Abstract
BACKGROUND:
Pregnant veterans with post-traumatic stress disorder (PTSD) are at increased risk for spontaneous preterm birth, yet the underlying reasons are unclear. We examined factors associated with spontaneous preterm birth among pregnant veterans with active PTSD.
METHODS:
This was an observational study of births from administrative databases reimbursed by the Veterans Health Association (VA) between 2005 and 2015. Singleton livebirths among veterans with active PTSD within 12 months prior to childbirth were included. The primary outcome was spontaneous preterm birth. Maternal demographics, psychiatric history, and pregnancy complications were evaluated as exposures. Covariates significant on bivariate analysis, as well as age and race/ethnicity as a social construct, were included in multivariable logistic regression to identify factors associated with spontaneous preterm birth. Additional analyses stratified significant covariates by the presence of active concurrent depression and explored interactions between antidepressant use and preeclampsia.
RESULTS:
Of 3,242 eligible births to veterans with active PTSD, 249 (7.7%) were spontaneous preterm births. The majority of veterans with active PTSD (79.1%) received some type of mental health treatment, and active concurrent depression was prevalent (61.4%). Preeclampsia/eclampsia (adjusted odds ratio [aOR] 3.30, 95% confidence interval [CI] 1.67-6.54) and ≥6 antidepressant medication dispensations within 12 months prior to childbirth (aOR 1.89, 95% CI 1.29-2.77) were associated with spontaneous preterm birth. No evidence of interaction was seen between antidepressant use and preeclampsia on spontaneous preterm birth (p=0.39). Findings were similar when stratified by active concurrent depression.
CONCLUSION:
Among veterans with active PTSD, preeclampsia/eclampsia and ≥6 antidepressant dispensations were associated with spontaneous preterm birth. While the results do not imply that people should discontinue needed antidepressants during pregnancy in veterans with PTSD, research into these factors might inform preterm birth prevention strategies for this high-risk population.
Keywords: Post-traumatic stress disorder, perinatal mental health, spontaneous preterm birth
INTRODUCTION:
Pregnant people with post-traumatic stress disorder (PTSD) are at increased risk of spontaneous preterm birth, which accounts for the majority of neonatal morbidity and mortality in the United States (Cook et al., 2018; Goldenberg et al., 2008; Sanjuan et al., 2021; Shaw et al., 2014; Shaw, Nelson, et al., 2018; Yonkers et al., 2014). Among people with active PTSD, an excess of 2 spontaneous preterm births per 100 births has been reported (Shaw et al., 2014). However, the mechanisms driving this risk have not been examined. Characterizing clinical factors contributing to spontaneous preterm birth is critical to developing prevention strategies.
While factors such as multiple gestation are known to increase the risk of spontaneous preterm birth in the general population (Goldenberg et al., 2008), little is known about how factors unique to people with psychiatric disease – such as engagement in psychotherapy or medication use – contribute to this risk. For example, treatment of underlying psychiatric disease with medications or psychotherapy might improve disease control and reduce pregnancy risks; alternatively, actively receiving mental health treatments may also be a proxy for greater disease severity and be associated with increased risks. The importance of these psychiatric factors has been suggested previously, but many studies are limited by a low prevalence of PTSD (Cook et al., 2018; Rogal et al., 2007; Yonkers et al., 2011). Investigating the impact of these characteristics on spontaneous preterm birth rates among a population with a high prevalence of PTSD would be a novel approach to better understanding risks and associations. Furthermore, a large dataset with granular information on other demographic or obstetric factors known to be related to spontaneous singleton preterm birth – such as maternal demographics, socioeconomic factors, preeclampsia, and substance use (ACOG, 2021) – would be useful in assessing independent associations.
As the largest integrated health system in the United States with universal PTSD screening and availability of demographic, obstetric, and psychiatric care data, Veterans Health Administration (VA) data are ideal to study for this purpose (Frayne et al., 2018; Quinn et al., 2021). Therefore, we conducted an exploratory analysis of clinical factors associated with spontaneous preterm birth among veterans with active PTSD during pregnancy. We hypothesized that factors related to obstetric course or psychiatric treatment – specifically receipt of medications or engagement in therapy – might affect spontaneous preterm birth rates, and that this association would be independent of demographic or obstetric factors that are known to have relationships with preterm birth.
MATERIALS AND METHODS:
Study Design
We conducted this study within an observational cohort of births reimbursed by the VA using administrative claims data. Non-obstetric care is provided for veterans at the VA, while obstetric care is outsourced and reimbursed by the VA; despite these differences, data from all visits are integrated into VA administrative claims databases. International Classification of Diseases, Ninth Revision Clinical Modification (ICD-9 CM) and current procedural technology (CPT) codes were used from inpatient and outpatient records to compile this dataset, which was developed using a validated algorithm previously published through 2012 and applied to additional pregnancies through the 2015 VA fiscal year (which ends in October) (Shaw et al., 2014; Shaw, Joyce, et al., 2018). The year 2005 was selected as the starting year because psychiatric treatments were not reliably tracked prior to 2005. Fiscal year 2015 was the study endpoint as it was the last year before the transition to ICD-10 coding, and using this end date avoided potential differential coding between ICD-9 and ICD-10 eras.
