Summary
Background
The overdose epidemic in the United States (US) continues to generate unprecedented levels of mortality. There is urgent need for a national data system capable of yielding high-quality, timely, and actionable information on existing and emerging drugs. Public health researchers have started using law enforcement forensic laboratory data to obtain surveillance information on illicit drugs. This study is the first to use drug reports from the entire US to examine correlations between a changing drug supply and increasing opioid-involved overdose deaths (OOD) on a national scale.
Methods
This study is observational and investigates associations between law enforcement drug reports and OOD for the US from 2014 to 2019. OOD data are from the Centers for Disease Control and Prevention’s National Vital Statistics System restricted-use multiple cause of death files. The US Drug Enforcement Administration’s National Forensic Laboratory Information System (NFLIS) contains forensic laboratory–tested drug exhibit information for the entire US (NFLIS-Drug). Counts of forensic laboratory reports and OOD were aggregated for each state by month, quarter, and year. A difference-in-differences framework was used to estimate contemporaneous and lagged associations.
Findings
Between 2014 and 2019 in the US, 249,522 OOD were reported, with the annual number nearly doubling from 28,723 to 50,179. OOD involving illicitly manufactured fentanyls (IMF) also increased substantially during this period, from 19.4% to 72.9%. In addition, 3,817,438 forensic laboratory reports in the US that were reported to NFLIS-Drug contained an opioid, stimulant, or benzodiazepine. Reports of fentanyl and fentanyl-related compounds (FFRC) had the strongest association with OOD. Each additional FFRC exhibit was associated with a 2.97% (95% CI: 1.7%, 4.1%) increase in OOD per 100,000 persons per quarter.
Interpretation
Adding to the emerging consensus, protracted growth in IMF supply was more strongly associated with OOD than all other illicit drugs reported to NFLIS-Drug over the study time period. Findings demonstrate NFLIS-Drug data usefulness for research that require proxy indicators for the illicit drugs supply. A concerted effort between public health and public safety to make NFLIS-Drug more timely could strengthen its utility as a national, public health, drug surveillance system.
Funding
Sangeetha Arctic Slope Mission Services, LLC, ASMS Contract No. ASM5-00017.
Keywords: Illicit drug supply, Opioid overdose deaths, Drug seizures, Illicit drug surveillance
Research in context.
Evidence before this study
There is a paucity of information on the trends of illicit drugs sold via unlawful markets in US and even less information on supply-side associations with drug overdose mortality. We searched PubMed using the search (NFLIS-Drug [Title] OR NFLIS [Title]) and reviewed the bibliographies of the resulting 10 articles for relevant articles. Of these, most (N = 5) employed NFLIS to identify prevalence of specific drugs and several (n = 3) compared NFLIS trends to policy changes or health outcomes. This search revealed that, to date, there are no published articles that uses a nationally representative sample of law enforcement exhibits of seized drugs (NFLIS-Drug) to estimate contemporaneous and lagged associations between trends in illicit drugs and drug overdose mortality over time for the entire US.
Added value of this study
This study is the first to use NFLIS to investigate associations between concurrent trends in the illicit drug supply and drug overdose mortality over time. Current study findings demonstrate NFLIS-Drug’s usefulness for research requiring proxy indicators of the illicit drug supply. Study results show how changes in opioid overdose mortality were associated with changes in the type of opioids sold in illicit markets, specifically IMF. Findings validate NFLIS-Drug’s utility for investigating the influence of the illicit drug supply and law enforcement drug seizures on drug overdose deaths.
Implications of all the available evidence
NFLIS-Drug is currently the largest national-level, publicly available database on laboratory-tested drugs sold in US illicit drug markets. By providing current researchers the capacity to both identify illicit drugs circulating in unlawful markets and assess their impact on overdose mortality in all 50 US states and the District of Columbia, study findings suggest NFLIS-Drug could serve as a national drug data system. Such a system could strengthen public health’s ability to identify emerging risks before they evolve into public health crises and provide impacted jurisdictions with timely and actionable information to strengthen response.
Introduction
The overdose epidemic in the United States (US) continues to generate unprecedented levels of mortality. The Centers for Disease Control and Prevention (CDC) reported an estimate of 107,622 drug overdose deaths from 2021, a 15% increase from 2020.1 National mortality data show that the evolution of the opioid epidemic involves three distinct but intersecting waves of mortality.2 The first wave began in the mid-1990s with the introduction of OxyContin® and subsequent increases in prescription opioid overdose deaths.3 The second wave appeared midway through the prescription opioid crisis (2008–2012) marked by sharp increases in heroin use and related overdose deaths.4 The third (and current) wave began in 2013 as illicitly manufactured fentanyls (IMF) started being detected in overdose deaths in the Northeast and Mid-Atlantic states before causing record-high mortality throughout the US.5 Most recently, sharp increases in opioid overdose deaths with co-occurring cocaine or methamphetamine indicate a growing 4th mortality wave involving illicit stimulants and illicit opioids.
Identifying the substances responsible for overdose deaths is customarily performed by medical examiners and coroners (ME/Cs) via blood and urine toxicology. Decedent toxicology helps establish the main cause of death and any contributing factors while providing a “snapshot” of drugs in illicit markets.6 Novel drugs can escape notice of ME/Cs or be recognized as toxic but remain unidentifiable.7,8 Prescription drug monitoring programs (PDMPs) were designed to monitor scheduled drugs prescribed to patients9 but no equivalent system exists for illicit drugs. Harm reduction organizations have started to implement community-based drug checking as a local strategy for obtaining timely information on substances sold in local markets; however, these efforts have yet to produce publicly available data with the breadth and scope needed for state or national level analyses. At present, information collected on illicit drugs originates solely from law enforcement agencies whose crime laboratories test drug items confiscated during arrests.10
Numerous states have begun making drug exhibit data available to the public. CDC11 has endorsed using drug reports in predictive models12 and, in a joint investigation with Ohio, has demonstrated the usefulness of this approach.13 Several recent studies have found strong correlations between concurrent trends in drug reports and opioid-involved overdose deaths (OOD).14 Zibbell et al. (2019)15 and Rosenblum et al. (2020)16 found statistically significant associations in Ohio between increases in FFRC reports and OOD involving IMF. To our knowledge, there have been limited studies at the national level that analyze the relationship between law enforcement drug exhibits and opioid overdose deaths.
