Abstract
Background
There is growing awareness that sex differences are associated with different patient outcomes in a variety of diseases. Studies investigating the effect of patient sex on sepsis-related mortality remain inconclusive and mainly focus on patients with severe sepsis and septic shock in the intensive care unit. We therefore investigated the association between patient sex and both clinical presentation and 30-day mortality in patients with the whole spectrum of sepsis severity presenting to the emergency department (ED) who were admitted to the hospital.
Materials and methods
In our multi-centre cohort study, we retrospectively investigated adult medical patients with sepsis in the ED. Multivariable analysis was used to evaluate the association between patient sex and all-cause 30-day mortality.
Results
Of 2065 patients included, 47.6% were female. Female patients had significantly less comorbidities, lower Sequential Organ Failure Assessment score and abbreviated Mortality Emergency Department Sepsis score, and presented less frequently with thrombocytopenia and fever, compared to males. For both sexes, respiratory tract infections were predominant while female patients more often had urinary tract infections. Females showed lower 30-day mortality (10.1% vs. 13.6%; p = .016), and in-hospital mortality (8.0% vs. 11.1%; p = .02) compared to males. However, a multivariable logistic regression model showed that patient sex was not an independent predictor of 30-day mortality (OR 0.90; 95% CI 0.67–1.22; p = .51).
Conclusions
Females with sepsis presenting to the ED had fewer comorbidities, lower disease severity, less often thrombocytopenia and fever and were more likely to have a urinary tract infection. Females had a lower in-hospital and 30-day mortality compared to males, but sex was not an independent predictor of 30-day mortality. The lower mortality in female patients may be explained by differences in comorbidity and clinical presentation compared to male patients.
KEY MESSAGES
Only limited data exist on sex differences in sepsis patients presenting to the emergency department with the whole spectrum of sepsis severity.
Female sepsis patients had a lower incidence of comorbidities, less disease severity and a different source of infection, which explains the lower 30-day mortality we found in female patients compared to male patients.
We found that sex was not an independent predictor of 30-day mortality; however, the study was probably underpowered to evaluate this outcome definitively.
Keywords: Sepsis, sex, sex differences, emergency department, critical care, mortality
Introduction
There is growing awareness that differences between men and women exist in presentation, treatment and outcome in many diseases. Sepsis is a life-threatening syndrome characterized by organ dysfunction caused by a dysregulated host response to infection [1]. With regard to sex-based differences, stronger innate, humoral and cellular immune responses to infection are found in females compared to males [2,3], which may be caused by genetic, hormonal as well as environmental factors [2–4].
Although females show a possible advantageous immune response during infections, studies investigating the effect of sex on sepsis related mortality are inconclusive. Some studies reported no difference [5–12], whereas others reported higher mortality in women [13–16], or conversely in men [17–21]. All of these sex-specific sepsis studies focused on sepsis patients in the intensive care unit (ICU) only, despite evidence that many sepsis patients never need intensive care [22]. Only limited data exist on sex differences in sepsis patients presenting to the emergency department (ED) and the results of these studies are also conflicting. Two studies included patients presenting to the ED with severe sepsis or septic shock [23,24]. Only one study analysed sex-related outcomes in patients with the whole spectrum of sepsis severity presenting to the ED [25]. Gaining insight into risk factors and sex differences in presentation and outcome in sepsis may help to personalize treatments and achieve better patient outcomes.
The aim of our multi-centre, retrospective cohort study was to investigate the association between patient sex and both clinical presentation and 30-day mortality in medical patients presenting with the whole spectrum of sepsis severity to the ED who were admitted to the hospital.
Materials and methods
Design, setting and study population
This multicentre retrospective cohort study was performed in three large teaching hospitals in the Netherlands. The Maastricht University Medical Centre+ (MUMC+) in Maastricht is a secondary and tertiary care university hospital with approximately 20,000 patients visiting the ED annually. Rijnstate Hospital in Arnhem and Zuyderland Medical Centre in Heerlen are both secondary care teaching hospitals with annually approximately 39,500 and 33,000 ED visits, respectively.
