Abstract
Research indicates strong connections between child ADHD, child ODD/CD, and sleep. Children experiencing these concerns also have caregivers who report feeling more stress. However, no studies have examined how child ADHD and ODD/CD interact together and with insufficient sleep to potentially exacerbate caregiver stress. Data were acquired from the 2018/2019 National Survey of Children’s Health, a nationally representative survey of parents or caregivers conducted across the United States (U.S.). The current study used data for children 6–17 years old with a final analytic sample size of 41,541, representing a total of 47,357,862 U.S. youth. Overall child ADHD and ODD/CD were each uniquely associated with increased caregiver stress, while adequate child sleep duration was related to decreased caregiver stress. However, these findings were qualified by a significant two-way interaction that revealed that caregiver stress among children with comorbid ADHD and ODD/CD was not significantly greater than that of children with ODD/CD alone. Significant interactions between sleep and ODD/CD on caregiver stress were generally not observed, except potentially in females with ADHD. Our findings underscore the importance of considering strategies to reduce both youth symptoms and caregiver stress simultaneously. Additionally, ensuring adequate sleep for all children is recommended.
Keywords: ADHD, ODD/CD, caregiver stress, sleep, sex
Introduction
Among all children, sleep problems are highly prevalent (Meltzer et al., 2010). Specifically, the estimated prevalence of children having at least one sleep disturbance symptom is as high as 41% (Honaker & Meltzer, 2016). Sleep problems are even more common among children with Attention-Deficit/Hyperactivity Disorder (ADHD) with between 55–74% of children with ADHD experiencing sleep difficulties, 30% experiencing mild sleep problems, and 45% experiencing moderate to severe sleep problems (Noble et al., 2012; Weiss & Salpekar, 2010). In addition, about half (45–65%) of children with ADHD have a comorbid behavior disorder, such as Oppositional Defiant Disorder (ODD; Ghanizadeh et al., 2008), and the incidence of sleep problems in children with ODD has been estimated to be 27% (Hvolby et al., 2021). Each of these three difficulties are robustly associated with increased caregiver stress (e.g., Byars et al., 2011; Leitch et al., 2019), but the manner in which sleep problems impact the association between behavioral problems and caregiver stress is unclear. Understanding the influences of caregiver stress is important as caregiver stress is associated with myriad negative outcomes for caregivers and their children, including the development of internalizing symptoms in both the caregiver and their child (Deault, 2010; Rollè et al., 2017) and decreased quality of the caregiver-child relationship (Ward & Lee, 2020).
Child ADHD, Behavior Disorders, and Sleep
Research demonstrates that children with ADHD experience more sleep problems compared to children without ADHD (Kirov & Brand, 2014). The most common sleep problems among children with ADHD as reported by caregivers or children are difficulties falling asleep (e.g., delayed sleep onset) and remaining asleep throughout the night (e.g., night waking; Sung et al., 2008). They also experience shorter sleep duration, poor quality sleep, and daytime sleepiness (Hvolby et al., 2009; Scott et al., 2013), which is impacted by the use of ADHD medication (particularly psychostimulants; Galland et al., 2010). Further, sleep problems in children with ADHD are associated with increased ADHD symptom severity (Sung et al., 2008) and problems with arousal/attention systems (Miano, 2012). Studies experimentally restricting sleep duration in children and adolescents with ADHD document higher levels of inattention (Becker et al., 2019; Gruber et al., 2011), increased sluggish cognitive tempo (Becker et al., 2019), decreased inhibitory control (Cremone-Caira et al., 2020), greater daytime sleepiness (Becker et al. 2019), and more oppositional symptoms (Becker et al. 2019).
Among children with oppositional and defiant problems, research reveals that ODD is independently related to sleep problems. Sleep problems in children with ODD may result from bedtime resistance or defiance related to the structure and limits placed around bedtime (Smedje et al., 2001). For instance, in a sample of preschool-aged children oppositionality was associated with increased sleep habit problems (e.g., not going to bed at the same time every night) when considered with inattentive symptoms (Coto et al., 2018). Regarding comorbid ADHD and ODD, children with ADHD and ODD experience increased bedtime resistance, sleep onset delay, shorter sleep duration, more frequent waking during the night, and problems waking in the morning (Moreau et al., 2014). In a study comparing sleep in children with ADHD and ODD/Conduct Disorder (CD) to ADHD alone, researchers found that children with comorbid ODD/CD and their caregivers reported more sleep problems and this difference was corroborated by actigraphy data (Aronen et al., 2014). This suggests that these conditions may be linked differently to sleep and understanding their interactive influences on caregiver stress may indicate different treatment considerations.
Child Sleep and Caregiver Stress
Insufficient sleep, as indicated by receiving less than age-appropriate sleep duration nightly, is relatively common in children (Wheaton & Claussen, 2021). In addition to the link between behavioral problems and caregiver stress, children who experience more sleep problems including insufficient sleep have caregivers who are more likely to experience greater levels of stress (Byars et al., 2011). For example, in a study examining caregiver-child pairs in a sample of children 1.5–10 years with insomnia, results showed that caregiver stress was associated with both child bedtime resistance and daytime sleepiness, and that child externalizing problems and daytime sleepiness predicted caregiver stress (Byars et al., 2011). Children who have difficulty sleeping are also more likely to be irritable, contentious, and may wake their caregivers up in the night (Ball et al., 1997). It is unclear, however, how the presence of insufficient child sleep may exacerbate the negative impact on caregiver stress that child ADHD and ODD/CD also have on stress, and whether insufficient child sleep also operates independently from these commonly comorbid conditions.
