Abstract
Humeral shaft fracture is a common injury which can be treated either conservatively with functional bracing or with surgical fixation. Current evidence shows an increase in the rate of nonunion after conservative treatment, suggesting that indications for conservative treatment may need to be re-examined. This article updates trends in treatment for humeral shaft fracture. Indications for surgery, both for plate osteosynthesis with open reduction and internal fixation (ORIF) as well as for minimally invasive plate osteosynthesis (MIPO) and intramedullary nailing (IMN) are described. Recognition of the advantages and disadvantages of each technique can better define the role of the plate or nail and can aid in the selection of an appropriate surgical approach. ORIF with compression plate continues to have a role in the treatment of simple or AO/OTA type A fractures. The primary goal of minimal invasive osteosynthesis, a surgical technique involving small incisions, closed reduction or mini-open reduction that minimizes soft tissue dissection and helps preserve the periosteal blood supply, is to achieve bone union and the best possible functional outcomes. MIPO of the humerus is now well accepted as being less invasive and providing relative stability to allow indirect (secondary) bone healing with callus formation. MIPO approaches can be performed circumferentially to the humerus, including the proximal, middle and distal shaft. The classic MIPO approach is anterior MIPO, followed by posterior, anterolateral and anteromedial MIPO. IMN is also an option for treating humerus fractures. In the past, IMN was not widely used due to the potential for complications such as shoulder impingement and elbow problems as well as the limited availability of implants and the steep learning curve of this surgical technique. Over the past decade, the launch of a new design of straight antegrade and retrograde IMN with established techniques has encouraged more surgeons to use IMN as an alternative option. Methods of dealing with concomitant and post-treatment radial nerve palsy have also been evolving, including the use of ultrasound for diagnosis of radial nerve conditions. Radial nerves with contusion, entrapment or laceration can be detected using ultrasound with reliability comparable to intraoperative findings. Trends in treatment of radial nerve palsy are described below. Future larger randomized controlled trials comparing conservative and operative management are necessary to further develop appropriate guidelines.
Keywords: Humeral shaft, Fracture, Treatment, Conservative, ORIF, MIPO, Intramedullary nailing, Radial nerve injury, Ultrasound
1. Introduction
1.1. Conservative treatment revisited
The efficacy of conservative treatment for humeral shaft fractures had been known for a long time. Conservative treatment provides distinct advantages over surgery, e.g., less risk of both deep infection1 and of radial nerve palsy compared to surgery.2 A classic study by Sarmiento A in 1977 reported excellent treatment outcomes with bracing,3 however, those results have not been reproduced. The standard treatment of humeral shaft fracture is still being debated. Many recent trials have been conducted to compare the efficacy of functional bracing with internal fixation. For example, in 2020, Ramo L et al. conducted the FISH randomized clinical trial which showed that internal fixation did not significantly improve functional outcomes compared to functional bracing. Additionally, 25% of the functional bracing group had nonunion which needed to be convert to surgery.4 Serrano R et al. emphasized the risk of nonunion with conservative treatment including comminution, segmental and butterfly fractures. That study reported one-third of patients with a humeral shaft fracture who received conservative treatment need to receive surgical treatment due to nonunion, malalignment and/or inability to tolerate the bracing.5 In 2022, Den Hartog D et al. conducted the HUMMER multicenter cohort study comparing the functional and clinical outcomes of surgical and conservative treatment of humeral shaft fractures. That study found that operative fixation was superior to conservative treatment in terms of incidence of nonunion, functional outcomes and complications.6
The location of the fracture site and the characteristics of the injury are important factors in determining if fracture reduction can be maintained by bracing. Generally, if the fracture zone is between the superior border of the pectoralis major tendon insertion and not higher than 5 cm from the upper border of the olecranon fossa the injury is suitable for bracing.4 Isolated simple fractures are ideal for bracing. Current evidence suggests that obesity, large breasts, fracture proximal third of a diaphysis, a transverse or short oblique fracture, and increased fracture gap or no callus formation at the 6 weeks follow-up increase the risk of nonunion.7,8
Some degree of malunion of the humeral shaft fracture is acceptable because the shoulder function is compensated by the wide range of motion of the glenohumeral joint. Klenerman L et al. reported that acceptable deformity of the humerus includes anterior angulation <20°, varus or valgus <30°, and shortening <2–3 cm.9 A common deformity following conservative treatment is varus and anterior apex angulation (Fig. 1). A list of indications and contraindications related to the risk of nonunion are provided in Table 1.
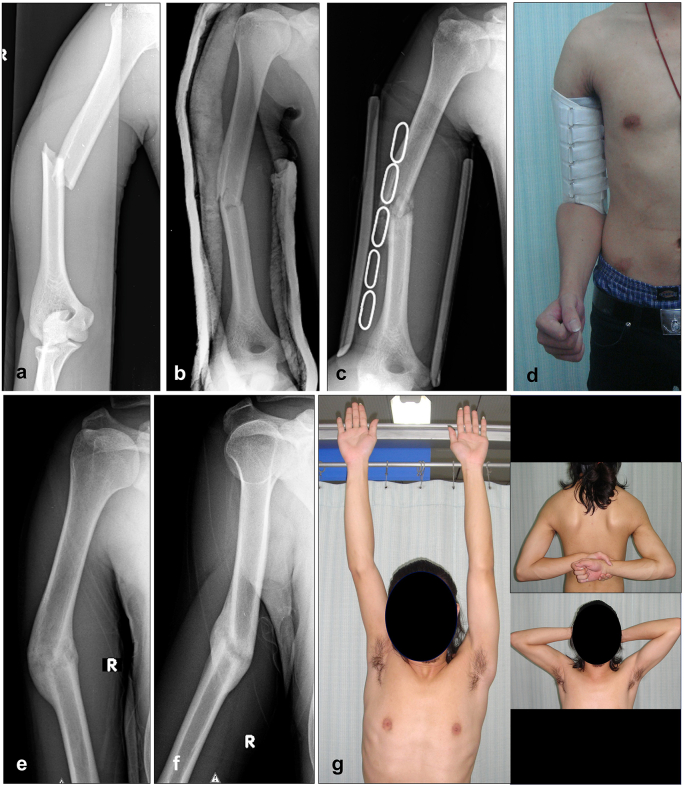
Fig. 1.
X-ray showing an oblique fracture of the midshaft humerus (a), X-ray after closed reduction with U slab (b), X-ray after change to functional brace (c), Humerus functional brace with adjustable strap (d), AP X-ray at 6 months showing complete healing with varus angulation (e), Lateral X-ray showing anterior angulation (f), Normal final functional outcome (g).
