Abstract
Introduction:
Heart failure (HF) has emerged as an important and increasing disease burden in India. We present the 5-year outcomes of patients hospitalized for HF in India.
Methods:
The Trivandrum Heart Failure Registry (THFR) recruited consecutive patients admitted for acute HF among 16 hospitals in Trivandrum, Kerala in 2013. Guideline-directed medical therapy (GDMT) was defined as the combination of beta-blockers (BB), renin angiotensin system blockers (RAS), and mineralocorticoid receptor antagonists (MRA) in patients with HF with reduced ejection fraction (HFrEF, EF < 40%) at discharge. We used Cox proportional hazards models and Kaplan-Meier survival plots for analysis. The MAGGIC risk score variables were included as exposure variables.
Results:
Among 1205 patients [69% male, mean (SD) age = 61.2 (13.7) years], HFrEF constituted 62% of patients and among them, 25% received GDMT. The 5-year mortality rate was 59% (n = 709 deaths), and median survival was 3.1 years. Sudden cardiac death and pump failure caused 46% and 49% of the deaths, respectively. In the multivariate Cox model, components of GDMT associated with lower 5-year mortality risks were discharge prescription of BB, RAS blocker, and MRA. Older age, lower systolic blood pressure, NYHA class III or IV, and higher serum creatinine were also associated with higher 5-year mortality.
Conclusions:
Three out of every 5 patients had died during 5-years of follow-up with a median survival of approximately 3 years. Lack of GDMT in patients with HFrEF and frequent readmissions were associated with higher 5-year mortality. Quality improvement programmes with strategies to improve adherence to GDMT and reduction in readmissions may improve HF outcomes in this region.
Keywords: Heart failure, Registry, Mortality, India, Cohort, Long term
1. Introduction
Heart failure (HF) is a global public health problem affecting more than 26 million people worldwide [1]. Most longitudinal outcome data for patients with HF are from high-income countries [2,3]. Available data from low- and middle-income countries (LMICs) are limited to short-term outcomes of patients with HF or single-centre studies and suggest that mortality rates for patients with HF are higher in LMICs than high-income countries [4,5–8]. Further, wide heterogeneity in the causes and associated comorbidities in patients with HF across the globe [9,10] limits the extrapolation of long-term mortality data from high-income regions to LMICs.
Long-term outcome data and identifying factors associated with long-term prognosis are important for devising policy strategies to address the growing burden and management strategies for HF in India. We describe 5-year outcomes of patients with HF and evaluate factors associated with mortality in the Trivandrum Heart Failure Registry (THFR), which is India’s first HF registry.
2. Methods
2.1. Study sample
The design of THFR has been reported previously [5–8]. Briefly, THFR is a prospective, hospital-based registry of patients admitted with acute HF who were longitudinally followed over time. Patients were recruited from 16 hospitals in the region of Trivandrum, Kerala, India that cared for patients with HF from January 2013 to December 2013. The registry covered the Trivandrum city area (urban area: 215 km2, population: 957,000 people) and an adjacent suburban rural area, Athiyannoor block panchayat, (rural area: 60 km2, population: 166,549 people).
Consecutive patients aged 18 years and above with HF, as defined by the 2012 European Society of Cardiology (ESC) criteria, were enrolled [11]. All patients had echocardiograms as recommended by the ESC heart failure guidelines [11]. Trained research nurses collected data using a structured questionnaire. Data collected included demographic characteristics, medical history, clinical presentation, laboratory values, treatment and clinical outcomes. The patients were followed up in the same hospitals where they were enrolled. Follow-up information for enrolled patients discharged following the index hospitalization was obtained every 3 to 6 months at follow-up visits, subsequent hospital readmissions, or by telephone. If unsuccessful at telephone contacts, the study team attempted to contact the subjects through surface mail, community-level health staff, postal delivery personnel, local civic body representatives, and religious institutions. Data collected at each follow-up included details of hospital readmissions (both cardiac and non-cardiac), cardiac procedures, and all-cause and cause-specific mortality. Dates of each event were captured and supporting hospital records were obtained whenever possible. Cause of death was ascertained by verifying hospital records or by verbal autopsy conducted by trained nurses. Deaths were classified as non-cardiac deaths, deaths due to worsening HF, and sudden cardiac death.
All study participants provided written informed consent. The study was approved by the Institutional Review Board of Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, India (SCT/IEC/477/December-2012) and was funded by the Indian Council of Medical Research.
