Abstract
Introduction/background
As a proxy for adiposity, body mass index (BMI) provides a practical public health metric to counter obesity-related disease trends. On an individual basis, BMI cannot distinguish fat and lean components of body composition. Further, the relationship between BMI and body composition may be altered in response to physical training. We investigated this dynamic relationship by examining the effect of US Army basic combat training (BCT) on the association between BMI and per cent body fat (%BF).
Methods
BMI and %BF were measured at the beginning (week 1) and end (week 9) of BCT in female (n=504) and male (n=965) trainees. Height and weight were obtained for BMI, and body composition was obtained by dual X-ray absorptiometry. Sensitivity and specificity of BMI-based classification were determined at two BMI thresholds (25 kg/m2 and 27.5 kg/m2).
Results
A progressive age-related increase in fat-free mass index (FFMI) was observed, with an inflection point at age 21 years. In soldiers aged 21+, BMI of 25.0 kg/m2 predicted 33% and 29% BF in women and 23% and 20% BF in men and BMI of 27.5 kg/m2 predicted 35% and 31% BF in women and 26% and 22% BF in men, at the start and end of BCT, respectively. Sensitivity and specificity of BMI-based classification of %BF were poor. Soldiers below BMI of 20 kg/m2 had normal instead of markedly reduced %BF, reflecting especially low FFMI.
Conclusions
BCT alters the BMI–%BF relationship, with lower %BF at a given BMI by the end of BCT compared with the beginning, highlighting the unreliability of BMI to try to estimate body composition. The specific BMI threshold of 25.0 kg/m2, defined as ‘overweight’, is an out-of-date metric for health and performance outcomes. To the extent that %BF reflects physical readiness, these data provide evidence of a fit and capable military force at BMI greater than 25.0 kg/m2.
Keywords: public health, preventive medicine, occupational & industrial medicine, diabetes & endocrinology, health policy
Key messages.
Body mass index (BMI) is commonly used to classify obesity but cannot distinguish fat and lean components of body composition.
The threshold of clinical overweight (BMI 25.0 kg/m2) has low precision in classifying high body fat in healthy young women (>30% body fat) and men (>20% body fat).
US Army basic combat training alters the relationship between BMI and relative body fat (per cent body fat, %BF), with lower %BF at a given BMI at the end of training.
Young age (<21 years) further affects the relationship between BMI and %BF due to lower fat-free mass index compared with older women and men.
Low BMI (<20 kg/m2) was associated with relative body fat of normal fit women and men, reflecting markedly reduced fat-free mass and fat-free mass indices.
Application of BMI to infer %BF may have continuing utility in health risk assessment, especially combined with other clinically available data and waist circumference, but requires a careful re-examination in its use to assess soldier physical readiness.
Introduction
In the US and UK armies, height and weight are usually the primary data available to estimate obesity prevalence, and these data have often been extrapolated to interpretations about fitness of the force. In both armies, height/weight tables are combined with an assessment of waist circumference or body circumference-based body fat estimate to further refine assessments of military health and performance readiness. Unfortunately, conclusions about military readiness are often drawn simply from height and weight data. The human weight and stature relationship is properly expressed as body mass index (BMI), with weight divided by stature squared, using metric units. While an estimated half of all US and British male soldiers exceed current public health goals for Americans of BMI <25 kg/m2, this does not mean that half of soldiers are ‘overweight’, when overweight is defined as excess fat resulting in increased health risk or poorer performance.1–3 In fact, US soldiers are healthier and stronger than any previous generation of soldiers, with an average increase of 14 kg of lean mass in male soldiers over the past century along with better nutrition and medical advances.1 Sanderson et al showed that the majority of British soldiers who attempted their annual physical testing were successful in the combat fitness test and physical fitness test, but soldiers with BMI >30 had higher failure rates, especially those soldiers who also had had high waist circumferences.3 Additionally, the association between BMI and mortality has also shifted in recent years. An analysis of US national data by Flegal et al 4 demonstrated the lowest mortality for men and women in national surveys has moved from a BMI of 18–25 kg/m2 to the previously designated ‘overweight’ category, 25–30 kg/m2. Together, these data suggest that although there are a large number of US and UK soldiers being classified as ‘overweight’ (ie, BMI >25.0 kg/m2), this categorisation may not necessarily equate directly with increased health risk or degraded performance.