In MUMC+, patients were included between January 2015 and December 2016. In Rijnstate Hospital and Zuyderland Medical Centre, patients were enrolled between July and December 2015. The medical records of all consecutive adult patients (≥18 years old) presenting to the ED and who were subsequently admitted to the general ward, the medium care (MC) or ICU for the departments of internal medicine or gastroenterology during this inclusion period were screened. Sepsis was defined as a suspected infection with two or more systemic inflammatory response syndrome (SIRS) criteria [26], a Sequential Organ Failure Assessment (SOFA) score ≥ two points or at least two criteria of the quick SOFA (qSOFA) score [27]. These clinical scores were calculated retrospectively. Septic shock was defined as follows: (1) a systolic arterial blood pressure below 90 mmHg, or a mean arterial blood pressure below 60 mmHg, or a reduction in systolic blood pressure of more than 40 mmHg from baseline despite adequate volume resuscitation [28,29]; (2) and/or a serum lactate level >2 mmol/L in the absence of hypovolemia and requiring vasopressors to maintain a mean arterial pressure >65 mmHg [27]. All patients who met the criteria for sepsis or septic shock, independent of the primary diagnosis made at the moment of admission, were included in this study.
We used the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for reporting this observational study [30]. The Ethics Committee of MUMC+, Zuyderland and Rijnstate hospital approved the protocol of this study and waived the requirement for informed consent because of the anonymous nature of the data set and the non-interventional nature of the study (METC 13-4-103.12).
Data collection
All data were retrieved from electronic hospital charts. The following premorbid parameters were extracted for all patients: age, sex, comorbidity using the Charlson Comorbidity Index (CCI) score [31], and living situation. Living situation was categorized as either independent, nursing- or care home, or other.
In addition, the following items were retrieved in the ED: triage category (using the Manchester Triage System (MTS)) [32], vital signs, laboratory data (leukocytes, C-reactive protein (CRP) and thrombocytes), SOFA score, abbreviated Mortality Emergency Department Sepsis (abbMEDS) score [33] and presence of septic shock. The SOFA score quantifies the degree of organ dysfunction and can be used to predict the prognosis of patients with sepsis. The abbMEDS score aims to assess sepsis severity and predicts 28-day mortality in patients with sepsis at the ED [33]. The five MTS triage categories were dichotomized in high treatment priority patients (red and orange) vs. lower treatment priority patients (yellow, green and blue) [32]. The used reference ranges for the laboratory values were: leukocytes 4.0–12.0 × 109/L, and thrombocytes >150 × 109/L. The CRP cut-off levels used in previous sepsis studies were between 50 mg/L and 150 mg/L [34–36]. A dichotomized CRP cut-off level of 100 mg/L was used.
The following outcome parameters were collected: all-cause mortality during hospital admission and within 30 days after admission, MC/ICU admission, length of ICU stay, length of stay in the hospital, and final diagnosis regarding focus of infection. The primary outcome was all-cause 30-day mortality after ED presentation. Mortality after hospital discharge was checked in the Municipal Personal Records Database. This national database registers all deaths and date of deaths of Dutch citizens in the Netherlands.
Sample size
A sample size calculation using a two-tailed test was performed. With an expected mortality in males of 22% [37], the sample size to show a ≥5% difference in 30-day mortality was calculated to be 1968 patients. These calculations assumed a power of 80% with an α value of 0.05.
Data analysis
We performed descriptive analyses of baseline characteristics, scores and outcome on the observed data without imputation of missing values. Continuous variables were presented as medians with the 25th and 75th percentile interquartile ranges (IQRs) and categorical variables as proportions. Comparisons between women and men were made using the Mann–Whitney U-test for continuous non-Gaussian data and Person’s χ2 for categorical data. The Kaplan–Meier method was used to calculate 30-day survival probability; a log-rank test was used to compare survival between the sexes.
To assess the association of patient sex and all-cause 30-day mortality, multivariable logistic regression was performed incorporating several potential predictors (age, CCI score, SOFA score and focus of infection) based on the set of adjustment factors suggested in a recent systematic review [38]. If patient data on any variable included in the multivariable analysis were missing, that patient was excluded from the analysis. Odds Ratios (ORs) with 95% confidence intervals (95% CIs) were calculated.
