Abstract
Tibiotalocalcaneal (TTC) arthrodesis is commonly performed to salvage a failed total ankle replacement. These salvage procedures are complicated by significant bone loss from the ankle replacement and are associated with low patient satisfaction. Here, we describe 2 cases of patients who presented with a failed total ankle replacement and underwent arthrodesis using a bulk femoral head allograft and a novel pseudoelastic intramedullary nail. The intramedullary nail contains an internal pseudoelastic element that adapts to bone resorption and settling allowing for compression to be maintained at the arthrodesis sites throughout healing. In the first case, a 65-year-old woman with a failed total ankle replacement underwent TTC arthrodesis. The second case involved an obese 53-year-old woman who had previously undergone 2 total ankle replacement procedures that resulted in unsuccessful outcomes. In both cases, union was demonstrated on computed tomographic scan by 6 months. At 2 years postsurgery, both patients were satisfied with the procedure. These cases provide preliminary evidence that tibiotalocalcaneal arthrodesis with a pseudoelastic IM nail and structural allograft is an appropriate treatment for failed total ankle replacements.
Level of Evidence: Level IV, therapeutic, case series.
Keywords: tibiotalocalcaneal arthrodesis, intramedullary nail, sustained compression, bulk structural graft, total ankle replacement conversion, NiTiNOL
Commentary: A report of 2 patients with failed total ankle replacement managed with an innovative fixation device, an elastic intramedullary nail along with a bulk femoral head allograft. It presents another treatment option for this challenging clinical problem.
Introduction
Total ankle replacements (TARs) are increasingly being performed to treat patients with severe ankle arthritis. 41 Though the latest generation TAR devices demonstrate improved short- to midterm outcomes compared with previous generation designs, failure rates are still reported around 10% to 20%,10,13,14,17,31 with their long-term success still unknown. Complications such as infection, mechanical failure, aseptic loosening, and implant migration are also frequent with occurrence reported up to 50%.10,11,16,18 Revising a failed TAR is a complex procedure often requiring a surgeon to address severe bone loss, weakened soft tissues, and significant hindfoot pathology. 38 Under these conditions, a new TAR prosthesis is not always a viable revision option, and the TAR frequently must be converted to a salvage tibiotalocalcaneal (TTC) arthrodesis11,25 or amputation.
A successful arthrodesis is dependent on having sufficient bone and healing capacity to facilitate fusion with either an external frame, an internal plate, or an intramedullary (IM) nail applied to rigidly fixate and stabilize the joints. IM nails are advantageous in that they have increased patient tolerance and fewer complications compared to external frames.3,22,23,43 Because of implant subsidence and extensive bone loss associated with TAR failures, the talus is often removed in the salvage procedure, and the large bony void filled with a bulk femoral head allograft. Achieving fusion with these structural allografts can be challenging because of the graft’s inherent poor healing capacity, with fusion rates reported as low as 50% when a femoral head allograft was used with an IM nail.5,24 Compression has been shown to be important not only in stabilizing the arthrodesis sites but also in promoting bone healing and allowing for load sharing between implanted devices and native osseous tissue to prevent fatigue fracture of hardware.2,40
Although most IM nails are designed to generate arthrodesis site compression at the time of surgery,35,43 this initial compression can be significantly reduced after surgery because of joint settling and bone resorption. In particular, studies using a synthetic bone model reported that 1 mm of simulated resorption can lead to a 90% or greater reduction in compressive load applied by an IM nail, whereas 1.4 mm of simulated resorption leads to a 98% or greater loss of compression for all IM nails tested.21,43 An additional study reported that patients treated with second-generation IM nails incorporating an internal compression mechanism experienced faster times to fusion and higher fusion rates than patients treated with first-generation IM nails lacking an internal compression feature. 40 However, when controlling for diabetic patients, these differences became insignificant, potentially a result of the second-generation IM nail not being able to maintain compression in response to bone resorption or settling. As such, evolving IM nail designs should focus on sustained compression as this could serve as a means to reduce the nonunion rate and number of complications with TTC arthrodeses, particularly when performed to convert failed TARs. 40
Here we present 2 cases of patients who presented with failed TARs and underwent conversion to TTC arthrodesis using a bulk femoral head allograft and a novel pseudoelastic IM nail. The pseudoelastic nail contains an internal compressive element made out of nickel titanium (NiTiNOL), which is stretched during surgery, and has the capacity to maintain postoperative compression for up to 6 mm of bone resorption and/or joint settling.21,27,30,32,43 This resorption or settling can be quantitatively tracked on radiographs by visualizing changes in the calcaneal screw positions relative to the nail outer body.27,32 As the NiTiNOL compressive element contracts to its original unstretched length, the calcaneal screws shift proximally within the nail’s outer body. The recovery of the pseudoelastic element can be quantified from the lateral radiograph by measuring the position of the distal screws in the slot in the body of the nail. Both patients provided written permission for publication of this data.
