Abstract
Objective:
Our objectives were to describe time intervals of EMS encounters for suspected stroke patients in North Carolina (NC) and evaluate differences in EMS time intervals by community socioeconomic status (SES) and rurality.
Methods:
This cross-sectional study used statewide data on EMS encounters of suspected stroke in NC in 2019. Eligible patients were adults requiring EMS transport to a hospital following a 9-1-1 call for stroke-like symptoms. Incident street addresses were geocoded to census tracts and linked to American Community Survey SES data and to rural-urban commuting area (RUCA) codes. Community SES was defined as high, medium, or low based on tertiles of an SES index. Urban, suburban, and rural tracts were defined by RUCA codes 1, 2–6, and 7–10, respectively. Multivariable quantile regression was used to estimate how the median and 90th percentile of EMS time intervals varied by community SES and rurality, adjusting for each other; patient age, gender, and race/ethnicity; and incident characteristics
Results:
We identified 17,117 eligible EMS encounters of suspected stroke from 2,028 census tracts. The population was 65% 65+ years old; 55% female; and 69% Non-Hispanic White. Median response, scene, and transport times were 8 (interquartile range, IQR 6–11) min, 16 (IQR 12–20) min, and 14 (IQR 9–22) minutes, respectively. In quantile regression adjusted for patient demographics, minimal differences were observed for median response and scene times by community SES and rurality. The largest median differences were observed for transport times in rural (6.7 min, 95% CI 5.8, 7.6) and suburban (4.7 min, 95% CI 4.2, 5.1) tracts compared to urban tracts. Adjusted rural-urban differences in 90th percentile transport times were substantially greater (16.0 min, 95% CI 14.5, 17.5). Low SES was modesty associated with shorter median (−3.3 min, 95% CI −3.8, −2.9) and 90th percentile (−3.0 min, 95% CI −4.0, −2.0) transport times compared to high SES tracts.
Conclusions:
While community-level factors were not strongly associated with EMS response and scene times for stroke, transport times were significantly longer rural tracts and modestly shorter in low SES tracts, accounting for patient demographics. Further research is needed on the role of community socioeconomic deprivation and rurality in contributing to delays in prehospital stroke care.
Keywords: emergency medical services, stroke, community, socioeconomic status, rurality
Introduction
Each year, more than 795,000 Americans suffer an acute stroke (1). “Time is brain” is often referenced by medical professionals to convey the importance of optimizing time management in the treatment of acute ischemic stroke. Each minute a stroke is untreated, a typical patient loses an estimated 1.9 million neurons (2). Current guidelines from the American Heart Association (AHA)/American Stroke Association (ASA) state intravenous (IV) recombinant tissue plasminogen activator (tPA) be given up to 4.5 hours after stroke symptom onset (3, 4). However, IV rt-TPA declines in efficacy over the 4.5-hour period (5–7). Recent advancements introduced endovascular reperfusion therapies as additional treatment options (8, 9). Unfortunately, access to such reperfusion therapies (i.e., intra-arterial thrombolysis, mechanical thrombectomy) is limited to select hospitals with specialized equipment and personnel, predominantly located in urban areas (10, 11). Similar to IV tPA, time to endovascular therapy is strongly associated with functional outcomes in acute stroke patients (12, 13), making these treatments highly time-dependent.
Emergency medical services (EMS) perform a significant role in the early management of acute stroke patients. Rapid EMS response, care, and transport is critical to ensuring timely management of acute stroke. Further, it is estimated that up to 65% of stroke patients utilize EMS to access hospital care (14). Evaluation by EMS for suspected acute stroke patients is associated with faster neurologic evaluation and reduced delays to time-sensitive treatment in the hospital (15–19). Current AHA/ASA guidelines recommend EMS limit response intervals to ≤ 9 minutes (90th percentile), scene intervals to ≤ 15 minutes (90th percentile), and minimize transport intervals to the nearest stroke-capable hospital (20). EMS optimization of prehospital stroke management is critical in reducing time-delays to treatment which contribute to preventable morbidity and mortality (7, 19, 21).
To date, the literature is mixed regarding the role of community factors, such as socioeconomic status (SES) and rurality, in the timely prehospital management of acute stroke patients. Kleindorfer et al. (22) observed that living in a poorer area did not appear to delay access to acute care for stroke in a clinically significant way. However, Ader et al. (23) and Kapral et al. (24) report that lower SES is associated with longer onset-to-treatment time. Furthermore, rural stroke patients have less access to acute care (25) and are at increased risk of mortality (26) compared to their urban counterparts. Given these stroke disparities, there is a need to understand variations in prehospital delays by community-level factors. Therefore, we compared EMS prehospital time intervals (i.e., response, scene, and transport times) by community socioeconomic status (SES) and urban-rural status among suspected stroke patients in North Carolina (NC). We hypothesized that underserved communities defined by low SES and rurality would have longer prehospital times.
Methods
Study Design and Setting
We conducted a cross-sectional study with retrospective data from the NC EMS Data System developed and overseen by the North Carolina Office of EMS (NCOEMS). The 100 county-based EMS systems in NC are state mandated to submit electronic data on all EMS encounters to the NC EMS Data System. These data are routinely collected to evaluate and improve patient care and EMS system performance. Data collected from EMS agencies are coded based on standardized data elements defined by the National EMS Information System (NEMSIS) Version 3 standard. Data elements include patient demographics (e.g., gender, race/ethnicity, age), incident street address, EMS response, scene and transport date/times, incident disposition, and destination facility (e.g., hospital). The data collected for this study are listed in Table S1. This study was reviewed by the University of North Carolina Institutional Review Board and was approved by expedited review. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies were followed for this manuscript.