2.2. Definitions
Patients were classified into three groups based on left ventricular ejection fraction (LVEF) measured during index hospitalization as per the ESC Guidelines 2016 [11]: 1) heart failure with reduced ejection fraction (HFrEF, LVEF <40%), 2) heart failure with mid-range ejection fraction (HFmrEF, LVEF 40–49%), and 3) heart failure with preserved ejection fraction (HFpEF, LVEF ≥50%). Guideline directed medical therapy (GDMT) was defined as being prescribed the combination of beta-blockers (BB), renin angiotensin system (RAS) blockers, such as angiotensin converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARB), and mineralocorticoid receptor antagonists (MRA) for patients with HFrEF at hospital discharge.
2.3. Statistical analysis
Categorical variables are reported as frequencies with proportions (%) and continuous variables as means with standard deviations (SD), or as medians with interquartile ranges (IQR), if data were skewed. Cumulative incidence rates are reported, accounting for all-cause and cause-specific mortality and rehospitalizations as separate outcomes, as well as a composite outcome. We created Kaplan-Meier survival plots and used log-rank statistics to compare time to event across subgroups based on baseline GDMT status and baseline LVEF. We created Cox proportional hazards models to compare event rates by the same subgroups and adjusted for covariates in the Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC) risk score [12]. Follow-up data were right censored at 5 years. A two-sided p value <0.05 defined statistical significance. Statistical analyses were performed using Stata version 13 (StataCorp, College Station, TX, USA).
3. Results
Baseline characteristics of 1205 participants (69% males, mean [SD] age 61.2 [13.7] years) are reported in Table 1. Ischaemic heart disease (72%) was the most common aetiology of HF followed by dilated cardiomyopathy and rheumatic heart disease (Table 2). Hypertension and diabetes mellitus were prevalent in 55% and 52% of the study participants, respectively. HFrEF was the most common group (62%), followed by HFpEF (20%) and HFmEF (18%). The in-hospital mortality was 8.4%. At discharge, beta blockers (58%), ACE-I or ARB (48%), and mineralocorticoid receptor antagonists (46%) were prescribed among patients.
Table 1.
Baseline data from the Trivandrum Heart Failure Registry, stratified by baseline left ventricular ejection fraction.
| HFrEF (n = 752) | HFmrEF (n = 263) | HFpEF (n = 190) | P value | |
|---|---|---|---|---|
|
| ||||
| Females, n (%) | 205 (27.3) | 83 (31.6) | 83 (43.7) | <0.001 |
| Age, mean (SD) | 61.8 (13.4) | 60.8 (13.7) | 59.4 (14.5) | 0.08 |
| Educational status, n (%) | 0.56 | |||
| No education | 97 (12.9) | 27 (10.3) | 18 (9.6) | |
| Up to primary | 329 (43.8) | 116 (44.6) | 95 (50.5) | |
| Secondary | 228 (30.4) | 85 (32.3) | 50 (26.6) | |
| Graduate and above | 97 (12.9) | 35 (13.3) | 25 (13.3) | |
| Acute, de novo heart failure, n (%) | 276 (36.7) | 117 (44.5) | 86 (45.3) | 0.02 |
| Aetiology of heart failure, n (%) | ||||
| Ischaemic heart disease | 561 (74.6) | 198 (79.3) | 107 (56.3) | <0.001 |
| Dilated cardiomyopathy | 128 (17.0) | 20 (7.6) | 8 (4.2) | |
| Hypertrophic cardiomyopathy | 6 (0.8) | 6 (2.3) | 15 (7.9) | |
| Rheumatic heart disease | 32 (4.3) | 23 (8.8) | 40 (21.1) | |
| Hypertension | 1 (0.1) | 3(1.1) | 7 (3.7) | |
| Miscellaneous | 24 (3.2) | 13 (4.9) | 13 (6.8) | |
| Tobacco use, n (%) | <0.001 | |||
| Never used | 411 (54.7) | 176 (66.9) | 129 (67.9) | |
| Current use | 130 (17.3) | 41 (15.6) | 17 (8.9) | |
| Past use | 211 (28.1) | 46 (17.5) | 44 (23.2) | |
| History of hypertension, n (%) | 442 (58.8) | 150 (57.0) | 104 (54.8) | 0.58 |