Case Report 1
A 65-year-old woman presented with a failed total ankle arthroplasty with painful hardware (Agility; DePuy), which displayed loosening on computed tomography (CT) images. The patient initially underwent ankle replacement 7 years prior to the subject surgery due to arthritis. She then required revision ankle replacement as a result of constant pain, leading to implantation of the Agility hardware 2 years prior to the subject surgery. An anterior incision was created followed by ankle arthrotomy where an extensive debridement and synovectomy were performed. Tibial and talar exostectomies were performed and the ankle Agility LP implants were removed. Screws were removed through multiple incisions. A curette and burr were used to expose part of the subtalar joint. A thawed fresh-frozen femoral head allograft was then shaped to fit the bone void. Then bone marrow aspirate was harvested and the femoral head allograft was soaked in the bone marrow. The allograft was then placed into the ankle joint along with human cellular matrix containing mesenchymal stem cells, neonatal fibroblasts, growth factors, and extracellular matrix 12 (Ovation; Osiris Therapeutics, Columbia, MD). Next, a 10×220-mm pseudoelastic IM nail (DynaNail; MedShape, Inc, Atlanta, GA) was placed according to the manufacturer’s recommended operative technique. The NiTiNOL compressive element was stretched 6 mm before fixating with screws. Next a proximal tibial bone graft was performed and further bone graft was placed into the sinus tarsi area of the subtalar joint and into the talar neck area where further Ovation was added. At this point, the talar neck was fixed to the allograft using a 5-mm fully threaded cannulated screw. All wounds were irrigated well, followed by closure. The patient was placed in a short-leg non-weight bearing splint.
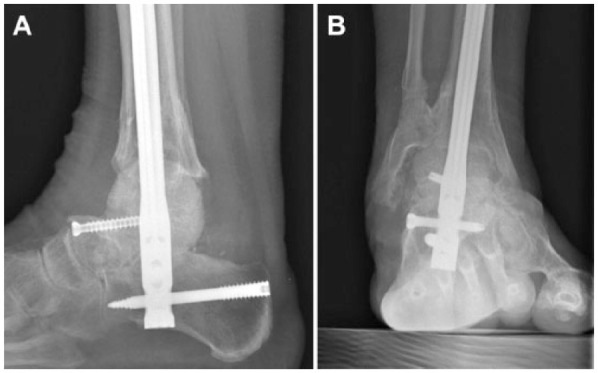
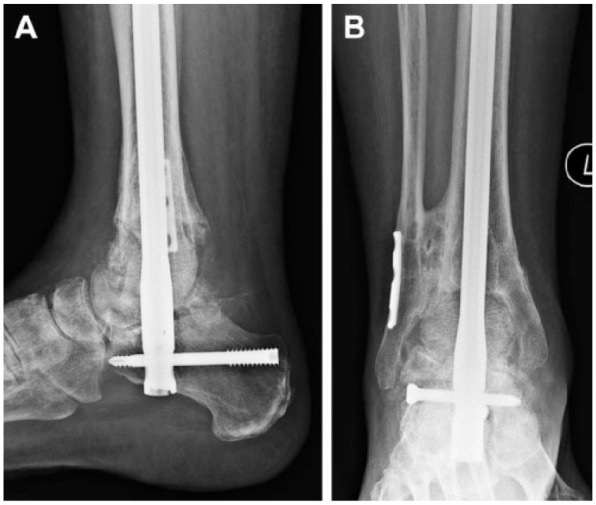
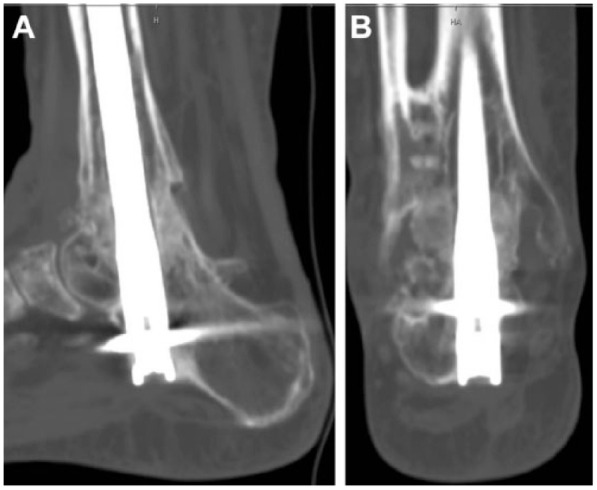
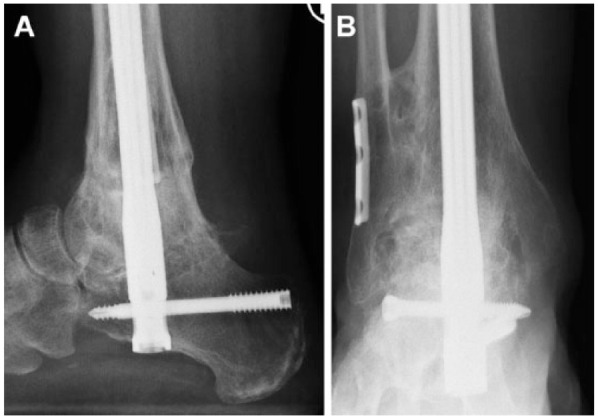
