Abstract
Few studies have evaluated environmental factors that predict survival to old age. Our study included 913 African American participants in the Jackson Heart Study (JHS) who resided in the tri-county area of the Jackson, MS metropolitan area and were 65–80 years at baseline. Participants were followed from 2000 through 2019 for the outcome of survival to 85 years old. We evaluated each of the following census tract-level measures of the social/physical environment as exposures: socioeconomic status, cohesion, violence, disorder, healthy food stores, residential land use, and walkability. We assessed mediation by physical activity and chronic conditions. As a complementary ecologic analysis, we used census-tract data to examine factors associated with a greater life expectancy. A total of 501 (55%) JHS participants survived to age 85 years or older. Higher social cohesion and greater residential land use were modestly associated with survival to old age (risk difference = 25%, 95% CI: 0–49%; and 4%, 95% CI: 1–7%, respectively). These neighborhood effects were modestly mediated through leisure time physical activity; additionally, social cohesion was mediated through home and yard activity. In our ecologic analysis, a greater percentage of homeowners and a greater proportion of people living in partnered families were associated with higher census-tract level life expectancy. African American older adults living in residential neighborhoods or neighborhoods with high social cohesion were more likely to survive to old age.
Keywords: Aging, Longevity, Black/African-American, Neighborhood, Environment, Epidemiology, Mediation
1. Introduction
Estimates of life expectancy at birth vary by over 40 years between census tracts in the United States (Arias et al., 2018). Life expectancy is a measure of population health, and defined as the age a person born in a given year could expect to live to, if the average age of death did not change over their lifetime (Arias et al., 2018). Although there is growing interest in the role of the environment on disparities in aging outcomes, only a few studies have focused on life expectancy. One study in Texas found that the Neighborhood Potential Health Impact Score, which models the collective impact of several neighborhood-level determinants of health, was associated with greater life expectancy (Prochaska et al., 2020). A study in Florida observed that census tracts with higher proportions of residents who were either Hispanic, younger than five years, or older than 65 years had greater life expectancy; and census tracts where residents were less likely to own automobiles or more likely to live in mobile homes had relatively lower life expectancy (Melix et al., 2020). Another study in Chicago found that greater proportion of African American residents and lower median household income were associated with lower life expectancy (Hunt et al., 2015). In this manuscript, the terms (non-Hispanic) Black and African American will be used interchangeably, and according to the source being referenced.
Survival to old age is an outcome distinct from life expectancy or mortality rate and represents a marker of healthy aging (Odden et al., 2022). Furthermore, by focusing on survival to old age, attention is directed towards aging-related assets and promotors. Average life expectancy can mask population-level differences in age at death, depending on when excess death peaks during the life course. For example, despite having different mortality distributions, a population with both high premature and older adult mortality could have a similar life expectancy as a population with mortality rates that peak at midlife. Moreover, factors that are associated with survival in midlife and early old age may not be associated with survival to very old age (Odden et al., 2014). Thus, survival to old age is an outcome that is distinct from life expectancy or mortality rate, and represents a unique marker of healthy aging.
Current and historical structural racism has shaped differences in the racial and ethnic composition of geographic regions and exacerbated spatial health inequities (Williams and Collins, 2001). Black people disproportionately reside in disadvantaged environments compared with White people in the U.S. Nonetheless, many Black people are able to thrive, in spite of the racist history, policies, and environmental differences of the U.S (Bailey et al., 2017, Williams and Collins, 2001). This likely represents a complex combination of self-efficacy and interpersonal, socioeconomic, and environmental resources. In this study, we focus on the environment and related contextual factors as resources that may help support healthy aging among Black and African American people, with the goal of informing urban planning and policies that have the potential to support more equitable environments.
