Abstract
There is a lack of data on the adequacy of nutrient intake and prevalence of malnutrition risk in Asian populations. The aim was to report on the nutrient intake and prevalence of malnutrition risk in a community sample of older adults in Singapore. Analysis was performed on 738 (n = 206 male, n = 532 male, aged 67.6 ± 6.0 years) adults 60 years and above. Intakes of macro- and micronutrients were evaluated against the Recommended Dietary Allowances (RDAs). Malnutrition risk was assessed using the Nutrition Screening Initiative Determine Your Nutritional Health checklist. It was found that 90.5% older adults exceeded the sugar intake, 68.5% males and 57.1% females exceeded the intake limit for saturated fat, and 33% males had inadequate dietary fiber intake when compared to the RDAs. Inadequate dietary calcium intake was found in 49.5% males and 55.3% females. There were 22.3% of older adults at moderate to high malnutrition risk. Singaporean older adults need to reduce their dietary intakes of sugar and saturated fat and increase their intakes in dietary fiber and calcium. Current findings provide public health awareness on the importance of healthy eating and will facilitate decision making by health promotors to deliver targeted nutrition care programs.
Keywords: nutrient, malnutrition, aged, nutritional assessment, Asian
1. Introduction
The older population represents the largest demographic group at risk of malnutrition [1]. It has been reported in the Western community that 10–30% of older adults aged 60 and above have malnutrition [2]. Malnutrition occurs when there is a deficiency, excess or imbalance in dietary intake that prevents normal bodily function, and leads to adverse clinical outcomes [3]. Malnutrition increases risks for morbidity and mortality [4]. Changes in nutritional status among older adults are insidious, often left unrecognized until pronounced physical changes are apparent. Therefore, screening and identifying nutrition problems among community older adults is of utmost importance. Early detection will not only allow public health professionals to address nutrition problems at its earliest stage, but also prevent future incidence of nutrition problems, and mitigate healthcare burden associated with a growing older adult population.
Possible reasons for malnutrition include age-related changes such as alterations in taste, poorer digestion, and chewing and swallowing difficulties, which may reduce ones motivations to eat or drink [5]. Ageism, and reduced mobility may cause older people to become socially isolated and lonely. Social isolation and loneliness are associated with reduced appetite [6], decreased food intakes [6,7], and increased malnutrition risk among older adults [8]. Moreover, poor dietary choices are often seen in socially isolated older adults, who tend to consume lesser fruits and vegetables [9] and have lower dietary variety [10]. Older adults are more likely to experience financial hardship due to retirement, out-living savings [11], and less opportunities for employment [12]. A diet that includes fruit, vegetables and fish is often perceived as a luxury for older adults on constraining food budgets [13]. To lower the cost of living, one might choose less heathy foods that are often high in saturated fat, sugar, and sodium and low in fiber and nutritional value.
Despite concerns over poor nutrition and the risk of malnutrition in the older adult population, there is limited data in this vulnerable population group in Asian countries. To date, no studies have looked at the adequacy of nutrient intakes and malnutrition risk of community-dwelling older adults aged 60 and above in Singapore. As a result, this study aimed to determine nutrient intake and malnutrition risk among community-dwelling older adults in Singapore. Given the difference in nutrition requirements between sex, males and females were investigated separately. Dietary practices and nutrition knowledge were also surveyed to understand the observed dietary intake pattern.
2. Materials and Methods
2.1. Study Design
Data were generated from the Diet and Healthy Ageing (DaHA) cohort, which is a prospective population-based study established between 2011 and 2017 [14]. The cohort recruited 1060 community-dwelling Singaporean or permanent residents aged 60 years and above. Recruitments were from the Jurong region of Singapore. Interviews were conducted in-person at the Training and Research Academy at Jurong Point (TaRA@JP) by trained research nurses. Structured questionnaires were used to collect information on demographic characteristics and dietary information.
2.2. Dietary Intakes
Habitual dietary intakes were measured using a validated semi-quantitative food frequency questionnaire (FFQ) developed by the Singapore Health Promotion Board (HPB) [15]. There are more than 300 food items in the FFQ designed to capture the calories, total fat, types of fats, cholesterol, and other nutrients consumed by the participants. The FFQ was administered by research nurses who were trained by an experienced research dietitian. Subjects were to report number of times the food is consumed per day, week, or month. Portion size pictures/food models and the Compendium of Food Pictures [16] were used to guide responses. Participants were asked for the venue at which food was consumed and cooking methods (e.g., steamed, stir-fried, curry without coconut) to consider for the different nutrient compositions. The intakes of various macro- and micronutrients were calculated based on the information obtained from the FFQ using a database system developed by the HPB. The level of intakes of nutrients were evaluated against the Recommended Dietary Allowances (RDAs) for healthy individuals and the Dietary Guidelines developed by the Health Promotion Board [17,18,19,20]. For vitamins and minerals, intake of less than 70% of the respective RDA is defined as insufficient [21]. For the intakes of polyunsaturated fatty acid (PUFA), monounsaturated fatty acid (MUFA) and saturated fat (SFA), it is recommended that the ratio for all adults is 1.00: 1.00: 1.00 (P: M: S ratio) [19].
2.3. Malnutrition Risk Screening
The malnutrition risk screening tool, Nutrition Screening Initiative Determine Your Nutritional Health (NSI Determine) checklist, was used to assess risk for malnutrition among older adults. The tool comprises of 10 checklist items on warning signs for poor nutrition [22]. Based on the aggregate point results, one can be classified as having low nutritional risk (0 to 2 points), moderate nutritional risk (3 to 5 points) or high nutritional risk (6 points and above). The greater the scores, the greater the risk of malnutrition.
2.4. Dietary Practices
Dietary practices such as choices of fats and oils (blended vegetable oil, polyunsaturated oil, monounsaturated oil, saturated fat or none) used in cooking, milk (creamer, sweetened condensed, evaporated, full cream, low-fat, skimmed, whitener or none) used in beverages and the habit of asking for less sugar/less sweet when ordering beverages and desserts were also captured to understand health behaviors related to the nutrient intakes.