Table 1.
Indications for conservative treatment of humeral shaft fracture.
| Indication | Contraindications | |
|---|---|---|
| Patient factors | Young female adult (cosmetic) | Obesity |
| Large breasts | ||
| Associated injury | – | Open fracture |
| Multiple trauma | ||
| Floating elbow | ||
| Vascular injury | ||
| Fracture site | Mid shaft | Proximal shaft |
| Fracture characteristic | Long oblique, spiral, spiral wedge | Comminuted |
| Segmental | ||
| Butterfly | ||
| Follow-up | Acceptable alignment at 6 weeks | Unacceptable alignment at 6 weeks |
Note: Acceptable alignment is anterior angulation <20°, varus or valgus <30°, shortening <2–3 cm.
Various different techniques have been used for conservative treatment, e.g., Velpeau® bandage, U-slab, hanging cast and functional brace. However, only the Sarmiento functional brace is still popular at present. Proposed treatment protocol for conservative treatment is described in Table 2.
Table 2.
Conservative treatment protocol.
| Timepoint | Immobilization technique | Follow-up plain radiography | Physical therapy |
|---|---|---|---|
| Initial | Coaptation slab 90° elbow flexion and arm sling | May need to evaluate the reduction and position of the slab |
|
| 1–2 weeks | Functional bracing and arm sling Continuously adjust the fitness of brace |
X-ray immediately after bracing |
|
| 6 weeks |
|
|
Abbreviations: F/E; flexion/extension.
Rehabilitation protocol for conservative treatment
The patient is immobilized in the U slab with arm sling for 7–10 days and change to functional brace. The patient is allowed to actively motion of the elbow in flexion and extension, passive shoulder forward flexion and extension in the arm sling for 4–6 weeks depending on the clinical healing and palpable callus. Then the arm sling is removed and active motion of the shoulder is started. The functional brace can be removed at 10–12 weeks.
1.2. Operative treatment
Indications for operative treatment include segmental fracture, vascular injury, radial nerve injury after closed reduction, open fracture, floating elbow, polytrauma, and failed conservative treatment. At present, the best fixation technique for humeral shaft fixation remains inconclusive. Open Reduction and Internal Fixation (ORIF) is a traditional technique which provides good treatment outcomes in simple fractures. Minimally Invasive Plate Osteosynthesis (MIPO) was introduced to minimize soft tissue dissection, thus helping to preserve the vascular supply at the fracture. MIPO may also lower the risk for nonunion and reintervention.10 Zhao JG et al. conducted a network meta-analysis of randomized controlled trials comparing results and complications with Intramedullary Nailing (IMN), ORIF and MIPO. That study found that IMN had resulted in greater shoulder impingement than either ORIF or MIPO. Iatrogenic radial nerve injury occurred more frequently with ORIF than with MIPO. The incidence of delayed union, nonunion and infection was not statistically clinically significantly different among the three methods.11 Patino AM et al. reported that plating results in better shoulder range of motion and Constant score compared to antegrade intramedullary nailing.12
The concept for treatment of humeral shaft fracture still follows the interfragmentary strain theory. Rellan I et al. compared 35 cases of simple humeral shaft fracture which were treated with absolute stability to 35 cases treated with relative stability. The results showed that achieving absolute stability in a simple humeral shaft fracture can reduce the healing time.13 They suggest that simple fractures (AO/OTA type A) should be treated with absolute stability. Relative stability should be reserved for multifragmentary fractures. MIPO of the humeral shaft is well-accepted due to less soft tissue dissection and less risk of iatrogenic radial nerve injury.11 However, MIPO is more technically demanding, particularly in the reduction of a displaced simple fracture. The indications that MIPO is necessary need to be clarified. In a simple fracture, ORIF with the classic compression plate is still a useful technique which provides absolute stability through direct bone healing. Another option is a bridging plate which can provide relative stability. Since closed reduction of simple fractures is difficult, the application of an external fixator on the lateral aspect by inserting the Schanz pin at the humeral head and lateral condyle of the distal humerus can be used to assist in creating and maintaining reduction.14 Segmental fractures are considered as double simple fractures. Reduction of a segmental fracture without opening the fracture site is technically demanding. One alternative is mini-open reduction at the fracture site with meticulous soft tissue dissection to assist fracture reduction.
The classic MIPO shaft of the humerus using the anterior approach was first described almost two decades ago.15 This technique is suitable for fixing a fracture that extends from 5 cm distal to the bicipital groove to 5 cm proximal to the coronoid fossa. Each fragment should be fixed with at least 3 screws (Fig. 2). However, in distal humeral shaft fractures, the number of screws which can purchase in cortical bone is limited. For that reason, various techniques of MIPO have been developed which are specific to the location of the fracture, the associated radial nerve injury and implant availability. Variations of MIPO include anterior reverse PHILOS,16 anteromedial,17, 18, 19 anterolateral20,21 and posterior approaches.22,23 Jitprapaikulsarn S et al. described a MIPO with anterior approach for the distal shaft humerus using a reverse PHILOS plate in comminuted fractures when the length of the distal fragment is greater than 3 cm above the coronoid fossa. The plate position must be checked in the lateral view during surgery to confirm that the plate does not obstruct the coronoid process during elbow flexion.16 (Fig. 3). Buranaphatthana T et al. proposed a MIPO with an anteromedial approach beneath the brachialis muscle tunnel using a 4.5 mm precontoured narrow locking compression plate (LCP) and placing it over the medial epicondyle. The distal fragment can be fixed with at least 2 or 3 medio-lateral long screws to gain adequate stability. This technique is indicated for fractures with anterior or lateral soft tissue problems. The incision scar is hidden on the medial side of the elbow.17 (Fig. 4). The anterolateral MIPO can be used with a distal shaft fracture. The plate must be contoured in 2 planes to match the anterolateral surface at the distal part and the radial nerve has to be identified (Fig. 5). The posterior approach is recommended for very distal shaft fractures where the length of the distal shaft fragment is less than 2 cm above the coronoid fossa. A 3.5 mm extraarticular distal humeral plate (EADHP) can be used by placing it on the lateral column of the distal humerus (Fig. 6). Jitprapaikulsarn S et al. performed a study of MIPO using the posterior approach and the EADHP. The authors demonstrated that the distal fragment had adequate length of cortical shaft for locking screw purchase at up to 5–6 cortices. The radial nerve must be identified at the proximal incision between the lateral head and the long head of the triceps. The elbow must be in extension during plate insertion in order to reduce the tension on the radial nerve. Clinical results were good to excellent in the series and technical tips and tricks were also described.23 Available MIPO techniques for humeral shaft fractures are shown in Table 3.
