Abstract
Introduction
As most public health decisions are made at the local level, public health interventions implemented at the local level may vary by their own unique circumstances, such as demographic composition or the availability of resources. Our objective is to estimate and characterize county-level flu vaccine uptakes among Medicare-covered adults aged ≥65 years.
Methods
The flu vaccine uptake was estimated from Medicare Fee-for-Service claims for those who continuously enrolled during the 2018–2019 flu season. County-level characteristics were obtained from Centers for Disease Control and Prevention (CDC)’s Minority Health Social Vulnerability Index and Behavioral Risk Factor Surveillance System data as well as Health Resources and Services Administration’s Area Health Resources File. A generalized linear regression was used to assess the relationship between selected characteristics and uptake.
Results
A total of 30,265,047 beneficiaries from 3,125 counties were identified, of which 53% received a flu vaccination during the 2018–2019 flu season. For 3,006 counties with more than 500 Medicare beneficiaries, the mean county-level uptake was estimated to be 47.7%. The mean uptakes in counties designated as a health professional shortage area (HPSA) (42.6% and 48.4%, respectively), were lower than the uptakes for the non-HPSA counties (53.8%). Metro counties (53.2%) showed higher uptakes than non-metro counties (44.2%). Regression analysis results showed that the percent of working adults aged 18–64 years and female were positively associated, while the percent of Black and Hispanic adults were negatively associated. Proportions of persons with limited proficiency of English, college education or above, single parent families, multi-unit housing, and living in group quarters were positively associated and significant.
Conclusions
The results confirmed that county-level flu vaccine uptakes are low, reflect persistent racial disparities in vaccine uptake, and that Medicare populations in medically underserved communities with lower socioeconomic status need more attention in improving flu vaccine uptake.
Keywords: Seasonal influenza vaccine, Medicare, Vaccine uptake, Small area assessment, Social vulnerability index
1. Introduction
Influenza (flu) is a highly contagious viral infection of the respiratory passages that can cause mild to severe illness, hospitalization, or death. The elderly, young children, and people with certain health conditions, pose the highest risk of serious flu complications [1]. The Centers for Disease Control and Prevention (CDC) estimated that flu has resulted in 9 million to 41 million illnesses, 140,000 to 710,000 hospitalizations, and 12,000 to 52,000 deaths annually from 2010 through 2020 [2]. To prevent flu, the US Advisory Committee on Immunization Practices (ACIP) recommends all persons in the US 6 months of age and older receive an annual flu vaccination [1]. Flu vaccination coverage for those aged ≥ 65 years was estimated to be at 70% for the 2019–2020 season [3], reaching the Healthy People 2030 initiative goal (70%) of flu vaccination coverage for persons aged 6 months of age and over [4]. Consequently, according to CDC, flu vaccinations prevented 7.5 million illnesses, 105,000 hospitalizations and 6,300 deaths associated with flu, during the 2019–2020 flu season [5].