Veterans with active PTSD who had a singleton livebirth between 2005 and 2015 were included in this study. Active PTSD was defined in accordance with prior literature (Seng et al., 2009; Shaw et al., 2014) as the presence of a PTSD diagnosis code during any encounter within 12 months prior to childbirth. We focused on active PTSD because prior research has identified an association between adverse obstetric outcomes and active (but not historical) PTSD (Seng et al., 2009; Shaw et al., 2014, 2017). A PTSD diagnosis was identified using the ICD-9 CM code 309.81 “post-traumatic stress disorder.” The reliability of this code for PTSD has been validated using VA data by correlating the code with responses to mental health questionnaires (Gravely et al., 2011). This code demonstrates good validity for a PTSD diagnosis in VA administrative data, with a positive predictive value of 74.8% when benchmarked against the PTSD checklist, a reliable and valid psychometric instrument for PTSD (Gravely et al., 2011). Furthermore, universal screening for PTSD in VA primary care minimizes risk of ascertainment bias for PTSD diagnoses. People were excluded if they had a stillbirth or multiple gestation given the known associations with spontaneous preterm labor. The Stanford Institutional Review Board approved this study prior to its initiation.
Outcomes
The primary outcome was spontaneous preterm birth <37 weeks. Spontaneous preterm birth was identified by the ICD-9-CM code 644.2 “spontaneous onset of delivery before 37 weeks” in the birth claim, which has been previously validated to correspond to a median gestational age at childbirth of 35 weeks with 98% specificity for birth before 37 weeks (Shaw et al., 2014).
Exposures
We selected psychiatric and obstetric exposures potentially related to spontaneous preterm birth as exposures in this analysis. One obstetric factor, the development of preeclampsia/eclampsia, was included in this analysis as it is increased in people with PTSD (Shaw et al., 2017) and associated with preterm birth (ACOG, 2019b, 2019a). Preeclampsia/eclampsia was defined using ICD-9 codes 642.5, 642.6, and 642.4, and was reported separately from gestational and chronic hypertension.
Psychiatric exposures of interest included presence of active concurrent psychiatric conditions, use and dispensations of psychotropic medications, and engagement in psychotherapy in the year prior to childbirth. These exposures were selected for their potential association with either 1) improved disease control and theoretically reducing preterm birth rates or 2) being a proxy for severe disease and theoretically increasing preterm birth rates. Concurrent mental health diagnoses that were examined were depression, anxiety, and severe mental illness (bipolar or schizophrenic disorder). Outpatient psychotropic medication dispensations were defined as the number of dispensations ≥1 week supply from the following categories: antidepressant, benzodiazepine, antipsychotic, tri-cyclic or sedative. Opiate dispensations were described separately. Mental health visits were identified using VA clinic stop codes and provider type codes. Psychotherapy was further defined using CPT codes. Any mental health treatment was operationalized as ≥1 medication dispensation or ≥1 mental health visit with a PTSD diagnosis. Pregnancies in which a medication dispensation or therapy visit occurred during the 13-24 months prior to the birth month, but not within 12 months prior to and inclusive of the birth month, were defined as pregnancies in which medication or therapy were stopped prior to pregnancy; this variable hereafter will be referred to as “stopped medications 12 months prior to childbirth” or “stopped therapy 12 months prior to childbirth”. Twelve months prior to childbirth was used as the ascertainment window for exposures given the exploratory nature of our study supported by prior sensitivity analyses demonstrating no significant differences when using 12 versus 9 month windows (Shaw et al., 2014).
Demographic Covariates
Demographic variables of interest included maternal age, substance use disorder with alcohol or drugs, opiate dispensations, chronic hypertension, diabetes, and race/ethnicity, marital status, and any claim for intimate partner violence within 12 months prior to childbirth as social constructs, which were abstracted using ICD-9 CM codes or directly from VA clinical encounter data. Social constructs were included because of disparities in opportunities and treatments across different groups related to structural racism and other forms of bias and disadvantage. Race/ethnicity groups were ascertained from VA administrative databases, which pull from data from clinical encounters based on direct patient report. The groups were condensed into Hispanic, Non-Hispanic Black, Non-Hispanic White, and Other due to small cell sizes. The “Other” category included American Indian, Asian, Pacific Islander, or mixed race. Alcohol use disorder was defined using ICD-9 CM codes (291.x, 303.0x, 303.9x, 305.0x), excluding any codes for remission. Drug use disorder was defined using the same approach with codes 292.0x, 292.8x, 304.2x-9x, 305.2x-9x which include substances such as cannabis, hallucinogens, opiates, cocaine, and amphetamines. Anticipating small numbers of substance use disorder and opiate dispensations, these codes were also combined into one overall substance use disorder variable in the multivariable model.
Statistical Analysis
Our primary analysis was to examine the associations between the demographic, obstetric, and psychiatric factors described above (independent variables) and spontaneous preterm birth (dependent variable) among veterans with active PTSD. Fisher’s exact and chi-square tests were used to compare categorical exposures, and Wilcoxon rank-sum tests were used to compare nonparametric continuous exposures between preterm and term births. Covariates significant at p<0.05 on bivariate analysis and those selected a priori as potential confounders (maternal age and race/ethnicity as a social construct) were included in a multivariable logistic regression to determine adjusted odds of preterm birth for each factor. Race/ethnicity was included as a potential social confounder given the known racial and ethnic disparities in preterm birth rates in the United States (March of Dimes, 2019). Although parity is an important consideration for spontaneous preterm birth, calculation of parity in the VA database is limited in that it includes only births reimbursed by the VA and not by other types of insurance carriers. Therefore births that occurred prior to enrollment with the VA would not be included in the parity calculation. Given this ambiguity, we opted not to include parity as a confounder. Given concerns about collinearity and overlap with exposures related to medication use, we planned to select the single psychiatric medication-related exposure variable with the strongest bivariate association for inclusion in the model. It is important to note intimate partner violence could influence associations with spontaneous preterm birth in many ways – as a confounder or a mediator of preterm birth due to trauma. Given this, it was not selected as an a priori confounder. Continuous covariates (maternal age, number of medication dispensations, number of therapy visits) were categorized given nonlinear associations in their continuous forms. Using the rare disease assumption for spontaneous preterm birth, odds were estimated to approximate risks in this study.
