Abstract
There is strong evidence linking stimulant use, namely methamphetamine use, to sexual risk behavior among sexual minority men (SMM); we do not, however, have a good understanding of this relationship among other at-risk populations. In this study, we systematically reviewed associations between stimulant use (i.e., methamphetamine, crack cocaine, cocaine) and sexual risk behaviors among populations facing elevated risk of HIV transmission and acquisition (i.e., SMM, people who inject drugs (PWID), and people living with HIV/AIDS (PLWH)). Random-effects meta-analyses and sensitivity analyses that included crude and adjusted estimates separately were conducted to evaluate the impact of potential confounding variables. The results showed strong relationships between stimulant use and condomless sex, transactional sex, and multiple sexual partners. Results were broadly consistent when analyses were stratified by type of stimulant (methamphetamine, crack cocaine, and other stimulants) and risk group. Sensitivity analyses with confounding variables did not greatly impact results. The results indicate that stimulant use is associated with numerous sexual risk behaviors regardless of risk group, suggesting prevention efforts focused on reducing methamphetamine-related HIV risk should target a range of at-risk populations.
Keywords: Stimulants, Sexual risk behaviors, Persons who inject drugs, HIV/AIDS, Meta-analysis
Introduction
Stimulant use including methamphetamine, cocaine, and crack cocaine continue to see increased use worldwide; according to the most recent World Drug Report in 2021, there was a 64% increase in global amphetamine type stimulant use (ATS) drug seizures compared to the year prior, representing the highest annual growth since 2001 [1]. This increase was largely fueled by methamphetamine, which saw a 10-fold increase from 2009 to 2019. Cocaine use increased modestly as well during the same reporting period while crack cocaine use has remained relatively stable (and remains as having the lowest prevalence of use among the three main ATS substances reported).
There are numerous studies that have documented associations between stimulant use and increased sexual risk behaviors such as unprotected sex, transactional sex, and having multiple sex partners [2–5]. There have also been several studies examining associations with infectious diseases including HIV [6, 7] and sexually transmitted infections (STI). Recent evidence also shows that more than one in three new HIV infections is linked to persistent methamphetamine use in sexual and gender minority populations [8]. Stimulant use among sexual and gender minority populations has been well described [5, 9–11] with sexual minority men (SMM) accounting for 69% of new HIV infections in 2019 in the United States [12]. Understanding how risks may differ among these different at-risk populations is important to tailoring effective interventions and harm reduction programs in locations with high HIV incidence or experiencing HIV outbreaks [13], which may include safer sex resources and education.
In many locations where HIV had been dominated by injection drug use, combined HIV prevention and harm reduction efforts for persons who inject drugs (PWID) [14] has led to transitions in HIV epidemics from injection dominated to sexually dominated transmission scenarios [15], many of which are fueled by stimulant use including methamphetamine use. Stimulant use is also a factor in sexually related HIV and STI transmission and may contribute to injection-related transmission as well. In fact, injection drug use has been associated with having an STI diagnosis [16] and approximately 15% of those with HIV are also co-infected with an STI [17]. Among PWID in the United States, nearly 70% have reported the use of methamphetamine, which is similar to rates seen among PWID populations surveyed in Southeast Asia [18].
A meta-analysis conducted in 2002 among people living with HIV (PLWH) found that over 70% of individuals remain sexually active after learning of their HIV diagnosis, with several studies showing that up to 60% of those sexually active continued to engage in risky sexual behaviors, including unprotected sex. These behaviors put others, as well as themselves, at risk for contracting other infections, including STIs [19].
There have been several studies that have attempted to systematically review and synthesize the quantitative data on associations between stimulant use and high-risk sexual behaviors, but given the long history of stimulant use among sexual minority populations such as SMM [20], many of the studies have focused on this population with limited evidence examining other risk groups such as PWID and non-SMM PLWH.
In order to address gaps in the literature on stimulant use and different at-risk populations, we performed a systematic review examining associations between stimulant use and different high-risk sexual behaviors among SMM, PWID and PLWH. We first aimed to evaluate the magnitude of the association between stimulant use and having unprotected sex, engaging in sex work (i.e., transactional sex), and having multiple sex partners. We then assess how these associations may differ across different at-risk populations (SMM, PWID and PLWH).
