Abstract
Background
There are sparse data on outcomes of patients with heart failure (HF) from India. The objective was to evaluate hospital readmissions and 1-year mortality outcomes of patients with HF in Kerala, India.
Methods
We followed 1,205 patients enrolled in the Trivandrum Heart Failure Registry for 1 year. A trained research nurse contacted each participant every 3 months using a structured questionnaire which included hospital readmission and mortality information.
Results
The mean (SD) age was 61.2 (13.7) years, and 31% were women. One out of 4 (26%) participants had HF with preserved ejection fraction. Only 25% of patients with HF with reduced ejection fraction received guideline-directed medical therapy at discharge. Cumulative all-cause mortality at 1 year was 30.8% (n = 371), but the greatest risk of mortality was in the first 3 months (18.1%). Most deaths (61%) occurred in patients younger than 70 years. One out of every 3 (30.2%) patients was readmitted at least once over 1 year. The hospital readmission rates were similar between HF with preserved ejection fraction and HF with reduced ejection fraction patients. New York Heart Association functional class IV status and lack of guideline-directed medical treatment after index hospitalization were associated with increased likelihood of readmission. Similarly, older age, lower education status, nonischemic etiology, history of stroke, higher serum creatinine, lack of adherence to guideline-directed medical therapy, and hospital readmissions were associated with increased 1-year mortality.
Conclusions
In the Trivandrum Heart Failure Registry, 1 of 3 HF patients died within 1 year of follow-up during their productive life years. Suboptimal adherence to guideline-directed treatment is associated with increased propensity of readmission and death. Quality improvement programs aiming to improve adherence to guideline-based therapy and reducing readmission may result in significant survival benefits in the relatively younger cohort of HF patients in India.
Heart failure (HF) is a global pandemic affecting an estimated 26 million people worldwide.1 Contemporary data on the burden of HF in India are sparse. India has undergone rapid epidemiological and demographic transitions in the last 2 decades. As a result, the burden of HF in India has increased by nearly 140% from 1990 to 2013.1 There are an estimated 1.3 to 4.6 million people with HF in India based on risk factor models.2
The treatment of HF is resource intensive and a major burden on the health care system. Angiotensin-converting enzyme inhibitors, β-blockers, aldosterone receptor blockers, and aldosterone antagonists are now standard therapies for HF. These medications are available in low- and middle-income countries, including India, as more affordable generic formulations. Despite the availability of cheaper generic formulations, their use remains limited, which leads to adverse patient outcomes.3 Data on long-term outcomes of HF patients are available from high-income countries but remain scarce from low- and middle-income countries.4–8 To fill this gap, we report hospital readmission rates and 1-year mortality outcomes of patients admitted with acute HF in the Trivandrum Heart Failure Registry (THFR).
Methods
Study population and settings
THFR is a prospective hospital-based registry in the Trivandrum district of Kerala, India, covering both urban and rural areas. The details of development of THFR, and inclusion and exclusion criteria have been described previously.3 Briefly, THFR enrolled consecutive patients with HF as defined by the European Society of Heart Failure9 from 18 hospitals in the region. The registry was started in 2013, and participants were followed for 1 year after enrolment.
Data collection
The details of THFR enrolment and initial data collection have also been described previously.3 After the index hospitalization for acute HF, the patients were contacted every 3 months by telephone or during hospital readmission by a trained research nurse from the study coordinating center at Sree Chitra Tirunal Institute for Medical Sciences and Technology in Trivandrum, Kerala. The research nurse collected follow-up data on hospital readmissions, invasive procedures, and events using a structured questionnaire. A verbal autopsy was performed in the case of mortality to determine the cause of death (sudden cardiac death, cardiogenic shock, unknown, or other). Participants who died prior to reaching the hospital or died within 24 hours of hospital admission were considered to have sudden cardiac death. Participants who died in the hospital after 24 hours of admission or required antecedent inotropic support were considered to have died from cardiogenic shock.