However, despite the benefits of flu vaccination, the burden among those at high-risk of flu complications and the disproportionate burden of flu by race/ethnicity and census-tract level poverty have been highlighted. To alleviate such concerns, identifying barriers and trends in flu vaccination can assist in improving vaccination rates by targeting those at highest risk and socially vulnerable groups in the community and can ultimately reduce illnesses, medical visits, hospitalizations, and deaths associated with flu. There have been several previous studies that have made significant efforts to identify these barriers and trends in the uptake of flu vaccine. In a 2012 study, authors used the 2009 Behavioral Risk Factor Surveillance System (BRFSS) data to examine the uptake of flu vaccine among two age groups: 18–64 years and ≥ 65 years. They found that having health care coverage was the strongest predictor of vaccination in both age groups, after accounting for other sociodemographic characteristics, health behaviors, and health status. Those reporting older age, White race, higher education, non-smoking status, being physically active, or having poor physical health or a personal history of various chronic conditions were also more likely to report having received the flu vaccine [6]. A 2017 study aimed to examine the relationship between pharmacist density and flu vaccination after controlling for both individual- and county-level characteristics. They found that the number of pharmacists per 1000 population was associated with higher odds of flu vaccination and was significant for non-Hispanic White and Hispanic persons, varying across county types (rural v. metro v. urban non-metro) and employment status. The largest effects were found in urban counties and among the self-employed, homemakers, and the retired [7]. To better understand utilization of Medicare vaccination benefits, researchers examined a retrospective cohort of more than 26 million Medicare fee-for-service beneficiaries aged ≥ 65 years from 2014 to 2017. Multivariate logistic regression was used to obtain marginal effects (ME) describing the association between patient-level characteristics and the likelihood of vaccination for seasonal flu, 23-valent pneumococcal polysaccharide, 13-valent pneumococcal conjugate, and herpes zoster vaccines. Results showed that Black beneficiaries were less likely to receive any of the three vaccines compared with White beneficiaries. Beneficiaries utilizing preventive services, particularly cardiovascular disease screening, other vaccinations, and the Medicare Annual Wellness Visit were predictors of vaccination for all three vaccines [8]. Another study conducted in 2020 considered the demographic, clinical, and geographic correlates of flu vaccination among Medicare Fee-for-Service (FFS) beneficiaries in 2015–2016 and mapped the data on a geographic information system (GIS) at the zip code level. They calculated the percentage of Medicare FFS beneficiaries vaccinated overall as well as by sociodemographic and clinical characteristics [9]. Lastly, in a 2021 study, researchers evaluated local spatial patterns by examining how the CDC’s Social Vulnerability Index (SVI) is associated with seasonal flu vaccination coverage among Medicare recipients at the county-level. They found that Medicare recipients in socioeconomically vulnerable counties had low flu vaccination rates, particularly in select regions of the country and suggested locally tailored interventions to address vaccine barriers associated with county socioeconomic vulnerability [10]. To add to this body of literature, we examined county-level flu vaccination rates across the United States for Medicare beneficiaries aged ≥ 65 years who were continuously enrolled during the 2018–2019 flu seasons and county-level characteristics associated with the uptakes such as demographic, socioeconomic, and geographic characteristics.
As most public health decisions are made at the local level, public health interventions implemented at the local level may vary by their own unique circumstances, such as demographic composition or the availability of resources. As a result, the estimation and characterization of flu vaccine uptake in small geographic areas is important for local public health stakeholders to inform (1) current levels of flu vaccinations, and (2) specific factors highly associated with flu vaccine uptake. Such information will be useful for local public health officials to improve suboptimal flu vaccine uptake of aged ≥ 65 years, Medicare-covered adults. Our primary objective is to estimate and characterize county-level flu vaccine uptakes among Medicare-covered adults while investigating select interventions to address county-level vaccine barriers for the United States.
2. Methods
2.1. Data and study population
We considered Medicare beneficiaries aged ≥ 65 years who were continuously enrolled during the 2018–2019 flu season from August 2018 through April 2019 under fee-for-service (FFS). For data extraction, we used the 2018 Master Beneficiary Summary Files (MBSF) to identify the beneficiaries who had enrolled before August 1, 2018. We followed these beneficiaries through April 2019 using an associated beneficiary ID to collect enrollment information. For enrollment, we used the monthly plan enrollment data to determine the plan for each month. We retained beneficiaries who enrolled in FFS for 9 consecutive months or until death. We excluded beneficiaries with missing demographic data (sex or race), or those living in US Protectorates (Puerto Rico, US Virgin Islands, US Minor Outlying Islands, Guam, American Samoa and Northern Mariana Islands).
For flu vaccinations, we extracted flu vaccination claims and encounter data of the beneficiaries included in the study population. In order to capture as many flu vaccination records as possible, we looked up professional services files including carrier and outpatient files, and other services or revenue files such as Inpatient, Home Health Agency (HHA), and Skilled Nursing Facilities (SNF). To check any missing flu vaccination records of dual eligible beneficiaries, we included all service files of Medicaid. For flu vaccination, the Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) from the Centers for Medicare and Medicaid Services (CMS) was used [11]. The National Drug Code (NDC) for flu vaccines, sale NDC and use NDC, were included as well [12].