Because depression is so frequently comorbid to PTSD, an analysis was performed stratifying by the presence of active concurrent depression to examine whether comorbid depression might modify the effects of obstetric factors and mental health treatment. An additional analysis was done testing for interaction between antidepressant dispensations and preeclampsia by adding an interaction term for antidepressant dispensations and preeclampsia to the primary logistic regression model.
Statistical significance was set at a two-sided p-value <0.05. STATA Version 16 (StataCorp, 2019, College Station, TX) was used for analysis. STROBE guidelines and reVITALize criteria were used for development of this manuscript.
RESULTS:
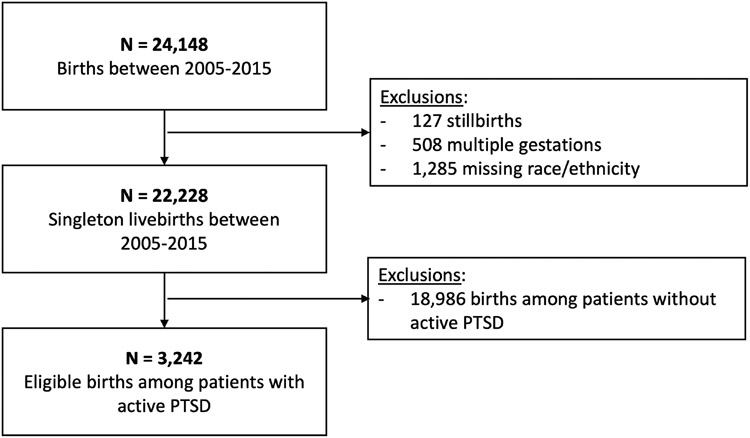
A total of 22,228 singleton livebirths among 15,411 veterans were identified over the 10-year study period. Of these, 3,242 (14.6%) were births among 2,293 people with active PTSD. Spontaneous preterm birth occurred in 249 (7.7%) births among people with active PTSD (Figure 1).
Figure 1.
Cohort inclusion diagram.
Demographics, obstetric characteristics, and psychiatric history of veterans with active PTSD are shown in Table 1. Veterans who gave birth preterm were older (p=0.02 across age categories) and more often had substance use disorders (37.0% versus 29.5%, p=0.01). Though active concurrent depression was prevalent (61.4% of all veterans with active PTSD), there were no significant differences in proportions of people with depression who gave birth preterm versus term (60.6% versus 61.5%, p=0.79).
Table 1.
Demographic and psychiatric characteristics among veterans with active post-traumatic stress disorder (PTSD) whose pregnancy care was reimbursed by the Veterans Health Administration, 2005-2015.
| Variable | Whole cohort N=3,242 N (%)a |
Term birth ≥37 weeks N=2,993 |
Spontaneous preterm birth <37 weeks N=249 |
P- valueb |
|---|---|---|---|---|
| Maternal age category | 0.02 | |||
| 19-24 | 361 (11.1) | 332 (11.1) | 29 (11.7) | |
| 25-29 | 1,257 (38.8) | 1,182 (39.5) | 75 (30.1) | |
| 30-34 | 1,071 (33.0) | 976 (32.6) | 95 (38.2) | |
| 35-39 | 433 (13.4) | 398 (13.3) | 35 (14.1) | |
| 40-46 | 120 (3.7) | 105 (3.5) | 15 (6.0) | |
| Race/Ethnicityc | 0.52 | |||
| Non-Hispanic White | 2,091 (64.5) | 1,938 (64.8) | 152 (61.5) | |
| Non-Hispanic Black | 685 (21.1) | 623 (20.8) | 62 (24.9) | |
| Hispanic | 357 (11.0) | 331 (11.1) | 26 (10.4) | |
| Other | 109 (3.4) | 101 (3.4) | <10d | |
| Married | 1,392 (43.2) | 1,289 (43.4) | 103 (41.5) | 0.58 |
| Chronic hypertension | 71 (2.2) | 61 (2.0) | 10 (4.0) | 0.07 |
| Pre-gestational diabetes | 78 (2.4) | 70 (2.3) | <10 | 0.39 |
| Active concurrent mental health diagnosise | 2,378 (73.4) | 2,193 (73.3) | 185 (74.3) | 0.63 |
| Depression | 1,992 (61.4) | 1,841 (61.5) | 151 (60.6) | 0.79 |
| Anxiety | 1,028 (31.7) | 939 (31.4) | 89 (35.7) | 0.16 |
| Bipolar disorder or schizophrenia (severe mental illness, SMI) | 309 (9.5) | 276 (9.2) | 33 (13.3) | 0.04 |
| Any substance use disorderf | 444 (13.7) | 401 (13.4) | 43 (17.3) | 0.09 |
| Alcohol use disorder | 287 (8.9) | 262 (8.8) | 25 (10.0) | 0.49 |
| Drug use disorder | 287 (8.9) | 258 (8.6) | 29 (11.7) | 0.11 |
| Any claim for intimate partner violence in 12 months prior to childbirth | 173 (5.3) | 162 (5.4) | 11 (4.4) | 0.50 |
Listed as column N (%) or median (Q1,Q3) unless otherwise specified.
Wilcoxon rank sum for continuous variables, Fisher or chi square for categorical. P-values ≥0.01 listed to one-hundredth decimal place, p-values <0.01 listed to one-thousandth decimal place.
Other includes American Indian, Asian, Pacific Islander, or mixed. Race/ethnicity categories presented in order of descending cell frequencies.