2.5. Nutrition Knowledges
Participants were tested upon their nutrition knowledge on the relationship between fat, salt, dietary fiber, calcium, iron and preserved foods and certain diseases. A total of 12 questions were administered with responses being ‘true’, ‘false’ or ‘don’t know. One point was awarded for each correct response, and no point was awarded for an incorrect response or non-response. The level of nutrition knowledge was defined as either low (0 to 3), moderate (4 to 6) or high (7 or above) based on the scores. Participants were also asked how much attention they pay to dietary and nutrition information and their most important sources of nutrition information (e.g., internet, friends, medical practitioners). The questionnaire was designed by an internal research dietitian and can be found in supplementary Text S1.
2.6. Statistical Methods
Only participants that completed the FFQ were included in the analysis. Participants that had inconsistencies in reporting between dietary practice items and FFQ items were excluded from the analysis. All statistical analyses were conducted in Stata (15.1, StataCorp LLC, College Station, TX, USA). Continuous data were tested for normality. Descriptive statistics were used to analyze the demographic and anthropometry data of the study participants. In the cases of skewed data, the median and interquartile range (IQR) were presented instead of the mean and standard deviation (SD). Sex differences in their median nutrient intakes and proportion of DRI consumed were compared using the Mann–Whitney test and Chi-squared test, respectively. The level of significance was set at p ≤ 0.05 for all statistical procedures.
3. Results
After removal of those that did not complete the interview (n = 44), or had repeated interviews (n = 6) or dietary information missing or incorrect (n = 272), 738 participants were included in this cross-sectional analysis. A flowchart of the selection process can be seen in Figure S1. Participant demographic characteristics are shown in Table 1. The mean age was 67.6 years (SD = 6.0, range: 60–92). Participants were mostly females (72.1%) and Chinese (95.7%). The majority of older adults lived with family. The average number of years of schooling was 6.1 ± 4.3. Around half of the older adults reported to have medically diagnosed high blood pressure (48.4%) and high cholesterol (52.6%). The prevalence of diabetes was found to be 18%. The majority (59.9%) had healthy weights.
Table 1.
Participants (n = 738) demographic characteristics.
| All | Male | Female | |
|---|---|---|---|
| n (%) | 738 (100) | 206 (27.9) | 532 (72.1) |
| Age, year ± SD | 67.6 ± 6.0 | 68.8 ± 6.2 | 67.1 ± 5.8 |
| Race, n (%) | |||
| Chinese | 706 (95.7) | 189 (91.8) | 517 (97.2) |
| Malay | 6 (0.8) | 5 (2.4) | 1 (0.2) |
| Indian | 15 (2.0) | 7 (3.4) | 8 (1.5) |
| Others | 11 (1.5) | 5 (2.4) | 6 (1.1) |
| Living status, n (%) | |||
| Alone | 49 (6.7) | 7 (3.4) | 42 (7.9) |
| With family | 688 (93.4) | 199 (96.6) | 489 (92.1) |
| Schooling, year ± SD | 6.1 ± 4.3 | 7.9 ± 0.31 | 5.4 ± 0.17 |
| Currently working, n (%) | 142 (19.4) | 49 (24.1) | 93 (17.6) |
| Physical activity, n (%) | 615 (83.7) | 173 (84.4) | 442 (83.4) |
| Current smokers, n (%) | 40 (5.4) | 30 (14.6) | 10 (1.9) |
| Alcohol drinkers, n (%) | 68 (9.2) | 33 (16.0) | 35 (6.6) |
| High blood pressure, n (%) | 357 (48.4) | 102 (49.5) | 255 (47.9) |
| High cholesterol, n (%) | 388 (52.6) | 108 (52.4) | 280 (52.6) |
| Diabetes, n (%) | 133 (18.0) | 41 (19.9) | 92 (17.3) |
| Stroke, n (%) | 26 (3.5) | 12 (5.8) | 14 (2.6) |
| GDS-15, mean ± SD | 1.3 ± 2.0 | 1.36 ± 0.2 | 1.3 ± 0.1 |
| GAI-20, mean ± SD | 1.1 ± 2.5 | 0.8 ± 0.2 | 1.2 ± 0.1 |
| MMSE, mean ± SD * | 27.7 ± 2.5 | 28.1 ± 0.1 | 27.5 ± 0.1 |
| Weight, kg ± SD | 59.7 ± 10.6 | 65.2 ± 10.0 | 57.6 ± 10.1 |
| Height, m ± SD | 1.57 ± 0.078 | 1.65 ± 0.065 | 1.54 ± 0.055 |
| BMI, kg/m2 ± SD | 24.2 ± 3.7 | 23.9 ± 3.3 | 24.3 ± 3.9 |
| BMI category (WHO) | |||
| Underweight < 23.0 | 24 (3.3) | 6 (2.9) | 18 (3.4) |
| Normal 23.0–28.0 | 438 (59.9) | 129 (63.2) | 309 (58.6) |
| Overweight > 28.0 | 269 (36.8) | 69 (33.8) | 200 (38.0) |
Abbreviations: n, number; SD, Standard Deviation; HDB: Housing and Development Board; BMI, Body Mass Index; GDS-15, 15-item Geriatric Depression Scale; GAI-20; 20-item Geriatric Anxiety Inventor; WHO: World Health Organization; CDH: United States National Research Council Committee on Diet and Health. * MMSE scores were re-calculated as out of a total score of 30.