The National Forensic Laboratory Information System (NFLIS) provides researchers with the capacity to analyze national data.17 NFLIS-Drug is the US Drug Enforcement Administration’s (DEA’s) program for systematically collecting analysis results from drug cases submitted to and analyzed by a near-census of all US forensic laboratories. DEA primarily uses NFLIS-Drug data to support its drug scheduling mission and threat assessments and publishes estimates from the NFLIS-Drug data in annual and midyear reports.18 The current study examines national data from a six-year period (2014–2019). Our main objective is to demonstrate how fluctuations in the illicit drug supply correlate with opioid overdose mortality rates. A broader goal of ours is to demonstrate how the opioid epidemic’s evolution from an iatrogenic prescription opioid crisis to a fentanyl-by-way-of-heroin epidemic was facilitated by these waves of supply.19
Methods
This observational study examines associations between forensic laboratory drug reports and OOD for the US from 2014 to 2019. Two assumptions underpin study analyses. First, confiscated drugs tested by crime laboratories can serve as reasonable proxies for drugs circulating in illicit markets. We hypothesize that changes in the type and quantity of drugs reflected in NFLIS-Drug data parallel changes in the composition and scale of the illicit drug supply. Second, informed by previous research,15 we believe that increases in the IMF supply within a state are likely to lead to increases in OOD in that state. Both assumptions recognize that law enforcement interdiction efforts and the types of drugs in illicit markets vary across geography and time. Accordingly, we constructed quarterly, state aggregates of detailed drug exhibit information from NFLIS-Drug that reflect different categories of opioids, stimulants, and benzodiazepines and merged them with OOD per capita counts for the same state and calendar-quarter. We present national estimates but our primary analysis is state level by quarter. Since NVSS and NFLIS-Drug are de-identified public databases, the study was deemed exempt from review by the Research Triangle Institute’s Institutional Review Board. All STROBE checklist items are included for observations studies.
Data and measures
We used overdose death data for 2014–2019 from CDC’s National Vital Statistics System (NVSS), specifically the restricted-use multiple cause of death files,20 which include data for all 50 US states and the District of Columbia. Each death record includes data on the decedent’s sex, age, race, county and state of residence, month and year of death, and county and state of death. Deaths are categorized by the following International Classification of Diseases, 10th revision (ICD-10), cause-of-death codes: unintentional (X40–X44), suicide (X60–X64), homicide (X85), or undetermined intent (Y10–Y14). ICD-10 codes for opioid-involved overdose deaths comprise T.40.0–T40.4 and T40.6 (Table 1). T40.4 (other synthetic narcotics) includes IMF.21 Cocaine- (T40.5), psychostimulants- (T43.6), and benzodiazepine-involved (T42.4) deaths were also identified (Supplementary Table S1).
Table 1.
Opioid-involved overdose deaths by specific drugs with and without synthetic opioids, US, 2014–2019.
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|
| # Opioid-involved fatal overdoses (T40.0, T40.1, T40.2, T40.3, T40.4, T40.6) | 28,723 | 33,204 | 42,435 | 47,885 | 47,096 | 50,179 |
| #(%) Heroin (T40.1) | 10,610 (36.9) | 13,051 (39.3) | 15,551 (36.6) | 15,594 (32.6) | 15,102 (32.1) | 14,116 (28.1) |
| #(%) Heroin (T40.1); no Synthetic Opioid (T40.4) | 9581 (33.4) | 10,358 (31.2) | 9745 (23.0) | 7444 (15.5) | 5981 (12.7) | 5313 (10.6) |
| #(%) Prescription Opioid (T40.2) | 12,187 (42.4) | 12,747 (38.4) | 14,534 (34.3) | 14,560 (30.4) | 12,620 (26.8) | 11,942 (23.8) |
| #(%) Prescription Opioid (T40.2); no Synthetic Opioid (T40.4) | 3181 (11.1) | 3030 (9.1) | 2828 (6.7) | 2423 (5.1) | 2138 (4.5) | 1775 (3.5) |
| #(%) Synthetic Opioid (T40.4) | 5561 (19.4) | 9610 (28.9) | 19,500 (46) | 28,660 (59.9) | 31,525 (66.9) | 36,603 (72.9) |
| #(%) Stimulant (T40.5, T43.6) | 5023 (17.5) | 6634 (20.0) | 10,302 (24.3) | 14,574 (30.4) | 16,314 (34.6) | 19,365 (38.6) |
| #(%) Cocaine (T40.5) | 3431 (11.9) | 4529 (13.6) | 7321 (17.3) | 10,218 (21.3) | 10,986 (23.3) | 12,108 (24.1) |
| #(%) Cocaine (T40.5); no Synthetic Opioid (T40.4) | 2798 (9.7) | 2979 (9.0) | 3101 (7.3) | 2906 (6.1) | 2253 (4.8) | 1875 (3.7) |
| #(%) Psychostimulant (T43.6) | 1813 (6.3) | 2366 (7.1) | 3446 (8.1) | 5239 (10.9) | 6466 (13.7) | 8716 (17.4) |
| #(%) Psychostimulant (T43.6); no Synthetic Opioid (T40.4) | 1536 (5.3) | 1871 (5.6) | 2398 (5.7) | 2678 (5.6) | 2831 (6.0) | 3106 (6.2) |
| #(%) Benzodiazepine (T42.4) | 6749 (23.5) | 7500 (22.6) | 9261 (21.8) | 10,038 (21.0) | 9166 (19.5) | 8330 (16.6) |
| #(%) Benzodiazepine (T42.4); no Synthetic Opioid (T40.4) | 5523 (19.2) | 5699 (17.2) | 5946 (14.0) | 5150 (10.8) | 4082 (8.7) | 3125 (6.2) |
Notes: Data are from the restricted-use, multiple cause-of-death mortality files from the National Vital Statistics System (NVSS) and cover all 50 states and DC. Drug categories are not mutually exclusive.
