Abstract
Objective
This implementation study aimed to enhance the key elements of clinical practice goal-setting across 5 rehabilitation services.
Design
This study followed a participatory action research approach guided by the Knowledge to Action framework.
Methods
Medical record audits and structured client interviews were conducted prior to and following 12 weeks of implementation, in order to evaluate the success of the goal-setting implementation package.
Results
Medical record audits and interviews conducted pre-implementation (audits n = 132, interviews n = 64), post-implementation (audits n = 130, interviews n = 56) and at 3-month follow-up (audits n = 30) demonstrated varied success across sites. Following implementation 2 sites significantly improved their common goal focus (site 1 p ≤ 0.001, site 2 p = 0.005), these sites also demonstrated a significant increase in clients reporting that they received copies of their rehabilitation goals (site 1 p ≤ 0.001, site 2 p ≤ 0.001). Four sites improved client action planning, feedback and review, and 3 sites enhanced their specificity of goal-setting. At 3-month follow-up 4 sites had continued to improve their common goal focus; however, all sites decreased the specificity of their goal-setting.
Conclusion
Elements of the implementation package were successful at enhancing the goal-setting process; however, how the package is implemented within the team may impact outcomes.
LAY ABSTRACT
There are 4 important elements of goal-setting in rehabilitation: including the client; having a team focus on common goals; setting specific and meaningful goals; and including action planning feedback and review of goals. A goal-setting package was developed to assist healthcare workers to complete all important elements of goal-setting. This study aimed to evaluate the use of the goal-setting package in 5 rehabilitation services. Client medical records were reviewed and interviews with clients were undertaken to evaluate the success of the goal-setting package. In 2 sites, using the goal-setting package resulted in a significant increase in establishing common goals among the client and team and providing written information to clients about their goals. More action plans were developed to assist clients to work towards goals at 4 sites, whilst 3 sites improved in terms of setting more specific goals.
Key words: behaviour change, shared decision-making, goals, implementation science, stroke rehabilitation
Goal-setting is used to enhance client outcomes and autonomy during rehabilitation, by providing motivation, enhancing the specificity of treatment plans, activating therapeutic benefits, such as increased self-awareness, and improving teamwork (1, 2). Key elements of best practice goal-setting include: a common goal focus across team members (3, 4); action planning, feedback and review of goals (2, 5); ensuring goals are meaningful and specific (6); and including the client in shared decision-making (SDM) throughout the goal-setting process (7). Evidence supports each of these 4 key elements of best practice goal-setting; however, these elements are not consistently implemented by clinicians in clinical practice.
Interdisciplinary teamworking, which includes having a common goal focus, has been shown to have a positive impact on functional outcomes for stroke survivors (8). However, a previous study conducted by the authors found that only 31% of goals set by inpatient rehabilitation teams had a common focus amongst the team (2). Furthermore, several studies have investigated clinician’s understanding of SDM in healthcare and, whilst clinicians have been able to demonstrate that they understand the principles of SDM, clinicians are still not implementing SDM principles in clinical practice (9, 10). Previous studies in rehabilitation populations in Queensland, Australia, have found that therapists heavily led the goal-setting process with clients (11). Therefore goals were predominantly focussed on mobility and self-care tasks (12).
For goal-setting to enhance client outcomes and autonomy, processes that address all key elements of goal-setting should be implemented in clinical practice. Given the complexity of goal-setting, the body of research implementing all key ingredients of goal-setting into clinical practice is limited (13, 14). To date, research has focussed predominantly on individual elements of goal-setting, such as setting specific goals, or implementing SDM (15–18). Due to the complexity of implementing all key elements of best practice goal-setting a theoretically informed implementation approach is required to ensure successful implementation in clinical practice (1).
Implementing practice change is challenging (19) and has been shown to be enhanced when interventions are tailored to specific contexts, when implementation is well planned, and when practice change can be supported by a facilitator (20). Approaches to intervention development, such as co-design, can also support teams to overcome barriers in their local context (21). A previous study in this programme of research has outlined the co-design of 6 interventions developed as a goal-setting implementation package to enhance the key elements of best practice goal-setting (Table I) (12).
Table I.
Interventions, purposes and active goal-setting ingredients addressed
| Intervention | Purpose | Materials | Best practice key elements addressed | Sites implementing |
|---|---|---|---|---|
|
Staff education and training Content:
|
Focus of sessions:
|
Training manual, handouts, references and PowerPoint presentations, online resources | Interdisciplinary goal-setting SDM Specific and meaningful goal-setting Action planning, feedback and review |
Inpatient sites 1, 2, 3 Community sites 4, 5 |
|
Keyworker model and workplace instruction Content: Workplace instruction defining role and responsibilities The primary role of the keyworker is to orientate the client to the rehabilitation service and enhance the communication between the interdisciplinary team and the client and family prior to and following case conference meetings. |
To enhance client and family involvement in goal-setting and rehabilitation | Workplace instruction providing description of role and responsibilities | Interdisciplinary goal-setting SDM Specific and meaningful goal-setting Action planning, feedback and review |
Inpatient site 2 Community site 4 |
|
Case conference restructure Content: Background client information, current function, common goal focus, long-term hope/dream goals, client goals for the episode of care, client weekly goals, client actions, staff actions and discharge plans. |
To provide a framework for meaningful interdisciplinary goal-setting and action planning | Workplace instruction Chairing guidelines Electronic template |
Interdisciplinary goal-setting Specific and meaningful goal-setting Action planning, feedback and review |
Inpatient sites 1, 2 |
|
Communication goal and action boards Content: Long-term goals, goals for the episode of care, weekly/short-term goals, client actions and estimated discharge dates |
To enhance client and family involvement in goal-setting and rehabilitation, to enhance the role of the nurse to support action planning | Paper copy | Interdisciplinary goal-setting SDM Action planning, feedback and review |
Inpatient sites 1, 2 |
|
Client workbook Content:
|
To enhance client knowledge and expectations, to provide a framework for staff to facilitate goal-setting and action planning | Editable PDF, provided as hard copy to clients | SDM Specific and meaningful goal-setting Action Planning, feedback and review |
Inpatient sites 2, 3 Community sites 4, 5 |
|
Client rehabilitation flyer Content:
|
To enhance client knowledge and expectations prior to rehabilitation admission | Paper flyer A4 size | SDM Specific and meaningful goal-setting |
Inpatient site 2 |
SDM: shared decision-making.
