Community health centers provide access to method switching and long-acting reversible contraception removal.
Abstract
OBJECTIVE:
To describe patterns of contraceptive method switching and long-acting reversible contraception (LARC) removal in a large network of community health centers.
METHODS:
We conducted a retrospective cohort study using individual-level electronic health record data from 489 clinics in 20 states from 2016 to 2021. We used logistic regression models, including individual-, clinic-, and state-level covariates, to calculate adjusted odds ratios and predicted probabilities of any observed contraceptive method switching and LARC removal among those with baseline incident LARC, both over 4-year time periods.
RESULTS:
Among 151,786 patients with 513,753 contraceptive encounters, 22.1% switched to another method at least once over the 4-year observation period, and switching patterns were varied. In patients with baseline LARC, the adjusted predicted probability of switching was 19.0% (95% CI 18.0–20.0%) compared with patients with baseline moderately effective methods (16.2%, 95% CI 15.1–17.3%). The adjusted predicted probability of switching was highest among the youngest group (28.6%, 95% CI 25.8–31.6% in patients aged 12–14 years) and decreased in a dose–response relationship by age to 8.4% (95% CI 7.4–9.4%) among patients aged 45–49 years. Latina and Black race and ethnicity, public or no insurance, and baseline Title X clinic status were all associated with higher odds of switching at least once. Among baseline LARC users, 19.4% had a removal (to switch or discontinue) within 1 year and 30.1% within 4 years; 97.6% of clinics that provided LARC also had evidence of a removal.
CONCLUSION:
Community health centers provide access to method switching and LARC removal. Contraceptive switching and LARC removal are common, and clinicians should normalize switching and LARC removal among patients.
Equitable access to contraception includes the ability to remove, discontinue, or switch methods without barriers.1,2 People may discontinue or switch methods because of method dissatisfaction, a preference for another method or for no method, desired pregnancy, or other reasons, including inconvenience of use, access, and availability.3–6 Despite recent increases in long-acting reversible contraception (LARC) use, barriers persist to accessing LARC removal services (eg, inadequate insurance coverage, cost, clinic policy, or clinician bias), which usually require a clinic visit.7–10 Research on contraceptive switching and discontinuation (usually defined as stopping a method without evidence of another method within 30 days) is generally limited to 6 or 12 months after initiation4,11–14 or is conducted among samples with no-cost initiation and removal as part of a study protocol, as opposed to real-world settings.4,13,14 We have limited evidence about method switching, specifically LARC removal, over longer periods and among large diverse settings.7,9,15,16
Community health centers, which include Federally Qualified Health Centers and Federally Qualified Health Center look-alikes,17 are an important access point for contraceptive services for people with low incomes18,19 regardless of insurance status or ability to pay.18,20 Furthermore, some community health centers participate in the federal Title X program, which provides greater access to the most effective reversible methods than community health centers without Title X funding.20 However, less is known about real-world patterns of method switching and access to LARC removal in the population served by community health centers; this study fills this gap with a large, diverse sample of patients seeking contraceptive services in community health centers. The purpose of this study is to describe patterns of method switching and LARC removal among patients in a large network of community health centers over 4-year periods. We further identify individual- and clinic-level factors associated with switching and LARC removal.
METHODS
We used individual-level electronic health record (EHR) data to conduct a historical cohort study using the ADVANCE (Accelerating Data Value Across a National Community Health Center Network) clinical research network. ADVANCE, a member of Patient-Centered Outcomes Research Network, is a multicenter collaborative lead by OCHIN that includes outpatient EHR data integrated and standardized into a common data model.21 ADVANCE data include information from more than 8 million patients across 32 states and are demographically similar to the national profile of patients in community health centers.22 Appendix 1, available online at http://links.lww.com/AOG/D252, provides details on ADVANCE data partners. ADVANCE EHRs have been validated in numerous studies.23–25 This study was reviewed and approved by the Western IRB.
We included clinics that were continuously open between January 1, 2016, and December 31, 2021. We first identified female patients aged 12–49 years with any ambulatory health care use in the calendar years 2016, 2017, or 2018 (Fig. 1). We included individuals coded as female in their EHRs; we were unable to comprehensively assess gender identity, and we recognize that individuals who do not identify as female seek contraceptive care, including transgender men and nonbinary individuals. We excluded 29,334 patients with infecundity (female infertility, natural menopause, hysterectomy, or oophorectomy) and 19,629 with previous sterilization (Fig. 1). We created three cohorts of patients with one or more contraceptive encounters (long-acting method prescription or placement, short-acting method prescription) in 2016, 2017, or 2018. Each cohort was followed up for a 4-year study period (2016–2019, 2017–2020, or 2018–2021); having three baseline periods allowed us to include more patients in our study. Cohorts were mutually exclusive and pooled for all analyses. We next refined the analytic sample to patients who had seven or fewer contraceptive method switching events observed during their 4-year study period (372 excluded because of more than seven switching events). The final analytic sample included 151,786 patients with 513,753 contraceptive encounters from 489 clinics in 20 states (Appendix 1, http://links.lww.com/AOG/D252, includes a list of states).