In this investigation, we evaluated neighborhood-level factors and survival to old age in the Jackson Heart Study (JHS). The goal of this study was exploratory; we examined a variety of neighborhood factors that were derived in the JHS Neighborhood Environment study and captured neighborhood socioeconomic status, conditions, food resources, and the built environment. These variables capture differences in neighborhood disadvantage as well as the contextual factors associated with these environments (Barber et al., 2016b). Few studies in this research area have evaluated causal mechanisms that link environmental factors to survival to older age. Therefore, we evaluated potential individual-level mediators between neighborhood measures and survival to old age to better understand the mechanisms linking the neighborhood to longevity. We explored physical activity and chronic conditions as mediators, as these factors can be influenced by the neighborhood environment (Barber et al., 2016a, Barber et al., 2016c, Chamberlain et al., 2020, Gebreab et al., 2017, Keats et al., 2020, Robinson et al., 2016). We complement this analysis and provide triangulation in evidence by evaluating census-tract level measures and life-expectancy estimates. A better understanding of factors that promote survival into old age could inform strategies that support healthy aging in African American communities.
2. Methods
The JHS is a community-based cohort study of African American adults in Jackson, MS, designed to investigate the causes of cardiovascular disease; details have been published (Keku et al., 2005). JHS recruited 5,306 African American men and women aged 21 years and older, living in the tri-county (Hinds, Madison, and Rankin) area of the Jackson metropolitan area. The baseline exam was conducted in 2000–2004 and included questionnaires, interviews, biospecimen collection, and a physical exam. Participant addresses were geocoded to generate the neighborhood-level measures. Two follow-up visits were conducted during 2005–2008 and 2009–2013, and a fourth exam is underway. Annual follow-up telephone calls were administered to collect data on health status and cardiovascular events. Vital status of participants was ascertained through annual follow-up interviews, death records from the Mississippi State Health Department, obituaries, and the National Death Index. The study was approved by the Institutional Review Boards of the University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided written informed consent.
Our study sample was restricted to the 913 participants born between 1923 and 1934 (aged 65–80 years at baseline) to minimize birth cohort effects and to ensure that participants had the opportunity to reach age 85 years, our outcome of interest, by the censor date of Dec. 31st, 2019. Although survival to age 90 has been used as an outcome of interest in other research (He and Muenchrath, 2011), there was a smaller number of JHS participants who had the opportunity to reach age 90 years at the time of this study (n = 629).
We also used census tract data from the 2015 American Community Survey (2011–2015) in the tri-county area of the Jackson metropolitan area. The goal of this analysis was to triangulate thematic findings from the individual level analysis. We explored two census tract-level predictor variables selected based on our strongest findings in the JHS cohort in the present study: proportion of homeownership and proportion of cohabitation status (married/partnered, family, other family, other non-family, living alone). We linked these data to life expectancy estimates by census tract for the period of 2010–2015. These estimates were derived from the Small-area Life Expectancy Estimates Project (Tejada-Vera et al., 2020). These data were averaged by census tract and therefore inclusive of residents of all racial/ethnic identities.
2.1. Neighborhood measures
The following measures were derived from the JHS Neighborhood Environment ancillary study and were selected based on study recommendations (Diez Roux, 2015). The neighborhood socioeconomic environment was derived using exploratory factor analysis based on 2000 U.S. Census-tract level measures of education, occupation, and income (Wang et al., 2017). Census tracts are small, relatively permanent statistical subdivisions of a county, and contain on average 4,000 residents. We followed the JHS Neighborhood study recommendations and selected the factor that included the following variables loaded to 60% (all reverse coded): percent of persons 25 + with at least a Bachelor’s degree, percent of persons with managerial/professional occupation, median owner value of households, percent persons 25 + with at least a high school diploma, percent of households with interest, dividend, or rental income, median household income (reverse coded), percent of household income >$50,000 (Diez Roux, 2015).
The JHS neighborhood survey data includes variables that capture features of the neighborhoods derived from a series of questions administered to JHS participants during follow-up exams between 2004 and 2008 (Barber et al., 2016c, Wang et al., 2017). Principal component analysis showed that the items could be grouped into domains which correspond to three identified constructs: social cohesion, violence, and neighborhood disorder (Mujahid et al., 2007). The internal consistencies for the three scales were adequate, with Cronbach’s alpha 0.77, 0.80, and 0.76 for neighborhood social cohesion, violence and disorder, respectively. The responses of all JHS participants reporting on the same census tract (used to proxy neighborhood) were averaged together, and empirical Bayes estimates were used to calculate scores (Mujahid et al., 2007).