North Carolina is a large, diverse state located within the Stroke Belt, a multi-state region in the southeast United States with a disproportionately higher burden of stroke morbidity and mortality than the rest of the country (27). Further, 43 percent and 13.6 percent of North Carolinians live in rural areas and in poverty, respectively (28, 29). To address geographic disparities in access to reperfusion therapy, the NCOEMS implemented a stroke triage and destination plan in 2010 that allows EMS to bypass hospitals without IV-tPA capabilities for stroke capable hospitals (30). These plans are specific to the local EMS system and consider the patient’s symptom onset time, stroke assessment, and transport times to the closest certified stroke center (31). Hospitals in NC are granted certification by The Joint Commission or Det Norske Veritas Global Healthcare accreditation agencies as Acute Stroke Ready Hospitals, Primary Stroke Centers, Thrombectomy Capable Stroke Centers, and Comprehensive Stroke Centers. Based on these stroke center certification levels, we classified EMS destination hospitals as non-certified, stroke-capable, and thrombectomy-capable.
Study Population
We analyzed prehospital data on EMS-suspected stroke encounters from 2019 occurring in NC. Eligible patients were adults (at least 18 years old) with a 9-1-1 call response by EMS for stroke-like symptoms (i.e., EMS provider impression of stroke or use of suspected stroke protocol). Encounters were excluded if the incident address was not able to be geocoded or located outside of NC and if EMS did not transport to a hospital.
Census Tract Characteristics
We geocoded incident addresses to census tracts using ArcGIS Pro (Esri, Redlands, CA). Census tract-level socioeconomic data were obtained from the 2015–2019 American Community Survey 5-year estimates (32). These data were summarized with an area-level SES index developed by the Agency for Healthcare Research and Quality that includes measures of income, wealth, education, occupation, and housing (33). This index ranges from 0–100 with higher scores indicating higher SES. For our study, scores were grouped into thirds using tertiles of the distribution for all 2,195 NC census tracts to define high, medium, and low community SES (>54.4, 51.1–54.4, and <51.1, respectively). Census tract rural-urban commuting area (RUCA) primary codes were grouped to define urban-rural status. Urban, suburban, and rural tracts were defined by RUCA codes 1, 2–6, and 7–10, respectively.
EMS Time Intervals
We examined three EMS time intervals: response, scene, and transport intervals. Response interval was defined as the time from EMS unit notification to arrival on scene. Scene interval was defined as the time from EMS arrival on scene to EMS left scene with patient. Transport interval was defined as the time EMS left scene to EMS arrival with patient to the destination hospital.
Study Covariates
Patient age (in years) was categorized into 18–44, 45–54, 55–64, 65–74, 75–84, and 85 and older groups. Patient gender was categorized as female or male. Patient race/ethnicity was categorized as non-Hispanic Black or African American, non-Hispanic White, non-Hispanic other (i.e., American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander), or Hispanic or Latino. Incident characteristics included time of day (7:00AM-2:59PM, 3:00PM-10:59PM, or 11:00PM-6:59AM) and day of week (weekend versus weekday) based on the date and time of EMS notification by 9-1-1 dispatch. The duration (in hours) of the complaint reported by the patient or historian was categorized into 0–3, 3–6, 6–24, and >24 hours based on acute stroke treatment windows. We identified incidents that had a complaint of stroke reported by 9-1-1 dispatch to EMS. The EMS provider’s primary impression was grouped into stroke, altered mental status, weakness, and other categories.
Statistical Analysis
Descriptive statistics were used to describe patient characteristics and times intervals of EMS encounters. Median, interquartile range (IQR), and 90th percentiles of EMS response, scene, and transport intervals were calculated. Kruskal-Wallis tests were used to compare EMS time intervals by community SES and rurality with p<0.05 considered statistically significant such that the null hypothesis that EMS time distributions are equal across tract SES and rurality is rejected. Complete-case analysis (i.e., only observations with data on all variables analyzed) was used to handle missing data. Quantile regression with both tract SES and urban-rural status was performed for each time interval. Since EMS systems are concerned with times for the majority of patients (represented by 90th percentiles) (34–36), quantile regression was used to estimate differences in 50th (median) and 90th percentiles (and their 95% confidence intervals, CIs) of the response, scene, and transport interval distributions by community SES and urban-rural status. In primary analyses, quantile regression was adjusted for patient age, gender, and race to account for demographic differences between tracts as a potential source of confounding. In secondary analyses, we further adjusted for incident characteristics (time of day, weekend, duration of complaint, 9-1-1 dispatch complaint of stroke, and EMS provider primary impression) although it is not clear these covariates are potential confounders or causal intermediates of the relationship between tract characteristics and EMS times. Given the descriptive nature of the study objectives, a formal sample size calculation was not performed, and all available data were used for the analysis. Statistical analyses were conducted in SAS 9.4 (Cary, NC).
Results
We identified 18,251 suspected stroke patients responded to by EMS. Of these, 79 were excluded because either occurring outside NC or not able to be geocoded, and another 1,055 were excluded because EMS did not transport to the hospital, leaving 17,117 eligible patients for this analysis. These EMS encounters occurred in 2,028 census tracts of the 2,195 total census tracts in NC shown in Figure 1. Patients located in urban tracts were more likely in higher SES tracts compared to patients in suburban and rural tracts (Table 1). All rurality-SES combinations were represented in these data although only 1% of suspected stroke encounters occurred in rural-high SES census tracts.
Figure 1.

North Carolina’s 2,195 Census Tracts by Urban-Rural Status and Socioeconomic Status
RUCA indicates rural-urban commuting area; AHRQ, Agency for Healthcare Research and Quality; SES, socioeconomic status
Table 1.