Methods
We performed a systematic review of studies evaluating the association between stimulant use and high-risk sexual behaviors, including unprotected sex, transactional sex, and multiple sex partners. As noted in the introduction, the search was focused on SMM, PWID and PLWH. While operationalization of these concepts varied from study to study, we used the following definitions to guide our inclusion/exclusion of studies from our review; stimulant use refers to cocaine, crack, methamphetamine, or amphetamine use [21]. Transactional sex refers to giving or receiving money, gifts, or other services in exchange for sexual intercourse [22]. Unprotected sex refers to condomless anal or vaginal sexual intercourse, including at last intercourse [23]. Multiple sex partners refer to sexual intercourse with two or more people, including partnerships that overlapped in time (i.e., concurrent) [24]. A protocol was not prepared for this report.
Search Strategy
We searched PubMed for English-language and human studies published through November 2020. Two searches were conducted; one search included keywords related to stimulant use and unprotected sex and the other search included keywords related to stimulant use, transactional sex, and multiple sex partners (See Appendix for search terms). We combined transactional sex and multiple sex partners into one literature search as we previously observed that several studies report both outcomes. We identified additional articles through a manual search of reference lists in relevant publications. We omitted unpublished data and non-English literature due to resource constraints.
Study Selection
We reviewed abstracts of studies obtained through the literature search and reviewed the full articles if the abstract reported an association between stimulant use and one of the sexual risk behaviors of interest. Upon full review, studies were selected if they included: (1) a stimulant using group, (2) a non-stimulant using comparison group, (3) sexual risk behavior outcome(s), and (4) a quantitative estimate of the association between stimulant use and the risk behavior or sufficient information to calculate an estimate (i.e., count data or stratified prevalence). Only studies that reported or permitted inferences of odds ratios (OR) and 95% confidence intervals (CI) were included in the meta-analyses. To ensure all relevant studies were captured, no restrictions were placed on publication date, study design, location, or population.
Data Extraction
A standardized form was used to extract the following data from eligible studies: year of publication, sample size, study design, setting, population, description of exposure and outcome, crude and adjusted measures of the association, and confounding variables. When quantitative estimates were not explicitly reported but sufficient information was available, an OR and 95% CI were calculated. Unless we were conducting a relevant subgroup analysis, if the study reported an OR for several study populations (e.g., men and women) or stimulants (e.g., crack and methamphetamine), we used available count data to calculate a summary unadjusted OR.
If multiple ORs were reported in a study and quantitative pooling was not possible, we implemented a set of decision rules to determine which estimate we would include. First, we selected the population or stimulant most reported across all other eligible studies (e.g., select the crack-specific estimate if most other studies included in the meta-analysis reported on crack). Second, if an OR was reported for multiple strata (e.g., frequent stimulant use vs. any stimulant use in the last year), we selected the strata that reflected the riskier behavior. Third, if an OR was reported for multiple timeframes, we chose the timeframe that increased the likelihood of temporality where the exposure precedes the outcome (e.g., stimulant use at last sexual encounter vs. lifetime stimulant use). Using forest plots, we qualitatively evaluated whether extracted estimates met the level of homogeneity necessary to perform a meta-analysis. A large number of studies in each meta-analysis makes traditional quantitative criteria of homogeneity too sensitive but not specific enough to exclude heterogeneous studies [25].
Two reviewers took part in the data extraction; consensus on what studies to include was discussed during regular meetings with the study team.
Data Analysis
Random-effects meta-analyses were performed using RStudio, Version 1.3.1093. We calculated a separate pooled estimate including all eligible studies regardless of population for each sexual risk behavior outcome (unprotected sex, transactional sex, and multiple sex partners). Subgroup analyses were performed by study population (SMM, PWID and PLWH). We assessed statistical heterogeneity using the I-squared test statistic and the Q-statistic. For sensitivity analyses we calculated estimates that excluded studies that reported multiple ORs to assess the effect of applying the decision rules described above. We also calculated pooled ORs that included only crude and adjusted estimates separately to evaluate the impact of confounding variables. The results were tabulated in tables and figures of included studies and their overall effects (see supplementary file for a full breakdown of all studies and summary measures).
