Abstract
Introduction:
New warning labels for alcohol could reduce alcohol-related health harms. This study examined consumer responses to alcohol warnings with different designs.
Methods:
A national sample of 3,051 U.S. adults completed an online survey in August 2021. Participants were randomized to 1 of 4 warning topics (addiction, liver damage, early death, or colon cancer). Participants viewed 3 labels, presented in random order: 2 types of warning labels (text-only and icon) showing a newly developed warning message about their assigned topic and a text-only control label showing a neutral message. Participants rated each label on effectiveness at discouraging alcohol consumption (primary outcome) and attention (secondary outcome) using 1 to 5 Likert-type scales. Participants also rated warnings with different causal language variants (e.g., “increases risk of,” “contributes to”) and marker words (e.g., “WARNING,” “SURGEON GENERAL WARNING”).
Results:
Both the text-only and icon warnings were perceived as more effective (Average Differential Effects [ADEs]=0.79 and 0.86, respectively) and more attention-grabbing (ADEs=0.43 and 0.69, respectively) than control labels (all ps<0.001). The icon warnings were rated as more effective and attention-grabbing than the text-only warnings (ADEs=0.07 and 0.27, respectively, both ps<0.001). Although all warning topics outperformed the control messages, warnings about addiction were rated as less effective and attention-grabbing than the other topics. A majority (60%) of participants selected “increases risk of” as the most discouraging causal variant and a plurality (47%) selected “SURGEON GENERAL WARNING” as the most discouraging marker word.
Conclusions:
New alcohol warnings could discourage alcohol consumption, especially if warnings include icons.
INTRODUCTION
Alcohol consumption poses substantial health risks, accounting for more than 140,000 deaths per year in the U.S.1–3 Even in light and moderate amounts, alcohol consumption is associated with chronic health problems, including some types of heart disease and cancer.4–11 Despite evidence of the harms of alcohol consumption, two-thirds of U.S. adults report drinking.12
Warning labels are an important tool for ensuring access to information about alcohol’s harms, increasing awareness of these harms, and reducing alcohol-related morbidity and mortality.13,14 However, the current alcohol warning in the U.S. was mandated more than 30 years ago15 and is now out of date. Evidence suggests warnings are likely to be more effective when labels are large,16–19 displayed prominently on the front of product packaging,17,19 and include a pictorial element such as an image or icon.17,19–25 The current U.S. alcohol warning, however, lacks each of these features: it is small, typically appears on the side or back of alcohol containers, and does not include a pictorial element (Figure 1a).26 Research suggests the current warning has had limited impact on overall alcohol consumption.15,27 By contrast, a quasi-experiment from the Yukon Territory in Canada found that displaying large warnings with icons on the front of alcohol containers increased attention to and processing of labels,28 improved recall of drinking guidelines,29 and reduced alcohol sales.30 Additionally, most (though not all31) laboratory and online experiments suggest that large, pictorial warnings can affect drinking-related outcomes including intentions,32 alcohol selection,33,34 and speed of drinking.35
Figure 1.
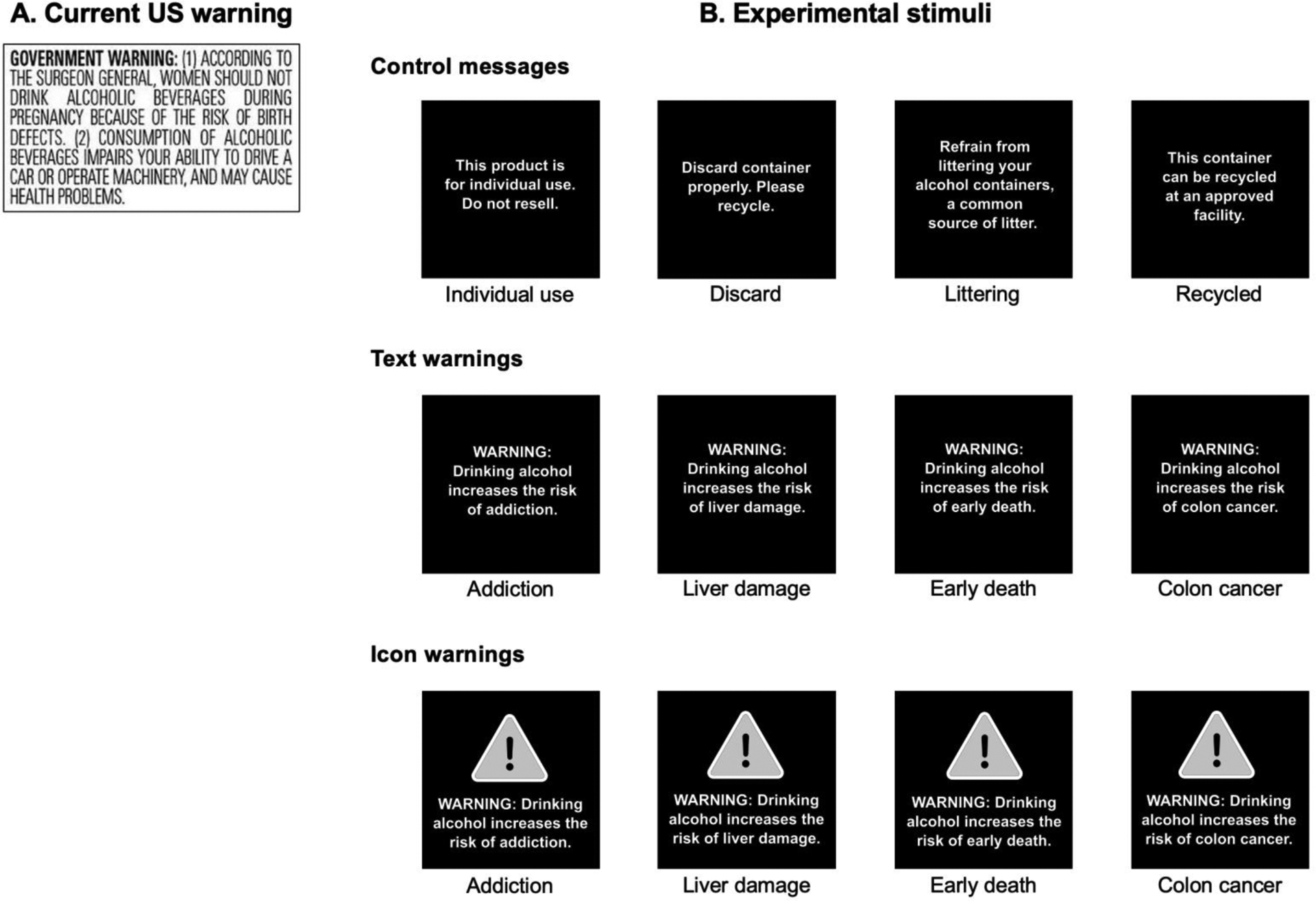
Current warning required in the U.S. (panel A) and experimental stimuli used in the present study (panel B).