To identify and evaluate the association between the county-level characteristics and the flu vaccine uptake, county-level variables from various sources were used. Firstly, to consider the differences in county-level circumstances, the demographic composition, socioeconomic status and healthcare professionals and facilities data for each county from CDC’s Minority Health Social Vulnerability Index (SVI) were included [13]. Secondly, to explore the association with other county-level variables, data not included in SVI from 2018 to 19 Area Health Resources File (AHRF) were reviewed and selected. ARHF includes county-level data on population characteristics, healthcare professionals and hospitals at the county level [14]. In addition, we used the preventive and health behavior data from BRFSS 2017 data via CDC PLACES [15]. Variable selection criteria were based on previous research and the prospect of affecting vaccination decision-making [8], [10], [16]. To represent demographics, we examined age, race, and gender of the county, and for socioeconomic characteristics we focused on language, poverty, education, disabilities, parental status, and housing elements. For transportation and communications, modes of transportations to work and internet access were included. Access to pharmacies and insurance availability represent access to healthcare and routine checkups, poor health, and medication represent health behaviors. Health professional shortage areas (HPSA) were examined in terms of an entire county being classified as a HPSA or not, or only part of a county classified as a HPSA. These variables are reported, along with sources, in Supplemental Table 1.
Table 1.
County-level seasonal influenza vaccine uptakes among fee-for-service medicare beneficiaries, 2018–19 flu season (N = 3,006).
| Variable | Mean | Median | Standard Deviation | Max | 3rd quartile | 2nd quartile | Min |
|---|---|---|---|---|---|---|---|
| County-level Uptakes (%) | |||||||
| Overall | 47.7 | 49.4 | 10.6 | 72.3 | 55.4 | 41.3 | 3.5 |
| Health Professional Shortage Areas (HPSA) | |||||||
| Whole (n = 692) | 42.6 | 43.4 | 10.1 | 69.0 | 50.0 | 36.5 | 3.5 |
| Part (n = 1,955) | 48.4 | 50.2 | 10.1 | 72.3 | 55.7 | 42.7 | 8.9 |
| Non-HPSA (n = 359) | 53.8 | 55.9 | 9.6 | 71.2 | 59.7 | 50.5 | 16.1 |
| NCHS Urban Rural Classification* | |||||||
| Metro (n = 1,155) | 53.2 | 54.2 | 7.4 | 72.3 | 58.5 | 48.9 | 21.7 |
| Large Central (n = 68) | 52.9 | 53.9 | 5.7 | 64.3 | 56.5 | 49.3 | 32.6 |
| Large Fringe (n = 367) | 54.6 | 55.5 | 6.5 | 68.5 | 59.0 | 51.1 | 30.3 |
| Medium (n = 369) | 52.7 | 54.1 | 7.9 | 70.3 | 58.5 | 47.7 | 22.1 |
| Small (n = 351) | 52.3 | 52.5 | 7.7 | 72.3 | 58.1 | 47.7 | 21.7 |
| Non-metro (n = 1,851) | 44.2 | 45.2 | 10.8 | 71.2 | 52.6 | 37.5 | 3.5 |
| Micropolitan (n = 629) | 49.1 | 50.6 | 8.9 | 68.8 | 55.5 | 43.5 | 35.1 |
| Noncore (n = 1,222) | 41.7 | 42.7 | 10.9 | 71.2 | 49.7 | 35.1 | 3.5 |
| Region | |||||||
| Northeast (n = 217) | 55.1 | 56.1 | 6.8 | 68.8 | 59.6 | 52.0 | 29.0 |
| Midwest (n = 1,003) | 47.7 | 49.8 | 11.6 | 72.3 | 56.5 | 40.1 | 8.9 |
| South (n = 1,389) | 47.9 | 49.3 | 9.5 | 70.3 | 54.8 | 42.3 | 13.5 |
| West (n = 397) | 42.8 | 44.4 | 10.5 | 65.9 | 50.5 | 36.9 | 3.5 |
*Based on the NCHS Urban-Rural Classification Scheme, metro counties include large central metro, large fringe metro, medium and small metro, and non-metro includes micropolitan and non-core counties.