Influence of Child Sex
Unfortunately, previous studies have largely ignored the influence of sex. Most researchers treat child sex as a covariate to adjust for differences (e.g., Ward & Lee, 2020), and fewer researchers have examined sex-specific associations (e.g., Hvolby et al., 2021). Indeed, calls for increased recognition and inclusion of studies expressly examining sex differences have occurred (Rucklidge, 2010), in part due to its importance when examining child behavior problems. For instance, the male to female ratio among children with ADHD in community samples is approximately 3:1 (Willcutt, 2012). Similarly, more boys than girls display ODD symptoms, though girls are more likely to display irritability while boys display more defiance problems (Leadbeater & Homel, 2015). Recently, Liu et al. (2018) found a negative relation between caregiver stress and ODD among girls, and a positive relation between boys, indicating that boys with ODD may be more likely to have caregivers with increased levels of caregiver stress.
Research examining child sleep shows discrepancies in whether sex differences influence sleep. Some studies indicate no sex differences regarding sleep functioning, duration, or quality (Lycett et al., 2015; Sung et al., 2008). Conversely, other research suggests females with ADHD experience more difficulty sleeping. Specifically, Becker et al. (2016) conducted a study of children with ADHD inattentive type and found that girls had a harder time getting up in the morning and worse caregiver-reported sleep functioning. Similarly, adult women with ADHD in another study reported high rates of sleep problem histories, including disrupted sleep and increased sleepiness during the day ((Robison et al., 2008). Thus, more research is needed to better understand sex differences regarding child behavior problems, insufficient child sleep, and caregiver stress. Understanding sex differences as they relate to this process is needed to inform treatment approaches and understand outcomes.
Current Study
Research indicates strong connections between child ADHD (Noble et al., 2012; Weiss & Salpekar, 2010), child ODD/CD (Coto et al., 2018), and sleep. Similarly, many children with ADHD have comorbid ODD/CD, and most research has shown the presence of both ADHD and ODD/CD is associated with greater sleep problems (Ghanizadeh et al., 2008). Although research has shown that children experiencing ADHD, ODD/CD, or insufficient levels of sleep have caregivers who report feeling more stress, no studies have examined how insufficient sleep duration interacts with child ADHD and ODD/CD to potentially exacerbate caregiver stress (Bode et al., 2016). Further, previous research has utilized clinical samples and generally smaller sample sizes (e.g., Byars et al., 2011); therefore, the scale of these associations from a population-level perspective is unclear. Larger sample sizes also provide a greater ability to detect potential sex differences given the somewhat inconsistent findings of past investigations. Thus, the current study addressed these gaps by investigating the combined and interactive contributions of child ADHD and ODD/CD on caregiver stress and examined whether insufficient child sleep duration and child sex moderated this association. Additionally, we addressed these gaps utilizing a large, nationally representative sample to understand levels of caregiver stress by child sleep duration and ODD/CD at the population level. The following hypotheses were made: (1) Insufficient child sleep duration, ADHD, and ODD/CD would each be associated with greater caregiver stress; and (2) insufficient child sleep duration would moderate the relationship between ADHD and ODD/CD with caregiver stress, such that insufficient sleep duration would be associated with greater caregiver stress for both diagnostic groups (Aim 1). Finally, (3) differences would emerge based on child sex, such that insufficient child sleep duration would be a stronger moderator for females than males, particularly among children with ADHD (Aim 2).
Method
Participants
Data were acquired from the 2018/2019 National Survey of Children’s Health (NSCH; available free for public download at https://www.census.gov/programs-surveys/nsch/data/datasets.html), a nationally representative survey of parents or caregivers conducted across the United States (U.S.). Respondents had to have at least one resident child aged 0 to 17 living in the home when the survey was conducted. The NSCH survey asked questions about the child’s physical and emotional well-being as well as other factors that might affect child development. Sampling procedures included mailed, self-administered surveys with the option to reply via paper or online. The overall weighted response rate for the period was 43.1 and 42.2% for 2018 and 2019, respectively. The interview completion rate was 78.0 and 79.5% among households with children. The survey employed a complex design whereby various sociodemographic factors were used to account for differential selection and responses. If the respondents reported they had more than one child living in the home, one child was randomly selected to be the subject of the survey. See Ghandour et al. (2018) for more details. The current study used data for children 6–17 years old with a final analytic sample size of 41,541 youth with complete data across measures representing a total weighted sample of 47,357,862 US youth.1
Measures
Demographics.
Respondents reported on the target child’s sex (male, female), age, race (White, Black, other), ethnicity (Hispanic, non-Hispanic), and poverty status (< 100% of federal poverty level, 100%–199% of federal poverty level, ≥ 200% of federal poverty level). Table 1 contains demographic summary statistics.
Table 1.
Sample Characteristics, Population and Estimates for US Youth Aged 6–17 years, 2018–2019.
| Unweighted Sample Size | Weighted Population | Weighted Mean/% [95% CI] | |
|---|---|---|---|
|
| |||
| All | 41,541 | 47,357,862 | — |
| Child sex | |||
| Male | 21,599 | 24,126,044 | 50.9 (49.9, 52.0) |
| Female | 19,942 | 23,231,818 | 49.1 (48.0, 50.1) |
| Age | — | 11.5 (11.4, 11.6) | |
| Child race/Ethnicity | |||
| White, non-hispanic | 28,967 | 23,813,610 | 50.3 (49.3, 51.3) |
| Black, non-hispanic | 2,690 | 6,427,177 | 13.6 (12.8, 14.4) |
| Hispanic | 4,858 | 12,152,447 | 25.7 (24.5, 26.8) |
| Multi-racial/Other race | 5,026 | 4,964,628 | 10.5 (9.9, 11.0) |
| Poverty status | |||
| <100% of FPL | 4637 | 8,862,316 | 18.7 (17.8, 19.7) |
| 100%–199% FPL | 6702 | 10,159,338 | 21.5 (20.5, 22.4) |
| 200%–399% FPL | 12,900 | 13,368,354 | 28.2 (27.3, 29.1) |
| >400% FPL | 17,302 | 14,967,855 | 31.6 (30.7, 32.5) |
| Children in household | — | 2.23 (2.21, 2.25) | |
| ADHD | |||
| Yes | 5070 | 4,887,741 | 10.3 (9.8, 10.9) |
| No | 36,471 | 42,470,121 | 89.7 (89.1, 90.2) |
| ODD/CD | |||
| Yes | 3263 | 3,586,607 | 7.6 (7.1, 8.1) |
| No | 38,278 | 43,771,255 | 92.4 (91.9, 92.9) |
| Meeting sleep guidelines | |||
| Yes | 28,549 | 31,059,577 | 65.6 (64.5, 66.6) |
| No | 12,992 | 16,298,285 | 34.4 (33.4, 35.5) |
| Caregiver stress* | — | −.04 (−.06, −.02) | |
Note:
latent factor sore.