Data were analysed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY). A p value <.05 was considered statistically significant.
Results
Patient characteristics
In total, 2065 patients were included (MUMC+ 1371 patients, Rijnstate Hospital 359 patients and Zuyderland Medical Centre 335 patients). There were 47.6% females and 52.4% males (Table 1). The median age was 69 (56–79) years and did not differ significantly between both groups.
Table 1.
Comparison of patient characteristics by sex.
| Female (N = 983, 47.6%) | Male (N = 1082, 52.4%) | p Value | |
|---|---|---|---|
| Premorbid characteristics | |||
| Age in yearsa | 69 (55–80) | 69 (57–79) | .95 |
| CCI | 2 (1–3) | 2 (1–4) | <.001 |
| 0 | 226 (23.1%) | 199 (18.6%) | |
| 1 | 177 (18.1%) | 169 (15.8%) | |
| 2 | 233 (23.8%) | 236 (22.1%) | |
| ≥3 | 342 (35.0%) | 464 (43.4%) | |
| Living situation | .50 | ||
| Independent | 829 (84.3%) | 919 (84.9%) | |
| Nursing- or care home | 89 (9.1%) | 84 (7.8%) | |
| Other | 65 (6.6%) | 79 (7.3%) | |
| On admission | |||
| MTS high treatment priority (red and orange) | 187 (19.4%) | 229 (21.6%) | .22 |
| Body temperature <36 °C | 51 (5.2%) | 59 (5.5%) | .76 |
| Body temperature >38 °C | 600 (61.4%) | 710 (66.4%) | .02 |
| Mean arterial pressure <65 mmHg | 103 (10.5%) | 94 (8.8%) | .17 |
| Heart rate >90/minute | 779 (79.2%) | 830 (77%) | .22 |
| Respiratory rate (cycles/minute) | 18 (14–22) | 18 (14–22) | .14 |
| Laboratory findings | |||
| Leukocytes <4 or >12 × 10/L | 725 (74.0%) | 769 (71.1%) | .15 |
| C-reactive protein >100 mg/L | 444 (45.2%) | 485 (44.9%) | .90 |
| Thrombocytes <150 × 10/L | 173 (18.0%) | 281 (26.6%) | <.001 |
| qSOFA score ≥2 | 194 (20.0%) | 190 (18.0%) | .24 |
| SOFA score ≥2 | 538 (54.7%) | 708 (65.4%) | <.001 |
| SIRS criteria ≥2 | 962 (97.9%) | 1049 (97%) | .19 |
| abbMEDS score | 5 (3–8) | 6 (3–8) | .001 |
| ≤4 (low risk) | 400 (40.7%) | 381 (35.2%) | |
| 5–12 (moderate risk) | 547 (55.6%) | 650 (60.1%) | |
| 13–24 (high risk) | 36 (3.7%) | 51 (4.7%) | |
| Septic shock | 73 (7.5%) | 99 (9.2%) | .15 |
| Outcome | |||
| MC admission | 21 (2.1%) | 21 (1.9%) | .75 |
| ICU admission | 65 (6.6%) | 75 (6.9%) | .70 |
| ICU length of stay in days | 3 (2–9) | 3 (2–7) | .96 |
| Hospital length-of-stay in days | 6 (3–11) | 6 (3–12) | .13 |
| Focus of infectiona | <.001 | ||
| Respiratory system | 293 (29.8%) | 363 (33.6%) | |
| Urinary tract | 251 (25.5%) | 216 (20.0%) | |
| Abdominal | 135 (13.7%) | 153 (14.2%) | |
| Skin and soft tissue | 58 (5.9%) | 91 (8.4%) | |
| Sepsis after chemotherapy | 59 (6.0%) | 34 (3.1%) | |
| Unknown origin | 86 (8.7%) | 102 (9.4%) | |
| Other | 44 (4.5%) | 70 (6.5%) | |
| No infection | 57 (5.8%) | 52 (4.8%) | |
| In-hospital mortality | 79 (8.0%) | 120 (11.1%) | .02 |
| 30-day mortality | 99 (10.1%) | 147 (13.6%) | .01 |
CCI: Charlson Comorbidity Index; MTS: Manchester Triage System; qSOFA: quick Sequential Organ Failure Assessment; SOFA: Sequential Organ Failure Assessment; SIRS: Systemic Inflammatory Response Syndrome; abbMEDS: abbreviated Mortality Emergency Department Sepsis; MC: medium care; ICU: intensive care unit.