NCHS: National Center for Health Statistics.
2.2. Statistical analysis
Counties with less than 500 Medicare beneficiaries were excluded from the analysis. The estimated county-level flu vaccine uptakes and county-level characteristics variables were merged using the Federal Information Processing Standard (FIPS) code. County-level uptake was calculated by applying the Kaplan-Meier (time-to-event) method using PROC LIFETEST in SAS to account for those who dropped out of Medicare due to death or plan changes. A descriptive analysis of county-level uptakes was conducted by county characteristics, including examining correlation coefficients between variables. If variables were too highly correlated, such as the proportions of minority races and population with limited English skills, one of the variables was removed (in this case minority races). A generalized linear model of the county-level flu vaccine uptake for the 2018–2019 flu season was fitted using PROC GENMOD with the fixed effects of states, and the test statistics were calculated using cluster robust standard errors. Only the summary statistics, regression results, and tables were downloaded for the manuscript preparation. As the unit of observation was county, no personal identifiable information was downloaded. CMS Medicare data were accessed via Virtual Research Data Center (VRDC, virtual desktop environment). County-level characteristics data were uploaded to VRDC for the analysis. Data management and analysis were conducted in a VRDC environment using SAS Enterprise Guide (ver.7.15 HF8).
3. Results
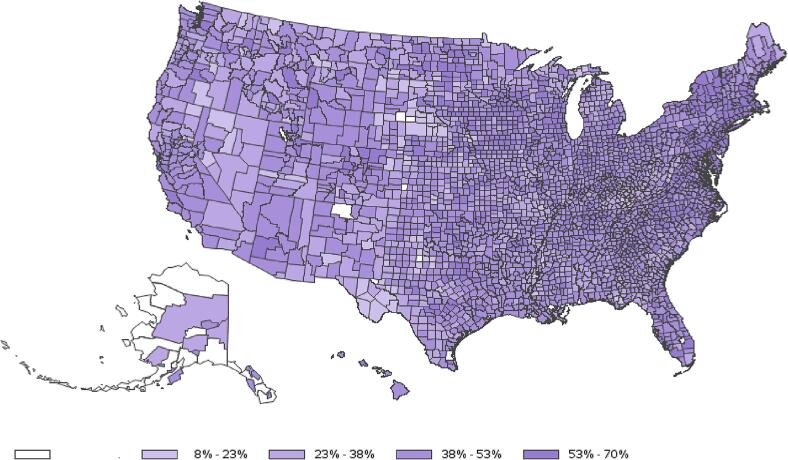
A total of 30,265,047 beneficiaries from 3,125 counties were identified, of which 53% received a flu vaccination during the 2018–2019 flu season. After eliminating counties with less than 500 Medicare beneficiaries, 3,006 counties were included in the sample. As shown in Fig. 1, the uptake varied by county within the same state. The mean county-level uptake was estimated to be 47.7%, ranging from 3.5 to 72.3% (Table 1). The mean uptakes in counties where a portion of, or an entire county was designated as a health professional shortage area (HPSA) (42.6% and 48.4%, respectively), were lower than the uptakes for the non-HPSA counties (53.8%). Metro counties (53.2%) showed higher uptakes than non-metro counties (44.2%). Mean county-level uptake was the highest in Northeast region (55.1%) followed by the South (47.9%), Midwest (47.7) and West (42.8%) regions. Descriptive statistics of county characteristics variables illustrate the variations (Supplemental Table 1 and 2). County-level uptake information is available upon request.
Fig. 1.