Patients were divided into 2 groups based on their ejection fraction: HF with preserved ejection fraction (HFpEF; EF ≥45%) and HF with reduced ejection fraction (HFrEF; EF <45%). Patients were categorized as receiving guideline-directed care or suboptimal care during initial enrolment in THFR. Optimal guideline-directed medical treatment included β-blockers, angiotensin-converting enzyme inhibitors (ACEIs), or angiotensin receptor blockers (ARBs) and aldosterone receptor blockers in patients with HFrEF.9
Statistical methods and analyses
Descriptive statistics were used to summarize the demographic and clinical characteristics of study population in men and women separately. Categorical variables are summarized as proportions, whereas continuous variables are presented as means with SD. We estimated 1-year mortality rate both as a proportion (number of deaths/total registered patients) and per 100 person-years of follow-up. Furthermore, we used survival analyses to study the relationship between exposure variables of interests and mortality outcomes at 1 year. Mortality rates per 100 person-years of follow-up with 95% CIs were calculated in men and women separately. The rates were estimated in the total population, in various subgroups based on baseline characteristics, and separately in individuals with HFrEF. Kaplan-Meier survival plots and log-rank tests were used to assess the unadjusted association between exposure variables of interest and mortality. Proportional hazards assumption was tested visually by plotting log-minus-log plots. Cox proportional hazards (Cox-PH) models were generated to assess multivariate-adjusted association of various exposure variables of interests with 1-year all-cause mortality. The multivariate model included all potential confounding variables as in our previous study.3 Additionally, the number of hospital readmissions during the follow-up period was also included in the multivariate model. Thus, the final model included demographic variables (age, sex, and educational status), type of HF (acute de novo and acute on chronic), disease etiology (ischemic and nonischemic), baseline comorbidities (diabetes, hypertension, pulmonary disease, and stroke), behavioral risk factors (alcohol and tobacco use), ejection fraction, serum creatinine, guideline-based treatment status at discharge, and number of hospital readmissions during the follow up period.
Results
Demographic and clinical characteristics
A total of 1,205 participants were enrolled in THFR. The characteristics of the study population are described in Table I. Most of the participants were men (834, 69%). The men were relatively younger with a mean (SD) age of 60.5 (13.2) years compared with women of 63 (14.6) years. Nearly half of the population had education beyond primary school or more than 4 years of formal education. More women (18.1%) compared with men (9%) reported no formal education.
Table I.
Characteristics of the study population
| Variable | Male (n = 834) | Female (n = 371) |
|---|---|---|
|
| ||
| Age (y), mean (SD) | 60.46(13.20) | 62.98 (14.56) |
| Educational status, n (%) | ||
| No education | 75 (9.00) | 67 (18.16) |
| Up to primary school | 351 (42.14) | 189 (51.22) |
| Secondary | 280 (33.61) | 83 (22.49) |
| Graduates and above | 127(15.25) | 30 (8.13) |
| Acute de novo HF, n (%) | 335 (40.17) | 144(38.81) |
| Etiology, n (%) | ||
| Ischemic heart disease | 620 (74.34) | 246 (66.31) |
| Dilated cardiomyopathy | 111 (13.31) | 45 (12.13) |
| Hypertrophic cardiomyopathy | 19(2.28) | 8 (2.16) |
| Rheumatic heart disease | 52 (6.24) | 43 (11.59) |
| Hypertension | 5 (0.60) | 6 (1.62) |
| Miscellaneous | 27 (3.24) | 23 (6.20) |
| Comorbid conditions, n (%) | ||
| Hypertension | 476 (57.07) | 220 (59.30) |
| Diabetes | 464 (55.64) | 198 (53.37) |
| Chronic kidney disease | 160(19.18) | 56 (15.09) |
| Chronic obstructive pulmonary disease | 130 (15.59) | 56 (15.09) |
| Atrial fibrillation/flutter | 109 (13.07) | 68 (18.33) |
| Stroke | 54 (6.47) | 21 (5.66) |
