Abstract
Background
The COVID-19 pandemic resulted in disruptions to routine HIV services for youth living with HIV (YLH), provoking rapid adaptation to mitigate interruptions in care. The Adolescent Transition to Adult Care for HIV-infected adolescents (ATTACH) study (NCT03574129) was a hybrid I cluster randomized trial testing the effectiveness of a healthcare worker (HCW)-delivered disclosure and transition intervention — the Adolescent Transition Package (ATP). During the pandemic, HCWs leveraged phone delivery of the ATP and were supported to make adaptations. We characterized real-time, provider-driven adaptations made to support phone delivery of the ATP.
Methods
We conducted continuous quality improvement (CQI) meetings with HCWs involved in phone delivery of the ATP at 10 intervention sites. CQI meetings used plan-do-study-act (PDSA) cycles and were audio-recorded. Adaptations were coded by two-independent coders using the Framework for Reporting Adaptations and Modifications to Evidence-based Implementation Strategies (FRAME-IS). Adaptation testing outcomes (adopt, retest, or abandon) and provider experience implementing the adaptations were also recorded. We summarized adaptation characteristics, provider experience, and outcomes.
Results
We identified 72 adaptations, 32 were unique. Overall, adaptations included modification to context (53%, n = 38), content (49%, n = 35), and evaluation processes (13%, n = 9). Context adaptations primarily featured changes to personnel, format, and setting, while content and evaluation adaptations were frequently achieved by simple additions, repetition, and tailoring/refining of the phone delivery strategy. Nine adaptations involved abandoning, then returning to phone delivery. HCWs sought to increase reach, improve fidelity, and intervention fit within their context. Most adaptations (96%, n = 69) were perceived to increase the feasibility of phone delivery when compared to before the changes were introduced, and HCWs felt 83% (n = 60) of adaptations made phone delivery easier. Most adaptations were either incorporated into routine workflows (47%) or tested again (47%).
Conclusion
Adaptation of phone delivery was a feasible and effective way of addressing challenges with continuity of care for YLH during the COVID-19 pandemic. Adaptations were primarily context adaptions. While FRAME-IS was apt for characterizing adaptations, more use cases are needed to explore the range of its utility.
Trial registration
Trial registered on ClinicalTrial.gov as NCT03574129.
Supplementary Information
The online version contains supplementary material available at 10.1186/s43058-023-00446-y.
Keywords: Adaptation, Implementation study, Implementation strategy, COVID-19, mHealth, Adolescents, Youth, FRAME-IS
Contributions to the literature.
This paper illustrates how team-based learning sessions in the form of CQI meetings can be utilized by frontline healthcare workers to systematically develop and apply adaptations to quickly adjust to changing context (i.e., COVID-19). This is useful for researchers exploring methods for integrating dynamic adaptation into routine healthcare worker workflow in constrained settings.
This paper demonstrates the retrospective application of FRAME-IS to characterize adaptations, highlighting an approach to further our understanding of implementation through the study of adaptation types and their characteristics.
This paper adds to the literature on the use of qualitative methods for studying adaptations and underscores the potential for framework or rapid analysis of qualitative data to quickly identify and characterize adaptations or adaptation traits associated with improved implementation outcomes in real time.
Background
The COVID-19 pandemic presented one of the most challenging health emergencies in recent history [1]. Disruptions were widespread, and movement restrictions posed unique challenges to health facilities around the world, particularly in low- and middle-income countries (LMICs) [2]. Vulnerable populations, including adolescents and young adults (AYA), were especially at risk of prolonged service disruptions [3]. AYA are also disproportionately affected by the HIV epidemic, making up 30% of incident HIV globally [4]. Interferences to HIV care due to COVID-19 posed a threat to HIV outcomes within this age group, especially older AYA aged 19–24 years who demonstrate worse outcomes than their younger counterparts [5, 6]. Strategies were urgently needed to avoid or mitigate service disruption to HIV care for this group. The use of digital technology to support provision of remote or virtual HIV services via mHealth (including telemedicine or telehealth) emerged as a common and important strategy for addressing pandemic-related service disruptions [7–12]. This offered a unique opportunity to examine the implementation of mHealth and its determinants when introduced to safeguard access to health services during emergencies.
The specific benefits of mHealth for adolescent HIV services are well known but how these interventions are implemented is less studied [13–16]. In the pandemic, the deployment of mHealth solutions was rapid, sometimes without guidelines, prior assessments of suitability to the context, or adequate formal training of healthcare workers (HCWs) to guide implementation. This kind of rapid implementation necessitated iteration of products or services to fit provider and client needs, as well as the context. Adaptations are formally defined as planned and purposeful changes made to the interventions or delivery strategies while maintaining the integrity of the core components or processes associated with the relevant effectiveness outcomes [17, 18]. Adaptations differ from modifications which are typically viewed as unplanned or spontaneous changes [19]. Although adaptations are intended to introduce improvements, when forced or introduced hurriedly, they may compromise service delivery and effectiveness by lowering feasibility and fidelity of implementation [20]. Studies have shown that HCWs are sometimes not systematic in the development of planned adaptations [21–24]. This is common where cultural adaptations are required to meet diverse needs but evidence on core components of the intervention or strategy is unknown [24]. Many adaptations generated during the pandemic, especially those targeting healthcare workers were ad hoc, making replication and comparison of adaptation procedures across implementation units challenging [7, 10, 25, 26]. Furthermore, the rapid nature of adaptation development may render the adaptations difficult to identify or test and may have a negative impact on implementation fidelity.
The importance of methodically detailing and understanding adaptations has been underscored in recent literature [27–29]. More recently standardized frameworks and language describing ways to develop, document, and describe adaptations have become available [30–34]. These tools offer ways to group and study adaptations by important elements such as the motivation, level of rationale, change idea involved, and targeting of core versus peripheral components of interventions or strategies. Lack of, or partial characterization and comprehension of adaptations limits our ability to identify and prioritize sustainable changes, and impedes the advancement of evidence on how mechanisms of change associated with specific services or interventions lead to outcomes.
The Adolescent Transition to Adult Care for HIV-infected adolescents (ATTACH) study was a cluster randomized trial (NCT03574129) that tested the effectiveness of an Adolescent Transition Package (ATP) in 20 HIV clinics in Kenya [35]. The ATP aimed to prepare youth with HIV as they transition to independent care by increasing HIV knowledge and self-management skills required for independent care [36]. In this trial, frontline HCWs applied continuous quality improvement (CQI) meetings and plan-do-study-act (PDSA) cycles to develop dynamic, provider-led adaptations to phone delivery of the ATP following the onset of the COVID-19 pandemic. In this paper, we characterize the adaptations using the expanded Framework for Reporting Adaptations and Modifications for Implementation Strategies (FRAME-IS) [34]. FRAME-IS provides a consistent approach for describing adaptations. FRAME-IS is derived from FRAME, which specifically focuses on categorizing adaptations to interventions, and can be applied to guide the adaptation process [31]. It comprises four core and three optional modules useful for describing adaptations. The modules document (1) a description of the evidence-based intervention, the implementation strategy, and adaptation; (2) a description of what was modified to obtain the adaptation; (3) the nature of the modification and whether it maintains fidelity to the core components; (4) the goal of the adaptation and the level of the system that had most sway in selection of the adaptation; (5) when in the phases of implementation the adaptation occurred, and if it was planned; (6) specification of individuals or groups participating in the decision to adapt; and (7) the spread of the adaptation within the context of implementation [34]. This paper tests the applicability of FRAME-IS for describing context-specific adaptations made during a pragmatic trial and demonstrates how the framework’s classification system may support the identification of patterns in adaptations selected. We also summarize feedback on implementing the adaptations after a brief testing period. Describing adaptations to the use of digital technology may highlight changes that can inform future actions, in analogous scenarios.