County-level Seasonal Influenza Vaccine Uptakes among Fee-for-Service Medicare Beneficiaries, 2018–19 flu season. Note: Blanked counties in white colored cells represent missing data.
Table 2 presents the linear regression analysis results for the county-level flu uptakes. In the full sample analysis, for demographics, the percent of working adults aged 18–64 years and female were positively associated, while the percent Black and Hispanic were negatively associated. For socioeconomic conditions, proportions of persons with limited proficiency of English, college education or above, single parent families, multi-unit housing, and living in group quarters were positively associated and significant. Under transportation and communications, the percent of workers commuting by public transportation was negatively associated. The proportions of workers who walk to work and have no internet access were also negatively associated and significant.
Table 2.
Linear regression estimation results with the fixed effects of states (N = 3,006).
| Variable | Estimate | SE | 95% CL | Pr > |Z| | |
|---|---|---|---|---|---|
| Intercept | −0.794 | 0.205 | −1.195 | −0.393 | 0.00 |
| Demographics | |||||
| % AGE 18–64 | 0.003 | 0.001 | 0.001 | 0.006 | 0.02* |
| % FEMALE | 0.009 | 0.002 | 0.005 | 0.013 | <0.0001* |
| % AFRICAN AMERICAN | −0.002 | 0.000 | −0.003 | −0.001 | <0.0001* |
| % HISPANIC | −0.003 | 0.001 | −0.004 | −0.001 | 0.00* |
| Socioeconomic conditions | |||||
| % NON-ENGLISH SPEAKERS | 0.002 | 0.001 | 0.000 | 0.003 | 0.02* |
| % FAMILIES BELOW POVERTY | −0.002 | 0.001 | −0.004 | 0.000 | 0.07 |
| % PERSONS WITH DISABLITIES | −0.001 | 0.001 | −0.003 | 0.001 | 0.21 |
| % COLLEGE + EDUCATION | 0.002 | 0.000 | 0.001 | 0.002 | 0.00* |
| % SINGLE PARENT | 0.003 | 0.001 | 0.000 | 0.005 | 0.03* |
| % MULTI-UNIT HOUSING | 0.003 | 0.001 | 0.001 | 0.004 | <0.0001* |
| % LIVING IN GROUP QUARTERS | 0.003 | 0.001 | 0.001 | 0.004 | 0.00* |
| Transportation and communications | |||||
| % PUBLIC TRANS TO WORK | −0.004 | 0.001 | −0.005 | −0.002 | <0.0001* |
| % WALK TO WORK | −0.007 | 0.001 | −0.010 | −0.005 | <0.0001* |
| % NO INTERNET ACCESS | −0.001 | 0.001 | −0.002 | 0.000 | 0.03* |
| Access to healthcare and health behaviors | |||||
| PHARMACY PER 100,000 | −0.001 | 0.000 | −0.002 | −0.001 | <0.0001* |
| % LACK OF HEALTH INSURANCE | 0.009 | 0.003 | 0.003 | 0.015 | 0.00* |
| % ROUTINE CHECK-UP | 0.006 | 0.003 | 0.001 | 0.011 | 0.02* |
| % TAKING HIGH BLOOD PRESSURE MEDICATIONS | 0.003 | 0.003 | −0.002 | 0.009 | 0.24 |
| % POOR HEALTH | −0.011 | 0.004 | −0.019 | −0.003 | 0.01* |
| % DENTAL VISITS | 0.002 | 0.001 | 0.000 | 0.003 | 0.11 |
| Health professional shortage areas | |||||
| PART | −0.023 | 0.008 | −0.038 | −0.008 | 0.00* |
| WHOLE | −0.036 | 0.009 | −0.053 | −0.019 | <0.0001* |
| NON-HPSA (Referent) | – | – | – | – | – |
SE: Standard Error, CL: Confidence Limits. *Statistically significant at 5% level.
Note: The dependent variable was county-level flu vaccine uptake for 2018–2019 flu season. PROC GENMOD was used for the regression with the fixed effects of states and cluster robust standard errors.