Caregiving Stress.
The current study operationalized caregiver stress using a latent factor score (described below in the Analyses section) represented by combining four NCHS caregiver stress items used previously in other studies examining caregiver stress (Tan et al., 2017; Williams & Burnfield, 2019). The four items asked caregivers about how often in the past 30 days: 1) they have felt their child was harder to care for than most children (his/her) age, 2) their child did things that really bothered them a lot, 3) they have felt angry with their child, and 4) how well they felt they were coping with the day to day demands of parenthood/raising children (reverse scored). Items 1–3 were measured using a 4-point (1 = Very well, 4 = Not very well at all) scale, while item 4 was measured utilizing a 5-point (1 = Never, 5 = Always) scale. Higher scores indicated more caregiver stress.
Sleep Duration.
The current study used a single-item question to determine the child’s quantity of sleep. The item asked, “Over the past week, how many hours of sleep did (child) get on an average weeknight?” on a scale of 1 (less than 6 hours) to7 (11 or more hours). Responses were recoded to indicate whether children met age-specific American Academy of Pediatrics’ sleep duration guidelines (9–12 hours for ages 6–12 years and 8–10 hours for ages 13–18 years). For the purposes of this study, children were coded as meeting the recommended sleep guidelines (1 = adequate sleep duration) while those who did not meet these guidelines were considered to be experiencing insufficient sleep (0 = insufficient sleep duration).
ADHD and ODD/CD.
To measure ADHD and ODD/CD, the current study used single items which asked about child behavior problems. Respondents were first asked if a doctor/health care provider had ever told them that their child had ADHD or ODD/CD. Next, caregivers who responded yes were asked whether their child was still experiencing behavioral problems. For the purposes of the current study, children were coded as experiencing current ADHD (0 = no, 1 = yes) and current behavior disorder (ODD/CD; 0 = no, 1 = yes).
Covariates.
In data analyses, the child’s age, number of children in the home, and respondents’ reported family poverty ratio were included as covariates.
Analyses
Data were analyzed using Stata SE version 17.0 (StataCorp, College Station, TX). Due to the sampling design of the NSCH, sampling weights were used to account for potential biases (i.e., nonresponse and noncoverage). First, exploratory factor analysis (using varimax rotation) with the four indicators of caregiver stress determined loadings for each item. Results indicated that items were related, with factor loadings ranging from .61 to .88 and the factor explaining 60.2% of the variance across the four items. Thus, these four items were associated with each other and represented a single latent variable estimating caregiver stress. A single latent factor score was computed using Bartlett weighted averages based on the intercorrelations among the four indicators using SPSS, and used in remaining analyses to represent caregiver stress (DiStefano et al., 2009). Observed variables included child sleep (meeting or not meeting sleep duration guidelines), child sex (male/female), and the presence/absence of ADHD and presence/absence of ODD/CD. A linear regression was conducted to determine the influence on caregiver stress among variables, including all 2-way interactions among ADHD, ODD/CD, and adequate child sleep duration. The regression was conducted overall and stratified by sex to account for potential 3-way interactions involving sex, and included covariates identified above consistent with previous research (Tan et al., 2017; Williams & Burnfield, 2019). Statistically significant results were considered as p < .05.
Results
Overall Associations with Caregiver Stress
Table 1 displays descriptive statistics for study variables. The mean age of the sample was 11.5 years, and the majority of the children were male (50.9%) and identified as Black, Non-Hispanic (13.6%), White, Non-Hispanic (50.3%), Hispanic (25.7%), or Multiracial/Other race (10.5%; see Table 1). Results indicated that family poverty level, child age, and the number of children in the home were significant covariates and positively related to higher caregiver stress (ps < .05). As shown in Table 2, meeting adequate sleep recommendations was associated with lower caregiver stress (p < .0005) of a small magnitude (B = −.11). Conversely, the presence of ADHD and ODD/CD were each significantly and independently related to higher caregiver stress (both p < .0005), with effects indicating that caregivers of children with ADHD and ODD/CD reporting stress .53 and 1.26 SDs above the national mean, respectively.
Table 2.
Association of Sleep, ADHD, and ODD/CD with Caregiver Stress.
| Overall sample (N = 41,541) | Males (N = 21,599) | Females (N = 19,942) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| B (95%CI) | t | p | B (95%CI) | t | p | B (95%CI) | t | p | |
|
| |||||||||
| Sleep | −0.11 (−0.16, −0.06) | −4.76 | <.0005 | −0.08 (−0.15, −0.02) | −2.59 | .009 | −0.13 (−0.20, −0.07) | −4.01 | <.0005 |
| ADHD | 0.53 (0.39, 0.66) | 7.71 | <.0005 | 0.59 (0.41, 0.76) | 6.69 | <.0005 | 0.42 (0.23, 0.62) | 4.24 | <.0005 |
| ODD/CD | 1.26 (1.04, 1.48) | 11.17 | <.0005 | 1.32 (1.05, 1.59) | 9.60 | <.0005 | 1.18 (0.82, 1.54) | 6.39 | <.0005 |
| ADHD × ODD/CD | −0.37 (−0.67, −0.07) | −2.38 | .017 | −0.46 (−0.81, −0.11) | −2.59 | .01 | −0.23 (−0.82, 0.36) | −0.77 | .44 |
| ADHD × sleep | 0.05 (−0.11, 0.21) | 0.59 | .55 | −0.07 (0.27, 0.14) | −0.62 | .53 | 0.25 (−0.002, 0.50) | 1.94 | .052 |
| Sleep × ODD/CD | 0.23 (−0.04, 0.49) | 1.65 | .10 | 0.17 (−0.18, 0.51) | 0.94 | .35 | 0.28 (−0.13, 0.69) | 1.35 | .18 |
| ADHD × sleep × ODD/CD | −0.16 (−0.54, 0.21) | −0.87 | .39 | −0.07 (−0.52, 0.38) | −0.29 | .77 | −0.27 (−0.96, 0.42) | −0.77 | .44 |
Note: Child age, number of children in the home, and family poverty ratio were included as model covariates but not displayed in table. Statistically significant results were considered as p < .05.
