Video
Complete internal migration of a cholecystoduodenal pigtail stent leading to recurrent cholecystitis, which was then rescued with new EUS-guided gallbladder drainage.
Introduction
EUS-guided gallbladder drainage (EUS-GBD) has emerged as minimally invasive alternative to manage cholecystitis in surgically unfit patients. When compared to percutaneous cholecystectomy in high-risk surgical patients, EUS-GBD has comparable technical and clinical success with reduced adverse events, reintervention rates, and recurrent cholecystitis.1 The evolution from plastic to lumen-apposing metal stents (LAMSs) has simplified and improved the efficacy of this technique.2,3 In a recent prospective multicenter study, 30 poor surgical candidates demonstrated a reliable technical success rate of 98% with a low recurrence (16.7%) and low risk of adverse events.4 After resolution of cholecystitis, some authors at 4 to 8 weeks replaced the LAMS for 1 or more pigtail stents to maintain the cholecystoenteric fistula.5
In this case, we present a rare adverse event of complete internal migration of such a cholecystoduodenal pigtail stent leading to recurrent cholecystitis, which was then rescued with a new EUS-GBD (Video 1, available online at www.videogie.org).
Case
A 51-year-old woman with metastatic pancreatic cancer and an indwelling biliary fully covered metal stent, coaxial common hepatic duct pigtail stent, transpapillary gallbladder stent, and transduodenal pigtail gallbladder stent presented with abdominal pain, fever, and a positive Murphy sign suspicious for recurrent cholecystitis. Given an indwelling transpapillary gallbladder stent, the presumed etiology for the cholecystitis was malignant progression to involve the cystic duct take-off, rather than the fully covered metal stent.
Twenty-one months prior, she had her first bout of cholecystitis managed with EUS-GBD (10- × 10-mm LAMS) and coaxial 7F × 3-cm complete pigtail stent. Nine months prior, while traveling out of state, she developed biliary obstruction. A new biliary fully covered self-expandable metal stent was inserted and the EUS-GB LAMS was replaced with a 7F × 3-cm, 3/4 pigtail stent to maintain the cholecystoduodenal fistula. They additionally placed a 7F × 15-cm transpapillary pigtail stent likely to further reduce the risk of recurrent cholecystitis.
At this presentation, a CT scan of the abdomen revealed the previously placed 3/4 pigtail stent residing completely within the gallbladder. Although there were no significant changes on CT scan in gallbladder distention, thickening, or pericholecystic fluid to suggest cholecystitis, there was no other cause of her fever and abdominal pain (with stable liver-associated enzymes and pneumobilia), making her clinical presentation with the internally migrated pigtail stent most suspicious for cholecystitis.
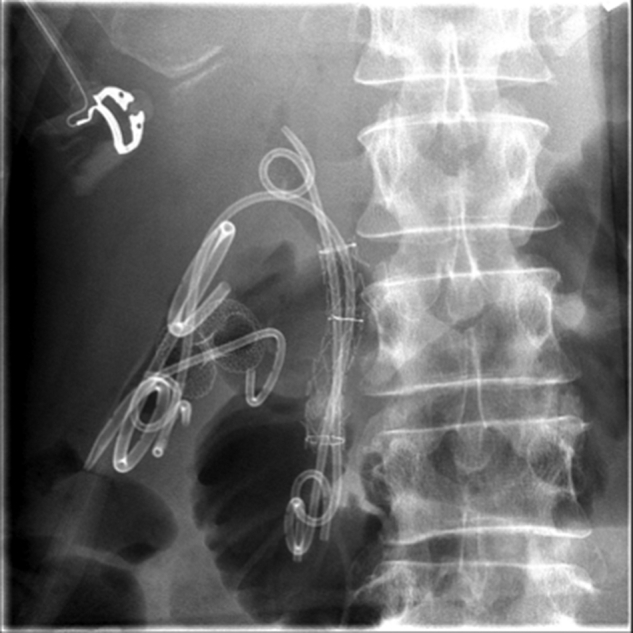
EUS showed that the cholecystoduodenal fistula was closed off and the pigtail stent was fully migrated into the gallbladder. Fluoroscopy confirmed there was 1 metal biliary stent, 1 pigtail stent in the common hepatic duct, 1 transpapillary 7F × 15-cm GB stent, and 1 fully internally migrated 3/4 pigtail 7F × 3-cm stent (Figs. 1 and 2). Since the gallbladder lumen was not markedly distended, we used a 10- × 10-mm cautery-enhanced LAMS, using the direct technique, for the EUS-GBD (Figs. 3 and 4). Over a 0.035-inch coaxial guidewire, a 7F × 3-cm complete pigtail stent was placed (Fig. 5). Following the procedure, her cholecystitis resolved, and she was discharged home the next day on antibiotics.