| History of diabetes, n (%) | 415 (55.2) | 156 (59.3) | 91 (47.9) | 0.05 |
| History of atrial fibrillation/flutter, n (%) | 97 (12.9) | 34(12.9) | 46 (24.2) | <0.001 |
| History of stroke, n (%) | 48 (6.4) | 16 (6.1) | 11 (5.8) | 0.95 |
| History of COPD, n (%) | 125 (16.6) | 29 (11.0) | 32 (16.8) | 0.08 |
| History of CKD, n (%) | 130 (17.3) | 54 (20.5) | 32 (16.8) | 0.45 |
| NYHA class, n (%) | 0.17 | |||
| NYHA class II or below | 18 (2.5) | 7 (2.7) | 11 (6.0) | |
| NYHA class III | 463 (63.9) | 167 (65.2) | 114(62.6) | |
| NYHA class IV | 243 (33.6) | 82 (32.0) | 57 (31.3) | |
| Heart rate in beats per minute, mean (SD) | 99 (22) | 96 (20) | 95 (25) | 0.001 |
| Systolic blood pressure in mmHg, mean (SD) | 126.8 (30.4) | 133.4 (35.3) | 133.7 (34.7) | 0.002 |
| Diastolic blood pressure in mmHg, mean (SD) | 80.1 (16.5) | 81.8 (16.9) | 80.6 (16.6) | 0.36 |
| Serum creatinine in mg/dL, mean (SD) | 1.5 (1.0) | 1.4 (0.7) | 1.3 (0.7) | 0.02 |
| Haemoglobin in g/dL, mean (SD) | 12.0 (2.0) | 12.1 (2.3) | 11.9 (1.9) | 0.48 |
| Serum sodium in mEq/L, mean (SD) | 134.9 (6.0) | 135.4 (0.2) | 135.8 (6.2) | 0.14 |
| Beta-blocker at discharge, n (%)* | 443 (65.9) | 149 (60.6) | 106 (57.3) | 0.06 |
| ACE-I or ARB at discharge n (%)* | 369 (49) | 126 (49.8) | 83 (43.6) | 0.03 |
| Aldosterone antagonists at discharge, n (%)* | 382 (51) | 110 (41.8) | 59 (31) | <0.001 |
| Guideline directed medical therapy, n (%) | 191 (25.4) | NA | NA | NA |
HFpEF: heart failurewith preserved ejectionfraction, EF>50%;HFrEF: heart failurewith reducedejection fraction,EF<40%;HFmrEF: heart failurewithmid-range ejection fraction,EF 40–49%; COPD: chronic obstructive pulmonary disease; CKD: chronic kidney disease; NYHA: New York Heart Association; ACE-I: angiotensin-converting enzyme inhibitor; ARB:angiotensin-receptor blocker,NA:notapplicable.Heart rate,bloodpressure, serumsodium, and serumcreatinineweremeasured at baseline.
minor differences fromour baseline paper due to further data cleaning (Beta-blocker at discharge =698 instead of 701; ACE-I or ARB at discharge =578 instead of 587; Aldosterone receptor antagonists at discharge= 551 instead of 553).
Table 2.
All-cause mortality rate (95% CI) per 100 person years (p-y) of follow-up.
| Variables | HFrEF (n = 752) | HFmrEF (n = 263) | HFpEF (n = 190) | Total (n = 1205) |
|---|---|---|---|---|
|
| ||||
| Men, per 100 p-y | 25.3 (22.8, 28.2) | 20.9 (17.3, 25.3) | 14.1 (10.6,18.7) | 22.7 (19.8, 25.9) |
| Women, per 100 p-y | 24.0 (20.1,28.6) | 25.5 (19.5, 33.4) | 17.4(12.8, 23.5) | 22.6 (20.7, 24.7) |
| Total, per 100 p-y | 24.9 (22.8,27.3) | 22.3 (19.1,26.0) | 15.5(12.6,19.0) | 22.6 (21.0, 24.3) |
One-quarter (25.4%) of patients with HFrEF were discharged on GDMT from index hospitalization, and less than 2% of patients had an implantable cardioverter defibrillator. Of 1205 patients enrolled in THFR, 72 (6%) patients were lost to follow-up. There were no significant differences between the patients lost to follow-up and those on follow-up except that those lost to follow-up were younger (57.7 vs 61.5 years) Table S1. The unadjusted 5-year mortality rate was 59% (61.3%, 60.5%, and 46.8% in HFrEF, HFmrEF and HFpEF groups, respectively) with a cumulative incidence rate of 22.6 per 100 person-years (95% CI: 21.0–24.3, Table 2). Median survival time was 3.1 years. Among patients with HFrEF who died, 48% (n = 219) died from sudden cardiac death, and 48% (n = 219) died from worsening HF. Kaplan-Meier curves for mortality demonstrate a higher survival rate in patients with HFrEF discharged from index hospitalization on GDMT as compared to those who were not discharged on GDMT (Fig. 1). The lowest cumulative incidence rate of mortality was in patients with HFpEF (log rank p < 0.001; Fig. 1).
Fig. 1.