EMS Encounters of Suspected Stroke Patients by Census Tract Urban-Rural Status and SES in North Carolina (N=17,117)
| Urban | Suburban | Rural | |
|---|---|---|---|
| High SES | 3,907 (22.8%) | 766 (4.5%) | 139 (0.8%) |
| Medium SES | 3,493 (20.4%) | 2,196 (12.8%) | 608 (3.6%) |
| Low SES | 2,504 (14.6%) | 2,677 (15.6%) | 827 (4.8%) |
SES indicates socioeconomic status; and NC, North Carolina
The study population was 65% 65 years or older, 55% female, and 70% Non-Hispanic White (Table 2). Suspected stroke encounters were more likely in urban (58%) census tracts compared to suburban (33%) and rural (9%). Non-Hispanic White patients were more likely found in suburban and medium-high SES tracts whereas Non-Hispanic Black patients were more likely found in urban or rural and low SES tracts. About half of incidents occurred between 3PM and 11PM across tract SES and urban-rural status. Similarly, about one-fourth occurred on the weekend. The majority of patients (70%) were responded to by EMS within 3 hours of complaint. A complaint of stroke by dispatch was more likely to be reported in high SES (61%) compared to low SES (53%) tracts. The majority of patients (85%) had an EMS provider primary impression of stroke across tract SES and urban-rural status. Most patients were transported to either a thrombectomy-capable (33%) or stroke-capable (51%) hospital. Transport to a non-certified hospital was more likely in suburban/rural and low-medium SES communities.
Table 2.
Descriptive Characteristics of Suspected Stroke Patients Transported by Emergency Medical Services in North Carolina, 2019 (N=17,117)
| Characteristic | Overall (N=17,117) | Census Tract Urban-Rural Status | Census Tract Socioeconomic Status | ||||
|---|---|---|---|---|---|---|---|
| Urban (N=9,904) |
Suburban (N=5,639) |
Rural (N=1,574) |
Low (N=6,008) |
Medium (N=6,297) |
High (N=4,812) |
||
|
| |||||||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| Age group (years) | |||||||
| 18–44 | 988 (5.8) | 603 (6.1) | 306 (5.4) | 79 (5.0) | 365 (6.1) | 347 (5.5) | 276 (5.7) |
| 45–54 | 1,770 (10.3) | 1,035 (10.5) | 572 (10.1) | 163 (10.4) | 719 (12.0) | 652 (10.4) | 399 (8.3) |
| 55–64 | 3,238 (18.9) | 1,836 (18.5) | 1,122 (20.0) | 280 (17.8) | 1,338 (22.3) | 1,195 (19.0) | 705 (14.7) |
| 65–74 | 4,103 (24.0) | 2,367 (23.9) | 1,362 (24.2) | 374 (23.8) | 1,497 (24.9) | 1,487 (23.6) | 1,119 (23.3) |
| 75–84 | 4,000 (23.4) | 2,291 (23.1) | 1,333 (23.6) | 376 (23.9) | 1,236 (20.6) | 1,481 (23.5) | 1,283 (26.7) |
| 85+ | 3,018 (17.6) | 1,772 (17.9) | 944 (16.7) | 302 (19.2) | 853 (14.2) | 1,135 (18.0) | 1,030 (21.4) |
|
| |||||||
| Gender | |||||||
| Female | 9,330 (54.5) | 5,417 (54.7) | 3,054 (54.2) | 859 (54.6) | 3,240 (54.0) | 3,499 (55.6) | 2,591 (53.9) |
| Male | 7,773 (45.5) | 4,480 (45.3) | 2,579 (45.8) | 714 (45.4) | 2,764 (46.0) | 2,792 (44.4) | 2,217 (46.1) |
| missing | 14 | 7 | 6 | 1 | 4 | 6 | 4 |
|
| |||||||
| Race/Ethnicity | |||||||
| Non-Hispanic Black/African American | 4,567 (27.1) | 2,941 (30.0) | 1,212 (21.9) | 414 (27.1) | 2,219 (37.8) | 1,519 (24.4) | 829 (17.5) |
| Non-Hispanic White | 11,839 (70.3) | 6,598 (67.4) | 4,159 (75.2) | 1,082 (70.8) | 3,471 (59.1) | 4,573 (73.5) | 3,795 (79.9) |
| Non-Hispanic Other | 207 (1.2) | 102 (1.0) | 90 (1.6) | 15 (1.0) | 112 (1.9) | 40 (0.6) | 55 (1.2) |
| Hispanic or Latino | 236 (1.4) | 149 (1.5) | 69 (1.3) | 18 (1.2) | 73 (1.2) | 93 (1.5) | 70 (1.5) |
| missing | 268 | 114 | 109 | 45 | 133 | 72 | 63 |
|
| |||||||
| Time of day | |||||||
| 7:00AM-2:59PM | 4,713 (27.5) | 2,677 (27.0) | 1,601 (28.4) | 435 (27.6) | 1,695 (28.2) | 1,729 (27.5) | 1,289 (26.8) |
| 3:00PM-10:59PM | 8,579 (50.1) | 5,072 (51.2) | 2,722 (48.3) | 785 (49.9) | 2,957 (49.2) | 3,119 (49.5) | 2,503 (52) |
| 11:00PM-6:59AM | 3,825 (22.4) | 2,155 (21.8) | 1,316 (23.3) | 354 (22.5) | 1,356 (22.6) | 1,449 (23.0) | 1,020 (21.2) |
