The COVID-19 pandemic has had profound implications across the breadth of national healthcare services. Inflammatory bowel disease (IBD) continues to carry an increased risk of colon cancer and national protocols for endoscopic surveillance are in place. Elective procedures such as IBD surveillance were stopped during the COVID-19 pandemic and have been slow to be re-started. We are acutely aware of the pressures on endoscopy services at the present time which is unlikely to improve at the pace needed for services to fully recover. At such times, we need to target this scarce resource to those who need it most, aligned to the principles of ethical healthcare which state that when resources are limited, they should be used to provide the most benefit for as great a number of people as possible. With this in mind, we propose an optional interim framework to aid risk stratification of patients on the IBD surveillance waiting lists where delays to timely surveillance occur. These measures could help address the backlog until a time when clinical services are able to fully recover. Finally, we propose the patient factors to consider when withdrawal of surveillance may be contemplated.
Key points
There is significant variation in the degree of endoscopy surveillance backlog across the UK.
For centres without a significant backlog, no major change to clinical practice is likely to be needed.
For centres with a significant backlog, we recommend employing a framework to aid risk stratification of patients on the IBD surveillance waiting list.
Those patients at highest risk should continue to be offered urgent surveillance colonoscopy at the earliest opportunity.
We propose an interim framework where patients at medium to low risk can be further triaged using, quantitative Faecal Immunochemical Test for haemoglobin (qFIT) and faecal calprotectin, stool tests used routinely in clinical practice.
Patients with a high qFIT (≥10 µg/g) and low calprotectin (<250 µg/g) should be treated as high risk for cancer and may therefore reflect those in greatest need of surveillance.
We also consider how the demand for surveillance procedures could be addressed by postponing and/or withdrawing patients from surveillance programmes if the overall risk of future dysplasia/cancer is low and unlikely to occur in the patient’s expected lifespan.
IBD dysplasia surveillance
IBD confers an increased risk of inflammation-associated colorectal cancer (CRC), herein termed IBD-CRC. The prevalence of IBD in the Western world, and therefore the population in need of surveillance, is increasing due to static incidence and low mortality.1 However, across the UK only 63% of all endoscopy surveillance procedure targets were met prior to the pandemic in 2019.2 Despite surveillance, it is estimated that 28–41% of IBD-CRCs present as interval cancers3 (post-colonoscopy cancers) between surveillance procedures. In the current post-pandemic environment, urgent strategies are required to identify those patients most likely to benefit from surveillance, while mitigating potential harm to those patients on wating lists.
The impact of the COVID-19 pandemic on IBD surveillance
In March 2020, the British Society of Gastroenterology (BSG) and the Joint Advisory Group advised a 6-week pause in non-emergency endoscopy in the wake of the COVID-19 pandemic.4 During this time, overall endoscopy activity reduced to 5% of pre-pandemic levels and has slowly recovered to near pre-pandemic levels,5 with a backlog of procedures awaiting to be scheduled. Data from the pandemic are emerging, with evidence of a significant reduction in 2-week wait referrals and CRC diagnoses. In Scotland, there was a 19% reduction in CRC diagnoses in 2020 compared with 20196; reflecting a reduction in clinical activity and not a true decrease in cancer rate. The Gastroenterology ‘Getting it Right First Time’ (GIRFT) national report has highlighted that Endoscopy units are continuing to perform at reduced capacity due to ongoing COVID-19 pandemic constraints and English Trusts have reported significant concerns in managing the substantial backlog in surveillance procedures.7 As of 31 December 2021, there were 34 224 patients waiting for an endoscopy in Scotland (including colonoscopy), a 53.1% increase compared with the 12-month average prior to the onset of the pandemic.8 In England in March 2022 there were 159 672 patients on the endoscopy waiting list, with 66 512 waiting for a colonoscopy.9
While the backlog of procedures overall is significant, surveillance procedures have been slower still to recover.10 Additional BSG advice was issued in April 2021 regarding surveillance colonoscopy (including for IBD) in the wake of these challenges, suggesting surveillance procedures should be carried out within 6–12 months of their due date.11 It is concerning that most patients will have already surpassed this timepoint, and thus additional measures are needed to help prioritise those awaiting surveillance procedures.