Methods
Setting and study design
This sub-study combines qualitative and quantitative data from the ATTACH study, which was a hybrid cluster randomized controlled trial (RCT) conducted in 4 counties in Kenya (Nairobi, Homa Bay, Kajiado, and Nakuru) [35]. Participants were recruited at 20 HIV comprehensive care clinics (CCCs) selected based on clinic location, size (> 500 clients in care, and ≥ 50 YLH in care), use of electronic medical records, and approval of facility leadership. CCCs are sites for the delivery of coordinated HIV care for adult, adolescent, and pediatric populations. Adolescent HIV care at participating sites is provided free of charge and the CCCs were typically staffed by clinical officers, medical officers, nurses, adherence counselors, and link officers, among others [37]. Ten clinics were randomized to receive the intervention, the ATP, while ten maintained the standard of care.
The ATP includes HCW tools to support the transition process, including a booklet (Taking Charge) designed to guide patient education and empowerment sessions during YLH clinic visits and a tracking tool to document YLH progress through the booklet. The intervention was designed to be delivered in-person by CCC HCWs. HCWs were trained to walk through the booklet step by step to facilitate YLH learning. After each exposure to the booklet, progress was noted in the tracking tool. The trial tested the effectiveness of the ATP and found that those receiving the intervention had significantly higher overall transition readiness scores and higher scores in HIV literacy domain compared to those in the control arm [36]. When COVID-19 social distancing and movement restrictions were put in place, the study pivoted from in-person to phone delivery of the ATP. HCWs made phone calls to YLH once a month for up to one hour to deliver the contents of the ATP. Calls were to be made during work hours at a time determined by each individual HCW. During calls, HCW introduced themselves and checked if YLH were ready to talk. HCW then read through and discussed relevant sections of the ATP.
This study was a partnership between the University of Washington, Kenyatta National Hospital (KNH), and University of Nairobi (UoN). Research ethics approval was granted by the University of Washington Institutional Review Board (UW IRB) and the Kenyatta National Hospital/University of Nairobi Ethics and Review Committee (KNH/UoN ERC). The study protocol is available online (https://pubmed.ncbi.nlm.nih.gov/33268417/). Findings in this paper were reported in accordance with Standards for Reporting Implementation Studies checklist [38].
Participants
HCWs were recruited from among clinic staff who work with YLH at all intervention sites. To enhance the representativeness of the study, we purposively sampled individuals from various cadres including clinical officers, nurses, physicians, counselors, and psychologists. All HCWs involved with the care of YLH at each selected to participate. Willing HCWs provided written consent, emphasizing voluntary participation and the option of opting out at any point without repercussions. HCWs joining clinic sites or clinic activities after the trial began were informed about the study and provided written consent.
Data collection
We collected qualitative data to identify and characterize adaptations and quantitative data to describe the CQI meeetings and participation. We facilitated CQI meetings using PDSA cycles to optimize ATP implementation by phone at ten intervention sites between June 29th and 19th of October 2020. Twice monthly CQI meetings were conducted over 4–5 months with each site completing at least 5 CQI cycles by the end of the adaptation period. A final CQI meeting was held to review all adaptations and gather HCW perspectives on the feasibility, ease, and success of implementing the adaptations. CQI meetings were led by study staff. During meetings, CCC HCWs identified changes to phone delivery of the ATP, evaluated previous adaptations (if any), reflected upon adaptation effectiveness, and decided to adopt, retest, or discontinue an adaptation (adaptation outcomes). The meetings were audio-recorded, and study staff completed PDSA worksheets during meetings to document key elements of the discussion.
We also collected quantitative data to describe the implementation of the phone strategy. For each call made to an adolescent, the following data points were recorded in a call log: when the call was made, who the call was made to, what time the call was made, in what environment the call was received, what chapter of the ATP was discussed and whether the call was successful.
Data processing
Adaptation data were extracted from audio files by a primary analyst and entered in a REDCap-based form which mirrored modules of FRAME-IS and FRAME because adaptations identified in this study were related to both the intervention and the implementation strategy. The select modules were (1) what is being modified, (2) the nature of the modification, (3) the main goal and rationale for the modification, and (4) the spread of the adaptation. Where audibility was a challenge, we utilized CQI facilitator notes and CQI recordings from each site’s final CQI meeting during which all changes made by each site underwent a final review. PDSA worksheets were also consulted in a few circumstances where audio recordings were of poor quality. Most meetings concluded with the identification of one adaptation but some sites selected multiple adaptations per cycle. Two independent primary coders (DM and NC) reviewed each adaptation, classifying adaption characteristics according to framework domains. Together, analysts reviewed the agreement in their coding and discussed convergence and divergence in their understanding of the adaptations. We also categorized adaptations based on whether they focus on the implementation strategy (phone delivery), the evidence-based intervention (the ATP), or both.
Data analysis
We used descriptive statistics to summarize CQI occurrence and duration, call characteristics, adaptation features, and adaptation outcomes using medians and ranges for continuous variables, and sums and proportions for binary or categorical variables. To analyze the adaptation data, we categorized the qualitative data and quantified it. We reported the number of adaptations to phone ATP delivery reported overall and by site, the feature or aspect targeted for adaptation, adaptation types, reasons for adaptations, level of rationale for the adaptation, and the groups targeted by the adaptation. We summarized the adaptation characteristics and the proportion of adaptations focused solely on the implementation strategy (phone delivery), the evidence-based intervention (the ATP), or both.
Results
Over a 4-month period following the introduction of phones for delivery of ATP, 59 CQI meetings were held to facilitate the adaptation process (average of 6 per facility) (Table 1). Meetings included a median of 5 (range: 4–10) frontline HCWs per site and involved a variety of cadres (nurses, clinical officers, peer educators, mentor mothers/fathers, adherence and HIV testing counselors, nutritionists, link officers, and records officers) primarily from CCC and prevention of mother to child transmission clinics. CQI meetings took a median of 21 min (range 13–75).
Table 1.