| Severity of HF, n (%) | ||
| NYHA class IV | 254 (31.20) | 128 (36.78) |
| Ejection fraction <45 | 645 (77.34) | 249 (67.12) |
| Habits, n (%) | ||
| Current tobacco use | 187 (22.42) | 1 (0.27) |
| Past tobacco use | 301 (36.09) | None |
| Current alcohol use | 234 (28.06) | None |
| Past alcohol use | 21 (2.52) | None |
| Clinical measurements, mean (SD) | ||
| Systolic blood pressure (mm Hg) | 128.53 (32.66) | 131.13 (31.63) |
| Diastolic blood pressure (mm Hg) | 80.23 (16.45) | 81.41 (16.92) |
| Serum creatinine (mg/dL) | 1.54 (0.92) | 1.29 (0.86) |
| Heart rate >100 beats/s, n (%) | 487 (58.53) | 233 (63.49) |
The most common etiology of HF in both men and women was ischemic heart disease (74.3% and 66.3%, respectively). Women reported a higher prevalence of rheumatic heart disease (11.6%) as compared with men (6.2%). There were no major differences between men and women in regard to comorbidities including hypertension, diabetes, chronic kidney disease, and stroke. However, women reported more atrial fibrillation/flutter at baseline (18.3%) compared with men (13.1%). HFpEF constituted 25.8% (n = 311) of the study population. The proportion of women with HFpEF was 33% as compared with 23% in men.
Based on baseline data, women were much less likely to use tobacco (0.3%) compared with men (22.4%), and no women reported current or past alcohol use. Guideline-directed medical treatment at discharge from index hospitalization was prescribed to 24.6% (95% CI 21.8–27.4) of participants with HFrEF. There were no major gender differences in guideline-directed medical treatment status at discharge (25.3% in men compared with 22.9% in women). Guideline-directed therapy was however prescribed to a lower proportion of individuals with poor educational level (χ2 P = .02) as compared with individuals with higher educational status.
Hospital readmissions
The 1-year hospital readmission rate was 30.2% (n = 333) among the 1,103 participants discharged from the index hospitalization. In total, 269 (24.4%) patients were readmitted once, and an additional 64 (5.8%) were readmitted more than once during the 1-year follow-up period. Seventy-five participants underwent an invasive procedure (coronary angiogram, percutaneous coronary intervention, implantable cardioverter/defibrillator, or coronary artery bypass graft surgery) during hospital readmission. Of the 333 (30.2%) participants readmitted after the index hospitalization, 268 (24.3%) participants were readmitted specifically for HF exacerbation. The hospital readmission rate was similar for both men (30.3%) and women (30.9%), as well as HFrEF (30.1%) and HFpEF (31.6%). Characteristics associated with increased propensity for hospital readmission included New York Heart Association (NYHA) functional class IV symptoms during index hospitalization (odds ratio 1.32, 95% CI 1.01–1.75) and suboptimal guideline-directed medical therapy (odds ratio 1.29, 95% CI 1.02–1.63).
One-year mortality outcomes
Of the initial 1,205 participants in THFR, 49 participants were lost to follow-up, resulting in a 1-year follow-up rate of 96%. During the index hospitalization, 102 participants died and another 269 participants died during the 1-year follow-up period. resulting in a cumulative all-cause mortality rate at 1 year of 30.8% (n = 371). The greatest risk of mortality was however in the initial 3 months of follow-up, with a mortality rate of 18.1%. Most deaths (61%) at 1-year follow-up occurred in patients younger than 70 years. The total time at risk was 890.5 person--years of follow-up. The overall mortality rate was 41.7 per 100 person-years of follow-up (40.8 and 43.5 per 100 person-years of follow-up in men and women, respectively). The mortality rate was lower in HFpEF (35.7 per 100 person-years of follow-up) as compared with HFrEF (43.8 per 100 person-years of follow-up). The mortality rates per 100 person-years of follow-up in men and women stratified by baseline variables are shown in Table II.
Table II.