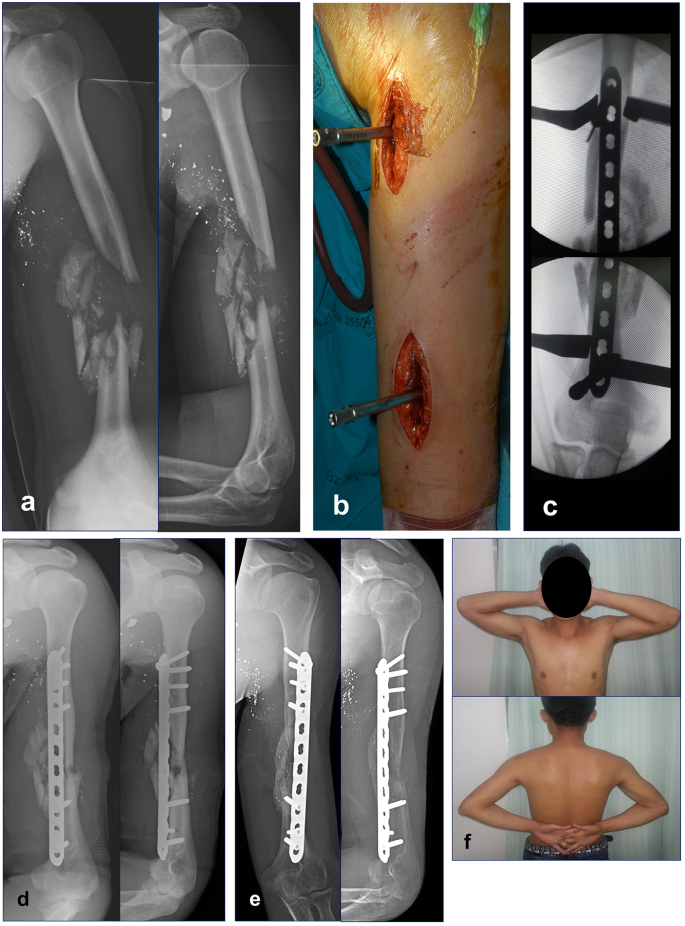
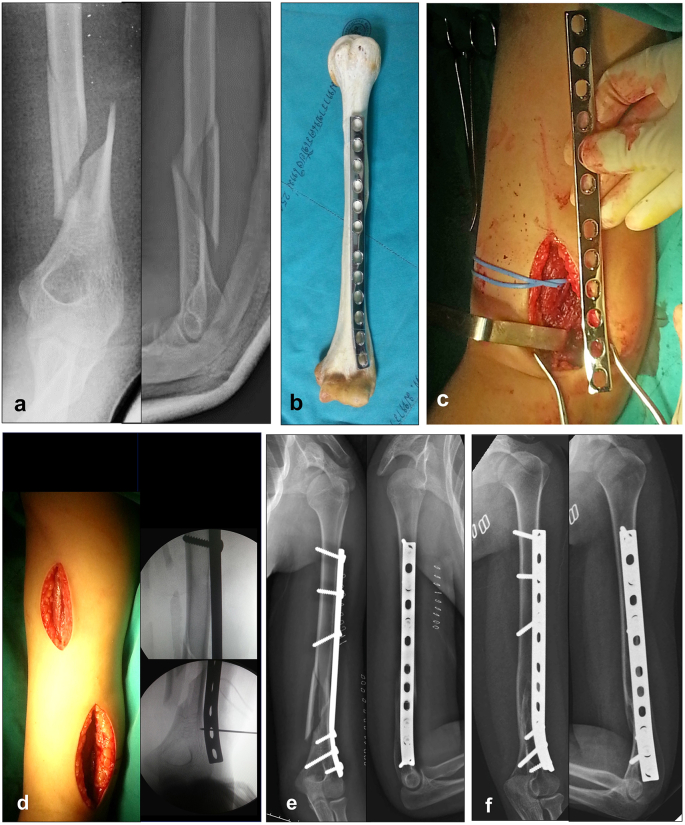
Fig. 2.
AP and lateral X-rays of the humerus showing comminuted fracture of the midshaft of the humerus from a gunshot injury (a), Proximal and distal incisions with drill sleeves controlling the alignment of the narrow LCP (b), The plate aligned in the center of the anterior surface of the proximal and distal humerus (c), Post op x-rays showing satisfactory alignment (d), X-rays at 6 months indicated good callus formation (e), Function outcome at 6 months (f).
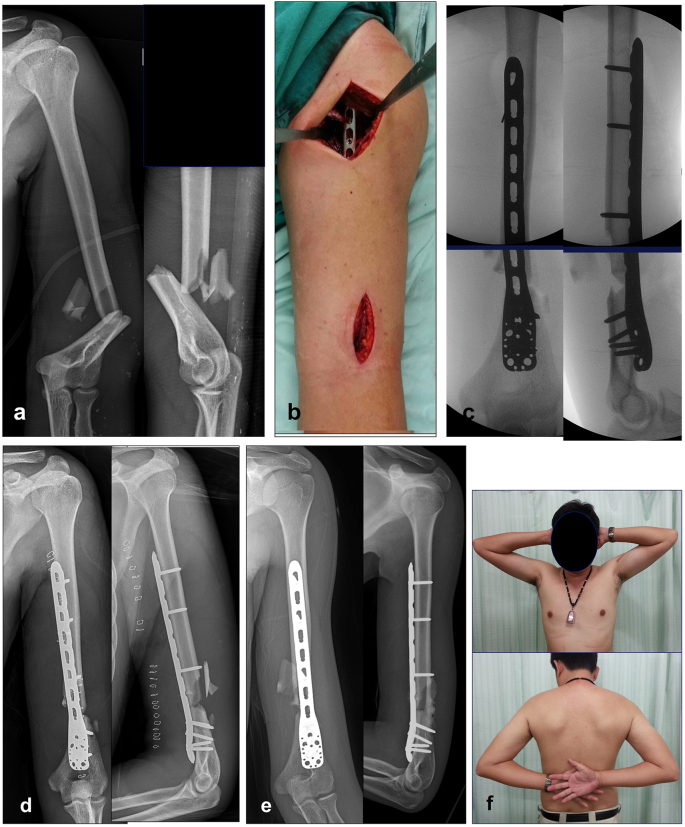
Fig. 3.