This study is part of a larger programme of research guided by the Knowledge to Action framework (KTA) and represents the evaluation and sustainability phases of implementation (22). This implementation study is to enhance the key elements of best practice rehabilitation goal-setting across 5 rehabilitation services. Specifically, the objectives of the study are to improve; (i) having a common goal focus across all team members; (ii) inclusion of action planning, feedback and review components in the goal-setting process; (iii) ensuring goals are meaningful and specific; and/or (iv) including the client in SDM throughout the goal-setting process.
Institutional ethics clearances were obtained from The Prince Charles Hospital and Health Service (HREC/17/QPCH/341) Human Research Ethics Committee and Griffith University (2017/893, Queensland, Australia) Ethics Committee prior to commencing the study, and written consent was provided by all client and clinician participants. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used to guide reporting of this study (Appendix S1).
METHODS
Study design and implementation process
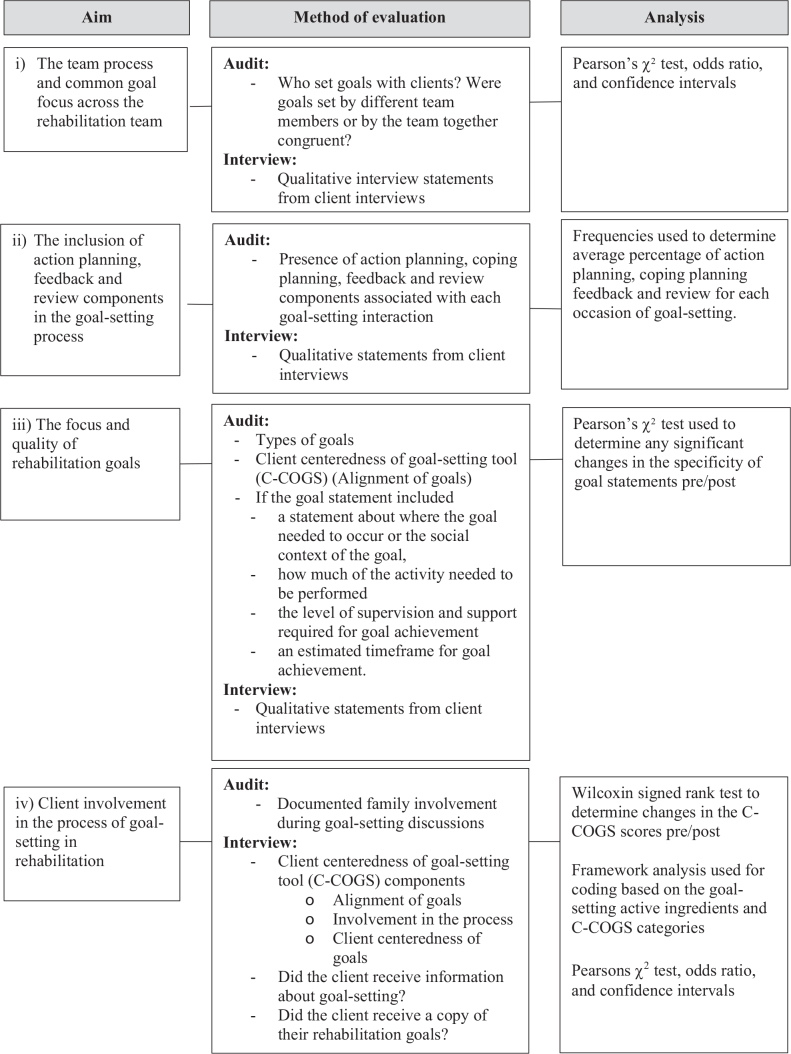
This mixed-methods study used both quantitative and qualitative data to evaluate the impact of the goal-setting implementation on key elements of goal-setting in clinical practice in 5 rehabilitation sites. This design, based on a participatory co-design approach (23), integrated quantitative and qualitative data so as to provide an understanding of the effect of the package from multiple perspectives. Co-design was essential in this implementation-evaluation project, to ensure that clinicians and clients of each rehabilitation site were encouraged to participate and take ownership of the interventions and implementation. A local site facilitator acted as the change facilitator at each rehabilitation site. Site facilitators were selected based on an expression of interest, they were required to be in stable positions in the rehabilitation team and to possess skills related to programme facilitation. All site facilitators were allied health clinicians with experience in rehabilitation settings. Clinicians at each site were also involved in completing their own medical record audits and client interviews, giving a unique opportunity to allow continuous reflection throughout the study. Clinicians were instructed not to complete audits or interviews for clients where they were directly delivering their care. Medical record audits were followed by client interviews, enabling both quantitative and qualitative evaluation of the goal-setting implementation package, and this information was synthesized to better understand the impact of the implementation (Fig. 1).