Fig. 1. Sample flow diagram. U.S. community health centers, 2016–2021.
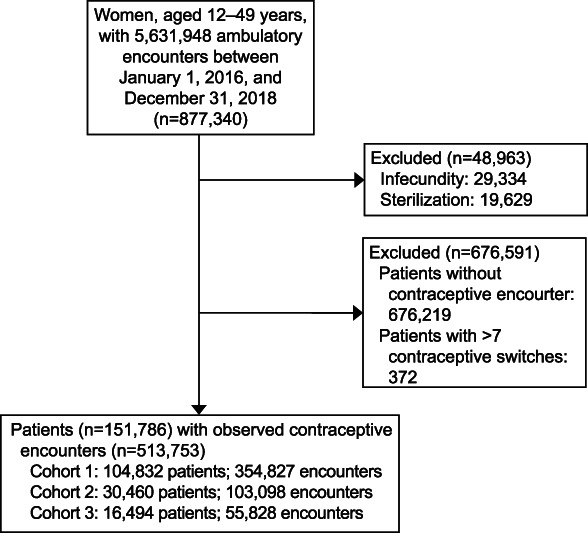
Darney. Method Switching and LARC Removal in the Safety Net. Obstet Gynecol 2023.
Our outcomes were any observed contraceptive method switching and LARC removal among those with incident (newly placed at baseline) LARC. We defined contraceptive switching as any observed change in contraceptive method type (eg, pill to patch, intrauterine device [IUD] to pill) during the study time period. Any observed change in a patient's contraceptive method type was categorized as a switching event. A change within a method type (eg, change in formulation of oral contraceptive) was not counted as a switch event. We are not able to assess barrier methods or spermicide because they are not well captured in our data. We also categorized methods as most (LARC) or moderately (short-acting hormonal) effective.26 We defined LARC removal as any observed LARC removal during the study time period for patients with incident LARC; removal thus includes switching to another method, having LARC replacements, and discontinuing. Removal of LARC was assessed with International Classification of Diseases, Tenth Revision code Z30.432 (encounter for removal of intrauterine contraceptive device) or Current Procedural Terminology code 11982 (removal, nonbiodegradable drug delivery implant) or 58301 (encounter for removal of intrauterine device). Removals of LARC were restricted to those that occurred temporally after the initial LARC method.
We assessed patient demographic characteristics at the first contraceptive visit, following our previous work.18 We included age (12–14 years at first study visit, 15–17 years, 18–19 years, then 5-year age bands to 49 years) and race and ethnicity because people of color experience poorer access to and quality of contraceptive care than White people (Latina, non-Latina White, non-Latina Black, non-Latina other [including Asian, American Indian/Alaska Native], non-Latina missing race, additional details on race and ethnicity are given in Appendix 1, http://links.lww.com/AOG/D252). We included patient income as a proportion of the federal poverty level category (less than 100% of the federal poverty level, 101–150%, 151–200%, 200% or higher, missing income), payer or insurance (private, public, or uninsured; additional details on insurance in Appendix 1, http://links.lww.com/AOG/D252), and health care professional (women's health specialist or not). If missing data were encountered, we then used the next most recent contraceptive visit with known data. Data were not missing at random for missing patient race and ethnicity (4.7%) (Appendix 2, available online at http://links.lww.com/AOG/D252); we therefore chose to include missingness as its own level in categorical variables and did not perform multiple imputation.