AP and lateral X-rays of the humerus showing a comminuted fracture of the distal shaft of the humerus (a), Proximal and distal incisions of anterior MIPO using reverse PHILOS plate (b), Intraoperative images reveal satisfactory alignment of the plate in the center of the anterior surface of the proximal and distal humerus in AP and lateral (c), Post op x-rays show satisfactory alignment (d), X-rays at 6 months indicate posterior bridging callus (e), Functional outcome at 6 months (f).
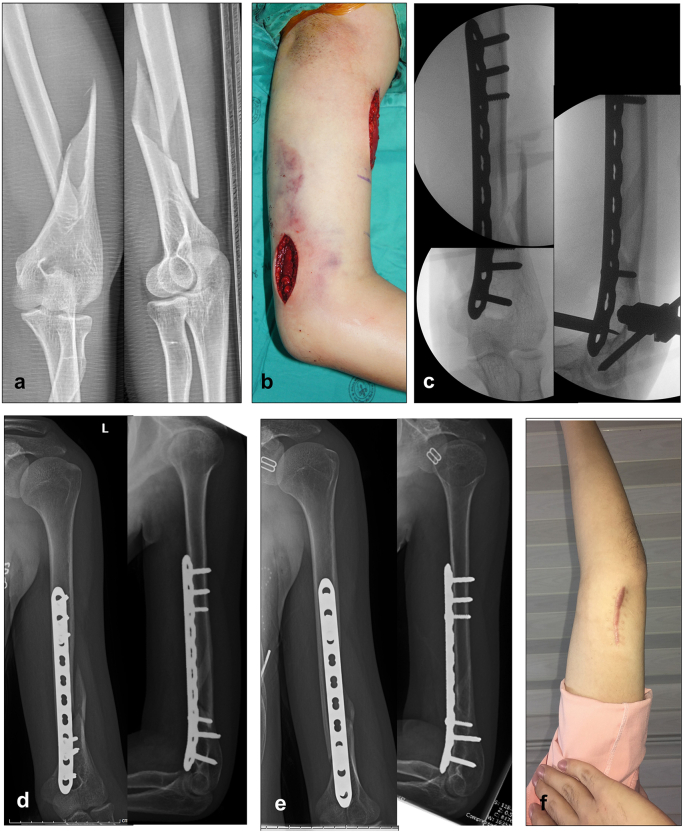
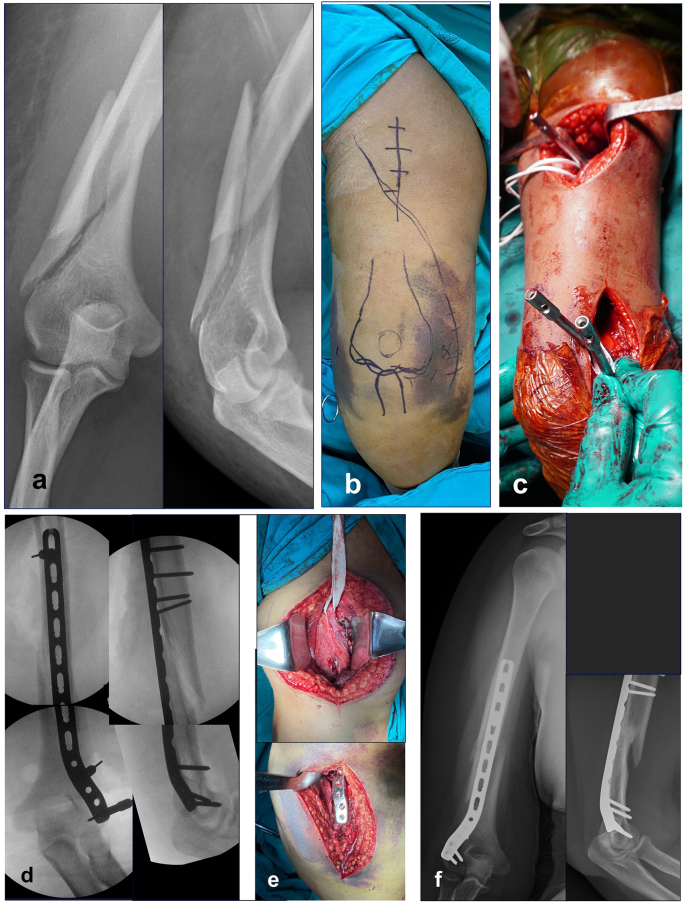
Fig. 4.
AP and lateral X-rays of the humerus show a spiral fracture of the distal shaft of the humerus (a), Proximal and distal incisions of anteromedial MIPO (b), Intraoperative images reveal satisfactory alignment of the plate in the center of the anterior surface of the proximal and distal humerus in AP and lateral (c), Post op x-rays show satisfactory alignment (d), X-rays at 6 months show complete fracture healing (e), Distal incision scar hidden on the medial side of the elbow (f).
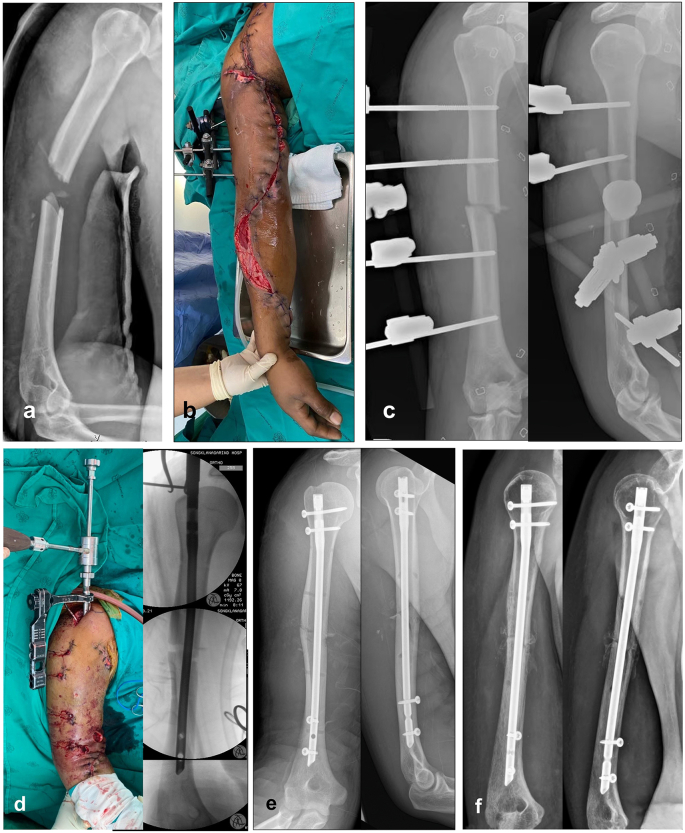
Fig. 5.