Note: The icon warnings were shown in color in the experiment; icons were yellow.
Adopting new, evidence-based warnings on alcohol containers in the U.S. could reduce harmful alcohol consumption, but questions remain about how to design these warnings. For example, studies show that warnings with graphic images are more effective than text-only warnings at reducing selection and consumption of unhealthy products (including alcohol);20,21,25,33,36 it is unknown, however, whether these findings extend to alcohol warnings with icons (i.e., symbolic depictions of the warning message). This is important because warnings with icons may be more politically or legally feasible than warnings with graphic images in some jurisdictions. Additionally, more evidence about which health harms most motivate consumers to reduce their alcohol consumption could guide selection of health topics to address in warnings, particularly given that most studies on alcohol warning topics have been conducted with non-U.S. samples.37–39 Warnings can also communicate causality in different ways (e.g., “contributes to” vs “increases risk of”) and adopt various “marker” words at the beginning of the message (e.g., “WARNING” vs. “GOVERNMENT WARNING”), but it remains unclear how consumers respond to different causal variants38 and marker words40 in alcohol warnings.41
This study aimed to evaluate U.S. adults’ reactions to text-only and text-plus-icon alcohol warnings discussing various warning topics (i.e., health harms). This study also evaluated which causal variants and marker words were perceived as most discouraging alcohol consumption.
METHODS
Study Sample
A national convenience sample of 3,674 adults was recruited in August 2021 by Cloud Research Prime Panels, a survey research firm. Participants were eligible if they lived in the U.S. and were ≥18 years old. Cloud Research focused recruitment efforts such that the sample approximately reflected the U.S. adult population in terms of gender, age, race/ethnicity, and Census region. Online convenience samples can yield generalizable findings for experiments such as the one in this study.42 The Harvard Longwood Campus IRB approved the study.
Procedures
Participants completed an online survey (median completion time, 13.1 minutes). After providing informed consent, participants completed 2 short experimental tasks unrelated to alcohol (one in which they selected their preferred snacks and non-alcoholic beverages and one in which they selected their preferred meals from restaurant menus). Next, participants completed the present experiment about alcohol warnings. The alcohol warnings experiment varied characteristics of warnings using a 4×2 plus control between-within subjects design. First, participants were randomly assigned to 1 of 4 between-subjects conditions representing different warning topics: (1) addiction, (2) liver damage, (3) early death, and (4) colon cancer. These topics were selected based on the epidemiological literature linking alcohol consumption with addiction,7,43–45 liver damage,46,47 early death,47–49 and colon cancer50–52 and to allow assessment of various types of harms. Additionally, prior studies have found that messages about these topics are promising for reducing use of e-cigarettes,22,53 sugary drinks,54,55 red meat,56 and alcohol.33,37,55,57
Participants viewed a message with their assigned warning topic twice, on 2 labels that differed on warning type: (1) a text-only warning (hereafter “text warning”) and (2) a text-plus-icon warning (hereafter “icon warning”). Participants additionally viewed a third label that displayed 1 of 4 randomly assigned control messages. Control messages discussed neutral topics unrelated to alcohol harms (e.g., recycling) using similar length and syntax as the warning messages, similar to prior studies.22,58,59 Participants viewed the 3 types of labels (text warning, icon warning, and control label) in random order. Message type was selected as the within-subjects factor to maximize power to detect differences between text and icon warnings. Appendix Figure 1 depicts the survey flow.
Warning labels were developed following recommendations from prior research.7,25,59,60 First, researchers created warning messages discussing the link between alcohol consumption and each of the 4 warning topics (addiction, liver damage, early death, and colon cancer) using language similar to the sugary drink warning message adopted in San Francisco, CA.61 Messages used simple wording, the marker word “WARNING,” and stronger causal language based on research indicating that these design characteristics enhance warning efficacy.62,63 This study focused on health harms rather than social outcomes because U.S. warnings for alcohol,26 cigarettes,64 and sugary drinks61 each describe health harms.
Next, a professional graphic designer developed 12 different labels: 4 labels for each message type (text warning, icon warning, or control label) (Figure 1b). The 4 text warnings displayed the 4 warning messages in white text centered in a black label, based on food warnings mandated in several Latin American countries65 and similar to prior studies.22,59,62 The 4 icon warnings added an icon above the warning message. The icon depicted an exclamation mark inside a triangle; this design was chosen because it was proposed for sugary drink warnings in California,66 could trigger automatic associations with yield signs,24 and is perceived as dangerous67 and unhealthy.60 The 4 control labels mimicked text warnings, but displayed the neutral control messages.
Measures
First, the survey assessed exposure to the warning label currently required on alcohol containers in the U.S. using an item adapted from the International Tobacco Control Policy Evaluation Survey,68 “Alcohol containers have health warning labels on them. In the last 30 days, how often have you read or looked closely at any of the health warning labels on alcohol containers?” Response options were “all of the time,” “often,” “sometimes,” “rarely,” or “never.”