Unadjusted mortality rate per 100 person-years of follow-up in patients with HF
| Overall rate (95% CI) | HFrEF (95% CI) | |
|---|---|---|
|
| ||
| Male | ||
| Total mortality rate | 40.84 (36.1–46.2) | 43.06 (37.5–49.4) |
| Age >55 y | 46.08 (39.8–53.3) | 50.15(42.8–58.8) |
| Primary or below primary education | 41.54 (34.9–49.4) | 43.36 (35.8–52.6) |
| History of hypertension | 38.99 (33.0–46.0) | 40.27 (33.4–48.5) |
| Diabetes | 41.09 (31.9–52.9) | 45.49 (38.1–54.4) |
| Chronic kidney disease | 58.38 (45.7–74.6) | 51.82 (38.7–69.4) |
| Ischemic heart disease etiology | 41.97(36.4–48.3) | 45.00 (38.6–52.4) |
| NYHA class IV | 50.36 (40.8–62.1) | 50.49 (39.8–63.9) |
| Female | ||
| Total mortality rate | 43.53 (36.4–52.1) | 45.82 (36.9–56.9) |
| Age >55 y | 50.55 (41.3–61.9) | 53.21 (41.9–67.5) |
| Primary or below primary education | 50.02 (40.7–61.5) | 55.78 (43.7–71.1) |
| History of hypertension | 46.31 (36.8–58.3) | 47.27(36.0–62.1) |
| Diabetes | 44.35 (37.8–52.1) | 42.26 (31.2–57.2) |
| Chronic kidney disease | 51.99 (33.9–79.6) | 45.48 (26.4–78.3) |
| Ischemic heart disease etiology | 44.90 (36.0–55.9) | 48.86 (37.9–62.9) |
| NYHA class IV | 69.55 (53.6–90.2) | 71.48 (52.0–98.2) |
Kaplan-Meier survival analyses