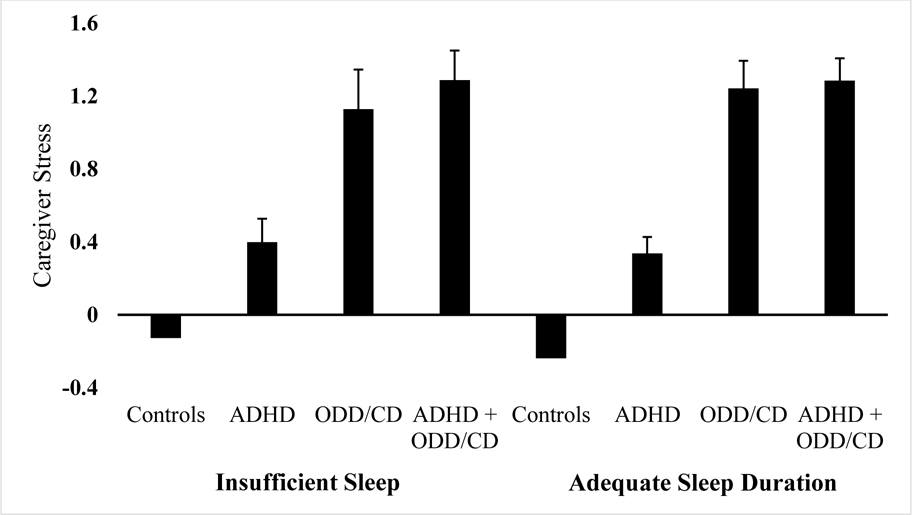
Interactions with Insufficient Sleep and Behavior Disorders
To test Aim 1, interactions between sleep, ADHD, and ODD/CD on caregiver stress were examined. Insufficient sleep duration did not significantly interact with either ADHD or ODD/CD, nor their 3-way interaction (ps > .10). In contrast, only the interaction of ADHD and ODD/CD was significant (p < .05). Specifically, the impact of ADHD among children without ODD/CD was significantly associated with increased caregiver stress (b = .56, SE = .04, p < .005), whereas the presence of ADHD among child ODD/CD was not associated with increased stress (Δ = .08, SE = .08, p = .31). Figure 1 displays the interaction. Inspection of adjusted means and overlapping/non-overlapping 95% confidence intervals indicated that caregivers of children without either ADHD or ODD/CD (i.e., No ADHD or ODD/CD; M = −.21; SE = .1, p < .001) reported significantly lower caregiver stress compared to caregivers of children with ADHD only (i.e., ADHD only; M = .36; SE = .38, p < .001), who in turn reported significantly lower caregiver stress compared to children with ODD/CD alone (i.e., ODD/CD only; M = 1.20; SE = 0.06, p < .001), or compared to comorbid ADHD and ODD/CD (i.e., ADHD + ODD/CD; M = 1.29; SE = 0.05, p = .309), who did not significantly differ.
Figure 1.
Caregiver stress as a function of ADHD and ODD/CD for full sample. Caption: Caregiver stress measured by latent factor score.
Sex Differences
The regression models were repeated and stratified by sex to test Aim 2. Among females, the model yielded identical results and magnitude of associations for the independent relations of ADHD, ODD/CD, and adequate sleep duration on caregiver stress (ps < .005). Specifically, caregivers of females with ADHD (B = .42) and ODD/CD (B = 1.18) reported moderately greater stress, respectively, than the national average, and caregivers of children receiving adequate sleep reported slightly lower stress (B = −.13). The interaction effect size between ADHD and sleep duration was moderate in magnitude (B = .25), but just failed to meet the significance cutoff (p = .052). Inspection of this interaction, which should be interpreted with caution, indicated that adequate sleep duration was associated with lower caregiver stress for female children without ADHD only (b = −.12, SE = .03, p= .001). Conversely, adequate sleep duration was not associated with caregiver stress for female children with ADHD (b = 0.11, SE = .11, p = .11). All other two-way interactions between ADHD, ODD/CD, and adequate sleep duration, along with the three-way interaction were non-significant for females (ps ≥ .18).
Among males, the stratified model also yielded identical results for the independent relations of ADHD, ODD/CD, and adequate sleep duration on caregiver stress (ps < .009). Their magnitude of associations was also comparable to, though slightly greater than, the overall model. Specifically, caregivers of males with ADHD (B = .59), and ODD/CD (B = 1.32) reported moderately greater stress, respectively, and caregivers of children receiving adequate sleep duration reported slightly lower stress (d = −.08). In contrast to females, there was no significant interaction between ADHD and adequate sleep duration (p = .53), though the ADHD and ODD/CD interaction was significant (p < .005). The ADHD and ODD/CD interaction was characterized by a negative influence of ADHD on caregiver stress only among male children without ODD/CD (b = .54, SE = .05, p < .005), whereas the presence of ADHD among male children with ODD/CD was not associated with increased stress (b = .04, SE = .10, p= .10). Inspection of means and overlapping/non-overlapping 95% confidence intervals indicated that caregivers of male children without either ADHD or ODD/CD (i.e., No ADHD or ODD/CD; M = −.18; SE = 0.16, p < .001) reported significantly lower caregiver stress compared to caregivers of children with ADHD only (i.e., ADHD only; M = .36; SE = .05, p < .001), who in turn reported significantly lower caregiver stress compared to male children with ODD/CD alone (i.e., ODD/CD only; M = 1.24.; SE = .09, p < .001), or compared to comorbid ADHD and ODD/CD (i.e., ADHD + ODD/CD; M = 1.28; SE = .05, p = .724), who did not significantly differ. All other two-way interactions between ADHD, ODD/CD, and adequate sleep duration, and the three-way interaction were non-significant (ps ≥ .22).