BMI and per cent body fat (%BF) are correlated, but the large interindividual variation makes BMI an unsuitable predictor of the body composition of an individual.1 The use of this surrogate measure for body composition to predict physical readiness of an individual is even less suitable. This was highlighted in 1942 by Navy Commander Albert Behnke and his colleagues5 in their early investigations of the use of hydrostatic weight to estimate body composition. Professional American football players, who are large yet actually very lean, averaging 91 kg body mass and 8.3% body fat, could be disqualified from military service based on weight-for-height tables.5 6 This, and the subsequent work by Wilmore and Behnke,7 8 led to the development of practical anthropometric estimations of body fat to replace weight-for-height standards in the US military in the 1980s. Weight-for-height tables were retained only as a screen to determine who may require further evaluation for excess fat, with physical readiness of every member of the force as the intended objective.9
Previous studies have estimated %BF values from existing BMI data, as BMI is the primary metric generally available to epidemiologists examining obesity-related health risk. Key factors in the interpretation of this BMI–%BF relationship are sex and age, while race/ethnicity has only a weak influence in some studies, depending on the race and ethnic representation in the sample.10–14 Sex is necessary to consider in the interpretation of body composition due to sex-specific differences in relative body fat. Age is also an important variable, especially for military populations, where a large number of soldiers are young and still in their late phase of physical maturation. This is reflected by continuing accretion of muscle and bone mass into the third decade of life, and BMI and body composition relationships at these younger ages are changing. Sanderson et al 3 used age 24 as the transition age for the UK sample, while the US Army uses age 21 as a transition to higher BMI and %BF allowances; lean mass maturation falls somewhere in this early 20s age range. At the higher reaches of %BF and BMI, beyond the levels normally seen in healthy soldiers, the relationship between BMI and %BF becomes curvilinear as further increases in BMI are primarily due to increases in fat mass, and accuracy of body composition measurement methods at these higher levels of BMI also becomes more tenuous.10 11 15
Physical fitness represents an additional factor to be considered in the relationship between BMI and body composition that has not been well highlighted in previous attempts to predict %BF from BMI. A recent study demonstrated that eight weeks of basic combat training (BCT) resulted in a substantial reduction in fat mass and increases in lean mass, despite relatively little net change in overall body mass.16 In the current analysis, we extend the findings of this earlier report to include the effect of physical training on the relationship between BMI and body composition.
Methods
Subjects
These data are part of a larger prospective observational study, the ARIEM Reduction in Musculoskeletal Injury Study.17 Volunteers were trainees from seven different BCT classes at Fort Jackson, South Carolina, during 2018–2019 and included 504 female and 965 male participants. Participants provided signed informed consent for this research. Participants were 17–42 years old (mode: 18 years old; median: 19 (women), 20 (men)) and had completed a comprehensive medical screening at a Military Entrance Processing Station. In accordance with the Department of Defense Instruction 3216.20, trainees who are 17 years of age are considered adults while in federal duty status and are allowed to consent without parent or guardian approval. The predominant race and ethnicity breakdowns are as follows: 47% white, 27% black and 21% Hispanic for women and 61% white, 16% black and 20% Hispanic for men.
BCT training exposure
A key focus of BCT is physical readiness training. This is well standardised and documented.18 19 BCT is divided into three phases of training that progress from Army core values and basic soldier tasks to self-discipline, teamwork and weapons training, and finally to leadership skills and field training. Throughout the course, there is an emphasis on physical training including callisthenics, running, and combatives and physically demanding tasks such as cadence march and tactical foot marches. Previous studies have documented the progressive increase in activity energy expenditure in terms of daily steps, averaging 16 000 steps/day or travel of roughly 12 km/day, with a peak in the field training phase near the end of BCT of 22 000 steps/day or roughly 16 km/day.18 A more recent study with research-grade accelerometry estimated time spent in specific activities, including 5% of total activity time in vigorous-intensity activities, with a progressive increase of moderate-vigorous activity each week for the first half of BCT.19 Sleep has been assessed as part of this current study using three sleep inventories and concluded that, initially, mean sleep exceeded seven hours per night with good quality sleep, but this was reduced for some of the soldiers later in the course.20 Food is not restricted during BCT and the Army has made continuous improvements in food service to promote healthy food choices and balanced nutritional intake.21
Procedures
Data collection occurred during week 1 (pre-BCT) and week 9 (post-BCT). Height (cm) was measured with a stadiometer (Model 217, SECA, Chino, California) and fasted total body mass (kg) was measured with a calibrated scale (Model 770, SECA; or Model DS6150, Doran, Batavia, Illinois), with participants in standardised physical training uniforms (athletic shorts and T-shirt) and without shoes. BMI (kg/m2) was calculated from this information.