Summary of CQI meetings and adoption of the ATTACH phone call strategy
| CQI summary | |
| Post-COVID CQI meetings | 59 |
| HCW per CQI (median) | 5 [4-10] |
| Duration (median, minutes) | 21 [13–75] |
| Phone call adoption success | |
| Calls attempts | N = 1444 |
| Calls reaching AYA | 82% (1180) |
| Calls successful | 96% (1137) |
| Phone charged | 99% (1175) |
| Call received in a conducive environment | 96% (1148) |
| Day call was made | N = 566 |
| Weekday | 88% (498) |
| Weekend/public holiday | 12% (68) |
| Time call was made | N = 566 |
| Morning | 28% (158) |
| Afternoon | 57% (323) |
| Evening | 15% (85) |
| At least one chapter discussed | N = 1180 |
| 93% (1096) | |
HCWs made 1444 call attempts, 82% (n = 1180) of which reached YLH. Ninety-six percent (n = 1137) of attempted calls were successful, meaning the HCW was able to discuss relevant ATP content with the adolescent. Most calls were made on weekdays (88%, n = 498), in the afternoon or evening (82%, n = 408), and nearly all calls, 93%, covered at least one chapter of the ATP tool.
Adaptation characteristics
We identified 72 adaptations, 32 of which were unique and mainly targeting the actor or implementer of the phone strategy to improve on HCW organization, workflow, and patient-HCW engagement. Tables 2 and 3 summarize unique adaptations and their characteristics. Most of the adaptations were simple and grounded in one main idea, however, there were a number that comprised multiple ideas but communicated as one adaptation.
Table 2.
Summary of phone strategy adaptations identified across sites during CQI meetings
| Adaptations | Frequency | |
|---|---|---|
| Action | Wait for the next scheduled clinic visit/Default to in-person | 5 |
| Provide shortened time to the next in-person clinic visit | 1 | |
| Schedule calls in advance, increase airtime, and shuffle HCWs | 2 | |
| Simplify language | 1 | |
| Add interactive elements | 1 | |
| Obtain/use alternate contact information | 7 | |
| Define notation for documenting client progress | 1 | |
| Total | 16 | |
| Actor | Divide adolescents among HCWs | 10 |
| Designate a specific cadre responsible for follow-up calls | 1 | |
| Reduce staff making calls and create targets | 1 | |
| Match HCW to client based on client language needs and assess understanding | 4 | |
| Use CHV/link person/community drug distribution to locate adolescent | 7 | |
| Create priority list to organize HCW access to phone | 1 | |
| Prioritizing HCWs going on leave and handing over pending clients | 1 | |
| Shuffling HCWs who are making calls | 2 | |
| Assign a specific cadre to oversee proper documentation | 1 | |
| Total | 28 | |
| Setting | Calling after hours | 3 |
| Carry phone home for afterhours calls | 1 | |
| Total | 4 | |
| Target | Ask clients to document important details | 1 |
| Target calls to caregivers | 3 | |
| Assign clients memorization activities and check recall | 2 | |
| Create a priority list based on adolescents with the fewest call attempts and schedule | 1 | |
| Implementing pre-calls to schedule and prepare adolescents | 8 | |
| Total | 15 | |
| Timing | Call at different times of day | 2 |
| Postponing calls during heavy workload seasons | 1 | |
| Designating call days | 1 | |
| Total | 4 | |
| Frequency | Repetition of ATP chapters | 2 |
| Repeating call attempts | 4 | |
| Increase volume of calls attempts made per day | 1 | |
| Total | 7 | |
| Dose | Spreading material over several calls | 1 |
| Reduce material covered during call and match clients’ language needs | 1 | |
| Total | 2 |
Frequencies represent unique or first-time appearances of an adaptation at each site. If a facility sustains a unique adaptation, it is not counted repeatedly. Some adaptations are a combination of > 1 change and may target different components of the phone strategy
Table 3.
Summary of the application of FRAME-IS AND FRAME to the ATTACH Phone Strategy
| The EBP being implemented is: The Adolescent Transition Package | |
| The Implementation Strategy being modified is: the phone delivery strategy | |
| Specification of the implementation strategy | |
| Action: Making a phone call | |
| Actor: Frontline HCW at CCC clinics | |
| Context/Setting: CCC clinics | |
| Target: YLH | |
| Timing: During working hours (8am–5 pm) | |
| Frequency: Once a month | |
| Dose: One chapter per call for up to 45 min | |
| The modifications being made are: | See Table 1 and Appendix 1 |
| The reasons for modification are: | Low phone ownership |
| Incorrect phone numbers | |
| Challenges incorporating calls to workflow | |
| Low-quality call experience | |
| Fear of unintended disclosure | |
| Scheduling conflict | |
| (See Appendix 1 for extensive list) | |
| What is modified: | Context (format, personnel, and setting) |
| Content | |
| Evaluation procedures | |
| What is the nature of the content, evaluation, or training modification? | Adding, tailoring, spreading |
| Relationship to core elements: | NA |
| What is the goal: | Increase adoption |
| Increase reach | |
| Increase fit | |
| Increase feasibility | |
| Increase fidelity and effectiveness | |
| What is the level of the adaptation rationale? | Implementer and patient level |
| When is the modification initiated? | Mid-implementation phase |
| Is the modification planned? | Planned/proactive |
| Who participants in the adaptation decision? | Entire team of implementers/care team |
| How widespread is the modification? | All implementers and patients |
| Sub-sets of implementers and patients who share similar characteristics | |
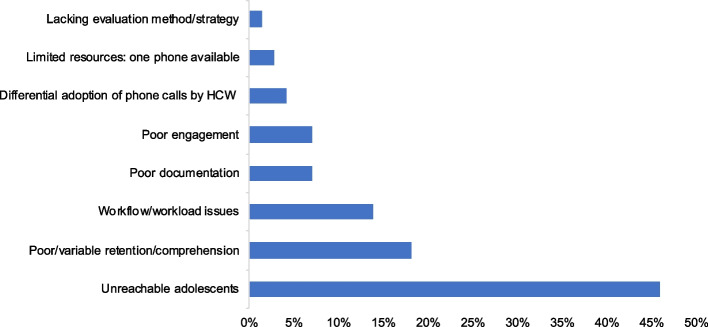
The reasons for adaptations were varied and constituted challenges in implementing the phone strategy or reaching YLH. HCWs most frequently adapted how they were implementing phone delivery to address barriers such as difficulties reaching YLH because of missing or incorrect contact information, scheduling challenges, low phone ownership in this group, limited availability of youth, and fear of unintended disclosure which manifested in YLH refusing or ending calls without warning (Fig. 1, Appendix 1). The phone strategy had limited success where YLH were sharing phones with unsupportive caregivers, siblings, or partners. HCW-level barriers that drove the decision to adapt were also identified. For example, initially, some HCWs did not consider making phone calls part of their job. Only one phone was available to HCWs at each site, forcing HCWs to share access. HCWs also experienced burdensome workloads, especially during reporting periods when the majority of their time was spent collating files, documenting, and enumerating outcomes. Decline in staffing numbers due to COVID-19 infection was also common.