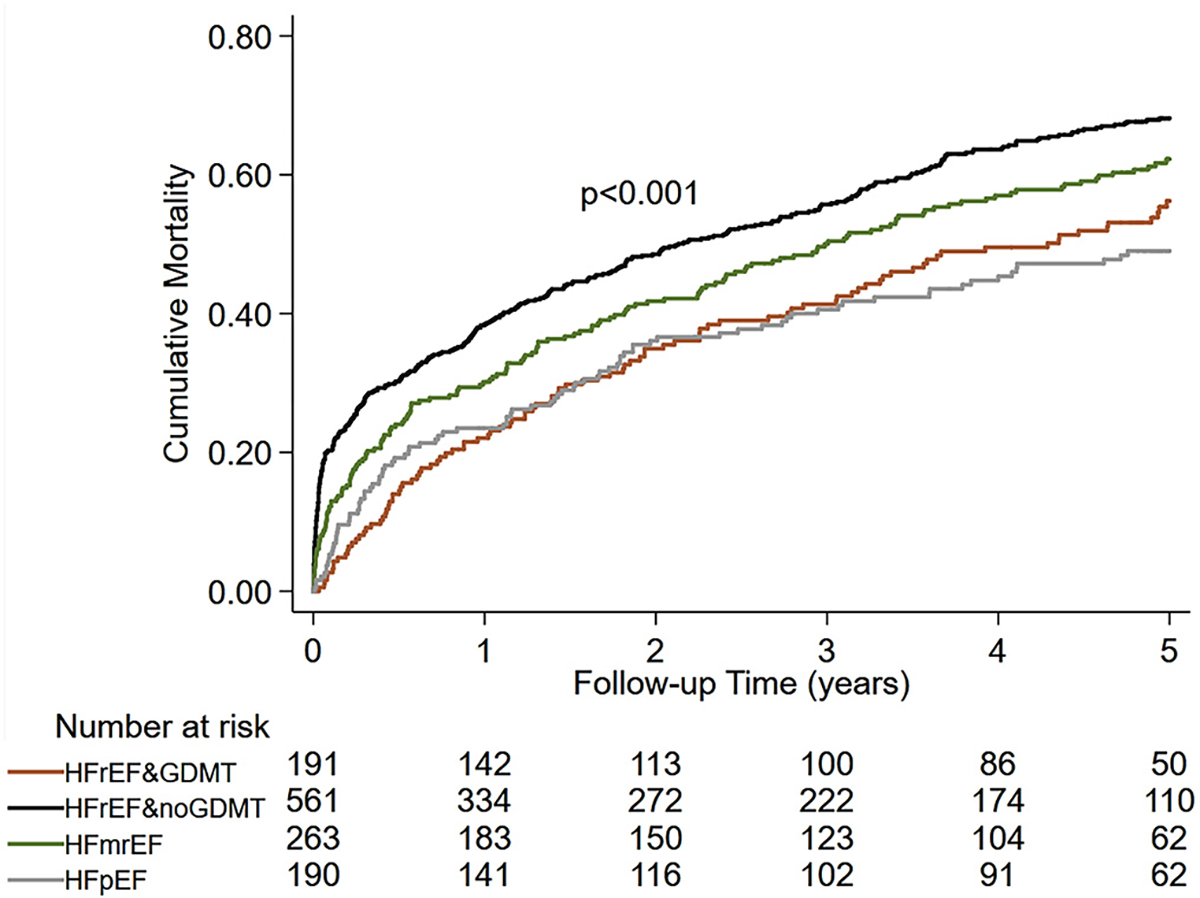
Five year cumulative incidence mortality rates by heart failure type and presence or absence of baseline guideline directed medial therapy.
The hospital readmission rate was 49% over the 5-year follow-up period. The 5-year cumulative mortality rate was 50% in patients with zero hospital readmissions and was 69% in individuals with ≥1 re-admission (Fig. 2).
Fig. 2.