NFLIS-Drug contains information on drugs seized and submitted to and tested by public laboratories nationwide.22 We flagged drug reports involving opioids (heroin, prescription opioids, fentanyl and fentanyl-related compounds [FFRC]), stimulants (cocaine, methamphetamine, other stimulants [e.g., methylphenidate]), and benzodiazepines (Table 1 and Supplementary Table S2). Each case, which may contain one or more items for testing, is categorized by the state, submitting agency, and laboratory submission date. Although a case may include more than one identified item, it should be noted that NFLIS-Drug data capture drugs co-reported within the same item. NFLIS-Drug data does not mean that the drugs were mixed or combined. The NFLIS-Drug participation rate, defined as the percentage of the national drug caseload represented by laboratories that have joined NFLIS, is greater than 98%. The NFLIS-Drug reporting rate, defined as the percentage of the national drug caseload represented by laboratories reporting to NFLIS-Drug, is greater than 97%. Since its inception, the laboratory retention rate for NFLIS-Drug participation has exceeded 99%.
Counts of OOD were aggregated for each state, month, quarter, and year. Separate counts were constructed for each drug category and combinations of categories (e.g., OOD with co-occurring cocaine). Counts of drug reports were similarly aggregated by state, month, quarter, or year. To characterize the relative scale of different types of drugs in OOD and reports, we calculated the percentage each drug represented (e.g., percentage of OOD with cocaine present). For NFLIS-Drug reports, we calculated percentages for the total number involving at least one drug from the opioid, stimulant, or benzodiazepine drug classes. Notably, the submission date for laboratory testing is likely not the same day when the drug was confiscated as lags often occur between law enforcement seizure and laboratory drug testing.23 The frequency of drug confiscations may be highly variable within short time periods, especially in less-populated areas. We therefore use state and quarter-level variables in our statistical models (N = 1224).
Two distinct identifiers are used to categorize OOD and drug reports. DEA employs the term fentanyl and fentanyl-related compounds (FFRC) to describe a comprehensive category that includes fentanyl and fentanyl analogs (e.g., carfentanil) in addition to fentanyl precursor compounds (e.g., 4-anilino-N-phenethylpiperidine [ANPP]) and chemical intermediaries used in manufacturing (e.g., norfentanyl) [Supplementary Table S3]. Furthermore, forensic laboratories do not indicate whether reported fentanyl is licitly or illicitly manufactured. Thus, diverted pharmaceuticals are not distinguished from illicitly manufactured drugs. In contrast, CDC uses the term illicitly manufactured fentanyls (IMF) to classify overdose deaths that involve non-prescription fentanyl and/or fentanyl analogs and to distinguish those involving prescription fentanyl. The current study maintains these respective terms and categories to be consistent with each agency’s nomenclature. This distinction recognizes that FFRC confiscated by law enforcement and analyzed by crime laboratories are the very substances involved in OOD as demonstrated by the strong association between FFRC reports and IMF-involved OOD described in this manuscript.
Data analysis
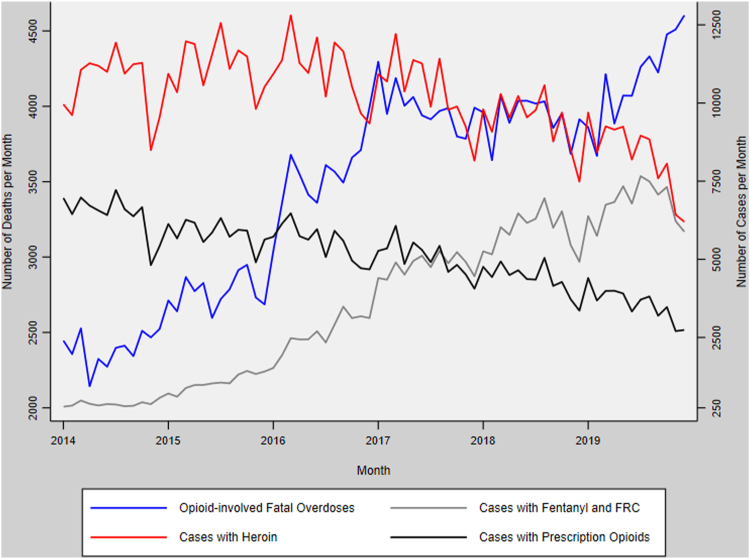
The number of OOD in the US is presented by year and the number and percentage of deaths that involved other drugs or drug combinations. Percentages of specific drugs or drug categories are based on the total number of drug reports with at least one opioid, stimulant, or benzodiazepine. US monthly counts of OOD over time are presented with counts of FFRC, heroin, and prescription opioid reports in Fig. 1.
Fig. 1.
Opioid-involved overdose deaths and NFLIS-Drug reports with fentanyl and fentanyl-related compounds (FFRC), heroin, and prescription opioids, United States, 2014–2019.
We used a two-way fixed effects (TWFE) model to estimate contemporaneous and lagged associations of drug reports and OOD. This approach is conventionally used to reduce bias from unobserved differences in state characteristics and heterogenous effects of different time periods.24,25 In the primary specification, OOD counts were a function of the number of heroin, prescription opioid, FFRC, methamphetamine, cocaine, and benzodiazepine reports per 100,000 reports by state and quarter. For TWFE estimation, fixed effects for state and fixed effects for each quarter since the beginning of 2014 were also included as control variables. A Poisson regression was used because deaths and deaths per 100,000 were skewed right and based on counts. Although overdispersion was marginal (<1.2), we also estimated negative binomial models and found results virtually the same as Poisson’s. We chose to report for Poisson models because of their stable solutions in all sensitivity analyses. State populations were used as the exposure variables in the models to yield per capita estimates (incidence rate ratios [IRRs]) and robust standard errors were used.26 Analysis were conducted using Stata 16.1 and xtpoisson specifically for the models. To improve interpretability, the IRRs were transformed into percentage differences.
Sensitivity analyses
Our primary model relates state trends in drug reports and OOD for the same calendar quarter. Relating drug reports to overdose deaths reflects real-world context because the types of drugs confiscated from illicit markets are comparable to drugs consumed by decedents. The current analysis is ecological because confiscated drugs reports reported to NFLIS-Drug are not the actual drugs involved in OOD. The date seized drugs are submitted to crime laboratories for testing may be delayed from the time when the confiscation occurred, which may extend the timeframe for reporting. To account for delays in reporting, we performed a sensitivity analysis to estimate single lag models in which the independent variables are reports from the previous quarter rather than from the contemporaneous quarter.