Results
We identified a total of 1476 eligible abstracts after removal of 285 duplicate abstracts identified. After the abstract screening, we fully reviewed 166 manuscripts of which 126 met the criteria for inclusion in the meta-analysis (Fig. 1). These manuscripts included 71 studies related to unprotected sex, 50 related to transactional sex, and 20 studies related to multiple sex partners.
Fig. 1.
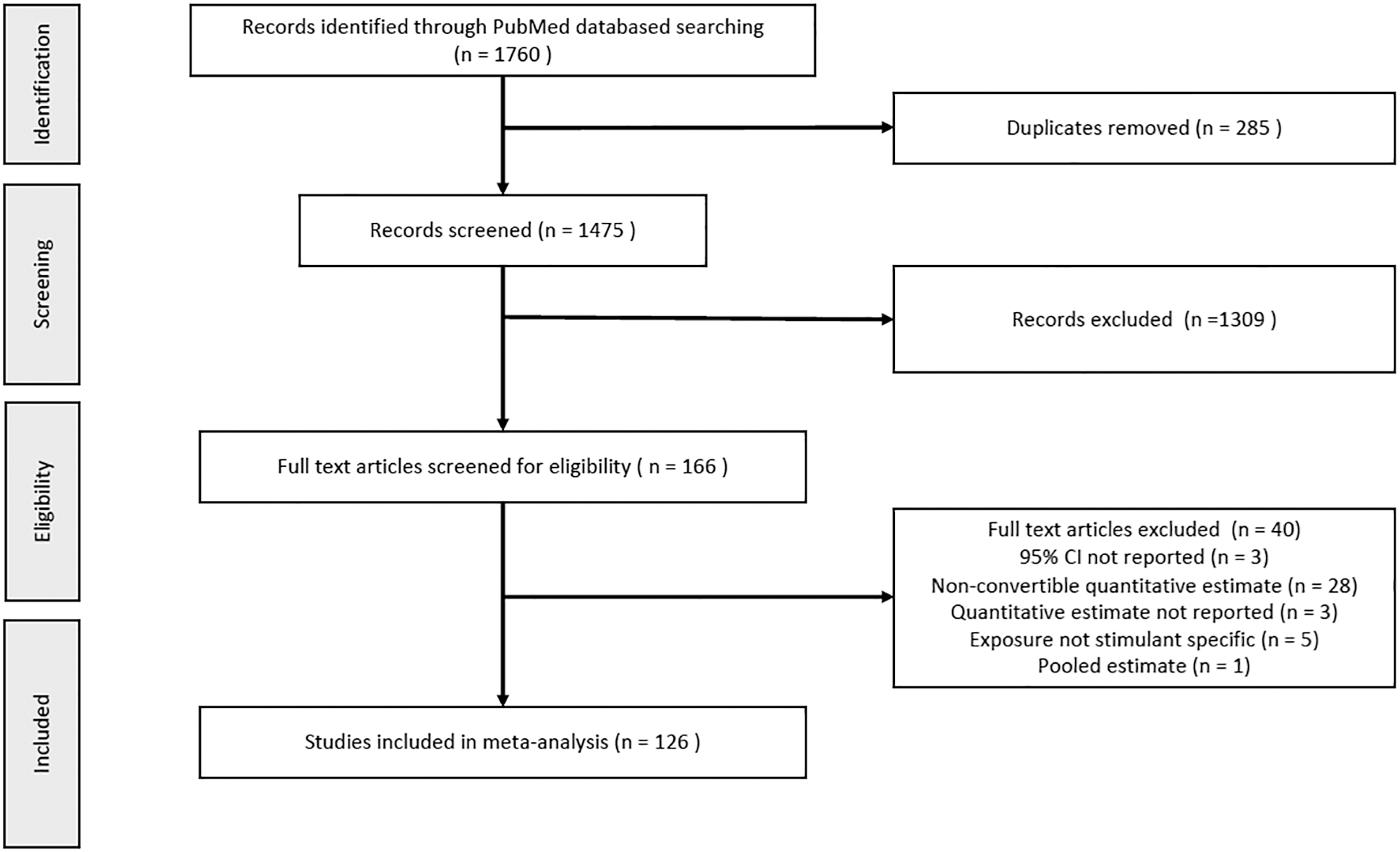
Study identification, screening, eligibility, and inclusion for in meta-analyses by outcome
Study characteristics varied and are summarized in Table 1 (see Appendix Tables S1–S6 and Figures S1–S6 for complete study characteristics and results by individual study). Across all outcomes, most studies were cross-sectional and took place in North America. The most frequently sampled populations were SMM for unprotected sex, PWID for transactional sex, and adults in general for multiple sex partners. Methamphetamine was the most investigated substance in the association with unprotected sex, while crack was the most investigated substance in the association with transactional sex and multiple sex partners. There was heterogeneity in the measurement of exposure and outcome. All studies but one assessed self-reported stimulant use, but the recall period varied widely from past week to lifetime. Additionally, the frequency of stimulant use varied from greater than daily to any use. Given the variability in the operationalization of outcomes, it was difficult to characterize their definitions. Unprotected sex was most commonly evaluated as any unprotected sex between the past 30 days and the past 12 months. Transactional sex was most commonly evaluated as any selling sex in the past 30 days to lifetime. Multiple sex partners was most commonly evaluated as greater than one sex partner in past 30 days to past 12 months.