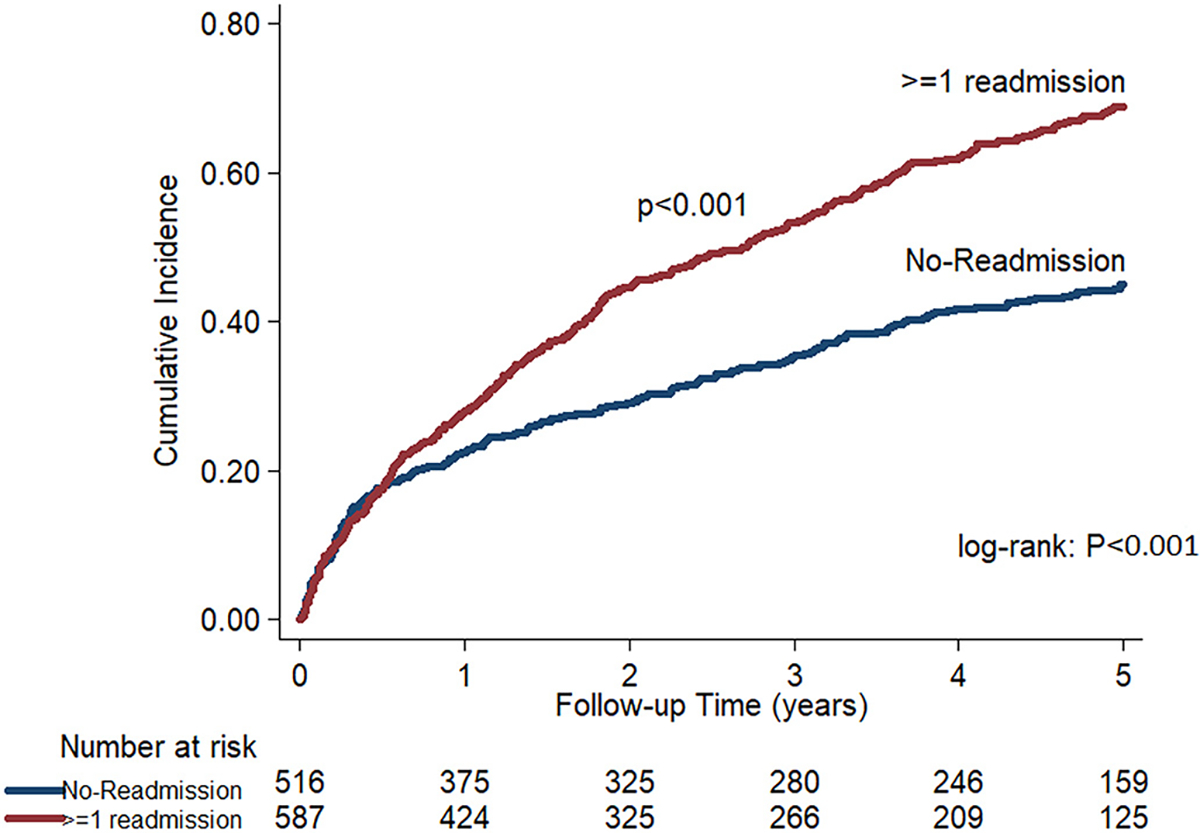
Five-year cumulative incidence rates for all-cause mortality based on the presence of hospital re-admission.
The adjusted Cox proportional models demonstrated that baseline age, systolic blood pressure, NYHA class III/IV status, serum creatinine, and discharge GDMT were independently associated with outcomes (Table 3). The components of GDMT were associated with lower 5-year mortality risk: 36% for beta-blockers (HR = 0.64; 95% CI: 0.55–0.74, p < 0.001), 22% for RAS blockers (HR = 0.78; 95% CI: 0.66–0.90, p = 0.002), and 25% for MRA (HR = 0.75; 95% CI: 0.64–0.88, p < 0.001).
Table 3.
Factors associated with 5-year mortality in the Trivandrum Heart Failure Registry.
| Variables | Model 1a |
Model 2b |
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
|
| ||||||
| HFmrEF (referent HFrEF) | 0.91 | 0.76,1.09 | 0.30 | 0.94 | 0.78,1.14 | 0.52 |
| HFpEF (referent HFrEF) | 0.65 | 0.51, 0.81 | <0.001 | 0.72 | 0.57, 0.92 | 0.01 |
| Age (per 10 years) | 1.22 | 1.15, 1.29 | <0.001 | 1.21 | 1.14, 1.29 | <0.001 |
| Male sex | 0.99 | 0.85, 1.17 | 0.98 | 0.97 | 0.81, 1.16 | 0.76 |
| Baseline smoking | 0.96 | 0.78, 1.19 | 0.73 | 1.12 | 0.89, 1.40 | 0.33 |
| Diabetes mellitus | 1.25 | 1.08, 1.46 | 0.003 | 1.15 | 0.97, 1.35 | 0.10 |
| COPD | 1.23 | 1.01, 1.50 | 0.04 | 0.95 | 0.76, 1.19 | 0.64 |
| SBP (per 10 mmHg) | 0.97 | 0.95, 0.99 | 0.02 | 0.94 | 0.92, 0.97 | <0.001 |
| NYHAclass III (reference Class I/II) | 2.32 | 1.28, 4.23 | 0.01 | 2.01 | 1.09, 3.67 | 0.02 |
| NYHA class IV (reference Class I/II) | 3.23 | 1.78, 5.91 | <0.001 | 2.82 | 1.53, 5.17 | 0.001 |
| Serum creatinine (per mg/dl) | 1.18 | 1.11, 1.25 | <0.001 | 1.11 | 1.03, 1.18 | 0.004 |
| Discharge beta-blocker | 0.55 | 0.47, 0.64 | <0.001 | 0.64 | 0.55, 0.74 | <0.001 |
| Discharge ACE-I or ARB | 0.67 | 0.58, 0.79 | <0.001 | 0.78 | 0.66, 0.90 | 0.002 |
| Discharge aldosterone receptor antagonist | 0.74 | 0.64, 0.86 | <0.001 | 0.75 | 0.64, 0.88 | <0.001 |
HFrEF: heart failure with reduced ejection fraction; HFmrEF: heart failurewithmidrange ejection fraction;HFpEF: heart failurewith preserved ejection fraction; COPD: chronic obstructive pulmonary disease; SBP: systolic blood pressure; NYHA: NewYork Heart Association; ACE-I: angiotensin-converting enzyme inhibitor; ARB: angiotensin-receptor blocker; GDMT: guideline-directed medical therapy.