Fig. 1.
Study aims, methods and analysis.
Study context (sites)
Five rehabilitation sites, representing public inpatient (n = 3) and community rehabilitation services (n = 2) in Queensland, Australia, volunteered to participate in this study. Each rehabilitation site provides care for a varied case mix of rehabilitation clients (Table II). Each site reported routinely using goal-setting in their rehabilitation team during case conferences and within individual discipline assessment and treatment sessions. All sites agreed that the best practice key elements for goal-setting could be enhanced in their practice.
Table II.
Rehabilitation service and client characteristics
| Site | Service type | Case mixa | Service capacity | Mean client age, years | |||
|---|---|---|---|---|---|---|---|
| Pre-, % | Post-, % | Pre- | Post | ||||
| 1 | Inpatient sub-acute generalist rehabilitation unit | Stroke Orthopaedic Reconditioning Fracture |
40 10 17 20 |
28 21 24 14 |
28 beds | 70.43 (SD 11.71) |
68.41 (SD 13.85) |
| 2 | Inpatient sub-acute generalist rehabilitation unit | Stroke Neurological Reconditioning Orthopaedic Other |
32 0 11 36 14 |
39 14 18 11 0 |
25 beds | 72.86 (SD 14.20) |
64.50 (SD 15.19) |
| 3 | Inpatient sub-acute generalist rehabilitation unit | Stroke Amputee Reconditioning Other |
25 0 32 11 |
55 9 9 0 |
48 beds | 65.89 (SD 20.42) |
69.18 (SD 13.57) |
| 4 | Community rehabilitation service. Predominantly centre-based service |
Stroke Brain dysfunction Neurological Reconditioning |
55 10 10 10 |
62 19 10 0 |
NA | 55.75 (SD 17.61) |
51.62 (SD 19.02) |
| 5 | Community rehabilitation service, 1 service operating from 3 geographical sites Home visiting and centre-based service |
Stroke Reconditioning Brain dysfunction Neurological |
42 12 12 8 |
35 24 10 3 |
NA | 63.65 (SD 14.12) |
66.93 (SD 12.50) |
Top diagnostic groups for each site.
SD: standard deviation; NA: not applicable.
Intervention
A co-design approach across the 5 sites was used to develop the goal-setting implementation package (12). Each rehabilitation site selected components of the goal-setting implementation package that they felt were feasible to implement and would best address their evidence practice gap in implementing the best practice key elements of goal-setting (Table 1). Details of the package development and implementation plans for each site have been described elsewhere (12). Throughout the intervention period internal site facilitators audited the uptake of the goal-setting implementation package on a fortnightly basis. Site facilitators delivered regular feedback from these audits as a behaviour change intervention, in writing and via an optional presentation to staff at each site throughout the 12-week implementation period. Action plans were made during these feedback sessions to adjust the package as required concurrently throughout implementation.
Data collection: medical record audits
This study aimed to evaluate 30 consecutive, prospectively recruited adult rehabilitation client medical records audits at each site pre- and post-implementation of the tailored goal-setting package. A further 10 adult medical record audits were undertaken at each site at 3 months post-implementation to evaluate the sustainability of the package. Medical record audit tools were specifically designed for this study to evaluate: (i) the common goal focus across the rehabilitation team; (ii) inclusion of components of action planning, coping planning, feedback and review; and (iii) the meaningful focus and specificity of goals set at each rehabilitation site. The medical record audit tool has been described and published elsewhere (2).
Data collection: Client Centeredness of Goal-setting tool interviews
Of the clients included in the medical record audits pre- and post-implementation of the tailored goal-setting package, clients were eligible for interview if they did not have any significant mental health concerns, medical stability concerns, or communication or cognitive impairments that would prevent them from participating in the interview format. For pragmatic reasons, no client interviews were conducted at 3-month follow-up. Client interviews were conducted using the structured Client Centeredness of Goal-setting tool (C-COGS) (24, 25). The C-COGS tool was used alongside the qualitative comments made by clients to evaluate the client involvement in SDM occurring during goal-setting at each site and to add context and depth to the medical record audit data for components (i), (ii) and (iii), listed above. The C-COGS scale evaluates the client’s perspectives of the alignment of the goals with their values and beliefs, their perspectives of involvement in the goal-setting process and the client centeredness of each goal set. These C-COGS items are scored on a 5-point Likert scoring system (1–5) by the client, rating from strongly disagree to strongly agree. Clients completing the interviews were asked 2 further questions: (i) Were they given written copies of their goals? (ii) Were they given information related to goal-setting in rehabilitation?
Procedure
Data were collected pre- and post- implementation by local staff who conducted medical record audits and client interviews with included participants following 2 weeks of the client’s inpatient rehabilitation stay or the first 6 occasions of service in community rehabilitation teams. Local staff were trained by the primary researcher to conduct the audits and interviews. Client interviews were audio-recorded and transcribed verbatim. Three-month follow-up audits were conducted by the primary researcher. Study data were collected and managed using REDCap electronic data capture tools hosted at Griffith University (26).