| Weekend | 4,448 (26.0) | 2,558 (25.8) | 1,485 (26.3) | 405 (25.7) | 1,589 (26.5) | 1,638 (26.0) | 1,221 (25.4) |
| Duration of complaint | |||||||
| 0–3 hours | 11,093 (70.4) | 6,178 (69.2) | 3,832 (71.5) | 1,083 (73.6) | 3,960 (70.9) | 4,182 (69.6) | 2,951 (71) |
| 3–6 hours | 1,177 (7.5) | 668 (7.5) | 399 (7.5) | 110 (7.5) | 403 (7.2) | 454 (7.6) | 320 (7.7) |
| 6–24 hours | 2,351 (14.9) | 1,406 (15.8) | 770 (14.4) | 175 (11.9) | 802 (14.4) | 938 (15.6) | 611 (14.7) |
| >24 hours | 1,130 (7.2) | 671 (7.5) | 356 (6.7) | 103 (7.0) | 421 (7.5) | 433 (7.2) | 276 (6.6) |
| missing | 1,366 | 981 | 282 | 103 | 422 | 290 | 654 |
| 9-1-1 dispatch complaint of stroke | 9,766 (57.1) | 5,648 (57) | 3,224 (57.2) | 894 (56.8) | 3,184 (53.0) | 3,671 (58.3) | 2,911 (60.5) |
| EMS provider primary impression | |||||||
| Stroke | 13,698 (84.8) | 8,015 (84.9) | 4,450 (84.8) | 1,233 (84.1) | 4,735 (84.8) | 5,014 (84.4) | 3,949 (85.4) |
| Altered Mental Status | 928 (5.7) | 505 (5.4) | 325 (6.2) | 98 (6.7) | 331 (5.9) | 345 (5.8) | 252 (5.5) |
| Weakness | 528 (3.3) | 329 (3.5) | 155 (3.0) | 44 (3.0) | 166 (3.0) | 224 (3.8) | 138 (3.0) |
| Other | 1,001 (6.2) | 594 (6.3) | 315 (6.0) | 92 (6.3) | 353 (6.3) | 360 (6.1) | 288 (6.2) |
| missing | 962 | 461 | 394 | 107 | 423 | 354 | 185 |
|
| |||||||
| Destination Hospital Classification | |||||||
| Thrombectomy-capable | 5,307 (32.7) | 4,018 (42.7) | 986 (18.4) | 303 (20.5) | 1,224 (21.3) | 1,892 (31.7) | 2,191 (48.3) |
| Stroke-capable | 8,254 (50.8) | 4,784 (50.9) | 2,778 (51.8) | 692 (46.8) | 2,967 (51.6) | 3,191 (53.5) | 2,096 (46.2) |
| Non-certified | 2,687 (16.5) | 606 (6.4) | 1,596 (29.8) | 485 (32.8) | 1,557 (27.1) | 881 (14.8) | 249 (5.5) |
| missing | 869 | 496 | 279 | 94 | 260 | 333 | 276 |
Median response, scene, and transport intervals were 8 (IQR 6–11, 90th percentile 15) min, 16 (IQR 12–20, 90th percentile 26) min, and 14 (IQR 9–22, 90th percentile 30) minutes, respectively. Differences in response time distributions were statistically significant by community SES (p<.001) and urban-rural status (p<.001) although differences in medians were minimal (Figure 2). Scene time distributions were not statistically different across community SES (p=0.086). While scene time distributions were statistically different across urban-rural status (p<.001), the differences were minimal. Transport time differences were statistically significant by community SES (p<.001) and urban-rural status (p<.001) and more clinically meaningful than response and scene times. In quantile regression adjusted for patient demographics, minimal differences were observed for median response and scene times by community SES and rurality (Table 3). Although differences were relatively small, rural tracts had greater 90th percentile response (4.5 min, 95% CI 3.8, 5.2) and scene (2.3 min, 95% CI 1.4, 3.3) than urban tracts. The largest median and 90th percentile differences were observed for transport times in rural and suburban tracts compared to urban tracts. Lastly, after adjusting for urban-rural status and patient demographics, low SES was modesty associated with shorter median (−3.3 min, 95% CI −3.8, −2.9) and 90th percentile (−3.0 min, 95% CI −4.0, −2.0) transport times compared to high SES tracts. Fully-adjusted models, which included incident characteristics in addition to tract SES and urban-rural status and patient demographics, produced comparable results.
Figure 2.
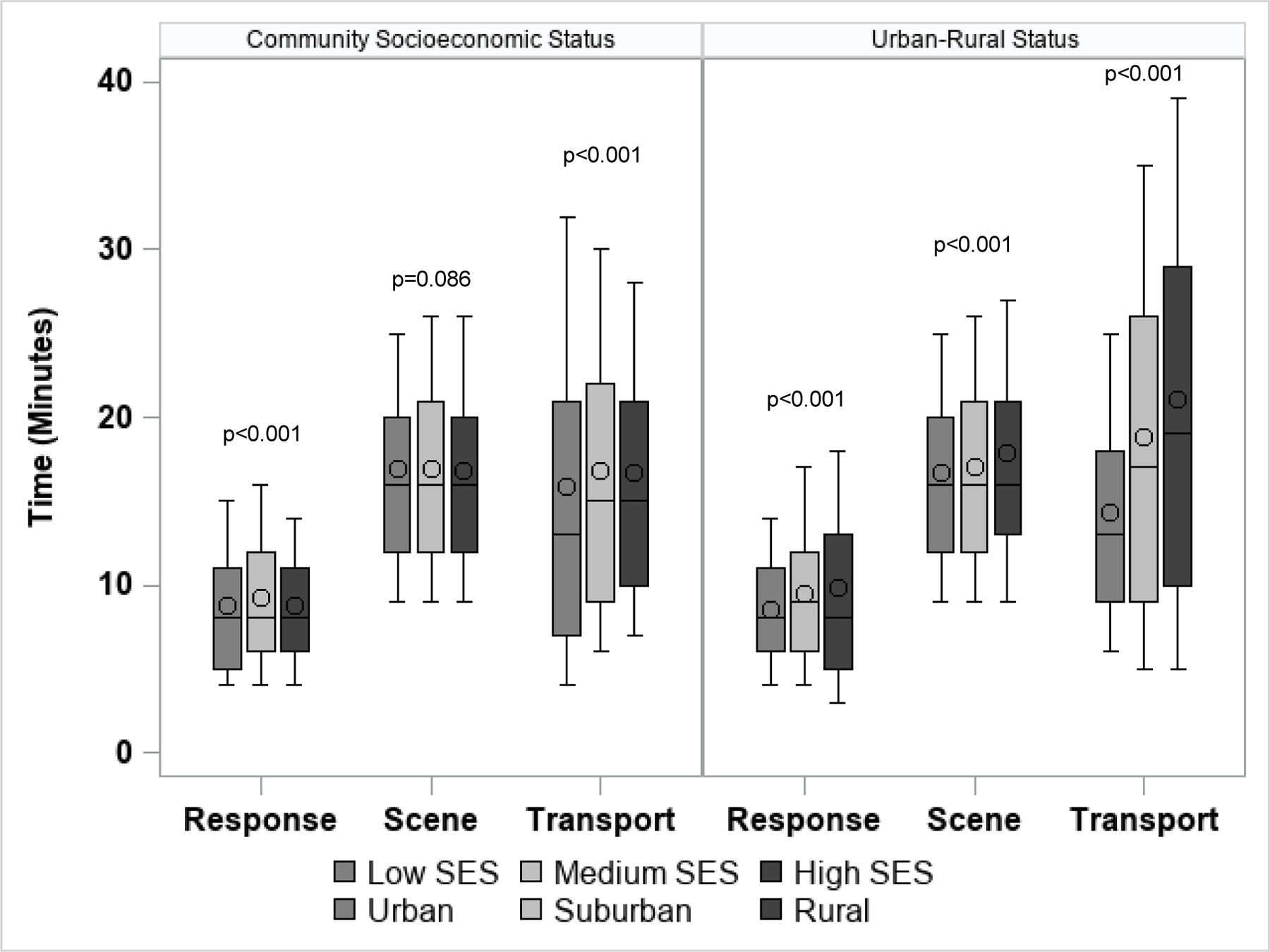
Boxplots of EMS Time Intervals by Community SES and Urban-Rural Status in North Carolina, 2019 (N=17,117)
EMS indicates emergency medical services; SES, socioeconomic status; and NC, North Carolina
circle=mean, horizontal line=median, box=interquartile range, whiskers=10th and 90th percentiles, p values from Kruskal Wallis tests
Table 3.