Bold values signify p < .05.
Categorical variables given in totals and valid percentages (%), continuous variables in medians (IQR).
Data missing for one patient (0.05%); bData missing for 19 patients (0.9%); cData missing for 38 patients (1.8%); dData missing for 14 patients (0.7%); eData missing for four patients (0.2%); fData missing for 10 patients (0.5%); gData missing for 47 patients (2.3%); hData missing for 37 patients (1.8%); iData missing for 13 patients (0.6%).
Clinical presentation
Females had a significantly lower median CCI, SOFA score and abbMEDS score and presented less frequently with thrombocytopenia and a body temperature above 38 °C at the ED, compared to males (Table 1). The leading focus of infection in both male and female patients was the respiratory tract. Female patients were more likely to have a urinary tract infection than male patients (25.5% vs. 20.0%; p = .003). There were no significant differences between the sexes regarding the prevalence of septic shock, MC/ICU admissions, nor hospital length-of-stay.
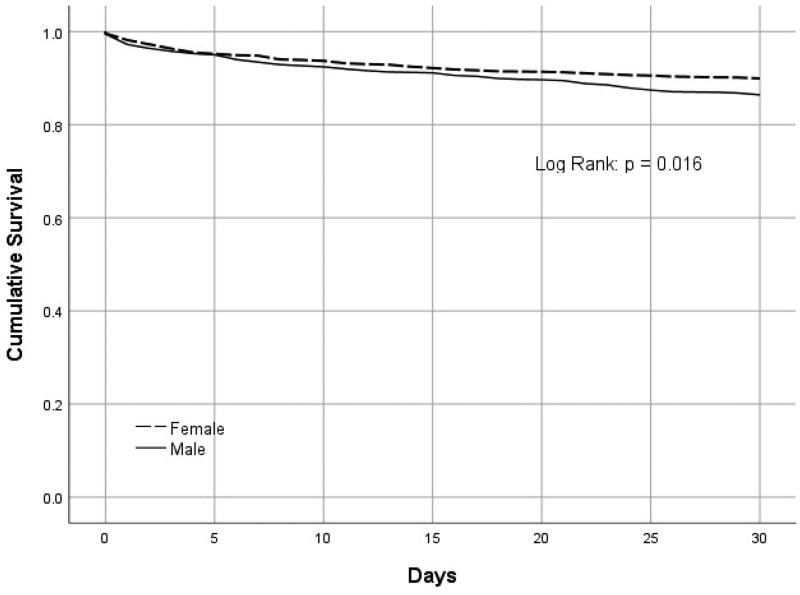
Mortality
Within 30 days of ED presentation, mortality was significantly lower in female patients (10.1%) compared to male patients (13.6%, log rank test, p = .016, Figure 1). In-hospital mortality was significantly lower in females compared to males as well (8.0% vs. 11.1%; p = .02).
Figure 1.
Kaplan–Meier’s survival curves for 30-days survival stratified by sex.
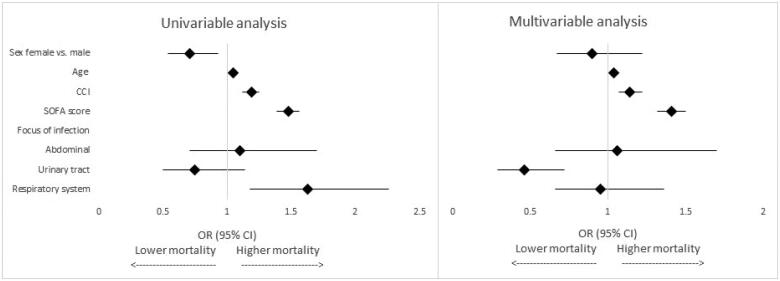
Logistic regression analysis
The univariable and multivariable analyses for all-cause 30-day mortality are shown in Table 2 and Figure 2. The multivariable logistic regression model excluded 21 patients (1.0%) because of missing values. After adjusting for age, comorbidity, SOFA score and focus of infection, the multivariable analysis showed that patient sex was not an independent predictor of 30-day mortality (OR 0.90; 95% CI 0.67–1.22; p = .51).