A lateral radiograph taken 4 days postsurgery demonstrated that the NiTiNOL compressive element had unloaded a total of 2.7 mm in response to bone resorption and settling while still maintaining compression (Figure 1). Two weeks postsurgery, the patient’s wounds had healed. She was no longer experiencing pain and displayed minimal swelling. Six weeks following surgery, the patient was transitioned to a weight-bearing cast. Radiographs (Figure 2) revealed that the compressive element had unloaded an additional 0.1 mm for a total of 3.6 mm. At 9 weeks postoperation, the patient was transitioned to a boot that she would wear for the following 4 weeks. A computed tomographic scan (Figure 3) taken at 6 months following surgery showed 100% fusion of both the tibiotalar and subtalar joints. The patient returned for follow-up 15 months following surgery, at which time she was hiking without pain, and she was experiencing no tenderness. The patient stated that her subject leg felt slightly shorter than the contralateral leg, and she wore a slight sole insert at times to account for the discrepancy. Radiographs taken at that time (Figure 4) showed continued ankle and subtalar fusion. A summary of the element unloading with time is shown in Figure 5 for both patients. Twenty-four months following the subject surgery, the patient completed a Foot and Ankle Ability Measure (FAAM) activities of daily living (ADL) survey. 33 She indicated that she had either slight or no difficulty with most tasks and activities (15/21), with a FAAM ADL score of 65, representing 77% of the total possible score. This score includes a zero value for the patient being unable to come up on her toes because of her fusion. She summarized her condition as “doing great,” adding that her “quality of life is restored to what it used to be before [her] first ankle replacement. . .but without the pain of a very arthritic ankle.”
Figure 1.

Case 1: Radiograph taken 4 days postsurgery displaying lateral view.
Figure 2.
Case 1: Radiographs displaying lateral (A) and oblique (B) views obtained 6 weeks following DynaNail and bulk femoral head allograft implantation.
Figure 3.

Case 1: Computed tomographic images displaying lateral (A) and anteroposterior (B) views obtained 6 months following DynaNail and bulk femoral head allograft implantation.
Figure 4.
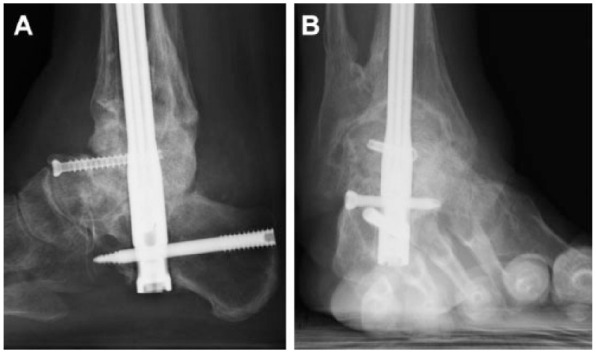
Case 1: Radiographs displaying lateral (A) and oblique (B) views obtained 15 months following DynaNail and bulk femoral head allograft implantation.
Figure 5.
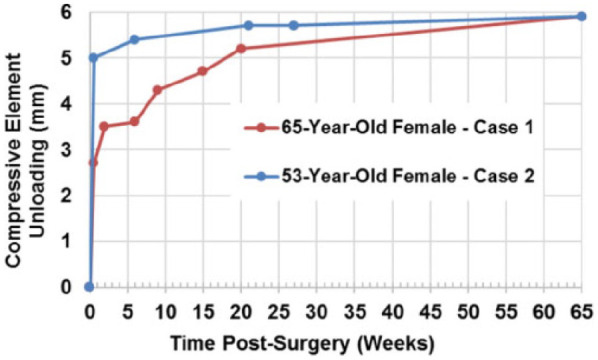
Compressive element unloading for both patients versus time postsurgery.