Discussion
Research has demonstrated the strong link among child ADHD, ODD/CD, and sleep problems (e.g., Coto et al., 2018; Hvolby et al., 2021; Kirov & Brand, 2014; Weiss & Salpekar, 2010). Research has also established that these factors influence caregiver stress (Evans et al., 2020; Leitch et al., 2019). However, no studies have investigated how insufficient sleep duration in children interact with ADHD and ODD/CD to exacerbate caregiver stress and if differences were present based on child sex. The present study addressed this gap in the literature in a large nationally representative survey of caregivers across the U.S. Insufficient sleep duration did not exacerbate the negative associations among ADHD and ODD/CD on stress, which was inconsistent with the hypothesis for our primary aim. Rather, findings demonstrated that overall child ADHD and ODD/CD were uniquely associated with increased caregiver stress, while adequate child sleep duration on its own was related to slightly decreased caregiver stress. Overall, these independent relations were consistent with the extant literature (e.g., Byars et al., 2011; Coto et al., 2018; Hvolby et al., 2021; Kirov & Brand, 2014; Weiss & Salpekar, 2010).
Interestingly, the findings revealed that caregiver stress among children with comorbid ADHD and ODD/CD was not significantly greater than that of children with ODD/CD alone. These specific findings were similar across sex which was also contrary to hypotheses for our secondary aim. However, some evidence cautiously indicated that adequate sleep duration for females without ADHD was associated with decreased caregiver stress. Further, sex did not alter the pattern of interactions among the other variables. All findings were independent of the influence of child age, family poverty level, and the number of children in the household.
Since this study utilized a nationally representative sample of caregivers, it was positioned to describe the magnitude of stress being experienced by caregivers of children with ADHD, ODD/CD, and insufficient sleep duration at the population level. Insufficient sleep in children demonstrated a small effect on caregiver stress compared to the national average. Notably, ADHD alone demonstrated a greater than one-half standard deviation increase in caregiver stress compared to the national average, whereas ODD/CD whether alone or in combination with ADHD demonstrated greater than a one standard deviation increase in caregiver stress. There are several potential explanations for this pattern. First, it is possible that caregivers of children with ODD/CD have more negative parent-child interactions due to increased child aggression (e.g., hitting, destruction of property) that leads to caregiver feelings of distress (Ljungström et al., 2020). This would be consistent with qualitative work that has documented that the externalizing behavior of children with ADHD is a major factor related to caregiver stress (Leitch et al., 2019; Mofokeng & van der Wath, 2017). Indeed, meta-analyses indicated that among children with ADHD, both inattentive symptoms and hyperactivity/impulsivity were associated with caregiver stress. However, inattention evinced a smaller effect size (r = .37) than hyperactivity/impulsivity (r = .49) on caregiver stress (Theule et al., 2013).
Overall, most findings were consistent across sex. It was hypothesized child sleep duration would moderate the relation between ADHD and ODD/CD and caregiver stress, particularly more so for females than males. Our findings suggested a marginally significant interaction between sleep duration and ADHD on caregiver stress in the stratified female sample. These findings may be the result of our study covering a broad age range that may have masked significant effects across this period compared to previous studies (e.g., Becker et al., 2016; Lycett et al., 2015). Child age has relevance for sleep as developmental changes occur across the ages included, though the current design accounted for age-based recommendations for adequate sleep duration and adjusted for the impact of age. For example, pubertal maturation during adolescence has been linked to increased night waking (Belmon et al., 2019). This may be further impacted by family contexts such as decreased caregiver involvement and enforcement of healthy sleep habits. Nonetheless, results support efforts to ensure children meet established sleep guidelines, regardless of sex, to promote positive development.
Child ADHD, ODD/CD, and insufficient sleep duration were each independently related to increased levels of caregiver stress. This underscores the importance of assessing caregiver stress when serving children with ADHD, ODD/CD, or sleep concerns as well as assessing each factor. Since an effect was observed with a four-item measure of caregiver stress, clinicians may consider briefly screening caregiver stress during diagnostic assessments and throughout psychosocial interventions with these four items. To assess caregiver stress more comprehensively, tools such as the Parenting Stress Index (Abidin, 1995) can offer clinicians information across multiple domains of caregiver stress (i.e., parental distress, dysfunctional parent-child interaction, and difficult child). Intervention selection should ensure that youth see symptom improvement and that this improvement is associated with decreased impairment in caregiver stress.
While not examined here, the relationship between caregiver stress and children’s behavioral functioning may be bidirectional, in that they influence each other over time. Specifically, Sameroff (2009) argued for a transactional model of child development, such that environmental factors like caregiver characteristics (e.g., caregiver stress) and child characteristics (e.g., ADHD, ODD, and sleep) affect each other. This further underscores the clinical importance of targeting both child behavior and caregiver stress simultaneously in interventions to ultimately lead to improved child and family functioning long-term (Sciberras et al., 2020). In particular, alleviating caregiver stress may decrease the use of ineffective parenting behaviors, which in turn, may lead to greater improvements in behavioral problems (Kochanova et al., 2021).
Regarding child sleep, our findings were somewhat consistent with literature that has demonstrated that females with ADHD have more difficulty sleeping (e.g., Becker et al., 2016). Because restricted sleep in children with ADHD exacerbates existing inattention symptoms and oppositional behaviors (Becker et al., 2019; Gruber et al., 2011; Sung et al., 2008), this indicates that consideration of using sleep interventions for children with ADHD is needed (e.g., Sciberras et al., 2020), and that clinicians providing sleep interventions to females should be aware of potentially greater caregiver stress.