The physical environment was assessed by favorable food stores, percent residential land use, and walkability (Besser et al., 2021). Favorable food stores were defined as supermarkets or fruit and vegetable markets, using a 1-mile kernel density (Walls and Associates, 2011). Land use was coded as residential, retail, and commercial, and defined using a 1-mile buffer from a participant’s residence. We used the network ratio within 1 mile to evaluate the walkability of a neighborhood. This measure of street connectivity is defined as the proportion of the total area that can be accessed through connected streets (Besser et al., 2021).
2.2. Other measures
Age, gender, educational attainment (<high school; high school or equivalent; trade school, vocational school, or college), occupation (management/professional, sales, military, retired, and student versus service, farming, construction, production, and sick), and insurance status were self-reported at baseline. Self-reported income status was derived from family size and calendar-year-specific poverty level (“poor,” “lower-middle,” “higher-middle,” and “affluent”). Self-reported smoking was categorized based on American Heart Association’s Life’s Simple 7 criteria: “poor” (current smokers), “intermediate” (quit < 12 months ago), and “ideal” (quit 12 months or more ago or never). The JHS physical activity questionnaire was used to generate the “sport index”, “home/yard index” and “active living index”, as measures of weekly sports activities, home and yard activity, and leisure-time physical activity (range: 1 = low to 5 = high) (Smitherman et al., 2009). Perceived discrimination was assessed by the frequency of everyday and lifetime subscales of the JHS Discrimination Instrument (Sims et al., 2009). Depressive symptoms were assessed by the 20-item Center for Epidemiological Studies-Depression questionnaire (range 0–60) (Radloff and Rae, 1979). The Global Perceived Stress Scale was created for the JHS and adapted from standardized stress scales (Whitfield et al., 2014). The conceptual model guiding the development and implementation of the sociocultural methods in JHS has been described previously (Payne et al., 2005).
Body mass index was calculated as [weight (kg) / height (m)2]. Systolic and diastolic blood pressure were derived from the mean of two sitting readings, separated by one minute. Hemoglobin A1c was standardized using the NGSP protocol. Lipid panel readings provided fasting high- and low-density lipoprotein cholesterol and triglycerides. Renal function was derived from the Chronic Kidney Disease Epidemiology Collaboration creatinine equation for estimated glomerular filtration rate (eGFR), that includes sex, race, and age. This was selected to be consistent with prior JHS publications, although we note race-free equations are now recommended. Type 2 diabetes was assessed based on the American Diabetes Association 2010 criteria or use of medication (American Diabetes, 2010). Hypertension was defined as blood pressure greater than 140/90 mmHg or use of medication (Chobanian et al., 2003). History of stroke, coronary heart disease, and heart failure events were adjudicated based on medical records for hospitalizations. History of lung disease, cardiac procedures, and cancer were assessed annually on phone calls by self-report. Current medication status was confirmed by participants bringing in prescriptions and/or self-reported taking medication within the two weeks preceding the exam.
2.3. Statistical analysis
We compared baseline characteristics between participants who did not and did survive to age 85 years. Chi-square tests were used to assess differences in categorical variables and t-tests or Mann-Whitney U tests were used to assess differences in continuous variables.
We first modeled the outcome of survival to age 85 years, using binomial regression adjusted for age, age-squared (to allow for a non-linear age association), gender, income, occupation and education. These variables were selected as potential confounders of the neighborhood variables and survival to old age. We next fit an exploratory model that included smoking status, home/yard index, active living index, total global stress score, body mass index, systolic blood pressure, total cholesterol, eGFR, history of hypertension, diabetes, stroke, coronary heart disease, cardiac procedure, chronic lung disease, and cancer. These variables could be conceptualized as either confounders or mediators as they could be in the causal pathway between the neighborhood level factors and survival to old age, the variables were selected as those that differ between survival groups at the p < 0.1 level.