Values <10 not shown due to data use agreement.
Documented within 12 months prior to childbirth. Some patients had multiple concurrent mental health diagnoses, so numbers will not add up to 100%.
Any substance use disorder defined using ICD-9 CM codes for alcohol or drug use disorder within 12 months prior to childbirth. See text for details.
Psychiatric treatment characteristics are shown in Table 2. The majority of veterans with active PTSD (79.1%) received some type of mental health treatment during pregnancy, and overall treatment rates (i.e., any treatment in the year prior) did not differ between groups. People with spontaneous preterm birth were more likely to receive a psychotropic medication dispensation (69.9% versus 61.4%, p=0.01) and be using multiple psychotropic medications (38.6% versus 27.2%, p=0.02). A greater proportion of people with spontaneous preterm births had ≥6 antidepressant medication dispensations (19.3% preterm had ≥6 dispensations versus 12.3% term, p<0.001) in the 12 months preceding childbirth. While many people participated in at least 1 psychotherapy visit, there were no significant differences in therapy utilization between groups. Similarly, no difference between groups was observed for the proportion that had evidence of having stopped medications or therapy 12 months prior to childbirth.
Table 2.
Psychiatric treatment patterns among veterans with active post-traumatic stress disorder (PTSD) whose pregnancy care was reimbursed by the Veterans Health Administration, 2005-2015.
| Treatment | Whole Cohort N=3,242 N (%)a |
Term birth ≥37 weeks N=2,993 |
Spontaneous preterm birth <37 weeks N=249 |
P-valueb |
|---|---|---|---|---|
| Any treatment within 12 months prior to childbirthc | 2,564 (79.1) | 2,356 (78.7) | 208 (83.5) | 0.07 |
| Any psychotropic medication within 12 months prior to childbirthd | 2,011 (62.0) | 1,837 (61.4) | 174 (69.9) | 0.01 |
| Any clinical visit for medication managemente | 1,907 (58.8) | 1,742 (58.2) | 165 (66.3) | 0.01 |
| Type of psychotropic medication dispensedd |
||||
| Antidepressant | 1,769 (54.6) | 1,606 (53.7) | 163 (65.5) | <0.001 |
| Benzodiazepine | 419 (12.9) | 380 (12.7) | 39 (15.7) | 0.18 |
| Antipsychotic | 381 (11.8) | 340 (11.4) | 41 (16.5) | 0.02 |
| Tri-cyclic antidepressant | 137 (4.2) | 121 (4.0) | 16 (6.4) | 0.07 |
| Sedative | 461 (14.2) | 419 (14.0) | 42 (16.9) | 0.21 |
| Number of antidepressant medication dispensations during pregnancyd | <0.001 | |||
| 0 | 1,473 (45.4) | 1,387 (46.3) | 86 (34.5) | |
| 1-2 | 737 (22.7) | 669 (22.4) | 68 (27.3) | |
| 3-5 | 616 (19.0) | 569 (19.0) | 47 (18.9) | |
| ≥6 | 416 (12.8) | 368 (12.3) | 48 (19.3) | |
| ≥1 opioid dispensation within 12 months prior to childbirth | 673 (20.8) | 607 (20.3) | 66 (26.5) | 0.02 |
| Number of unique medication categories used | 0.02 | |||
| Monotherapy (1 medication type) | 1,188 (36.6) | 1,097 (36.7) | 91 (36.5) | |
| Polytherapy (>1 medication type) | 911 (28.1) | 815 (27.2) | 96 (38.6) | |
| Any psychotherapy visit in 12 months prior to childbirthe |
1,768 (54.5) | 1,621 (54.2) | 147 (59.0) | 0.14 |
| 0 sessions | 1,474 (45.5) | 1,372 (45.8) | 102 (41.0) | |
| 1-7 sessions | 1,300 (40.1) | 1,195 (39.9) | 105 (42.2) | 0.27 |
| ≥8 sessions | 468 (14.4) | 426 (14.2) | 42 (16.9) | |
| Stopped medications 12 months childbirth | 332 (10.2) | 306 (10.2) | 26 (10.4) | 0.91 |
| Stopped therapy 12 months prior to childbirth | 525 (16.2) | 492 (16.4) | 33 (13.3) | 0.19 |
Listed as column N (%) or median (Q1,Q3) unless otherwise specified.
Wilcoxon rank sum, Fisher or Chi where appropriate. P-values ≥0.01 listed to one-hundredth decimal place, p-values <0.01 listed to one-thousandth decimal place.
Any psychotropic medication dispensation or therapy visit within 12 months prior to childbirth.
1 or more fills of at least a 7-day supply of any included psychotropic prescription in the 12 months prior to childbirth.
Multiple visits in a single day were counted as 1 visit. Includes any visit within 12 months prior to childbirth.
Multivariable logistic regression was performed including the following covariates: preeclampsia/eclampsia, number of antidepressant medication dispensations, number of psychotherapy sessions, active bipolar disorder or schizophrenia, alcohol, drug or opiate use, maternal age, and race/ethnicity. The strongest association for a psychiatric covariate was for number of antidepressant dispensations, so this was selected as the sole “medication-related” covariate for the model to limit issues related to collinearity. After accounting for clustering of births among people, only preeclampsia/eclampsia (adjusted odds ratio [aOR] 3.30, 95% CI 1.67-6.54) and ≥6 antidepressant medication dispensations (aOR 1.89, 95% CI 1.29-2.77) remained significantly associated with spontaneous preterm birth. When restricting the model to just psychiatric exposures and demographic covariates (removing preeclampsia), antidepressant dispensations remained the only factor associated with spontaneous preterm birth (aOR for ≥6 antidepressant dispensations 1.89, 95% CI 1.28-2.77) and no other factors emerged as significant. The addition of an interaction term for preeclampsia and antidepressant dispensations in the primary logistic regression model was not significant (p=0.39), suggesting no evidence of interaction on spontaneous preterm birth.