In terms of healthcare access, the number of pharmacies per 100,000 people was negatively associated and significant. While the proportion of residents with the lack of health insurance was positively associated, it was significant. The percent of healthcare provider visits was positively associated and significant. The percent of persons with poor health was negatively associated and significant. The percent taking high blood pressure and dental visits presented positive associations. Counties with HPSA designation had lower flu vaccine uptakes. In particular, counties where a whole county was designated as HPSA were associated with much lower flu vaccine uptakes than non-HPSA counties. Counties where parts of the counties were HPSA were also associated with much lower flu vaccine uptakes than non-HPSA counties.
4. Discussions
We analyzed how flu vaccination rates vary by counties and identified strategic county characteristics associated with higher or lower county vaccination rates. The county-level uptake varied widely and was lower than the national average: an overall mean of 47.7% with a wide range of 3.5% to 72.3% for the flu season of 2018 – 2019. This study demonstrates that counties with higher estimated flu vaccination uptakes were associated with having a higher percentage of females, persons with a college education or higher, multi-unit housing, persons living in group quarters, a lower percentage of workers walking to work, and with no internet access. In addition, the percentage of Black and Hispanic population were negatively associated with flu vaccine uptake, confirming the presence of racial disparities at the county level. Results derived from the general regression model indicated that poverty negatively affects uptake. Recently, specific socioeconomic conditions have been acknowledged as major obstacles for national and local public health stakeholders to intervene the low coverage of flu vaccination as well as to respond to the pandemics [10], [17], [18]. Previous literature also highlights the importance of tailoring public health interventions to the needs of populations with lower socioeconomic status such as public-housing residents, single-parent families, and low income populations [19]. Early intervention of community mitigation is crucial in the prevention of vaccine-preventable diseases and for a pandemic countermeasure among those at greater risk for disproportionate impact. Thus, to increase vaccine uptake, it is in the interest of local and national public health stakeholders, healthcare providers, and community groups, to account for the needs of medically underserved populations with lower socioeconomic status when designing a public health intervention.
Despite the long-standing flu vaccination coverage under Medicare Part B, the national flu vaccine uptake among adults age 65 and older has been suboptimal, plateauing around 65% [20]. Our overall flu uptake estimate is much lower (53%). Of note is that the study population is Medicare FFS beneficiaries who are not necessarily representative of adults aged 65 and older. Also, the claims data are designed for Medicare reimbursement, not for research. Thus, such wide variation may reflect a mix of variation by county in uptakes and the limitation of the data. Nevertheless, the wide range of the county-level uptake implies that the same flu vaccination benefits may not yield similar levels of impact in the prevention of flu disease. This warrants a locally differentiated approach to improve flu vaccine uptake to minimize the burden of disease. Previous literature has characterized the individual flu vaccination receipt among beneficiaries by health insurance status, the nativity and access-to-care status [16]. One of our findings that flu vaccine uptake was lower in areas where there was a shortage of healthcare professions confirms such concern. However, the positive association of flu vaccine uptake with the percent of provider visits may imply that utilizing health check-up visits may help vaccinate more people during the flu season. The positive association of flu vaccine uptake with the lack of health insurance among adults may be reassuring that Medicare can serve as safety-net health insurance in the counties with less health insurance access. Although the number of pharmacies per 100,000 people was negatively associated, the role of pharmacy in immunization practices should not be undermined as more recent studies have found that more pharmacies are offering vaccinations to adults [21], [22]. The lack of internet access was negatively and significantly associated with flu vaccine uptake, implying that information access may play important role in immunization intervention in addition to healthcare access. Previous study reported higher flu vaccination coverages among US citizens compared with foreign-born responders based on the survey.