We conducted causal mediation analysis for the two neighborhood environment variables that were significant in the demographic-adjusted models. Causal mediation allows for the potential values of the mediator and outcome to be estimated under the different levels of exposure (Lee et al., 2019, VanderWeele, 2014). We separately tested whether the effect of the dichotomized neighborhood variables was mediated by individual-level factors including home/yard index, active living index, and total diagnoses (hypertension, diabetes, stroke, heart failure, coronary heart disease, cardiac procedures, cancer, chronic lung disease). We estimate the total effect, the controlled direct effect (the effect of the exposure in the absence of the mediator), and the pure indirect effect (mediated effect) (VanderWeele, 2014).
As a complementary census-tract level analysis, we evaluated proportion of homeownership and cohabitation status (married/partnered family, other family, other non-family, living alone) with life expectancy estimates in the tri-county area of Jackson, MS.
All analyses were performed using Stata, 15.0 (College Station, TX).
3. Results
Age at baseline was higher in the group who survived to 85 years or older, and the proportion of participants who were female and overweight were also higher in this group than in those who did not survive to 85 years (Table 1). The proportion of participants who did not smoke and report higher stress were also greater in the group who survived to 85 years or older. Home/yard and leisure-time physical activity, cholesterol, and eGFR were all higher among those who survived to 85 years, and systolic blood pressure was lower in this group than in those who did not survive to 85 years. The prevalence of hypertension, diabetes, stroke, coronary heart disease, cardiac procedures, chronic lung disease, and cancer were higher in those who survived to age 85 years than in those who died before 85 years. Among the neighborhood measures, only percent residential land use was greater among those who survived to 85 years or older.
Table 1.
Jackson Heart Study (Jackson, MS) Participant Characteristics at Baseline, 2000–2004.
| Did not survive to 85 years N = 412 |
Survived to 85 years N = 501 |
P-value* | |
|---|---|---|---|
| N (%) or mean (SD) | |||
| Age at visit 1 (years) | 71.1 (3.4) | 72.4 (3.2) | <0.001 |
| Birth year (%) | <0.001 | ||
| 1923–1925 | 41 (10.0) | 90 (18.0) | |
| 1926–1928 | 83 (20.2) | 120 (24.0) | |
| 1929–1931 | 100 (24.3) | 151 (30.1) | |
| 1932–1934 | 188 (45.6) | 140 (27.9) | |
| Female (%) | 236 (57.3) | 372 (74.3) | <0.001 |
| Income (%) | 0.640 | ||
| Poor | 82 (19.9) | 80 (16.0) | |
| Lower middle | 133 (32.3) | 165 (32.9) | |
| Upper middle | 74 (18.0) | 95 (19.0) | |
| Affluent | 63 (15.3) | 81 (16.2) | |
| Missing | 60 (14.6) | 80 (16.0) | |
| Education (%) | 0.238 | ||
| < High school | 189 (45.9) | 199 (39.7) | |
| High school grad | 77 (18.7) | 109 (21.8) | |
| Attended vocational school, trade school or college | 143 (34.7) | 191 (38.1) | |
| Missing | 3 (0.7) | 2 (0.4) | |
| Insured (%) | 404 (98.1) | 489 (97.6) | 0.811 |
| Occupation (%) | |||
| Professional | 258 (62.6) | 285 (56.9) | 0.151 |
| Labor | 154 (37.4) | 215 (42.9) | |
| Missing | 0 | 1 (0.2) | |
| Body mass index (%) | 0.034 | ||
| Normal | 69 (16.8) | 79 (15.8) | |
| Underweight | 4 (1.0) | 0 (0) | |
| Overweight | 142 (34.5) | 188 (37.5) | |