Next, an additional analysis was conducted examining significant covariates stratified by presence (N=1,992) or absence (N=1,250) of active concurrent depression. Preterm birth was increased in people with active concurrent depression and preeclampsia/eclampsia (OR 4.21, 95% CI 1.76-10.10) as well as in people with ≥6 antidepressant dispensations (OR 1.92, 95% CI 1.17-3.13, Table 4).
Table 4.
Risk of preterm birth stratified by active concurrent depression status among patients with post-traumatic stress disorder (PTSD) who gave birth between 2005 and 2015.
| Covariates | Crude ORsa for spontaneous preterm birth, no active depression (95% CI) N=1,250 |
Crude ORs for spontaneous preterm birth, with active depression (95% CI) N=1,922 |
|---|---|---|
| Preeclampsia/eclampsia | 2.41 (0.81-7.19) | 4.21 (1.76-10.10) |
| Number of antidepressant dispensations during pregnancyb | ||
| 0 | Ref | Ref |
| 1-2 | 1.53 (0.90-2.61) | 1.78 (1.14-2.78) |
| 3-5 | 1.37 (0.71-2.64) | 1.40 (0.87-2.27) |
| ≥6 | 3.21 (1.75-5.91) | 1.92 (1.17-3.13) |
Run as separate models for preeclampsia/eclampsia and number of antidepressant medication dispensations.
1 dispensation defined as number of fills of at least a 7-day supply of antidepressant prescription in the 12 months prior to childbirth.
DISCUSSION:
In our exploratory study of pregnant veterans with active PTSD, preeclampsia/eclampsia and 6 or more antidepressant medication dispensations in the year prior to giving birth were identified as factors independently associated with increased spontaneous preterm birth. Despite our hypothesis that psychiatric treatment factors would impact preterm birth rates, antidepressant medication dispensation was the only psychiatric factor found to be significantly associated with our outcome of interest. Our exploratory analysis results highlight the importance of future research further interrogating antidepressant dispensations and preeclampsia, with the ultimate goal of helping to reduce preterm birth in the veteran population. Importantly, our data do not suggest that discontinuing needed antidepressants among pregnant veterans with PTSD would reduce the risk of preterm birth.
Preeclampsia/eclampsia emerged as the factor associated with the greatest increased risk of spontaneous preterm birth. While preeclampsia often results in medically indicated preterm birth (Ananth & Vintzileos, 2008; Goldenberg et al., 2008), an association with spontaneous preterm birth has been suggested (Ananth et al., 1997). One hypothesis is that preeclampsia and spontaneous preterm birth share similar pathophysiologic mechanisms through placental dysfunction or inflammation (Leonard & Maes, 2012; Osborne & Monk, 2013; Rasmussen et al., 2017). For some with PTSD, perhaps preeclampsia is the first manifestation of a worsening inflammatory state that precedes spontaneous preterm birth.
Our results also add to a growing body of research exploring the observational association between preterm birth and antidepressant use, where much of this prior work has focused on people with depression rather than PTSD (Eke et al., 2016; Huybrechts et al., 2014; Sujan et al., 2017). Though ongoing antidepressant dispensations were associated with spontaneous preterm birth in our study, active concurrent depression was not. The evidence surrounding antidepressant use and spontaneous preterm birth is conflicting, and has been unable to quell debate around whether the association is simply confounded by indication (Eke et al., 2016; Palmsten & Hernández-díaz, 2012; Venkatesh et al., 2016). Antidepressant dispensations may serve as a proxy for PTSD severity, which is supported by the fact that ≥6 antidepressant dispensations was associated with the highest risk of preterm birth but there was not a clear dose-response relationship, which would be expected from a true biologic effect of a drug. While it seems likely that this factor is serving as a proxy for PTSD severity, whether this association could be due to the treatment itself remains to be elucidated in a larger or prospective study with more nuanced clinical data that would allow adjustment for disease severity, and more granular data on antidepressant drug type, timing, and continuation. Also needed is translational study that invokes evaluation of biomarkers and genetics that might correspond and connect the heightened stress or inflamamtory states of PTSD, preeclampsia, and preterm birth – for example, the promise of novel datasets such as the Million Veteran Program (Department of Veterans Affairs Office of Research and Development, 2022).
Strengths of this study include a large cohort with a high prevalence of active PTSD, enabling a granular investigation of risk factors for preterm birth. The near universal screening for PTSD in VA settings minimizes ascertainment bias of the exposure that is characteristic of large cohort studies. Because screening can detect cases that would not otherwise come to clinical attention, the sample likely includes good variation in the range of PTSD severity. Our descriptive results alone outlining psychiatric therapies in pregnancy are unique contributions to the literature, and interestingly it did not appear that engagement in psychotherapy reduced the risk of spontaneous preterm birth in this cohort.