Fig. 1.
Reasons for adaptations across all intervention sites (n = 10)
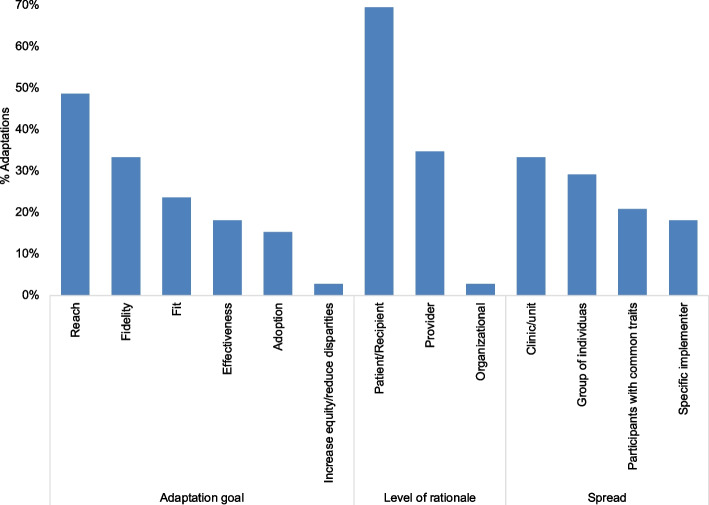
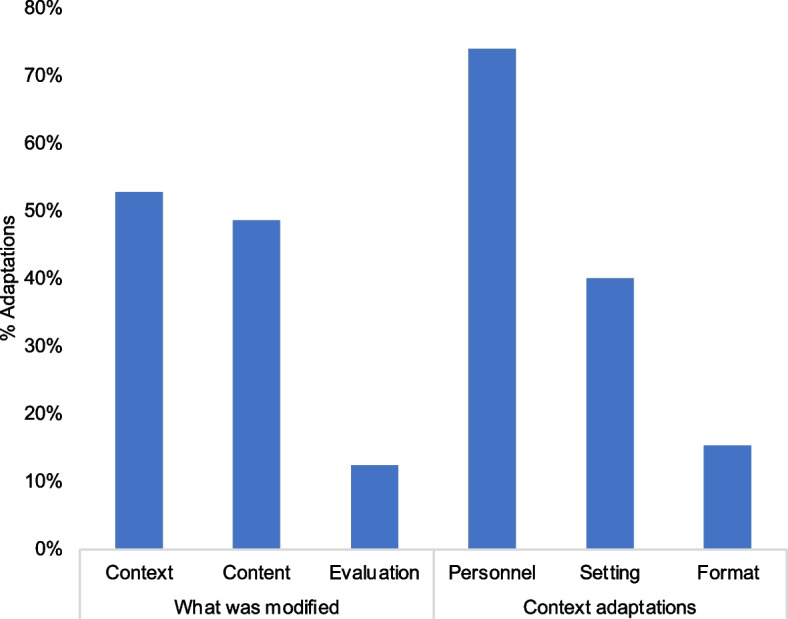
Adaptations were primarily context adaptions (53%, n = 38); 28 adaptations involved only context changes (Fig. 2, Appendix 1) These featured personnel (74%, n = 26) and setting (40%, n = 14) changes affecting the overall way the phone strategy was delivered. Personnel-related context adaptations included sharing of tasks among available staff, prioritizing phone use for HCWs based on an agreed-upon schedule, or redistribution of tasks to HCWs with more availability, or with better rapport or language skills compatible with specific YLH.
Fig. 2.
Targets of adaptations across all intervention sites (n = 10)
The frequency of content adaptations was similar to context adaptations (49%, n = 35, with 28 exclusively classified as such). Lastly, we noted 13% (n = 9) evaluation adaptations to respond to the need to document and evaluate the progress YLH made during calls. The nature of content and evaluation adaptations ranged from addition of discrete elements like questions or the use of scripts (32%, n = 20), focused refinements or tailoring (8%, n = 5), repetition for example repeating calls or repeating call content (15%, n = 9), shortening (2%, n = 1), spreading material over several calls (5%, n = 3) and integration of home tracing using community health volunteers as another strategy alongside the phone strategy (8%, n = 5; Fig. 3). There were several instances of drift with return (8%, n = 5) to the original strategy. For example, when YLH could not be reached at all HCWs resorted to inviting them to attend clinic visits to discuss the ATP.
Fig. 3.
Nature of content and evaluation adaptations across all intervention sites (n = 10)
The goals of the adaptations were most frequently to increase reach (49%, n = 35), fidelity of implementation (33%, n = 24), and fit of the strategy to the HCWs’ schedules, preferences, environment, and workload (24%, n = 17; Fig. 4). Improving effectiveness of the intervention was less frequently discussed and, in some instances, co-occurred with the fidelity goal. The same was noted with adoption, which co-occurred with a few discussions about improving the reach and fit of the strategy.
Fig. 4.
Goals, level of rationale, and spread of adaptations across all intervention sites (n = 10)
The level of the organization that most directly informed the adaptations was the recipient level (69%, n = 50), aligning with the goal of increasing the number of calls reaching YLH (Fig. 4). There was also much focus on adaptation rationale from the HCW level (35%, n = 25) which influenced the selection of modifications that aimed at improving adoption by removing or reducing workflow-related barriers. We noted that majority of adaptations were intended to reach all HCWs in the implementing unit (33%, n = 24) and all YLH clients receiving the ATP intervention (29%, n = 21; Fig. 4). Targeted adaptations were present but less frequent: 21% (n = 15) for youth with specific characteristics or issues and 18% (n = 13) for individual implementers whose specific role, skills, or experience were leveraged to address client- or HCW-level barriers.
Site-level differences
Comparison of adaptations across sites demonstrated that sites were tackling similar challenges to phone-based ATP delivery and conceived of similar adaptations. A few differences were in the number of adaptations per site: the median number of adaptations per site was 7 (range: 4–11) and some variation across sites in what was modified. For example, one facility implemented context adaptations exclusively while another had 25% context modifications and 75% content modifications. For all facilities, most context modifications involved format changes except for one facility that primarily implemented personnel-related adaptations. Only six facilities enacted evaluation adaptations. Figure 5 summarizes the variation in adaptation characteristics across sites.
Fig. 5.
Heatmap summarizing characteristics of adaptations, overall and by site
Outcomes of adaptation implementation
HCWs perceived that 96% (n = 69) of adaptations made implementation of the phone strategy more feasible than before the change was introduced. Overall, 83% (n = 60) of the adaptations were perceived to make delivery of the phone strategy easier than when there was no adaptation (Table 4). Temporary or permanent migration of adolescents, phones that were turned off, wrong numbers and a reduction in number of staff available to make calls due to COVID-19 infection are examples of factors that made phone delivery of the ATP less successful. After testing, most adaptations were either incorporated immediately into routine workflows (47%) or selected for further testing and then adopted after secondary review (47%) (Table 4). Very few adaptations were abandoned after testing (6%): for example, home visits that leveraged community health volunteers (CHVs) were abandoned at one site because of lack of funds to support that cadre’s activities.