Body composition was assessed by DXA (GE Lunar Prodigy, GE Healthcare, Madison, Wisconsin). Total body estimates of %BF and fat-free mass (FFM) (kg) were determined using manufacturer-described procedures and supplied algorithms (Encore, V.11.40, Lunar, Madison, Wisconsin). Coefficient of variation for DXA %BF measurements has been previously reported to be <2%.22 Fat-free mass index (FFMI) was calculated as FFM divided by height in metres squared (kg/m2).
Statistical analyses were performed using SPSS for Windows V.24. Descriptive statistics were calculated and reported as mean±SD, and analysis of variance (ANOVA) with linear contrasts was used to assess differences by age group (17–<21, 21–<25, 25–<29, 29+ years old). Significance between age groups was assessed with post-hoc Tukey adjustments. Linear regression best fit models provided r values and SEM. Multivariate (BMI, timepoint) regression was used to assess differences in the intercept (vertical shift) and slope of the relationship between BMI and %BF pre-BCT and post-BCT. %BF was estimated for a BMI of 25.0 kg/m2 and 27.5 kg/m2 (representing the full range of current US Army screening weight tables) from the linear regressions. Sensitivity and specificity were calculated for BMI cut-offs of 25.0 kg/m2 and 27.5 kg/m2, as well as for %BF cut-offs. Relevant Army %BF cut-offs vary by age and sex as follows: 17–20, 21–27 and 28–39 years: 30%, 32% and 34% for women and 20%, 22% and 24% for men, respectively.
Results
Relationship between BMI, stature, FFMI and %BF with age
The mean values for BMI, stature, FFMI and %BF were compared across four age categories in this sample of female and male Army recruits (Table 1). Across age groups, there was a significantly lower BMI and FFMI in the youngest group (age 17–<21) compared with older age categories for men and women (ANOVA with linear contrasts, p<0.02). For men only, mean %BF was also significantly lower in the youngest group (age 17–<21) compared with older age categories.
Table 1.
Mean values for BMI, stature, FFMI and %BF compared across four age categories of female and male Army recruits at entry to BCT
| Age category | P value for trend | ||||
| 17–<21 | 21–<25 | 25–<29 | 29+ | ||
| Women (n) | 339 | 98 | 42 | 26 | |
| Height (cm) | 162±6 | 162±7 | 162±7 | 160±7 | 0.22 |
| Mass (kg) | 61.4±8.3*† | 64.8±9.5‡ | 66.2±9.2‡ | 64.4±8.4 | <0.01 |
| BMI (kg/m2) | 23.5±2.7*†§ | 24.6±2.9‡ | 25.0±2.8‡ | 25.1±2.6‡ | <0.01 |
| FFMI (kg/m2) | 15.4±1.5*†§ | 15.9±1.6‡ | 16.5±1.7‡ | 16.5±1.6‡ | <0.01 |
| %BF | 31.9±5.3 | 33.0±4.8 | 32.0±4.5 | 32.3±6.7 | 0.33 |
| Men (n) | 568 | 244 | 84 | 68 | |
| Height (cm) | 176±7§ | 176±8§ | 176±7 | 179±7*‡ | <0.01 |
| Mass (kg) | 75.3±12.1*†§ | 79.1±13.6‡§ | 82.2±11.3‡ | 85.6±12.4*‡ | <0.01 |
| BMI (kg/m2) | 24.4±3.5*†§ | 25.7±4.1‡ | 26.5±3.3‡ | 26.8±3.3‡ | <0.01 |
| FFMI (kg/m2) | 18.4±1.9*†§ | 18.9±2.2‡ | 19.3±1.9‡ | 19.6±1.7‡ | <0.01 |
| %BF | 22.0±6.1*†§ | 23.5±6.5‡ | 24.6±6.1‡ | 24.5±6.0‡ | <0.01 |
Mean±SD.
*Significantly different from age 21–<25, p<0.05.
†Significantly different from age 15–<29, p<0.05.
‡Significantly different from age 17–<21, p<0.05.
§Significantly different from age 29+, p<0.05.
BCT, basic combat training; %BF, per cent body fat; BMI, body mass index; FFMI, fat-free mass index.