Our results must be interpreted within the context of our study design. Firstly, diagnoses can be underreported with ICD codes. It is possible that some medically indicated preterm births received the code for spontaneous preterm birth, resulting in misclassification of the outcome. Conventional risk factors for preterm birth established in other studies – such as race/ethnicity as a social construct (Goldenberg et al., 2008) – did not emerge as predictors in this analysis. This may be because restricting to veterans with PTSD results in a cohort with less heterogeneity in social factors than what is reported in other studies on preterm birth (Ekeke et al., 2020). Notably, the majority of people in this cohort (79.1%) had some type of psychiatric care during pregnancy. While this may represent the robust mental health care provided by the VA (Kroll-Desrosiers et al., 2020; Shivakumar et al., 2020), it also may be an artifact of detection bias in the ICD- 9 method used to classify a PTSD diagnosis as active. We were also limited in our ascertainment of prior obstetric history given limitations of the estimation of nulliparity in VA data; however, from what was available to us for this cohort, 2,707 (83.5%) of the cohort of 3,242 were estimated to be nulliparous. Additionally, due to limitations in ascertainment of medication timing, polytherapy could include people who took two medications concurrently or transitioned between two medications during pregnancy. Lastly, although the VA is the largest integrated health care system in the United States and is increasingly being utilized by pregnant veterans (Frayne et al., 2018), our results may not be generalizable to veterans who do not utilize VA services or to the non-veteran pregnant population.
IMPLICATIONS FOR PRACTICE AND/OR POLICY
Our results highlight which veterans with PTSD appear to be at highest risk for spontaneous preterm birth; namely, those who develop preeclampsia/eclampsia and those who are actively filling antidepressant prescriptions throughout pregnancy. With this knowledge, healthcare providers can incorporate the risk of spontaneous preterm birth into pregnancy counseling and surveillance. Additionally, healthcare researchers can appropriately increase focus on translational and treatment-focused research that includes awareness of these higher risk sub-populations.
As with many observational studies, the factors we identified as contributors to spontaneous preterm birth now warrant further investigation, prospectively and on a more granular level. For preeclampsia, a targeted evaluation of spontaneous versus medically-indicated preterm births in people with active PTSD is necessary to disentangle causality. Furthermore, in concert with previous findings on the risks of preeclampsia in veterans with active PTSD (Shaw et al., 2017), our results make a case for future research examining the potential for preeclampsia prophylaxis with low-dose aspirin in people with PTSD; mental health conditions are not currently included as indications for this prevention strategy (ACOG, 2018). For antidepressant medications, future research interrogating dosage, timing, and medication type in unison with PTSD disease severity are needed to better delineate the risk of spontaneous preterm birth. It is important to note that our data are exploratory, and that there is no causal link established between antidepressant medications, preeclampsia, and spontaneous preterm birth; rather, these factors appear to have independent associations that warrant further research. Our results highlight these areas of future research to be worth pursuing in an effort to reduce preterm birth rates in veterans with active PTSD during pregnancy.
CONCLUSIONS
Our exploratory study in veterans with active PTSD identified significant associations between spontaneous preterm birth and preeclampsia/eclampsia as well as between spontaneous preterm birth and ≥6 antidepressant medication dispensations in the year prior to childbirth. As discussed above, our data do not suggest any direct relationship between antidepressant medications and preterm birth; rather, ≥6 dispensations is likely serving as a proxy for PTSD disease severity. Validation and interrogation of these associations in larger cohorts is an important step towards informing preterm birth prevention strategies for this population.
Table 3.
Clinical factors associated with spontaneous preterm birth among veterans with active post-traumatic stress disorder (PTSD) (N=3,242).
| Covariates | Term birth N= 2,993 N (%) |
Spontaneous preterm birth N = 249 N (%) |
Adjusted OR for spontaneous preterm birtha (95% CI) |
|---|---|---|---|
| Preeclampsia/eclampsiab | 41 (1.4) | 11 (4.4) | 3.30 (1.67-6.54) |
| Number of antidepressant dispensations during pregnancyc | |||
| 0 | 1,387 (46.3) | 86 (34.5) | Ref |
| 1-2 | 669 (22.4) | 68 (27.3) | 1.54 (1.11-2.14) |
| 3-5 | 569 (19.0) | 47 (18.9) | 1.26 (0.86-1.83) |
| ≥6 | 368 (12.3) | 48 (19.3) | 1.89 (1.29-2.77) |
| Number of psychotherapy sessions during pregnancyd | |||
| 0 | 1,372 (45.8) | 102 (41.0) | Ref |
| 1-7 | 1,195 (39.9) | 105 (42.2) | 1.08 (0.82-1.44) |
| ≥8 | 426 (14.2) | 42 (16.9) | 1.13 (0.76-1.67) |
| Concurrent severe mental illness | 276 (9.2) | 33 (13.3) | 1.35 (0.91-2.00) |
| ≥1 opiate dispensation within 12 months prior to childbirth | 607 (20.3) | 66 (26.5) | 1.27 (0.94-1.71) |
| Advanced maternal age ≥35 years | 503 (16.8) | 50 (20.1) | 1.18 (0.85-1.63) |
| Race / ethnicity as a social construct | |||
| Non-Hispanic White | 1,938 (64.8) | 152 (61.5) | Ref |
| Non-Hispanic Black | 623 (20.8) | 62 (24.9) | 1.23 (0.90-1.69) |
| Hispanic | 331 (11.1) | 26 (10.4) | 1.07 (0.69-1.66) |
| Othere | 101 (3.4) | <10f | 1.00 (0.47-2.12) |
Adjusted for all covariates shown in table. Covariates were selected based on p<0.05 in bivariate analysis and a priori selection of maternal age, number of therapy sessions, and race/ethnicity. Race/ethnicity included as a representation of social constructs, not as a biologic risk factor for preterm birth. See text for details.
Not including chronic hypertension with superimposed preeclampsia.
1 dispensation defined as 1 fill of at least a 7-day supply of antidepressant prescription within 12 months prior to childbirth.
Multiple visits in a single day were counted as 1 visit. Includes any visit within 12 months prior to childbirth.
Other includes American Indian, Asian, Pacific Islander, or mixed. Race/ethnicity categories presented in order of descending cell frequencies.