Next, for the main experimental task, participants viewed 3 labels (text warning, icon warning, control label) one at a time in random order and responded to questions about each label. The primary outcome was perceived effectiveness at discouraging alcohol consumption, assessed using a single item adapted from the UNC Perceived Message Effectiveness Scale69: “How much does this message discourage you from wanting to drink alcohol?” The secondary outcome was attention to the labels, assessed using a single item adapted from studies of cigarette warnings68,70: “How much does this message grab your attention?” Both items used 5-point Likert-type response options ranging from “Not at all” (coded as 1) to “A great deal” (coded as 5). These outcomes were selected because they are predictive of warnings’ potential to influence health behaviors.70–73
Next, to provide additional insights on alcohol warning design, the survey assessed the causal language variant and marker words participants perceived as most effective at discouraging alcohol consumption using additional survey questions shown after participants completed the main experimental task. To identify discouraging causal variants, participants viewed 4 warning messages for alcohol (displayed simultaneously in random arrangement) that varied the causal language used in the warning: “increases risk of,” “contributes to,” “can contribute to,” and “may contribute to.” The warning read: “WARNING: Drinking alcohol [causal variant] stroke” (underlining shown in survey). Participants selected the message that would most discourage them from wanting to drink alcohol, similar to a prior study.63 To identify discouraging marker words, participants viewed 4 warning messages (displayed simultaneously in random arrangement) that varied the marker words used in the warning: “WARNING,” “GOVERNMENT WARNING,” “ALCOHOL AND TOBACCO TAX AND TRADE BUREAU WARNING,” and “SURGEON GENERAL WARNING.” The warnings read: “[MARKER WORDS]: Drinking alcohol increases risk of stroke” (underlining shown in survey). Participants selected the message that would most discourage them from wanting to drink alcohol. To reduce respondent burden, the survey randomly selected a subsample of participants to respond to the causal variant question (n=676) and a separate subsample to respond to the marker words question (n=678).
The survey assessed standard demographic characteristics (e.g., age, gender, race/ethnicity, income) and frequency of alcohol consumption. Alcohol consumption was only assessed among participants aged 21 years or older.
Statistical Analysis
Analyses excluded participants who did not complete the survey or requested their data be excluded in the survey debrief (Appendix Figure 2). Primary analyses included 3,051 participants.
Analyses examined exposure to the current alcohol warning by calculating the proportion of participants who reported reading or looking closely at the current warning all of the time, often, sometimes, rarely, or never. Sensitivity analyses examined exposure among participants who reported consuming alcohol at least 1 day in the prior 30 days.
Analyses of the main experiment used mixed effects linear regression to (1) test the main effect of message type (text warning, icon warning, control label); (2) test the main effect of warning topic (addiction, liver damage, early death, colon cancer); (3) assess whether the impact of message type differed by warning topic; and (4) assess whether the impact of message type differed by demographic characteristics. Models regressed outcomes on indicator variables for each combination of experimental factors plus indicators for the 4 control messages. Models assessing moderation by demographic characteristics additionally included indicator variables representing interactions between message type and participant characteristics. Analyses used the mixed models to estimate average differential effects (ADEs, i.e., differences in predicted means between groups) for each comparison of interest and to test the significance of interaction terms, following standard procedures.74 Sensitivity analyses controlled for the random order in which messages were displayed; results were identical to the uncontrolled analyses, so the uncontrolled analyses are presented. Additional sensitivity analyses examined main effects of the experimental factors among participants who reported consuming alcohol at least 1 day in the prior 30 days.
Finally, analyses examined the proportion of participants who selected each causal language variant and each marker word as most discouraging. All tests were 2-sided and used critical alpha=0.05. Analyses were conducted in 2022 in Stata MP version 17. Prior to data collection, the study questions, predictions, design, and analysis plan were pre-registered on AsPredicted.org (https://aspredicted.org/KZS_DV3). Deviations from this plan are described and justified in Appendix Exhibit 1.
RESULTS
Participants had an average age of 45.6 years (SD=18.7). Approximately 60% identified as women (Table 1; Appendix Table 1 reports characteristics by experimental group). Two-thirds of participants (66%) identified as White and 19% identified as Black. Approximately 13% identified as Latino(a) (regardless of race). One-third had household income less than 150% of the Federal Poverty Level. Among those aged 21 years and older, about 60% reported consuming alcohol on at least 1 day in the prior 30 days. The study sample was similar to the U.S. overall in distributions of age, race, ethnicity, education, and alcohol consumption, but had a higher proportion of females and households with lower income than the U.S. overall (Appendix Table 2).
Table 1.
Participant Characteristics, n=3,051 U.S. Adults
| Characteristic | N (%) |
|---|---|
| Age | |
| 18‒29 years | 775 (25) |
| 30‒44 years | 786 (26) |
| 45‒59 years | 610 (20) |
| ≥60 years | 880 (29) |
| Gender | |
| Female | 1,828 (60) |
| Male | 1,154 (38) |
| Non-binary or another gender | 52 (2) |
| Gay, lesbian, or bisexual | 392 (13) |
| Latino(a) or Hispanic | 386 (13) |
| Race | |
| White | 2,005 (66) |
| Black or African American | 574 (19) |
| American Indian or Alaska Native | 59 (2) |
| Asian or Pacific Islander | 166 (5) |
| Other or Multiracial | 230 (8) |
| Education | |
| High school diploma or less | 907 (30) |
| Some college | 794 (26) |
| College graduate or associates degree | 1,014 (33) |
| Graduate degree | 320 (11) |
| Household income, annual | |
| $0 to $24,999 | 935 (31) |
| $25,000 to $49,999 | 864 (29) |
| $50,000 to $74,999 | 517 (17) |
| ≥$75,000 | 705 (23) |
| Household income <150% Federal Poverty Level | 1,003 (33) |
| Days with alcohol consumption during past 30 days | |
| 0 days | 1,098 (40) |
| 1 to 5 days | 986 (36) |
| ≥6 days | 690 (25) |
| Read or look at current alcohol warning label | |
| Never | 1,481 (49) |
| Rarely | 564 (19) |
| Sometimes | 609 (20) |
| Often | 230 (8) |
| All of the time | 163 (5) |
| Political party identification | |
| Democrat | 1,317 (44) |
| Republican | 789 (26) |
| Independent or another party | 917 (30) |
Note: Missing data ranged from 0.0% to 1.4% for all demographics except for alcohol consumption (9.1%), which was not queried for participants younger than age 21 years. Appendix Table 1 provides sample characteristics by experimental group.
Exposure to the current alcohol warning label was low: only 13% of participants reported reading or looking closely at the label often (8%) or all of the time (5%), while 20% reported reading or looking closely sometimes (Appendix Figure 3). Two-thirds of participants reported they never (49%) or rarely (19%) read or look closely at the current alcohol warnings. Exposure to the current warning was similarly low in sensitivity analyses examining participants who reported consuming alcohol in the past 30 days (Appendix Figure 3).