Limitations and Future Directions
Despite the investigation’s strengths (i.e., large nationally representative sample, focus on sex differences, stress measurement approach, differentiation of ADHD and ODD/CD), the findings should be interpreted in light of several limitations. While the present findings indicated that adequate sleep duration did not alter the relation between child ODD/CD and caregiver stress, this may be due to sleep-related factors (e.g., behavioral features of sleep resistance) other than sleep quantity that also contribute to caregiver stress (Aronen et al., 2014; Coto et al., 2018; Smedje et al., 2001). Relatedly, the item used to measure sleep duration in the current study is best regarded as a proxy for sleep duration as measurement did not account for sleep latency, night awakenings, and sleep termination that are also used when considering sleep parameters (e.g., Combs et al., 2019; Lucas-Thompson et al., 2021). As such, future research should consider these aspects of sleep duration in conjunction and how they contribute to caregiver stress. Further, this work examined caregiver-report of average sleep duration which could lead to biased estimation of child sleep compared to self-report, sleep diary, and actigraphy data (e.g., Short et al., 2013). The ability to examine associations at a population level provided substantial statistical power and breadth but traded off precision of clinical measurement (and diagnosis) of ADHD and ODD/CD (i.e., clinician substantiated diagnosis rather than caregiver report) and sleep parameters. Use of multiple reporters, multiple methods, and large clinical samples would reduce single source bias shared method variance. Lastly, findings should be interpreted in the context of the study’s cross-sectional design, which prevented determination of the causal direction of the associations or potential longitudinal influences that may exist.
Conclusion
The present findings highlighted the associations between child ADHD, ODD/CD, sleep duration, and caregiver stress. Overall, sleep duration did not appear to moderate the relation between child ADHD and ODD/CD and caregiver stress. At the population level, the influence of child sleep duration on caregiver stress was small in magnitude, while the influence of child ADHD and ODD/CD were considerable. Sex-specific influences for adequate sleep’s association with lower caregiver stress were generally not observed, except potentially for females with ADHD. Ensuring adequate sleep duration for all children is recommended, and intervention selection should consider strategies that target both youth symptoms and caregiver stress simultaneously.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Mental Health (award number T32MH016434-43), and by the National Institutes of Health/Environmental Influences on Child Health Outcomes (award number 3UG1OD024942-04S1).
Biographies
Author biographies
Tre D. Gissandaner, PhD is a Postdoctoral Fellow in the Division of Child and Adolescent Psychiatry at the New York State Psychiatric Institute and Columbia University Irving Medical Center. He received his doctorate from Texas Tech University and completed a clinical internship at the University of Mississippi Medical Center.
Melanie A. Stearns, PhD is a Postdoctoral Fellow in the College of Nursing at the University of South Florida. She received her doctorate from Mississippi State University and completed a clinical internship at the University of Mississippi Medical Center.
Dustin E. Sarver, PhD is an Associate Professor in the Department of Psychiatry and Human Behavior at the University of Mississippi Medical Center. His interests are in child neurodevelopmental and behavioral disorders and the continuums of care supporting youth.
Benjamin H. Walker, PhD is an Assistant Professor in the Department of Population Health Science at the University of Mississippi Medical Center. He conducts research on social and geographic disparities in health and mortality.
Hannah Ford, PhD is an Associate Professor at the University of Mississippi Medical Center where she also serves as the Training Director for the Psychology Internship Program. Her interests include pediatric chronic pain and sleep. She received her doctorate from the University of Maine. She attended Indiana University School of Medicine for her internship and Children’s Hospital of Pittsburgh of UPMC for her postdoctoral fellowship.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
1. The age range for this study was selected due to inconsistencies with the NSCH instruments administered to caregivers of children 0–5 years and 6–17 years. The data use file included sleep duration variables separately for the two age groups and they were unable to be reconciled due to differences in the response options at the upper and lower extremes of the two versions. Specifically, the instrument used for the 0–5 years group was scaled from 1 (less than 7 hours) to 7 (12 or more hours), whereas the instrument used for the 6–17 years group was scaled from 1 (less than 6 hours) to 7 (11 or more hours). To ensure consistency across all participants, we elected to use only the 6–17 years group and not combine measures where it would be difficult to discriminate hours at the lower and upper extreme options.