Not reported due to data use agreement.
FUNDING SOURCE:
Partial funding for this research was provided by grant number IIR 20-314 from the Department of Veterans Affairs, Health Services Research and Development Service. Dr. Danielle Panelli's time is partially supported by an NIH K12HD103084 grant
Biographies
1.
Danielle M. Panelli MD
Maternal-Fetal Medicine physician in Division of Maternal-Fetal Medicine and Obstetrics, Department of Obstetrics and Gynecology, Stanford University. Research interests include maternal mental health and adverse pregnancy outcomes.
2.
Caitlin S. Chan SM
Biostatistician affiliated with the VA Health Economics Resource Center at VA Palo Alto Health Care System. Research interests include reproductive health outcomes for Veterans.
3.
Jonathan G. Shaw MD MS
Family Medicine physician in the Division of Primary Care & Population Health, Department of Medicine, Stanford University, and health research affiliate with VA HSR&D Center for Innovation to Implementation, VA Palo Alto.
4.
Megha Shankar MD
Internal Medicine physician affiliated with the UC San Diego Division of General Internal Medicine; graduate of Advanced Fellowship in Health Services Research and Development at the VA Palo Alto. Research interests include women’s health and health equity.
5.
Rachel Kimerling, PhD
Clinical psychologist affiliated with the National Center for PTSD. Research interests include health services research that addresses women’s health and gender issues in the detection, treatment, and impacts of traumatic stress.
6.
Susan M. Frayne MD MPH
Internal Medicine physician, Director of Women’s Health Evaluation Initiative, VA Palo Alto, affiliated with the Division of Primary Care & Population Health, Department of Medicine, Stanford University. Research interests include primary care for women with mental illness.
7.
Tiffany C. Herrero MD
Maternal-Fetal Medicine physician in Division of Maternal-Fetal Medicine and Obstetrics, Department of Obstetrics and Gynecology, Stanford University. Research interests include maternal morbidity and high-risk pregnancy conditions.
8.
Deirdre J. Lyell MD
Maternal-Fetal Medicine physician in Division of Maternal-Fetal Medicine and Obstetrics, Department of Obstetrics and Gynecology, Stanford University. Research interests include severe maternal morbidity, population health, obstetric outcomes and placenta accreta spectrum.
9.
Ciaran S. Phibbs PhD
Associate Director of VA Women’s Health Evaluation Initiative, VA Palo Alto and Associate Professor of Pediatrics. Research interests include pregnancy outcomes and disparities for veterans, particularly those with mental health conditions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE: The authors report no conflict of interest.
PRESENTATION: Presented at the 40th Annual Meeting of the Society for Maternal Fetal Medicine, Feb 3-8, 2020, Grapevine, TX and the 41st Annual Meeting of the Society for Maternal-Fetal Medicine, Jan 25-30, 2021 (virtual)
DISCLAIMER: Development of the Women’s Health Evaluation Initiative (WHEI) data which were used in this study was supported by Veteran’s Health Administration Women’s Health Services.
REFERENCES
- ACOG. (2018). Committee Opinion 743: Low-Dose Aspirin Use During Pregnancy. Obstet Gynecol, 132(1), 44–52. [DOI] [PubMed] [Google Scholar]
- ACOG. (2019a). Practice Bulletin 202: Gestational Hypertension and Preeclampsia. Obstetrics and Gynecology, 133(1), 211–214. [DOI] [PubMed] [Google Scholar]
- ACOG. (2019b). Practice Bulletin 204: Fetal growth restriction. Obstetrics & Gynecology, 133(5), 1063–1066. 10.1097/aog.0000000000003242 [DOI] [PubMed] [Google Scholar]
- ACOG. (2021). Prediction and prevention of spontaneous preterm birth. Obstetrics & Gynecology, 138(2), e65–e90. 10.5935/2238-3182.20130052 [DOI] [PubMed] [Google Scholar]
- Ananth CV, Savitz DA, Luther ER, & Bowes WA (1997). Preeclampsia and preterm birth subtypes in Nova Scotia, 1986 to 1992. Am J Perinatol, 14(1), 17–23. [DOI] [PubMed] [Google Scholar]
- Ananth CV, & Vintzileos AM (2008). Medically Indicated Preterm Birth: Recognizing the Importance of the Problem. Clinics in Perinatology, 35(1), 53–67. 10.1016/j.clp.2007.11.001 [DOI] [PubMed] [Google Scholar]
- Cook N, Ayers S, & Horsch A (2018). Maternal posttraumatic stress disorder during the perinatal period and child outcomes : A systematic review. Journal of Affective Disorders, 225(July 2017), 18–31. 10.1016/j.jad.2017.07.045 [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs Office of Research and Development. (2022). https://www.research.va.gov/mvp/ [Google Scholar]
- Eke AC, Saccone G, & Berghella V (2016). Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG: An International Journal of Obstetrics and Gynaecology, 123(12), 1900–1907. 10.1111/1471-0528.14144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekeke P, Mendez DD, Yanowitz TD, & Catov JM (2020). Racial Differences in the Biochemical Effects of Stress in Pregnancy. Environ Res and Pub H, 17(19), 6941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne S, Phibbs C, Saechao F, Friedman S, Shaw J, Romodan Y, Berg E, Lee J, Ananth L, Iqbal S, Hayes P, & Haskell S (2018). Sourcebook: Women Veterans in the Veterans Health Administration. Volume 4: Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution. Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, 4(February). [Google Scholar]