In the main experimental task examining responses to new alcohol warnings, both the text warnings (ADE=0.79; 95% CI=0.74, 0.83; p<0.001) and the icon warnings (ADE=0.86; 95% CI=0.82, 0.90; p<0.001) received higher ratings on the primary outcome, perceived effectiveness at discouraging alcohol consumption, than the control labels (Figure 2, Appendix Table 3). Moreover, the icon warnings received higher perceived effectiveness ratings than the text warnings (ADE=0.07; 95% CI=0.03, 0.12; p<0.001). Results for the secondary outcome, attention to the labels, followed a similar pattern. Both the text warnings and icon warnings led to higher attention ratings than the control labels (range of ADEs=0.43–0.69, both ps<0.001) and the icon warnings led to higher attention ratings than the text warnings (ADE=0.27; 95% CI=0.22, 0.31; p<0.001, Figure 2, Appendix Table 3).
Figure 2.
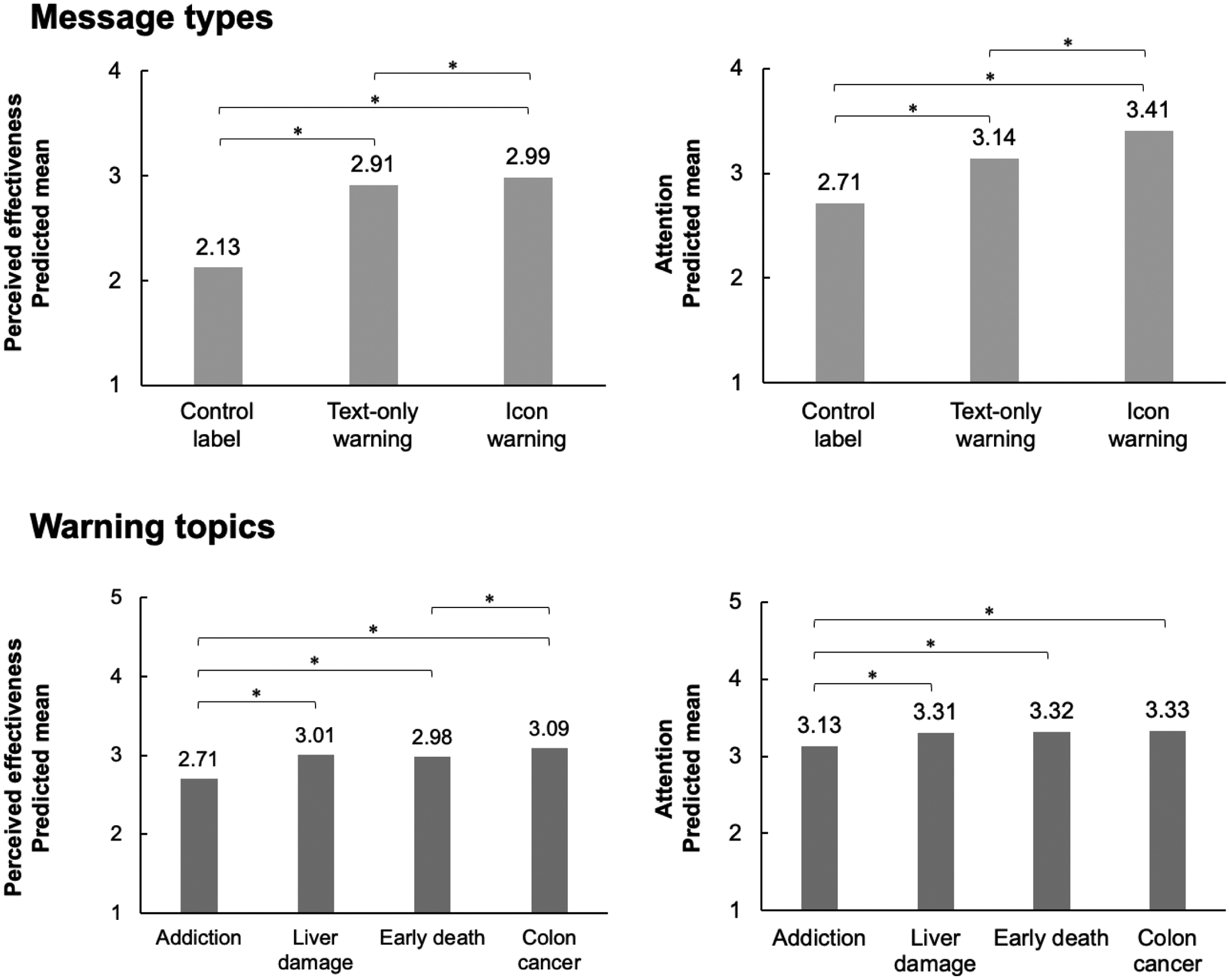
Perceived effectiveness and attention by message type and warning topic, n=3,051 U.S. adults.
Note: Figure shows predicted mean perceived effectiveness and attention by message type and warning topic, as estimated using mixed effects linear regression. *p<0.05. Comparisons without brackets are not significantly different from one another (p>0.05).
Warnings about any of the 4 warning topics (addiction, liver damage, early death, and colon cancer) received higher perceived effectiveness ratings than the control labels (range of ADEs=0.58–0.97, all ps<0.001, Figure 2, Appendix Table 3). When comparing warning topics to one another, warnings about liver damage, early death, and colon cancer received higher perceived effectiveness ratings than the addiction warning (range of ADEs=0.27–0.39, all ps<0.001). Additionally, the cancer warning was perceived to be more effective than the early death warning (ADE=0.11; 95% CI=0.02, 0.21; p=0.02). The pattern of results was similar for attention. The 4 warning topics received higher attention ratings than the control labels (range of ADEs=0.42–0.62, all ps<0.001). Warnings about liver damage, early death, and colon cancer received higher attention ratings than the addiction warning (range of ADEs=0.17–0.20, all ps<0.001). There were no other differences in attention between the warning topics. The pattern of results was similar in sensitivity analyses examining participants who reported consuming alcohol in the past 30 days (Appendix Table 4).
In moderation analyses examining the interaction between message type and topic, the impact of message type (i.e., control, text warning, or icon warning) on the outcomes did not differ across the 4 warning topics (all ps for interaction>0.08). In analyses examining potential moderation of message type by demographic characteristics, the impact of message type on perceived effectiveness did not differ by any of the 9 characteristics studied, including by gender, age, sexual orientation, frequency of alcohol consumption, race, ethnicity, educational attainment, political party, or income (all ps for interaction >0.23).
