Abstract
Introduction and importance
Meckel's diverticulum (MD) is a common congenital malformation of the digestive tract, often asymptomatic but occasionally leading to complications such as bowel obstruction and ischemia. Timely recognition and treatment of these complications are crucial.
Presentation of case
We report the case of a 27-year-old male patient presenting with complete intestinal obstruction and ischemia of the ileum due to a fibrous band associated with MD. The patient presented with severe abdominal pain lasting for 10 h. Physical examination revealed a distended abdomen, antalgic position, and positive decompression. Laboratory tests showed leukocytosis and elevated lactic acid levels. Computed tomography revealed dilated small bowel loops with signs of intestinal ischemia. Emergency exploratory laparoscopy confirmed a complete ileum with ischemia and identified a fibrous band originating from the mesentery, strangulating the affected loop. The fibrous band was dissected and sectioned, confirming its association with the MD, which was resected with subsequent recovery of peristalsis and vascularization of the compromised segment. The patient had a favorable postoperative recovery without complications.
Discussion
MD is a rare cause of bowel obstruction, requiring a high index of suspicion for diagnosis. Despite the challenges in preoperative identification, early surgical intervention is crucial to prevent adverse outcomes. This case emphasizes the importance of promptly recognizing and managing MD-related complications to optimize patient outcomes.
Conclusion
MD should be considered in cases of acute occlusive abdomen, despite its infrequent occurrence. Early diagnosis and timely surgical intervention are essential to minimize morbidity and mortality associated with MD-related complications.
Keywords: Meckel's diverticulum, Intestinal obstruction, Ischemia, Case report
Highlights
-
•
Complications of Meckel's diverticulum (MD) are rare, but bowel obstruction is a frequent complication.
-
•
Bowel obstruction in MD can be due to volvulus, intussusception, or meso-diverticular band entrapment
-
•
Timely diagnosis and surgical intervention are crucial in MD-related complications to reduce risks.
-
•
Laparoscopic resolution of MD associated intestinal obstruction and ischemia is feasible in centers with trained personnel.
1. Introduction