Table 2.
Risk factors for all-cause 30-day mortality.
| Variables | Univariable analysis |
Multivariable analysis (missing: N = 21) |
||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Sex female vs. male | 0.71 (0.54–0.93) | .01 | 0.90 (0.67–1.22) | .51 |
| Age per year | 1.05 (1.04–1.06) | <.001 | 1.04 (1.03–1.06) | <.001 |
| CCI | 1.19 (1.12–1.25) | <.001 | 1.14 (1.07–1.22) | <.001 |
| SOFA score | 1.48 (1.39–1.56) | <.001 | 1.41 (1.32–1.50) | <.001 |
| Focus of infection | ||||
| Abdominal | 1.10 (0.71–1.70) | .69 | 1.06 (0.66–1.70) | .82 |
| Urinary tract | 0.75 (0.50–1.14) | .17 | 0.46 (0.29–0.72) | .001 |
| Respiratory system | 1.63 (1.18–2.26) | .003 | 0.95 (0.66–1.36) | .77 |
| Other focus, unknown or missing | Reference | – | Reference | – |
OR: odds ratio; 95% CI: 95% confidence interval; CCI: Charlson Comorbidity Index; SOFA: Sequential Organ Failure Assessment.
Bold values signify p < .05.
Figure 2.
Forest plots based on the results of the univariable and multivariable analyses of the risk factors associated with all-cause 30-day mortality. CCI: Charlson Comorbidity Index; SOFA: Sequential Organ Failure Assessment; OR: odds ratio; 95% CI: 95% confidence interval.
Higher age, a higher CCI score and a higher SOFA score were independently associated with higher 30-day mortality in patients with sepsis. Urinary tract infections were associated with a lower 30-day mortality risk.
Discussion
This multicentre retrospective cohort study is one of the first studies that analysed sex-related outcomes in patients with the whole spectrum of sepsis severity presenting to the ED and admitted to the hospital. We found several differences in presentation and outcome of sepsis between the sexes. Female patients had fewer comorbidities and were more likely to have a urinary tract infection compared to males. Females had a lower frequency of thrombocytopenia and fever, and a lower abbMEDS and SOFA score compared to males. Furthermore, we showed that females had a lower rate of in-hospital and 30-day mortality compared to males. However, after adjusting for other predictors of mortality in sepsis (age, comorbidities, disease severity at presentation, and focus of infection), we found that patient sex was not an independent predictor of 30-day mortality.
We found some differences in clinical presentation between females and males. Female patients were more likely to have a urinary tract infection compared to male patients, a finding that has also been reported in other studies [39,40]. Patients with a urinary tract infection had a lower 30-day mortality risk in our study, which is in line with other studies that found a lower mortality rate in patients with genitourinary tract infections compared to patients with lower respiratory tract infections [41,42]. Furthermore, in our study, females had significantly less comorbidities at presentation. Comorbid medical conditions like chronic lung disease, chronic kidney disease, coronary artery disease and diabetes are risk factors for developing sepsis, and a higher number of comorbidities is associated with developing acute organ dysfunction and hospital mortality in sepsis [39,43,44]. In addition, thrombocytopenia and fever were less frequently present in female patients. Platelets are not only involved in the activation of coagulation, but also play a role in the acute phase response in infectious diseases and promote innate immune cells responses [45]. Thrombocytopenia is often seen during sepsis and is associated with organ failure, a more disturbed immunological response, and poor outcome [45,46]. Despite the fact that we found no significant sex differences in the prevalence of septic shock, both the abbMEDS score and the SOFA score were significantly lower in female patients compared to male patients. This lower disease severity in female patients can possibly be explained by the lower prevalence of comorbidities and a more favourable focus of infection in females. All these factors can play a role in the lower mortality we found in female sepsis patients.