3.1. Macro- and Micronutrient Intakes
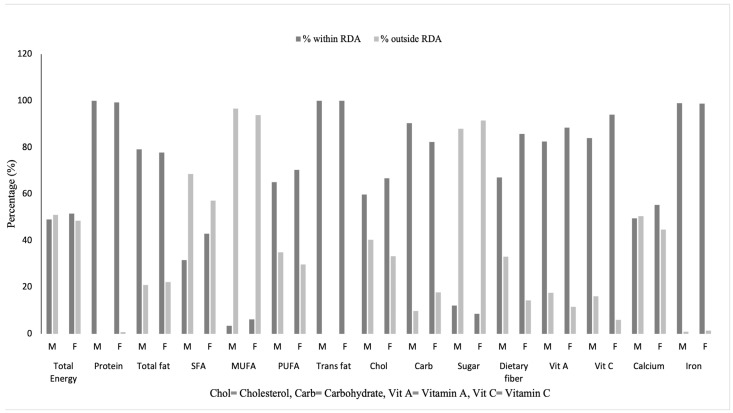
Table 2 shows the intake levels with comparison to the Recommended Dietary Allowances (RDAs). The percentages of males and females meeting the RDA for energy and each of the macro- and micronutrients can be seen in Figure 1. Both males and females had median energy intake (males: 2258 kcal, females: 2058 kcal) within the RDA range based on different physical activity levels. The majority of older adults met the RDA for protein, total fat, and carbohydrate. A proportion of 68.5% males and 57.1% females exceeded the limit for SFAs, PUFAs and MUFAs. The P:M:S ratios for both males and females were 0.50:1.00:1.00 (Table 2). The majority (males: 59.7%, females: 66.7%) had a median intake of cholesterol within the recommended limit of 300 mg daily. Almost all males (87.9%) and females (91.5%) exceeded the intake limit for sugar. The majority of older adults met the requirements for vitamin A (males: 82.5%, females: 88.5%), vitamin C (males: 84%, females: 94%) and iron (males: 99.0%, females: 98.7%). A proportion of 50.5% of males and 44.7% of females had calcium intakes lesser than 70% of their RDA. The majority of females (85.7%) met the RDA for dietary fiber, while 33% of males had inadequate dietary fiber intake. In the sensitivity analysis, one participant with severe cognitive impairment was removed from the analysis to reduce recall bias, but this did not change the results.
Table 2.
Macro- and micronutrient intakes with comparison to the Recommended Dietary Allowances.
| Nutrients | 25% | Median | 75% | % Energy Intake | RDA | % within RDA | % under RDA | % over RDA | p-Value (Mann–Whitney) ^ | Chi-Squared Test # |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Energy, E (kcal) | ||||||||||
| Male | 1743 | 2258 | 2853 | - | 1885–3070 | 49.0 | 32.0 | 18.9 | 0.016 | - |
| Female | 1656 | 2058 | 2633 | - | 1570–2560 | 51.5 | 20.9 | 27.6 | ||
| Protein (g) | 10–15% of total E | |||||||||
| Male | 67.1 | 88.4 | 113 | 15.6 | 36.4 | 0.0 | 63.6 | 0.263 | - | |
| Female | 63.6 | 87.0 | 107 | 16.1 | 31.4 | 0.7 | 67.9 | |||
| Total fat (g) | 20–35% of total E | |||||||||
| Male | 57.6 | 74.0 | 99.9 | 30.4 | 79.1 | 2.9 | 18.0 | 0.025 | - | |
| Female | 51.2 | 68.9 | 92.0 | 29.9 | 77.8 | 5.6 | 16.5 | |||
| Saturated fat (g) | <10% of total E | χ2(1) = 7.9260, p = 0.005 |
||||||||
| Male | 19.7 | 27.2 | 36.7 | 11.1 | 31.6 | - | 68.5 | 0.002 | ||
| Female | 17.7 | 24.3 | 32.8 | 10.5 | 42.9 | - | 57.1 | |||
| Monounsaturated fat (g) | 15–20% of total E | |||||||||
| Male | 19.9 | 27.5 | 37.5 | 11.3 | - | - | - | 0.026 | - | |
| Female | 19.0 | 25.2 | 35.0 | 11.1 | - | - | - | |||
| Polyunsaturated fat (g) | 5–10% of total E | |||||||||
| Male | 10.0 | 14.0 | 19.9 | 5.7 | - | - | - | 0.511 | - | |
| Female | 10.2 | 13.8 | 18.7 | 6.0 | - | - | - | |||
| P: M: S ratio | 1.00: 1.00: 1.00 | |||||||||
| Male | 0.50:1.00:1.00 | - | - | - | - | - | - | |||
| Female | 0.50:1.00:1.00 | - | - | - | - | |||||
| Trans fat (g) | negligible intake | 0% of total E | ||||||||
| Male | 0.246 | 0.361 | 0.476 | 100 | 0 | - | - | |||
| Female | 0.251 | 0.338 | 0.470 | 100 | - | 0 | ||||
| Cholesterol (mg) | 0.018 | χ2(1) = 3.2076, p = 0.073 |
||||||||
| Male | 193 | 270 | 372 | <300 | 59.7 | - | 40.3 | |||
| Female | 170 | 250 | 326 | <300 | 66.7 | - | 33.3 | |||
| Carbohydrate (g) | 45–65% of total E | |||||||||
| Male | 234 | 297 | 389 | 53.3 | 90.3 | 5.8 | 3.9 | 0.010 | - | |
| Female | 222 | 271 | 343 | 53.3 | 82.3 | 11.7 | 6.0 | |||
| Sugar (g) | keep at minimal | χ2(1) = 2.3389, p = 0.126 |
||||||||
| Male | 61.0 | 80.9 | 107 | 14.7 | 12.1 | - | 87.9 | 0.556 | ||
| Female | 58.4 | 77.8 | 102 | 15.3 | 8.5 | - | 91.5 | |||
| Dietary fiber (g) | χ2(1) = 33.1500, p < 0.001 |
|||||||||
| Male | 16.1 | 22.0 | 28 | - | 26 | 67.0 * | 33 | - | 0.761 | |
| Female | 16.8 | 22.3 | 28.9 | - | 20.4 | 85.7 * | 14.3 | - | ||
| Vitamin A (mcg) | χ2(1) = 4.6978, p = 0.030 |
|||||||||
| Male | 602 | 894 | 1146 | - | 750 | 82.5 * | 17.5 | - | 0.015 | |
| Female | 713 | 958 | 1263 | - | 750 | 88.5 * | 11.5 | - | ||
| Vitamin C (mg) | χ2(1) = 18.5049, p < 0.001 |
|||||||||
| Male | 88 | 125 | 170 | - | 105 | 84.0 * | 16 | - | 0.015 | |
| Female | 102 | 140 | 188 | - | 85 | 94.0 * | 6 | - | ||
| Calcium (mg) | χ2(1) = 1.9735, p = 0.160 |
|||||||||
| Male | 476 | 690 | 961 | - | 1000 | 49.5 * | 50.5 | - | 0.161 | |
| Female | 528 | 745 | 996 | - | 1000 | 55.3 * | 44.7 | - | ||
| Iron (mg) | χ2(1) = 0.1467, p = 0.702 |
|||||||||
| Male | 12.0 | 16.4 | 21.7 | - | 8 | 99.0 * | .97 | - | 0.495 | |
| Female | 12.2 | 16.1 | 20.0 | - | 8 | 98.7 * | 1.3 | - | ||
RDA: Recommended Dietary Allowances. * Meeting 70% of RDA. ^ Sex differences in median nutrient intakes. # Sex differences in proportion of DRI consumed.