| Obese | 193 (46.8) | 234 (46.7) | |
| Missing | 4 (1.0) | 0 (0) | |
| Alcohol drinking in past 12 months (%) | 113 (27.4) | 130 (26.0) | 0.487 |
| Smoking categorization (%) | <0.001 | ||
| Current smoker | 44 (10.7) | 17 (3.4) | |
| Quit < 12 months ago | 7 (1.7) | 1 (0.2) | |
| Never smoked or quit 12 + mths ago | 351 (85.2) | 474 (94.6) | |
| Missing | 10 (2.4) | 9 (1.8) | |
| Sport index | 1.89 (1.18) | 1.99 (1.29) | 0.378 |
| Home/yard index | 2.03 (0.59) | 2.23 (0.59) | <0.001 |
| Active living index | 1.82 (0.79) | 1.96 (0.84) | 0.016 |
| Everyday Discrimination | 1.70 (0.89) | 1.73 (0.81) | 0.109 |
| Lifetime Discrimination | 2.18 (1.85) | 2.37 (1.94) | 0.165 |
| Depression symptom score (n = 505) | 10.29 (7.02) | 11.04 (6.89) | 0.118 |
| Total global stress score | 2.80 (3.27) | 3.42 (3.58) | 0.006 |
| Systolic blood pressure (mmHg) | 135.79 (18.45) | 132.98 (17.12) | 0.023 |
| Diastolic blood pressure (mmHg) | 72.17 (9.24) | 72.34 (8.02) | 0.615 |
| Hemoglobin A1c (%) | 6.21 (1.27) | 6.10 (1.14) | 0.228 |
| Total cholesterol (mg/dL) | 201.00 (42.28) | 207.03 (38.82) | 0.036 |
| eGFR (ml/min/1.73 m2) (%) | <0.001 | ||
| 90+ | 119 (28.9) | 175 (34.9) | |
| 60–89 | 191 (46.4) | 261 (52.1) | |
| 30–59 | 78 (18.9) | 51 (10.2) | |
| 15–29 | 8 (1.9) | 3 (0.6) | |
| <15 | 8 (1.9) | 1 (0.2) | |
| Missing | 8 (1.9) | 10 (2.0) | |
| eGFR (ml/min/1.73 m2) | 74.08 (23.33) | 80.10 (17.26) | 0.002 |
| Hypertension status (%) | 347 (84.2) | 394 (78.6) | 0.032 |
| Diabetes status (%) | 159 (38.6) | 153 (30.5) | 0.038 |
| Stroke (%) | 50 (12.1) | 35 (7.0) | 0.008 |
| Coronary heart disease (%) | 72 (17.5) | 49 (9.8) | 0.001 |
| Cardiac procedures (%) | 71 (17.2) | 41 (8.2) | <0.001 |
| Chronic heart failure (%) | 15 (3.6) | 26 (5.2) | 0.261 |
| Chronic lung disease (%) | 32 (7.8) | 30 (6.0) | <0.001 |
| Cancer (%) | 52 (12.6) | 42 (8.4) | <0.001 |
| Census tract socioeconomic score | 0.81 (0.55) | 0.79 (0.54) | 0.274 |
| Neighborhood problems | 1.64 (0.16) | 1.63 (0.17) | 0.078 |
| Neighborhood social cohesion | 2.98 (0.13) | 3.00 (0.12) | 0.094 |
| Neighborhood violence | 1.31 (0.11) | 1.30 (0.12) | 0.085 |
| Favorable food store | 0.35 (0.21) | 0.35 (0.20) | 0.844 |
| Percent residential land use per square mile | 0.30 (0.10) | 0.32 (0.09) | 0.048 |
| Network Ratio (Street connectivity) | 0.33 (0.12) | 0.33 (0.12) | 0.824 |
*p values are based on t test or Mann-Whitney U test for continuous variables and Chi square test for categorical variables.
Abbreviation: eGFR: estimated glomerular filtration rate.
In models adjusted for age, gender, income, education, and occupation, neighborhood social cohesion and percent residential land use were associated with a greater likelihood of surviving to age 85 years or older; risk difference = 0.25 (95% CI: 0.00, 0.49, p = 0.05) per 1-point greater social cohesion and 0.04 (95% CI: 0.01, 0.07, p = 0.008) per 10% greater residential land use (Table 2). Census-tract SES disadvantage, neighborhood problems, neighborhood violence, favorable food stores, and network ratio were not associated with survival to 85 years after adjustment. There were no differences by gender. Further adjustment for additional potentially mediating health variables attenuated these relationships, and the associations of percent residential land use and social cohesion with survival to old age no longer reached statistical significance (Supplemental Table 1).