Meckel's diverticulum (MD) is the most common congenital malformation of the digestive tract. It occurs in up to 3 % of the population as a result of the persistence of the intestinal yolk duct [1]. It has a symptomatic course in only 0.08 % of patients, generally associated with complications [2]. The most frequent complication is the bowel obstruction which can occur by a volvulus or twisting of the bowel around a fibrous band from the MD to the umbilicus; by an intussusception or inversion of the MD in the ileum or cecum or by a meso-diverticular band that traps the small bowel under the vascular supply of the MD and can lead to strangulation of the affected loop [3]. The most common complication in adults is intestinal obstruction, which can be caused by volvulus of the intestine around a fibrous band that attaches the MD to the abdominal wall or by intussusception of the MD into the ileum or cecum [3]. In all these cases surgery is mandatory [[4], [5], [6]]. We present the case of a patient with complete intestinal obstruction and ischemia of the ileum due to a fibrous band compatible with MD. This case report is reported in line with the SCARE Guidelines [7].
2. Presentation of case
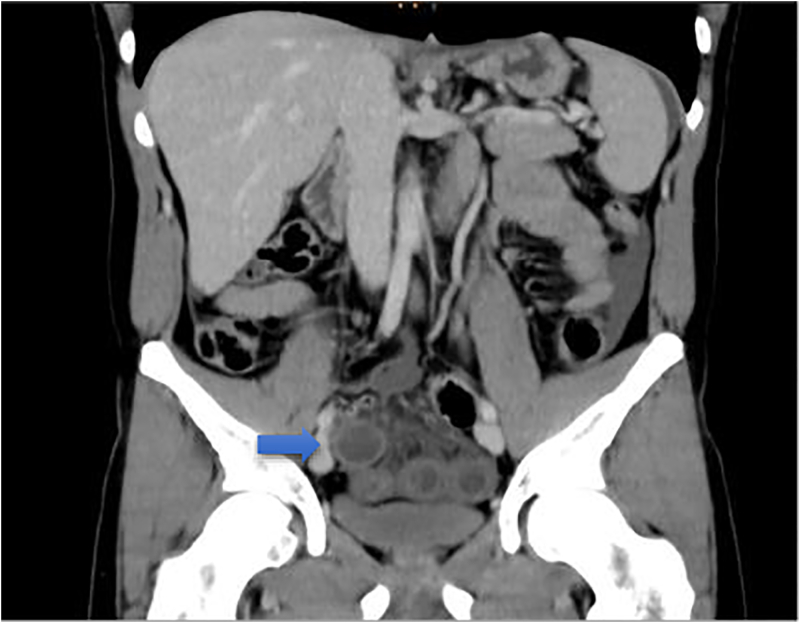
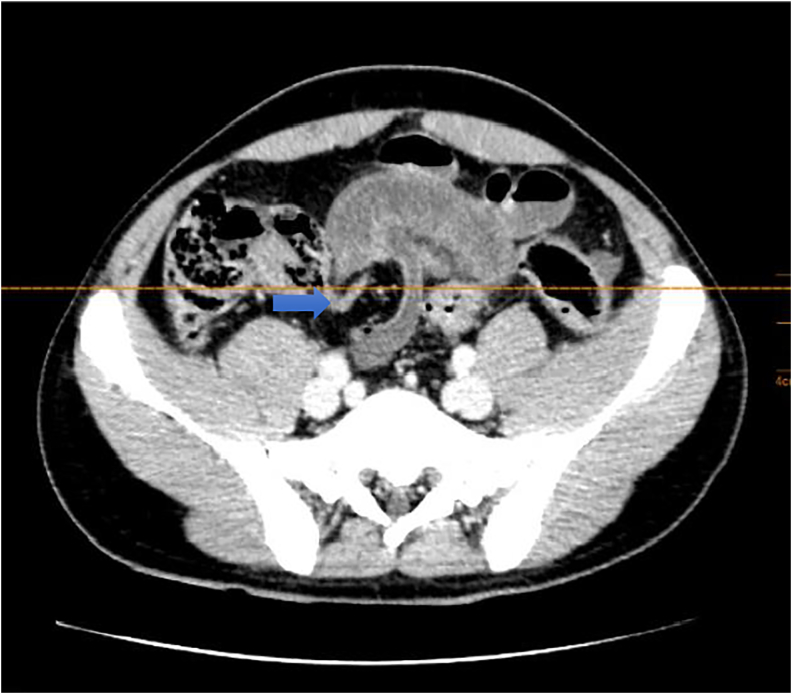
27 year old male patient with no pathological or surgical history admitted to the emergency department with severe abdominal pain of 10 h of evolution located in the hypogastrium. On physical examination cardiac frequency: 100 lpm; blood pressure: 140/80 mmHg; oxygen saturation 99 %, generalized mucocutaneous paleness, antalgic position, distended abdomen, without hydroaerial sounds, with pain on palpation in the lower abdomen, and positive decompression. Laboratory tests reported leukocytes of 23,400 (U/mL) (normal value 4500–11,000 U/mL) and lactic acid 3.85 mmol/L. (normal value: 0,5–2 mmol/L). Computed tomography (CT) of the abdomen and pelvis with contrast showed dilated small bowel loops with hydroaerial levels and signs of parietal hypoperfusion with change of caliber at the level of the terminal ileum close to the ileocecal valve (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Coronal abdominal CT scan with distended small bowel loops, wall edema.
Fig. 2.
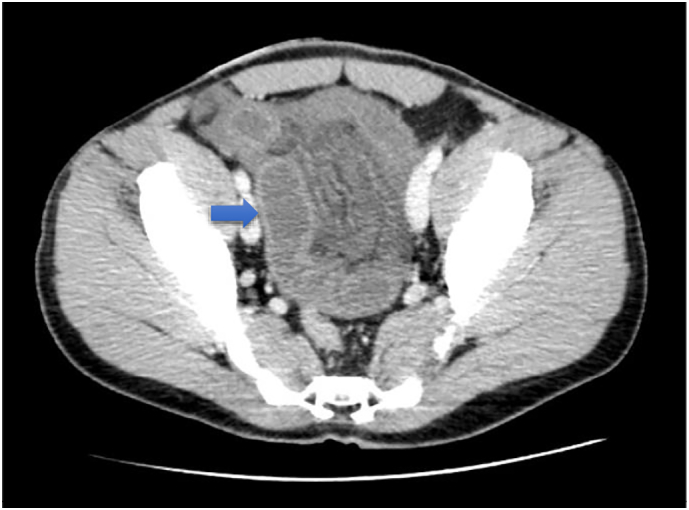
Axial abdominal CT scan with distended small bowel loops, wall edema.
Fig. 3.
Axial abdominal CT scan where a change of caliber is visualized at the level of the small bowel loop.