Data analysis
Audit data and quantitative client interview data were exported to Excel (Redmond, WA, USA) and SPSS (Armonk, NY, USA) for analysis (27). Quantitative data from the medical record audits were combined with qualitative data from analysis of the interviews in order to explore components (i), (ii) and (iii) of the study aim. Both quantitative and qualitative data from the client interviews were used to explore the final study aim (Fig. 1).
Component (i). Congruency analysis was completed by the primary researcher (AB) and cross-checked with the research team. All goal statements were classified based on the International Classification of Functioning Disability and Health (ICF) (28). To evaluate common goal focus for inpatient sites, congruency of goals set by individual disciplines was compared with goals set by the inpatient team at case conference. Goal statements were considered congruent if they were classified as belonging to the same ICF activity or participation category. For community rehabilitation sites goals set by individual disciplines were compared with goals set on admission by the intake officer or care coordinator. For example, goal statements, such as “to be able to walk with a stick” and “to be able to walk 10 m to my letter box” would be categorized as congruent, under the ICF category “mobility”. Comparative analysis using descriptive statistics and Pearson’s χ2 analysis were used to evaluate changes in goal congruency pre- and post- the implementation period. Odds ratios and confidence intervals were used to demonstrate the effect size.
Component (ii). For each occasion at which goals were documented in the medical record, the entry was analysed to determine if there was a staff action, client action, point of feedback or review of goal progress included in the entry. Frequency statistics were used to demonstrate changes in the presence of action planning, coping planning, review of goals, and specificity of goal statements.
Component (iii). Specificity of goal statements were analysed based on whether they included (a) a statement about where the goal needed to be performed or the context of the goal, (b) a statement about how well the goal needed to be performed in relation to available supports, (c) a statement regarding the quantity of goal performance required, and (d) a statement about estimated timeframe for goal achievement. For example “to be able to walk with a stick” includes a statement about the quality of goal performance (using a stick as an available support) whilst the statement “to be able to walk 10 m to my letter box” includes a statement about where the goal needs to be performed and a description of the quantity of goal performance required.
Component (iv). Transcripts from C-COGS interviews were exported to Nvivo 25 for analysis (29). Interviews were coded by 2 researchers (AB, CS). Framework analysis was used to facilitate coding at 2 levels: first, using the categories of the C-COGS tool, and, secondly, coded to the relevant key element of best practice goal-setting. For quantitative C-COGS data analysis, where data was not normally distributed, non-parametric statistics (Wilcoxon signed-rank test) were used to determine changes in the quantitative interview data pre- and post-implementation. C-COGS scores and qualitative data from the client interviews were used to evaluate the client involvement, alongside quantitative audit data of documented family involvement in the goal-setting process. Pearson’s χ2 analysis was used to determine any significant changes in clients receiving copies of their goals or information about the goal-setting process.
RESULTS
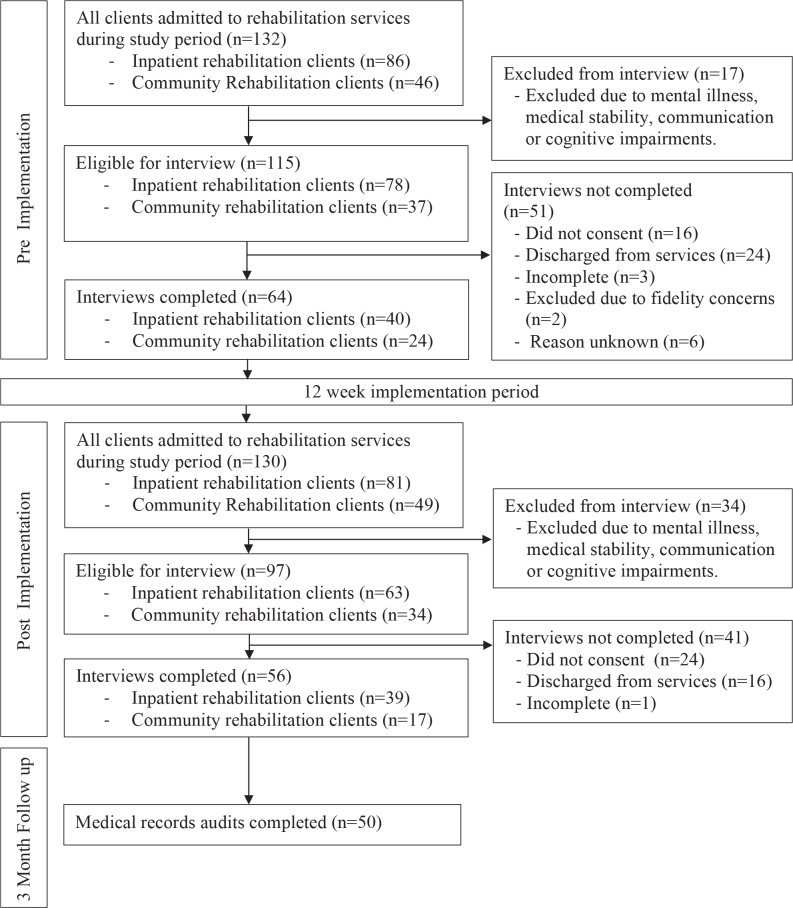
Audits were conducted on 132 client medical records prior to implementation. A total of 130 clients across all sites had medical record audits completed following the 12-week implementation of the goal-setting package, and a further 30 medical record audits were completed 3 months after the implementation period. Site and participant demographics are detailed in Table II. A total of 64 client interviews were completed from 115 eligible clients pre-implementation. Following the implementation period 97 clients were eligible for interview, of which 56 interviews were completed (Fig. 2).