Kaplan-Meier survival curves reveal the clear impact of guideline-directed medical therapy on long-term mortality (Figure 1). Participants who did not receive guideline-directed medical treatment experienced higher mortality as compared with those who received guideline-directed therapy (P < .001). The cumulative 1-year mortality rate was significantly higher in participants who had 1 or more hospital readmission (Figure 2).
Figure 1.

Guideline-based optimal medical treatment and all-cause mortality in HF patients in THFR in Kerala, India.
Figure 2.
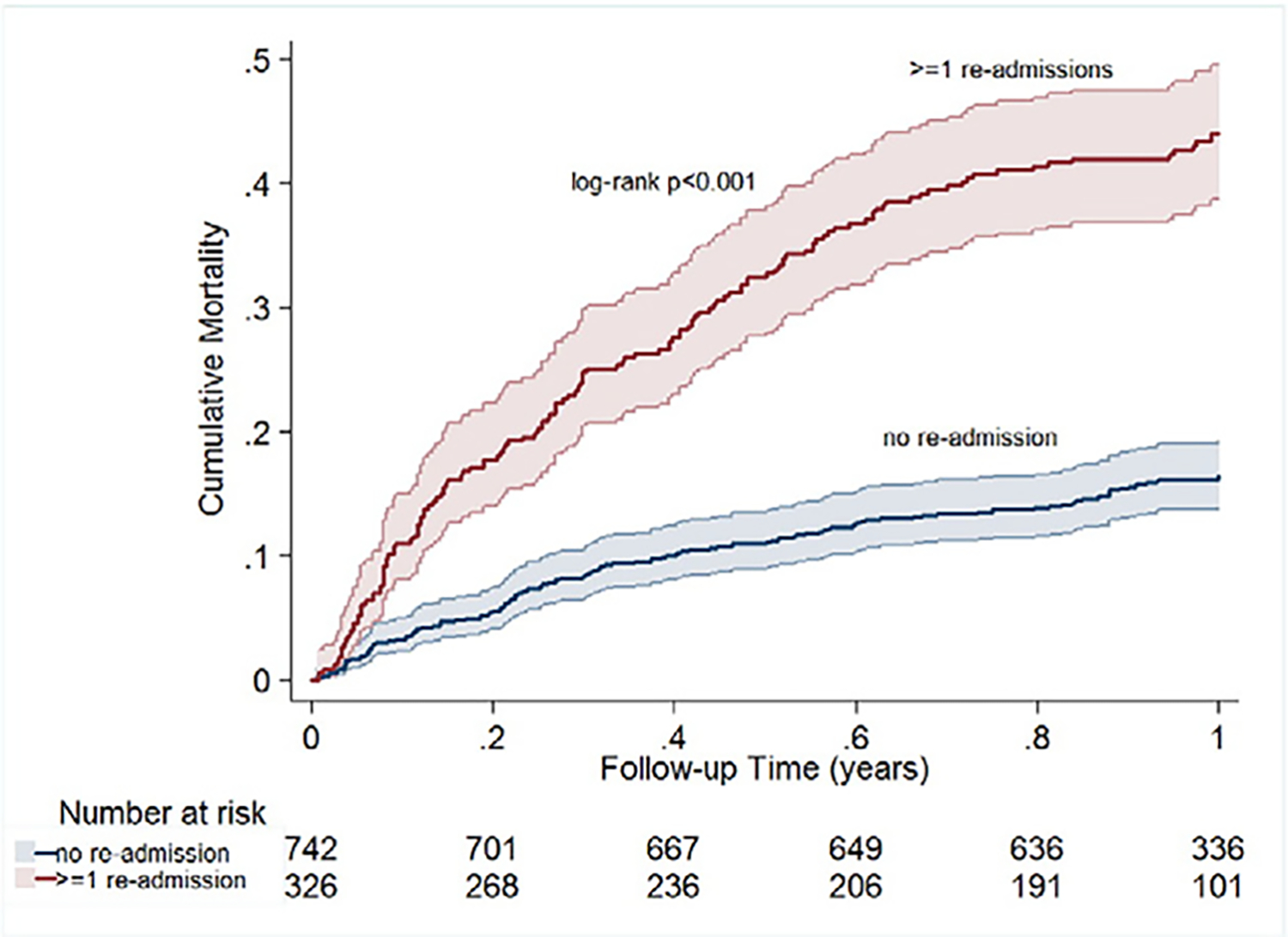
Readmission and mortality in HF patients in THFR in Kerala, India.
Multivariate Cox-PH model
In the multivariate Cox-PH model for all-cause mortality, older age (hazard ratio [HR] 1.31 per SD increase in age, 95% CI 1.12–1.52), history of stroke (HR 1.58, 95% CI 1.04–2.38), higher education level (HR 0.52 in graduates as compared with individuals with no formal education, 95% CI 0.32–0.87), higher serum creatinine (HR 1.13 per SD increase, 95% CI 1.02–1.24), 1 or more hospital readmissions (HR 2.99 for individuals with 1 hospitalization, 95% CI 2.28–3.94 and HR 3.15 in individuals with 2 or more hospitalizations, 95% CI 2.00–4.96), and prescription of guideline-directed medical treatment (HR 0.73, 95% CI 0.52–1.01) were associated with 1-year mortality (Table III).
Table III.