We identified clinic Title X funding status, which is known to be associated with LARC provision.20 We classified clinics as rural using 2010 Rural-Urban Commuting Area codes; small towns and lower were categorized as rural.27 We also included state-level indicators: presence of a state family planning program (1115 or state plan amendment/family planning waiver) status,28 and Medicaid expansion status (as of January 1, 2016).29
We first described our sample characteristics by whether a patient had switched methods during the time period, stratified by method type used at baseline (most or moderately effective). Next, we described the proportion of the sample with at least one method switch by baseline method (most or moderately effective). Then we described observed LARC removal at the clinic level and then at the patient level, by type of LARC (IUD or implant), over the 4-year observation period and within 1 year. Next, to capture the combinations of contraceptive use patterns among those with at least one switching event, we visually described detailed patterns of method switching (ie, initial method, next method switched to, and any subsequent method switching within the study period) and calculated time to switching. We restricted this analysis to the first three switches among the 22.1% of the sample who switched at least once. Finally, we developed two multilevel generalized estimating equation logistic regression models with an exchangeable working correlation structure for our dichotomous outcomes: any switching (among the full sample of baseline contraceptive users) and LARC removal (among those with baseline LARC). For the multilevel models, patients are nested within clinics; thus, we included a random intercept for the clinic in both models. We controlled for patient-, clinic-, and state-level factors as fixed effects as described above. We included a random effect for clinic in both models. For regressions, we collapsed the income levels attributable to sample size as follows: 150% of the federal poverty level or less, 151% or greater, and missing. We calculated predicted probabilities to improve the interpretability of our results.30 We conducted a sensitivity analysis of our switching outcome stratified by baseline method type (most or moderately effective) to qualitatively evaluate any differences in covariate patterns. We conducted all analyses in SAS 8.3; we prepared figures in PowerPoint or R 4.1.0 using the ggsankey package.
RESULTS
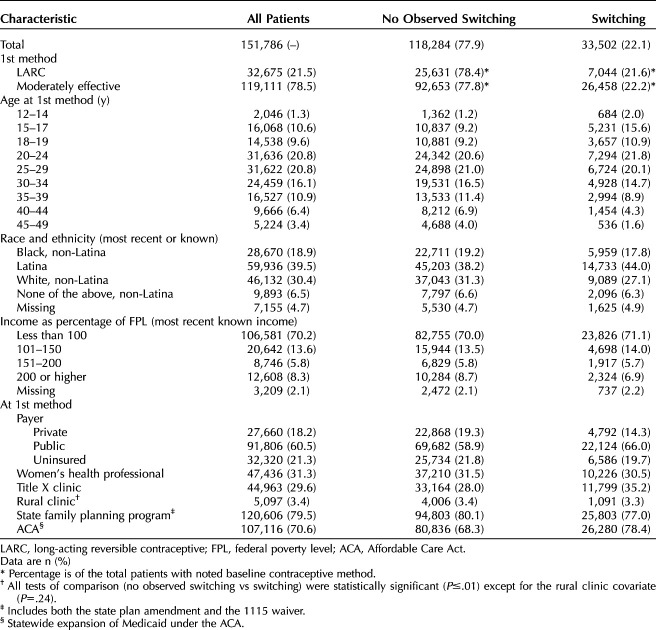
Overall, 22.1% (33,502/151,786) of patients in our sample of contraceptive users had at least one contraceptive method switching event (Table 1). Compared with patients who had no observed switching, a larger proportion of patients who switched were aged 15–17 years (15.6% of those who switched vs 9.2% of those with no observed switching). Similarly, a larger proportion of patients were Latina (44.0% among those who switched vs 38.2% of those with no observed switching), had public insurance (66.0% vs 58.9% of those with no observed switching), visited a Title X clinic (35.2% vs 28.0% of those with no observed switching), or were in a Medicaid expansion state at their first contraceptive visit (78.4% vs 68.3% of those with no observed switching). A smaller proportion of patients with evidence of contraceptive switching had private insurance (14.3% vs 19.3% of those with no observed switching).
Table 1.
Patient-Level Demographics of 151,786 Patients With Contraceptive Use at Baseline in U.S. Community Health Centers, 2016–2021
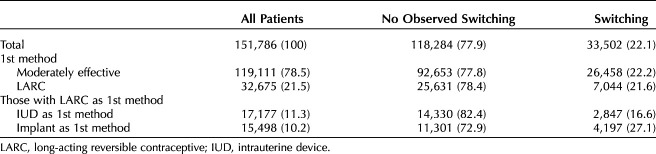
Among patients with a most effective method at baseline (LARC; IUD or implant), 21.6% were observed to switch at least once compared with 22.2% of patients with moderately effective contraception at baseline (Table 2). Fewer than one-fifth (16.6%) of baseline IUD users switched methods over the 4-year study period compared with more than one-quarter (27.1%) of patients with implants at baseline.
Table 2.