Fig. 2.
Flow of participant recruitment across sites.
(i) Common goal focus
Overall, 2,858 goal statements were audited across the 5 rehabilitation sites (pre- = 1,120, post- = 1,179, follow-up = 559). Mixed results were observed when reviewing the common goal focus in each rehabilitation service. Following implementation, sites 1 and 2 demonstrated a significant improvement in the congruence of individual discipline goals with goals set by the team at case conference (site 1 p ≤ 0.001, site 2 p = 0.005; Table III). Site 3 had limited data available for congruency analysis as the model of goal setting in this service only occurred within individual discipline assessments. No significant change was seen in the congruency of goals set between individual disciplines and by 1 member on behalf of the team in sites 4 and 5.
Table III.
Congruency of goals set by individual disciplines compared with goals set by the team or a single member on behalf of the team
| Goals set by individual disciplines | Congruency of goals discipline goals with team goals prior to implementation n (%) | Congruency of goals discipline goals with team goals post-implementation n (%) | p-value (OR; 95% CI) |
|---|---|---|---|
| Site 1 (inpatient) (Pre- n=162) (Post- n=160 ) |
50 (30.9) | 79 (49.4) | <0.001 (2.185; 1.386:3.444) |
| Site 2 (inpatient) (Pre- n=200) (Post- n=170) |
58 (29.0) | 72 (42.4) | 0.005 (1.799; 1.169:2.768) |
| Site 3 (inpatient) (Pre- n=176) (Post- n=175) |
27 (15.3) | 9 (5.17) | 0.002 (0.299; 0.136:0.657) |
| Site 4 (community) (Pre- n=91) (Post- n=57) |
37 (40.7%) | 30 (52.6%) | 0.154 (1.622; 0.832:3.160) |
| Site 5 (community) (Pre- n=4) (Post- n=57) |
2 (50%) | 29 (53.7%) | 0.886 (1.160; 0.152:8.847) |
OR: odds ratio; 95% CI: confidence interval.
On review of goal congruence at 3-month follow-up, sites 1 and 2 further improved their congruency of individual discipline goals congruent to goals set by the team in a case conference (site 1 58.7% (n = 27), site 2 (58.62%, n = 17)). Sites 4 and 5 also improved the congruency of their goal-setting (site 4; 82.61% (n = 38), site 5; 63.49% (n = 40)), whilst minimal changes were seen in site 3 (6.67%, n = 7).
Clients also commented on their experience when team members did or did not have a common goal focus:
You know what you’ve been told, and then you get told something completely different by someone else, and where does that leave you? (Site 1)
Even though I had a long-term goal of being able to go home, I was able to break that down into what I needed to do to get there. That was good. In each therapy group, I had …goals that interwove with each other. (Site 2)
(ii) Action planning, feedback, and review
The presence of staff action plans to address client goals improved at 3 sites at completion of the 12-week implementation (sites 1, 2 and 5) (see supplementary material Table SI). Improvements were observed in the inclusion of client action planning at 4 sites (sites 1, 2, 4 and 5). Whilst improvements were seen in client action planning, the audit still indicated that clients only had documented client action plans 32% of the time and this was also backed up by 1 client reporting:
If I was going to write a goal…, I would say, “This is my ultimate target and the goal.” but I’d like to know what are the processes to reach that goal? (Site 4).
Whilst sites 1, 2, 3 and 4 all improved in documenting points of goal feedback and review, 1 client still stated:
I think the goals could be refined more frequently because as the patient changes…the goals can change as well… I think it’s probably a good idea that the link worker reminds the patient of those goals more often. (Site 2)
(iii) Focus and quality of goal statements
Overall, clients reported goals aligned with their values and beliefs (C-COGS alignment subscale score 4.45/5), but there was still evidence of meaningful goal-setting being missed:
One area that I raised and has never been addressed, … was to do with continence. (Site 2)
More activity and participation goal-setting and less impairment level goal-setting was seen in sites 2 and 3, whilst there was a decrease in staff actions being stated as client goals in all inpatient sites (see Table SII).