When responding to the additional survey questions querying which causal language variant would most discourage them from warning to drink alcohol, a majority (60%) of participants selected the warning that used “increases the risk of,” followed by “contributes to” (21%), “can contribute to” (11%) and “may contribute to” (9%) (Figure 3). When asked to select the most discouraging marker words, about half (47%) of participants selected the warning that used “SURGEON GENERAL WARNING” (the attributed source in the current alcohol warning), followed by “WARNING” (27%), “ALCOHOL AND TOBACCO TAX AND TRADE BUREAU WARNING” (17%) and “GOVERNMENT WARNING” (9%) (Figure 3).
Figure 3.
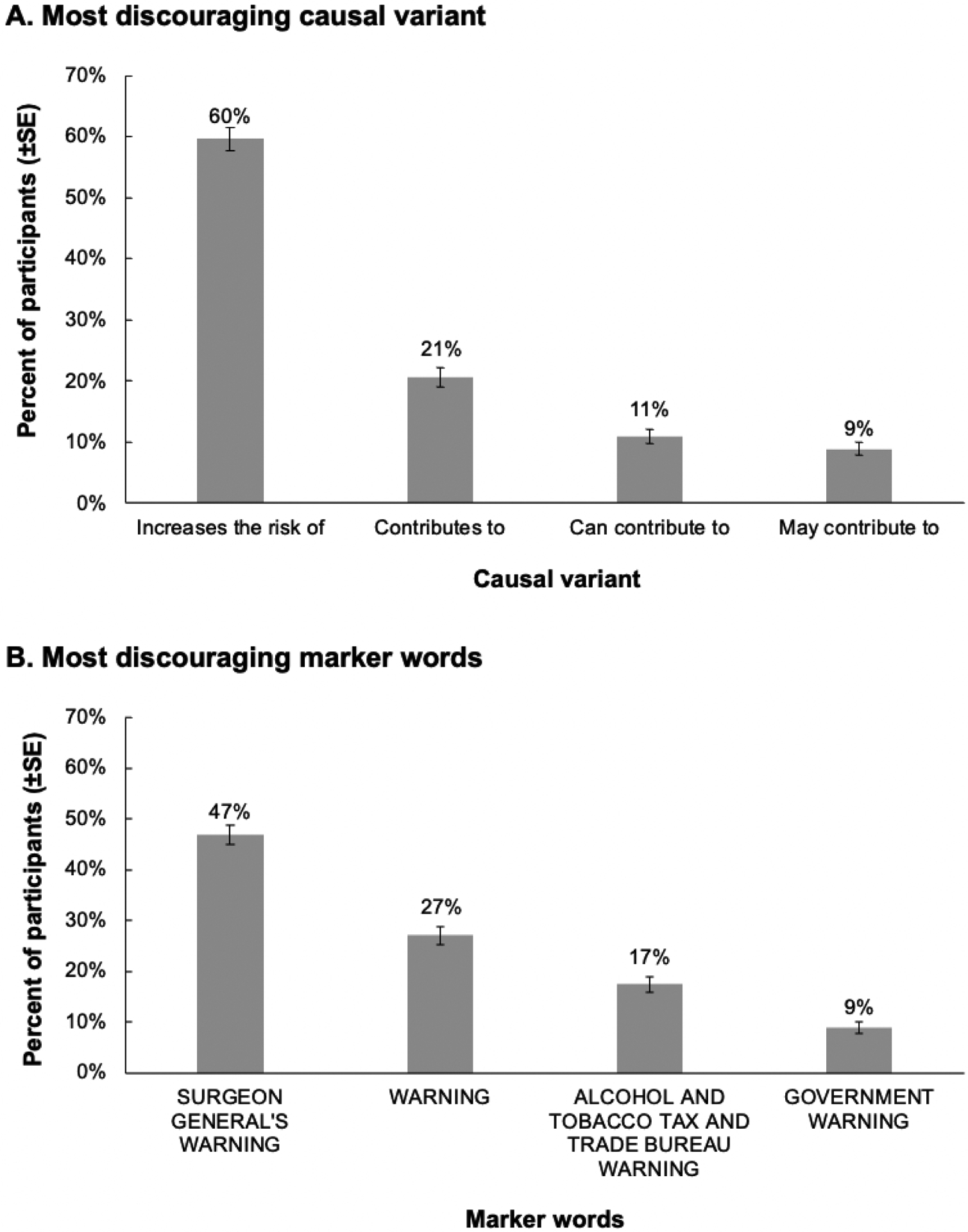
Percentage of participants selecting most discouraging causal variants (panel A, n=676 U.S. adults) and marker words (panel B, n=678 U.S. adults).
DISCUSSION
In this experiment with a large sample of U.S. adults, a minority of participants reported reading or looking closely at the current U.S. alcohol warnings. By contrast, participants perceived newly-developed, evidence-based alcohol warnings – particularly warnings with icons – as more effective and more attention-grabbing than control labels. Warning effectiveness did not differ by participant characteristics including age, gender, race/ethnicity, and alcohol consumption, providing early evidence that well-designed alcohol warnings may not exacerbate disparities. The findings in this study align with a quasi-experiment from the Yukon Territories that showed that implementation of large warnings with icons (which depicted standard drink amounts and low-risk drinking guidelines) increased attention to warnings28 and lowered alcohol sales.30 This study’s findings are also consistent with experimental evidence that pictorial alcohol warnings with graphic images can exert beneficial effects on behavioral intentions,32 alcohol selection,33,34 and speed of drinking.35
Prior studies have shown that alcohol warnings with graphic images are more effective than text-only warnings at increasing fear32 and reducing hypothetical selection of alcohol.33 Studies have not, however, examined alcohol warnings with icons. This experiment found icon warnings were rated as more effective and more attention-grabbing than text-only warnings, indicating that adding icons to warnings could enhance warnings’ effectiveness. These findings may be especially important in the U.S. context, where implementation of warnings with graphic images for tobacco has been delayed due to industry litigation,75 but icon warnings have been successfully implemented in New York76 and Philadelphia77 for high-sodium restaurant menu items. Future studies should compare alcohol warnings with graphic images to those with icons. More research is also needed to evaluate additional aspects of warning design such as label color,60,62,78,79 other warning topics, and additional icon designs.
All warning topics (addiction, liver damage, early death, colon cancer) were rated as more effective and attention-grabbing than the control messages. Although the addiction warning was perceived to be less effective and less attention-grabbing than the other topics (similar to tobacco control research on addiction messages22,53), there were few other differences between the warning topics. These results suggest that policymakers have several options for harms to describe in alcohol warnings.