Adjusted Quantile Regression Estimates Comparing Median and 90th Percentile EMS Time Intervals by Community Socioeconomic Status and Urban-Rural Status Adjusting for Each Other and (a) Patient Demographics* plus (b) Incident Characteristics†
| Model #1a*: Response time | Median | 90th Percentile | ||
|---|---|---|---|---|
| Estimate | (95% CI) | Estimate | (95% CI) | |
| Low SES | −1.00 | (−1.06. −0.94) | −0.50 | (−0.98, −0.02) |
| Medium SES | 0.00 | (−0.02, 0.02) | 0.50 | (0.08, 0.92) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 1.00 | (0.44, 1.56) | 4.50 | (3.81, 5.19) |
| Suburban | 1.00 | (0.97, 1.03) | 3.00 | (2.54, 3.46) |
| Urban (ref) | 0 | 0 | ||
| Model #1b†: Response time | Median | 90th Percentile | ||
| Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||
| Low SES | −1.00 | (−1.28. −0.72) | −0.75 | (−1.33, −0.17) |
| Medium SES | 0.00 | (−0.19, 0.19) | 0.25 | (−0.26, 0.76) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 0.00 | (−0.38, 0.38) | 4.00 | (2.90, 5.09) |
| Suburban | 1.00 | (0.79, 1.21) | 3.00 | (2.54, 3.46) |
| Urban (ref) | 0 | 0 | ||
| Model #2a*: Scene time | Median | 90th Percentile | ||
| Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||
| Low SES | 0.00 | (−0.07, 0.07) | −0.67 | (−1.35, 0.02) |
| Medium SES | 0.00 | (−0.07, 0.07) | 0.00 | (−0.62, 0.62) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 1.00 | (0.86, 1.14) | 2.33 | (1.38, 3.28) |
| Suburban | 0.00 | (−0.08, 0.08) | 0.67 | (0.08, 1.25) |
| Urban (ref) | 0 | 0 | ||
| Model #2b†: Scene time | Median | 90th Percentile | ||
| Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||
| Low SES | 0.11 | (−0.21, 0.42) | −0.50 | (−1.19, 0.19) |
| Medium SES | 0.27 | (−0.01, 0.56) | 0.17 | (−0.48, 0.81) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 1.02 | (0.63, 1.42) | 2.50 | (1.50, 3.50) |
| Suburban | 0.44 | (0.17, 0.71) | 0.83 | (0.18, 1.49) |
| Urban (ref) | 0 | 0 | ||
| Model #3a*: Transport time | Median | 90th Percentile | ||
| Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||
| Low SES | −3.33 | (−3.75, −2.92) | −3.00 | (−4.00, −2.00) |
| Medium SES | −1.00 | (−1.40, −0.60) | −2.00 | (2.69, −1.31) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 6.67 | (5.76, 7.58) | 16.00 | (14.53, 17.47) |
| Suburban | 4.67 | (4.19, 5.14) | 11.00 | (10.13, 11.87) |
| Urban (ref) | 0 | 0 | ||
| Model #3b†: Transport time | Median | 90th Percentile | ||
| Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||
| Low SES | −2.93 | (−3.37, −2.50) | −1.44 | (−2.49, −0.39) |
| Medium SES | −0.69 | (−1.12, −0.26) | −1.27 | (−1.96, −0.58) |
| High SES (ref) | 0 | 0 | ||
|
| ||||
| Rural | 7.13 | (6.23, 8.04) | 15.39 | (13.52, 17.26) |
| Suburban | 4.91 | (4.43, 5.39) | 11.13 | (10.23, 12.04) |
| Urban (ref) | 0 | 0 | ||
Demographics-adjusted models include main effects for tract SES, rurality, and patient age, gender, and race
Fully-adjusted models include main effects for tract SES, rurality; patient age, gender, and race; and time of day, weekend, duration of complaint, 9-1-1 dispatch complaint of stroke, and EMS provider primary impression
EMS indicates emergency medical services; and SES, socioeconomic status
Discussion
In this statewide study, we identified important differences in EMS prehospital time intervals for suspected acute stroke patients by community factors (i.e., SES and urban-rural status). Multivariable adjusted regression results suggest patient encounters within rural tracts experience longer transport times to the hospital compared to urban and suburban tracts whereas those patients in low SES tracts experience modestly shorter transport times compared to high SES tracts. Further, the 90th percentile EMS response and scene intervals were also longer in rural tracts versus urban tracts although differences were minimal and likely not clinically meaningful.