Table 1.
Summary of studies included in meta-analyses including all eligible studies
| Study characteristics: | Unprotected Sex N (%) |
Transactional sex N (%) |
Multiple Partners N (%) |
|---|---|---|---|
|
| |||
| Total (N) | 71 | 50 | 20 |
| Study design Case-control | 2 (2.8) | 1 (2) | 1 (5) |
| Cohort | 11 (15.5) | 8 (16) | 2 (10) |
| Cross-sectional | 57 (80.2) | 40 (80) | 16 (80) |
| Natural history | 1 (1.5) | 0 (0) | 1 (5) |
| Study population* | |||
| Adolescents/Young adults | 10 (13) | 6 (12) | 6 (30) |
| Adults | 10 (13) | 16 (32) | 8 (40) |
| FSW | 3 (3.9) | 0 (0) | 2 (10) |
| SMM | 35 (45.4) | 9 (18) | 1 (5) |
| PLWH | 8 (10.4) | 1 (2) | 1 (5) |
| PWID | 11 (14.3) | 18 (36) | 2 (10) |
| Study setting Internet-Based | 3 (4.2) | 3 (6) | 0 (0) |
| Africa | 1 (1.5) | 0 (0) | 0 (0) |
| Asia | 5 (7) | 5 (10) | 2 (10) |
| Australia | 2 (2.8) | 1 (2) | 2 (10) |
| Europe | 2 (2.8) | 3 (6) | 2 (10) |
| North America | 55 (77.5) | 36 (72) | 14 (70) |
| South America | 3 (4.2) | 2 (4) | 0 (0) |
| Study population* | |||
| Adolescents/Young adults | 10 (13) | 6 (12) | 6 (30) |
| Adults | 10 (13) | 16 (32) | 8 (40) |
| FSW | 3 (3.9) | 0 (0) | 2 (10) |
| SMM | 35 (45.4) | 9 (18) | 1 (5) |
| PLWH | 8 (10.4) | 1 (2) | 1 (5) |
| PWID | 11 (14.3) | 18 (36) | 2 (10) |
| Stimulant type Cocaine | 11 (15.5) | 8 (16) | 4 (20) |
| Crack | 7 (9.9) | 24 (48) | 9 (45) |
| Cocaine/crack (dual use) | 4 (5.6) | 4 (8) | 1 (5) |
| Methamphetamine | 41 (57.7) | 8 (16) | 5 (25) |
| Other stimulants | 8 (11.3) | 6 (12) | 1 (5) |
Sum of studies by study population may be greater than the total number of studies included in meta-analyses, as some studies include populations that represent more than one category (ex. HIV seropositive SMM)
Stimulant Use and Unprotected Sex
For the 71 studies investigating the association between stimulant use and unprotected sex, the pooled OR was 2.08 (95% CI, 1.87–2.30) when all eligible studies were included (Fig. 2A). We found variability in estimates, and significant heterogeneity was detected (Q = 251.3, p < 0.001; I2 = 70.7%). However, all but two studies reported a positive association between stimulant use and unprotected sex, and the 95% CIs overlapped in most cases (Appendix Figure S2). Pooled estimates did not differ greatly by study population. For the 35 studies of SMM, the pooled OR was 2.14 (95% CI, 1.65–2.77); for the eight studies of PLWH, the pooled OR was 2.56 (95% CI, 1.73–3.87); and for the seven studies of PWID, the pooled OR was 2.35 (95% CI, 1.97–2.81) (Fig. 2A).