Relationships between BMI and %BF
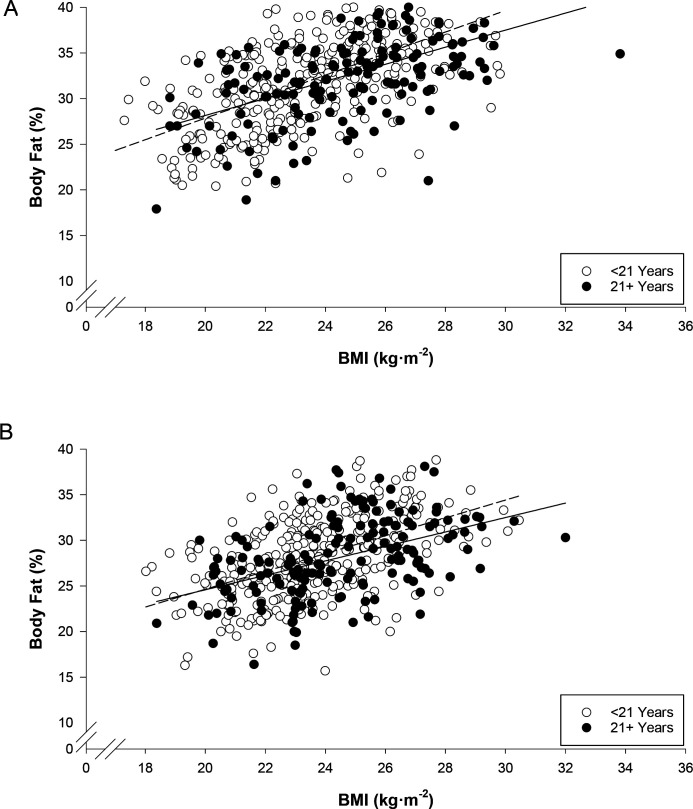
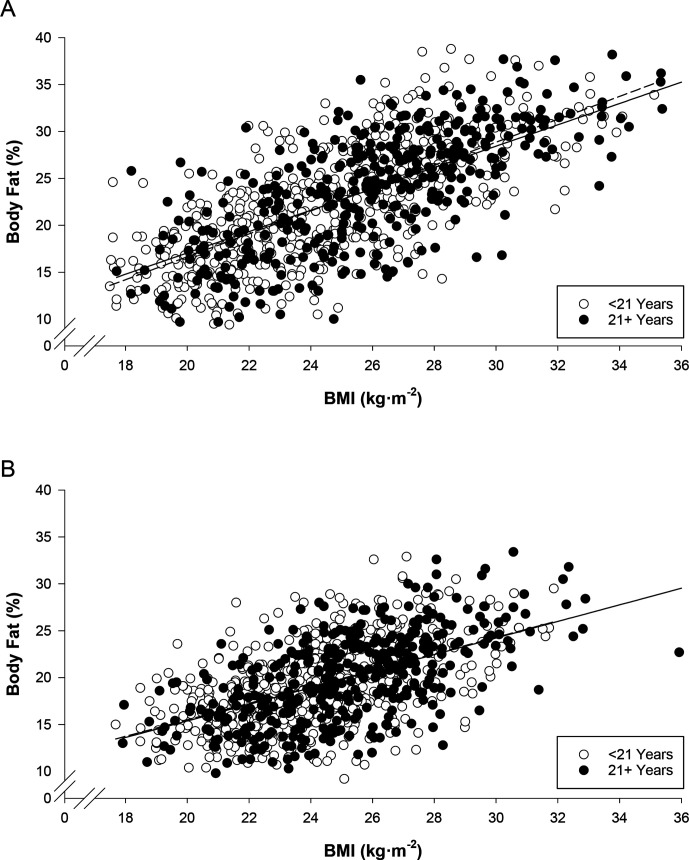
The relationships between BMI and %BF are shown in Figure 1 (women) and Figure 2 (men), with individuals separated by age <21 and age 21+, and with relationships shown at the start of BCT and at the end of BCT. Regression equations, linear correlations and standard estimate of the estimates (%BF) are shown in Table 2. The only significant vertical shift in the regressions pre-BCT to post-BCT was in the younger men (p<0.01). The slopes of the lines were significantly different pre-BCT to post-BCT in both groups of men (p≤0.01) and tended to be different in younger women (p=0.085).
Figure 1.
Relationship between BMI and per cent body fat in women at the start of BCT (A) and at the end of BCT (B). Data are separated by age, <21 years (open circles, dashed regression line) and 21+ years (filled circles, solid regression line). BCT, basic combat training; BMI, body mass index.
Figure 2.
Relationship between BMI and per cent body fat in men at the start of BCT (A) and at the end of BCT (B). Data are separated by age, <21 years (open circles, dashed regression line) and 21+ years (filled circles, solid regression line). BCT, basic combat training; BMI, body mass index.