Case Report 2
A 53-year-old obese woman, with a BMI of 34, had a failed right ankle replacement (Agility; DePuy) causing pain 10 years following initial placement. A revision ankle replacement was performed including initial hardware removal, placement of hardware components (INBONE; Wright Medical), right subtalar fusion with cannulated screw, and Achilles tendon lengthening. Fourteen months later, the replacement revision had failed with the patient experiencing pain and nonunion of the subtalar joint, necessitating additional operative treatment. An anterior incision was made and hardware including cannulated screw, talar dome, and tibial tray was removed. Joint surfaces were decorticated, autograft bone was excised from the proximal lateral tibia, and right iliac crest bone marrow aspirate was collected. Next, a femoral head allograft was fashioned, soaked in bone marrow aspirate, and placed into the fusion site to hold the patient out to length. A 10×220-mm pseudoelastic nail (DynaNail) was then implanted according to the manufacturer’s recommend operative technique with the NiTiNOL compressive element stretched 6 mm prior to nail fixation with transverse screws. A small rhBMP-2-soaked absorbable collagen sponge (InFuse; Medtronic, Minneapolis, MN) was placed posteriorly, bridging between the tibia and talus along with bone and marrow reamings from the tibial IM canal, and then an additional small rhBMP-2-soaked absorbable collagen sponge (InFuse) was placed anteriorly along with additional reamings and bone marrow aspirate. At this point, the talar neck was stable against the femoral head, and an extra cannulated screw was not necessary to compress them together. The patient was placed in a non-weight bearing splint.
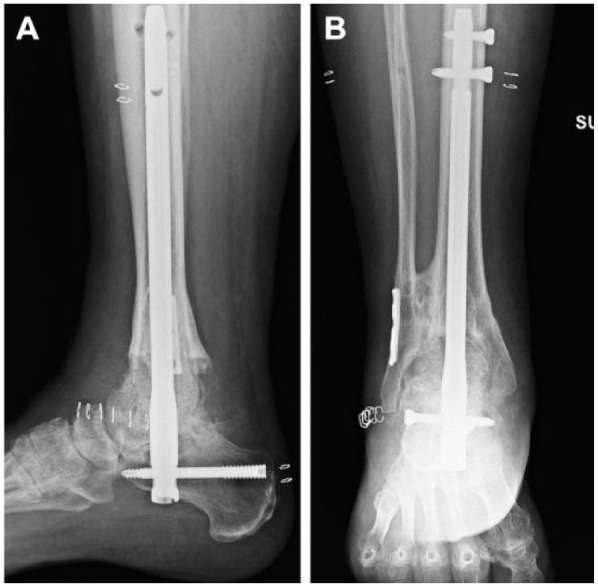
Radiographs taken 4 days postsurgery demonstrated that the position of the P-A screw had shifted proximally in the outer nail body slot corresponding to the compressive element unloading a total of 5 mm (Figure 6). Two weeks following surgery, the wound was well healed. Radiographs taken 6 weeks following surgery indicated that the compressive element had unloaded an additional 0.4 mm (Figure 7), with no evidence of hardware loosening or failure. The patient was transitioned to a weight-bearing cast. By 9 weeks postsurgery the patient was no longer experiencing pain or swelling and was transitioned to a boot for the next 6 weeks. A CT scan obtained 14 weeks postsurgery revealed 70% osseous fusion of the total surface area available at both the subtalar joint and ankle joint. Seven months following surgery, CT imaging (Figure 8) indicated 100% osseous fusion across both the subtalar and ankle joints. Fifteen months after surgery, the patient reported that she was doing well, and radiographs demonstrated that the element had unloaded a total of 5.9 mm (Figure 9). The patient stated that she feels her subject leg feels slightly shorter than the contralateral leg, and she wears a thin lift under her orthotic to account for the discrepancy. Twenty-three months after surgery, the patient completed a FAAM activities of daily living survey. She indicated that she had either slight or no difficulty with most tasks and activities (17/21), with a FAAM ADL score of 67, representing 80% of the total possible score. This score includes a zero value for the patient being unable to come up on her toes due to her fusion. She self-assessed her current level of function during daily activities at 85% of the level prior to the initiation of her foot and ankle problems.