Muitivariate Cox-PH model for all-cause mortality
| Variables | HR | 95% CI | P value |
|---|---|---|---|
|
| |||
| Age (1 SD increase) | 1.31 | 1.12–1.52 | .001 |
| Male | 1 | ||
| Female | 1.01 | 0.72–1.43 | .933 |
| Educational status | |||
| Illiterate or no formal education | 1 | ||
| Up to primary level education | 0.67 | 0.46–0.99 | .043 |
| Secondary school education | 0.71 | 0.47–1.09 | .123 |
| Graduates and above | 0.52 | 0.32–0.87 | .012 |
| Ischemic etiology | 1 | ||
| Nonischemic etiology | 1.54 | 1.13–2.08 | .006 |
| Hypertension (no) | 1 | ||
| Hypertension (yes) | 0.84 | 0.62–1.11 | .222 |
| Diabetes (no) | 1 | ||
| Diabetes (yes) | 1.09 | 0.82–1.45 | .547 |
| Stroke (no) | 1 | ||
| Stroke (yes) | 1.58 | 1.04–2.38 | .031 |
| Chronic obstructive pulmonary disease (no) | 1 | ||
| Chronic obstructive pulmonary disease (yes) | 1.09 | 0.78–1.54 | .619 |
| Alcohol use (no) | 1 | ||
| Alcohol use (yes) | 0.86 | 0.63–1.17 | .330 |
| Tobacco use (no) | 1 | ||
| Tobacco use (yes) | 1.13 | 0.95–1.35 | .177 |
| Serum creatinine per SD increase | 1.13 | 1.02–1.24 | .017 |
| Heart rate per SD increase | 0.95 | 0.83–1.07 | .394 |
| Ejection fraction per SD increase | 0.96 | 0.84–1.08 | .510 |
| NYHA class I-III | 1 | ||
| NYHA class IV | 1.25 | 0.96–1.67 | .113 |
| No readmission | 1 | ||
| 1 Readmission | 2.99 | 2.28–3.94 | <.001 |
| ≥2 Readmissions | 3.15 | 2.00–4.96 | <.001 |
| Suboptimal treatment | 1 | ||
| Guideline-directed treatment | 0.73 | 0.52–1.01 | .051 |
Discussion
THFR is the first organized HF registry in India to report 1-year outcomes. Patients in THFR are relatively younger with a clear male predominance. Only 2 of 3 HF patients survive at 1 year, with a cumulative all-cause mortality rate of 30.8%. Poor adherence to guideline-directed medical treatment is associated with increased propensity of hospital readmission and death. Patients with reduced ejection fraction (HFrEF) have a significantly higher mortality than patients with preserved ejection fraction (HFpEF).
More than 1.2 billion people live in India, yet data on HF in India remain sparse. A recent systematic review on HF care in low- and middle-income countries included only 1 study from India, which highlights the lack of evidence.5 THFR suggests that the phenotype of HF in India may be different because participants are relatively younger in comparison to other HF registries in the United States and Europe.4,6,10,11 This is consistent with the demographic findings of the PINNACLE India Quality Improvement Programme (PIQIP) registry of outpatients with HFrEF in India where the mean age was 56 years.12 Both ASIAN-HF registry13 and INTER-CHF7 report a mean age of 60 years in Asian patients. More than two-thirds of cases report ischemic etiology, and this is not surprising because it reflects the advanced stage of epidemiological transition in India with more ischemic cardiac events.14
Despite the relatively younger age of participants in THFR, all-cause mortality at 1 year was 30.8%. In the European ESC-HF-LT and American ADHERE registries, the all-cause mortality at 1 year for acute HF was 23.6% and 38.3%, respectively.6,15 THFR demonstrates that most deaths due to HF occur during the most productive years of life, which has profound economic implications for the affected families and the country at large.
THFR illustrates that hospital readmission occurs in nearly 1 of every 3 patients over the course of 1 year. Most of these readmissions are attributable to HF exacerbation. Importantly, the propensity for hospital readmission over 1 year was 30% higher in individuals who did not receive optimal guideline-based medical therapy. Both hospital readmissions and lack of optimal guideline-based medical treatment are also independently associated with increased mortality in HF patients in India. This implies that prescription of guideline-directed medical therapy at discharge from the index HF hospitalization is of paramount importance and significantly affects patient outcomes. In the PIQIP of outpatients with HFrEF in India, only 30% of patients received both ACEI/ARB and β-blockers.12 Despite compelling scientific evidence that ACEI/ARB, β-blockers, and mineralocorticoid receptor antagonists reduce hospitalizations and mortality in HF patients,16 these therapies continue to be underused in India.
The mortality gap between participants who received guideline-directed medical therapy compared with those who did not suggests a large potential effect of hospital-based quality improvement initiatives to improve HF care in India. Protocol-driven postdischarge transitional care at the primary care level has been shown to reduce hospital readmissions.17 The lack of comprehensive postdischarge transitional care in India may be one reason for the high readmission rates for HF in this population. With the increasing burden of HF in India, reducing hospital readmissions and improving adherence to guideline-based medical therapy through quality improvement initiatives will be of paramount public health importance.