Figure 1.
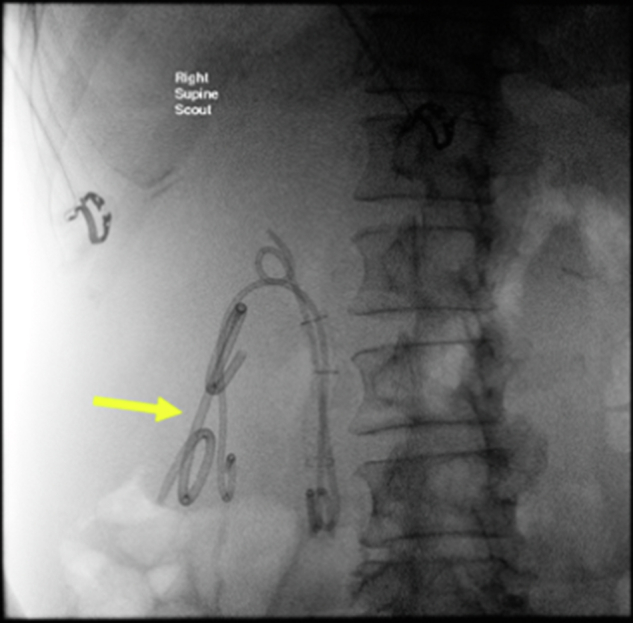
Fluoroscopic image demonstrating the internally migrated pigtail stent (arrow).
Figure 2.
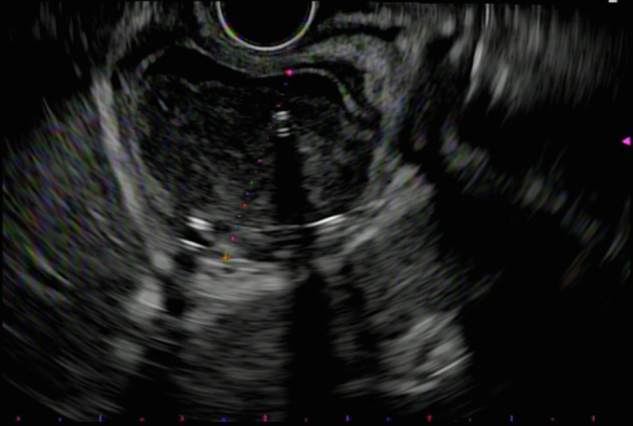
EUS demonstrating cholecystitis with the internally migrated pigtail stent.
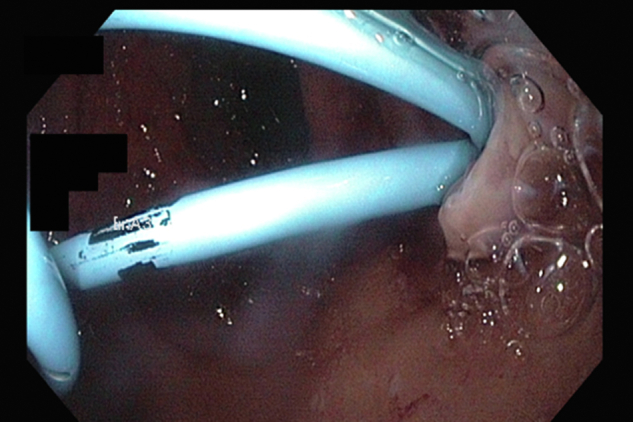
Figure 3.
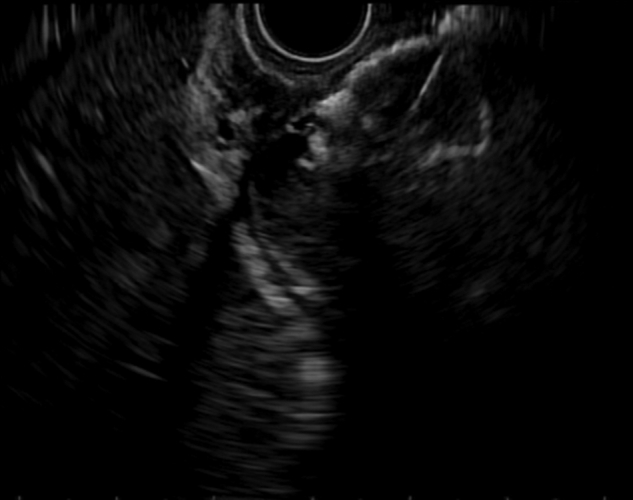
The duodenal flange being deployed under EUS guidance.