One challenge to this hypothesis—that trends in the number of drug reports correlate proportionally with the changing quantities of those drugs in the market—is that law enforcement efforts may change in ways that confound estimates. For example, law enforcement agencies may increase the number of drug searches in response to increasing overdose deaths. In a second sensitivity analysis we replaced drug report counts per capita measures with drug case percentage measures. The new specification used the percentage of all reports (involving opioids, stimulants, or benzodiazepines) in a state and calendar-quarter found to each drug. We also included the total number of drug reports as a control variable. In contrast to report counts, estimates for the percentages of drug reports are independent of the scale of law enforcement efforts in a state and quarter and may better reflect the relative supply of each drug.
Finally, states with smaller populations often have fewer OOD, a smaller supply of certain drugs, and forensic laboratory drug reports compared with more populated states.27 Although our main results are representative of the whole US, low-event states can make estimates from models of per capita deaths less relevant to states with larger populations. To provide alternative estimates, we re-estimated models by excluding states with either less than 1000 total OOD or less than 10,000 total opioid, stimulant, and benzodiazepine reports from 2014 to 2019.
Role of the funding source
The funders/sponsors had no role in the design and conduct of the study; acquisition, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Results
Opioid-involved overdose deaths (OOD)
There were 249,522 OOD in the US between 2014 and 2019, with the annual number nearly doubling from 28,723 in 2014 to 50,179 in 2019 (Table 1). Heroin (36.9%, 10,610/28,723) and prescription opioids (42.4% [12,187/28,723]) were the most prevalent opioids in 2014 but fell as a percentage of all deaths in 2019 (to 28.1% [14,116/50,179] and 23.9% [11,942/50,179], respectively). Meanwhile, overdose deaths involving IMF increased substantially, from 19.4% (5561/28,723) in 2014 to 72.9% (36,603/50,179) in 2019; by 2019, a majority of heroin- (62.4% [8803/14,116]) and prescription opioid-involved deaths had co-occurring IMF 85.1% [10,167/11,942]). Both opioid- and stimulant-involved deaths increased over the six-year study period but only when IMF was involved. For example, cocaine’s co-involvement in OOD more than doubled from 2014 to 2019 (from 11.9% [3431/28,723] to 24.1% [12,108/50,179]). Yet, when cocaine-involved overdose deaths with co-occurring IMF are excluded, the trend in cocaine-involved deaths decreases from 9.7% [2798/28,723] to 3.7% [1875/50,179], respectively, as does the overall number of drug overdose deaths without IMF.
National Forensic Laboratory Information System (NFLIS-drug)
From 2014 to 2019, there were 3,817,438 drug reports in the US in which an opioid, stimulant, and/or benzodiazepine was detected by local and state crime laboratories and reported to NFLIS-Drug (Table 2). Overall, drug reports involving any opioid (i.e., prescription opioids, heroin, FFRC) decreased slightly, from 203,114 in 2014 to 182,389 in 2019, while reports involving FFRC increased dramatically, from 4495 to 81,471 over the same time period. In 2019, 12.2% (81,417/670,515 reports) of drug reports in which an opioid, stimulant, and/or benzodiazepine was detected involved an FFRC. Illicit stimulants were the largest category of reports and their involvement increased over the six-year period, from 63.9% (359,742/562,732) in 2014 to 76.8% (514,933/670,515) in 2019. This increase was driven primarily by methamphetamine, which was identified in slightly more than half (53.8% [360,791/670,515]) of all drug reports in which an opioid, stimulant, and/or benzodiazepine was detected in 2019.
Table 2.
Counts of Cases involving specific drugs, US, 2014–2019.
| Drug | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|
| # NFLIS Cases (Opioids, Stimulants and Benzodiazepines) | 562,732 | 583,892 | 629,441 | 676,699 | 694,159 | 670,515 |
| #(%) Opioids (Heroin, Prescription Opioids, and Fentanyl and Fentanyl-Related Compounds) | 203,114 (36.1) | 205,940 (35.3) | 210,091 (33.4) | 208,090 (30.8) | 194,031 (28.0) | 182,389 (27.2) |
| #(%) Heroin | 127,523 (22.7) | 134,418 (23.0) | 132,786 (21.1) | 125,203 (18.5) | 113,260 (16.3) | 100,029 (14.9) |
| #(%) Prescription Opioids | 77,184 (13.7) | 70,088 (12.0) | 66,595 (10.6) | 60,715 (9.0) | 52,542 (7.6) | 42,941 (6.4) |
| #(%) Fentanyl and Fentanyl-Related Compounds | 4495 (0.8) | 12,763 (2.2) | 31,670 (5.0) | 57,721 (8.5) | 71,039 (10.2) | 81,471 (12.2) |
| #(%) Stimulants | 359,742 (63.9) | 382,238 (65.5) | 426,498 (67.8) | 482,474 (71.3) | 518,796 (74.7) | 514,933 (76.8) |
| #(%) Cocaine | 161,303 (28.7) | 158,308 (27.1) | 163,547 (26.0) | 179,719 (26.6) | 175,396 (25.3) | 156,320 (23.3) |
| #(%) Methamphetamine | 192,459 (34.2) | 219,175 (37.5) | 259,859 (41.3) | 301,930 (44.6) | 343,537 (49.5) | 360,791 (53.8) |
| #(%) Other Stimulants | 12,122 (2.2) | 12,240 (2.1) | 12,967 (2.1) | 13,122 (1.9) | 12,883 (1.9) | 11,342 (1.7) |
| #(%) Benzodiazepines | 46,389 (8.2) | 49,152 (8.4) | 56,417 (9.0) | 53,789 (7.9) | 46,745 (6.7) | 36,232 (5.4) |
Notes: Data are from the Drug Enforcement Administrations' National Forensic Laboratory Information System (NFLIS) for all 50 states and D.C. Labs may test and identify more than one drug for a single case; drug counts are not mutually exclusive. Other Stimulants primarily comprise prescription stimulants (93.9%).