Figure 6.
Case 2: Radiographs displaying lateral (A) and anteroposterior (B) views obtained 4 days following DynaNail and bulk femoral head allograft implantation.
Figure 7.
Case 2: Radiographs displaying lateral (A) and anteroposterior (B) views obtained 6 weeks following DynaNail and bulk femoral head allograft implantation.
Figure 8.
Case 2: Computed tomographic images displaying lateral (A) and anteroposterior (B) views obtained 7 months following DynaNail and bulk femoral head allograft implantation.
Figure 9.
Case 2: Radiographs displaying lateral (A) and anteroposterior (B) views obtained 15 months following DynaNail and bulk femoral head allograft implantation.
Discussion
The operative management of failed TARs via conversion to TTC arthrodesis is a challenging procedure with multiple reports of low patient satisfaction and function compared with primary TTC fusion.4,11,38 This study presents 2 reports of patients who underwent conversion to TTC arthrodesis for a failed TAR using a bulk femoral head allograft to fill the void of the missing talus in combination with a pseudoelastic IM nail. Both patients achieved fusion across the ankle and subtalar joints at the 6-month follow-up visit with no reported complications.
The pseudoelastic IM nail contains an internal NiTiNOL element that is stretched during surgery like a spring and unloads postsurgery in response to resorption or joint settling. 43 This unloading allows the nail to dynamically adapt to changes in the healing environment and local osseous architecture, and consequently maintain compression across the joints.2,21,27,32 As bone resorption is a biological process that occurs over time, involving the activity of a cascade of events including the actual resorption via activity of the osteoclasts, it would be unlikely that the 5 mm of element travel observed in patient 2 4 days postsurgery was fully due to resorption. This travel could have been caused by joint settling, which could occur due to any potential shift between appositional surfaces. Additionally, the femoral head graft could have partially collapsed under loads encountered during that 5-day process, such as those due to shifting of the limb leading to gravity-induced loads and muscle contractions, the constant compression generated by the compressive element, or any potential early weight-bearing by the patient done against clinician direction.21,27,32
The use of a TTC arthrodesis IM nail to convert a failed TAR has been previously described with generally modest outcomes reported*. Fusion times range from 3 to 12 months, with complication rates varying from 13% to 78%. Nonunion is the most noted complication, with 5 studies reporting at least 20% of patients experiencing nonunion.1,4,6,13,20 In particular, one study partially attributed the nonunions to the significant bone loss associated with failed TARs and suggest the importance of holding compression to achieve fusion. Other reported complications with IM nails include deep infection, pain at nail insertion site, and proximal tibial stress fractures. Additionally, potential IM nail technical issues include difficulty keeping out of varus using a straight nail and the potential for limited distal fixation because of the nail’s fairly medial position in the calcaneus.
Though the fusion and patient satisfaction rates compare similarly to external fixation,1,7,28 IM nails offer advantages such as a simpler technique and shorter rehabilitation times. Plate fixation is another option, as plates have been reported to be biomechanically stable, especially in osteopenic bone.8,9 However, IM nails are the most attractive fixation choice for use in many patients because of less dissection and potential wound healing issues than plates. Additionally, IM nail dynamization allows for load sharing and avoidance of stress shielding.36,37
Because of the significant bone loss associated with failed TARs because of talar resection and secondary osteolysis, bulk structural allografts are used to reconstruct the talus and restore limb length. However, these graft materials introduce new challenges with achieving fusion given their poor healing capacity and propensity to resorb over time. When resorption occurs, compression is lost and the bones are no longer in direct apposition, potentially compromising the healing process. 11 Therefore, the maintenance of compression is critical in ensuring bone healing with femoral allografts. 34 The authors were only able to identify a small number of studies where femoral allografts were used with an IM nail to convert TARs. In 2 separate case series, the operative technique and reported symptomatic relief are described for 3 patients in each study.34,42 In 2 larger retrospective studies, reported nonunion rates were approximately 50%.4,11 The authors highlighted the importance of compression being applied across the entire joint surfaces.