Despite the fact that we found a lower mortality rate in female patients, sex was not an independent predictor of mortality when correcting for other risk factors. Previous research focused on seriously ill patients admitted to the ICU or only included patients at the ED with severe sepsis or septic shock. A recently published systematic review and meta-analysis with more than 80,000 sepsis patients admitted to the ICU, concluded that the role of sex as a prognostic factor of mortality was uncertain because the quality of the evidence was very low [38]. Two studies which included patients with severe sepsis or septic shock presenting to the ED showed conflicting results. One study showed that females with severe sepsis or shock had a higher chance of in-hospital mortality than males [23], while another study did not identify sex as independent predictor of mortality in patients presenting to the ED with septic shock [24]. In our study, the sepsis diagnosis encompassed the whole spectrum of sepsis severity, including those patients with a low mortality risk. To date, only one other study analysed the impact of sex differences in patients with sepsis in the ED regardless of sepsis severity [25]. They reported that sex was not a risk factor of in-hospital mortality, despite a trend towards lower female mortality. In contrast to their study, which included patients meeting sepsis-2 criteria, we included patients who met the sepsis-3 criteria as well, since the use of SIRS or SOFA/qSOFA score alone may lead to missed sepsis diagnoses [47]. However, despite this difference, our results are comparable. We showed that female patients had a lower mortality in sepsis, but sex was not an independent predictor of mortality. The lower mortality might be explained by the lower incidence of comorbidities, less disease severity and a different source of infection in female patients compared to male patients.
The strengths of our study are its multicentre design, a large population of ED patients, and inclusion of patients with the whole spectrum of sepsis severity. The study population included in different hospitals created a representative population of sepsis patients in the ED. Furthermore, patients admitted to the hospital with sepsis may receive another primary admission diagnosis (e.g. pneumonia) and these patients might be missed as sepsis patients. We therefore included all patients presenting to the ED who met the criteria of sepsis or septic shock, independent of the primary diagnosis made during admission. A limitation may be the retrospective nature of the study. Furthermore, we found significant and relevant differences in presentation, comorbidities and mortality between the sexes. The study was probably underpowered to detect patient sex as an independent predictor of mortality, because of the lower observed than expected mortality rate. To achieve enough power, we would have needed a sample size of 600 patients more (total of 2674 patients). However, we found relevant differences in clinical presentation between women and men with sepsis. Given the importance of the subject, to be able to individualize treatment and to take sex-dependent factors into account, this study needs to be repeated in an even larger, multicentre study population in several countries.
Conclusions
Females with sepsis presenting to the ED and admitted to the hospital had fewer comorbidities, lower disease severity, lower frequency of thrombocytopenia and fever, were more likely to have a urinary tract infection and had a lower in-hospital and 30-day mortality compared to males. Sex was not an independent predictor of 30-day mortality, however, with regard to this outcome, the study was probably underpowered. The lower mortality in female patients may be explained by differences in comorbidity and clinical presentation compared to male patients.
Funding Statement
The authors did not receive any funding for this article.