Model 1: unadjusted model.
Model 2: adjusted for age per 10 years, sex, current smoking status, SBP per 10 mmHg increase, diabetes, NYHA function class, COPD, serum creatinine, baseline beta-blocker and ACE-I or ARB on index admission.
Patients with HFpEF had a 28% lower 5-year mortality (HR = 0.72; 95% CI: 0.57–0.92, p = 0.010) in comparison to HFrEF. The 5-year mortality was almost 3 times higher in individuals with NYHA class III and class IV as compared to NYHA class II (HR = 2.8; 95% CI: 1.53–5.17, p = 0.001). Each 10 mmHg increase in systolic blood pressure was associated with 6% (HR = 0.94; 95% CI: 0.92–0.97, p < 0.001) lower 5-year mortality risk. Each unit increase in serum creatinine in mg/dl (per 1 mg/dL) was associated with 11% higher risk of 5-year mortality (HR = 1.11; 95% CI: 1.03–1.18, p = 0.004).
4. Discussion
We report that 59% of patients with HF in THFR died at 5 years, which represents the longest follow-up data of patients with HF in India. Our cohort of patients with acute HF is a much younger cohort compared to high-income country cohorts. The younger mean age of patients in the THFR also contrasts with the median age of 73 years among patients hospitalized with heart failure in China [13]. The in-hospital mortality of 8.4% and one year mortality of 30.8% is higher than the observed figures in similar recent registries like the ESC-EORP-HFA Heart Failure Long-Term Registry [14]; 5.3% and 22.8%, respectively. Median survival time of 3.1 years is alarming because the mean age of patients with HF in THFR is over a decade younger than observed in high-income countries and China. Despite substantially younger age of patients with HF in India, the 5-year mortality rate mirrors that of high-income countries including United States (75%), Denmark (61%), Sweden (68%), and United Kingdom (63%) [2,15–17].
Most deaths in THFR were due to worsening HF or sudden cardiac death. Comparatively, cardiovascular deaths are less common in patients with HF in high income countries and are being increasingly replaced by causes related to infections or neoplasms [3]. The treatment of patients with HFrEF using optimal GDMT and appropriate device use may be key reasons for lower cardiovascular deaths observed in HF patients from high-income countries compared with this study. Sudden cardiac death was a major cause of death in approximately half of the patients in THFR. The high risk for sudden cardiac death in patients with HFrEF and HFpEF has been documented in high-income countries, though not to this extent in India [18,19]. Despite evidence on implantable cardioverter defibrillator therapy in reducing overall mortality for patients with HFrEF, less than 2% of patients in THFR received these guideline-recommended devices, likely due to health system and resource constraints.
Discharge prescription rates of GDMT at index hospitalization were inversely associated with mortality throughout the study period and was maintained at 5 years. Only one-quarter of patients were prescribed GDMT at the time of discharge at index hospitalization. Several factors could have influenced the prescription of GDMT, including hemodynamic factors and renal function. Given the long-term consequences, it might help to explore these reasons and incorporate the information gained from the same in future quality-improvement measures. The ongoing National Heart Failure Registry is expected to provide information on patterns of GDMT utilisation in patients with acute heart failure in India [20]. The readmission rate at 5 years was 49% in THFR, which is similar to readmission rates reported from the United States [15]. Hospital HF readmissions are a risk factor for mortality, and many are preventable. Care coordination, team-based care, and telemonitoring, including medication adherence interventions, can reduce the risk of readmissions and HF-associated mortality [19,21]. Quality improvement interventions targeting at increased prescription, adherence, and accessibility rates of GMDT in India aimed at patients, healthcare providers, and health systems should be priorities to reduce the burden of HF in LMIC settings, but have not been widely tested [22]. Implementation strategies need to account for health system factors, including relative emphasis on HF quality improvement compared with other conditions, use of technology and combination therapy for better GDMT initiation and long-term adherence, and investments to reduce out-of-pockets costs associated with GDMT [23].