X-rays AP and lateral view of the humeral shaft showing spiral wedge fracture of the distal shaft of the humerus (a), Contoured anterolateral plate on the cadaveric bone (b), Distal incision between the brachialis and brachioradialis muscles to identify the radial nerve (c), Proximal and distal incisions of the anterolateral MIPO with the intraoperative alignment (d), Post op x-rays show satisfactory alignment (e), X-rays at 6 months indicated complete bone healing (f).
Fig. 6.
AP and lateral X-rays of the humeral shaft show a low spiral wedge fracture of the distal shaft of the humerus (a), Proximal and distal incisions of posterior MIPO are marked on the skin (b), Proximal and distal incisions with drill sleeves using the extra articular distal humerus locking plate (c), the intraoperative alignment in AP and lateral view (d), Radial nerve lies over the plate at the proximal incision (e), X-rays at 6 months indicated complete bone healing (f).
Table 3.
Options for plate position, approaches, and critical points with MIPO.
| Plate position | Approach | Plate type | Risks and point of concern | References |
|---|---|---|---|---|
| Proximal 1/3 | Deltoid split/deltopectoral | Proximal humerus plate Helical plate |
|
24 |
| Anterior | Narrow LCP |
|
15,25 | |
| Midshaft | Anterior | Narrow DCP Narrow LCP |
|
15,25 |
| Anteromedial |
|
17,18 | ||
| Anterolateral |
|
20 | ||
| Posterior |
|
20 | ||
| Distal 1/3 | Anterior | Specific plate, e.g., reverse PHILOS |
|
16 |
| Anteromedial | Contoured LCP |
|
17,18 | |
| Anterolateral | Contoured LCP |
|
21 | |
| Posterior | EADHP |
|
22,23 |
Abbreviations: DCP - dynamic compression plate; EADHP - extraarticular distal humerus plate; LCP - locking compression plate.
Intramedullary nailing (IMN) is another option for humeral shaft fixation (see Table 4). Compared to ORIF with plate, IMN has a lower risk of infection and of postoperative radial nerve palsy.26 IMN also increases the risk of shoulder impingement, pain, shoulder range of motion restriction, and hardware removal.12,27,28 Zhao JG et al. compared the results and complications among IMN, ORIF and MIPO. They found that treatment with IMN had a higher risk of shoulder impingement than that with ORIF or MIPO.11 Shoulder impingement is a common drawback of IMN found in many reports.26 To the best of our knowledge, some reports which describe experience with shoulder impingement problems state that curved nails were used.29,30 The entry point of a curved nail is at the sulcus between the greater tuberosity and the humeral head which is the supraspinatus tendon insertion. Tendon injury from a curved nail insertion may cause shoulder impingement (Fig. 7). For that reason, the entry point of a new nail design is targeted more medially and the nail curvature has been re-designed a straight nail with a central insertion point. Mocini F et al. reported on short term clinical and radiographic results of proximal and mid shaft humerus fractures treated with straight-shaped nails, stating that the functional results were good to excellent with moderate recovery of muscle strength and almost complete recovery of range of motion.31 El Ghazoui A et al. similarly reported that the percutaneous straight IMN improved the anatomical and functional outcomes in 36 patients.32 However, in both these reports the evidence was level IV.
Table 4.
Comparison of ORIF, MIPO plating and intramedullary nailing.
| Anterior/anterolateral ORIF | Anterior MIPO | IMN | |
|---|---|---|---|
| Characteristics of fracture | Simple | Comminuted | Simple |
| Segmental | Comminuted | ||
| Segmental | |||
| Concerning point | Distal shaft | Short distal fragment | Narrow humeral canal |
| Structure at risks | Musculocutaneous nerve | Musculocutaneous nerve | Rotator cuff (antegrade) |
| Radial nerve | Radial nerve | Triceps (retrograde nail) | |
| Complications | Delayed union | Nonunion | Shoulder impingement |
| Delayed union | |||
| Malreduction |
Fig. 7.
A 31-year-old man had a right humerus fracture with axillary artery and brachial plexus injury. X-rays showed a transverse fracture of the right humerus (a), Axillary artery was repaired and fasciotomy of the arm and forearm were followed by external fixator for temporary immobilization (b), X-rays after external fixator (c), Closed humeral nailing was done. The intraoperative X-rays show good reduction and fixation (d), Immediate post-op radiography showed a good alignment (e), At the 3-month follow-up, callus formation is seen at fracture site (f).
Indications for IMN should be considered together with the inherent advantages and disadvantages of that method. Hudson PW et al. proposed that indications for the use of IMN include complex comminuted, segmental, or long wedge fractures, particularly in patients with comorbidities such as obesity or polytrauma.33 In 2022, Hu Y et al. reported on a meta-analysis which showed that IMN was superior to ORIF in terms of operative time, postoperative infection and bleeding. However, ORIF was reported to be better than IMN in terms of American Shoulder and Elbow Surgeons score (ASES).34 Poor surgical technique when using antegrade nailing can potentially negatively impact shoulder range of motion and result in poor recovery.35 Another drawback of IMN is the expense of the procedure which is significantly greater than ORIF with plate.36
The surgical technique of IMN consists of antegrade and retrograde nailing. With the previous curved nail design, retrograde nailing had a high rate of complications in supracondylar fractures.37 However, Hessmann M et al. and Kuma D et al. found that the rate of success and the incidence of complications of both antegrade and retrograde IMN were not statistically and clinically significantly different.38,39 Antegrade humeral nailing is a familiar surgical technique. It can, however, disturb the shoulder function. Retrograde nailing is technically demanding and may involve the negatively impact elbow function.39,40 Retrograde nailing is contraindicated for patients who have a narrow canal diameter.
1.2.1. Rehabilitation protocol for operative treatment
Since the fracture is stabilized with internal fixation using MIPO or IM nail aim for indirect bone healing with micromotion at the fracture, the patients should move the arm actively after the pain and swelling subside. The postoperative protocol allowed the patients to initiate shoulder and elbow movement in all direction immediately but advised them to avoid from weight-bearing activities, push up or lifting heavy object until 6 weeks post-operation. When the follow up X rays demonstrate bridging callus, progressive weight-bearing is increased and usually full weight-bearing regain in 4–5 months.