Contraceptive Method Switching Over a 4-Year Period by Baseline Method Type (Long-Acting Reversible Contraception or Moderately Effective), U.S. Community Health Centers, 2016-2021
At the clinic level, of the 339 clinics with LARC placement, 97.6% (331) had evidence of providing LARC removal services during the full study time period (data not shown). At the individual level, 30.1% of those with LARC at baseline had evidence of removal (This is larger than the proportion with evidence of switching because it also includes discontinuation and replacement; Fig. 2). Over the study period, IUD removals as a proportion of all IUDs at baseline were more frequent than implant removals (35.8% IUD, 23.7% implant; 30.1% all LARC combined). The pattern was similar for removal within 1 year (26.3% IUD, 11.7% implant; 19.4% all LARC combined; Fig. 2).
Fig. 2. Long-acting reversible contraception (LARC) removal overall and by LARC method in a 4-year observation period and within 1 year; U.S. community health centers, 2016–2021. IUD, intrauterine device.
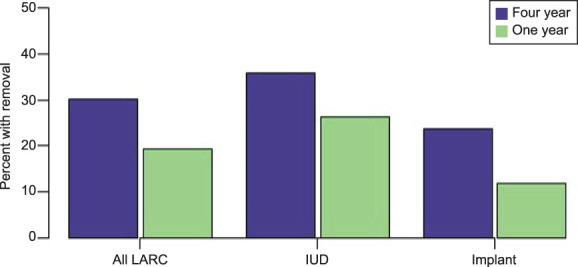
Darney. Method Switching and LARC Removal in the Safety Net. Obstet Gynecol 2023.
We next visually described the pattern of contraceptive method switching among the 22.1% of patients (n=33,502) with at least one method switch during the 4-year follow-up period (Fig. 3). Nearly three-quarters of patients who switched had only one switch (71.8%, n=24,055); 21.1% (n=7,069) had two switches; and 7.1% (n=2,378) had three switches. We observed a dynamic pattern of contraceptive method switching. Of patients with LARC as their first contraceptive method and a contraceptive switching event (n=7,044), 2.7% (n=189) received sterilization, 12.7% (n=894) switched to a different LARC method, and 84.6% (n=5,961) chose a moderately effective method. Of patients who switched from another method to LARC in the first switching event (n=11,866), 33.8% (4,315 patients) switched from injectable, 51.4% (6,565 patients) from the pill, 4.6% (593 patients) from patch, and 3.2% (413 patients) from the ring. A minority of patients switched from a reversible method at baseline to sterilization. The median number of months to the first switch among those using LARC at baseline was 11 (interquartile range 4–23); median months to the first switch among those using moderately effective methods at baseline was 13 (interquartile range 4–20; data not shown).
Fig. 3. Contraceptive switching patterns among patients with at least one observed contraceptive method switch at U.S. community health centers, 2016–2021 (n=33,502). IUD, intrauterine device.
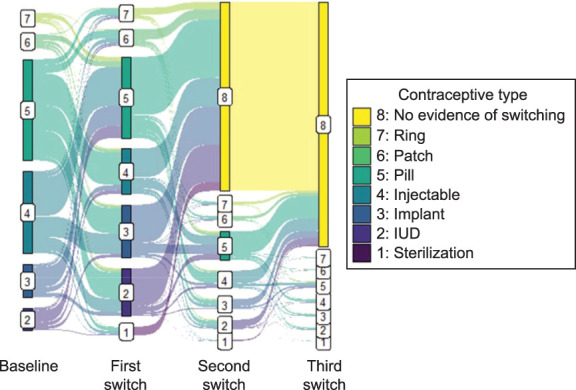
Darney. Method Switching and LARC Removal in the Safety Net. Obstet Gynecol 2023.