Fig. 2.
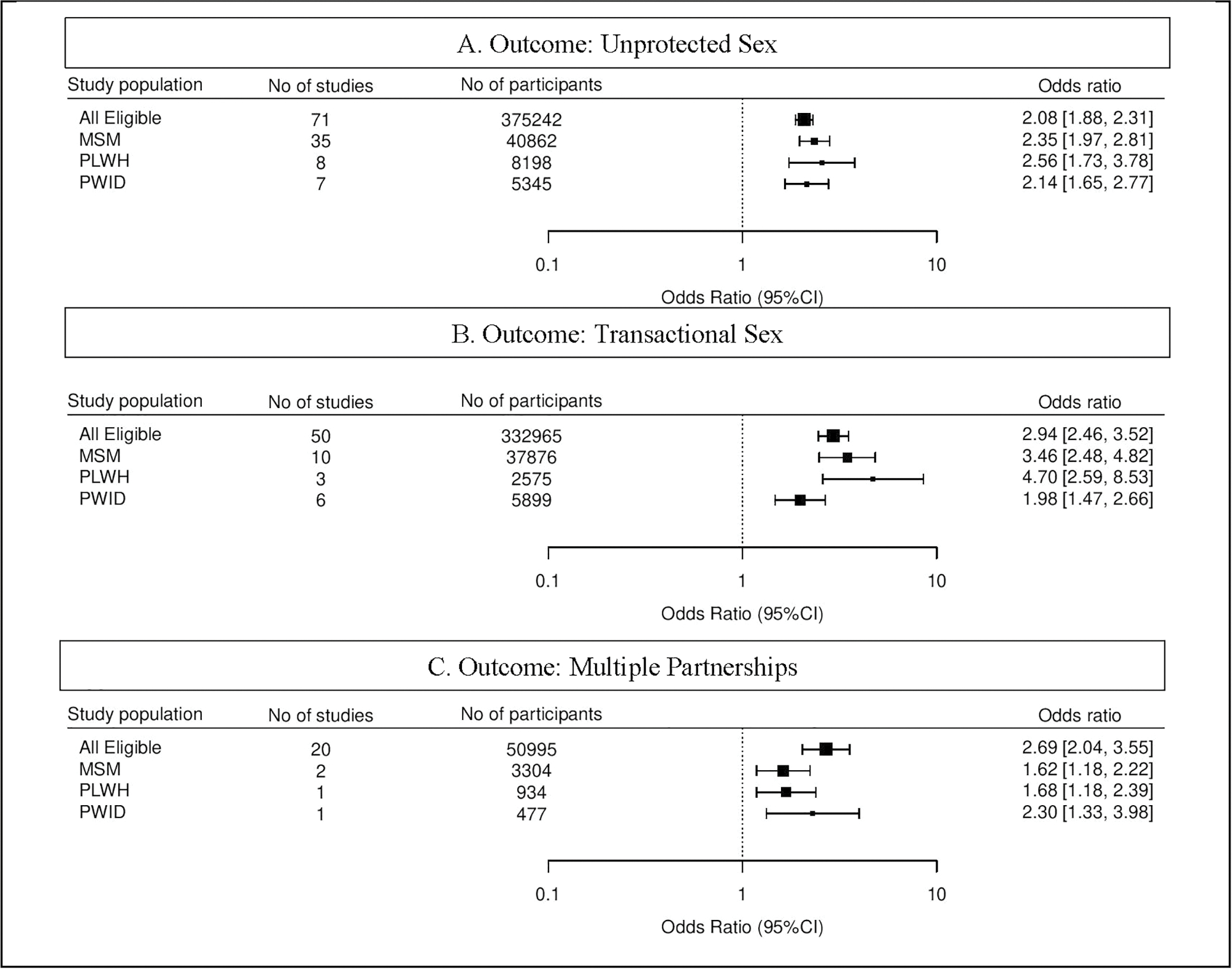
Summary estimates of the association between stimulant use and risky sexual behavior by study population; (A) unprotected sex, (B) transactional sex, (C) multiple sex partner
Stimulant Use and Transactional Sex
For the 50 studies investigating the association between stimulant use and transactional sex, the pooled OR was 2.69 (95% CI, 2.04–3.55) when all eligible studies were included (Fig. 2B). We found a significant amount of heterogeneity between estimates (Q = 463.67, p < 0.0001; I2 = 89.2%). However, all but one study found a positive association between stimulant use and transactional sex, with substantial overlap in the 95% CIs (Appendix Figure S4). Pooled estimates appeared to differ by population, but confidence intervals were wide. For the ten studies of SMM, the pooled OR was 3.46 (95% CI, 2.48–4.82); for the three studies of PLWH, the pooled OR was 4.70 (95% CI, 2.59–8.53); and for the six studies of PWID, the pooled OR was 1.98 (95% CI, 1.47–2.66) (Fig. 2B).