Table 2.
Relationships between BMI and %BF
| Age/sex category | Timepoint | Predictive equation | r2 | SEE (%BF) |
| Female | ||||
| <21 years | Pre-BCT | y=1.19x+4.05 | 0.36 | 4.26 |
| Post-BCT | y=0.97x+5.20 | 0.26 | 3.72 | |
| 21+ years | Pre-BCT | y=0.95x+9.26 | 0.27 | 4.36 |
| Post-BCT | y=0.79x+8.79 | 0.21 | 3.84 | |
| Male | ||||
| <21 years | Pre-BCT | y=1.22−7.83 | 0.49 | 4.37 |
| Post-BCT | y=0.88x−2.12 | 0.28 | 3.74 | |
| 21+ years | Pre-BCT | y=1.14x−5.72 | 0.48 | 4.58 |
| Post-BCT | y=0.89x−2.42 | 0.31 | 4.05 |
BCT, basic combat training; %BF, per cent body fat; BMI, body mass index.
Predicted mean %BF at BMI 25 kg/m2 and 27.5 kg/m2
At the start of training, a BMI of 25.0 kg/m2 predicted body fat of 34, 33% (young and older women) and 23% (all men). At the end of training, this was reduced to 29% (all women) and 20% (all men) (Table 3). At the start of training, a BMI of 27.5 kg/m2 predicted 37, 35% (young and old women) and 25% (all men), and this reduced to 31, 32% (young and older women) and 22% (all men) at the end of BCT.
Table 3.
Per cent body fat predicted by BMI (25 kg/m2 and 27.5 kg/m2) for men and women, separated by age
| Age/sex category | BMI 25 kg/m2 | BMI 27.5 kg/m2 | ||
| Pre-BCT | Post-BCT | Pre-BCT | Post-BCT | |
| Female | ||||
| <21 years | 33.8 | 29.4 | 36.8 | 31.9 |
| 21+ years | 33.0 | 28.5 | 35.4 | 30.5 |
| 29.4* | 32.4* | |||
| Male | ||||
| <21 years | 22.6 | 19.9 | 25.7 | 22.1 |
| 21+ years | 22.8 | 19.9 | 25.6 | 22.1 |
| 18.6* | 21.6* | |||
*Deurenberg et al equation prediction for men and women aged 21.14
BCT, basic combat training; BMI, body mass index.
Categorisation of %BF by BMI
The sensitivity and specificity of %BF categorisation by a BMI of 25.0 kg/m2 and 27.5 kg/m2 for recruits at the end of training are shown for %BF standards currently used by the US Army in Table 4. The results reveal poor sensitivity and specificity at a BMI threshold of 25.0 kg/m2, particularly at the lower %BF standard used in the youngest recruits. At a threshold of 27.5 kg/m2, specificity is improved, but sensitivity is much lower, particularly in women.
Table 4.
Sensitivity (correct detection of individuals above the %BF value) and specificity (correct rejection of individuals below the %BF value) of BMI classification of %BF for women and men in the total sample at the end of BCT
| Body fat | BMI 25.0 kg/m2 | BMI 27.5 kg/m2 | ||
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |
| Women | ||||
| 30% | 55.1 | 79.0 | 15.1 | 98.1 |
| 32% | 62.4 | 74.5 | 13.8 | 95.2 |
| 34% | 61.7 | 69.4 | 8.5 | 93.4 |
| Men | ||||
| 20% | 64.4 | 76.2 | 27.1 | 95.1 |
| 22% | 71.9 | 72.1 | 34.2 | 94.0 |
| 24% | 79.1 | 66.7 | 41.7 | 91.3 |
BCT, basic combat training; %BF, per cent body fat; BMI, body mass index.
Body composition at the lowest BMI (<20 kg/m2)
At the start of training, 46 women (9.1% of all women) and 69 men (7.2% of all men) were below BMI 20 kg/m2. The women and men were relatively lean (women: 26.6±3.8 %BF; men: 15.8±3.8 %BF), but also remarkably low in mean FFM and FFMI (women: 35.5±3.8 kg and 13.6±0.9 kg/m2; men: 49.0±5.1 kg and 15.6±0.9 kg/m2). By the end of training, the mean body mass in these two groups had increased from 49.7±4.0 kg to 52.6±4.3 kg (women) and from 59.6±5.2 kg to 63.0±6.2 (men) and the mean FFMI increased to 15.0±1.0 kg/m2 (women) and 16.6±1.1 kg/m2 (men).