Disparities in stroke care and outcomes by rurality and SES are well documented (24, 37–40). Further, prior research found neighborhood-level geospatial clustering of stroke prevalence across the United States (41). Our findings highlight the important role of community factors in EMS time intervals for suspected stroke patients for large, diverse regions. Our results are comparable to the median EMS time intervals for suspected acute stroke patients reported by previous studies which range from 6 – 9 min for response interval, 13–20 min for scene interval, and 12 – 14 min for transport interval (22, 36, 42–44). Our findings conflict with Kleindorfer et al.’s (22) conclusion that poorer community SES is associated with longer response and transport interval, and decreased scene interval by EMS. In fact, our data revealed encounters within low SES communities had modestly shorter transport times compared to high SES communities. This observation may be explained by low SES tracts within urban areas that are closer to stroke-capable hospitals even though our regression estimates by community SES were adjusted for urban-rural status. Further, there may be inherent regional differences between our study conducted in NC and the study conducted by Kleindorfer et al. (22) which was conducted using data from the Greater Cincinnati metropolitan region. Lastly, Kleindorfer et al. (22) is based on 2006 data and may be less applicable as recent clinical advancements and updates to stroke care guidelines may have led to changes in EMS practices.
Interventions designed to mitigate the role of community socioeconomic deprivation and rurality in EMS prehospital times may improve the likelihood of acute stroke patients receiving time sensitive treatment and address health disparities. Even though the largest prehospital time difference by rurality was observed in EMS transport interval, it is likely due to longer distances to stroke-capable hospitals and NC EMS systems using stroke triage and destination plans (30). However, in our study, one-third of suspected stroke patients were still transported by EMS to a non-certified hospital. With further regionalization of acute stroke care and a trend towards routing potential large vessel occlusion strokes to thrombectomy-capable stroke centers, rural stroke patients may experience even longer prehospital delays. Rural communities may benefit from helicopter or fixed-wing transport by EMS to minimize transport times and reduce delays to stroke reperfusion therapies although the benefit of air medical services on stroke outcomes is not well-established (45). Addressing the modest urban-rural differences in scene time, arguably the most modifiable EMS time interval, through streamlined workflows may serve to decrease overall prehospital delays for rural stroke patients. Lastly, response times in rural and suburban tracts were modestly longer in our study, suggesting further optimization of ambulance station and unit placement might be needed in these communities. Additional research is needed on how EMS quality improvement, optimal resource allocation, and regionalization to improve acute stroke care and patient outcomes are influenced by community-level factors, especially in underserved areas.
Our study has some strengths and limitations to note. A major strength was the use of statewide data from a large and diverse region. The NCOEMS ensures data are collected in a standardized format from all EMS systems in the state. We had a very high match rate of geocoding incident addresses. Furthermore, our data were representative of all levels of community SES and urban-rural status. However, there are important limitations that must be considered. First, encounters missing data on inclusion variables (i.e., EMS provider impression, stroke protocol use) reduced the size of the study sample. Second, as this is a secondary analysis of the NC EMS Data System collected to evaluate and improve patient care and EMS system performance, there is an inherent potential for inaccurate or incomplete data, which we were not able to assess in this study. Also, by using existing data, we may not have been able to account for all potential sources of confounding, even though our demographics- and fully-adjusted models had similar results. Third, although the use of RUCA codes is an accepted method to characterize urbanicity, there are alternate methods to identify urbanicity (e.g., Urban Influence Codes, Census place or urban area designation, etc.) which may change the findings reported in this publication. Final patient diagnosis (e.g., stroke type, stroke mimic, etc.), and ways in which prehospital times correspond to treatment rates or patient outcomes were not available in these data. Lastly, our results are based on data from a single state, which may not be generalizable to other states or regions.
Conclusion
Our analysis of statewide EMS data revealed meaningful differences in EMS time intervals for suspected acute stroke patients by community factors. Urban-rural differences in EMS transport intervals were most pronounced whereas differences by community SES were modest. Findings from this study can inform future research exploring the role of community socioeconomic deprivation and rurality in contributing to delays in prehospital stroke care and develop EMS interventions to address rural-urban and SES stroke disparities.
Supplementary Material
Acknowledgements:
The NC OEMS and the NC EMS Data System supports state, regional and local EMS and healthcare related service delivery from a patient care, resource allocation, and regulatory perspective. This work has been reviewed by NC EMS Data System investigators for scientific content and consistency of data interpretation with previous NC EMS Data System publications and significant comments have been incorporated.
Funding:
Dr. Patel is supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through Grant KL2TR002490. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosure of Conflicts of Interests: The authors report there are no conflicts of interests to declare.