Author contributions
VW, JB, DB and PS were involved in the conception and design of this study. VW, MC and JS acquired the data. VW, NZ and PS analysed the data. VW and PS drafted the first version of the manuscript. MC, JS, JB, DB and NZ critically reviewed the manuscript. All authors revised and approved the final manuscript and agreed to be held accountable for all aspects of the work.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):1–8. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruggieri A, Anticoli S, D’Ambrosio A, et al. The influence of sex and gender on immunity, infection and vaccination. Ann Ist Super Sanita. 2016;52:198–204. [DOI] [PubMed] [Google Scholar]
- 3.Pennell LM, Galligan CL, Fish EN.. Sex affects immunity. J Autoimmun. 2012;38(2–3):J282–J291. doi: 10.1016/j.jaut.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Giefing-Kröll C, Berger P, Lepperdinger G, et al. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 2015;14(3):309–321. doi: 10.1111/acel.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wichmann MW, Inthorn D, Andress HJ, et al. Incidence and mortality of severe sepsis in surgical intensive care patients: the influence of patient gender on disease process and outcome. Intensive Care Med. 2000;26(2):167–172. doi: 10.1007/s001340050041. [DOI] [PubMed] [Google Scholar]
- 6.Madsen TE, Simmons J, Choo EK, et al. The DISPARITY study: do gender differences exist in surviving sepsis campaign resuscitation bundle completion, completion of individual bundle elements, or sepsis mortality? J Crit Care. 2014;29(3):473.e7–473.e11. doi: 10.1016/j.jcrc.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013;17(2):R50. doi: 10.1186/cc12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park DW, Chun BC, Kim JM, et al. Epidemiological and clinical characteristics of community-acquired severe sepsis and septic shock: a prospective observational study in 12 university hospitals in Korea. J Korean Med Sci. 2012;27(11):1308–1314. doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobson S, Liedgren E, Johansson G, et al. Sequential Organ Failure Assessment (SOFA) scores differ between genders in a sepsis cohort: cause or effect? Ups J Med Sci. 2012;117(4):415–425. doi: 10.3109/03009734.2012.703255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Vught LA, Scicluna BP, Wiewel MA, et al. Association of gender with outcome and host response in critically ill sepsis patients. Crit Care Med. 2017;45(11):1854–1862. doi: 10.1097/CCM.0000000000002649. [DOI] [PubMed] [Google Scholar]
- 11.Ponce-Alonso M, Fernández-Félix BM, Halperin A, et al. Propensity-score analysis reveals that sex is not a prognostic factor for mortality in intensive care unit-admitted patients with septic bacteremia. Int J Infect Dis. 2021;110:36–44. doi: 10.1016/j.ijid.2021.07.034. [DOI] [PubMed] [Google Scholar]
- 12.Wernly B, Bruno RR, Mamandipoor B, et al. Sex-specific outcomes and management in critically ill septic patients. Eur J Intern Med. 2021;83:74–77. doi: 10.1016/j.ejim.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Eachempati SR, Hydo L, Barie PS.. Gender-based differences in outcome in patients with sepsis. Arch Surg. 1999;134(12):1342–1347. doi: 10.1001/archsurg.134.12.1342. [DOI] [PubMed] [Google Scholar]
- 14.Pietropaoli AP, Glance LG, Oakes D, et al. Gender differences in mortality in patients with severe sepsis or septic shock. Gend Med. 2010;7(5):422–437. doi: 10.1016/j.genm.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nachtigall I, Tafelski S, Rothbart A, et al. Gender-related outcome difference is related to course of sepsis on mixed ICUs: a prospective, observational clinical study. Crit Care. 2011;15(3):R151. doi: 10.1186/cc10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sunden-Cullberg J, Nilsson A, Inghammar M.. Sex-based differences in ED management of critically ill patients with sepsis: a nationwide cohort study. Intensive Care Med. 2020;46(4):727–736. doi: 10.1007/s00134-019-05910-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nasir N, Jamil B, Siddiqui S, et al. Mortality in sepsis and its relationship with gender. Pak J Med Sci. 2015;31(5):1201–1206. doi: 10.12669/pjms.315.6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schröder J, Kahlke V, Staubach KH, et al. Gender differences in human sepsis. Arch Surg. 1998;133(11):1200–1205. doi: 10.1001/archsurg.133.11.1200. [DOI] [PubMed] [Google Scholar]
- 19.Adrie C, Azoulay E, Francais A, et al. Influence of gender on the outcome of severe sepsis: a reappraisal. Chest. 2007;132(6):1786–1793. doi: 10.1378/chest.07-0420. [DOI] [PubMed] [Google Scholar]