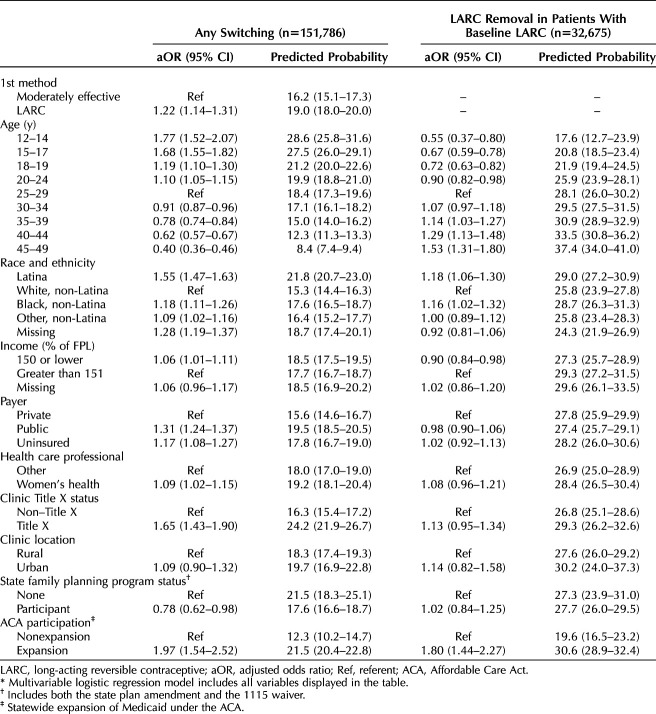
In multivariable analyses of factors related to any method switching compared with not switching over the 4-year observation period, baseline LARC; younger age; Latina, Black, and other ethnicity; public or no insurance; and baseline Title X clinic status (Table 3) were associated with switching. Among patients with baseline LARC, the adjusted predicted probability of switching was 19.0% (95% CI 18.0–20.0%); for patients without baseline LARC, the adjusted predicted probability of switching was 16.2% (95% CI 15.1–17.3%). The adjusted predicted probability of switching was highest among the youngest group: 28.6% (95% CI 25.8–31.6%) in patients aged 12–14 years. The adjusted probability of switching was lower with increasing age, with the lowest probability (8.4%, 95% CI 7.4–9.4%) among patients aged 45–49 years. Latina patients had the greatest adjusted predicted probability of switching at 21.8% (95% CI 20.7–23.0%), and White non-Latina patients had the lowest (15.3%, 95% CI 14.4–16.3%). Patients with incomes 150% of the federal poverty level or less had a greater adjusted probability of switching at 18.5% (95% CI 17.5–19.5%) compared with patients with incomes greater than 151% of the federal poverty level. In sensitivity analyses stratified by moderately or most effective baseline method (instead of including baseline method as a covariate), we observed qualitatively similar covariate patterns (Appendix 3, available online at http://links.lww.com/AOG/D252).
Table 3.
Multivariable Models* Examining Any Method Switching or Long-Acting Reversible Contraception Removal in Patients With Baseline Long-Acting Reversible Contraception Over a 4-Year Period, U.S. Community Health Centers, 2016–2021
In the subset of patients with baseline LARC (21.5% of sample, n=32,675), there was a dose-response relationship between age and LARC removal, with the youngest patients having the lowest adjusted probability (12–14 years 17.6%, 95% CI 12.7–23.9%) and the oldest patients having the highest adjusted probability (37.4%, 95% CI 34.0–41.0%) of LARC removal (Table 3). Latina and Black race and ethnicity were also associated with greater adjusted predicted probability of removal (29.0%, 95% CI 27.2–30.9%; 28.7%, 95% CI 26.3–31.3%, respectively). Receiving care at a clinic in a Medicaid expansion state under the Affordable Care Act was associated with an increased predicted probability of removal (30.6%, 95% CI 28.9–32.4%) compared with receiving care in no-expansion states.
DISCUSSION
We show, in a large and diverse sample receiving contraceptive services at community health centers across the United States, that 22% switched to another method at some point over a 4-year observation period. Implant users were more likely to switch than IUD users or users of moderately effective methods, and switching patterns were varied. In patients with baseline LARC, the adjusted probability of switching was 19.0% compared with 16.2% among patients with baseline moderately effective methods. The adjusted probability of switching was highest among the youngest group and decreased with age. We also found that 19.4% of baseline LARC users removed their IUD or implant within 1 year and 30.1% did so within 4 years. Among clinics that provided LARC services, 97.6% had evidence of offering removal services, that is, providing at least one removal.
Our large, diverse, real-world sample of patients served by community health centers builds on prior studies. Similar findings were seen in a sample that received no-cost contraception and reported that 12.4% switched methods at 6 months.4 In a Texas postpartum sample, the discontinuation rate among patients who used short-acting hormonal contraception during the postpartum period ranged from 30% at 3 months to 80% at 18 months.31 Another study showed that 12-month discontinuation rates were 19% among patients aged 14–19 years using no-cost LARC methods.13 Consistent with some prior research,14 our study showed that implant users were more likely to switch than IUD users (27.1% vs 16.6%, respectively). Implant users are known to be, on average, younger than IUD users,18 and this likely helps explain the higher adjusted probability of switching among LARC users, specifically implant users, compared with users of moderately effective methods in our sample.
Unlike prior research that found no difference in contraceptive switching by age,4 we found that age was inversely associated with switching (adjusted probability of switching was higher among younger ages) but positively associated with LARC removal (adjusted probability of removal was higher among older ages). It is possible that because side effects are one of the most common reasons for method switching,4,31 younger people have had less time to find a method that they are satisfied with, whereas older patients may be discontinuing LARC and not starting a new method because they are more likely to desire pregnancy32 or sterilization33 than younger patients. Data suggest that contraceptive switching is expected among young people, and clinicians should normalize and support switching among their young patients in particular.