1.2.2. Complications of operative treatment
Since the radial nerve is closed proximity to the humerus shaft, minimal invasive fixation with closed reduction and insertion of implants using small incisions increase the risk of iatrogenic nerve injury. Understanding the anatomy, internervous plane of dissection and structure at risk is necessary. Some approaches needs identification of the nerve which is directly related to the approach eg. radial nerve identification at the distal incision of the anterolateral MIPO21 or proximal incision of the posterior MIPO.22 Anterior MIPO or ORIF with brachialis split does not need radial nerve identification because the lateral half of the brachialis act as a cushion to protect the radial nerve and avoid to use the Hohmann retractor on the lateral side of the humerus is recommended.15 Percutaneous insertion of the screw at the distal arm in MIPO or IM nail is high risk of musculocutaneous nerve injury. Mini incision with carefully dissection down to the bone and using the protection sleeve is necessary.25
Malalignment is common in MIPO and IM nail. Knowing the reduction technique and intraoperative evaluation of the humeral rotation is essential. Simple fracture should be reduced by open anatomical reduction and multifragmentary fracture should be reduced by closed reduction.13 Intraoperative evaluation of the proximal humerus profile in anteroposterior (AP) view corresponds to the AP view of the distal humerus using the bicondylar axis profile is recommended.14 In simple fracture with malreduction may caused not only the malaligment but also the delayed union when the fracture has a gap with high strain.13 Selection of the appropriate approach and internal fixation techniques should be considered.
1.3. How to deal with radial nerve palsy
Approximately 10–25% of humeral shaft fractures are associated with radial nerve palsy (RNP)41, 42, 43, 44, 45, 46 and 70–90% of RNP cases resolve through self-recovery.42,43 Fractures located at the middle and distal one-third of the shaft, and those with transverse and/or spiral characteristics have a greater risk of RNP.44 In 2020, Ilyas A et al. reported on 638 cases of humeral fracture with RNP and received nerve exploration. The nerve exploration determined that the continuity of the radial nerve was maintained in approximately 63.7% of the cases. An additional 26.8% had a lacerated nerve, and in 10.5% of the cases the nerve was incarcerated within the fracture site.43 Entezari V et al. reported that RNP associated with vascular injury had less successful nerve recovery.41
Whether radial nerve exploration in primary RNP of a closed humeral shaft fracture should be conducted is still being debated. In the past, observation of nerve recovery has been suggested. If there is no evidence of recovery after 3–4 months following an injury, surgical exploration is recommended. Nerve exploration is also indicated in some situations such as major vascular injury, open fracture, multiple injury and can be done concurrently while performing ORIF. Presently, early exploration seems to improve the nerve recovery rate. IIyas, A et al. reported that 638 patients who were treated without exploration had a recovery rate of 77.2%. Patients who received early nerve exploration (within 3 weeks of the injury) had a recovery rate of 89.75%, while patients with late nerve exploration (more than 8 weeks after the injury) had a nerve recovery rate of 68.1%.43
The incidence of RNP after surgery has been reported to be 6%.45 The best method of management of “secondary radial nerve injury” or radial nerve injury after treatment is still inconclusive. Schwab TR et al. recommended early fixation revision and nerve exploration as the authors found that the causes of secondary RNP are either directly associated with the injury or with implant irritation.45 To prevent intra-operative radial nerve injury, Belayneh, R et al. recommended that routine nerve exploration should be conducted to reduce the incidence of iatrogenic palsy.47 Apivatthakakul T et al. described the danger zone of the radial nerve during MIPO with the anterior approach. The authors suggested avoiding anterior to posterior bicortical screw insertion over the range of central 40–60% of the humeral length. Over that range, the radial nerve, which is located posteriorly, is at risk of injury from the drill bit or a screw tip. If fixation is needed, unicortical screw insertion is recommended. They also suggested avoiding insertion of a Hohmann retractor on the lateral side to retract the lateral half of the brachialis muscle.25
Currently, ultrasound (US) is widely used in selective nerve blocks. It can also be used for detection of the nerve injuries. US provides the benefit of being able to detect the continuity or bony entrapment of a radial nerve in a closed humeral fracture48,49 and is recommended to be performed within 3 weeks of the injury. Esparza M et al. used US to evaluate the continuity of a radial nerve associated with a humerus shaft fracture. They found a 92% concordance between US and intraoperative findings. They also suggested that RNP with only contusions and continuity can be treated conservatively using functional bracing. Early exploration is recommended for entrapped nerves or lacerated nerve injuries.50 As mentioned above, we suggest the use of US to detect the condition of the radial nerve in every case of closed fracture with RNP. If the US shows that radial nerve has continuity, either conservative treatment or operative treatment (ORIF, MIPO or IMN) without radial nerve exploration is recommended. If, however, the radial nerve lacks continuity or if it cannot be identified, radial nerve exploration is compulsory (Fig. 8).
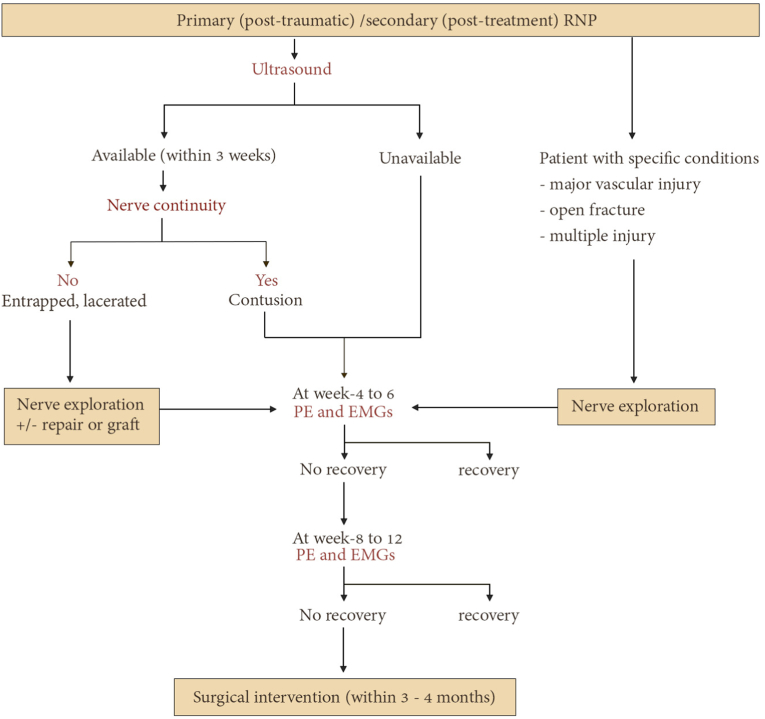
Fig. 8.