There have been attempts to implement quality improvement initiatives for HF management in India. The PIQIP in India concluded that in a country with disproportionate provider-patient ratios and low levels of government funding for quality improvement research, physician-driven initiatives for practice-based learning and improvement are extremely difficult.18 The key barriers include lack of electronic medical records, virtually nonexistent outpatient record-keeping, and difficulty engaging physicians due to hectic clinical schedules. The current health system is struggling with effective management of the existing clinical burden. Hence, new innovative cost-effective methods are required to address the rising burden of HF in resource-limited settings including India. Task-sharing and task-shifting strategies of engaging nonphysician health workers have been proposed as a cost-effective alternative strategies for the management of chronic diseases in resource-limited settings.19 Similar strategies have been useful in secondary prevention of acute coronary syndrome in India by improving adherence to guideline-based medical therapy and healthy lifestyles.20
Several studies have been conducted in high-income countries with trained speciality nurses leading the management of HF.21–25 In most of these studies, a specialist nurse assesses patients with HF and guides medical therapy with the use of evidence-based management protocols. Additional roles of these speciality nurses include patient counseling on self-management of HF at home including daily weights. These strategies have been effective in decreasing hospital readmission rates, reducing hospital length of stay, and increasing adherence to guideline-based optimal medical therapy. Adjunctive innovative strategies in resource-limited settings could include mobile health tools to facilitate HF management.
Limitations of this study include enrolment of participants restricted to Trivandrum district in Kerala which may not be representative of the broader population of India. Additionally, the prescribed dose of guideline-based medications was not recorded, and hence, medications may not have been titrated to recommended maximum doses.
Policy implication
Higher mortality in HF patients especially in the immediate postdischarge period calls for innovative and cost-effective quality improvement programs in management of HF in resource-sensitive settings. A technology-enabled nurse as an immediate access point for all HF patients and an intermediary between patients and physicians may improve health outcomes. Such strategies need to be tested and evaluated in Indian settings. Availability of low-cost generic medicines to everyone may improve adherence to guideline-directed therapy. Primary prevention efforts to control the incidence of ischemic events, better secondary care facilities for all high-risk patients, and efficient transportation to hospitals in case of acute events may help to reduce the number of patients with HF at the population level.
Conclusion
THFR is the first such registry in India to report long-term mortality outcomes. In THFR, 1 of 3 HF patients died within 1-year follow-up. Poor adherence to guideline-directed medical treatment is associated with increased hospital readmissions and mortality. Quality improvement programs targeting improved adherence to guideline-based medical therapy and reducing hospital readmissions may result in significant survival benefits in the relatively younger cohort of HF patients in India.
Acknowledgements
ICMR: for funding the study. We thank Krishna Sanker, Suresh Babu, Vineeth Purushothaman, Anand Kumar, Ajeesh C., and Manas Chacko for data collection, data entry, and follow-up data collection. We also thank Dr. Priya Sosa James, Department of Medicine, and Dr. Abdul Salam and Dr. Anil Balachandran, Department of Cardiology, Medical College, Trivandrum, for data collection.
Funding:
Indian Council for Medical Research, New Delhi, India.
Footnotes
Disclosures
P Jeemon is supported by a Clinical and Public Health intermediate fellowship from the Wellcome Trust-Department of Biotechnology, India Alliance (2015–2020).