References:
- 1.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021;143(8):e254–e743. Epub 2021/01/28. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL. Time is brain--quantified. Stroke 2006;37(1):263–6. Epub 2005/12/13. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 3.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019;50(12):e344–e418. Epub 2019/10/31. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 4.Adams HP Jr., del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation 2007;115(20):e478–534. Epub 2007/05/23. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 5.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010;375(9727):1695–703. Epub 2010/05/18. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 6.Lansberg MG, Schrooten M, Bluhmki E, Thijs VN, Saver JL. Treatment time-specific number needed to treat estimates for tissue plasminogen activator therapy in acute stroke based on shifts over the entire range of the modified Rankin Scale. Stroke 2009;40(6):2079–84. Epub 2009/04/18. doi: 10.1161/STROKEAHA.108.540708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000;55(11):1649–55. Epub 2000/12/13. doi: 10.1212/wnl.55.11.1649. [DOI] [PubMed] [Google Scholar]
- 8.Bhaskar S, Stanwell P, Cordato D, Attia J, Levi C. Reperfusion therapy in acute ischemic stroke: dawn of a new era? BMC Neurol 2018;18(1):8. Epub 2018/01/18. doi: 10.1186/s12883-017-1007-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jahan R, Saver JL, Schwamm LH, Fonarow GC, Liang L, Matsouaka RA, et al. Association Between Time to Treatment With Endovascular Reperfusion Therapy and Outcomes in Patients With Acute Ischemic Stroke Treated in Clinical Practice. JAMA 2019;322(3):252–63. Epub 2019/07/17. doi: 10.1001/jama.2019.8286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aroor SR, Asif KS, Potter-Vig J, Sharma A, Menon BK, Inoa V, et al. Mechanical Thrombectomy Access for All? Challenges in Increasing Endovascular Treatment for Acute Ischemic Stroke in the United States. J Stroke 2022;24(1):41–8. Epub 2022/02/09. doi: 10.5853/jos.2021.03909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilcock AD, Schwamm LH, Zubizarreta JR, Zachrison KS, Uscher-Pines L, Richard JV, et al. Reperfusion Treatment and Stroke Outcomes in Hospitals With Telestroke Capacity. JAMA Neurol 2021;78(5):527–35. Epub 2021/03/02. doi: 10.1001/jamaneurol.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulder M, Jansen IGH, Goldhoorn RB, Venema E, Chalos V, Compagne KCJ, et al. Time to Endovascular Treatment and Outcome in Acute Ischemic Stroke: MR CLEAN Registry Results. Circulation 2018;138(3):232–40. Epub 2018/03/28. doi: 10.1161/CIRCULATIONAHA.117.032600. [DOI] [PubMed] [Google Scholar]
- 13.Fransen PS, Berkhemer OA, Lingsma HF, Beumer D, van den Berg LA, Yoo AJ, et al. Time to Reperfusion and Treatment Effect for Acute Ischemic Stroke: A Randomized Clinical Trial. JAMA Neurol 2016;73(2):190–6. Epub 2015/12/31. doi: 10.1001/jamaneurol.2015.3886. [DOI] [PubMed] [Google Scholar]
- 14.Adeoye O, Lindsell C, Broderick J, Alwell K, Jauch E, Moomaw CJ, et al. Emergency medical services use by stroke patients: a population-based study. Am J Emerg Med 2009;27(2):141–5. Epub 2009/04/18. doi: 10.1016/j.ajem.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018;49(3):e46–e110. Epub 2018/01/26. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 16.Saver JL, Fonarow GC, Smith EE, Reeves MJ, Grau-Sepulveda MV, Pan W, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013;309(23):2480–8. Epub 2013/06/20. doi: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- 17.Tong D, Reeves MJ, Hernandez AF, Zhao X, Olson DM, Fonarow GC, et al. Times from symptom onset to hospital arrival in the Get with the Guidelines--Stroke Program 2002 to 2009: temporal trends and implications. Stroke 2012;43(7):1912–7. Epub 2012/04/28. doi: 10.1161/STROKEAHA.111.644963. [DOI] [PubMed] [Google Scholar]
- 18.Mohammad YM. Mode of arrival to the emergency department of stroke patients in the United States. J Vasc Interv Neurol 2008;1(3):83–6. Epub 2008/07/01. [PMC free article] [PubMed] [Google Scholar]
- 19.Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes 2012;5(4):514–22. Epub 2012/07/13. doi: 10.1161/CIRCOUTCOMES.112.965210. [DOI] [PubMed] [Google Scholar]
- 20.Jauch EC, Saver JL, Adams HP Jr., Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44(3):870–947. Epub 2013/02/02. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 21.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehosp Emerg Care 2008;12(4):426–31. Epub 2008/10/17. doi: 10.1080/10903120802290828. [DOI] [PubMed] [Google Scholar]
- 22.Kleindorfer DO, Lindsell CJ, Broderick JP, Flaherty ML, Woo D, Ewing I, et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: do poorer patients have longer delays from 911 call to the emergency department? Stroke 2006;37(6):1508–13. Epub 2006/05/13. doi: 10.1161/01.STR.0000222933.94460.dd. [DOI] [PubMed] [Google Scholar]
- 23.Ader J, Wu J, Fonarow GC, Smith EE, Shah S, Xian Y, et al. Hospital distance, socioeconomic status, and timely treatment of ischemic stroke. Neurology 2019;93(8):e747–e57. Epub 2019/07/20. doi: 10.1212/WNL.0000000000007963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kapral MK, Fang J, Chan C, Alter DA, Bronskill SE, Hill MD, et al. Neighborhood income and stroke care and outcomes. Neurology 2012;79(12):1200–7. Epub 2012/08/17. doi: 10.1212/WNL.0b013e31826aac9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dwyer M, Rehman S, Ottavi T, Stankovich J, Gall S, Peterson G, et al. Urban-rural differences in the care and outcomes of acute stroke patients: Systematic review. Journal of the neurological sciences 2019;397:63–74. Epub 2018/12/30. doi: 10.1016/j.jns.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 26.Georgakakos PK, Swanson MB, Ahmed A, Mohr NM. Rural Stroke Patients Have Higher Mortality: An Improvement Opportunity for Rural Emergency Medical Services Systems. J Rural Health 2022;38(1):217–27. Epub 2020/08/07. doi: 10.1111/jrh.12502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glymour MM, Kosheleva A, Boden-Albala B. Birth and adult residence in the Stroke Belt independently predict stroke mortality. Neurology 2009;73(22):1858–65. Epub 2009/12/02. doi: 10.1212/WNL.0b013e3181c47cad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cline M Is North Carolina Rural or Urban? 2020. 04/04/2022. Available from: https://www.osbm.nc.gov/blog/2020/11/19/north-carolina-rural-or-urban.