Opioid-involved overdose deaths (OOD) and NFLIS-drug reports
Nationally, both the monthly number of FFRC reports from NFLIS-Drug and the monthly number of OOD increased substantially from 2014 to 2019. These synchronized patterns correspond visually as both short-term (quarter-to-quarter) changes and as broad trends (year-to-year) save an anomalous divergence in late 2019 (Supplementary Fig. S1). In contrast, monthly reports of heroin and prescription opioids fell consistently and did not track with increasing OOD over the study’s six years. Descriptive statistics for the state-quarter variables used in the statistical models are presented (Supplementary Table S4). An average of 203.9 OOD was reported across all states and during all quarters from 2014 to 2019, with a quarterly overdose mortality rate of 3.5 per 100,000 persons (corresponding to an annual rate of 13.9). The number of reports per quarter containing opioids, stimulants, or benzodiazepines averaged 3118.8, of which methamphetamine was the most frequently identified drug (45.2% [1409/3118]), followed by cocaine (23.5% [732/3118]), heroin (21.8% [679/3118]), and prescription opioids (10.4% [324/3118]). The average quarterly percent of reports containing opioids, psychostimulants, or benzodiazepines with FFRC was lower (7.7% [244/3118]) reflecting its negligible presence in 2014 (<2.0% of reports [4495/562,732]) before growing to nearly 14% (460/3286) in 2019.
Model results
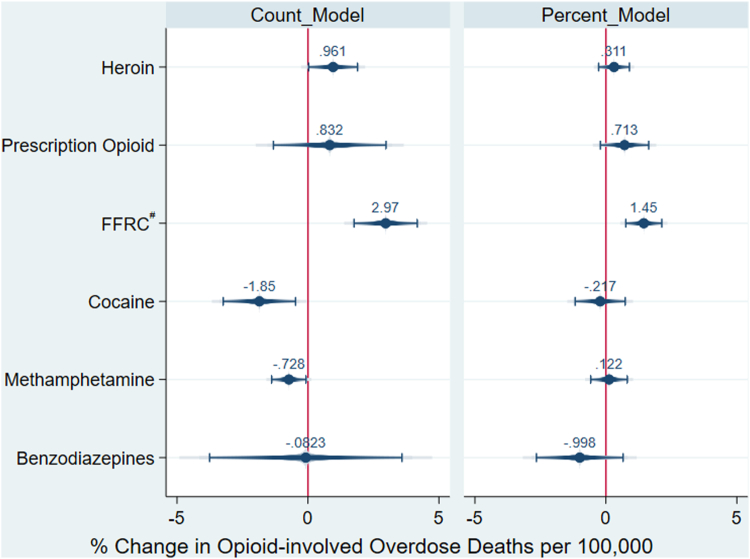
Results from the TWFE models of associations between OOD per 100,000 persons and laboratory-tested reports with selected drugs are presented (Fig. 2). Results are presented for all states and results for both report count and drug report percentage models are shown. Full model results (as IRRs) are offered and include sensitivity analyses (Supplementary Tables S5 and 6). The count of FFRC reports has the largest association with OOD. The IRR (1.03, 95% CI: 1.02, 1.04) translates to one additional FFRC drug report per 100,000 reports correlated with 2.97% (95% CI: 1.7%, 4.1%) more OOD per 100,000 persons per quarter. Heroin reports were also found associated OOD, with an additional 0.961% (95% CI: .028%, .189%) OOD per 100,000 persons per quarter. Contrastingly, NFLIS-Drug reports of methamphetamine (−0.7%; 95% CI: −1.3%, −.001%) and cocaine (−1.8%; 95% CI: −3.2%, −.004%) were negatively associated with OOD but with a smaller magnitude than FFRC reports. These findings are consistent across the lag, subgroup, and later period sensitivity analyses, and the percentage of reports shows similar patterns of association for all NFLIS-Drug report variables; however, only FFRC reports remained statistically significant (IRR = 1.015; 95% CI: 1.008, .0217)). For the reports’ percentage models, the association between FFRC reports and OOD translates to a 1.5% (95% CI: .008%, .0215%) increase in the OOD rate per 100,000 persons per quarter for each percentage-point increase in FFRC reports (as a share of all drug reports).
Fig. 2.
Percentage change in opioid-involved overdose deaths per 100,000 persons, United States, 2014–2019∗. ∗Results for law enforcement drug exhibits from state-quarter difference-in-differences models. #Fentanyl and fentanyl-related compounds.
Discussion
This study examined associations between forensic laboratory drug reports and OOD in the entire US from 2014 to 2019. Because no existing PDMP tracks the distribution of illicit drugs, we used drug report data from NFLIS-Drug as proxy indicators for the illicit drug supply. By integrating OOD data from the NVSS with drug report data from NFLIS-Drug, we demonstrate a number of significant associations between a changing illicit drug supply and an increasing opioid overdose mortality in the US.
Our most notable finding is that increasing FFRC reports were the strongest predictor of OOD over the six-year period; each additional FFRC report was associated with an increase of 2.97% more OOD per 100,000 persons per quarter. The strong association between FFRC reports and IMF-involved overdose deaths suggests that the national surge in opioid overdose mortality from 2014 to 2019 was facilitated by sharp increases in the FFRC supply. This national-level finding is consistent with national28 and state evidence15,16,29 from comparable analyses covering the same 6-year study period. In aggregate, a growing body of national and state-level evidence confirms that IMF has been the key driver of overdose mortality since its emergence in 2013.5
No comparable association with OOD was found for reports of prescription opioids or heroin. These findings are consistent with CDC reports30,31 showing steady declines in the number of OOD involving prescription opioids and heroin from 2014 to 2019. These inverse trends illustrate how changes in the market share of prescription opioids, heroin, and IMF contributed to corresponding changes in overdose mortality. More broadly, these supply-side trends show how a surging supply of FFRC radically transformed the illicit opioid supply by displacing heroin as the predominant opioid on the illicit market. These findings provide supply-side evidence that further establishes the opioid epidemic as a national crisis whose deadly arc for more than two decades has been facilitated by a radical transformation of America’s illicit opioid supply.2,32
Also notable are the substantial increases in NFLIS-Drug reports and OOD involving cocaine and methamphetamine. In sharp contrast to our main finding, no concomitance was found between illicit stimulant reports and illicit stimulant overdose deaths. Illicit stimulants comprised the largest category of all NFLIS-Drug reports from 2014 to 2019 and the number of cocaine and methamphetamine reports far surpassed reports of FFRC. Methamphetamine accounted for the majority of illicit stimulant reports over the six years and appeared in slightly more than half of reports in which an opioid, stimulant, and/or benzodiazepine was detected in 2019, but this growth in methamphetamine reports did not correlate with surging methamphetamine deaths. A surging illicit stimulant supply with no correlation to drug overdose mortality suggests that the sharp increases in stimulant-involved deaths were facilitated by a growing supply of FFRC and not by increases in the supply of cocaine and methamphetamine. These findings suggest that America’s illicit stimulant crisis is not a crisis of mortality,29 as has been reported,33 but a mounting morbidity crisis involving surging cases of mental illness and stimulant use disorder along with growing infectious disease and soft tissue infections.34
Lastly, current study findings demonstrate NFLIS-Drug’s usefulness for research that requires proxy indicators for the illicit drug supply. By merging NFLIS-Drug data with OOD using per capita counts of reports and deaths for the same state and calendar-quarter, the current study validates NFLIS-Drug as having the capacity to demonstrate associations between trends in illicit drug supply and drug overdose mortality. This capacity is consistent with a recent national-level study that used NFLIS and OD data from 2018 to 2019 and showed NFLIS’s important surveillance potential.28 The current study expands NFLIS’s potential for surveillance by showing concrete relationships between concurrent trends in drug exhibits and OD deaths. At present, NFLIS-Drug is the largest national-level, publicly available database on laboratory-tested illicit drugs sold in unlawful markets. By providing current researchers with the capacity to examine supply-side impacts on drug overdose mortality in all 50 US states and the District of Columbia, our study findings establish NFLIS-Drug as a national data system that can be used to track illicit drugs and highlight supply-side impacts on drug overdose mortality.