4.1. Strengths and limitations
Strengths of this study include enrolment of consecutive HF patients in all the hospitals in the region during the one-year recruitment period and a high 5-year follow-up rate.
Limitations include a relatively small cohort with 1205 patients. The treatment details, risk factor control, and drug doses were not available in all patients over time. However, longitudinal factors are not included in most heart failure risk calculators, including MAGGIC risk calculator for HF, so the influence of these limitations is uncertain. The accuracy of adjudication of cause of death in non-hospitalized patients is another potential limitation, but the overall mortality rate remains high.
5. Conclusions
Three out of every 5 patients died during the 5-year follow-up period in the first HF registry in India. Only 25% of patients were discharged from the index hospitalization on GDMT and importantly, prescription of GDMT at discharge was associated with lower 5-year mortality rates in patients with HFrEF. Quality improvement interventions to increase evidence-based management and prevention of hospital readmissions may substantially improve outcomes of patients with HF in India.
Supplementary Material
Acknowledgements
The authors thankKochumoni, SureshBabu,VineethPurushothaman, Anand Kumar, Ajeesh C, Krishna Sanker and Manas Chacko for data collection, data entry and follow-up data collection. The contributions of Dr. Jayapal and Dr. Arun of General Hospital, Dr. BVR Kumar of Jubilee hospital and Dr. Suman of KIMS hospital are acknowledged. We also thank Dr. Priya Sosa James, Dr. Abdul Salam and Dr. Anil Balachandran for data collection.
Funding
We thank Indian Council of Medical Research (ICMR), India (Project No. 5/4/1–11/11-NCD-II - Comprehensive heart failure intervention program) and Indian Council of Medical Research (ICMR), India - Trivandrum Heart Failure Cohort. File number 50/1(5) / TF CVD / 16 / NCD-II for funding this study.
Footnotes
Disclosures
SH has received project funds from ICMR for Trivandrum HF Cohort, National HF registry and CARE HF (2019–2023). PJ is supported by a Clinical and Public Health intermediate fellowship (grant number IA/CPHI/14/1/501497) from the Wellcome Trust-Department of Biotechnology, India Alliance (2015–2020). MDH has received previous support from the World Heart Federation via Boehringer Ingelheim, Bupa, and Novartis and the American Heart Association, Verily, and AstraZeneca for work unrelated to this research. MDH has received salary support from the American Medical Association for his role as an associate editor for JAMA Cardiology. The George Institute for Global Health has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy through its social enterprise business, George Medicines, but MDH is not directly involved with this research.
CRediT authorship contribution statement
Conceptualization: SH, SG, SV, MS, GV, CB, TN, NR, KS, MH. Data curation: SH, SG, SV, MS, GV, CB, RB, TN, NP, KK, NR, KS. Formal analysis: PJ, SH, MH, AA. Funding acquisition: SH, SG. Methodology: SH, SG, MH. Project administration: SH SG. Writing - original draft; SH, SG, PJ, AA, MH. Writing - review & editing. SH, SG, PJ, AA, MH, SV, MS, GV, CB, RB, TN, NP, KK, NR, KS.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcard.2020.10.012.
References
- [1].Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, et al. , The Global Health and economic burden of hospitalizations for heart FailureLessons learned from hospitalized heart failure registries, J. Am. Coll. Cardiol. 63 (12) (2014. Apr 1) 1123–1133. [DOI] [PubMed] [Google Scholar]
- [2].Taylor CJ, Ordóñez-Mena JM, Roalfe AK, Lay-Flurrie S, Jones NR, Marshall T, et al. , Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study, BMJ. 364 (2019. Feb 13) l223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Conrad N, Judge A, Canoy D, Tran J, Pinho-Gomes A-C, Millett ERC, et al. , Temporal trends and patterns in mortality after incident heart failure: a longitudinal analysis of 86 000 individuals, JAMA Cardiol. 4 (11) (2019. Nov 1) 1102–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Callender T, Woodward M, Roth G, Farzadfar F, Lemarie J-C, Gicquel S, et al. , Heart failure care in low- and middle-income countries: a systematic review and meta-analysis, PLoS Med. 11 (8) (2014. Aug), e1001699,. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sanjay G, Jeemon P, Agarwal A, Viswanathan S, Sreedharan M, Vijayaraghavan G, et al. , In-hospital and three-year outcomes of heart failure patients in South India: the Trivandrum heart failure registry, J. Card. Fail 24 (12) (2018. Dec 1) 842–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Harikrishnan S, Sanjay G, Agarwal A, Kumar NP, Kumar KK, Bahuleyan CG, et al. , One-year mortality outcomes and hospital readmissions of patients admitted with acute heart failure: data from the Trivandrum heart failure registry in Kerala, India, Am. Heart J. 189 (2017. Jul) 193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Harikrishnan S, Sanjay G, Anees T, Viswanathan S, Vijayaraghavan G, Bahuleyan CG, et al. , Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum heart failure registry, Eur. J. Heart Fail 17 (8) (2015. Aug) 794–800. [DOI] [PubMed] [Google Scholar]