In the 2 cases presented here where bulk femoral allografts were used with a pseudoelastic nail, both patients went on to fusion of the TTC joints, with no reported pain and minimal functional limitation. In addition, these patients started weight-bearing sooner than previously treated patients without an increase in pain and without jeopardizing the fusion rates. The timing of weight-bearing should be based on the progress of the patient and osseous growth/bridging, as well as the likely influence of added mechanical loading on future healing. If a static IM nail or nondynamized IM nail has been utilized, then weight-bearing loads in the absence of solid bony contact between joints can lead to most of the loads being transmitted by the implanted nail/hardware rather than the bone.2,26 This premature loading could stress-shield the bone, leading to fatigue failure of implanted hardware, in particular the cross screws within the nail. In contrast, the pseudoelastic nail’s sustained compression and immediate dynamization at time of surgery potentially mean that a transfer of loads can occur between compressed bone surfaces, with greater load sharing between hardware and bone. This could limit the risk of hardware failure and potentially allow for earlier safe weight bearing.32,43 Furthermore, both nails were still maintaining compression at the time of fusion as the compressive elements remained stretched and no gapping was visualized, as shown on the radiographs.
The principal limitation of this study is that it is a case study of only 2 patients with relatively limited follow-up. A secondary limitation is the parallel use of orthobiologics alongside the pseudoelastic nail in both patients, such that it is impossible to directly ascertain the contributions of each to the fusion process. However, one study reported a fusion rate of 48% in a series of 25 patients that underwent retrograde IM nail treatment with femoral head allograft for bulk defects. 5 This union rate was reported despite parallel orthobiologics use in 92% of patients and parallel bone stimulation use in 76% of patients, suggesting that differing outcomes obtained could be associated with type of IM nail used. A tertiary limitation of the study is the potential for inaccuracy in the quantification of compressive element travel from radiographic images, which in this study was measured to the nearest 0.1 mm. 15 Accurate quantification of element contraction is highly dependent on the quality and resolution of the source images. Additionally, variations in patient positioning can affect the observed lengths in images, such as out-of-plane tilt. However, all assessments were made using lateral radiographs to limit patient positional variance, and one assessor performed compressive element contraction quantification to limit any observer variance.
A strength of this report is that quantified imaging, both on radiographs and on CT, was employed to evaluate both the extent of osseous fusion and arthrodesis site resorption and settling with time. The ability to monitor the amount of resorption and settling is unique to this IM nail and could potentially allow opportunities to increase knowledge of the healing process that occurs after TTC arthrodesis, particularly when performed with bulk structural allografts where resorption is common.
In conclusion, these 2 cases provide preliminary evidence that the use of a novel pseudoelastic hindfoot fusion nail combined with a bulk femoral head allograft can achieve hindfoot arthrodesis in salvage procedures for patients who previously experienced failed total ankle replacement. Future work in the form of larger retrospective or prospective studies will allow for statistical quantitative comparisons between patient outcomes following treatment with bulk graft plus pseudoelastic nail and bulk graft plus alternate IM nail.
Footnotes
This article was originally published as: Conklin MJ, Smith KE, Blair JW, Dupont KM. Total ankle replacement conversion to tibiotalocalcaneal arthrodesis with bulk femoral head allograft and pseudoelastic intramedullary nail providing sustained joint compression. Foot Ankle Orthop. 2018 Dec 19;3(4):2473011418804487. doi:10.1177/2473011418804487.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Kathryn Elizabeth Smith, PhD, and Jeremy Webster Blair, MBA, are employees of and report other from MedShape, Inc., outside the submitted work. Kenneth Michael Dupont, PhD, is an employee of and reports other from MedShape, Inc., during the conduct of the study; other from MedShape, Inc., outside the submitted work. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Anderson JG, Coetzee JC, Hansen ST. Revision ankle fusion using internal compression arthrodesis with screw fixation. Foot Ankle Int. 1997;18(5):300-309. [DOI] [PubMed] [Google Scholar]