- 20.Xu J, Tong L, Yao J, et al. Association of sex with clinical outcome in critically ill sepsis patients: a retrospective analysis of the large clinical database MIMIC-III. Shock. 2019;52(2):146–151. doi: 10.1097/SHK.0000000000001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin S, He W, Hu Z, et al. Sex differences in short- and long-term survival among critically ill patients with sepsis. Int J Gen Med. 2021;14:613–622. doi: 10.2147/IJGM.S294229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sands KE, Bates DW, Lanken PN, et al. Epidemiology of sepsis syndrome in 8 academic medical centers. JAMA. 1997;278(3):234–240. doi: 10.1001/jama.1997.03550030074038. [DOI] [PubMed] [Google Scholar]
- 23.Failla KR, Connelly CD, Ecoff L, et al. Does gender matter in septic patient outcomes? J Nurs Scholarsh. 2019;51(4):438–448. doi: 10.1111/jnu.12478. [DOI] [PubMed] [Google Scholar]
- 24.Luethi N, Bailey M, Higgins A, et al. Gender differences in mortality and quality of life after septic shock: a post-hoc analysis of the ARISE study. J Crit Care. 2020;55:177–183. doi: 10.1016/j.jcrc.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Ward HH, Kiernan EA, Deschler CL, et al. Clinical and demographic parameters of patients treated using a sepsis protocol. Clin Ther. 2019;41(6):1020–1028. doi: 10.1016/j.clinthera.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 26.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 27.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med. 2003;29(4):530–538. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 29.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 30.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 31.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 32.Mackway-Jones KC, Marsden J, Windle J. Emergency triage: Manchester Triage Group. Chichester: John Wiley & Sons, Ltd; 2014. [Google Scholar]
- 33.Vorwerk C, Loryman B, Coats TJ, et al. Prediction of mortality in adult emergency department patients with sepsis. Emerg Med J. 2009;26(4):254–258. doi: 10.1136/emj.2007.053298. [DOI] [PubMed] [Google Scholar]
- 34.Li HX, Liu ZM, Zhao SJ, et al. Measuring both procalcitonin and C-reactive protein for a diagnosis of sepsis in critically ill patients. J Int Med Res. 2014;42(4):1050–1059. doi: 10.1177/0300060514528483. [DOI] [PubMed] [Google Scholar]
- 35.Castelli GP, Pognani C, Meisner M, et al. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care. 2004;8(4):R234–R242. doi: 10.1186/cc2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Póvoa P, Almeida E, Moreira P, et al. C-reactive protein as an indicator of sepsis. Intensive Care Med. 1998;24(10):1052–1056. doi: 10.1007/s001340050715. [DOI] [PubMed] [Google Scholar]
- 37.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 38.Antequera A, Lopez-Alcalde J, Stallings E, et al. Sex as a prognostic factor for mortality in critically ill adults with sepsis: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e048982. doi: 10.1136/bmjopen-2021-048982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Esper AM, Moss M, Lewis CA, et al. The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med. 2006;34(10):2576–2582. doi: 10.1097/01.CCM.0000239114.50519.0E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Chou EH, Mann S, Hsu TC, et al. Incidence, trends, and outcomes of infection sites among hospitalizations of sepsis: a nationwide study. PLOS One. 2020;15(1):e0227752. doi: 10.1371/journal.pone.0227752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Motzkus CA, Luckmann R.. Does infection site matter? A systematic review of infection site mortality in sepsis. J Intensive Care Med. 2017;32(8):473–479. doi: 10.1177/0885066615627778. [DOI] [PubMed] [Google Scholar]
- 43.Wang HE, Shapiro NI, Griffin R, et al. Chronic medical conditions and risk of sepsis. PLOS One. 2012;7(10):e48307. doi: 10.1371/journal.pone.0048307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang Y, Yang KS, Hsann YM, et al. The effect of comorbidity and age on hospital mortality and length of stay in patients with sepsis. J Crit Care. 2010;25(3):398–405. doi: 10.1016/j.jcrc.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Vardon-Bounes F, Ruiz S, Gratacap MP, et al. Platelets are critical key players in sepsis. Int J Mol Sci. 2019;20:3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Claushuis TA, van Vught LA, Scicluna BP, et al. Thrombocytopenia is associated with a dysregulated host response in critically ill sepsis patients. Blood. 2016;127(24):3062–3072. doi: . [DOI] [PubMed] [Google Scholar]
- 47.Prasad PA, Fang MC, Abe-Jones Y, et al. Time to recognition of sepsis in the emergency department using electronic health record data: a comparative analysis of systemic inflammatory response syndrome, sequential organ failure assessment, and quick sequential organ failure assessment. Crit Care Med. 2020;48(2):200–209. doi: 10.1097/CCM.0000000000004132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.