Table 2.
Demographic-adjusted association of neighborhood-level variables and survival to age 85 years among participants in the Jackson Heart Study (Jackson, MS), 2000–2019.
| Demographic Adjusted* Risk Difference (95 %CI) | |
|---|---|
| Census tract SES disadvantage score | −0.01 (-0.06, 0.05) |
| Neighborhood problems | −0.17 (-0.35, 0.02) |
| Neighborhood social cohesion | 0.25 (0.00, 0.49) |
| Neighborhood violence | −0.18 (-0.45, 0.09) |
| Favorable food store | 0.00 (-0.15, 0.14) |
| Percent residential land use per square mile (per 10%) | 0.04 (0.01, 0.07) |
| Network ratio | 0.06 (-0.19, 0.31) |
*Binomial model adjusted for age, age-squared, gender, income, education, occupation.
In causal mediation analyses, total effect sizes ranged from 4 to 5% for the difference in the 75% vs. 25% percentile of residential land use and social cohesion. Active living index appeared to have a modest although not statistically significant indirect effect mediating the relationships between both percent residential land use and social cohesion and survival to 85 years or older (risk difference = 0.005, 95% CI: −0.001, 0.010, p = 0.09 and 0.005, 95% CI: −0.001, 0.011, p = 0.09, respectively) (Table 3, Table 4). Home and yard activity had an indirect effect of 0.010 (95% CI: 0.001, 0.018, p = 0.03) for the relationship of social cohesion and survival to age 85 years or older (Table 4).
Table 3.
Mediation analyses for the relationship between percent residential land use per square mile (75th vs. 25th percentile) and survival to age 85 years or older, including indirect effects through active living index, home/yard index, global stress, and number of chronic conditions, among Jackson Heart Study participants (Jackson, MS), 2000–2019.
| Mediator | Total Effect Risk Difference* (95% CI) | Controlled Direct Effect Risk Difference* (95% CI) | Pure Indirect Effect Risk Difference* (95% CI) |
|---|---|---|---|
| Active living index | 0.048 (0.009, 0.088) | 0.044 (0.004, 0.083) | 0.005 (-0.001, 0.010) |
| Home/yard index | 0.046 (0.007, 0.086) | 0.047 (0.008, 0.086) | 0.000 (-0.007, 0.006) |
| Total number of chronic conditions** | 0.049 (0.010, 0.088) | 0.048 (0.009, 0.086) | 0.002 (-0.006, 0.010) |
*Linear regression models for both mediator and outcome adjusted for age, age-squared, gender, income, education, and occupation.
**Total number of chronic conditions includes hypertension, diabetes, stroke, heart failure, coronary heart disease, cardiac procedures, cancer, chronic lung disease.
Table 4.
Mediation analyses for the relationship between neighborhood social cohesion (75th vs. 25th percentile) and survival to age 85 years or older, including indirect effects through active living index, home/yard index, global stress, and number of chronic conditions, among Jackson Heart Study participants (Jackson, MS), 2000–2019.
| Mediator | Total Effect Risk Difference (95% CI) | Controlled Direct Effect Risk Difference (95% CI) | Pure Indirect Effect Risk Difference (95% CI) |
|---|---|---|---|
| Active living index | 0.043 (-0.002, 0.088) | 0.037(-0.007, 0.082) | 0.005 (-0.001, 0.011) |
| Home/yard index | 0.042 (-0.003, 0.087) | 0.031 (-0.013, 0.076) | 0.010 (0.001, 0.018) |
| Total number of chronic conditions | 0.044 (-0.001, 0.088) | 0.045 (0.001, 0.089) | −0.001 (-0.008, 0.005) |
*Linear regression models for both mediator and outcome adjusted for age, age-squared, gender, income, education, and occupation.
**Total number of chronic conditions includes hypertension, diabetes, stroke, heart failure, coronary heart disease, cardiac procedures, cancer, chronic lung disease.