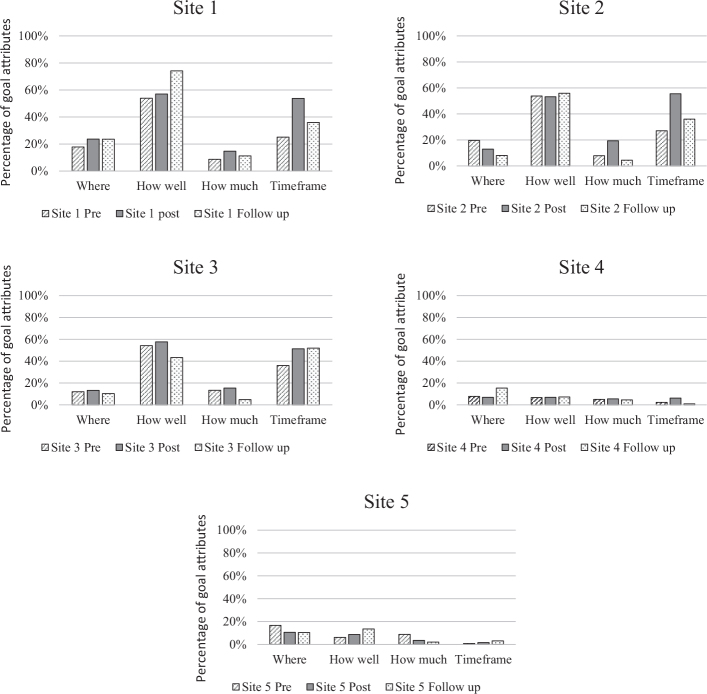
Inpatient rehabilitation teams improved the specificity of documented goal statements more than community rehabilitation teams (Fig. 3). Specifically, inpatient rehabilitation teams improved the quality of their goal statements through addition of either documented time-frames, the context of where the goal was to occur, or improvements in quantifying the amount of performance required for goal achievement. However, the majority of these improvements were diminished at the 3-month follow-up. Some clients reported that setting specific goals made the rehabilitation process clearer:
Fig. 3.
Inclusion of goal attributes pre, post and at 3 months follow up.
It’s explained very well to me about it being relevant, measured, timely. Things like that. Even though I had a long-term goal of being able to go home, I was able to break that down into what I needed to do to get there. (Site 2)
Alternatively, some clients did not want to set such specific goals:
Personally, I’m not that sort of targeted person. I believe in doing the best you can do. (Site 1)
There were minimal changes in the specificity of goals set in community rehabilitation teams where the primary process for goal-setting was completed by 1 member on behalf of the team.
(iv) Client involvement in shared decision making during goal-setting
There were minimal changes in C-COGS scores between pre- and post-implementation (see Table SIII). Whilst clients generally agreed or strongly agreed that their goals aligned with their values and what they wanted to work on, several clients highlighted the impact of the individualized approach that clinicians take when conducting goal-setting:
It probably depends on who you get, too. That allows you to be free to choose your own goals… When I was here the first time, they definitely persuaded me towards goals that I think they thought they could achieve. (Site 4)
Furthermore, there remains evidence of very ingrained rehabilitation assessments and practice, which clinicians conduct despite client’s values and needs:
We went in the kitchen and they said, “Can you make a cup of tea?” I’ve never drank tea. I’ve never made a cup of tea. I said, “How do you turn the jug on?” Because I’ve never done it. (Site 1)
Clients agreed or strongly agreed that they were included in the process of goal-setting:
Yes. I’d probably be the leading partner in it [the goal-setting process]. (Site 5)
I think it’s a good idea that seems to be discussed with the patients more nowadays. Whereas before, they weren’t. Now, it seems that they have made it more cooperative. (Site 1)
However, 1 client reported differences in their involvement in the process of goal-setting between the goals they set on admission with a team member and the goals occupational therapists and physiotherapists prioritized beyond the initial goal-setting:
The initial goals that I set were set almost on admission. Then the goals that were set after that were pretty much set by the OTs or physios relative to what condition I was in…They were more goals for the OTs or the physios. They weren’t my personal goals. Even though I agree with them in principle that wasn’t my primary motivation. I think of a goal as a primary motivator. (Site 2)
Clients reported agreeing or strongly agreeing that their family were involved in the goal-setting process (as much as they wanted them to be) equally both pre- and post-implementation (pre- n = 46, 72%, post- n = 41, 73.21%). However, medical record audits demonstrated an increase in documented family participation in goal-setting processes following the implementation period (pre- n = 11, 8%, post- n = 27, 20.61%) specifically in community rehabilitation.
Clients in sites 2 and 3 reported receiving more information about the team’s approach to goal-setting, thus demonstrating an improvement in the inclusion of SDM principles. Overall, more clients reported receiving copies of their rehabilitation goals across all sites in this study, with a significant improvement in 2 inpatient services (site 1 p ≤ 0.001, site 2 p ≤ 0.001), which implemented the provision of client goal boards following case conferences (see Table SIV).
DISCUSSION
This study aimed to evaluate how components of the implementation package enhanced the key elements of best practice goal-setting. The mixed results of this study highlight the importance of considering not just the components of the goal-setting implementation package themselves, but how teams and individual clinicians chose to implement these components within their clinical practice.
Of interest in this study were the large improvements made by those sites that embraced the use of the goal-setting implementation package as a team. Sites 1 and 2 did this by setting common goals with the team during the case conference. Implementing an intervention at the level of the team where clinicians took on defined roles with specific expectations and were accountable to the team may have been a key component contributing to the enhanced key elements of best practice goal-setting at sites 1 and 2. Accountability has long been identified as a key requirement to support effective teamworking, in some instances; however, how accountability is delivered in the healthcare settings can be either productive or conflictual. Accountability within healthcare teams has been found to be implemented most successfully when there are clear expectations outlined, when the team have appropriate skills and resourcing and when there are clear targets and ongoing feedback (30).