Flow diagram depicting of the management of radial nerve palsy associated with humerus fracture. The authors recommend utilizing ultrasound to evaluate nerve continuity in the initial phase. If evidence of nerve entrapment or nerve laceration is detected, immediate nerve exploration is advised. In certain conditions, such as major vascular injury, open fracture, or multiple injuries, early radial nerve exploration is required. When the ultrasound shows good continuity of the nerve, nerve contusion is suspected. Then, it is recommended to monitor clinical symptoms and perform electromyography (EMG) to evaluate the recovery status. The absence of signs and symptoms indicating recovery after 2–3 months suggests the requirement for surgical intervention, depending on the nature of the nerve pathology.
2. Conclusions
Various strategies are available to treat a humerus shaft fracture. Conservative treatment requires close follow-up. The selection of surgical fixation depends on the fracture characteristics and the mode of bone healing needed to achieve bone union. All techniques, including ORIF, MIPO and IMN, have both advantages and disadvantages. Most instances of primary radial nerve palsy with humeral shaft fracture spontaneously self-recover. We recommend the use of ultrasound to evaluate the continuity of the radial nerve.
Declaration of competing interest
The authors do not received funding from any source. We received no payments or other benefits from any commercial entity.
Acknowledgements
We wish to thank Dr. G. Lamar Robert, Ph.D., for reviewing and proofreading of our manuscript
Acknowledgements
We wish to thank Dr. G. Lamar Robert, Ph.D., for reviewing and proofreading of our manuscript.
References
- 1.Lode I., et al. Operative versus nonoperative treatment of humeral shaft fractures: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29(12):2495–2504. doi: 10.1016/j.jse.2020.05.030. [DOI] [PubMed] [Google Scholar]
- 2.Oliver W.M., et al. Surgical versus nonsurgical management of humeral shaft fractures: a systematic review and meta-analysis of randomized trials. J Am Acad Orthop Surg. 2023;31(2):e82–e93. doi: 10.5435/JAAOS-D-22-00432. [DOI] [PubMed] [Google Scholar]
- 3.Sarmiento A., et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(5):596–601. [PubMed] [Google Scholar]
- 4.Rämö L., et al. Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: the FISH randomized clinical trial. JAMA. 2020;323(18):1792–1801. doi: 10.1001/jama.2020.3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serrano R., et al. Modern results of functional bracing of humeral shaft fractures: a multicenter retrospective analysis. J Orthop Trauma. 2020;34(4):206–209. doi: 10.1097/BOT.0000000000001666. [DOI] [PubMed] [Google Scholar]
- 6.Den Hartog D., et al. Functional and clinical outcome after operative versus nonoperative treatment of a humeral shaft fracture (HUMMER): results of a multicenter prospective cohort study. Eur J Trauma Emerg Surg. 2022;48(4):3265–3277. doi: 10.1007/s00068-022-01890-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ali E., et al. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg. 2015;24(2):210–214. doi: 10.1016/j.jse.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Neuhaus V., et al. Risk factors for fracture mobility six weeks after initiation of brace treatment of mid-diaphyseal humeral fractures. J Bone Joint Surg Am. 2014;96(5):403–407. doi: 10.2106/JBJS.M.00089. [DOI] [PubMed] [Google Scholar]
- 9.Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br. 1966;48(1):105–111. [PubMed] [Google Scholar]
- 10.van de Wall B.J.M., et al. MIPO versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2022;48(1):47–59. doi: 10.1007/s00068-020-01585-w. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J.G., et al. Surgical interventions to treat humerus shaft fractures: a network meta-analysis of randomized controlled trials. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patino J.M., et al. Plates vs. nails in humeral shaft fractures: do plates lead to a better shoulder function? JSES Int. 2021;5(4):765–768. doi: 10.1016/j.jseint.2021.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rellán I., et al. Time until union in absolute vs. relative stability MIPO plating in simple humeral shaft fractures. Eur J Orthop Surg Traumatol. 2022;32(1):191–197. doi: 10.1007/s00590-021-02920-6. [DOI] [PubMed] [Google Scholar]
- 14.Lee H.J., et al. Minimally invasive plate osteosynthesis for humeral shaft fracture: a reproducible technique with the assistance of an external fixator. Arch Orthop Trauma Surg. 2013;133(5):649–657. doi: 10.1007/s00402-013-1708-7. [DOI] [PubMed] [Google Scholar]
- 15.Apivatthakakul T., Arpornchayanon O., Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36(4):530–538. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 16.Jitprapaikulsarn S., et al. Anterior minimally invasive plating osteosynthesis using reversed proximal humeral internal locking system plate for distal humeral shaft fractures. Eur J Orthop Surg Traumatol. 2020;30(8):1515–1521. doi: 10.1007/s00590-020-02708-0. [DOI] [PubMed] [Google Scholar]
- 17.Buranaphatthana T., Apivatthakakul T., Apivatthakakul V. Anteromedial minimally invasive plate osteosynthesis (MIPO) for distal third humeral shaft fractures - is it possible?: a cadaveric study. Injury. 2019;50(6):1166–1174. doi: 10.1016/j.injury.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 18.Cañada-Oya H., et al. New, minimally invasive, anteromedial-distal approach for Plate Osteosynthesis of distal-third humeral shaft fractures: an anatomical study. JB JS Open Access. 2020;5(1):e0056. doi: 10.2106/JBJS.OA.19.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang J., et al. Treatment of humeral shaft fractures: a new minimally-invasive plate osteosynthesis versus open reduction and internal fixation: a case control study. BMC Surg. 2021;21(1):349. doi: 10.1186/s12893-021-01347-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Q., et al. Anterolateral approach with two incisions versus posterior median approach in the treatment of middle- and distal-third humeral shaft fractures. J Orthop Surg Res. 2021;16(1):197. doi: 10.1186/s13018-021-02355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao W., et al. Antero-lateral minimally invasive plate osteosynthesis (MIPO) with the radial nerve exploration for extra-articular distal-third diaphyseal fractures of the humerus. Int Orthop. 2017;41(9):1757–1762. doi: 10.1007/s00264-017-3514-2. [DOI] [PubMed] [Google Scholar]
- 22.Jiamton C., et al. The safety and feasibility of minimal invasive plate osteosynthesis (MIPO) of the posterior aspect of the humerus: a cadaveric study. Clin Anat. 2019;32(2):176–182. doi: 10.1002/ca.23220. [DOI] [PubMed] [Google Scholar]