- 29.Logan Rockefeller Harris AD. 2020. Poverty Report: Persistent poverty demands a just recovery for North Carolinians2020 04/04/2022 Available from: https://www.ncjustice.org/publications/2020-poverty-report-persistent-poverty-demands-a-just-recovery-for-north-carolinians/#:~:text=In%202019%2C%2013.6%20percent%20of,experience%20poverty%20during%20their%20lifetimes.
- 30.Asimos AW, Ward S, Brice JH, Enright D, Rosamond WD, Goldstein LB, et al. A geographic information system analysis of the impact of a statewide acute stroke emergency medical services routing protocol on community hospital bypass. J Stroke Cerebrovasc Dis 2014;23(10):2800–8. Epub 2014/10/09. doi: 10.1016/j.jstrokecerebrovasdis.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 31.NC Division of Health Service Regulation OoEMS. NC EMS Triage and Destination Plan Templates 2009. [updated 01/25/2021; cited 2022 04/26/2022]. Available from: https://www.ncems.org/triageanddestination.html.
- 32.Macdonald H The American Community Survey: Warmer (More Current), but Fuzzier (Less Precise) than the Decennial Census. Journal of the American Planning Association 2006;72(4):491–503. doi: 10.1080/01944360608976768. [DOI] [Google Scholar]
- 33.Bonito AJ BC, Eicheldinger C, Carpenter L. Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries. .Final Report [Google Scholar]
- 34.Austin PC, Schull MJ. Quantile regression: a statistical tool for out-of-hospital research. Acad Emerg Med 2003;10(7):789–97. Epub 2003/07/03. doi: 10.1111/j.1553-2712.2003.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 35.Do YK, Foo K, Ng YY, Ong ME. A quantile regression analysis of ambulance response time. Prehosp Emerg Care 2013;17(2):170–6. Epub 2012/12/12. doi: 10.3109/10903127.2012.729127. [DOI] [PubMed] [Google Scholar]
- 36.Patel MD, Brice JH, Moss C, Suchindran CM, Evenson KR, Rose KM, et al. An evaluation of emergency medical services stroke protocols and scene times. Prehosp Emerg Care 2014;18(1):15–21. Epub 2013/09/14. doi: 10.3109/10903127.2013.825354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gonzales S, Mullen MT, Skolarus L, Thibault DP, Udoeyo U, Willis AW. Progressive rural-urban disparity in acute stroke care. Neurology 2017;88(5):441–8. Epub 2017/01/06. doi: 10.1212/WNL.0000000000003562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shultis W, Graff R, Chamie C, Hart C, Louangketh P, McNamara M, et al. Striking rural-urban disparities observed in acute stroke care capacity and services in the pacific northwest: implications and recommendations. Stroke 2010;41(10):2278–82. Epub 2010/09/04. doi: 10.1161/STROKEAHA.110.594374. [DOI] [PubMed] [Google Scholar]
- 39.Koifman J, Hall R, Li S, Stamplecoski M, Fang J, Saltman AP, et al. The association between rural residence and stroke care and outcomes. Journal of the neurological sciences 2016;363:16–20. Epub 2016/03/24. doi: 10.1016/j.jns.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 40.Kapral MK, Wang H, Mamdani M, Tu JV. Effect of socioeconomic status on treatment and mortality after stroke. Stroke 2002;33(1):268–73. Epub 2002/01/10. doi: 10.1161/hs0102.101169. [DOI] [PubMed] [Google Scholar]
- 41.Dworkis DA, Marvel J, Sanossian N, Arora S. Neighborhood-level stroke hot spots within major United States cities. The American journal of emergency medicine 2020;38(4):794–8. [DOI] [PubMed] [Google Scholar]
- 42.Schwartz J, Dreyer RP, Murugiah K, Ranasinghe I. Contemporary Prehospital Emergency Medical Services Response Times for Suspected Stroke in the United States. Prehosp Emerg Care 2016;20(5):560–5. Epub 2016/03/10. doi: 10.3109/10903127.2016.1139219. [DOI] [PubMed] [Google Scholar]
- 43.Li T, Cushman JT, Shah MN, Kelly AG, Rich DQ, Jones CMC. Prehospital time intervals and management of ischemic stroke patients. Am J Emerg Med 2021;42:127–31. Epub 2020/02/16. doi: 10.1016/j.ajem.2020.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Heemskerk JL, Domingo RA, Tawk RG, Vivas-Buitrago TG, Huang JF, Rogers A, et al. Time Is Brain: Prehospital Emergency Medical Services Response Times for Suspected Stroke and Effects of Prehospital Interventions. Mayo Clin Proc 2021;96(6):1446–57. Epub 2021/03/15. doi: 10.1016/j.mayocp.2020.08.050. [DOI] [PubMed] [Google Scholar]
- 45.Tal S, Mor S. The impact of helicopter emergency medical service on acute ischemic stroke patients: A systematic review. The American Journal of Emergency Medicine 2021;42:178–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


