumartyawati NM, et al. Psychological impact among health workers in effort to facing the COVID-19 in Indonesia. Int J Public Health Sci (IJPHS) 2021;10:181. [Google Scholar]
- 20.Ning X, Yu F, Huang Q, Li X, Luo Y, Huang Q, et al. The mental health of neurological doctors and nurses in Hunan Province, China during the initial stages of the COVID-19 outbreak. BMC Psychiatry. 2020;20:436. doi: 10.1186/s12888-020-02838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan X, Xiao Y, Ren D, Xu ZM, Zhang Q, Yang LY, et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: A cross-sectional survey. Asia Pac Psychiatry. 2022;14:e12427. doi: 10.1111/appy.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pouralizadeh M, Bostani Z, Maroufizadeh S, Ghanbari A, Khoshbakht M, Alavi SA, et al. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: A web-based cross-sectional study. Int J Afr Nurs Sci. 2020;13:100233. doi: 10.1016/j.ijans.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prasad A, Civantos AM, Byrnes Y, Chorath K, Poonia S, Chang C, et al. Snapshot Impact of COVID-19 on Mental Wellness in Nonphysician Otolaryngology Health Care Workers: A National Study. OTO Open. 2020;4:2473974X20948835. doi: 10.1177/2473974X20948835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr. 2020;33:e100259. doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9:113. doi: 10.1186/s40249-020-00724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wańkowicz P, Szylińska A, Rotter I. Assessment of Mental Health Factors among Health Professionals Depending on Their Contact with COVID-19 Patients. Int J Environ Res Public Health. 2020;17:5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ching SM, Ng KY, Lee KW, Yee A, Lim PY, Ranita H, et al. Psychological distress among healthcare providers during COVID-19 in Asia: Systematic review and meta-analysis. PLoS One. 2021;16:e0257983. doi: 10.1371/journal.pone.0257983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int J Nurs Stud. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16:e0246454. doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kourkouta L, Iliadis C, Sialakis C, Adamakidou T, Ouzounakis P, Kleisiaris C. Quality of health services. World Journal of Advanced Research and Reviews. 2021;12:498–502. [Google Scholar]