Limitations
This study involves a number of notable limitations. First, it is observational. Although the TWFE models reduce confounding from unobserved time invariant state-level factors (including measurement error) and nationwide quarter and time trend factors, dynamic relationships within states over time may bias our estimates. At a minimum, measurement error in reporting agencies attenuate our model estimates but could also lead to spurious correlation if the form of the measurement error changes over time. Moreover, there may be some confounding from omitted time varying variables such as changes in federal policies. We note that our interpretation of the results depends on the assumption that all individuals at risk of a fatal overdose are equally exposed to changes in state-aggregated features of the illicit drug supply. However, the current analysis does not rule out the possibility that aggregate changes are driven by certain geographic regions within a state that are not the same regions in which the overdose deaths are occurring. Although decedent data are available at the county level, the reporting agencies for drug exhibits do not easily map to concrete geographic areas within a state. In contrast, the TWFE estimates could also be biased due to drug supply factors in neighboring states. Second, although current study findings were robust when estimating lagged models (i.e., previous quarter’s reports predicting current quarter OODs), omitted variables may explain trends in both drug reports and OODs. Third, substantial time lags occur in the processing of drug reports submitted to and analyzed by crime laboratories. Time lags from when a drug is confiscated to when it is tested and reported by crime laboratories make NFLIS-Drug fairly inefficient for timely analysis and rapid response; despite this limitation, NFLIS-Drug has been lauded as the timeliest national resource for chemically verified drug data.35 Time constraints can serve as critical impediments when, for example, overdose prevention programs want to use NFLIS-Drug to monitor unsafe substances in communities to direct timely response. Time lags are less of a concern for retrospective analyses like the current study and may be more problematic for prospective analyses or direct interventions because time lags are not conducive to rapid response. Fourth, NFLIS-Drug coverage, while comprehensive and representing greater than 97% of the national drug caseload by reporting laboratories, is not 100% due, in part, to heterogeneity in the consistency of reporting and testing across agencies and even within agencies over time. Moreover, testing and identification of FFRC may have lagged in some agencies during the first few years of the fentanyl wave (2013–2015), before law enforcement agencies recognized IMF in drug reports and prior to crime laboratories systematically testing for IMF. Additionally, while NFLIS-Drug is based on a nationally and regionally representative sample and has evolved into a near-census of forensic laboratories in the US., data provided by laboratories are influenced by samples submitted for testing by law enforcement. This process reflects agencies’ priorities and practices and further determined by prevailing discourses in addition to the effectiveness of drug distributors to avoid detection.36 Finally, and most important to the overdose epidemic, NFLIS-Drug does not capture whether a confiscated substance was mixed with other drugs at the point of confiscation. Stated differently, NFLIS-Drug reports are not counts of true combinations (e.g., mixed powders) but separate drugs reported together as a single item. For example, a sealed bag of heroin found alongside a sealed bag of fentanyl in a backpack could be considered a single item by a participating laboratory and reported as two substances within that item.37 This reporting technique does not allow for investigations into adulterated or contaminated drugs (e.g., fentanyl-adulterated heroin) and can lead unwitting researchers to misinterpret findings or present erroneous depictions of confiscated drugs (e.g., a NFLIS-Drug report identifying cocaine and fentanyl that is reported by researchers as fentanyl-adulterated cocaine).38 Still, the presence of each particular laboratory-tested substance is known and reports of all drugs present are known within an individual case.
Conclusion
This study uses NFLIS-Drug data as proxy indicators for trends in the illicit drug supply to better understand supply-side drivers of overdose mortality. With the unprecedented lethality of IMF and growing use of tranquilizing anesthetics (e.g., xylazine39, 40, 41) and benzimidazole opioids (i.e., nitazenes42,43) as adulterants of illicit opioids, there is urgent need for an improved system.44 Ideally, a system that can distinguish between individually packaged drugs and adulterated supplies. Systems that rely solely on blood and urine toxicology (e.g., CDC’s Drug Overdose Surveillance and Epidemiology [DOSE] system) are similarly unable to determine whether two drugs were taken as separate doses or combined within a single formulation. They also have difficulty identifying unknown or novel synthetic drugs and have shown serious limitations in their ability to identify emerging drug threats (e.g., the IMF crisis) in a timely manner. Recent advances in community-based drug checking represent growing capacity for timely monitoring of illicit drug markets at the local level.45 To further boost NFLIS-Drug’s effectiveness, DEA could pair StarLIMS, a replacement of STRIDE (System to Retrieve Information from Drug Evidence), with NFLIS-Drug to expand surveillance capacity to include adulterants, diluents, fillers, and their proportions.46 This capacity would strengthen public health surveillance of new and emerging drugs and provide timely and actionable information to identify emerging threats before becoming public health crises; it would also augment NFLIS-Drug’s Snapshot Report Series, which highlights new drugs reported to DEA on a quarterly basis. A concerted effort between public health and public safety to expand NFLIS-Drug’s capacity can help strengthen America’s public health response to the widespread contamination of the illicit drug supply and save lives.