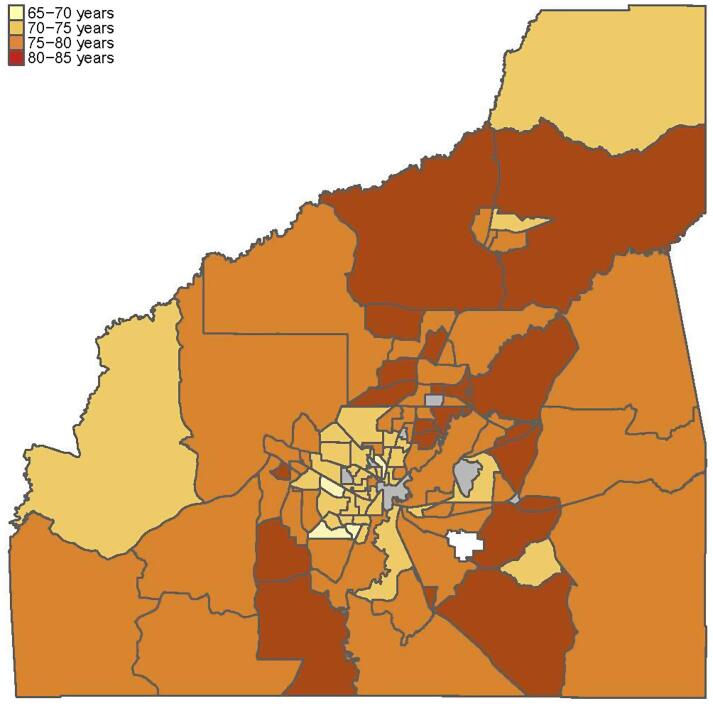
Life expectancy estimates varied from 67.8 to 85 years by census tract in the tri-county area of the Jackson, MS metropolitan area (Fig. 1). In ecologic analyses, a greater percentage of home ownership was associated with greater life expectancy at the tract level. A 10% higher tract percentage of homeowners was associated with a 1.0 (95% CI: 0.56, 1.45) year greater life expectancy in the tract. Compared to residents who live in married/partnered households, a 10% greater tract percentage of people cohabitating with other family members was associated with a −2.0 (95% CI: −4.6, −1.6) year lower life expectancy; a 10% greater tract percentage of people living alone was associated with a −0.9 (95% CI: −1.5, −0.3) year lower life expectancy. The proportion of people living with non-family members was not statistically significantly associated with life expectancy (-0.9 years, 95% CI: −3.0, 1.1).
Fig. 1.
Life expectancy among residents in the Jackson metropolitan area varies by over 17 years from 85 years in census tract 0301.04 in Madison County to 67.8 years in Census tract 0011.00 in Hinds County, 2010–2015.
4. Discussion
In this study of older African American adults, we found that neighborhood social cohesion and percent residential land use had a small association with survival to age 85 years. These associations were mediated modestly by leisure-time activity and activity while performing house- and yardwork. Although effect sizes were small, the ubiquitous nature of the exposures suggests that favorable neighborhood environments have the potential to support health and longevity. These observed effects may be driven, in part, by greater engagement in physical activity. We complemented this analysis by an ecologic study at the census-tract level that found greater home ownership and proportion of those living in partnered family households were associated with greater life expectancy. Our research adds to a growing body of literature that demonstrates the importance of the neighborhood environment for healthy aging.
In previous research, land use has been conceptualized as an aspect of the walkability of an environment, as greater retail land use or mixed-use land can provide increased opportunities for walking (Frank et al., 2010, Hirsch et al., 2013, Todd et al., 2016). Contrary to our expectations, we found that residential land use was associated with greater likelihood of survival to old age. In communities where destination walking is not the norm, as is true for a large part of the American South, land use mix may represent a different construct than in areas where destination walking is common. Compared to areas with more retail amenities, residential land use may improve neighborhood quality via the built environment as well as social connectivity.