Figure 1.
Percentages of males and females meeting the Recommended Dietary Allowances (RDA).
3.2. Malnutrition Risk
The NSI Determine found that 15.9% of all, 17.0% of males and 15.4% in females were at moderate nutritional risk. A high nutritional risk was found in 6.4% of participants (males: 5.8%, females: 6.6%). No statistically significant differences in risk were observed on sex (χ2(2) = 0.3783, p < 0.828). The questions with the most positive answers included taking three or more different prescribed or over-the-counter drugs a day (30.5%), eating alone most of the time (24.1%), or having an illness or condition that made them change the kind and/or amount of food they eat (22.2%) (Table 3).
Table 3.
Frequency of positive answers to the questions constituting the NSI Determine Checklist, n (%).
| NSI Determine Checklist Questions | All | Males | Females |
|---|---|---|---|
| 1. I have an illness or condition that made me change the kind and/or amount of food I eat | 164 (22.2) | 44 (21.5) | 120 (22.8) |
| 2. I eat fewer than 2 meals per day | 43 (5.8) | 9 (4.4) | 34 (6.4) |
| 3. I eat few fruits or vegetable or milk products (less than once a day) | 74 (10.0) | 24 (11.8) | 50 (9.4) |
| 4. I have 3 or more drinks of beer, liquor or wine almost every day | 6 (0.8) | 4 (1.95) | 2 (0.38) |
| 5. I have tooth or mouth problems that make it hard to eat | 37 (5.0) | 10 (4.9) | 27 (5.1) |
| 6. I don’t always have enough money to buy the food I need | 7 (0.90) | 2 (0.97) | 5 (0.94) |
| 7. I eat alone most of the time | 178 (24.1) | 46 (22.3) | 132 (24.8) |
| 8. I take 3 or more different prescribed or over-the-counter drugs a day | 225 (30.5) | 68 (33.0) | 157 (29.5) |
| 9. I have lost 10 pounds (4.5 kg) in the last 6 months unintentionally | 5 (0.70) | 1 (0.49) | 4 (0.75) |
| 10. I am not always physically able to shop, cook and/or feed myself | 2 (0.30) | 0 (0.0) | 2 (0.38) |
| Aggregate score in the NSI scale, mean ± SD | 1.5 ± 2.1 | 1.5 ± 2.1 | 1.5 ± 2.1 |
3.3. Dietary Practices
Table 4 shows the dietary practices among older adults. Monounsaturated oil (e.g., olive oil and canola oil) (40.7%) was the most commonly used oil for cooking at home, followed by polyunsaturated oils (e.g., corn oil and sunflower oil) (36.0%) and blended vegetable oil (22.1%). Only a small number of older adults used saturated oil such as butter, ghee and lard for cooking at home (1.2%). There was no difference in the choices of oil/fat between sex. The most common types of milk/milk substitute used in beverages (tea, coffee, malt beverages) were sweetened condensed milk (19.0%) and creamer (18.8%). Low-fat milk/powder (12.2%) was used more widely than full cream milk/powder (5.0%) and skimmed milk/powder (2.2%). A proportion of 5.2% used evaporated milk, whereas 38.4% of the older adults did not add any milk/milk substitutes to their beverages. Males (21.9%) were more likely to use sweetened condensed milk than females (17.5%), and females (13.2%) were more likely to used low-fat milk/powder than males (9.9%). When ordering beverages or desserts, 43.9% of males and 46.9% of females would ask for less sugar/less sweet options.
Table 4.
Use of cooking oils, milk/milk substitutes and sugar/sweet options among older adults.
| n (%) | ||
|---|---|---|
| Type of Oil Used for Cooking | Male | Female |
| Blended vegetable oil | 96 (23.7) | 239 (21.5) |
| Polyunsaturated oil | 135 (33.3) | 411 (37.0) |
| Monounsaturated oil | 168 (41.5) | 449 (40.4) |
| Saturated oil | 6 (1.5) | 12 (1.1) |
| p-value (Chi-square) | 0.5 | |
| Types of milk/milk substitute used in beverages | Male | Female |
| Creamer | 9 (21.9) | 181 (17.0) |
| Sweetened condensed milk | 93 (21.5) | 186 (18.0) |
| Evaporated milk | 28 (6.5) | 49 (4.7) |
| Full cream milk/power | 14 (3.2) | 52 (5.0) |
| Low-fat milk/powder | 43 (9.9) | 137 (13.2) |
| Skimmed milk/powder | 3 (0.7) | 23 (2.2) |
| No added milk | 157 (36.3) | 408 (39.3) |
| Whitener | 0 (0.0) | 1 (0.1) |
| Ask for less sugar/less sweet | Male | Female |
| No | 231 (56.1) | 565 (53.1) |
| Yes | 181 (43.9) | 499 (46.9) |
| p-value (Chi-square) | 0.3 | |
3.4. Nutrition Knowledge
As shown in Table 5, 57.3% of all participants scored 7 or above out of a total score of 12, with no difference in nutrition knowledge between sex (χ2(2) = 4.4421, p = 0.108). A percentage of 37.5% of participants had a moderate, and 5.1% had a low level of nutrition knowledge. A proportion of 47.8% reported that they always pay attention to dietary and nutrition information, followed by 34.5%, sometimes and 14.1%, seldomly pay attention to dietary and nutrition information. No difference was found between sex (χ2(3) = 3.3430, p = 0.342) The top three most important sources of nutrition information for the older adults were book/newspaper/magazine, TV/radio, internet (77.4%), relatives, friends and neighbors (32.0%), and medical practitioners, nurses, dietitians (16.5%) (Table 6).
Table 5.