Discussion
The results demonstrate that at the end of BCT there is a leaner soldier population compared with civilian populations described in several other DXA-based national studies. Gallagher et al 11 found that a BMI of 25.0 kg/m2 predicted a %BF of 35% and 23% for women and men in a large convenience sample. Heo et al 12 analysed the combined 1999–2004 National Health and Nutrition Examination Survey data sets and found that a BMI of 25.0 kg/m2 predicted slightly higher values for %BF at ~37% and ~25% for women and men, with small differences between non-Hispanic white, non-Hispanic black and Hispanic participants. These values roughly equate to the 36% and 26% BF used in Army standards for an upper limit of body fat permitted in the oldest (40+ years) male and female soldiers; these limits of %BF in the Army regulation are anchored to chronic health thresholds derived backwards from a BMI of 25.0 kg/m2 from 1980s soldier data,1 and these most liberal relative body fat standards (but not the BMI of 25.0) may still be appropriate for health thresholds. Post-training BMI–%BF relationships for men and women were very close to the predictions from the 1991 Deurenberg equation based on a fit and healthy Dutch cohort,14 with values as shown in Table 3.
The upper limits of %BF in the US Army regulation are 30% and 20% for those up to age 21, and 32% and 22% for women and men ages 21–27.6 Based on the sensitivity analyses in this study, setting the screening weight tables at a BMI of 27.5 kg/m2 for men and women at any age could be used to identify those largest individuals who may exceed the body fat standards.23 BMI-based screening weights below 27.5 have a lower specificity and setting the levels lower may stigmatise many soldiers who are within body fat standards. The 27.5 kg/m2 BMI cut point was the original recommendation of the 1985 NIH Consensus Panel recommendations that defined obesity at a BMI of >27.3 (women) and >27.8 (men), drawn from the 85th percentile of the BMI for Americans aged 20–30 years old at the time.24 It should again be underlined, consistent with many previous studies, that body fat is not well predicted by BMI; the very large variability in this relationship is evident in the scatterplots in Figures 1 and 2 and in the results described in Table 4. A better solution to modern military body composition standards might be to abandon this imprecise weight-for-height (BMI) screening with routine assessment of lean mass and relative fat against lower and upper sex-adjusted standards for every soldier.
Army standards for lower limits of body mass (BMI >19 kg/m2) attempt to ensure a minimum lean mass and reduce the number of musculoskeletal injuries in BCT, as the latter increase most dramatically at the lowest quintiles of BMI (women <20.7 kg/m2; men <21.7 kg/m2).25 26 Just as BMI is an inadequate surrogate of excessive fat, it is also an inadequate indicator of extremely low relative body fat. In this sample, recruits starting BCT below a BMI of 20 kg/m2 averaged relative fat similar to fit young women and men (ie, 25% BF and 15% BF, respectively), instead of very low relative fat complemented by relatively higher FFM. Those individuals in the lower end of BMI represent a special subset of the emerging digital generation ‘skinny fat’ (metabolically obese normal weight), with recruits who may have a normal relative fat (%BF) and therefore an even lower than expected FFM.27 This particular group will not be flagged by current BMI screening for further body composition assessment. Therefore, different strategies that assess low levels of lean mass or reliance on fitness testing that requires greater demonstration of strength capability than the current Army fitness test are needed. Currently, the Army is moving to the new Army combat fitness test, which has strength and power-specific components.28 Training for this new fitness test is expected to further increase lean mass in women and men, resulting in bigger, stronger and leaner soldiers.29
Body composition continues to change into the third decade, with a non-continuous inflection in FFMI in the early 20s, where some stability in musculoskeletal development occurs. This transition to stable body composition merits further research, along with further focus on physical development trajectories of current digital-era girls and boys of premilitary age (~14–18 years). Further examination of the influence of a fitness culture on expected age-related changes in body composition of ageing soldiers (>40 years) is also merited.