Alternative strategies, such as the qFIT and virtual colonoscopy (either via CT or capsule), have not been used in IBD surveillance. qFIT, which measures the concentration of degraded haemoglobin and is raised in ulcerative colitis (UC) patients with active inflammation,12 13 has not been validated as a marker of IBD-related dysplasia. Virtual colonoscopy via CT or capsule imaging may not be sufficiently sensitive to detect flat dysplastic lesions associated IBD-CRC. While there is a lack of data on the rate of post-colonoscopy colorectal cancer (PCCRC) in the wake of the COVID-19 pandemic, the high rate of pre-pandemic PCCRC, together with the backlog of procedures, raises concerns that this rate could increase further as the time interval between surveillance extends. Such concerns have also been reported in the media.14
Possible strategies to tackle current challenges in IBD surveillance colonoscopy for centres with a significant backlog in procedures
For some centres without a backlog in surveillance procedures, no change may be required. For centres with a significant backlog and under unprecedented pressure, we first propose that colonoscopy waiting lists be reviewed and stratified, such that patients with IBD are identified (through International Classification of Diseases 10 codes, faecal calprotectin, mesalazine prescription, for example1 or using the IBD Registry,15 if available), and triaged according to the existing surveillance framework.16 While we have not set a specific lower age limit for this framework, we do not anticipate it applying to most paediatric IBD centres.
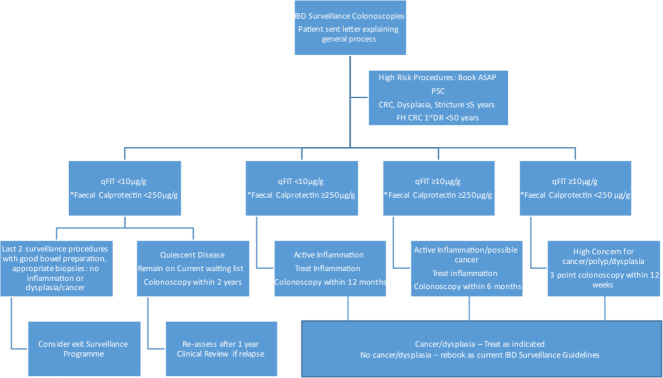
Identifying these patients on undifferentiated waiting lists can be challenging. We recognise that this level of waiting list validation will require additional resources. Acknowledging the significant numbers of patients who are likely to be overdue surveillance, we propose that clinical risk stratification should be used to prioritise those at highest risk of dysplasia. Those due annual colonoscopy, including those with extensive moderately to severely active colitis or primary sclerosing cholangitis,17 previous IBD-related dysplasia or cancer or colonic stricture or with a first degree relative with CRC diagnosed at <50 years are highest risk and should be scheduled immediately.16 Those not due annual colonoscopy are deemed moderate or low risk and may be further triaged using the proposals described in figure 1.
Figure 1.
Proposed algorithm for the management of patients currently on moderate to low risk IBD surveillance waiting list where significant delays to surveillance are experienced. A faecal calprotectin threshold of >250 µg/g to indicate disease activity is based on consensus and published evidence.31–33 A three-point colonoscopy indicates a 45-minute procedure. 1st DR, first degree relative; CRC, colorectal cancer;FH, family history; IBD, inflammatory bowel disease; PSC, primary sclerosing cholangitis; qFIT, quantitative Faecal Immunochemical Test for haemoglobin
The Gastroenterology GIRFT report has recommended the use of stool biomarkers to aid in the prioritisation of colonoscopy procedures on waiting lists. Faecal calprotectin is widely used in patients with IBD. qFIT has been shown to preform equally18 or superiorly19 than faecal calprotectin in identifying mucosal healing in UC. Using qFIT in this way is an untested strategyalthough similar COVID-19 adapted colorectal cancer pathways have been used for symptomatic patients using qFIT.20 Extrapolated from the work in symptomatic colorectal patients, a qFIT cut-off of 10 µg/g could be used to aid prioritisation.21 Patients who have a qFIT of ≥10 µg/g could be prioritised for more urgent procedures with further prioritisation if the level is ≥400 µg/g.22 qFIT in combination with faecal calprotectin may be a promising risk stratification tool and the combination of qFIT and calprotectin in one study has been shown to have a higher specificity for histological healing than when using qFIT alone.18 Therefore, stratifying patients by both qFIT and faecal calprotectin could provide an indication as to those in most urgent need of surveillance colonoscopy. In figure 1, we present a model of how this could be undertaken depending on the potential outcomes for both tests in tandem. For example, a patient who has a faecal calprotectin level suggestive of remission (<250 µg/g) and a qFIT ≥10 µg/g may have serious non-inflammatory pathology and could be prioritised in the waiting list. Alternatively, a patient with a negative qFIT <10 µg/g and low calprotectin are at a lower risk and could remain on the current waiting list without prioritisation. In the latter scenario, the negative predictive value of a qFIT is exploited while accepting the predicted poor sensitivity and specificity of a positive test in those with active IBD. We have proposed a calprotectin cut-off of 250 µg/g as this is commonly used in clinical practice, but an alternative of <150 µg/g has been proposed as a more stringent end point for mucosal healing.23
Patients with a high faecal calprotectin are also likely to have a high qFIT suggesting active IBD and therefore optimising IBD treatment before conducting a surveillance procedure would be a reasonable approach, given the challenges of surveying an inflamed colon and the association with PCCRC rate.24 Importantly, capturing the patients who are stratified using these proposals in a database with prospective data collection linked with colonoscopy outcomes will inform the risk stratification and future guidelines.