Nutrition knowledge and acquisition.
| n (%) | |||
|---|---|---|---|
| Scores to answering questions on ‘diet can be related to certain diseases.’ | All | Male | Female |
| Low (0–3) | 38 (5.1) | 16 (7.8) | 22 (4.1) |
| Moderate (4–6) | 277 (37.5) | 79 (38.4) | 198 (37.2) |
| High (7 or above) | 423 (57.3) | 111 (53.9) | 312 (58.7) |
| p-value (Chi-square) | 0.1 | ||
| Do you pay attention to dietary and nutrition information? | All | Male | Female |
| Always | 346 (47.8) | 90 (44.6) | 256 (49.0) |
| Sometimes | 250 (34.5) | 68 (33.7) | 182 (34.9) |
| Seldom | 102 (14.1) | 35 (17.3) | 67 (12.8) |
| I don’t know | 26 (3.6) | 9 (4.5) | 17 (3.3) |
| p-value (Chi-square) | 0.3 | ||
Note: non-respondence treated as ‘I don’t know’.
Table 6.
Sources of nutrition information for older adults (multiple choice).
| Rank | Sources of Nutrition Information | n (%) |
|---|---|---|
| 1 | book/newspaper/magazine, TV/radio, internet | 571 (77.4) |
| 2 | relatives, friends and neighbors | 236 (32.0) |
| 3 | medical practitioners, nurses, dietitians | 122 (16.5) |
| 4 | courses or lectures | 54 (7.3) |
| 5 | spouse | 27 (3.7) |
| 6 | children | 27 (3.7) |
| 7 | salespeople | 17 (2.3) |
4. Discussion
Older adults are more vulnerable to nutritional deficiencies and unhealthy eating. Globally, the prevalence of nutritional deficiency or malnutrition ranges from 0.8% to 24.6% [23]. Malnutrition can lead to poor wound healing, increased propensity for developing infections [5] and anemia [24], while poor dietary choices along with unhealthy lifestyles are associated with an increased risk of diabetes [25], hypertension [26], heart diseases [27] and dementia [28,29]. To promote good nutrition and provide optimal care in community-dwelling older adults, one must first identify nutrition problems, and then implement nutrition strategies to alleviate the effect of poor nutrition and prevent future incidence. Yet, there is still a lack of data on the adequacy of nutrient intake and prevalence of malnutrition risk in older adults in Asian countries. Therefore, the present study combined detailed clinical and dietary measures, and malnutrition risk screening to make inference on the nutritional status of community-dwelling older adults in Singapore.
In the current sampling cohort of older adults, more than 50% of older adults met the RDA for energy, protein, vitamin A, vitamin C and iron. These results are encouraging as previous studies have suggested that Singaporean older adults are likely to be deficient in protein, vitamins and minerals [17,30] However, there were also some less optimistic findings. It was found that almost half of older adults failed to meet calcium recommendations. Calcium has an important role in the prevention of bone mass loss and osteoporotic fractures [31,32]. Calcium absorption is impaired in the later decades of life, and requirements increases from 800 mg to 1000 mg per day after the age of 50. Ho et al. (2004) suggested that at least 900 mg per day of dietary calcium intake is needed to prevent bone loss in Asian postmenopausal women [33]. According to the National Nutrition Survey (NNS) 2010, a low calcium intake could be due to the low intakes of dairy foods such as milk, yoghurt, and cheese in the older adults [21]. Moreover, it was reported that 50% of Singaporean residents aged 18 to 69 do not consume any milk, with older adults consuming the least amount of milk [21]. Moreover, the older adults reported not enjoying drinking milk and lacked awareness of alternative calcium sources or even the existence of calcium [21]. Therefore, there is an urgent need for public health measures to prevent health consequences associated with calcium deficiencies. This could be in the form of health education or the prescription of calcium and vitamin D supplements by health professionals for those at-risk groups.
Furthermore, Singaporean older adults are exceeding the recommended limits for saturated fat (SFA) and sugar and have comparably low intakes for polyunsaturated fat (PUFA) and monounsaturated fat (MUFA). A diet high in SFAs and sugar, and low in PUFAs and MUFAs is associated with higher blood pressure [34] and cholesterol [35], and increased risks for obesity, type 2 diabetes, heart diseases [27], and cognitive decline [36,37]. Around 50% of older adults were found to have high blood pressure and high cholesterol in this study, highlighting the need for public health intervention. Based on the dietary practice survey, we did not identify sources of saturated fat. However, the NNS 2010 suggested that saturated fat intakes were likely to come from plant-based sources such as coconut oil and coconut milk, which are commonly used in local Malay and Indian dishes. Other major contributors of saturated fat included biscuits, pastries, cakes, snacks and local snacks [21]. These foods are also high in added sugar. The dietary guideline for Singaporeans suggests that consumption of sugar should be no more than 10% of the daily energy intake [38], but 90.5% of older adults exceeded this intake limit. This could be due to the common dietary practices found in the older adults, such as adding sweetened condensed milk and sugar to beverages and desserts. The prevalence of type 2 diabetes was found to be 18% in the representative Singaporean older adult population, which was very close to the global estimate of 19.3% in adults 65 years or older [39]. We are one of the rare studies to provide regional sources of diabetes prevalence on those aged 65 years and over, and the evidence continues to point to diabetes as a significant global chronic disease burden in ageing populations.
Dietary fiber has important roles to play in lowering blood cholesterol and sugar, and hence reducing the risk of heart diseases [40,41] and type 2 diabetes [42]. Dietary fiber can be found abundantly in whole-grain products, fruits, vegetables, legumes, and nuts and seeds. It was found that 33% male older adults had inadequate dietary fiber intake and were significantly more likely to have insufficient dietary fiber intake compared to female older adults. According to NNS 2010, three in four adult Singapore residents could not meet the Dietary Guidelines of eating at least two servings of fruit daily, and seven in ten could not meet the two-servings-a-day recommendation for vegetables. Moreover, a recent study found that one in every four Singaporeans would choose to dine out every day [43]. A higher rate of eating out has been associated with poorer diet quality, characterized by greater energy, sugar, sodium and SFA intakes and lower dietary fiber, fruit, vegetable, and micronutrient intakes [44]. Whether the same eating-out pattern is found in the older adult population requires further investigation.