Table 4.
Outcomes of implementing adaptations to the phone strategy, overall and by site
| N = number of adaptations | All (N = 72) | Site 1 (N = 7) | Site 2 (N = 6) | Site 3 (N = 7) | Site 4 (N = 10) | Site 5 (N = 6) | Site 6 (N = 8) | Site 7 (N = 6) | Site 8 (N = 7) | Site 9 (N = 4) | Site 10 (N = 11) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Implementation of adaption went as planned: | 96% (69) | 86% (6) | 100% (6) | 100% (7) | 100% (10) | 100% (6) | 100% (8) | 100% (6) | 100% (7) | 75% (3) | 91% (10) |
| Phone delivery after adaptation easier than in-person: | 83% (60) | 86% (6) | 100% (6) | 71% (5) | 100% (10) | 100% (6) | 63% (5) | 83% (5) | 71% (5) | 75% (3) | 91% (10) |
| Decisions made after adaptation testing: | |||||||||||
| Adapt | 47% (34) | 14% (1) | 67% (4) | 86% (6) | 40% (4) | 50% (3) | 25% (2) | 50% (3) | 71% (5) | 25% (1) | 27% (3) |
| Adopt | 47% (34) | 86% (6) | 33% (2) | 14% (1) | 60% (6) | 50% (3) | 38% (3) | 50% (3) | 14% (1) | 75% (3) | 73% (8) |
| Abandon | 6% (4) | - | - | - | - | - | 38% (3) | - | 14% (1) | - | - |
HCWs recommended the use of the WhatsApp platform to augment the phone strategy by facilitating individual or group communication, sharing of ATP text and pictures, and allowing storage of information in text form so that adolescents can refer to it when needed. Other recommendations from HCWs included providing shorter times to clinic appointments, providing phones to clients, increasing airtime allocation, and increasing the number of phones available to HCWs. The use of video calls was suggested to improve the remote visit experience. HCWs also felt increasing call frequency may help adolescents retain what they have learned.
Discussion
The objective of our study was to characterize dynamic, provider-led adaptations to phone delivery of the ATP using FRAME-IS. We found that adaptation was a feasible way of addressing barriers to continuity of transition support care for YLH during the early stages of the COVID-19 pandemic. FRAME -IS was a useful tool for characterizing and understanding adaptations (summarized in Table 3). Adaptations were similar across all sites and originated from 32 unique ideas. The inability to reach clients was a recurrent reason for adaptations. The need for adaptations emerged from challenges integrating the phone delivery strategy into their workload and workflow. We identified primarily context adaptations which were frequently intended for the whole care team or all YLH receiving the intervention. To our knowledge, this is the first study in our setting to characterize adaptations using FRAME-IS.
In our study, the main motivation for proposing adaptations was to improve the reach of the phone strategy. HCWs were unable to reach adolescents for a variety of reasons. For example, when called, YLH were busy, with many competing interests which resulted in scheduling conflicts. There were also frequent refusals to answer calls or abrupt ending of calls because of fear of unintended disclosure. Limited phone ownership was also a common challenge in this population and many YLH were reliant on phones owned by a caregiver, sibling, or partner. Uptake of the phone strategy was impacted by scheduling conflicts with caregivers or the unwillingness of caregivers, sibling, or partner to support the client by availing the phone at necessary times, for a sufficient duration, or fostering privacy and confidentiality needed by the adolescents. These and other barriers appear elsewhere in literature examining the implementation of digital technologies for health [39, 40]. Additionally, the role of stigma on youth engagement with health services is not new and has an impact on adoption and uptake of health services in the clinic setting as well as virtually [41, 42]. Our study demonstrates how using CQIs facilitated the identification of challenges and the selection of adaptations to address them successfully.
Addressing barriers in the HCW workflow was another important motivation for adaptations to phone delivery. At each facility, HCW were sharing one phone to implement the strategy and were not always able to complete their call loads when scheduled at the same time as other colleagues. The addition of new activities to their workflow at times conflicted with pre-existing responsibilities. For instance, HCWs found it hard to adopt the phone strategy during monthly reporting periods when the majority of their time was required to collate reports. Key adaptations useful for improving reach beyond the trial were scheduling calls ahead of time and incorporating separate preparatory calls targeted to caregivers. HCW identified these changes as priorities for long-term integration into their routine activities. This trial exemplified how frontline HCWs in our context can be engaged in adaptation selection and testing to mitigate challenges in accessing health services. This was especially important during the pandemic when health systems were facing staffing shortages due to illness or redistribution of HCWs to areas of highest need, interruptions in the supply chain, and reallocation of financial resources.
Most adaptations involved context changes, that is tweaking the way the phone strategy was delivered. In implementation science, context refers to the constellation of cultural, organizational, social, financial, and leadership aspects that influence how an innovation or strategy is provided or received. Given that all these spheres were affected by the pandemic in one way or another, the frequency of context adaptations is not unexpected [25, 43, 44]. For example, task shifting aspects of phone delivery to community health workers was a context adaptation to address gaps in reaching adolescents when they failed to answer calls or lacked contact information in their patient files.
The rest of the adaptations we identified were primarily content changes achieved by making simple additions or refinements to the intervention. In our scenario, these kinds of simple adaptations may represent opportunities for optimization that are low-lying-fruit as they neither required extensive time nor resources and would introduce minimal disruption to the overall functioning of the health system. Simple adaptations make sense where HCWs are not trained in the language and concepts of adaptations or improvement science. Nonetheless, it was highly advantageous to involve frontline HCWs, including members of informal cadres like mentor mothers or fathers, in the adaptation process. Their proximity to clients, opportunity for rapport-building, and familiarity with clients provided access to information necessary to customize and optimize phone delivery of the ATP to their needs and contexts. Engaging community perspectives is important for leveraging local knowledge and expertise to create programs that are relevant and customized to the target population, to encourage trust-building, and to promote positive and sustainable involvement in facility-based care [19, 45, 46].
Post-CQI evaluations underscore the acceptability, feasibility, and appropriateness of the adaptations as most of them were either adopted immediately after testing or adapted and then adopted after a second round of testing. However, the occurrence of drifts from the strategy cannot be ignored: we identified nine instances where the adaptation involved abandoning the phone strategy because previous adaptations were infeasible or unsuccessful. For example, the use of CHVs was limited by a lack of funds to support their commute. The phone strategy was also abandoned when HCW identified certain individuals’ inability to retain information, or who were virally unsuppressed and required further clinical examination. The limited capacity of telemedicine for physical examination, HCW-patient relationship-building, and as a medium for patient education has been noted as a persistent barrier and fuel for HCWs’ resistance to the use of this and other digital health strategies [40, 43, 47].