- 2. Anderson R, Pacaccio DJ, Yakacki CM, Carpenter RD. Finite element analysis of a pseudoelastic compression-generating intramedullary ankle arthrodesis nail. J Mech Behav Biomed Mater. 2016;62:83-92. [DOI] [PubMed] [Google Scholar]
- 3. Anderson T, Rydholm U, Besjakov J, Montgomery F, Carlsson A. Tibiotalocalcaneal fusion using retrograde intramedullary nails as a salvage procedure for failed total ankle prostheses in rheumatoid arthritis A report on sixteen cases. Foot Ankle Surg. 2005;11(3):143-147. [Google Scholar]
- 4. Berkowitz MJ, Clare MP, Walling AK, Sanders R. Salvage of failed total ankle arthroplasty with fusion using structural allograft and internal fixation. Foot Ankle Int. 2011;32(5):S493-S502. [DOI] [PubMed] [Google Scholar]
- 5. Bussewitz B, DeVries JG, Dujela M, McAlister JE, Hyer CF, Berlet GC. Retrograde intramedullary nail with femoral head allograft for large deficit tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2014;35(7):706-711. [DOI] [PubMed] [Google Scholar]
- 6. Carlsson A. Unsuccessful use of a titanium mesh cage in ankle arthrodesis: a report on three cases operated on due to a failed ankle replacement. J Foot Ankle Surg. 2008;47(4):337-342. [DOI] [PubMed] [Google Scholar]
- 7. Carlsson AS, Montgomery F, Besjakov J. Arthrodesis of the ankle secondary to replacement. Foot Ankle Int. 1998;19(4):240-245. [DOI] [PubMed] [Google Scholar]
- 8. Chiodo CP, Acevedo JI, Sammarco VJ, et al. Intramedullary rod fixation compared with blade-plate-and-screw fixation for tibiotalocalcaneal arthrodesis: a biomechanical investigation. J Bone Joint Surg Am. 2003;85(12):2425-2428. [DOI] [PubMed] [Google Scholar]
- 9. Clifford C, Berg S, McCann K, Hutchinson B. A biomechanical comparison of internal fixation techniques for ankle arthrodesis. J Foot Ankle Surg. 2015;54(2):188-191. [DOI] [PubMed] [Google Scholar]
- 10. Daniels TR, Younger AS, Penner M, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96(2):135-142. [DOI] [PubMed] [Google Scholar]
- 11. Deleu PA, Devos Bevernage B, Maldague P, Gombault V, Leemrijse T. Arthrodesis after failed total ankle replacement. Foot Ankle Int. 2014;35(6):549-557. [DOI] [PubMed] [Google Scholar]
- 12. Dikis J, Scanlan R. Injectable human stem cellular matrix for plantar diabetic foot ulcerations. Paper presented at: Desert Foot Conference; Phoenix, Arizona; 2014. [Google Scholar]
- 13. Doets HC, Zurcher AW. Salvage arthrodesis for failed total ankle arthroplasty. Acta Orthop. 2010;81(1):142-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ellington JK, Gupta S, Myerson MS. Management of failures of total ankle replacement with the agility total ankle arthroplasty. J Bone Joint Surg Am. 2013;95(23):2112-2118. [DOI] [PubMed] [Google Scholar]
- 15. Fowler JR, Ilyas AM. The accuracy of digital radiography in orthopaedic applications. Clin Orthop Relat Res. 2011;469(6):1781-1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Glazebrook MA, Arsenault K, Dunbar M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009;30(10):945-949. [DOI] [PubMed] [Google Scholar]
- 17. Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(1):199-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gross C, Erickson BJ, Adams SB, Parekh SG. Ankle arthrodesis after failed total ankle replacement: a systematic review of the literature. Foot Ankle Spec. 2015;8(2):143-151. [DOI] [PubMed] [Google Scholar]
- 19. Henricson A, Carlsson A, Rydholm U. What is a revision of total ankle replacement? Foot Ankle Surg. 2011;17(3):99-102. [DOI] [PubMed] [Google Scholar]
- 20. Hopgood P, Kumar R, Wood PL. Ankle arthrodesis for failed total ankle replacement. J Bone Joint Surg Br. 2006;88(8):1032-1038. [DOI] [PubMed] [Google Scholar]
- 21. Hsu AR, Ellington JK, Adams SB, Jr. Tibiotalocalcaneal arthrodesis using a nitinol intramedullary hindfoot nail. Foot Ankle Spec. 2015;8(5):389-396. [DOI] [PubMed] [Google Scholar]
- 22. Hsu AR, Szatkowski JP. Early tibiotalocalcaneal arthrodesis intramedullary nail for treatment of a complex tibial pilon fracture (AO/OTA 43-C). Foot Ankle Spec. 2015;8(3):220-225. [DOI] [PubMed] [Google Scholar]