When can cessation of surveillance be safely considered?
In addition to targeting endoscopic surveillance to those most at risk and using a combination of biomarkers and risk factors to identify these patients, we should also be reviewing the appropriateness of ongoing surveillance. Although prompted by the situation we currently face, this aligns with the principle of sustainable healthcare, in reducing unnecessary procedures. We recognise the effects on healthcare usage and expenditure but also highlight the potential reduction in need for invasive procedures often disliked by patients and carrying small procedure-related risks.25 The current cessation advice is that surveillance should cease when the ‘risks of the procedure and its associated implications outweigh the benefits’.26 In practice, identifying individuals who will benefit from cessation of surveillance is less likely to have an age-specific cut-off, and more likely to involve both patient engagement and clinical features.27 The aim of surveillance for IBD-CRC is to prevent premature death from CRC and we therefore need to consider the likelihood of IBD-CRC occurring during the patient’s expected remaining life span. Two retrospective studies have suggested that a lack of histological inflammation in two consecutive procedures predict a low risk of future CRC.28 29 This approach could be considered for patients who are currently in the 5-year follow-up category based on the BSG guidance, freeing up capacity for higher-risk patients.
Cessation of surveillance considerations should ideally be formally addressed by a future BSGGrading of Recommendations, Assessment, Development and Evaluations (GRADE) compliant guideline process. Until that time, in the post-pandemic setting, cessation of IBD surveillance could be considered at the age of 75 years after a good quality normal procedure, as the expected natural lifespan30 would be fewer years than the time taken to develop dysplasia and CRC. Second, stopping surveillance after two good quality consecutive normal procedures, (and at the time of quiescent disease), where no dysplasia or cancer is detected, could also be considered. Patients in whom surveillance is suspended should remain under regular review and be offered regular qFIT and faecal calprotectin tests to mitigate a future delayed diagnosis of CRC. Importantly, surveillance could be restarted if a patient develops a future flare. Additionally, patients in whom surveillance is suspended using this interim framework should be captured in a database and their ongoing surveillance need reviewed once GRADE-compliant consensus guidance on IBD surveillance cessation is available. This temporary post-pandemic approach would help to ensure that patients who are in greatest need of surveillance are appointed first.
Patient engagement
Feedback on the proposed changes were captured by a focus group invitation through social media publicised by the UK patient charity Crohn’s & Colitis UK. Eight participants (6F:2M) living with IBD (4 Crohn's Disease:4 UC) for more than 5 years in the age groups 25 to over 65 years, responded to the invitation of whom six had experience of regular surveillance procedures.
There was a unanimous positive response to developing a strategy addressing the COVID-19-related backlog in surveillance procedures. A non-invasive approach to guide surveillance colonoscopy timing was welcomed, including prioritising those at higher risk. Many patients are familiar with stool tests and therefore this seemed a reasonable approach. A single stool sample is often a ‘snapshot’ of disease at time and participants were reassured that disease flares will be pro-actively managed as in figure 1. The participants reported that colonoscopy can be an uncomfortable procedure and therefore an approach which could tailor procedures safely without compromising care would be greatly received (further detailed responses from seven of the eight participants can be found in online supplemental appendix 1).