Limitations
Strengths of this study include the experimental design and the large, diverse sample. Limitations include that outcomes were self-reported and may not reflect real-world responses; studies using objective measures (e.g., eye tracking) are warranted. Additionally, this message development experiment did not assess alcohol consumption, precautionary behaviors,80 or other aspects of the persuasion process (e.g., emotional reactions, risk perceptions), and did not assess awareness of health harms. The study also did not assess all relevant causal variants, marker words, or health harms. Finally, survey items were adapted from research on tobacco warnings and their psychometric properties have not been studied in the context of alcohol warnings.
CONCLUSIONS
Health warnings could discourage harmful alcohol consumption, but most adults in this study rarely or never read or looked closely at the alcohol warnings currently mandated in the U.S. New, evidence-based alcohol warnings could attract attention and reduce harmful alcohol consumption, especially if warnings include icons.
Supplementary Material
ACKNOWLEDGMENTS
The NIH (K01 HL158608 and T32 HL098048) supported AHG’s time writing the manuscript. The NIH (K01 HL147713) supported MGH’s time writing the manuscript. Center Grant P50 AA005595 from the National Institute on Alcohol Abuse and Alcoholism supported TKG’s time. The funders had no role in the management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. Views expressed are those of the authors and do not necessarily reflect official positions of the NIH.
Footnotes
The authors have no conflicts of interest to declare. The authors have no financial disclosures.
REFERENCES
- 1.US Burden of Disease Collaborators. The State of US Health, 1990–2010: Burden of Diseases, Injuries, and Risk Factors. JAMA. 2013;310(6):591–606. 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esser MB. Deaths and years of potential life lost from excessive alcohol use: United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2020;69(39). 10.15585/mmwr.mm6939a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Alcohol-Related Deaths. Centers for Disease Control and Prevention. https://www.cdc.gov/alcohol/features/excessive-alcohol-deaths.html. Published April 19, 2022. Accessed April 26, 2022. [Google Scholar]
- 4.LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: A statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36(1):83–93. 10.1200/JCO.2017.76.1155. [DOI] [PubMed] [Google Scholar]
- 5.Rumgay H, Shield K, Charvat H, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22(8):1071–1080. 10.1016/S1470-2045(21)00279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson DE, Jarman DW, Rehm J, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103(4):641–648. 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Global Status Report on Alcohol and Health 2018. WHO; 2019. https://apps.who.int/iris/rest/bitstreams/1151838/retrieve. Accessed November 10, 2021. [Google Scholar]
- 8.Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB. Key findings on alcohol consumption and a variety of health outcomes from the Nurses’ Health Study. Am J Public Health. 2016;106(9):1586–1591. 10.2105/AJPH.2016.303336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Agency for Research on Cancer. Personal Habits and Indoor Combustions. International Agency for Research on Cancer; 2012. https://www.ncbi.nlm.nih.gov/books/NBK304391/. Accessed July 7, 2022. [Google Scholar]
- 10.Cogliano VJ, Baan R, Straif K, et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103(24):1827–1839. 10.1093/jnci/djr483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rehm J, Patra J, Brennan A, et al. The role of alcohol use in the aetiology and progression of liver disease: A narrative review and a quantification. Drug Alcohol Rev. 2021;40(7):1377–1386. 10.1111/dar.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boersma P, Villarroel MA, Vahratian A. Heavy Drinking among US Adults, 2018. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/nchs/products/databriefs/db374.htm. Accessed May 12, 2022. [Google Scholar]
- 13.WHO. Health Warning Labels on Alcoholic Beverages: Opportunities for Informed and Healthier Choices. WHO; 2021. https://www.who.int/publications-detail-redirect/9789240044449. Accessed July 5, 2022. [Google Scholar]
- 14.Stockwell T, Solomon R, O’Brien P, Vallance K, Hobin E. Cancer warning labels on alcohol containers: A consumer’s right to know, a government’s responsibility to inform, and an industry’s power to thwart. J Stud Alcohol Drugs. 2020;81(2):284–292. 10.15288/jsad.2020.81.284. [DOI] [PubMed] [Google Scholar]
- 15.Greenfield TK, Graves KL, Kaskutas LA. Long‐term effects of alcohol warning labels: Findings from a comparison of the United States and Ontario, Canada. Psychol Market. 1999;16(3):261–282. . [DOI] [Google Scholar]
- 16.Jones D, Moodie C, Purves RI, Fitzgerald N, Crockett R. Health information, messaging and warnings on alcohol packaging: a focus group study with young adult drinkers in Scotland. Addict Res Theory. 2021;29(6):469–478. 10.1080/16066359.2021.1884229. [DOI] [Google Scholar]
- 17.Hammond D Health warning messages on tobacco products: A review. Tob Control. 2011;20(5):327–337. 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- 18.Al-Hamdani M, Smith SM. Alcohol warning label perceptions: Do warning sizes and plain packaging matter? J Stud Alcohol Drugs. 2017;78(1):79–87. 10.15288/jsad.2017.78.79. [DOI] [PubMed] [Google Scholar]
- 19.Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. 10.1016/j.socscimed.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brewer NT, Hall MG, Noar SM, et al. Effect of pictorial cigarette pack warnings on changes in smoking behavior: A randomized clinical trial. JAMA Intern Med. 2016;176(7):905–912. 10.1001/jamainternmed.2016.2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly G, Zatz L, Svirsky D, John L. The effect of graphic warnings on sugary-drink purchasing. Psychol Sci. 2018;29(8):1321–1333. 10.1177/0956797618766361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brewer NT, Jeong M, Hall MG, et al. Impact of e-cigarette health warnings on motivation to vape and smoke. Tob Control. 2019;28(e1):e64–e70. 10.1136/tobaccocontrol-2018-054878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monk RL, Westwood J, Heim D, Qureshi AW. The effect of pictorial content on attention levels and alcohol-related beliefs: An eye-tracking study. J Appl Soc Psychol. 2017;47(3):158–164. 10.1111/jasp.12432. [DOI] [Google Scholar]
- 24.Roberto CA, Ng SW, Ganderats-Fuentes M, et al. The influence of front-of-package nutrition labeling on consumer behavior and product reformulation. Annu Rev Nutr. 2021;41:529–550. 10.1146/annurev-nutr-111120-094932. [DOI] [PubMed] [Google Scholar]
- 25.Noar S, Hall M, Francis D, Ribisl K, Pepper J, Brewer N. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tob Control. 2015;25:341–354. 10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alcoholic Beverage Labeling Act of 1988. https://www.govinfo.gov/content/pkg/USCODE-2014-title27/pdf/USCODE-2014-title27-chap8-subchapII.pdf. Published 1988. Accessed July 7, 2022.