Differences in switching and discontinuation by race and ethnicity are important to identify because of the role of structural and interpersonal racism. People of color are more likely to feel pressure from clinicians to use specific methods,16,34 and pressure is associated with greater contraceptive discontinuation.35 In the current study, Latina and Black patients were more likely to switch methods and discontinue LARC than White patients. Previous work suggests that people of Latina and other ethnicities are more likely to discontinue but not switch a method than are White people,4 whereas another population-based study found similar rates of satisfaction and continuation of LARC by race or ethnicity but lower rates of satisfaction and continuation of short-acting hormonal methods among Black and Latina patients than White patients.36 Our data do not allow us to assess reasons for switching or removal, and most studies that assess reasons for removal or switching do not assess differences by race or ethnicity. Given that individuals of color, including immigrants, have reported poor-quality care, including non–patient-centered contraceptive counseling, clinician bias, and dismissiveness,35,37,38 and more access barriers,38–40 future research should identify reasons for contraceptive switching and discontinuation and the role of barriers, including racism and clinician bias, to quality care.
Strengths of our study include a large and diverse sample of community health center patients, objective real-world clinical data, ability to include people who are uninsured and missing from research relying on claims data, and ability to observe switching and removal over a 4-year period. We focus on switching patterns and LARC removal to center access to both changing methods when desired and removing IUDs and implants, which involve interaction with the health care system (There is emerging literature on IUD self-removal,41,42 but LARC methods still largely require clinician involvement to both initiate and remove). Our results are not without limitations. Most important, reasons for switching or LARC removal are outside the scope of this study, and we do not know whether there are patients in the sample who were unable to switch methods or remove their LARC when desired. Second, we may have missed some removals if patients had their LARCs removed outside of the community health centers included in this study (eg, had it inserted at a study clinic but removed at a clinic not included in our study). Third, we have assessed removal, not discontinuation; thus, our results are not always easy to compare with literature that focuses on discontinuation. We felt that access to removal was an important outcome and wanted to avoid framing discontinuation as a negative outcome. Fourth, our study period includes the COVID-19 pandemic, which disrupted primary care services, including contraception, and may have affected access to switching or LARC removal. Fifth, we were unable to assess use of barrier methods and other methods that do not require interaction with a primary care physician; condom use, for example, may be an important part of switching dynamics and is not captured in our data. Finally, generalizability is limited outside community health centers in the sample, but this is a large sample, and community health centers have the advantage of high continuity of care.
This study adds to a body of evidence about the important role that community health centers play in providing access to contraceptive services,18–20 including switching methods and LARC removal, in the United States. Contraceptive switching and LARC removal are common, and clinicians should normalize switching and LARC removal among patients.
Footnotes
Financial Disclosure Blair G. Darney's institution receives research support from Merck/Organon. Dr. Darney serves on the Board of Directors of the Society of Family Planning. Kate Coleman-Minahan was a consultant for The Lawyering Project. The other authors did not report any potential conflicts of interest.
Presented at the Population Association of America’s Annual Meeting, April 12–15, 2023, New Orleans, Louisiana.
This study was supported by a Merck/Organon investigator-initiated grant (IIS No. 60206), Dr. Darney, principal investigator. The funder had no role in the conception, analysis, or interpretation of data. Partial support from the Office of Population Affairs (1 FPRPA006071-01-00; Dr. Darney, principal investigator) and the Agency for Healthcare Research and Quality (AHRQ) (1R01HS025155-01; Dr. Cottrell, principal investigator).
This work was conducted with the ADVANCE (Accelerating Data Value Across a National Community Health Center Network) CRN (Clinical Research Network). ADVANCE is a CRN in PCORnet®, the National Patient Centered Outcomes Research Network. ADVANCE is led by OCHIN in partnership with Health Choice Network, Fenway Health, and Oregon Health & Science University. ADVANCE's participation in PCORnet® is funded through the Patient-Centered Outcomes Research Institute, contract RI-OCHIN-01-MC.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/D253.
Figure.