There are many factors affecting the nutritional intake and dietary choices among the older people. For example, living alone or with others would influence dietary habits and quality of life among the older adult population. When cooking for one, older adults may choose quick, nutritionally suboptimal meals such as tea and toast over cooking and enjoying a ‘proper meal’ [45]. The small proportion of older adults living alone in the present study could partly explain the low proportions of micronutrient deficiencies identified. Nutritional knowledge is another factor shown to positively affect eating in older adults [46]. Despite low education levels in our sample, over 90% of them had moderate to high levels of nutritional knowledge, and majority reported that they pay attention to dietary and nutrition information. However, this could not explain for the high saturated fat and sugar intakes and low intakes of calcium and dietary fiber in males in the older adults. It has been suggested that nutritional knowledge could only explain one’s ability to understand food-related and nutrition-related terminology and not the attitudes and beliefs around the individual’s eating behavior toward food. Studies have also suggested that healthy eating in older adults is multi-faceted and is determined by both individual (e.g., age, sex, education, beliefs and behaviors) and collective (accessible food labels, food shopping environment, social support) factors [47]. As a result, studies are warranted to understand contributors to healthy eating to facilitate the development of programs and services designed to encourage healthy eating.
According to the NSI Determine Your Health checklist, 6.4% of the older adults were at high malnutrition risk. This is consistent with previous findings from the Singapore Longitudinal Ageing Study (SLAS) [48,49]. However, there was a reduction in the percentage of moderate risk compared to SLAS (15.9% vs. 24.7%) [49]. Given that both DaHA and SLAS used the NSI checklist for the screening of malnutrition risk, the discrepancies could be due to the different recruitment periods between studies. The recruitment periods for SLAS were 2003 to 2004, and 2009 to 2013, whereas the recruitment period for DaHA was 2011 to 2017. Therefore, the finding from the latter could be reflective of a reduction in malnutrition risk in community-dwelling older adults. Compared to other malnutrition screening tools, the NSI checklist had the advantage of being quick and less invasive (i.e., does not require blood indicators). It also helped to raise awareness in older adults of factors that affect their nutritional health and encourage them to improve their dietary and lifestyle habits to reduce their risk of nutrition-related health problems. The malnutrition screening will also help construct public health interventions, which will incorporate risk factors identified to construct more targeted nutritional health interventions for the local older adult population.
5. Conclusions
The current study reported, for the first time, the adequacy of nutrient intakes and malnutrition risk of the community-dwelling older adult population in Singapore. Attention is needed towards the excessive intakes of saturated fat and sugar, and the inadequate intakes of calcium and dietary fiber from diet alone. Nutrition advice for older adults needs to focus on the selection of nutrient-dense foods, and to replace excessive saturated fat and sugar intakes with intakes of dairy and high-fiber products while ensuring nutrient adequacy. Screening for calcium deficiency should be part of routine health check-ups, along with nutrition education on the importance of calcium in a healthy balanced diet. Therefore, the early identification and understanding of the nutrition needs is the key to prevention of malnutrition risk and associated diseases in this growing segment of the population.
6. Limitations and Strengths
The current study was not without limitations. First, there was a potential bias in the recruitment procedure. Recruitments were conducted in community settings and those who were most likely to be malnourished were less inclined to attend and be recruited into the study. However, subjects were offered financial incentives to promote participations. Second, FFQs are not the best dietary assessment tool for older adults due to their reliance on memory, and the results may be influenced by factors such as social desirability bias. However, the FFQ used in this study was carried across from the NNS 2010 survey, which has been validated in the Singapore population. Third, intakes for sodium (added salt), which taken in excess is associated with high blood pressure and cardiovascular risk [50], was not examined. Fourth, we did not look at supplementation use, but our findings suggest that nutrient intake from diet alone was adequate for most micronutrients except calcium. Nevertheless, the present study had its strengths. It is one of the very rare studies in Asian countries, and the first in Singapore, to report on the nutrient intake of community older adults. Factors that could have contributed to the observed nutrition intake were also examined and served importance in public health promotion.
Acknowledgments
The authors would like to thank the Training and Research Academy at Jurong Point (TARA@JP), the Lee Kim Tah Holding Ltd., Singapore, the Kwan Im Thong Hood Cho Temple, Singapore, and the Presbyterian Community Services for their support.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15153446/s1, Text S1: Nutritional Knowledge questionnaire; Figure S1: Flowchart of selection process.
Author Contributions
L.F. designed the research; L.F. and K.X.Y. conducted the research; K.X.Y. conducted the statistical data analysis and worked with L.F., L.S., S.L.L., J.L., B.K.K. and A.B.M. to draft the paper. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study obtained approval from the National University of Singapore Institutional Review Board [Reference number 10-517], 8 July 2011.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Requests for access to the DaHA data will be considered on a case-to-case basis. Request should be submitted to Lei Feng, who may be contacted by email (pcmfl@nus.edu.sg).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
The study is supported by the following grants awarded to Lei Feng: the National Medical Research Council of Singapore [grant numbers NMRC/TA/0053/2016 and NMRC/CSA/0009/2022].