Understanding the relationships between public health outcomes and community-level data can help identify targeted public health interventions at a local level. In April 2023, a set of new Z codes (Z55 – Z65) for reporting social determinants of health (SDOH) was added to collect and document SDOH data of patients from providers [23]. These codes may enhance the ability to identify social risk factors at the individual level in addition to identification of individual risk factors, such as clinical history or demographic characteristics. Such data would allow for deeper understanding of the role of SDOH. Also, while our study considered only one seasonal influenza season, pre-COVID-19 pandemic, the landscape of flu vaccination at the county-level, as well as the individual behaviors, may have changed. Therefore, future studies including more seasons to examine the dynamics of barriers and public health countermeasures to increase flu vaccination uptakes will be useful.
This study was subject to limitations. First, as stated earlier, this study is based on FFS claims submitted to CMS for reimbursement. Thus, flu vaccinations received by beneficiaries for which claims were not submitted by the provider cannot be captured. Second, this study did not include Medicare beneficiaries covered under Medicare Advantage (MA) Plans as the data were not available. Beneficiaries under MA plans may show different patterns in provider encounters for preventive care. Secondly, as the outcome measure of this study is the county-level flu uptake of FFS Medicare beneficiaries, the impact of socioeconomic and county-level characteristics may impact other public health outcomes such as census tract level uptakes differently. Lastly, this study did not distinguish the receipts of standard dose and high-dose flu vaccines. ACIP recently updated the recommendations for seasonal influenza vaccination that adults aged ≥ 65 years are recommended to preferentially receive higher dose or adjuvanted influenza vaccines [24]. The assessment of any opportunities or challenges in such changes of recommendations could be another aspect of addressing the disparities or heterogeneity in flu vaccination uptakes as reported in previous literature [25].
Given the large proportion of beneficiaries covered by the FFS plan whose claims data we included in our analysis, the results confirmed that county-level flu vaccine uptakes are low, reflect persisting racial disparities in vaccine uptake, and Medicare populations in medically underserved communities with lower socioeconomic status need more attention in improving flu vaccine uptakes.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Cindy Weinbaum, Shannon Stokely, Yuping Tsai, Fangjun Zhou, Andrew Leidner, James Singleton and Kai Hong for their insightful comments and suggestions.
Data availability
The data that has been used is confidential.
References
- 1.Grohskopf L.A., Alyanak E., Ferdinands J.M., Broder K.R., Blanton L.H., Talbot H.K., et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2021–22 Influenza Season. MMWR Recomm Rep. 2021;70(5):1–28. doi: 10.15585/mmwr.rr7005a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Estimated Flu-Related Illnesses, Medical visits, Hospitalizations, and Deaths in the United States — 2019–2020 Flu Season. In: National Center for Immunization and Respiratory Diseases, editor.2021.
- 3.Centers for Disease Control and Prevention. Influenza Vaccination Coverage for Persons 6 Months and Older. FluVaxView. May 28, 2021 edVarious Years.
- 4.U.S. Department of Health and Human Services. Increase the proportion of people who get the flu vaccine every year — IID‑09. In: Office of Disease Prevention and Health Promotion, editor. Healthy People 2030.
- 5.Centers for Disease Control and Prevention. Estimated Influenza Illnesses, Medical visits, and Hospitalizations Averted by Vaccination in the United States — 2019–2020 Influenza Season. In: National Center for Immunization and Respiratory Diseases, editor.2020. p. This web page provides estimates on the burden of influenza and the effects of annual influenza vaccination in the United States for the 2019–20 influenza season.