No available caption
REFERENCES
- 1.World Health Organization. Ensuring human rights in the provision of contraceptive information and services: guidance and recommendations. Accessed March 23, 2022. https://apps.who.int/iris/bitstream/handle/10665/102539/9789241506748_eng.pdf [PubMed]
- 2.Coalition to Expand Contraceptive Access. Priority roadmap for policy-ready contraceptive research. Accessed March 23, 2022. https://www.contraceptionaccess.org/roadmap
- 3.Population Council. Contraceptive discontinuation: reasons, challenges, and solutions. Accessed March 23, 2022. https://popdesenvolvimento.org/images/imprensa/FP2020_ContraceptiveDiscontinuation_SinglePageRevise_12.16.15.pdf
- 4.Simmons RG, Sanders JN, Geist C, Gawron L, Myers K, Turok DK. Predictors of contraceptive switching and discontinuation within the first 6 months of use among Highly Effective Reversible Contraceptive Initiative Salt Lake study participants. Am J Obstet Gynecol 2019;220:376.e1–12. doi: 10.1016/j.ajog.2018.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grady WR, Billy JO, Klepinger DH. Contraceptive method switching in the United States. Perspect Sex Reprod Health 2002;34:135–45. doi: 10.2307/3097712 [DOI] [PubMed] [Google Scholar]
- 6.Ali MM, Cleland JG, Shah IH, World Health Organization. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. 2012. Accessed April 21, 2023. https://apps.who.int/iris/handle/10665/75429
- 7.Strasser J, Borkowski L, Couillard M, Allina A, Wood SF. Access to removal of long-acting reversible contraceptive methods is an essential component of high-quality contraceptive care. Womens Health Issues 2017;27:253–5. doi: 10.1016/j.whi.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 8.Jacinto A, Ronda AV, Lee C, Fikree FF, Ramirez-Ferrero E. Introducing long-acting contraceptive removal indicators in a pilot study in Mozambique: dynamics of discontinuation and implications for quality of care. Glob Health Sci Pract 2022;10:e2100252. doi: 10.9745/GHSP-D-21-00252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amico JR, Heintz C, Bennett AH, Gold M. Access to IUD removal: data from a mystery-caller study. Contraception 2020;101:122–9. doi: 10.1016/j.contraception.2019.10.008 [DOI] [PubMed] [Google Scholar]
- 10.Ela EJ, Broussard K, Hansen K, Burke KL, Thaxton L, Potter JE. Satisfaction, resignation, and dissatisfaction with long-acting reversible contraception among low-income postpartum Texans. Womens Health Issues 2022;32:334–42. doi: 10.1016/j.whi.2022.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol 2013;122:1214–21. doi: 10.1097/01.AOG.0000435452.86108.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sznajder KK, Tomaszewski KS, Burke AE, Trent M. Incidence of discontinuation of long-acting reversible contraception among adolescent and young adult women served by an urban primary care clinic. J Pediatr Adolesc Gynecol 2017;30:53–7. doi: 10.1016/j.jpag.2016.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol 2012;120:1298–305. doi: 10.1097/aog.0b013e31827499bd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, Secura G. Continuation and satisfaction of reversible contraception. Obstet Gynecol 2011;117:1105–13. doi: 10.1097/aog.0b013e31821188ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christofield M, Lacoste M. Accessible contraceptive implant removal services: an essential element of quality service delivery and scale-up. Glob Health Sci Pract 2016;4:366–72. doi: 10.9745/GHSP-D-16-00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JA, Kramer RD, Ryder KM. Provider bias in long-acting reversible contraception (LARC) promotion and removal: perceptions of young adult women. Am J Public Health 2016;106:1932–7. doi: 10.2105/AJPH.2016.303393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Health Services Research Administration. Health center program look-alikes. Accessed April 23, 2023. https://bphc.hrsa.gov/funding/funding-opportunities/health-center-program-look-alikes#what
- 18.Darney BG, Biel FM, Oakley J, Rodriguez MI, Cottrell EK. US “safety net” clinics provide access to effective contraception for adolescents and young women, 2017–2019. Am J Public Health 2022;112:S555–62. doi: 10.2105/AJPH.2022.306913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darney BG, Jacob RL, Hoopes M, Rodriguez MI, Hatch B, Marino M, et al. Evaluation of Medicaid expansion under the Affordable Care Act and contraceptive care in US community health centers. JAMA Netw Open 2020;3:e206874. doi: 10.1001/jamanetworkopen.2020.6874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Darney BG, Biel FM, Hoopes M, Rodriguez MI, Hatch B, Marino M, et al. Title X improved access to most effective and moderately effective contraception in US safety-net clinics, 2016–18. Health Aff (Millwood) 2022;41:497–506. doi: 10.1377/hlthaff.2021.01483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeVoe JE, Gold R, Cottrell E, Bauer V, Brickman A, Puro J, et al. The ADVANCE network: accelerating data value across a national community health center network. J Am Med Inform Assoc 2014;21:591–5. doi: 10.1136/amiajnl-2014-002744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Association of Community Health Centers. Community health center chartbook. Accessed August 5, 2021. https://nachc.org/wp-content/uploads/2021/04/Chartbook-Final-2021.pdf