- 23.Jitprapaikulsarn S., et al. Minimally invasive plate osteosynthesis via posterior approach for type b and c fractures of distal humeral shaft: surgical tactics and a clinical series. Eur J Orthop Surg Traumatol. 2022 doi: 10.1007/s00590-022-03255-6. [DOI] [PubMed] [Google Scholar]
- 24.García-Virto V., et al. MIPO helical pre-contoured plates in diaphyseal humeral fractures with proximal extension. Surgical technique and results. Injury. 2021;52(Suppl 4):S125–S130. doi: 10.1016/j.injury.2021.01.049. [DOI] [PubMed] [Google Scholar]
- 25.Apivatthakakul T., Patiyasikan S., Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury. 2010;41(2):169–172. doi: 10.1016/j.injury.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Beeres F.J.P., et al. Open plate fixation versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2022;48(4):2667–2682. doi: 10.1007/s00068-021-01728-7. [DOI] [PubMed] [Google Scholar]
- 27.Kurup H., Hossain M., Andrew J.G. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;(6):Cd005959. doi: 10.1002/14651858.CD005959.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Akalın Y., et al. Locking compression plate fixation versus intramedullary nailing of humeral shaft fractures: which one is better? A single-centre prospective randomized study. Int Orthop. 2020;44(10):2113–2121. doi: 10.1007/s00264-020-04696-6. [DOI] [PubMed] [Google Scholar]
- 29.Muccioli C., et al. Rotator cuff integrity and shoulder function after intra-medullary humerus nailing. Orthop Traumatol Surg Res. 2020;106(1):17–23. doi: 10.1016/j.otsr.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Cocco L.F., et al. Quality of life after antegrade intramedullary nail fixation of humeral fractures: a survey in a selected cohort of Brazilian patients. Patient Saf Surg. 2018;12:4. doi: 10.1186/s13037-018-0150-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mocini F., et al. Clinical and radiographic outcomes after antegrade intramedullary nail fixation of humeral fractures. Injury. 2020;51(3):S34–S38. doi: 10.1016/j.injury.2020.04.043. [DOI] [PubMed] [Google Scholar]
- 32.El Ghazoui A., et al. Humeral shaft fracture: outcomes of percutaneous antegrade intramedullary nailing using the long Telegraph® nail with dynamic distal locking. Orthop Traumatol Surg Res. 2022;108(5) doi: 10.1016/j.otsr.2022.103286. [DOI] [PubMed] [Google Scholar]
- 33.Hudson P.W., et al. Percutaneous intramedullary nailing of complex humeral shaft fractures: a retrospective case series. Cureus. 2022;14(12) doi: 10.7759/cureus.32999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu Y., et al. Efficacy and safety evaluation of intramedullary nail and locking compression plate in the treatment of humeral shaft fractures: a systematic review and meta-analysis. Comput Math Methods Med. 2022;2022 doi: 10.1155/2022/5759233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flinkkilä T., et al. Recovery of shoulder joint function after humeral shaft fracture: a comparative study between antegrade intramedullary nailing and plate fixation. Arch Orthop Trauma Surg. 2004;124(8):537–541. doi: 10.1007/s00402-004-0727-9. [DOI] [PubMed] [Google Scholar]
- 36.Stephens A.R., et al. Comparison of direct surgical cost for humeral shaft fracture fixation: open reduction internal fixation versus intramedullary nailing. JSES Int. 2021;5(4):734–738. doi: 10.1016/j.jseint.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahaisavariya B., et al. Mismatch analysis of humeral nailing: antegrade versus retrograde insertion. J Orthop Sci. 2011;16(5):644–651. doi: 10.1007/s00776-011-0127-2. [DOI] [PubMed] [Google Scholar]
- 38.Hessmann M.H., Mittlmeier T. [Antegrade and retrograde nailing of humeral shaft fractures] Oper Orthop Traumatol. 2021;33(2):139–159. doi: 10.1007/s00064-021-00706-x. [DOI] [PubMed] [Google Scholar]
- 39.Kumar D., et al. Antegrade vs retrograde intramedullary nailing in humerus shaft fractures: a systematic review and meta-analysis. J Orthop. 2022;34:391–397. doi: 10.1016/j.jor.2022.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hollister A.M., et al. New technique for humerus shaft fracture retrograde intramedullary nailing. Tech Hand Up Extrem Surg. 2011;15(3):138–143. doi: 10.1097/BTH.0b013e31820246ee. [DOI] [PubMed] [Google Scholar]
- 41.Entezari V., Olson J.J., Vallier H.A. Predictors of traumatic nerve injury and nerve recovery following humeral shaft fracture. J Shoulder Elbow Surg. 2021;30(12):2711–2719. doi: 10.1016/j.jse.2021.04.025. [DOI] [PubMed] [Google Scholar]
- 42.Hendrickx L.A.M., et al. Radial nerve palsy associated with closed humeral shaft fractures: a systematic review of 1758 patients. Arch Orthop Trauma Surg. 2021;141(4):561–568. doi: 10.1007/s00402-020-03446-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ilyas A.M., Mangan J.J., Graham J. Radial nerve palsy recovery with fractures of the humerus: an updated systematic review. J Am Acad Orthop Surg. 2020;28(6):e263–e269. doi: 10.5435/JAAOS-D-18-00142. [DOI] [PubMed] [Google Scholar]
- 44.Shao Y.C., et al. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87(12):1647–1652. doi: 10.1302/0301-620X.87B12.16132. [DOI] [PubMed] [Google Scholar]
- 45.Schwab T.R., et al. Radial nerve palsy in humeral shaft fractures with internal fixation: analysis of management and outcome. Eur J Trauma Emerg Surg. 2018;44(2):235–243. doi: 10.1007/s00068-017-0775-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hegeman E.M., et al. Incidence and management of radial nerve palsies in humeral shaft fractures: a systematic review. Cureus. 2020;12(11) doi: 10.7759/cureus.11490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Belayneh R., et al. The standardized exploration of the radial nerve during humeral shaft fixation reduces the incidence of iatrogenic palsy. Arch Orthop Trauma Surg. 2023;143(1):125–131. doi: 10.1007/s00402-021-04028-2. [DOI] [PubMed] [Google Scholar]
- 48.Bodner G., et al. Radial nerve palsy associated with humeral shaft fracture: evaluation with US--initial experience. Radiology. 2001;219(3):811–816. doi: 10.1148/radiology.219.3.r01jn09811. [DOI] [PubMed] [Google Scholar]
- 49.Bodner G., et al. Sonographic detection of radial nerve entrapment within a humerus fracture. J Ultrasound Med. 1999;18(10):703–706. doi: 10.7863/jum.1999.18.10.703. [DOI] [PubMed] [Google Scholar]
- 50.Esparza M., et al. Ultrasound evaluation of radial nerve palsy associated with humeral shaft fractures to guide operative versus non-operative treatment. Acta Med Acad. 2019;48(2):183–192. doi: 10.5644/ama2006-124.257. [DOI] [PubMed] [Google Scholar]