Of note, the use of WhatsApp to deliver the ATP intervention was proposed up to three times across all CQI meetings but not selected for testing in the PDSA cycle. HCWs in non-clinical cadres who are primarily tasked with retaining clients in care noted that communication via WhatsApp had been effective for maintaining contact, information sharing including appointment reminders, and engaging youth in support groups. The feasibility and success of using WhatsApp for reaching adolescents has been identified in several studies [41, 44, 48]. The novelty of the application, affordability of data required to operate it, capacity for text and voice messages, video calls, and sharing of documents, exemplify the youth-friendliness of the platform, making it a promising avenue for improving the ATTACH phone strategy and other mHealth interventions. More work is needed to explore the best ways of utilizing this technology to support YLH transitioning out of pediatric care.
FRAME-IS is the first tool developed specifically to address modifications and adaptations to implementation strategies. Its modular structure and flexibility make it an apt and systematic tool for classifying the adaptations. Few studies have applied FRAME-IS to track and/or characterize adaptations [49–54], but more examples are needed to explore the range of its utility for Implementation Science and to identify areas of improvement. Currently, FRAME-IS is not designed to capture or describe adaptation outcomes and may benefit from incorporating a module that does this. An outcomes module may inspire a more careful selection of adaptations. Within LMICs, tracking outcomes may provide the information needed by frontline HCWs in LMICs to focus adaptations. One study merged FRAME-IS and RE-AIM frameworks so that HCWs could leverage reach and adoption outcomes to track progress following a given adaptation [50]. This allowed the teams to compare between adaptations and select for the high-yield ones. Future work may focus on cataloging adaptations that support the best yield in clinics, including their FRAME-IS-defined characteristics. This resource would introduce efficiencies to adaptation development by allowing HCWs to focus on identifying solutions that fit their context or reconfiguring adaptation characteristics of select ideas to improve fit and feasibility in their clinics. Incorporating more instructions and a user-friendly design to guide the process of adaptation selection and specification may increase use of FRAME-IS among adaptation teams. This could support real-time documentation and characterization of adaptations and may offer more benefits to implementers than the retrospective application of the framework. Furthermore, there is room to strengthen our understanding of adaptations and their downstream influence on outcomes by adding another module that documents micro-contextual changes coinciding with the introduction of adaptations, for example when trained HCWs transfer out or a champion for the strategy emerges within the care team.
This study used PDSA protocols to structure the adaptation process, thereby introducing a degree of methodological rigor. Guided by research staff who introduced in simple terms the process and importance of this approach, HCWs engaged in consensus discussions to identify context-specific adaptations. However, we observed that leading and coaching teams to identify specific change concepts or ideas was challenging. The implementation team may have benefited from broad knowledge about the range of changes possible and linkages between barriers and adaptations that are most suited to address them.
Although we were able to characterize the adaptations, we noted that the coding process was challenging. Coding directly from audio-recordings to structured forms defining FRAME-IS modules was not a 1:1 process; it involved condensing a lot of information to fit the discrete modules. In some cases, overlap in the categorization of adaptations was unavoidable. The groups within the modules did not always allow for parsimonious characterization such that some adaptations fell into several categories at the same time. Additionally, it was challenging to apply it to adaptations that were an amalgamation of several change ideas e.g., an adaptation that consists of an additional element delivered at a different frequency by a different cadre of HCW. This may impact our ability to recognize patterns or associations in adaptation data when examining and comparing across similar studies. Lastly, the categorization of adaptations was retrospective, and coding was done by researchers. Real-time, prospective characterization of the adaptations using forms or checklists modeled after FRAME-IS may be an advantageous approach, especially in the context of a pandemic or other emergencies. We note that rapid qualitative analysis using FRAME-IS as a coding guide may be a game-changer in ensuring that adaptation data can be fed back to facilities and policy makers within a shorter timeline [55, 56].
Study limitations
The extraction and characterization of adaptation data happened retrospectively and relied primarily on audio recordings that were of variable quality. However, we overcame this issue by looking to data in PDSA forms for clarification. CQI process differed from site to site. There was a degree of subjectivity in the way the meetings were structured and run, which depended on the ATTACH staff. For example, not all teams discussed what to do with the adaptation after two weeks of testing during the meeting. In some cases, the decision was made and captured two or three CQI meetings later. It is possible that the experiences and variation of adaptations presented in this study may not mirror what is possible in other contexts. In this study we attempted to track implementation outcomes linked to each adaptation using a survey, however, due to pandemic-related protocol changes these data were incomplete and insufficient for inclusion. We also did not specify core versus peripheral elements of the phone strategy to HCWs nor assess their fidelity to the implementation strategy. Therefore, we were unable to ascribe changes in study outcomes to specific adaptations.
Conclusion
Knowledge that interventions are not always effective when transferred to new contexts provides impetus for further study of the role of adaptations. The need for rapid adaptation is also underscored in significant emergencies like the COVID-19 pandemic which introduce sudden changes in the immediate context. To study adaptations, it is important to identify, document, and evaluate them, while considering the dynamism of implementation contexts. In this study, we saw how the introduction of adaptations allowed frontline HCWs to introduce and implement solutions that impacted their ability to adopt the phone delivery strategy. We identified and characterized a range of challenges associated with phone delivery of the ATP, which may occur at other facilities if we were to scale out to new clinics. Using FRAME-IS we classified what were a majority of context adaptations to address these gaps. This study adds to the literature describing a range of possible adaptations which allowed HCWs to maintain engagement with clients during the COVID-19 pandemic when many health systems experienced prolonged service interruptions. Additionally, it demonstrates the utility of FRAME-IS and adds to existing examples of its application in research.
Supplementary Information
Additional file 1: Appendix 1. Adaptations Coding
Acknowledgements
We would like to acknowledge all the healthcare workers at each of the study facilities and all the study participants for taking time to contribute to this research. We also thank the research assistants for their work leading the CQI meetings. We gratefully acknowledge and thank the Ministry of Health representatives from Kisumu, Siaya, Homa Bay, and Nairobi counties. Additionally, we would like to acknowledge all the research staff at the Research & Programs Department, Kenyatta National Hospital, Department of Paediatrics and Child Health, University of Nairobi, and University of Washington, that made this trial possible.
Abbreviations
- YLH
Youth living with HIV
- ATP
Adolescent Transition Package
- ATTACH
Adolescent Transition to Adult Care for HIV-infected adolescents
- HCW
Healthcare worker
- CQI
Continuous quality improvement
- PDSA
Plan Do Study Act
- FRAME-IS
Framework for Reporting Adaptations and Modifications to Evidence-based Implementation Strategies
- CCC
Comprehensive care clinic
Authors’ contributions
KBS, IN, and GJS wrote the proposal and secured the funding for this trial. KBS, IN, GJS, CM, and DW drafted the study protocol, obtained ethical approvals, developed the study forms, and oversaw the collection of all study data. DW, CM, AO, and CM oversaw implementation research activities in Kenya. DM developed the analysis plan for this work with feedback from ARM and BJW. DM analyzed the data with support from NC. KBS, CM, AO, and DM had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. DM drafted the manuscript, which was reviewed and edited by all authors. All authors approved the manuscript for publication.