Figure 4.
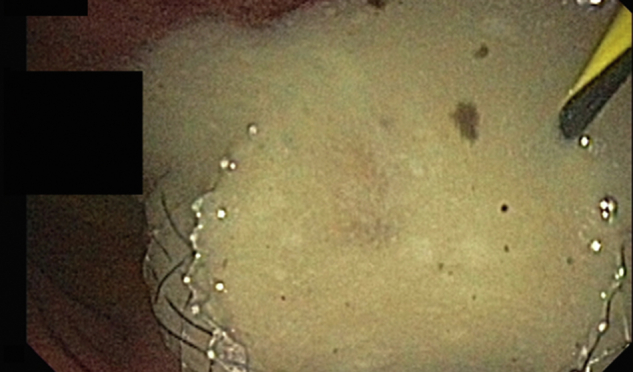
Endoscopic view following lumen-apposing metal stent placement with a large amount of purulence.
Figure 5.
Fluoroscopic view following EUS-guided gallbladder drainage with 10- × 10-mm lumen-apposing metal stent and coaxial 7F × 3-cm complete pigtail stent placed over a 0.035-inch guidewire.
She returned 4 weeks later for removal of the internally migrated pigtail stent with cholecystoscopy using a gastroscope (Fig. 6). A cholangiogram demonstrated patency of the cystic duct and common bile duct stent. Confirmation of the correct stent to pull was made by moving the stent with rat-tooth forceps under fluoroscopy. The LAMS was then replaced with two 7F × 3-cm complete pigtail stents to maintain a cholecystoduodenal fistula (Fig. 7). She lived an additional 9 months without recurrent cholecystitis before she died of metastatic cancer.
Figure 6.

The internally migrated pigtail stent following removal with rat-tooth forceps.
Figure 7.
Final endoscopic view after the lumen-apposing metal stent was replaced with 2 complete pigtail stents in the gallbladder to maintain a cholecystoduodenal fistula.
Conclusion
Complete internal migration of cholecystoduodenal pigtail stents leading to recurrent cholecystitis is rare but can be successfully managed with EUS-GBD. Cholecystitis should be suspected in the right clinical setting (prior cholecystitis, pain, fever, and indwelling stents), even if cross-sectional imaging does not support it. EUS can help confirm and treat this. Furthermore, cholecystoscopy allows removal of internally migrated stents and can be done even through a 10-mm LAMS. Lastly, if replacing LAMSs with pigtail stents, consider placing 2, as this can allow drainage in between stents if they occlude, and strongly consider using full and not 3/4 pigtail stents as they are less likely to migrate.
Disclosure
Dr Irani is a consultant for Boston Scientific and Gore. All other authors disclosed no financial relationships.
Supplementary data
Complete internal migration of a cholecystoduodenal pigtail stent leading to recurrent cholecystitis, which was then rescued with new EUS-guided gallbladder drainage.
References
- 1.Teoh A.Y.B., Kitano M., Itoi T., et al. Endosonography-guided gallbladder drainage versus percutaneous cholecystostomy in very high-risk surgical patients with acute cholecystitis: an international randomised multicentre controlled superiority trial (DRAC 1) Gut. 2020;69:1085–1091. doi: 10.1136/gutjnl-2019-319996. [DOI] [PubMed] [Google Scholar]
- 2.Dollhopf M., Larghi A., Will U., et al. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86:636–643. doi: 10.1016/j.gie.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 3.Walter D., Teoh A.Y., Itoi T., et al. EUS-guided gall bladder drainage with a lumen-apposing metal stent: a prospective long-term evaluation. Gut. 2016;65:6–8. doi: 10.1136/gutjnl-2015-309925. [DOI] [PubMed] [Google Scholar]
- 4.Irani SS, Sharma NR, Storm AC, et al. EUS-guided transluminal gallbladder drainage in patients with acute cholecystitis: a prospective multicenter trial. Ann Surg. Epub 2022 Dec 20. [DOI] [PMC free article] [PubMed]
- 5.Chan S.M., Teoh A.Y.B., Yip H.C., et al. Feasibility of per-oral cholecystoscopy and advanced gallbladder interventions after EUS-guided gallbladder stenting (with video) Gastrointest Endosc. 2017;85:1225–1232. doi: 10.1016/j.gie.2016.10.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete internal migration of a cholecystoduodenal pigtail stent leading to recurrent cholecystitis, which was then rescued with new EUS-guided gallbladder drainage.
Complete internal migration of a cholecystoduodenal pigtail stent leading to recurrent cholecystitis, which was then rescued with new EUS-guided gallbladder drainage.