- 23. Jehan S, Shakeel M, Bing AJ, Hill SO. The success of tibiotalocalcaneal arthrodesis with intramedullary nailing–a systematic review of the literature. Acta Orthop Belg. 2011;77(5):644-651. [PubMed] [Google Scholar]
- 24. Jeng CL, Campbell JT, Tang EY, Cerrato RA, Myerson MS. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int. 2013;34(9):1256-1266. [DOI] [PubMed] [Google Scholar]
- 25. Kamrad I, Henricson A, Magnusson H, Carlsson A, Rosengren BE. Outcome after salvage arthrodesis for failed total ankle replacement. Foot Ankle Int. 2016;37(3):255-261. [DOI] [PubMed] [Google Scholar]
- 26. Karakasli A, Satoglu IS, Havitcioglu H. A new intramedullary sustained dynamic compression nail for the treatment of long bone fractures: a biomechanical study. Eklem Hastalik Cerrahisi. 2015;26(2):64-71. [DOI] [PubMed] [Google Scholar]
- 27. Kildow BJ, Gross CE, Adams SD, Parekh SG. Measurement of nitinol recovery distance using pseudoelastic intramedullary nails for tibiotalocalcaneal arthrodesis. Foot Ankle Spec. 2016;9(6):494-499. [DOI] [PubMed] [Google Scholar]
- 28. Kitaoka HB, Romness DW. Arthrodesis for failed ankle arthroplasty. J Arthroplasty .1992;7(3):277-284. [DOI] [PubMed] [Google Scholar]
- 29. Kotnis R, Pasapula C, Anwar F, Cooke PH, Sharp RJ. The management of failed ankle replacement. J Bone Joint Surg Br. 2006;88(8):1039-1047. [DOI] [PubMed] [Google Scholar]
- 30. Kreulen C, Lian E, Giza E. Technique for use of trabecular metal spacers in tibiotalocalcaneal arthrodesis with large bony defects. Foot Ankle Int. 2017;38(1):96-106. [DOI] [PubMed] [Google Scholar]
- 31. Labek G, Todorov S, Iovanescu L, Stoica CI, Bohler N. Outcome after total ankle arthroplasty—results and findings from worldwide arthroplasty registers. Int Orthop. 2013;37(9):1677-1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Latt LD, Smith KE, Dupont KM. Revision tibiotalocalcaneal arthrodesis with a pseudoelastic intramedullary nail: a case study. Foot Ankle Spec. 2017;10(1):75-81. [DOI] [PubMed] [Google Scholar]
- 33. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26(11):968-983. [DOI] [PubMed] [Google Scholar]
- 34. Moor B, Klammer G, Maquieira G, Espinosa N. Salvage arthrodesis after failed total ankle replacement: reconstruction with structural allograft and intramedullary nail. Tech Foot Ankle Surg. 2008;7(4):271-278. [Google Scholar]
- 35. Muckley T, Eichorn S, Hoffmeier K, et al. Biomechanical evaluation of primary stiffness of tibiotalocalcaneal fusion with intramedullary nails. Foot Ankle Int. 2007;28(2):224-231. [DOI] [PubMed] [Google Scholar]
- 36. Mueckley TM, Eichorn S, von Oldenburg G, et al. Biomechanical evaluation of primary stiffness of tibiotalar arthrodesis with an intramedullary compression nail and four other fixation devices. Foot Ankle Int. 2006;27(10):814-820. [DOI] [PubMed] [Google Scholar]
- 37. Pelton K, Hofer JK, Thordarson DB. Tibiotalocalcaneal arthrodesis using a dynamically locked retrograde intramedullary nail. Foot Ankle Int. 2006;27(10):759-763. [DOI] [PubMed] [Google Scholar]
- 38. Rahm S, Klammer G, Benninger E, Gerber F, Farshad M, Espinosa N. Inferior results of salvage arthrodesis after failed ankle replacement compared to primary arthrodesis. Foot Ankle Int. 2015;36(4):349-359. [DOI] [PubMed] [Google Scholar]
- 39. Schill S. Ankle arthrodesis with interposition graft as a salvage procedure after failed total ankle replacement [in German]. Oper Orthop Traumatol. 2007;19(5-6):547-560. [DOI] [PubMed] [Google Scholar]
- 40. Taylor J, Lucas DE, Riley A, Simpson GA, Philbin TM. Tibiotalocalcaneal arthrodesis nails: a comparison of nails with and without internal compression. Foot Ankle Int. 2016;37(3):294-299. [DOI] [PubMed] [Google Scholar]
- 41. Terrell RD, Montgomery SR, Pannell WC, et al. Comparison of practice patterns in total ankle replacement and ankle fusion in the United States. Foot Ankle Int. 2013;34(11):1486-1492. [DOI] [PubMed] [Google Scholar]
- 42. Thomason K, Eyres KS. A technique of fusion for failed total replacement of the ankle: tibio-allograft-calcaneal fusion with a locked retrograde intramedullary nail. J Bone Joint Surg Br. 2008;90(7):885-888. [DOI] [PubMed] [Google Scholar]
- 43. Yakacki CM, Gall K, Dirschl DR, Pacaccio DJ. Pseudoelastic intramedullary nailing for tibio-talo-calcaneal arthrodesis. Expert Rev Med Devices. 2011;8(2):159-166. [DOI] [PubMed] [Google Scholar]