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Brownie S. Why are elderly individuals at risk of nutritional deficiency? Int. J. Nurs. Pract. 2006;12:110–118. doi: 10.1111/j.1440-172X.2006.00557.x. [DOI] [PubMed] [Google Scholar]
- 2.Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care. Nutr. Diet. 2009;66:S1–S34. doi: 10.1111/j.1747-0080.2009.01383.x. [DOI] [Google Scholar]
- 3.Saunders J., Smith T. Malnutrition: Causes and consequences. Clin. Med. 2010;10:624–627. doi: 10.7861/clinmedicine.10-6-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim S.L., Ong K.C., Chan Y.H., Loke W.C., Ferguson M., Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin. Nutr. 2012;31:345–350. doi: 10.1016/j.clnu.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Beers M.H. The Merck manual of geriatrics. Aorn J. 2000;73:711. [Google Scholar]
- 6.Ramic E., Pranjic N., Batic-Mujanovic O., Karic E., Alibasic E., Alic A. The effect of loneliness on malnutrition in elderly population. Med. Arh. 2011;65:92–95. [PubMed] [Google Scholar]
- 7.Walker D., Beauchene R.E. The relationship of loneliness, social isolation, and physical health to dietary adequacy of independently living elderly. J. Am. Diet. Assoc. 1991;91:300–304. doi: 10.1016/S0002-8223(21)01111-1. [DOI] [PubMed] [Google Scholar]
- 8.Ferry M., Sidobre B., Lambertin A., Barberger-Gateau P. The SOLINUT study: Analysis of the interaction between nutrition and loneliness in persons aged over 70 years. J. Nutr. Health Aging. 2005;9:261–268. [PubMed] [Google Scholar]
- 9.Kobayashi L.C., Steptoe A. Social Isolation, Loneliness, and Health Behaviors at Older Ages: Longitudinal Cohort Study. Ann. Behav. Med. 2018;52:582–593. doi: 10.1093/abm/kax033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishikawa M., Takemi Y., Yokoyama T., Kusama K., Fukuda Y., Nakaya T., Nozue M., Yoshiike N., Yoshiba K., Hayashi F., et al. “Eating Together” Is Associated with Food Behaviors and Demographic Factors of Older Japanese People Who Live Alone. J. Nutr. Health Aging. 2017;21:662–672. doi: 10.1007/s12603-016-0805-z. [DOI] [PubMed] [Google Scholar]
- 11.Cohen C. Social and economic factors in the nutrition of the elderly. Proc. Nutr. Soc. 1974;33:51–57. doi: 10.1079/PNS19740010. [DOI] [PubMed] [Google Scholar]
- 12.Hank K., Erlinghagen M. Perceptions of job security in Europe’s ageing workforce. Soc. Indic. Res. 2011;103:427–442. doi: 10.1007/s11205-010-9710-8. [DOI] [Google Scholar]
- 13.Denny A. An overview of the role of diet during the ageing process. Br. J. Community Nurs. 2008;13:58–67. doi: 10.12968/bjcn.2008.13.2.28157. [DOI] [PubMed] [Google Scholar]
- 14.Yu R., Sun Y., Ye K.X., Feng Q., Lim S.L., Mahendran R., Cheah I.K.-M., Foo R.S.Y., Chua R.Y., Gwee X., et al. Cohort profile: The Diet and Healthy Aging (DaHA) study in Singapore. Aging. 2020;12:23889–23899. doi: 10.18632/aging.104051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neelakantan N., Whitton C., Seah S., Koh H., Rebello S.A., Lim J.Y., Chen S., Chan M.F., Chew L., van Dam R.M. Development of a Semi-Quantitative Food Frequency Questionnaire to Assess the Dietary Intake of a Multi-Ethnic Urban Asian Population. Nutrients. 2016;8:528. doi: 10.3390/nu8090528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Nutrition, Ministry of Health . A Compendium of Food Pictures: For Dietitians and Nutritionists. Department of Nutrition, Ministry of Health; Singapore: 1999. [Google Scholar]
- 17.Healthhub Recommended Dietary Allowances. [(accessed on 28 February 2022)]. Available online: https://www.healthhub.sg/live-healthy/192/recommended_dietary_allowances.
- 18.Medicine I.O. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. The National Academies Press; Washington, DC, USA: 2005. p. 1358. [Google Scholar]
- 19.Krauss R.M., Eckel R.H., Howard B., Appel L.J., Daniels S.R., Deckelbaum R.J., Erdman J.W., Jr., Kris-Etherton P., Goldberg I.J., Kotchen T.A., et al. AHA Dietary Guidelines: Revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation. 2000;102:2284–2299. doi: 10.1161/01.CIR.102.18.2284. [DOI] [PubMed] [Google Scholar]
- 20.Cheong T. Fibre: Health Benefits and Best Food Sources. [(accessed on 28 March 2022)]. Available online: https://www.healthxchange.sg/food-nutrition/food-tips/dietary-fibre-health-benefits-sources-fibre.
- 21.Report of the National Nutrition Survey 2010. Health Promotion Board; Singapore: 2010. [Google Scholar]
- 22.Barrocas A., Bistrian B.R., Blackburn G.L., Chernoff R., Lipschitz D.A., Cohen D., Dwyer J., Rosenberg I.H., Keller G.C., Wellman N.S., et al. Appropriate and Effective Use of the NSI Checklist and Screens. J. Am. Diet. Assoc. 1995;95:647–648. doi: 10.1016/S0002-8223(95)00177-8. [DOI] [PubMed] [Google Scholar]
- 23.Crichton M., Craven D., Mackay H., Marx W., de van der Schueren M., Marshall S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing. 2019;48:38–48. doi: 10.1093/ageing/afy144. [DOI] [PubMed] [Google Scholar]
- 24.Chatta G., Lipschitz D. Anemia. In: Hazzard W., Blass J., Halter J., Ouslander J., Tinetti M., editors. Principles of Geriatric Medicine and Gerontology. 5th ed. Volume 20. McGraw-Hill; New York, NY, USA: 2003. pp. 771–777. [Google Scholar]
- 25.Sami W., Ansari T., Butt N.S., Hamid M.R.A. Effect of diet on type 2 diabetes mellitus: A review. Int. J. Health Sci. 2017;11:65–71. [PMC free article] [PubMed] [Google Scholar]
- 26.Cherfan M., Vallée A., Kab S., Salameh P., Goldberg M., Zins M., Blacher J. Unhealthy behaviors and risk of uncontrolled hypertension among treated individuals-The CONSTANCES population-based study. Sci. Rep. 2020;10:1925. doi: 10.1038/s41598-020-58685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller V., Micha R., Choi E., Karageorgou D., Webb P., Mozaffarian D. Evaluation of the Quality of Evidence of the Association of Foods and Nutrients With Cardiovascular Disease and Diabetes: A Systematic Review. JAMA Netw. Open. 2022;5:e2146705. doi: 10.1001/jamanetworkopen.2021.46705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sullivan D., Johnson L. Nutrition and aging. In: Hazzard W., Blass J., Halter J., Ouslander J., Tinetti M., editors. Principles of Geriatric Medicine and Gerontology. 5th ed. McGraw-Hill; New York, NY, USA: 2003. pp. 1151–1169. [Google Scholar]