Stimulant Use and Multiple Sex Partners
For the 20 studies investigating the association between stimulant use and multiple sex partners, the pooled OR was 2.94 (95% CI, 2.46–3.52) when all eligible studies were included (Fig. 2C). We found a significant amount of heterogeneity in estimates (Q = 113.32, p < 0.001; I2 = 84.5%). All studies found a positive association between stimulant use and having multiple sex partners (Appendix Figure S6). Subgroup analyses were not conducted for PWID or PLWH, as we found only one eligible study for each risk group. For the two studies of SMM, the pooled OR was 1.62 (95% CI, 1.18–2.22); for the one study of PLWH, the OR was 1.68 (95% CI, 1.18–2.39); and for the one study of PWID, the OR was 2.30 (95% CI, 1.33–3.98) (Fig. 2C).
Sensitivity Analyses
The exclusion of studies reporting multiple estimates did not result in an OR that differed greatly from when all eligible studies were pooled, suggesting that decision rules did not affect the magnitude of association between exposure and outcome. Across all outcomes, summary estimates that included all eligible studies did not differ greatly from those that included only adjusted estimates. Additionally, studies that adjusted for other substance use (including alcohol, tobacco, or opioid use) or mental health conditions (anxiety, chronic pain, or depression) did not differ substantially from those adjusted for any covariate. However, the inclusion of only crude estimates resulted in a summary estimate greater in magnitude than when all eligible studies were pooled.
Discussion
In our analysis and review, we found that associations between stimulant use and high-risk sexual behavior varied by behavior with odds ratios ranging from 2.08 to 2.94 with the strongest associations seen when examining associations between stimulant use and transactional sex. Although there were slight differences in associations by sexual risk behavior, all associations had an odds ratio above 2 and suggest that stimulant use by individuals in any population significantly increases the likelihood of all high-risk sexual behaviors. These associations also support stimulant use as a driver of HIV and STI incidence through sexual transmission; indeed, a recent systematic review has linked ATS use to increasing HIV infection [26].
When examining transactional sex among specific risk groups, we noted positive associations across the different risk groups, with the strongest associations seen among people living with HIV and sexual minority males. Although there are a number of studies that have linked injection drug use to transactional sex [27, 28], in many locations where PWID reside, the dominant form of drug use is heroin. Given the prior literature that has linked heroin use to sexual dysfunction [29], the weaker associations seen among PWID could be a result of their dual heroin/stimulant poly-drug use. It also suggests that transactional sex carried out by PWID may be less influenced by stimulant use compared to SSM and PLWH; indeed, many studies that have examined transactional sex among PWID have highlighted heroin as the dominant drug that sex workers typically use and what drives their continued transactional sex work [30, 31].
When examining unprotected sex, we found similar relationships for all three different risk groups of SMM, PWID and PLWH, ranging from 2.14 to 2.56, which are similar to effects obtained from a recent meta-analysis examining heterosexual methamphetamine use and unprotected sex [3]. Our analysis further extends this meta-analysis to consider similar high-risk sexual risk behaviors with inclusion of other high-risk groups including PWID and SMM and supports the findings that stimulant use is a consistent risk factor for unprotected sex across multiple at-risk populations.
Despite the inclusive nature of our search that covered multiple at-risk populations for elevated HIV and STI incidence, there are several other risk groups that deserve mention and have been consistently under-studied in the literature, including racial minority women, homeless individuals, transgender women, and people on medicated assisted treatment such as methadone and buprenorphine for heroin dependence. Further research is needed to explore relationships among these at-risk populations, with subsequent reviews conducted once an ample number of studies have been conducted on these groups. This should be done in conjunction with continued studies among SMM, PWID and PLWH to ascertain changes in risk over time.