References
- Abidin RR (1995). Parenting stress index (4th edn.). Odessa, FL: Psychological Assessment Resource. [Google Scholar]
- Aronen ET, Lampenius T, Fontell T, & Simola P (2014). Sleep in children with disruptive behavioral disorders. Behavioral Sleep Medicine, 12(5), 373–388. 10.1080/15402002.2013.821653 [DOI] [PubMed] [Google Scholar]
- Ball JD, Tiernan M, Janusz J, & Furr A (1997). Sleep patterns among children with attention-deficit hyperactivity disorder: A reexamination of parent perceptions. Journal of Pediatric Psychology, 22(3), 389–398. 10.1093/jpepsy/22.3.389 [DOI] [PubMed] [Google Scholar]
- Becker SP, Epstein JN, Tamm L, Tilford AA, Tischner CM, Isaacson PA, Simon JO, & Beebe DW (2019). Shortened sleep duration causes sleepiness, inattention, and oppositionality in adolescents with attention-deficit/hyperactivity disorder: Findings from a crossover sleep restriction/extension study. Journal of the American Academy of Child and Adolescent Psychiatry, 58(4), 433–442. 10.1016/j.jaac.2018.09.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Pfiffner LJ, Stein MA, Burns GL, & McBurnett K (2016). Sleep habits in children with attention-deficit/hyperactivity disorder predominantly inattentive type and associations with comorbid psychopathology symptoms. Sleep Medicine, 21(2016), 151–159. 10.1016/j.sleep.2015.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belmon LS, van Stralen MM, Busch V, Harmsen IA, & Chinapaw MJ (2019). What are the determinants of children’s sleep behavior? A systematic review of longitudinal studies. Sleep Medicine Reviews, 43(2019), 60–70. 10.1016/j.smrv.2018.09.007 [DOI] [PubMed] [Google Scholar]
- Bode AA, George MW, Weist MD, Stephan SH, Lever N, & Youngstrom EA (2016). The impact of parent empowerment in children’s mental health services on parenting stress. Journal of Child and Family Studies, 25(10), 3044–3055. 10.1007/s10826-016-0462-1 [DOI] [Google Scholar]
- Byars KC, Yeomans-Maldonado G, & Noll JG (2011). Parental functioning and pediatric sleep disturbance: An examination of factors associated with parenting stress in children clinically referred for evaluation of insomnia. Sleep Medicine, 12(9), 898–905. 10.1016/j.sleep.2011.05.002 [DOI] [PubMed] [Google Scholar]
- Combs D, Goodwin JL, Quan SF, Morgan WJ, Hsu CH, Edgin JO, & Parthasarathy S (2019). Mother knows best? Comparing child report and parent report of sleep parameters with polysomnography. Journal of Clinical Sleep Medicine, 15(1), 111–117. 10.5664/jcsm.7582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coto J, Garcia A, Hart KC, & Graziano PA (2018). The associations between disruptive behavior problems, parenting factors, and sleep problems among young children. Journal of Developmental and Behavioral Pediatrics: JDBP, 39(8), 610–620. 10.1097/dbp.0000000000000595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cremone-Caira A, Root H, Harvey EA, McDermott JM, & Spencer RM (2020). Effects of sleep extension on inhibitory control in children with ADHD: A pilot study. Journal of Attention Disorders, 24(4), 601–610. 10.1177/1087054719851575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deault LC (2010). A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD). Child Psychiatry and Human Development, 41(2), 168–192. 10.1007/s10578-009-0159-4 [DOI] [PubMed] [Google Scholar]
- DiStefano C, Zhu M, & Mindrila D (2009). Understanding and using factor scores: Considerations for the applied researcher. Practical Assessment, Research, and Evaluation, 14(20), 1–11. [Google Scholar]
- Evans S, Sciberras E, & Mulraney M (2020). The relationship between maternal stress and boys’ ADHD symptoms and quality of life: An Australian prospective cohort study. Journal of Pediatric Nursing, 50(2020), e33–e38. 10.1016/j.pedn.2019.09.029 [DOI] [PubMed] [Google Scholar]
- Galland BC, Tripp EG, & Taylor BJ (2010). The sleep of children with attention deficit hyperactivity disorder on and off methylphenidate: A matched case–control study. Journal of Sleep Research, 19(2), 366–373. 10.1111/j.1365-2869.2009.00795.x [DOI] [PubMed] [Google Scholar]
- Ghandour RM, Jones JR, Lebrun-Harris LA, Minnaert J, Blumberg SJ, Fields J, Bethell C, & Kogan MD (2018). The design and implementation of the 2016 national survey of children’s health. Maternal and Child Health Journal, 22(8), 1093–1102. 10.1007/s10995-018-2526-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanizadeh A, Mohammadi MR, & Moini R (2008). Comorbidity of psychiatric disorders and parental psychiatric disorders in a sample of Iranian children with ADHD. Journal of Attention Disorders, 12(2), 149–155. 10.1177/1087054708314601 [DOI] [PubMed] [Google Scholar]
- Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R, & Carrier J (2011). Impact of sleep restriction on neurobehavioral functioning of children with attention deficit hyperactivity disorder. Sleep, 34(3), 315–323. 10.1093/sleep/34.3.315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honaker SM, & Meltzer LJ (2016). Sleep in pediatric primary care: A review of the literature. Sleep Medicine Reviews, 25, 31–39. 10.1016/j.smrv.2015.01.004 [DOI] [PubMed] [Google Scholar]
- Hvolby A, Christensen J, Gasse C, Dalsgaard S, & Dreier JW (2021). Cumulative incidence and relative risk of sleep problems among children and adolescents with newly diagnosed neurodevelopmental disorders: A nationwide register-based study. Journal of Sleep Research, 30(3), e13122. 10.1111/jsr.13122 [DOI] [PubMed] [Google Scholar]
- Hvolby A, Jørgensen J, & Bilenberg N (2009). Parental rating of sleep in children with ADHD. European Child & Adolescent Psychiatry, 18(7), 429–438. 10.1007/s00787-009-0750-z [DOI] [PubMed] [Google Scholar]
- Kirov R, & Brand S (2014). Sleep problems and their effect in ADHD. Expert Review of Neurotherapeutics, 14(3), 287–299. 10.1586/14737175.2014.885382 [DOI] [PubMed] [Google Scholar]
- Kochanova K, Pittman LD, & Pabis JM (2021). Parenting stress, parenting, and adolescent externalizing problems. Journal of Child and Family Studies, 30(9), 2141–2154. 10.1007/s10826-021-01996-2 [DOI] [Google Scholar]