gutjnl-2022-328309supp001.pdf (62.7KB, pdf)
Conclusion
There are significant ongoing barriers to cancer surveillance in patients with IBD as a consequence of the COVID-19 pandemic. There is no perfect solution to the growing pressures endoscopy units face. Leaving patients with IBD on long overdue surveillance waiting lists in a permanent ‘holding’ pattern, or conversely, putting people at very low risk through invasive procedures for little benefit, is equally not acceptable. There is an urgent requirement to survey those patients at highest risk. We propose an interim mitigation strategy, pending formal GRADE-compliant consensus guidance, for those not at highest risk using a combination of qFIT and faecal calprotectin prioritising those in need of endoscopic assessment now. Clinical units adopting this approach are encouraged to prospectively collect data, as rigorous data collection, analysis and safety netting will be crucial in determining the impact of the interim proposals. Regular review of waiting lists, effective triage and resources assigned appropriately to facilitate this are also important steps to ensure an effective safe service in the post-pandemic phase.
Acknowledgments
We are grateful to the patients living with IBD who provided feedback guiding the final proposals.
Footnotes
Twitter: @amd_churchhouse, @victoria_moffat, @ChristianSelin3, @DrChrisLamb, @GastronauIan, @ShahidaDin1
Collaborators: Scottish IBD Surveillance Group: Mark Arends, Ian Arnott, Gillian Bain, Zahra Bayaty, Nick Church, Antonia Churchhouse, Shahida Din, James Duncan, Jonathan Fletcher, Dan Gaya, Hasnain Jafferbhoy, Gareth-Rhys Jones, Kathryn Kirkwood, Selina Lamont, Mairi McLean, Michael Miller, Victoria Moffat, Craig Mowat, Graham Naismith, Colin Noble, Ian Penman, Elaine Robertson, Richard Russell, Santosh Salunke, John Paul Seenan, Malcolm Smith, Ali Taha, Michelle Thornton, Jack Winter. BSG Committee Representation: Rachel Ainley, Ibrahim Al-Bakir, Antonia Churchhouse, Rachel Cooney, Shahida Din, Melissa Ganendran, Morris Gordon, Ailsa Hart, Chris Lamb, Noor Mohammed, Gordon Moran, Ian Penman, Christian Selinger, Ruth Wakeman.
Contributors: SD and MT instigated and conceptualised the proposal. Members of the BSG & Scottish IBD Surveillance Group provided ongoing critical appraisal of the proposal. AC, VM and SD wrote the manuscript. CL, CS and IP provided critical sub-committee input and advice. All authors reviewed the manuscript and approved the final version. AC and VM contributed equally to this work and should be considered joint first authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: AC reports grants from the Wellcome Trust and royalties from Elsevier all outside the submitted work. VM reports personal speaker fees from Takeda UK, and meeting and travel grants from Dr Falk Pharma (UK), Janssen-Cilag, Takeda UK, all outside the submitted work. CS reports consulting fees from Ferring, personal speaker fees from Takeda, Janssen, Abbvie, Tillotts, Norgine, Fresenius Kabi, meeting and travel grants from Tillots, Abbvie, Janssen, and advisory board fees from Galapagos, AbbVie, Arena, Janssen, Fresenius Kabi all outside the submitted work. CL reports grants from Genentech, grants and personal fees from Janssen, grants and personal fees from Takeda, grants from AbbVie, personal fees from Ferring, grants from Eli Lilly, grants from Pfizer, grants from Roche, grants from UCB Biopharma, grants from Sanofi Aventis, grants from Biogen IDEC, grants from Orion OYJ, personal fees from Dr Falk Pharma, grants from AstraZeneca, outside the submitted work. IP reports speaker fees from Olympus, Boston Scientific, and Dr Falk outside the submitted work. SD reports grants from The Helmsley Charitable Trust, Edinburgh and Lothians Health Foundation, Pathological Society of Great Britain and Northern Ireland, Lord Leonard and Lady Estelle Wolfson Foundation, consulting fees from Abbvie, personal speaker fees from Janssen and Takeda, and meeting and travel grants from Janssen, Takeda and Dr Falk, all outside the submitted work.