Limitations
Several limitations should be noted. As this was a literature search conducted using key search terms, there is a possibility that we may have missed certain studies or published manuscripts examining the relationship between stimulant use and sexual risk behaviors. We did, however, attempt to be exhaustive in our search terminology used to locate relevant studies. Second, a lack of studies limits our ability to assess how populations might differ in their association between stimulant use and having multiple sex partners. Third, we found substantial heterogeneity in effect sizes across all outcomes and subgroup analyses, as evidenced by significant Q values; this finding could be due to the substantial variability observed in the operationalization of exposure and outcomes. Finally, as this analysis was focused on SMM, PWID, and PLWH, the results may not be generalizable to other HIV affected populations.
Conclusion
The results from this review show robust associations between the stimulant use and different high-risk sexual behaviors, with consistent positive associations seen regardless of sexual risk or risk group. The findings highlight the importance of addressing stimulant use and mitigating its risks across all populations that may be at risk for elevated HIV and STI transmission risk. Future research and clinical practice should explore approaches to jointly address stimulant use and sexual risk behavior across all HIV affected populations as our findings suggested increased risk for HIV transmission and acquisition in the context of stimulant use.
Supplementary Material
Funding
The study was funded by the National Institutes of Health/The National Institute on Alcohol Abuse and Alcoholism NIH/NIAAA, R01 AA024706 and NIH/NIAAA, U01 AA020799.
Footnotes
Declarations
Conflicts of Interest (include appropriate disclosures) No conflicts of interest.
Ethics Approval (include appropriate approvals or waivers) This research is exempt from IRB approval or review as it utilizes publicly available data from peer reviewed publications.
Consent to Participate Not applicable
Consent for Publication Not applicable
Code Availability (software application or custom code) Code availability for the analysis is available from the primary author
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10461-023-04012-4.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Data Availability
All data in the analysis are available from the primary studies in the main document and supplementary material appendices
References
- 1.Office on Drugs and Crime (UNODC). UNODC report on East and Southeast Asia: continued growth in the supply of methamphetamine while synthetic opioids spread. Geneva; 2021. [Google Scholar]
- 2.Hittner JB, Schachne ER. Meta-analysis of the association between ecstasy use and risky sexual behavior. Addict Behav. 2012;37:790–6. [DOI] [PubMed] [Google Scholar]
- 3.Hittner JB. Meta-analysis of the association between methamphetamine use and high-risk sexual behavior among heterosexuals. Psychol Addict Behav. 2016;30(2):147–57. [DOI] [PubMed] [Google Scholar]
- 4.Cretzmeyer M, Sarrazin MV, Huber DL, Block RI, Hall JA. Treatment of methamphetamine abuse: research findings and clinical directions. J Subst Abuse. 2003;24:267–77. [DOI] [PubMed] [Google Scholar]
- 5.Mansergh G, Shouse R, Marks G, Guzman R, Rader M, Buchbinder S, Colfax G. Methamphetamine and sildenafil (Viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. Sex Transm Infect. 2006;82:131–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nerlander LM, Hoots BE, Bradley H, Broz D, Thorson A, Paz-Bailey G, Group N. HIV infection among MSM who inject methamphetamine in 8 US cities. Drug Alcohol Depend. 2018;190:216–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hahn JA, Page-Shafer K, Lum PJ, Ochoa K, Moss AR. Hepatitis C virus infection and needle exchange use among young injection drug users in San Francisco. Hepatology. 2001;34:180–7. [DOI] [PubMed] [Google Scholar]
- 8.Grov C, Westmoreland D, Morrison C, Carrico AW, Nash D. The Crisis We Are Not Talking About: One-in-Three Annual HIV Seroconversions Among Sexual and Gender Minorities Were Persistent Methamphetamine Users. Journal of Acquired Immune Deficiency Syndromes (1999) 2020, 85:272–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: a systematic review of the literature. Int J Drug Policy. 2019;63:74–89. [DOI] [PubMed] [Google Scholar]