References
- 1.GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (Lond Engl) 2016;388(10053):1459–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huffman MD, Prabhakaran D. Heart failure: epidemiology and prevention in India. Natl Med J India 2010;23(5):283–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Harikrishnan S, Sanjay G, Anees T, et al. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum Heart Failure Registry. Eur J Heart Fail 2015;17(8):794–800. [DOI] [PubMed] [Google Scholar]
- 4.Adams KF, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J 2005;149(2):209–16. [DOI] [PubMed] [Google Scholar]
- 5.Callender T, Woodward M, Roth G, et al. Heart failure care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med 2014;11(8). [Internet, cited 2016 Sep 9, Available from: , http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4130667/]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crespo-Leiro MG, Anker SD, Maggioni AP, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail 2016;18(6):613–25. [DOI] [PubMed] [Google Scholar]
- 7.Dokainish H, Teo K, Zhu J, et al. Heart failure in Africa, Asia, the Middle East and South America: the INTER-CHF study. Int J Cardiol 2016;204:133–41. [DOI] [PubMed] [Google Scholar]
- 8.Sivadasan Pillai Harikrishnan, Sanjay G. Heart failure in South Asia. Curr Cardiol Rev 2013;9(2):102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McMurray JJV, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2012;14(8):803–69. [DOI] [PubMed] [Google Scholar]
- 10.Maggioni AP, Anker SD, Dahlström U, et al. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail 2013;15(10):1173–84. [DOI] [PubMed] [Google Scholar]
- 11.Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J 2006;27(22):2725–36. [DOI] [PubMed] [Google Scholar]
- 12.Pokharel Y, Wei J, Hira RS, et al. Guideline-directed medication use in patients with heart failure with reduced ejection fraction in India: American College of Cardiology’s PINNACLE India Quality Improvement Program. Clin Cardiol 2016;39(3):145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lam CSP, Teng T-HK, Tay WT, et al. Regional and ethnic differences among patients with heart failure in Asia: the Asian sudden cardiac death in heart failure registry. Eur Heart J 2016;7. [DOI] [PubMed] [Google Scholar]
- 14.Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation 2016;133(16):1605–20. [DOI] [PubMed] [Google Scholar]
- 15.Kociol RD, Hammill BG, Fonarow GC, et al. Associations between use of the hospitalist model and quality of care and outcomes of older patients hospitalized for heart failure. JACC Heart Fail 2013;1(5):445–53. [DOI] [PubMed] [Google Scholar]
- 16.Poelzl G, Altenberger J, Pacher R, et al. Dose matters! Optimisation of guideline adherence is associated with lower mortality in stable patients with chronic heart failure. Int J Cardiol 2014;175(1):83–9. [DOI] [PubMed] [Google Scholar]
- 17.Avaldi VM, Lenzi J, Castaldini I, et al. Hospital readmissions of patients with heart failure: the impact of hospital and primary care organizational factors in Northern Italy. PLoS One 2015;10(5):e0127796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalra A, Pokharel Y, Hira RS, et al. Cardiovascular disease performance measures in the outpatient setting in India: insights from the American College of Cardiology’s PINNACLE India Quality Improvement Program (PIQIP). J Am Heart Assoc 2015;4(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaziano T, Abrahams-Gessel S, Surka S, et al. Cardiovascular disease screening by community health workers can be cost-effective in low-resource countries. Health Aff 2015;34(9):1538–45, 10.1161/JAHA.115.001910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xavier D, Gupta R, Kamath D, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol 2016;4(3):244–53. [DOI] [PubMed] [Google Scholar]
- 21.Blue L, Lang E, McMurray JJ, et al. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ 2001;323(7315):715–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunagan WC, Littenberg B, Ewald GA, et al. Randomized trial of a nurse-administered, telephone-based disease management program for patients with heart failure. J Card Fail 2005;11(5):358–65. [DOI] [PubMed] [Google Scholar]
- 23.Sisk JE, Hebert PL, Horowitz CR, et al. Effects of nurse management on the quality of heart failure care in minority communities: a randomized trial. Ann Intern Med 2006;145(4):273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith CE, Piamjariyakul U, Dalton KM, et al. Nurse-led multidisciplinary heart failure group clinic appointments: methods, materials, and outcomes used in the clinical trial. J Cardiovasc Nurs 2015;30(4 Suppl 1):S25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smeulders ESTF, van Haastregt JCM, Ambergen T, et al. Nurse-led self-management group programme for patients with congestive heart failure: randomized controlled trial. J Adv Nurs 2010;66(7):1487–99. [DOI] [PubMed] [Google Scholar]