Study limitations
An important caveat in the interpretation of BMI–%BF relationships observed for women in this study is that this is an extrapolation from a relatively lean subset of the civilian population, reflecting the effects of a stricter weight screen in current Army female accession standards. Young women exceeding BMI ~25 kg/m2 are generally expected to meet entry body fat standards of <32% (age <27).25 Therefore, the female soldiers in this study represent individuals who have been preselected on the basis of within-fat standards if they exceed BMI screening limits. This skews the relationship between BMI and body fat, but it represents the current accession and retention standards applied to female soldiers. Moving to a female weight-for-height screening based on BMI 27.5 kg/m2 would increase weight allowances by ~8–15 lbs-.26
A second caveat is the effect of age. It is anticipated that a sample of older male and female soldiers may demonstrate increasing %BF for BMI 27.5 kg/m2, but this age group was not captured in the current analysis of predominantly young recruits. It should be noted that the age-related increase in %BF has been accommodated by the Army’s current age-related body fat limits, where >40 age limits are 36% and 26% BF for women and men.1
Conclusions
Attempts to predict %BF from BMI are problematic due to human variability in body composition that is not simply accounted for by age and sex. In this study, US Army BCT also altered the relationship between BMI and adiposity, with lower %BF at a given BMI at the end of BCT compared with the beginning, further highlighting the unreliability of BMI to try to estimate body composition. Furthermore, age was a discontinuous variable in this sample, with an inflection point in body mass, BMI and FFMI in the third decade. The very low end of BMI did not reflect an extraordinarily low %BF but, rather, a normal relative fat with even lower than expected FFM. In addition to being an unreliable predictor of an individual’s body composition, the specific BMI threshold of 25.0 kg/m2, typically labelled ‘overweight’ and attributed to increased medical risk, is an out-of-date metric for health and performance outcomes. To the extent that %BF reflects physical readiness, these data provide evidence of a fit and capable military force at BMI greater than 25.0 kg/m2.
Acknowledgments
The authors thank the US Army Training and Doctrine Command Center for Initial Military Training for their support, as well as all the researchers and soldiers who participated in the data collection.
Footnotes
Contributors: SAF, JH, SPP and KEF planned the body composition component of this study. SAF and JH submitted and led the study. SAF, JH, BAS, LAW, KIG and KMT collected and managed the data. SAF and KEF analysed and interpreted the data and wrote the first draft of the manuscript. All authors were involved in the final version of the manuscript.
Funding: This study was funded by the Military Operational Medicine Research Program, US Army Medical Research and Materiel Command.
Disclaimer: The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Army or the Department of Defense.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. Not applicable.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the Institutional Review Board of the US Army Medical Research and Development Command, Fort Detrick, Maryland.
References
- 1. Friedl KE. Can you be large and not obese? the distinction between body weight, body fat, and abdominal fat in occupational standards. Diabetes Technol Ther 2004;6:732–49. 10.1089/dia.2004.6.732 [DOI] [PubMed] [Google Scholar]
- 2. Friedl KE, Leu JR. Body fat standards and individual physical readiness in a randomized army sample: screening weights, methods of fat assessment, and linkage to physical fitness. Mil Med 2002;167:994–1000. [PubMed] [Google Scholar]
- 3. Sanderson PW, Clemes SA, Biddle SJH. Prevalence and socio-demographic correlates of obesity in the British Army. Ann Hum Biol 2014;41:193–200. 10.3109/03014460.2014.881918 [DOI] [PubMed] [Google Scholar]
- 4. Flegal KM, Graubard BI, Williamson DF, et al. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861–7. 10.1001/jama.293.15.1861 [DOI] [PubMed] [Google Scholar]
- 5. Welham WC, Behnke AR. The specific gravity of healthy men: body weight ÷ volume and other physical characteristics of exceptional athletes and of naval personnel. J Am Med Assoc 1942;118:498–501. [Google Scholar]
- 6. U.S. Department of the Army . The Army Body Composition Program. Army Regulation 600-9. Washington, DC: U.S. Department of the Army, 2019. [Google Scholar]
- 7. Wilmore JH, Behnke AR. An anthropometric estimation of body density and lean body weight in young men. J Appl Physiol 1969;27:25–31. 10.1152/jappl.1969.27.1.25 [DOI] [PubMed] [Google Scholar]