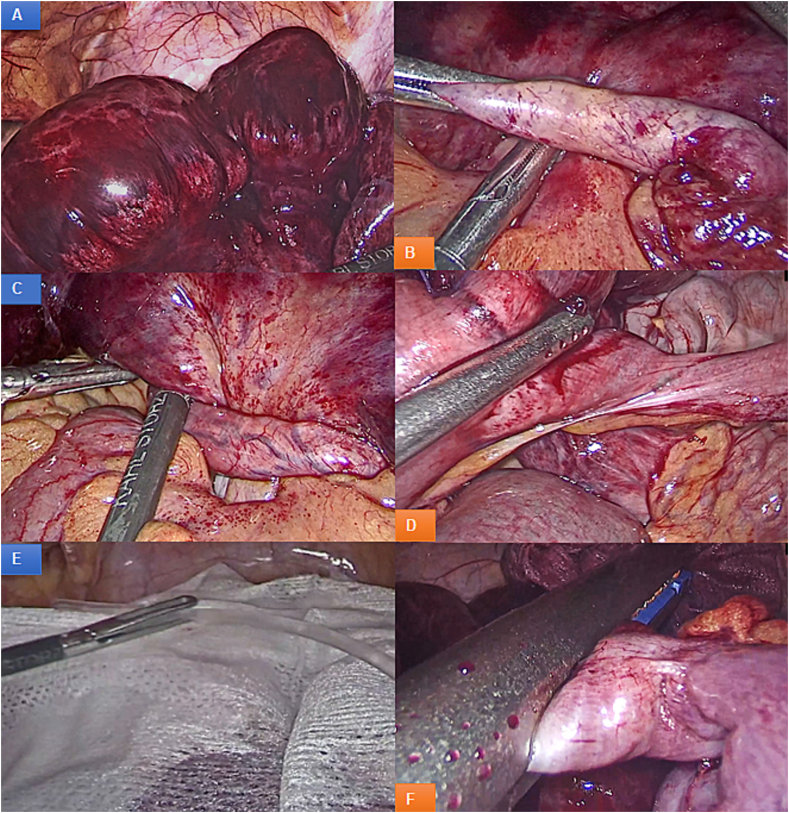
An emergency exploratory laparoscopy showed a ileum with distal ischemia of 80 cm in length (Fig. 4A). The cause was identified as a fibrous band that “strangled” the ileum starting from the root of the mesentery and completely surrounded a cluster of loops between the last 100 cm proximal and 20 cm distal segments near the ileocecal valve (Fig. 4B-C). The fibrous band was dissected and sectioned, identifying it as a MD (Fig. 4D). Intraperitoneal lidocaine lavage was performed after placing gauze over dilated intestinal loops for 5 min (Fig. 4E), during which time peristalsis and partial improvement of intestinal coloration were observed. Finally, the MD was resected from its base with a 60 mm laparoscopic linear mechanical suture (Fig. 4F) and a Jackson Pratt drain was left at the pelvic level. The patient had a favorable evolution in the immediate postoperative period, with tolerance to diet at 48 h and recovery of intestinal transit on the third day. Drainage was removed on the fourth day, and the patient was discharged on the seventh day without complications.
Fig. 4.
Surgical findings: A. Ileum with distal ischemia of 80 cm in length. B. Fibrous band that “strangled” the ileum. C. Dissected and sectioned fibrous band, identifying it as a Meckel's Diverticulum (MD). E. Intraperitoneal lidocaine lavage for 5 min. F. Resected from its base with a 60 mm laparoscopic linear mechanical suture.
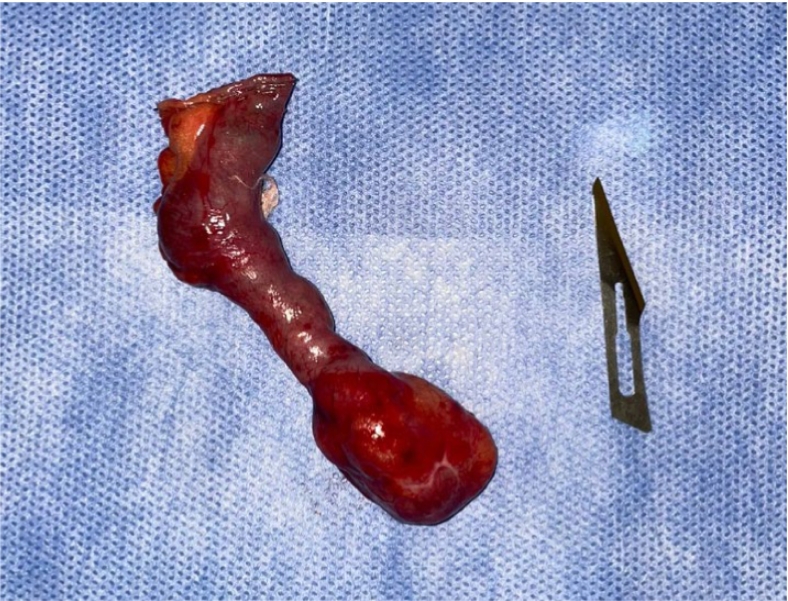
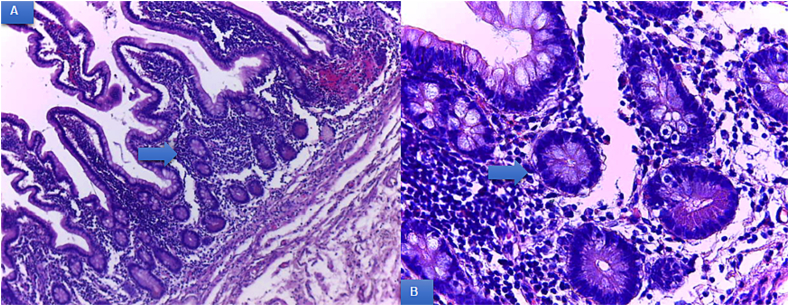
The pathological anatomy of the surgical specimen reported a MD with intestinal-type mucosa and sectors of body-type gastric mucosa, without atypia (Fig. 5, Fig. 6).