- 23.Heintzman J, Marino M, Hoopes M, Bailey S, Gold R, Crawford C, et al. Using electronic health record data to evaluate preventive service utilization among uninsured safety net patients. Prev Med 2014;67:306–10. doi: 10.1016/j.ypmed.2014.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heintzman J, Marino M, Hoopes M, Bailey SR, Gold R, O'Malley J, et al. Supporting health insurance expansion: do electronic health records have valid insurance verification and enrollment data? J Am Med Inform Assoc 2015;22:909–13. doi: 10.1093/jamia/ocv033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Angier H, Gold R, Gallia C, Casciato A, Tillotson CJ, Marino M, et al. Variation in outcomes of quality measurement by data source. Pediatrics 2014;133:e1676–82. doi: 10.1542/peds.2013-4277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.HHS Office of Population Affairs. Measure CCW: contraceptive care–all women ages 15-44. Accessed March 2, 2022. https://opa.hhs.gov/sites/default/files/2020-12/2019-measure-specifications-ccw-for-opa-website.pdf
- 27.US Department of Agriculture, Economic Research Service. Rural-Urban Commuting Area codes. Accessed March 30, 2019. https://ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx
- 28.Guttmacher Institute. Medicaid family planning eligibility expansions. Accessed March 2, 2022. https://guttmacher.org/state-policy/explore/medicaid-family-planning-eligibility-expansions
- 29.Henry J. Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. Accessed October 3, 2018. https://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 30.King G, Tomz M, Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. Am J Polit Sci 2000;44:347–61. doi: 10.2307/2669316 [DOI] [Google Scholar]
- 31.Burke KL, Thaxton L, Potter JE. Short-acting hormonal contraceptive continuation among low-income postpartum women in Texas. Contracept X 2021;3:100052. doi: 10.1016/j.conx.2020.100052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rocca CH, Parra M, Muñoz I, Foster DG, Boscardin WJ, Ralph LJ. Comparison of pregnancy preferences preceding vs year 1 of the COVID-19 pandemic. JAMA Netw Open 2022;5:e2220093. doi: 10.1001/jamanetworkopen.2022.20093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kavanaugh ML, Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception 2018;97:14–21. doi: 10.1016/j.contraception.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dehlendorf C, Ruskin R, Grumbach K, Vittinghoff E, Bibbins-Domingo K, Schillinger D, et al. Recommendations for intrauterine contraception: a randomized trial of the effects of patients' race/ethnicity and socioeconomic status. Am J Obstet Gynecol 2010;203:319.e1–8. doi: 10.1016/j.ajog.2010.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalmuss D, Davidson AR, Cushman LF, Heartwell S, Rulin M. Determinants of early implant discontinuation among low-income women. Fam Plann Perspect 1996;28:256–60. Erratum in: Fam Plann Perspect 1997;29:60 [PubMed] [Google Scholar]
- 36.Littlejohn KE. Hormonal contraceptive use and discontinuation because of dissatisfaction: differences by race and education. Demography 2012;49:1433–52. doi: 10.1007/s13524-012-0127-7 [DOI] [PubMed] [Google Scholar]
- 37.Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol 2014;57:659–73. doi: 10.1097/GRF.0000000000000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson T-AM, Young Y-Y, Bass TM, Baker S, Njoku O, Norwood J, et al. Racism runs through it: examining the sexual and reproductive health experience of Black women in the South. Health Aff (Millwood) 2022;41:195–202. doi: 10.1377/hlthaff.2021.01422 [DOI] [PubMed] [Google Scholar]
- 39.Burke KL, Potter JE, White K. Unsatisfied contraceptive preferences due to cost among women in the United States. Contracept X 2020;2:100032. doi: 10.1016/j.conx.2020.100032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Potter JE, Coleman-Minahan K, White K, Powers DA, Dillaway C, Stevenson AJ, et al. Contraception after delivery among publicly insured women in Texas: use compared with preference. Obstet Gynecol 2017;130:393–402. doi: 10.1097/AOG.0000000000002136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Broussard K, Becker A. Self-removal of long-acting reversible contraception: a content analysis of YouTube videos. Contraception 2021;104:654–8. doi: 10.1016/j.contraception.2021.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amico JR, Stimmel S, Hudson S, Gold M. “$231 … to pull a string!!!” American IUD users' reasons for IUD self-removal: an analysis of internet forums. Contraception 2020;101:393–8. doi: 10.1016/j.contraception.2020.02.005 [DOI] [PubMed] [Google Scholar]