- 8. Wilmore JH, Behnke AR. An anthropometric estimation of body density and lean body weight in young women. Am J Clin Nutr 1970;23:267–74. 10.1093/ajcn/23.3.267 [DOI] [PubMed] [Google Scholar]
- 9. U.S. Department of Defense . Study of the military services physical fitness. Washington, DC: Office of the Assistant Secretary of Defense for Manpower, Reserve Affairs and Logistics, 1981. [Google Scholar]
- 10. Gallagher D, Visser M, Sepúlveda D, et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996;143:228–39. 10.1093/oxfordjournals.aje.a008733 [DOI] [PubMed] [Google Scholar]
- 11. Gallagher D, Heymsfield SB, Heo M, et al. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000;72:694–701. 10.1093/ajcn/72.3.694 [DOI] [PubMed] [Google Scholar]
- 12. Heo M, Faith MS, Pietrobelli A, et al. Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999-2004. Am J Clin Nutr 2012;95:594–602. 10.3945/ajcn.111.025171 [DOI] [PubMed] [Google Scholar]
- 13. Jackson AS, Stanforth PR, Gagnon J, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: the heritage family study. Int J Obes Relat Metab Disord 2002;26:789–96. 10.1038/sj.ijo.0802006 [DOI] [PubMed] [Google Scholar]
- 14. Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr 1991;65:105–14. 10.1079/BJN19910073 [DOI] [PubMed] [Google Scholar]
- 15. Williams JE, Wells JCK, Wilson CM, et al. Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component model. Am J Clin Nutr 2006;83:1047–54. 10.1093/ajcn/83.5.1047 [DOI] [PubMed] [Google Scholar]
- 16. Foulis SA, Hughes JM, Walker LA, et al. Body mass does not reflect the body composition changes in response to similar physical training in young women and men. Int J Obes 2021;45:659–65. 10.1038/s41366-020-00730-0 [DOI] [PubMed] [Google Scholar]
- 17. Hughes JM, Foulis SA, Taylor KM, et al. A prospective field study of U.S. Army trainees to identify the physiological bases and key factors influencing musculoskeletal injuries: a study protocol. BMC Musculoskelet Disord 2019;20:282. 10.1186/s12891-019-2634-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Knapik JJ, Darakjy S, Hauret KG, et al. Ambulatory physical activity during United States Army basic combat training. Int J Sports Med 2007;28:106–15. 10.1055/s-2006-924147 [DOI] [PubMed] [Google Scholar]
- 19. Simpson K, Redmond JE, Cohen BS, et al. Quantification of physical activity performed during us army basic combat training. US Army Med Dep J 2013:55–65. [PubMed] [Google Scholar]
- 20. Ritland BM, Hughes JM, Taylor KM, et al. Sleep health of incoming army trainees and how it changes during basic combat training. Sleep Health 2021;7:37–42. 10.1016/j.sleh.2020.10.005 [DOI] [PubMed] [Google Scholar]
- 21. Crombie AP, Funderburk LK, Smith TJ, et al. Effects of modified foodservice practices in military dining facilities on AD libitum nutritional intake of US army soldiers. J Acad Nutr Diet 2013;113:920–7. 10.1016/j.jand.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 22. Toombs RJ, Ducher G, Shepherd JA, et al. The impact of recent technological advances on the trueness and precision of DXA to assess body composition. Obesity 2012;20:30–9. 10.1038/oby.2011.211 [DOI] [PubMed] [Google Scholar]
- 23. Friedl KE. Body composition and military performance--many things to many people. J Strength Cond Res 2012;26 Suppl 2:S87–100. 10.1519/JSC.0b013e31825ced6c [DOI] [PubMed] [Google Scholar]
- 24. Kuczmarski RJ, Carroll MD, Flegal KM, et al. Varying body mass index cutoff points to describe overweight prevalence among U.S. adults: NHANES III (1988 to 1994). Obes Res 1997;5:542–8. 10.1002/j.1550-8528.1997.tb00575.x [DOI] [PubMed] [Google Scholar]
- 25. U.S. Department of the Army . Standards of Medical Fitness. Army Regulation 40-501. Washington, DC: U.S. Department of the Army, 2019. [Google Scholar]
- 26. Jones BH, Hauret KG, Dye SK, et al. Impact of physical fitness and body composition on injury risk among active young adults: a study of army trainees. J Sci Med Sport 2017;20:S17–22. 10.1016/j.jsams.2017.09.015 [DOI] [PubMed] [Google Scholar]
- 27. Foulis SA, Hughes JM, Friedl KE. New Concerns About Military Recruits with Metabolic Obesity but Normal Weight (“Skinny Fat”). Obesity 2020;28:223. 10.1002/oby.22724 [DOI] [PubMed] [Google Scholar]
- 28. U.S. Department of the Army . Holistic Health and Fitness. Army Field Manual 7-22. Washington, DC: U.S. Department of the Army, 2020. [Google Scholar]
- 29. Kraemer WJ, Nindl BC, Ratamess NA, et al. Changes in muscle hypertrophy in women with periodized resistance training. Med Sci Sports Exerc 2004;36:697–708. 10.1249/01.MSS.0000122734.25411.CF [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available. Not applicable.