Fig. 5.
Surgical specimen: anatomy of the surgical specimen reported a Meckel's Diverticulum.
Fig. 6.
A. Low magnification image (4×); MD microscopy. Areas of intestinal and gastric mucosa are visualized, without atypia. B. High magnification image (40×); MD microscopy. Areas of intestinal and gastric mucosa are visualized, without atypia.
3. Discussion
MD is one of several congenital anomalies that develop as a consequence of a defect in the obliteration of the vitelline or omphalomesenteric duct [8]. It remains asymptomatic in the vast majority of cases; however, 4 % of patients will develop symptoms secondary to its complications, with bowel obstruction (BO) and inflammation being the most common in adults [9]. Since symptomatic MD patients represent only 0.08 % of the total population, the infrequency of the condition leads to low rates of preoperative diagnosis [8].
The causes of bowel obstruction are varied and include diverticulum inversion, intussusception, volvulus, Littré hernia (protrusion of the MD through a hernial orifice), malignancy and rarely coprolites [10]. In our case, the patient consulted for a picture of nonspecific abdominal pain accompanied by abdominal distension with the surgical finding of a mesodiverticular band surrounding the terminal ileum producing a complete obstruction and venous ischemia of the loop. The mesodiverticular band is a structure that is present in 3–8 % of patients with MD, which can surround the ileum, strangling it. It is an exceptional situation that is within the possibilities of obstruction due to MD [11]. In these cases, early recognition of the clinical picture and scheduling surgery as a therapeutic option is of vital importance, since a delay in surgery of 36 h or more can triple the mortality rate from 8 to 25 % [12].
The preoperative diagnosis of BO due to MD is a real challenge. Bani-Hani and Shatnawi reported a preoperative diagnostic effectiveness of less than 10 % in a group of 28 patients [13]. The sensitivity and specificity of CT for diagnosing a MD as a cause of BO is low due to the inability to distinguish MD among dilated small bowel loops [14]. In our case, CT revealed conclusive findings of occlusive acute abdomen with signs of intestinal ischemia without identifying MD as the cause. Because of this, in cases of complete BO without apparent cause, we believe that laparoscopic surgical exploration is mandatory.
When MD is found, it is advisable to resect it and evaluate whether or not intestinal resection is necessary, depending on the degree of ischemia accompanying the involved loop, the location of the BO and the clinical condition of the patient.
In a recently published literature review of BO secondary to MD [15], researchers support the idea of abdominal exploration with subsequent performance of diverticulectomy and evaluation of the affected bowel for eventual resection and anastomosis.
4. Conclusion
BO due to DM is an extremely rare condition that requires a high degree of diagnostic suspicion in adults diagnosed with acute occlusive abdomen. Early detection by imaging techniques and timely surgical intervention are essential to avoid serious complications including intestinal necrosis and eventual perforation. Laparoscopic resolution of BO and ischemia associated with MD is feasible in centers with personnel trained in laparoscopic surgery.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Given that this publication is a case report that does not contain identifiable patient information, this publication is exempt from ethical approval by the Institutional Ethics Committee.
Funding
No source to be stated.
Credit authorship contribution statement
Dr. Ramiro Alberto, Vargas Aignasse (writing the paper, data analysis, and interpretation, literature review).