- 10.Sandfort TG, Knox JR, Alcala C, El-Bassel N, Kuo I, Smith LR. Substance use and HIV risk among men who have sex with men in Africa: a systematic review. Journal of Acquired Immune Deficiency Syndromes (1999) 2017, 76:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher DG, Reynolds GL, Napper LE. Use of crystal methamphetamine, Viagra, and sexual behavior. Curr Opin Infect Dis. 2010;23:53–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.HIV in the United States and, Areas D. [https://www.cdc.gov/hiv/statistics/overview/ataglance.html]
- 13.Des Jarlais DC, Sypsa V, Feelemyer J, Abagiu AO, Arendt V, Broz D, Chemtob D, Seguin-Devaux C, Duwve JM, Fitzgerald M. HIV outbreaks among people who inject drugs in Europe, North America, and Israel. The Lancet HIV. 2020;7:e434–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Des Jarlais DC, Arasteh K, McKnight C, Feelemyer J, Hagan H, Cooper HL, Perlman DC. Combined HIV Prevention, the New York City Condom distribution program, and the evolution of Safer Sex Behavior among Persons who inject drugs in New York City. AIDS Behav. 2014;18:443–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Mathers BM, Degenhardt L, Hagan H. Transitions from injection-drug-use-concentrated to self-sustaining heterosexual HIV epidemics: patterns in the international data. PLoS ONE. 2012;7:e31227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brookmeyer KA, Haderxhanaj LT, Hogben M, Leichliter J. Sexual risk behaviors and STDs among persons who inject drugs: a national study. Prev Med. 2019;126:105779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sexualy Transmmited Infections. 2011;87:183–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Des Jarlais DC, Feelemyer J, Arasteh K, Huong DT, Oanh KTH, Khue PM, Giang HT, Thanh NTT, Moles JP, Vinh VH, et al. The methamphetamine epidemic among persons who inject heroin in Hai Phong, Vietnam. J Subst Abuse Treat. 2021;126:108320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: a review of social, psychological, and medical findings. AIDS. 2002;16:135–49. [DOI] [PubMed] [Google Scholar]
- 20.Chesney M, Barrett DC, Stall R. Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health. 1998;88:113–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abuse Susbstance and Mental Health Services Administration (SAMHSA). 2020 National Survey on Drug Use and Health (NSDUH). Bethesda MD; 2021. [Google Scholar]
- 22.McMillan K, Worth H, Rawstorne P. Usage of the terms prostitution, sex work, transactional sex, and survival sex: their utility in HIV prevention research. Arch Sex Behav. 2018;47:1517–27. [DOI] [PubMed] [Google Scholar]
- 23.When Sex Goes Wrong. [https://www.nhs.uk/live-well/sexual-health/when-sex-goes-wrong/ ]
- 24.Mutinta G, Govender K, George G, Gow J. The influence of bio-logical factors on students’ sexual behaviour at the University of KwaZulu-Natal, South Africa. Afr J AIDS Res. 2014;13:321–9. [DOI] [PubMed] [Google Scholar]
- 25.von Hippel PT. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urb Health. 2003;80:iii7–iii14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Booth RE, Watters JK, Chitwood DD. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. Am J Public Health. 1993;83:1144–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilchrist G, Gruer L, Atkinson J. Comparison of drug use and psychiatric morbidity between prostitute and non-prostitute female drug users in Glasgow, Scotland. Addict Behav. 2005;30:1019–23. [DOI] [PubMed] [Google Scholar]
- 29.Smith DE, Moser C, Wesson DR, Apter M, Buxton ME, Davison JV, Orgel M, Buffum J. A clinical guide to the diagnosis and treatment of heroin-related sexual dysfunction. J Psychoactive Drugs. 1982;14:91–9. [DOI] [PubMed] [Google Scholar]
- 30.Gossop M, Powis B, Griffiths P, Strang JJ. Sexual behaviour and its relationship to drug-taking among prostitutes in south London. Addiction. 1994;89:961–70. [DOI] [PubMed] [Google Scholar]
- 31.Reuben J, Serio-Chapman C, Welsh C, Matens R, Sherman SG. Correlates of current transactional sex among a sample of female exotic dancers in Baltimore, MD. J Urb Health. 2011;88:342–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data in the analysis are available from the primary studies in the main document and supplementary material appendices