Funding
This work was supported by NIH/NICHD 1R01HD089850, NIH/FIC D43TW009783 (IN), NIH/FIC AHISA Small Grant Award, CRDF Global, G-202012–67159, and the UW Global Center for Integrated Health of Women, Adolescents and Children (Global WACh).
Availability of data and materials
The processed data supporting the conclusions of this article are included within the article (and its additional file(s)). The source data from the study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Research ethics approval was granted by the University of Washington Institutional Review Board (UW IRB) and the Kenyatta National Hospital Ethics and Review Committee (KNH ERC).
Consent for publication
All authors included have received and reviewed previous and current versions of the manuscript and have consented to its submission for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. COVID-19 weekly epidemiological update, edition 83, 6 July 2022. World Health Organization; 2022.
- 2.World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. World Health Organization; 2020.
- 3.Govender K, Cowden RG, Nyamaruze P, Armstrong RM, Hatane L. Beyond the disease: Contextualized implications of the COVID-19 pandemic for children and young people living in Eastern and Southern Africa. Front Public Health. 2020;8:504. doi: 10.3389/fpubh.2020.00504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS. Young People and HIV. https://www.unaids.org/sites/default/fles/media_asset/ young-people-and-hiv_en.pdf (2021).
- 5.Slogrove, A. L., Mahy, M., Armstrong, A. & Davies, M. A. Living and dying to be counted: What we know about the epidemiology of the global adolescent HIV epidemic. Journal of the International AIDS Society vol. 20 Preprint at 10.7448/IAS.20.4.21520 (2017). [DOI] [PMC free article] [PubMed]
- 6.Jewell BL, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. The Lancet HIV. 2020;7:e629–e640. doi: 10.1016/S2352-3018(20)30211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Golin, R. et al. PEPFAR’s response to the convergence of the HIV and COVID-19 pandemics in Sub-Saharan Africa. Journal of the International AIDS Society vol. 23 Preprint at 10.1002/jia2.25587 (2020). [DOI] [PMC free article] [PubMed]
- 8.Wood SM, et al. Outcomes of a Rapid Adolescent Telehealth Scale-Up During the COVID-19 Pandemic. J Adolesc Health. 2020;67:172–178. doi: 10.1016/j.jadohealth.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guaraldi G, Milic J, Martinez E, Kamarulzaman A, Mussini C, Waters L, Pozniak A, Mallon P, Rockstroh JK, Lazarus JV. Human Immunodeficiency Virus (HIV) Care models during the coronavirus disease 2019 (COVID-19) Era. Clin Infect Dis. 2021;73(5):e1222–7. doi: 10.1093/cid/ciaa1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. 2020;67(2):164-71. 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed]
- 11.Slater, H., Campbell, J. M., Stinson, J. N., Burley, M. M. & Briggs, A. M. End User and implementer experiences of mhealth technologies for noncommunicable chronic disease management in young adults: Systematic review. Journal of Medical Internet Research vol. 19 Preprint at 10.2196/jmir.8888 (2017). [DOI] [PMC free article] [PubMed]
- 12.El-Nahal WG, Shen NM, Keruly JC, Jones JL, Fojo AT, Lau B, Manabe YC, Moore RD, Gebo KA, Lesko CR, Chander G. Telemedicine and visit completion among people with HIV during the coronavirus disease 2019 pandemic compared with prepandemic. AIDS. 2022;36(3):355–62. doi: 10.1097/QAD.0000000000003119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcolino, M. S. et al. The impact of mHealth interventions: Systematic review of systematic reviews. JMIR mHealth and uHealth vol. 6 Preprint at 10.2196/mhealth.8873 (2018). [DOI] [PMC free article] [PubMed]
- 14.Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PloS one. 2017;12(2):e0170581. 10.1371/journal.pone.0170581. [DOI] [PMC free article] [PubMed]
- 15.Hamine, S., Gerth-Guyette, E., Faulx, D., Green, B. B. & Ginsburg, A. S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. Journal of Medical Internet Research vol. 17 Preprint at 10.2196/jmir.3951 (2015). [DOI] [PMC free article] [PubMed]
- 16.Scott Kruse, C. et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare vol. 24 Preprint at 10.1177/1357633X16674087 (2018). [DOI] [PMC free article] [PubMed]
- 17.Stirman SW, Gamarra J, Bartlett B, Calloway A, Gutner C. Empirical Examinations of Modifications and Adaptations to Evidence-Based Psychotherapies: Methodologies, Impact, and Future Directions. Clin psychol. 2017;24:396–420. doi: 10.1111/cpsp.12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiltsey Stirman S, et al. Relationships between clinician-level attributes and fidelity-consistent and fidelity-inconsistent modifications to an evidence-based psychotherapy. Implement sci. 2015;10:115. doi: 10.1186/s13012-015-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans, R. E., Moore, G., Movsisyan, A. & Rehfuess, E. How can we adapt complex population health interventions for new contexts? Progressing debates and research priorities. 10.1136/jech-2020-214468. [DOI] [PMC free article] [PubMed]
- 20.Castro FG, Yasui M. Advances in EBI development for diverse populations: Towards a science of intervention adaptation. Prev Sci. 2017;18:623–9. doi: 10.1007/s11121-017-0809-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen EK, Reid MC, Parker SJ, Pillemer K. Tailoring evidence-based interventions for new populations: a method for program adaptation through community engagement. Eval Health Prof. 2013;36(1):73–92. doi: 10.1177/0163278712442536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, Gelaude D, Carey JW, ADAPT team. Adapting evidence–based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(supp):59–73. 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed]
- 23.Prisco V, Prisco L, Donnarumma B. Telepsychiatry in adults and adolescents: A useful tool against CoViD-19. Recenti Prog Med. 2020;111:411–414. doi: 10.1701/3407.33923. [DOI] [PubMed] [Google Scholar]
- 24.Domenech-Rodríguez M, Wieling E. Developing Culturally Appropriate, Evidence-Based Treatments for Interventions with Ethnic Minority Populations. Voices of Color: First-Person Accounts of Ethnic Minority Therapists. 2012 doi: 10.4135/9781452231662.n18. [DOI] [Google Scholar]
- 25.Linnemayr S, et al. HIV Care Experiences During the COVID-19 Pandemic: Mixed-Methods Telephone Interviews with Clinic-Enrolled HIV-Infected Adults in Uganda. AIDS Behav. 2021;25:28–39. doi: 10.1007/s10461-020-03032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galle A, Semaan A, Huysmans E, Audet C, Asefa A, Delvaux T, Afolabi BB, El Ayadi AM, Benova L. A double-edged sword—telemedicine for maternal care during COVID-19: findings from a global mixed-methods study of healthcare providers. BMJ Glob Health. 2021;6(2):e004575. 10.1136/bmjgh-2020-004575. [DOI] [PMC free article] [PubMed]