- [8].Ganapathi S, Jeemon P, Krishnasankar R, Kochumoni R, Vineeth P, Nair KKM, et al. , Early and Long-Term Outcomes of Decompensated Heart Failure Patients in a Tertiary-Care Centre in India, ESC Heart Fail. 7 (2) (2020. Apr) 467–473, 10.1002/ehf2.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tromp J, Bamadhaj S, Cleland JGF, Angermann CE, Dahlstrom U, Ouwerkerk W, et al. , Post-discharge prognosis of patients admitted to hospital for heart failure by world region, and national level of income and income disparity (REPORT-HF): a cohort study, Lancet Glob. Health 8 (3) (2020. Mar) e411–e422. [DOI] [PubMed] [Google Scholar]
- [10].Naik N, Narula J, Heart failure in low-income and middle-income countries: failing REPORT card grades, Lancet Glob. Health 8 (3) (2020. Mar) e318. [DOI] [PubMed] [Google Scholar]
- [11].Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. , 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failureThe task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)developed with the special contribution of the heart failure association (HFA) of the ESC, Eur. Heart J. 37 (27) (2016. Jul 14) 2129–2200. [DOI] [PubMed] [Google Scholar]
- [12].Pocock SJ, Ariti CA, McMurray JJV, Maggioni A, Køber L, Squire IB, et al. , Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies, Eur. Heart J. 34 (19) (2013. May) 1404–1413. [DOI] [PubMed] [Google Scholar]
- [13].Gupta A, Yu Y, Tan Q, Liu S, Masoudi FA, Du X, et al. , Quality of Care for Patients Hospitalized for heart failure in China, JAMA Netw. Open 3 (1) (2020. Jan 3), e1918619,. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chioncel O, Mebazaa A, Maggioni AP, Harjola V-P, Rosano G, Laroche C, et al. , Acute heart failure congestion and perfusion status - impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA heart failure long-term registry, Eur. J. Heart Fail 21 (11) (2019) 1338–1352. [DOI] [PubMed] [Google Scholar]
- [15].Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, et al. , Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes, J. Am. Coll. Cardiol. 70 (20) (2017. Nov 14) 2476–2486. [DOI] [PubMed] [Google Scholar]
- [16].Schmidt M, Ulrichsen SP, Pedersen L, Bøtker HE, Sørensen HT, Thirty-year trends in heart failure hospitalization and mortality rates and the prognostic impact of comorbidity: a Danish nationwide cohort study, Eur. J. Heart Fail 18 (5) (2016) 490–499. [DOI] [PubMed] [Google Scholar]
- [17].Kontogeorgos S, Thunström E, Johansson MC, Fu M, Heart failure with preserved ejection fraction has a better long-term prognosis than heart failure with reduced ejection fraction in old patients in a 5-year follow-up retrospective study, Int. J. Cardiol 232 (2017. Apr 1) 86–92. [DOI] [PubMed] [Google Scholar]
- [18].Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KKL, et al. , Long-term trends in the incidence of and survival with heart failure, N. Engl. J. Med. 347 (18) (2002. Oct 31) 1397–1402. [DOI] [PubMed] [Google Scholar]
- [19].Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar-Jacob JM, Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials, J. Am. Heart Assoc 5 (2016. 17) 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Harikrishnan S, Bahl A, Roy A, Mishra A, Prajapati J, Nanjappa MC, et al. , National Heart Failure Registry, India: design and methods, Indian Heart J. 71 (6) (2019. Dec) 488–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Huffman M, Roth G, Sliwa K, Yancy C, Prabhakaran D, Heart failure, in: Prabhakaran D, Anand S, Gaziano T, Mbanya J, Wu Y, Nugent R (Eds.), Disease Control Priorities (third edition): Volume 5, Cardiovascular, Respiratory, and Related Disorders, World Bank, Washington, DC, 2018. [Google Scholar]
- [22].Agarwal A, Bahiru E, Yoo SGK, Berendsen MA, Harikrishnan S, Hernandez AF, et al. , Hospital-based quality improvement interventions for patients with heart failure: a systematic review, Heart Br. Card Soc 105 (6) (2019. Mar) 431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Agarwal A, Davies D, Goenka S, Prabhakaran D, Huffman MD, Mohanan PP, Facilitators and barriers of heart failure care in Kerala, India: a qualitative analysis of health-care providers and administrators, Indian Heart J. 71 (3) (2019. Jun) 235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