- 27.Wilkinson C, Room R. Warnings on alcohol containers and advertisements: international experience and evidence on effects. Drug Alcohol Rev. 2009;28(4):426–435. 10.1111/j.1465-3362.2009.00055.x. [DOI] [PubMed] [Google Scholar]
- 28.Hobin E, Schoueri-Mychasiw N, Weerasinghe A, et al. Effects of strengthening alcohol labels on attention, message processing, and perceived effectiveness: A quasi-experimental study in Yukon, Canada. Int J Drug Policy. 2020;77:102666. 10.1016/j.drugpo.2020.102666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schoueri-Mychasiw N, Weerasinghe A, Vallance K, et al. Examining the impact of alcohol labels on awareness and knowledge of national drinking guidelines: A real-world study in Yukon, Canada. J Stud Alcohol Drugs. 2020;81(2):262–272. 10.15288/jsad.2020.81.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao J, Stockwell T, Vallance K, Hobin E. The effects of alcohol warning labels on population alcohol consumption: An interrupted time series analysis of alcohol sales in Yukon, Canada. J Stud Alcohol Drugs. 2020;81(2):225–237. 10.15288/jsad.2020.81.225. [DOI] [PubMed] [Google Scholar]
- 31.Clarke N, Blackwell AK, De‐loyde K, et al. Health warning labels and alcohol selection: a randomised controlled experiment in a naturalistic shopping laboratory. Addiction. 2021;116(12):3333–3345. 10.1111/add.15519. [DOI] [PubMed] [Google Scholar]
- 32.Wigg S, Stafford LD. Health Warnings on Alcoholic Beverages: Perceptions of the Health Risks and Intentions towards Alcohol Consumption. PLoS One. 2016;11(4):e0153027. 10.1371/journal.pone.0153027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clarke N, Pechey E, Mantzari E, et al. Impact of health warning labels communicating the risk of cancer on alcohol selection: an online experimental study. Addiction. 2021;116(1):41–52. 10.1111/add.15072. [DOI] [PubMed] [Google Scholar]
- 34.Clarke N, Pechey E, Kosīte D, et al. Impact of health warning labels on selection and consumption of food and alcohol products: systematic review with meta-analysis. Health Psychol Rev. 2021;15(3):430–453. 10.1080/17437199.2020.1780147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stafford LD, Salmon J. Alcohol health warnings can influence the speed of consumption. Z Gesundh Wiss. 2017;25(2):147–154. 10.1007/s10389-016-0770-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hall MG, Grummon AH, Higgins I, et al. The impact of pictorial health warnings on purchases of sugary drinks for children: A randomized controlled trial. PLOS Med. 2022;19(1):e1003885. 10.1371/journal.pmed.1003885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pechey E, Clarke N, Mantzari E, et al. Image-and-text health warning labels on alcohol and food: Potential effectiveness and acceptability. BMC Public Health. 2020;20(1):1–14. 10.1186/s12889-020-8403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pettigrew S, Jongenelis M, Chikritzhs T, et al. Developing cancer warning statements for alcoholic beverages. BMC Public Health. 2014;14:786. 10.1186/1471-2458-14-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jongenelis MI, Pratt IS, Slevin T, Chikritzhs T, Liang W, Pettigrew S. The effect of chronic disease warning statements on alcohol-related health beliefs and consumption intentions among at-risk drinkers. Health Educ Res. 2018;33(5):351–360. 10.1093/her/cyy025. [DOI] [PubMed] [Google Scholar]
- 40.Hassan LM, Parry S, Shiu E. Exploring responses to differing message content of pictorial alcohol warning labels. Int J Consum Stud. Published online 2022:1–20. 10.1111/ijcs.12779. [DOI] [Google Scholar]
- 41.Kokole D, Anderson P, Jané-Llopis E. Nature and potential impact of alcohol health warning labels: A scoping review. Nutrients. 2021;13(9):3065. 10.3390/nu13093065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jeong M, Zhang D, Morgan J, et al. Similarities and differences in tobacco control research findings from convenience and probability samples. Ann Behav Med. 2018;53(5):476–485. 10.1093/abm/kay059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rehm J The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34(2):135–143. [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Alcohol Use and Your Health. https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm. Published December 29, 2021. Accessed March 28, 2022.
- 45.Greenfield TK, Ye Y, Bond J, et al. Risks of alcohol use disorders related to drinking patterns in the US general population. J Stud Alcohol Drugs. 2014;75(2):319–327. 10.15288/jsad.2014.75.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roerecke M, Vafaei A, Hasan OS, et al. Alcohol consumption and risk of liver cirrhosis: A systematic review and meta-analysis. Am J Gastroenterol. 2019;114(10):1574–1586. 10.14309/ajg.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Griswold MG, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015–1035. 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wood AM, Kaptoge S, Butterworth AS, et al. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391(10129):1513–1523. 10.1016/S0140-6736(18)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rehm J, Greenfield TK, Kerr W. Patterns of drinking and mortality from different diseases: An overview. Contemp Drug Probl. 2006;33(2):205–235. 10.1177/009145090603300203. [DOI] [Google Scholar]
- 50.McNabb S, Harrison TA, Albanes D, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2020;146(3):861–873. 10.1002/ijc.32377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choi YJ, Myung SK, Lee JH. Light alcohol drinking and risk of cancer: A meta-analysis of cohort studies. Cancer Res Treat. 2018;50(2):474. 10.4143/crt.2017.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br J Cancer. 2015;112(3):580–593. 10.1038/bjc.2014.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rohde JA, Noar SM, Mendel JR, et al. E-cigarette health harm awareness and discouragement: Implications for health communication. Nicotine Tob Res. 2019;(ntz194). 10.1093/ntr/ntz194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carl A, Taillie L, Grummon AH, et al. Awareness of and reactions to the health harms of sugary drinks: An online study of U.S. parents. Appetite. 2021;164(105234). 10.1016/j.appet.2021.105234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hall MG, Grummon AH, Lazard AJ, Maynard OM, Taillie LS. Reactions to graphic and text health warnings for cigarettes, sugar-sweetened beverages, and alcohol: An online randomized experiment of US adults. Prev Med. 2020;137:106120. 10.1016/j.ypmed.2020.106120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taillie LS, Prestemon CE, Hall MG, Grummon AH, Vesely A, Jaacks LM. Developing health and environmental warning messages about red meat: An online experiment. PLoS One. 2022;17(6):e0268121. 10.1371/journal.pone.0268121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pettigrew S, Jongenelis MI, Glance D, et al. The effect of cancer warning statements on alcohol consumption intentions. Health Educ Res. 2016;31(1):60–69. 10.1093/her/cyv067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brewer NT, Jeong M, Mendel JR, et al. Cigarette pack messages about toxic chemicals: A randomised clinical trial. Tob Control. 2019;28(1):74–80. 10.1136/tobaccocontrol-2017-054112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hall MG, Lazard AJ, Grummon AH, et al. Designing warnings for sugary drinks: A randomized experiment with Latino and non-Latino parents. Prev Med. 2021;148:106562. 10.1016/j.ypmed.2021.106562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cabrera M, Machín L, Arrúa A, et al. Nutrition warnings as front-of-pack labels: Influence of design features on healthfulness perception and attentional capture. Public Health Nutr. 2017;20(18):3360–3371. 10.1017/S136898001700249X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.City and County of San Francisco. Sugar-Sweetened Beverage Warning Ordinance. Vol Article 42; 2020. https://codelibrary.amlegal.com/codes/san_francisco/latest/sf_health/0-0-0-58530#JD_4203. Accessed July 7, 2022.