- 6.Takayama M., Wetmore C.M., Mokdad A.H. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev Med. 2012;54(5):358–362. doi: 10.1016/j.ypmed.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Gai Y., Feng L.i. Relationship between pharmacist density and adult influenza vaccination after controlling for individual and neighborhood effects. J Am Pharm Assoc. 2017;57(4) doi: 10.1016/j.japh.2017.03.011. 474-482.e12. [DOI] [PubMed] [Google Scholar]
- 8.Shen A.K., Warnock R., Selna W., MaCurdy T.E., Chu S., Kelman J.A. Vaccination among Medicare-fee-for service beneficiaries: characteristics and predictors of vaccine receipt, 2014–2017. Vaccine. 2019;37(9):1194–1201. doi: 10.1016/j.vaccine.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Hall L.L., Xu L., Mahmud S.M., Puckrein G.A., Thommes E.W., Chit A. A map of racial and ethnic disparities in influenza vaccine uptake in the medicare fee-for-service program. Adv Ther. 2020;37(5):2224–2235. doi: 10.1007/s12325-020-01324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strully K.W., Yang T.-C. County social vulnerability and influenza vaccine rates: national and local estimates for medicare recipients. Am J Prev Med. 2022;62(1):e1–e9. doi: 10.1016/j.amepre.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services. Medicare Part B Immunization Billing: Seasonal Influenza Virus, Pneumococcal, and Hepatitis B. Medicare Learning Network Educational Tool; 2018.
- 12.Centers for Disease Control and Prevention. Immunization Information Systems: NDC Lookup Crosswalk. 2021.
- 13.Centers for Disease Control and Prevention USDoHaHSOoMH. Minority Health Social Vulnerability Index (SVI). 2021.
- 14.Health Resources and Services Administration. Area Health Resources Files - 2019-2020 County Level Data. July 20, 2020 ed2019-20.
- 15.Centers for Disease Control and Prevention. PLACES: County Data (GIS Friendly Format), 2020 release. PLACES: Local Data for Better Health. September 29, 2021 ed.
- 16.Williams W.W., Lu P.-J., O’Halloran A., Kim D.K., Grohskopf L.A., Pilishvili T., et al. Surveillance of Vaccination Coverage among Adult Populations - United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28. doi: 10.15585/mmwr.ss6611a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tolbert J., Orgera K., Garfield R., Kates J., Artiga S. Kaiser Family Foundation; Issue Brief: 2021. Vaccination is Local: COVID-19 Vaccination Rates Vary by County and Key Characteristics. [Google Scholar]
- 18.Hughes M.M., Wang A., Grossman M.K., Pun E., Whiteman A., Deng L.i., et al. County-Level COVID-19 Vaccination Coverage and Social Vulnerability - United States, December 14, 2020-March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431–436. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouye K., Truman B.I., Hutchins S., Richard R., Brown C., Guillory J.A., et al. Pandemic influenza preparedness and response among public-housing residents, single-parent families, and low-income populations. Am J Public Health. 2009;99(S2):S287–S293. doi: 10.2105/AJPH.2009.165134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2019–20 Influenza Season. FluVaxView. 10/01/2020 ed2020.
- 21.Berenbrok L.A., Gabriel N., Coley K.C., Hernandez I. Evaluation of frequency of encounters with primary care physicians vs visits to community pharmacies among medicare beneficiaries. JAMA Netw Open. 2020;3(7):e209132-e. doi: 10.1001/jamanetworkopen.2020.9132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bartsch S.M., Taitel M.S., DePasse J.V., Cox S.N., Smith-Ray R.L., Wedlock P., et al. Epidemiologic and economic impact of pharmacies as vaccination locations during an influenza epidemic. Vaccine. 2018;36(46):7054–7063. doi: 10.1016/j.vaccine.2018.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. ICD-10-CM Official Guidelines for Coding and Reporting FY 2023 -- UPDATED April 1, 2023 (October 1, 2022 - September 30, 2023) 2023 release of ICD-10-CM. 2023:103-4.
- 24.Grohskopf L.A., Blanton L.H., Ferdinands J.M., Chung J.R., Broder K.R., Talbot H.K., et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices - United States, 2022–23 Influenza Season. MMWR Recomm Rep. 2022;71(1):1–28. doi: 10.15585/mmwr.rr7101a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahmud S.M., Xu L., Hall L.L., Puckrein G., Thommes E., Loiacono M.M., et al. Effect of race and ethnicity on influenza vaccine uptake among older US Medicare beneficiaries: a record-linkage cohort study. Lancet Healthy Longev. 2021;2(3):e143–e153. doi: 10.1016/S2666-7568(20)30074-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.