Provenance and peer review: Not commissioned; internally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
the BSG, Scottish IBD Surveillance Group:
Antonia Churchhouse, Victoria MoffatIan Penman, Shahida DinMichelle Thornton, Cathy Dunn, Malcolm Smith, Gillian Bain, Mairi McLean, Craig Mowat, Michael Miller, Hasnain Jafferbhoy, Colin Noble, Nick Church, Ian Arnott, Gareth-Rhys Jones, Jonathan Fletcher, Zahra Bayaty, Elaine Robertson, Selina Lamont, Ali Taha, Graham Naismith, John Paul Seenan, Dan Gaya, Jack Winter, Santosh Salunke, James Duncan, Richard Russell, Mark Arends Kathryn Kirk Wood, Antonia ChurchhouseIan Penman, Shahida Din, Christian Selinger, Chris Lamb, Rachel Cooney, Noor Mohammed, Gordon Moran, Morris Gordon, Ailsa HartIbrahim Al-Bakir, Ruth Wakeman, Melissa Ganendran, and Rachel Ainley
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. Jones G-R, Lyons M, Plevris N, et al. Ibd prevalence in Lothian, Scotland, derived by capture-recapture methodology. Gut 2019;68:1953–60. 10.1136/gutjnl-2019-318936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ravindran S, Bassett P, Shaw T. National census of UK endoscopy services in 20190:flgastro-2020-101538. Frontline Gastroenterol 2021;12:451–60. 10.1136/flgastro-2020-101538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stjärngrim J, Ekbom A, Hammar U, et al. Rates and characteristics of postcolonoscopy colorectal cancer in the Swedish IBD population: what are the differences from a non-IBD population? Gut 2019;68:1588–96. 10.1136/gutjnl-2018-316651 [DOI] [PubMed] [Google Scholar]
- 4. The British Society of Gastroenterology . Bsg rationale around current advice to all endoscopy units | the British Society of gastroenterology, 2020. Available: https://www.bsg.org.uk/covid-19-advice/bsg-rationale-around-current-advice-to-all-endoscopy-units/ [Accessed 19 May 2021].
- 5. Rutter MD, Brookes M, Lee TJ, et al. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a national endoscopy database analysis. Gut 2021;70:537–43. 10.1136/gutjnl-2020-322179 [DOI] [PubMed] [Google Scholar]
- 6. Information Services Division Scotland . Cancer incidence in Scotland. published online, 2022. Available: www.publichealthscotland.scot [Accessed 17 May 2022].
- 7. Oates B. Gastroenterology GIRFT programme national specialty report, 2021. Available: https://www.bsg.org.uk/wp-content/uploads/2021/10/Gastroenterology-Oct21v.pdf [Accessed 2 December 2021].
- 8. Information Services Division Scotland . Diagnostic waiting times a national statistics release for Scotland. published online, 2022. Available: www.publichealthscotland.scot [Accessed 17 May 2022].
- 9. Nhs diagnostic waiting times and activity data March 2022 monthly report.
- 10. Ho KMA, Banerjee A, Lawler M, et al. Predicting endoscopic activity recovery in England after COVID-19: a national analysis. Lancet Gastroenterol Hepatol 2021;6:381–90. 10.1016/S2468-1253(21)00058-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. The British Society of Gastroenterology . An update to information and guidance for endoscopy services in the COVID-19 pandemic. Available: https://www.bsg.org.uk/covid-19-advice/an-update-to-information-and-guidance-for-endoscopy-services-in-the-covid-19-pandemic-2/ [Accessed 19 May 2021].
- 12. Nakarai A, Kato J, Hiraoka S, et al. Evaluation of mucosal healing of ulcerative colitis by a quantitative fecal immunochemical test. Am J Gastroenterol 2013;108:83–9. 10.1038/ajg.2012.315 [DOI] [PubMed] [Google Scholar]
- 13. Din S, Gaya DR, Arnott IDR. COVID-19: colorectal cancer endoscopic surveillance in IBD. Lancet Gastroenterol Hepatol 2021;6:526. 10.1016/S2468-1253(21)00168-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. The Sunday Times . Long delays for surgery ‘will trigger public health crisis’ | News. Available: https://www.thetimes.co.uk/article/long-delays-for-surgery-will-trigger-public-health-crisis-mdphkqhkd [Accessed 30 June 2022].
- 15. Home - UK IBD Registry. Available: https://ibdregistry.org.uk/ [Accessed 19 July 2022].