- Goldenberg RL, Culhane JF, Iams JD, & Romero R (2008). Epidemiology and causes of preterm birth. Lancet, 371, 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravely AA, Cutting A, Nugent S, Grill J, Carlson K, & Spoont M (2011). Validity of PTSD diagnoses in VA administrative data: Comparison of VA administrative PTSD diagnoses to self-reported PTSD Checklist scores. Journal of Rehabilitation Research and Development, 48(1), 21–30. 10.1682/JRRD.2009.08.0116 [DOI] [PubMed] [Google Scholar]
- Huybrechts KF, Sanghani RS, Avorn J, & Urato AC (2014). Preterm birth and antidepressant medication use during pregnancy: A systematic review and meta-analysis. PLoS ONE, 9(3). 10.1371/journal.pone.0092778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroll-Desrosiers AR, Crawford SL, Moore Simas TA, Clark MA, & Mattocks KM (2020). Treatment and Management of Depression Symptoms in Pregnant Veterans: Varying Experiences of Mental Health Care in the Prenatal Period. Psychiatric Quarterly, 91(2), 475–493. 10.1007/s11126-019-09676-7 [DOI] [PubMed] [Google Scholar]
- Leonard B, & Maes M (2012). Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neuroscience and Biobehavioral Reviews, 36(2), 764–785. 10.1016/j.neubiorev.2011.12.005 [DOI] [PubMed] [Google Scholar]
- March of Dimes. (2019). March of Dimes Preterm Birth Report Card. 1–144. https://www.marchofdimes.org/peristats/tools/reportcard.aspx?reg=44 [Google Scholar]
- Osborne LM, & Monk C (2013). Perinatal depression-The fourth inflammatory morbidity of pregnancy? Theory and literature review. Psychoneuroendocrinology, 38(10), 1929–1952. 10.1016/j.psyneuen.2013.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmsten K, & Hernández-díaz S (2012). Commentary: Can Nonrandomized Studies on the Safety of Antidepressants DuringPregnancy Convincingly Beat Confounding, Chance, and Prior Beliefs? Epidemiology, 23(5), 686–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DA, Mor MK, Sileanu FE, Zhao X, Callegari LS, Zephyrin LC, Frayne DJ, & Borrero S (2021). Measuring Female Veterans’ Prepregnancy Wellness Using Department of Veterans Affairs’ Health Record Data. Obstet Gynecol, 137(3), 471–480. 10.1097/AOG.0000000000004293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S, Ebbing C, & Irgens LM (2017). Predicting preeclampsia from a history of preterm birth. PLoS ONE, 12(7), 1–10. 10.1371/journal.pone.0181016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, & Yonkers KA (2007). Effects of posttraumatic stress disorder on pregnancy outcomes. 102, 137–143. 10.1016/j.jad.2007.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanjuan PM, Fokas K, Tonigan JS, Henry MC, Christian K, Rodriguez A, Larsen J, Yonke N, & Leeman L (2021). Prenatal maternal posttraumatic stress disorder as a risk factor for adverse birth weight and gestational age outcomes: A systematic review and meta-analysis. Journal of Affective Disorders, 295(September), 530–540. 10.1016/j.jad.2021.08.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, & Liberzon I (2009). Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and Gynecology, 114(4), 839–847. 10.1097/AOG.0b013e3181b8f8a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw JG, Asch SM, Katon JG, Shaw KA, Kimerling R, Frayne SM, & Phibbs CS (2017). Post-traumatic Stress Disorder and Antepartum Complications a Novel Risk Factor for Gestational Diabetes and Preeclampsia. Paediatric and Perinatal Epidemiology, 31(3), 185–194. [DOI] [PubMed] [Google Scholar]
- Shaw JG, Asch SM, Kimerling R, Frayne SM, Shaw KA, & Phibbs CS (2014). Posttraumatic stress disorder and risk of spontaneous preterm birth. Obstetrics and Gynecology, 124(6), 1111–1119. [DOI] [PubMed] [Google Scholar]
- Shaw JG, Joyce VR, Schmitt SK, Frayne SM, Shaw KA, Danielsen B, Kimerling R, Asch SM, & Phibbs CS (2018). Selection of Higher Risk Pregnancies into Veterans Health Administration Programs: Discoveries from Linked Department of Veterans Affairs and California Birth Data. Health Services Research, 53, 5260–5284. 10.1111/1475-6773.13041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw JG, Nelson DA, Shaw KA, Woolaway-bickel K, Phibbs CS, & Kurina LM (2018). Deployment and Preterm Birth Among US Army Soldiers. Am J Epi, 187(4), 687–695. 10.1093/aje/kwy003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shivakumar G, Kroll-Desrosiers AR, Copeland L, Anderson EH, Maydon A, & Mattocks K (2020). Patterns of Treatment Utilization Across the Perinatal Period in the Center for Maternal and Infant Outcomes and Research in Translation (COMFORT) Veterans Study. Journal of Women’s Health, 00(00), 1–9. 10.1089/jwh.2020.8435 [DOI] [PubMed] [Google Scholar]
- Sujan AC, Rickert ME, Patrick D, Almqvist C, Larsson H, Sciences B, & Institutet K (2017). Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/ hyperactivity disorder in offspring. JAMA, 317(15), 1553–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh KK, Riley L, Castro VM, Perlis RH, & Kaimal AJ (2016). Association of antenatal depression symptoms and antidepressant treatment with preterm birth. Obstetrics and Gynecology, 127(5), 926–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, & Belanger K (2014). Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry, 71(8), 897–904. 10.1001/jamapsychiatry.2014.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers KA, Vigod S, & Ross LE (2011). Diagnosis, Pathophysiology, and Management of Mood Disorders in Pregnant and Postpartum Women. Obstetrics & Gynecology. 10.1097/AOG.0b013e31821187a7 [DOI] [PubMed] [Google Scholar]