- 27.Bunger AC, Powell BJ, Robertson HA, MacDowell H, Birken SA, Shea C. Tracking implementation strategies: a description of a practical approach and early findings. Health Res Policy and Syst. 2017;15(1):1–2. doi: 10.1186/s12961-017-0175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haley AD, Powell BJ, Walsh-Bailey C, Krancari M, Gruß I, Shea CM, Bunce A, Marino M, Frerichs L, Lich KH, Gold R. Strengthening methods for tracking adaptations and modifications to implementation strategies. BMC Med Res Methodol. 2021;21(1):1–2. doi: 10.1186/s12874-021-01326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walsh-Bailey C, Palazzo LG, Jones SM, Mettert KD, Powell BJ, Wiltsey Stirman S, Lyon AR, Rohde P, Lewis CC. A pilot study comparing tools for tracking implementation strategies and treatment adaptations. Implement Res Pract. 2021;2:26334895211016028. 10.1177/26334895211016028. [DOI] [PMC free article] [PubMed]
- 30.Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implement Sci. 2013 doi: 10.1186/1748-5908-8-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stirman SW, Baumann AA, Miller CJ. The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. 2019 doi: 10.1186/s13012-019-0898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Powell BJ, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. 2012;69:123–157. doi: 10.1177/1077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Powell BJ, et al. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller CJ, Barnett ML, Baumann AA, Gutner CA, Wiltsey-Stirman S. The FRAME-IS: a framework for documenting modifications to implementation strategies in healthcare. Implement Sci. 2021;16:1–2. 10.1186/s13012-021-01105-3. [DOI] [PMC free article] [PubMed]
- 35.Njuguna IN, et al. Adolescent transition to adult care for HIV-infected adolescents in Kenya (ATTACH): study protocol for a hybrid effectiveness-implementation cluster randomised trial. BMJ Open. 2020;10:e039972. doi: 10.1136/bmjopen-2020-039972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Njuguna IN, et al. Transition to independent care for youth living with HIV: a cluster randomised clinical trial. Lancet HIV. 2022;9:e828–e837. doi: 10.1016/S2352-3018(22)00244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Njuguna I, et al. What happens at adolescent and young adult HIV clinics? A national survey of models of care, transition and disclosure practices in Kenya. Trop Med Int Health. 2020;25:558–65. doi: 10.1111/tmi.13374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pinnock H, et al. Standards for Reporting Implementation Studies (StaRI): explanation and elaboration document. BMJ Open. 2017;7:e013318. doi: 10.1136/bmjopen-2016-013318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. 2014;14:188. doi: 10.1186/1471-2458-14-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goldstein, M. et al. Systematic Review of mHealth Interventions for Adolescent and Young Adult HIV Prevention and the Adolescent HIV Continuum of Care in Low to Middle Income Countries. AIDS Behav 1–22 (2022) 10.1007/s10461-022-03840-0. [DOI] [PMC free article] [PubMed]
- 41.Zanoni BC, et al. Mobile Phone-Based Intervention Among Adolescents Living With Perinatally Acquired HIV Transitioning from Pediatric to Adult Care: Protocol for the Interactive Transition Support for Adolescents Living With HIV using Social Media (InTSHA) Study. JMIR Res Protoc. 2022;11:e35455. doi: 10.2196/35455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cornell M, Dovel K. Reaching key adolescent populations. Curr Opin HIV AIDS. 2018;13:274–280. doi: 10.1097/COH.0000000000000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Armand K, et al. Telemedicine and COVID-19: Experience of Medical Doctors in Cameroon. Am J Health, Med Nurs Pract. 2021;6:32–37. doi: 10.47672/ajhmn.666. [DOI] [Google Scholar]
- 44.Dambi J, et al. A Digital Mental Health Intervention (Inuka) for Common Mental Health Disorders in Zimbabwean Adults in Response to the COVID-19 Pandemic: Feasibility and Acceptability Pilot Study. JMIR mental health. 2022;9:e37968. doi: 10.2196/37968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jain M, et al. Use of community engagement interventions to improve child immunisation in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2022;12:e061568. doi: 10.1136/bmjopen-2022-061568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Denison JA, et al. Youth engagement in developing an implementation science research agenda on adolescent HIV testing and care linkages in sub-Saharan Africa. AIDS (London, England) 2017;31(Suppl 3):S195–S201. doi: 10.1097/QAD.0000000000001509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moyo J, Madziyire G. Use of telemedicine in obstetrics and gynaecology in Zimbabwe during a lockdown period. Pan Afr Med J. 2020;35:89. doi: 10.11604/pamj.supp.2020.35.2.23675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chory A, et al. A Pilot Study of a Mobile Intervention to Support Mental Health and Adherence Among Adolescents Living with HIV in Western Kenya. AIDS Behav. 2022;26:232–242. doi: 10.1007/s10461-021-03376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zehner ME, et al. Electronic health record closed-loop referral (‘eReferral’) to a state tobacco quitline: a retrospective case study of primary care implementation challenges and adaptations. Implement sci commun. 2022;3:107. doi: 10.1186/s43058-022-00357-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sjoberg H, Kenney RR, Morgan B, Connelly B, Jones CD, Ali HN, Battaglia C, Gilmartin HM. Adaptations to relational facilitation for two national care coordination programs during COVID-19. Front Health Serv. 2022;2:952272. 10.3389/frhs.2022.952272. [DOI] [PMC free article] [PubMed]
- 51.Legenza L, et al. Application of consolidated framework for implementation research to improve Clostridioides difficile infection management in district hospitals. Res social adm pharm. 2022;18:4100–4111. doi: 10.1016/j.sapharm.2022.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quimby KR, et al. Adaptation of a community-based type-2 diabetes mellitus remission intervention during COVID-19: empowering persons living with diabetes to take control. Implement sci commun. 2022;3:5. doi: 10.1186/s43058-022-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arena, L. et al. Modifications in Primary Care Clinics to Continue Colorectal Cancer Screening Promotion During the COVID-19 Pandemic. Journal of community health 1–14 (2022) 10.1007/s10900-022-01154-9. [DOI] [PMC free article] [PubMed]
- 54.De Geest S, et al. The SMILe integrated care model in allogeneic SteM cell TransplantatIon faciLitated by eHealth: a protocol for a hybrid effectiveness-implementation randomised controlled trial. BMC Health Serv Res. 2022;22:1067. doi: 10.1186/s12913-022-08293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open. 2018;8:e019993. doi: 10.1136/bmjopen-2017-019993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Keith RE, Crosson JC, O’Malley AS, Cromp DA, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: A rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017 doi: 10.1186/s13012-017-0550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. Adaptations Coding
Data Availability Statement
The processed data supporting the conclusions of this article are included within the article (and its additional file(s)). The source data from the study are available from the corresponding author on reasonable request.