- 16. Lamb CA, Kennedy NA, Raine T, et al. British Society of gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019;68:s1–106. 10.1136/gutjnl-2019-318484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cairns SR, Scholefield JH, Steele RJ. Guidelines for Colorectal Cancer Screening and Surveillance in Moderate and High Risk Groups (Update from 2002). Vol 59. BMJ Publishing Group 2010:666–89. [DOI] [PubMed] [Google Scholar]
- 18. Shi HY, Chan FKL, Chan AWH, et al. Accuracy of faecal immunochemical test to predict endoscopic and histological healing in ulcerative colitis: a prospective study based on validated histological scores. J Crohns Colitis 2017;11:1071–7. 10.1093/ecco-jcc/jjx088 [DOI] [PubMed] [Google Scholar]
- 19. Hiraoka S, Inokuchi T, Nakarai A, et al. Fecal immunochemical test and fecal calprotectin results show different profiles in disease monitoring for ulcerative colitis. Gut Liver 2018;12:142–8. 10.5009/gnl17013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miller J, Thomson LJ, Stewart LSP, et al. Implementation of a risk mitigating COVID-adapted colorectal cancer pathway. BMJ Open Qual 2021;10:e001135. 10.1136/bmjoq-2020-001135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Monahan KJ, Davies MM, Abulafi M, et al. Faecal Immunochemical testing (FIT) in patients with signs or symptoms of suspected colorectal cancer (CRC): a joint guideline from the Association of Coloproctology of great Britain and Ireland (ACPGBI) and the British society of Gastroenterology (BSG). Gut 2022;71:1939–62. 10.1136/gutjnl-2022-327985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McSorley ST, Digby J, Clyde D, et al. Yield of colorectal cancer at colonoscopy according to faecal haemoglobin concentration in symptomatic patients referred from primary care. Colorectal Dis 2021;23:1615–21. 10.1111/codi.15405 [DOI] [PubMed] [Google Scholar]
- 23. Bromke MA, Neubauer K, Kempiński R, et al. Faecal calprotectin in assessment of mucosal healing in adults with inflammatory bowel disease: a meta-analysis. J Clin Med 2021;10:2203. 10.3390/jcm10102203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wintjens DSJ, Bogie RMM, van den Heuvel TRA, et al. Incidence and classification of postcolonoscopy colorectal cancers in inflammatory bowel disease: a Dutch population-based cohort study. J Crohns Colitis 2018;12:777–83. 10.1093/ecco-jcc/jjy044 [DOI] [PubMed] [Google Scholar]
- 25. Tomaszewski M, Sanders D, Enns R, et al. Risks associated with colonoscopy in a population-based colon screening program: an observational cohort study. Cmajo 2021;9:E940–7. 10.9778/cmajo.20200192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Colorectal Cancer Prevention: Colonoscopic Surveillance in Adults with Ulcerative Colitis, Crohn’s Disease or Adenomas Clinical Guideline, 2011. Available: www.nice.org.uk/guidance/cg118 [Accessed 28 May 2021]. [PubMed]
- 27. Abdalla M, Herfarth H. Rethinking colorectal cancer screening in IBD, is it time to revisit the guidelines? J Crohns Colitis 2018;12:757–9. 10.1093/ecco-jcc/jjy073 [DOI] [PubMed] [Google Scholar]
- 28. Choi C-HR, Al Bakir I, Ding N-SJ, et al. Cumulative burden of inflammation predicts colorectal neoplasia risk in ulcerative colitis: a large single-centre study. Gut 2019;68:414–22. 10.1136/gutjnl-2017-314190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ten Hove JR, Shah SC, Shaffer SR, et al. Consecutive negative findings on colonoscopy during surveillance predict a low risk of advanced neoplasia in patients with inflammatory bowel disease with long-standing colitis: results of a 15-year multicentre, multinational cohort study. Gut 2019;68:615–22. 10.1136/gutjnl-2017-315440 [DOI] [PubMed] [Google Scholar]
- 30. scotpho.org.uk . Available: https://www.scotpho.org.uk/population-dynamics/healthy-life-expectancy/data/scotland/ [Accessed 2 December 2021].
- 31. Malvão LDR, Madi K, Esberard BC, et al. Fecal calprotectin as a noninvasive test to predict deep remission in patients with ulcerative colitis. Medicine 2021;100:e24058. 10.1097/MD.0000000000024058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen F, Hu Y, Fan Y-H, et al. Clinical value of fecal calprotectin in predicting mucosal healing in patients with ulcerative colitis. Front Med 2021;8:988. 10.3389/fmed.2021.679264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Penna FGC E, Rosa RM, Da Cunha PFS, et al. Faecal calprotectin is the biomarker that best distinguishes remission from different degrees of endoscopic activity in Crohn’s disease. BMC Gastroenterol 2020;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2022-328309supp001.pdf (62.7KB, pdf)