Dra. Diana Alejandra, Pantoja Pachajoa (revising and editing the paper, data analysis, and interpretation, literature review, study concept and approved the final version).
Dra. Florencia Llahi (literature review, data analysis, and interpretation.
Dr. Matias Parodi (data analysis).
Dr. Alejandro Marcelo Doniquian (data analysis).
Dr. German Rodrigo, Viscido (literature review, data analysis, and interpretation).
Guarantor
Dr. Matias Parodi: matiasparodi@curf.ucc.edu.ar
Dr. German Rodrigo Viscido: germanviscido@gmail.com.
Research registration number
N/A.
Declaration of competing interest
The authors declare that there is no conflict of interest.
Acknowledgements
Not applicable.
References
- 1.Sagar J., Kumar V., Shah D.K. Meckel’s diverticulum: a systematic review. J. R. Soc. Med. 2006;99(10):501. doi: 10.1177/014107680609901011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dumper J., Mackenzie S., Mitchell P., Sutherland F., Quan M.L., Mew D. Complications of Meckel’s diverticula in adults. Can. J. Surg. 2006;49(5):353–357. PMCID: PMC3207587 PMID: 17152574. [PMC free article] [PubMed] [Google Scholar]
- 3.Intestinal obstruction: role of CT. Gastroenterol. Clin. N. Am. 2002;31(3):777–799. doi: 10.1016/s0889-8553(02)00026-2. [DOI] [PubMed] [Google Scholar]
- 4.Lequet J., Menahem B., Alves A., Fohlen A., Mulliri A. Meckel’s diverticulum in the adult. J Visc Surg. 2017;154(4):253–259. doi: 10.1016/j.jviscsurg.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Antonia Montenegro M., Núñez H., Maroto L., Abril C., Gago P. Cir Esp. 2009;85(1):59–60. doi: 10.1016/S0009-739X(09)70091-0. https://doi.org/10.1016/S0009-739X(09)70091-0. [DOI] [PubMed] [Google Scholar]
- 6.Beltran S.M., Larenas U.R., Almonacid F.J., Danilova T., Cruces B.K., Barria C., et al. Meckel’s diverticulum volvulus: report of one case. Rev Chil Cir. 2006;58(1):50–53. [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Yahchouchy E.K., Marano A.F., Etienne J.C., Fingerhut A.L. Meckel’s diverticulum. J. Am. Coll. Surg. 2001;192(5):658–662. doi: 10.1016/s1072-7515(01)00817-1. [DOI] [PubMed] [Google Scholar]
- 9.Mulita F., Verras G.I., Tchabashvili L., Liolis E., Kaplanis C., Perdikaris I., et al. Small bowel obstruction in a 42-year-old patient? Be aware of Meckel’s diverticulum. Prz Gastroenterol. 2022;17(3):245–247. doi: 10.5114/pg.2021.109979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chatterjee A., Harmath C., Vendrami C.L., Hammond N.A., Mittal P., Salem R., et al. Reminiscing on remnants: imaging of Meckel diverticulum and its complications in adults. American Journal of Roentgenology [Internet]. 2017;209(5):W287–W296. doi: 10.2214/AJR.17.18088. [DOI] [PubMed] [Google Scholar]
- 11.Frager D. Intestinal obstruction role of CT. Gastroenterol. Clin. N. Am. 2002;31(3):777–799. doi: 10.1016/s0889-8553(02)00026-2. [DOI] [PubMed] [Google Scholar]
- 12.Rami Reddy S.R., Cappell M.S. A systematic review of the clinical presentation, diagnosis, and treatment of small bowel obstruction. Curr Gastroenterol Rep. 2017;19(6):1–14. doi: 10.1007/s11894-017-0566-9. [DOI] [PubMed] [Google Scholar]
- 13.Bani-Hani K.E., Shatnawi N.J. Meckel’s diverticulum: comparison of incidental and symptomatic cases. World J. Surg. 2004;28(9):917–920. doi: 10.1007/s00268-004-7512-3. [DOI] [PubMed] [Google Scholar]
- 14.Kuru S., Bulus H., Kismet K., Aydin A., Yavuz A., Tantoglu U., et al. Mesodiverticular band of Meckel’s diverticulum as a rare cause of small bowel obstruction: case report and review of the literature. VIS. 2013;29(6):401–405. https://doi.org/10.1159/000357533. [Google Scholar]
- 15.Meckel'’s Diverticulum Causing Acute Intestinal Obstruction A case report and comprehensive review of the literature. Ann West Med Surg. 2022;1(78) doi: 10.1016/j.amsu.2022.103734. [DOI] [PMC free article] [PubMed] [Google Scholar]