Sites implementing interventions embedded in existing processes (case conferences, key worker models) enhanced the key elements of goal-setting more than sites which implemented components of the package (client workbooks) as a new process. Site 2 embedded the use of goal boards and the client workbook using an existing key worker process, whilst site 1 restructured the end of each case conference to nominate a clinician to provide feedback to each client using the new goal boards. Previous studies have shown that implementing interventions that include prompts and restructuring of physical, social environment and processes can enhance the uptake of interventions (31) and these strategies also appeared effective in this study.
No sites included the client as a member of the team in the case conference. To ensure truly interdisciplinary teamworking clients should be included as a member of the rehabilitation team and be involved in goal-setting. Previous research has highlighted that including the client in team meetings can take clinicians up to an additional 4 h per week (32). This level of time commitment was not deemed feasible by any of the rehabilitation sites in this study, instead sites 1 and 2 chose to provide clients with written copies of their goals following case conferences. Whilst provision of accessible written material has been shown to enhance client understanding (33) it does not replicate the iterative discourse, information sharing and SDM that should occur between the rehabilitation team and client when setting truly client-centred common goals and actions across the rehabilitation journey. Therefore goal-setting in this study remained predominantly therapist led. How clients can be more actively involved as a member of the rehabilitation team warrants further investigation.
There was limited carryover of changes to the specificity of goal statements at 3 months after data collection. The lack of sustainability may have been impacted by inconsistent use of the training resources. Previous studies by Hassett et al. (18) and Marsland et al. (16) have shown increased specificity of goal-setting following education and training. All sites in this study undertook education and training; however, significant increases in specificity of goal-statements were predominantly seen in inpatient sites where audit and feedback were able to be implemented regularly. Previous studies using audit and feedback have found that this strategy can itself increase clinician’s adherence to recommendations, specifically when action plans are designed to address the feedback (34), as was implemented by the facilitator throughout the 12-week implementation period in this study. Further evidence to support the importance of audit feedback was demonstrated by the decrease in specificity of inpatient goal statements at 3-month follow-up after cessation of audit and feedback and the site facilitator role.
Using a participatory co-design approach for this research was hypothesized to impact implementation and sustainability beyond withdrawal of formal implementation support. Involving the staff in designing their own strategies for change (12) was done to provide them with skills and tools for future self-reflection and to enhance ownership over the goal-setting implementation package being implemented. Many rehabilitation services consist of rotational staff with significant staff turnover. How staff turnover beyond the short 12-week implementation period impacted the sustainability of the goal-setting implementation package is unknown and further research is warranted.
This study was based on theoretical constructs (2) and supported by implementation process models and determinant frameworks (22, 35). Overall, the multifaceted nature of the goal-setting implementation package in this study was based on a strong conceptual framework and was targeted at multiple participants (clients, staff and the team).
Limitations of this study include the possibility of confirmation bias due to the co-design and participatory approach followed during the pre- and post- data collection phase. Due to time limitations with this study, limited data could be collected to evaluate the sustainability of changes. The high scoring on the C-COGS tool may be due to ceiling affects noted with this measure in this study. Furthermore, for pragmatic reasons limited audit data and no interview data could be collected for 3-month follow-up, impacting the understanding of sustainability of the goal-setting implementation package over time. Further information regarding the process of implementation and sustainability of the goal-setting package in this study is warranted and would further support teams implementing goal-setting strategies in rehabilitation services.
Clinical implications
Several clinical implications have been identified throughout this study. Firstly, interventions targeting the team together appeared to best enhance the key elements of goal-setting. This may have been influenced by the shared ownership and “built in” accountability to the team. Rehabilitation teams should consider how they implement the key elements of goal-setting together as a team. Teams should also consider embedding key elements of goal-setting practice into existing processes. Sites in this study that embedded the use of the goal-setting implementation package into existing processes demonstrated a greater propensity to improve their goal-setting in alignment with best practice. Finally, teams should consider the use of facilitation, regular audit and feedback, as these aspects of implementation appear to be a key element in the sustainability of best practice goal-setting.
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge the Statewide Rehabilitation Clinical Network for funding this research project, the goal-setting working group for their clinical advice and guidance, and the local site facilitators for supporting the implementation of the project. NAL is supported by National Heart Foundation of Australia Future Leader Fellowship (102055).