Contributors
JZ and AA conceived of the study. JZ, AA, MG, HSM contributed to the study design. AA and DH conducted the data analysis. JZ, MG and DH verified the data. JZ, AA and SDC drafted the manuscript. All coauthors critically revised the manuscript and approved the final version to be published.
Data sharing statement
Mortality data from NVSS and NFLIS-Drug data from DEA are both publicly available for access.
Declaration of interests
All authors signed an Author Statement Form and completed an individual ICMJE COI Form. No authors have declared any relevant conflicts of interest.
Acknowledgements
Funding: This study was supported in part by Arctic Slope Mission Services, LLC, ASMS Contract No. ASM5-00017. In addition, this study was also supported by funding from grants DA046444 and DA047334 from the US National Institutes of Health, National Institute on Drug Abuse to Dr Zibbell (PI).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100569.
Appendix A. Supplementary data
References
- 1.CDC. National Center for Health Statistics U.S. overdose deaths in 2021 increased half as much as in 2020 – but are still up 15% 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm [updated 2022; cited 2022 Jul 10]; Available from:
- 2.Zibbell J.E. The latest evolution of the opioid crisis: changing patterns in fentanyl adulteration of heroin, cocaine, and methamphetamine and associated overdose risk. Insights. RTI International. 2019. https://www.rti.org/insights/latest-evolution-opioid-crisis-changing-patterns-fentanyl-adulteration-heroin-cocaine-and Available from:
- 3.Centers for Disease Control and Prevention Vital signs: overdoses of prescription opioid pain relievers---United States, 1999--2008. MMWR Morb Mortal Wkly Rep. 2011;60:1487–1492. [PubMed] [Google Scholar]
- 4.Jones C.M., Logan J., Gladden R.M., Bohm M.K. Vital signs: demographic and substance use trends among heroin users - United States, 2002-2013. MMWR Morb Mortal Wkly Rep. 2015;64:719–725. [PMC free article] [PubMed] [Google Scholar]
- 5.O'Donnell J., Tanz L.J., Gladden R.M., Davis N.L., Bitting J. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls - United States, 2019-2020. MMWR Morb Mortal Wkly Rep. 2021;70:1740–1746. doi: 10.15585/mmwr.mm7050e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Donnell J., Gladden R.M., Kariisa M., Mattson C.L. Using death scene and toxicology evidence to define involvement of heroin, pharmaceutical morphine, illicitly manufactured fentanyl and pharmaceutical fentanyl in opioid overdose deaths, 38 states and the District of Columbia, January 2018-December 2019. Addiction. 2022;117:1483–1490. doi: 10.1111/add.15768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institute of Standards and Technology (NIST) Novel psychoactive substance (NPS) data. 2018. https://www.nist.gov/programs-projects/novel-psychoactive-substance-nps-data-hub [updated 2018; cited 2022 Jul 10]; Available from:
- 8.Verkouteren J.R., Staymates J.L. Reliability of ion mobility spectrometry for qualitative analysis of complex, multicomponent illicit drug samples. Forensic Sci Int. 2011;206:190–196. doi: 10.1016/j.forsciint.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Martin H.D., Modi S.S., Feldman S.S. Barriers and facilitators to PDMP IS Success in the US: a systematic review. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108460. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Drug Enforcement Administration (DEA) 2013 survey of crime laboratory drug chemistry sections. NFLIS. 2014. https://www.nflis.deadiversion.usdoj.gov/publicationsRedesign.xhtml [updated 2014; cited 2022 Jul 10]; Available from:
- 11.Gladden R.M., Martinez P., Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65:837–843. doi: 10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- 12.Hall O.E., Trent Hall O., Eadie J.L., et al. Street-drug lethality index: a novel methodology for predicting unintentional drug overdose fatalities in population research. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peterson A.B., Gladden R.M., Delcher C., et al. Increases in fentanyl-related overdose deaths - Florida and Ohio, 2013-2015. MMWR Morb Mortal Wkly Rep. 2016;65:844–849. doi: 10.15585/mmwr.mm6533a3. [DOI] [PubMed] [Google Scholar]
- 14.Ray B., Korzeniewski S.J., Mohler G., et al. Spatiotemporal analysis exploring the effect of law enforcement drug market disruptions on Overdose, Indianapolis, Indiana, 2020-2021. Am J Publ Health. 2023;113(7):750–758. doi: 10.2105/AJPH.2023.307291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zibbell J.E., Aldridge A.P., Cauchon D., DeFiore-Hyrmer J., Conway K.P. Association of law enforcement seizures of heroin, fentanyl, and carfentanil with opioid overdose deaths in Ohio, 2014-2017. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.14666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenblum D., Unick J., Ciccarone D. The rapidly changing US illicit drug market and the potential for an improved early warning system: evidence from Ohio drug crime labs. Drug Alcohol Depend. 2020;208 doi: 10.1016/j.drugalcdep.2019.107779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Drug Enforcement Administration (DEA) U.S. Drug Enforcement Administration, NFLIS; Springfield, VA: 2019. NFLIS brief: toxicology testing practices for opiates and opioids across the nation.https://www.nflis.deadiversion.usdoj.gov/publicationsRedesign.xhtml [updated 2019; cited 2022 Jul 10]; Available from: [Google Scholar]
- 18.U.S. Drug Enforcement Administration (DEA) U.S. Drug Enforcement Administration, Diversion Control Division; Springfield, VA: 2021. National forensic laboratory information system: NFLIS-drug 2020 midyear report.https://www.nflis.deadiversion.usdoj.gov/nflisdata/docs/13915NFLISdrugMidYear2020.pdf [updated 2021; cited 2022 Jul 10]; Available from: [Google Scholar]
- 19.Fischer B., Pang M., Jones W. The opioid mortality epidemic in North America: do we understand the supply side dynamics of this unprecedented crisis? Subst Abuse Treat Prev Policy. 2020;15:14. doi: 10.1186/s13011-020-0256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CDC. National Center for Health Statistics. National Vital Statistics System Restricted-use vital statistics data. 2022. https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm [updated 2022; cited 2021 Mar]; Available from:
- 21.Hedegaard H., Bastian B.A., Trinidad J.P., Spencer M., Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011-2016. Natl Vital Stat Rep. 2018;67:1–14. [PubMed] [Google Scholar]
- 22.Pressley D., Moore K., Weimer B., Smiley-McDonald H., Ropero-Miller J. National forensic laboratory information system. Forensic Sci Rev. 2018;30:83–87. doi: 10.1111/1556-4029.15269. [DOI] [PubMed] [Google Scholar]
- 23.Strom K.J., Hickman M.J., Smiley-McDonald H.M., Ropero Miller J., Stout P.R. Crime laboratory personnel as criminal justice decision-makers: a study of controlled substance case processing in ten jurisdictions. Forensic Sci Pol Manag. 2011;2:57–69. [Google Scholar]
- 24.Goldstein H. John Wiley & Sons; 2011. Multilevel statistical models. Online ISBN:9780470973394. [DOI] [Google Scholar]
- 25.Dowell D., Zhang K., Noonan R.K., Hockenberry J.M. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood) 2016;35:1876–1883. doi: 10.1377/hlthaff.2016.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen W., Qian L., Shi J., Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18:63. doi: 10.1186/s12874-018-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Drug Early Warning System (N-DEWS) The NIDA-funded NDEWS coordinating center at UF. National Institutes of Health. 2022. https://ndews.org/ [updated 2022; cited 2022 Jul 10]; Available from:
- 28.Sumner S.A., Bowen D., Holland K., et al. Estimating weekly national opioid overdose deaths in near real time using multiple proxy data sources. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.23033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zibbell J.E., Clarke S.D., Kral A.H., Richardson N.J., Cauchon D., Aldridge A. Association between law enforcement seizures of illicit drugs and drug overdose deaths involving cocaine and methamphetamine, Ohio, 2014-2019. Drug Alcohol Depend. 2022;232 doi: 10.1016/j.drugalcdep.2022.109341. [DOI] [PubMed] [Google Scholar]
- 30.Scholl L., Seth P., Kariisa M., Wilson N., Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419–1427. doi: 10.15585/mmwr.mm675152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.CDC. National Center for Health Statistics. National Vital Statistics System Provisional drug overdose death counts. 2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm [updated 2022; cited 2020 Jun 2]; Available from:
- 32.Duhart Clarke S., Kral A.H., Zibbell J.E. Consuming illicit opioids during a drug overdose epidemic: illicit fentnayls, drug discernment, and the radical transformation of the illicit opioid market. Int J Drug Policy. 2022;99 doi: 10.1016/j.drugpo.2021.103467. PMCID: PMC8755588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kariisa M., Scholl L., Wilson N., Seth P., Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68:388–395. doi: 10.15585/mmwr.mm6817a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Panenka W.J., Procyshyn R.M., Lecomte T., et al. Methamphetamine use: a comprehensive review of molecular, preclinical and clinical findings. Drug Alcohol Depend. 2013;129:167–179. doi: 10.1016/j.drugalcdep.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 35.Morrow J.B., Ropero-Miller J.D., Catlin M.L., et al. The opioid epidemic: moving toward an integrated, holistic analytical response. J Anal Toxicol. 2019;43:1–9. doi: 10.1093/jat/bky049. [DOI] [PubMed] [Google Scholar]
- 36.Pitts W.J., Heller D., Smiley-McDonald H., et al. Understanding research methods, limitations, and applications of drug data collected by the National Forensic Laboratory Information System (NFLIS-Drug) J Forensic Sci. 2023;68(4):1335–1342. doi: 10.1111/1556-4029.15269. [DOI] [PubMed] [Google Scholar]
- 37.U.S. Drug Enforcement Administration (DEA) National Forensic Laboratory Information System, U.S. Drug Enforcement Administration, Office of Diversion Control; Springfield, VA: 2017. Opiates and related drugs reported in NFLIS, 2009–2014.https://www.nflis.deadiversion.usdoj.gov/publicationsRedesign.xhtml [updated 2017; cited 2022 Jul 10]; Available from: [Google Scholar]
- 38.Park J.N., Rashidi E., Foti K., Zoorob M., Sherman S., Alexander G.C. Fentanyl and fentanyl analogs in the illicit stimulant supply: results from U.S. drug seizure data, 2011-2016. Drug Alcohol Depend. 2021;218 doi: 10.1016/j.drugalcdep.2020.108416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kariisa M., Patel P., Smith H., Bitting J. Notes from the field: xylazine detection and involvement in drug overdose deaths—United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70:1300–1302. doi: 10.15585/mmwr.mm7037a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.FDA alerts health care professionals of risks to patients exposed to xylazine in illicit drugs (U.S. Food and Drug Administration) 2022. https://www.fda.gov/drugs/drug-safety-and-availability/fda-alerts-health-care-professionals-risks-patients-exposed-xylazine-illicit-drugs
- 41.Readout of evolving and emerging drug threats committee meeting regarding xylazine. The White House. 2023. https://www.whitehouse.gov/ondcp/briefing-room/2023/01/18/readout-of-evolving-and-emerging-drug-threats-committee-meeting-regarding-xylazine/
- 42.Krotulski A.J., Papsun D.M., Walton S.E., Logan B.K. New synthetic opioid protonitazene increasing in prevalence as “nitazenes” gain traction across the United States and Canada. 2021. https://www.cfsre.org/nps-discovery/public-alerts#:∼:text=New%20Synthetic%20Opioid%20Protonitazene%20Increasing,is%20nationally%20and%20internationally%20controlled [updated 2021; cited 2023 February 21]; Available from:
- 43.Roberts A., Korona-Bailey J., Mukhopadhyay S. Notes from the field: nitazene-related deaths - Tennessee, 2019-2021. MMWR Morb Mortal Wkly Rep. 2022;71:1196–1197. doi: 10.15585/mmwr.mm7137a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta R., Holtgrave D.R. A national tracking system for nonfatal drug overdoses. JAMA. 2022;328:239–240. doi: 10.1001/jama.2022.10815. [DOI] [PubMed] [Google Scholar]
- 45.Masterton W., Falzon D., Burton G., et al. A realist review of how community-based drug checking Services could Be designed and implemented to promote engagement of people who use drugs. Int J Environ Res Publ Health. 2022;19(19) doi: 10.3390/ijerph191911960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Research Council . The National Academies Press; Washington, DC: 2001. Informing America's policy on illegal drugs: what we don't know keeps hurting us. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.