- 29.Zhou Y.-F., Song X.-Y., Pan X.-F., Feng L., Luo N., Yuan J.-M., Pan A., Koh W.-P. Association Between Combined Lifestyle Factors and Healthy Ageing in Chinese Adults: The Singapore Chinese Health Study. J. Gerontol. Ser. A. 2021;76:1796–1805. doi: 10.1093/gerona/glab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tay M.E., Ong S.H., Ho X.L., Tsen S.Y., Chu G., Loong C., Khaw R., Lee J.M.K., Loke W.M. Nutrition deficiency risk assessment of free-living older adults in Singapore. J. Aging Res. Clin. Pract. 2016;5:102–110. doi: 10.14283/jarcp.2016.99. [DOI] [Google Scholar]
- 31.Dawson-Hughes B., Dallal G.E., Krall E.A., Sadowski L., Sahyoun N., Tannenbaum S. A Controlled Trial of the Effect of Calcium Supplementation on Bone Density in Postmenopausal Women. N. Engl. J. Med. 1990;323:878–883. doi: 10.1056/NEJM199009273231305. [DOI] [PubMed] [Google Scholar]
- 32.Tang B.M., Eslick G.D., Nowson C., Smith C., Bensoussan A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: A meta-analysis. Lancet. 2007;370:657–666. doi: 10.1016/S0140-6736(07)61342-7. [DOI] [PubMed] [Google Scholar]
- 33.Ho S.C., Chen Y.M., Woo J.L., Lam S.S. High habitual calcium intake attenuates bone loss in early postmenopausal Chinese women: An 18-month follow-up study. J. Clin. Endocrinol. Metab. 2004;89:2166–2170. doi: 10.1210/jc.2003-031338. [DOI] [PubMed] [Google Scholar]
- 34.Sabour H., Norouzi-Javidan A., Soltani Z., Mousavifar S.A., Latifi S., Emami-Razavi S.H., Ghodsi S.M. The correlation between dietary fat intake and blood pressure among people with spinal cord injury. Iran. J. Neurol. 2016;15:121–127. [PMC free article] [PubMed] [Google Scholar]
- 35.Siri-Tarino P.W., Sun Q., Hu F.B., Krauss R.M. Saturated fat, carbohydrate, and cardiovascular disease. Am. J. Clin. Nutr. 2010;91:502–509. doi: 10.3945/ajcn.2008.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rippe J., Angelopoulos T. Relationship between Added Sugars Consumption and Chronic Disease Risk Factors: Current Understanding. Nutrients. 2016;8:697. doi: 10.3390/nu8110697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duffy C., Hofmeister J., Nixon J.P., Butterick T. High fat diet increases cognitive decline and neuroinflammation in a model of orexin loss. Neurobiol. Learn. Mem. 2019;157:41–47. doi: 10.1016/j.nlm.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee B.L. Dietary Guidelines in Singapore. Asia Pac. J. Clin. Nutr. 2011;20:472–476. [PubMed] [Google Scholar]
- 39.Sinclair A., Saeedi P., Kaundal A., Karuranga S., Malanda B., Williams R. Diabetes and global ageing among 65–99-year-old adults: Findings from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2020;162:108078. doi: 10.1016/j.diabres.2020.108078. [DOI] [PubMed] [Google Scholar]
- 40.Soliman G.A. Dietary Fiber, Atherosclerosis, and Cardiovascular Disease. Nutrients. 2019;11:1155. doi: 10.3390/nu11051155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brum J., Ramsey D., McRorie J., Bauer B., Kopecky S.L. Meta-Analysis of Usefulness of Psyllium Fiber as Adjuvant Antilipid Therapy to Enhance Cholesterol Lowering Efficacy of Statins. Am. J. Cardiol. 2018;122:1169–1174. doi: 10.1016/j.amjcard.2018.06.040. [DOI] [PubMed] [Google Scholar]
- 42.McRae M.P. Dietary Fiber Intake and Type 2 Diabetes Mellitus: An Umbrella Review of Meta-analyses. J. Chiropr. Med. 2018;17:44–53. doi: 10.1016/j.jcm.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Naidoo N., van Dam R.M., Ng S., Tan C.S., Chen S., Lim J.Y., Chan M.F., Chew L., Rebello S.A. Determinants of eating at local and western fast-food venues in an urban Asian population: A mixed methods approach. Int. J. Behav. Nutr. Phys. Act. 2017;14:69. doi: 10.1186/s12966-017-0515-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gesteiro E., García-Carro A., Aparicio-Ugarriza R., González-Gross M. Eating out of Home: Influence on Nutrition, Health, and Policies: A Scoping Review. Nutrients. 2022;14:1265. doi: 10.3390/nu14061265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Whitelock E., Ensaff H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients. 2018;10:413. doi: 10.3390/nu10040413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeruszka-Bielak M., Kollajtis-Dolowy A., Santoro A., Ostan R., Berendsen A.A.M., Jennings A., Meunier N., Marseglia A., Caumon E., Gillings R., et al. Are Nutrition-Related Knowledge and Attitudes Reflected in Lifestyle and Health Among Elderly People? A Study Across Five European Countries. Front. Physiol. 2018;9:994. doi: 10.3389/fphys.2018.00994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin W., Lee Y.W. Nutrition knowledge, attitudes and dietary restriction behaviour of Taiwanese elderly. Asia Pac. J. Clin. Nutr. 2005;14:221–229. [PubMed] [Google Scholar]
- 48.Chye L., Wei K., Nyunt M.S.Z., Gao Q., Wee S.L., Ng T.P. Strong Relationship between Malnutrition and Cognitive Frailty in the Singapore Longitudinal Ageing Studies (SLAS-1 and SLAS-2) J. Prev. Alzheimers Dis. 2018;5:142–148. doi: 10.14283/jpad.2017.46. [DOI] [PubMed] [Google Scholar]
- 49.Wei K., Nyunt M.S.Z., Gao Q., Wee S.L., Ng T.P. Frailty and Malnutrition: Related and Distinct Syndrome Prevalence and Association among Community-Dwelling Older Adults: Singapore Longitudinal Ageing Studies. J. Am. Med. Dir. Assoc. 2017;18:1019–1028. doi: 10.1016/j.jamda.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 50.Foote J.A., Giuliano A.R., Harris R.B. Older adults need guidance to meet nutritional recommendations. J. Am. Coll. Nutr. 2000;19:628–640. doi: 10.1080/07315724.2000.10718961. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Requests for access to the DaHA data will be considered on a case-to-case basis. Request should be submitted to Lei Feng, who may be contacted by email (pcmfl@nus.edu.sg).