- Leadbeater BJ, & Homel J (2015). Irritable and defiant sub-dimensions of ODD: Their stability and prediction of internalizing symptoms and conduct problems from adolescence to young adulthood. Journal of Abnormal Child Psychology, 43(3), 407–421. 10.1007/s10802-014-9908-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitch S, Sciberras E, Post B, Gerner B, Rinehart N, Nicholson JM, & Evans S (2019). Experience of stress in parents of children with ADHD: A qualitative study. International Journal of Qualitative Studies on Health and Well-Being, 14(1), 1690091. 10.1080/17482631.2019.1690091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Lin X, Heath MA, Zhou Q, Ding W, & Qin S (2018). Longitudinal linkages between parenting stress and oppositional defiant disorder (ODD) symptoms among Chinese children with ODD. Journal of Family Psychology, 32(8), 1078–1086. 10.1037/fam0000466 [DOI] [PubMed] [Google Scholar]
- Ljungström BM, Kenne Sarenmalm E, & Axberg U (2020). “Since his birth, I’ve always been old” the experience of being parents to children displaying disruptive behavior problems: A qualitative study. BMC Psychology, 8, 1–14. 10.1186/s40359-020-00465-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas-Thompson RG, Crain TL, & Brossoit RM (2021). Measuring sleep duration in adolescence: Comparing subjective and objective daily methods. Sleep Health, 7(1), 79–82. 10.1016/j.sleh.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lycett K, Sciberras E, Mensah FK, & Hiscock H (2015). Behavioral sleep problems and internalizing and externalizing comorbidities in children with attention deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 24(1), 31–40. 10.1007/s00787-014-0530-2 [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Johnson C, Crosette J, Ramos M, & Mindell JA (2010). Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics, 125(6), e1410–e1418. 10.1542/peds.2009-2725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miano S (2012). The complex relationship between ADHD and pediatric sleep disorders. The ADHD Report, 20(6), 1–6. 10.1521/adhd.2012.20.6.1 [DOI] [Google Scholar]
- Mofokeng M, & van der Wath AE (2017). Challenges experienced by parents living with a child with ADHD. Journal of Child & Adolescent Mental Health, 29(2), 137–145. 10.2989/17280583.2017.1364253 [DOI] [PubMed] [Google Scholar]
- Moreau V, Rouleau N, & Morin CM (2014). Sleep of children with ADHD: Actigraphic and parental reports. Behavioral Sleep Medicine, 12(1), 69–83. 10.1080/15402002.2013.764526 [DOI] [PubMed] [Google Scholar]
- Noble GS, O’Laughlin L, & Brubaker B (2012). Attention deficit hyperactivity disorder and sleep disturbances: Consideration of parental influence. Behavioral Sleep Medicine, 10(1), 41–53. 10.1080/15402002.2012.636274 [DOI] [PubMed] [Google Scholar]
- Robison RJ, Reimherr FW, Marchant BK, Faraone SV, Adler LA, & West SA (2008). Gender differences in 2 clinical trials of adults with attention-deficit/hyperactivity disorder: A retrospective data analysis. The Journal of Clinical Psychiatry, 69(2), 7640–8221. 10.4088/jcp.v69n0207 [DOI] [PubMed] [Google Scholar]
- Rollè L, Prino LE, Sechi C, Vismara L, Neri E, Polizzi C, Trovato A, Volpi B, Molgora S, Fenaroli V, Ierardi E, Ferro V, Lucarelli L, Agostini F, Tambelli R, Saita E, Riva Crugnola C, & Brustia P (2017). Parenting stress, mental health, dyadic adjustment: A structural equation model. Frontiers in Psychology, 8(2017), 839. 10.3389/fpsyg.2017.00839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucklidge JJ (2010). Gender differences in ADHD. Psychiatric Clinics, 33(2), 357–373. 10.1016/j.psc.2010.01.006 [DOI] [PubMed] [Google Scholar]
- Sameroff A (2009). The transactional model. In Sameroff A (Ed), The transactional model of development: How children and contexts shape each other (pp. 3–21). American Psychological Association. [Google Scholar]
- Sciberras E, Mulraney M, Mensah F, Oberklaid F, Efron D, & Hiscock H (2020). Sustained impact of a sleep intervention and moderators of treatment outcome for children with ADHD: A randomised controlled trial. Psychological Medicine, 50(2), 10–219. 10.1017/s0033291718004063 [DOI] [PubMed] [Google Scholar]
- Scott N, Blair PS, Emond AM, Fleming PJ, Humphreys JS, Henderson J, & Gringras P (2013). Sleep patterns in children with ADHD: A population-based cohort study from birth to 11 years. Journal of Sleep Research, 22(2), 121–128. 10.1111/j.1365-2869.2012.01054.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Lack LC, Wright HR, & Chatburn A (2013). Estimating adolescent sleep patterns: Parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nature and Science of Sleep, 5(2013), 23–26. 10.2147/nss.s38369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedje H, Broman JE, & Hetta J (2001). Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: A study based on parents’ perceptions. European Child & Adolescent Psychiatry, 10(1), 1–9. 10.1007/s007870170041 [DOI] [PubMed] [Google Scholar]
- Sung V, Hiscock H, Sciberras E, & Efron D (2008). Sleep problems in children with attention-deficit/hyperactivity disorder: Prevalence and the effect on the child and family. Archives of Pediatrics & Adolescent Medicine, 162(4), 336–342. 10.1001/archpedi.162.4.336 [DOI] [PubMed] [Google Scholar]
- Tan TX, Wang Y, & Ruggerio AD (2017). Childhood adversity and children’s academic functioning: Roles of parenting stress and neighborhood support. Journal of Child and Family Studies, 26(10), 2742–2752. 10.1007/s10826-017-0775-8 [DOI] [Google Scholar]
- Theule J, Wiener J, Tannock R, & Jenkins JM (2013). Parenting stress in families of children with ADHD: A meta-analysis. Journal Emotional & Behavioral Disorders, 21(1), 3–17. 10.1177/1063426610387433 [DOI] [Google Scholar]
- Ward KP, & Lee SJ (2020). Mothers’ and fathers’ parenting stress, responsiveness, and child wellbeing among low-income families. Children and Youth Services Review, 116(2020), 105218. 10.1016/j.childyouth.2020.105218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss MD, & Salpekar J (2010). Sleep problems in the child with attention-deficit hyperactivity disorder. CNS Drugs, 24(10), 811–828. 10.2165/11538990-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Wheaton AG, & Claussen AH (2021). Short sleep duration among infants, children, and adolescents aged 4 months–17 years—United States, 2016–2018. MMWR. Morbidity and Mortality Weekly Report, 70(38), 1315–1321. 10.15585/mmwr.mm7038a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG (2012). The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics: the Journal of the American Society for Experimental Neurotherapeutics, 9(3), 490–499. 10.1007/s13311-012-0135-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams NA, & Burnfield JM (2019). Psychological difficulties and parental well-being in children with musculoskeletal problems in the 2011/2012 National Survey of Children’s Health. Rehabilitation Psychology, 64(1), 87–97. 10.1037/rep0000251 [DOI] [PubMed] [Google Scholar]