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Levack WM, Dean SG, Siegert RJ, McPherson KM. Purposes and mechanisms of goal planning in rehabilitation: the need for a critical distinction. Disabil Rehabil 2006; 28: 741–749. [DOI] [PubMed] [Google Scholar]
- 2.Baker A, Cornwell P, Gustafsson L, Lannin NA. An exploration of goal-setting practices in Queensland rehabilitation services. Disabil Rehabil 2022; 44: 4368–4378. [DOI] [PubMed] [Google Scholar]
- 3.Cifu DX, Stewart DG. Factors affecting functional outcome after stroke a critical review of rehabilitation interventions. PM R 1999; 80: 35–39. [DOI] [PubMed] [Google Scholar]
- 4.Kornor M. Interprofessional teamwork in medical rehabilitation: a comparison of multidisciplinary and interdisciplinary team approach. Clin Rehabil 2010; 24: 745–755. [DOI] [PubMed] [Google Scholar]
- 5.Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: a development of a theorectically informed practice framework. Clin Rehabil 2011; 25: 468–482. [DOI] [PubMed] [Google Scholar]
- 6.Bovend’Erdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil 2009; 23: 352–361. [DOI] [PubMed] [Google Scholar]
- 7.Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: a systematic review. Patient Educ Couns 2017; 100: 65–75. [DOI] [PubMed] [Google Scholar]
- 8.Strasser DC, Falconer JA, Stevens AB, Uomoto JM, Herrin J, Bowen SE, et al. Team training and stroke rehabilitation outcomes: a cluster randomized trial. Arch Phys Med Rehabil 2008; 89: 10–15. [DOI] [PubMed] [Google Scholar]
- 9.Cameron LJ, Somerville LM, Naismith CE, Watterson D, Maric V, Lannin NA. A qualitative investigation into the patient-centered goal-setting practices of allied health clinicians working in rehabilitation. Clin Rehabil 2018; 32: 827–840. [DOI] [PubMed] [Google Scholar]
- 10.Rose A, Soundy A, Rosewilliam S. Shared decision-making within goal-setting in rehabiliation: a mixed-methods study. Clin Rehabil 2019; 33: 564–574. [DOI] [PubMed] [Google Scholar]
- 11.Leach E, Cornwell P, Fleming J, Haines T. Patient centered goal-setting in a subacute rehabilitation setting. Disabil Rehabil 2010; 32: 159–172. [DOI] [PubMed] [Google Scholar]
- 12.Baker A, Cornwell P, Gustafsson L, Stewart C, Lannin N. Developing tailored theoretically informed goal-setting interventions for rehabilitation services: a co-design approach. BMC Health Serv Res 2022; 22: 811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitaiton setting: development of a theoretically informed practice framework. Clin Rehabil 2011; 25: 468–482. [DOI] [PubMed] [Google Scholar]
- 14.Kathryn M. McPherson NMK, Kersten P. MEANING as a smarter approach to goals in rehabilitation. In: Sigert RJ, Levack WMM, editors. Rehabilitaiton goal setting theory, practice and evidence. Boca Ratan: CRC Press; 2014, 18 p. [Google Scholar]
- 15.Bowman J, Mogensen L, Marsland E, Lannin N. The development, content validity and inter-rater reliability of the SMART-Goal Evaluation Method: a standardised method for evaluating clinical goals. Aust Occup Ther J 2015; 62: 420–427. [DOI] [PubMed] [Google Scholar]
- 16.Marsland E, Bowman J. An interactive education session and follow-up support as a strategy to improve clinicians’ goal-writing skills: a randomized controlled trial. J Eval Clin Pract 2010; 16: 3–13. [DOI] [PubMed] [Google Scholar]
- 17.Lenzen SA, Daniels R, van Bokhoven MA, van der Weijden T, Beurskens A. Development of a conversation approach for practice nurses aimed at making shared decisions on goals and action plans with primary care patients. BMC Health Serv Res 2018; 18: 891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hassett L, Simpson G, Cotter R, Whiting D, Hodgkinson A, Martin D. A prospective interrupted time series study of interventions to improve the quality, rating, framing and structure of goal-setting in community-based brain injury rehabilitaiton. Clin Rehabil 2015; 29: 327–338. [DOI] [PubMed] [Google Scholar]
- 19.McCluskey A, O’Connor D. Implementing and sustaining practice change. In: Hoffmann T, Bennett S, Del Mar C, editors. Evidence based practice across the health professions. (3rd edn). Sydney: Elsevier; 2017, p. 384–408. [Google Scholar]
- 20.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 2013; 50: 587–592. [DOI] [PubMed] [Google Scholar]
- 21.Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Design J 2015; 18: 227–248. [Google Scholar]
- 22.Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006; 26: 13–24. [DOI] [PubMed] [Google Scholar]
- 23.Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health 2006; 60: 854–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doig E, Prescott S, Fleming J, Cornwell P, Kuipers P. Development and construct validation of the Client-Centredness of Goal Setting (C-COGS) scale. Scand J Occup Ther 2015; 22: 302–310. [DOI] [PubMed] [Google Scholar]
- 25.Doig E, Prescott S, Fleming J, Cornwell P, Kuipers P. Reliability of the Client-Centeredness of Goal Setting (C-COGS) Scale in acquired brain injury rehabilitation. Am J Occup Ther 2016; 70: 7004290010. [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.IBM Corp . Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- 28.World Health Organization (WHO) . International classification of functioning, disability and health: ICF. Geneva: WHO; 2001. [Google Scholar]
- 29.QSR International Pty Ltd . 2020, NVivo (released in March 2020). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 30.Zajac S, Woods A, Tannenbaum S, Salas E, Holladay CL. Overcoming challenges to teamwork in healthcare: a team effectiveness framework and evidence-based guidance. Front Commun 2021; 6: 606445 [Google Scholar]
- 31.Michie S, Atkins L, West R. A guide to using the behaviour change wheel. London: Silverback Publishing; 2014. [Google Scholar]
- 32.Dongen JJJ, Habets IGJ, Beurskens A, Bokhoven MA. Successful participation of patients in interprofessional team meetings: a qualitative study. Health Expect 2017; 20: 724–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giguere A, Legare F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012; 10: CD004398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jolliffe L, Morarty J, Hoffmann T, Crotty M, Hunter P, Cameron ID, et al. Using audit and feedback to increase clinician adherence to clinical practice guidelines in brain injury rehabilitation: a before and after study. PLoS One 2019; 14: e0213525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.