- 62.Grummon AH, Hall MG, Taillie LS, Brewer NT. How should sugar-sweetened beverage health warnings be designed? A randomized experiment. Prev Med. 2019;121:158–166. 10.1016/j.ypmed.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hall MG, Grummon AH, Maynard OM, Kameny MR, Jenson D, Popkin BM. Causal language in health warning labels and US adults’ perception: A randomized experiment. Am J Public Health. 2019;109(10):1429–1433. 10.2105/AJPH.2019.305222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Food and Drug Administration. FDA requires new health warnings for cigarette packages and advertisements. https://www.fda.gov/news-events/press-announcements/fda-requires-new-health-warnings-cigarette-packages-and-advertisements. Published March 24, 2020. Accessed July 1, 2022.
- 65.Global Food Research Program. Countries with mandatory or voluntary interpretative labels on packaged foods and drinks. https://docs.google.com/viewer?url=https%3A%2F%2Fwww.globalfoodresearchprogram.org%2Fwp-content%2Fuploads%2F2021%2F09%2FFOP_Regs_maps_2021_September.pdf. Published September 2021. Accessed June 12, 2022.
- 66.Monning B Sugar-Sweetened Beverages: Safety Warnings. http://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200SB347. Published 2019. Accessed February 27, 2019.
- 67.Riley MW, Cochran DJ, Ballard JL. An investigation of preferred shapes for warning labels. Hum Factors. 1982;24(6):737–742. 10.1177/001872088202400610. [DOI] [Google Scholar]
- 68.Nonnemaker J, Farrelly M, Kamyab K, Busey A, Mann N. Experimental Study of Graphic Cigarette Warning Labels. RTI International; 2010. https://www.fda.gov/media/136126/download. Accessed June 12, 2022. [Google Scholar]
- 69.Baig SA, Noar SM, Gottfredson NC, Boynton MH, Ribisl KM, Brewer NT. UNC Perceived Message Effectiveness: Validation of a brief scale. Ann Behav Med. 2019;53(8):732–742. 10.1093/abm/kay080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brewer N, Parada H Jr., Hall M, Boynton M, Noar S, Ribisl K. Understanding why pictorial cigarette pack warnings increase quit attempts. Ann Behav Med. 2019;53(3):232–243. 10.1093/abm/kay032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Noar SM, Barker J, Bell T, Yzer M. Does perceived message effectiveness predict the actual effectiveness of tobacco education messages? A systematic review and meta-analysis. Health Commun. 2018;35(2):148–157. 10.1080/10410236.2018.1547675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Noar SM, Rohde JA, Prentice-Dunn H, Kresovich A, Hall MG, Brewer NT. Evaluating the actual and perceived effectiveness of e-cigarette prevention advertisements among adolescents. Addict Behav. 2020;109:106473. 10.1016/j.addbeh.2020.106473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bigsby E, Cappella JN, Seitz HH. Efficiently and effectively evaluating public service announcements: Additional evidence for the utility of perceived effectiveness. Commun Monogr. 2013;80(1):1–23. 10.1080/03637751.2012.739706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Himmelfarb S What do you do when the control group doesn’t fit into the factorial design? Psychol Bull. 1975;82(3):363. 10.1037/0033-2909.82.3.363. [DOI] [Google Scholar]
- 75.Curfman G Graphic cigarette warning labels, the first amendment, and public right to accurate public health information: Graphic cigarette warning labels back under legal scrutiny. JAMA Health Forum. 2021;2(9):e212886. 10.1001/jamahealthforum.2021.2886. [DOI] [PubMed] [Google Scholar]
- 76.New York City. Sodium Warning. Vol §81.49. https://docs.google.com/viewer?url=https%3A%2F%2Fwww1.nyc.gov%2Fassets%2Fdoh%2Fdownloads%2Fpdf%2Fabout%2Fhealthcode%2Fhealth-code-article81.pdf. Published 2015. Accessed April 15, 2021.
- 77.City of Philadelphia. Sodium Safety Warning Labeling for Chain Establishments. Vol §6–310. https://codelibrary.amlegal.com/codes/philadelphia/latest/philadelphia_pa/0-0-0-190525#JD_6-310. Published 2019. Accessed July 5, 2022.
- 78.Pham C, Rundle-Thiele S, Parkinson J, Li S. Alcohol warning label awareness and attention: A multi-method study. Alcohol Alcohol. 2018;53(1):39–45. 10.1093/alcalc/agx087. [DOI] [PubMed] [Google Scholar]
- 79.Acton R, Vanderlee L, Roberto CA, Hammond D. Consumer perceptions of specific design characteristics for front-of-package nutrition labels. Health Educ Res. 2018;33(2):167–174. 10.1093/her/cyy006. [DOI] [PubMed] [Google Scholar]
- 80.Greenfield TK. Warning labels: Evidence on harm reduction from long-term American surveys. In: Plant M, Single E, Stockwell T, eds. Alcohol: Minimizing the Harm. Vol 1997. Free Association Books; 1997:105–125. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