The hypothesis that social connectivity may be a key factor is supported by the finding that greater social cohesion was associated with increased longevity. Previous investigations in the JHS have found that greater neighborhood social cohesion is associated with lower incidence of diabetes (Gebreab et al., 2017), risk of smoking (Wang et al., 2017), and cumulative biologic risk among those residing in neighborhoods with high levels of disadvantage (Barber et al., 2016a). A 2012 systematic review noted a consistent association between greater social cohesion and lower mortality (Meijer et al., 2012), yet we are aware of no prior studies that have evaluated survival to old age.
We observed modest evidence of mediation through leisure-time physical activity and home/yard activity for the relationships between residential land use and social cohesion with longevity. Residential land use could support physical activity through features that promote walking such as the presence of sidewalks, speed bumps, and crosswalks (Sallis et al., 2015). Substantial research has demonstrated that features of the built environment can facilitate older adults’ engagement in incidental and formal physical activity (Barnett et al., 2017). Health behaviors are often socially patterned, and greater social resources could positively influence activity patterns through healthy social norms, greater health information access, self-efficacy, and lower distress (McNeill et al., 2006, Samuel et al., 2015). A previous investigation in the Multi-Ethnic Study of Atherosclerosis found that greater neighborhood social cohesion was associated with walking for exercise (Echeverria et al., 2008). Social cohesion additionally appeared to act through home/yard activities, which could be due to an increased sense of community pride and desire to be a good neighbor.
Our study adds to the literature regarding the importance of the physical and social environment for older adult longevity. Moreover, we study an African American population in a Southern metropolitan area, a population that has been underrepresented in healthy aging research. Nonetheless, our study has limitations that should be considered when interpreting the findings. This hypothesis-generating study explored multiple neighborhood-level exposures, which are subject to multiple comparisons. Given that our study aimed to serve as an exploratory analysis rather than a confirmatory one, we followed the approach advocated by some experts in the field, opting to present the confidence intervals to offer readers a contextual reference point (Greenland, 2021, Rothman, 1990). We used triangulation of evidence to support our findings, nonetheless further studies are needed. Further studies using built environmental audits or additional participant questionnaires may better evaluate how the residential environment supports healthy aging. JHS participants were in midlife at enrollment; therefore, the majority have not had the opportunity to reach age 85 years even less have had the opportunity to reach age 90 years. This resulted in a modest sample size which likely also contributed to the limited precision of many of the estimates. Further investigation of survival to old age should be conducted when the population has aged. Finally, the modest evidence for mediation suggests that there are unmeasured pathways that contribute to the relationship between the neighborhood measures and survival to old age.
In summary, JHS participants who lived in residential neighborhoods with high social cohesion were more likely to survive to old age than those who did not. This study contributes to the evidence that structural inequalities and lack of access to neighborhood communities could worsen aging outcomes. Interventions to promote longevity and healthy aging should consider factors at the neighborhood and community-level as foundational to healthy aging.
5. Study support
This study was funded by R01-AG071019. HAM was funded by K99HL161479. The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I) and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD). The authors also wish to thank the staff and participants of the JHS.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
CRediT authorship contribution statement
Michelle C. Odden: Conceptualization, Methodology, Writing – original draft, Supervision, Funding acquisition. Yongmei Li: Methodology, Software, Formal analysis, Writing – review & editing. Roland J. Thorpe: Writing – review & editing. Annabel Tan: Software, Visualization, Writing – review & editing. Kendra Sims: Writing – review & editing. Jourdan Ratcliff: Data curation, Writing – review & editing. Hoda Abdel Magid: Writing – review & editing. Mario Sims: Investigation, Resources, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102360.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias, E., Escobedo, L.A., Kennedy, J., Fu, C., Cisewski, J., 2018. U.S. small-area life expectancy estimates project: Methodology and results summary, in: Statistics, N.C.f.H. (Ed.), Vital Health Stat, Hyattsville, Maryland. [PubMed]
- Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Barber S., Hickson D.A., Kawachi I., Subramanian S.V., Earls F. Double-jeopardy: The joint impact of neighborhood disadvantage and low social cohesion on cumulative risk of disease among African American men and women in the Jackson Heart Study. Soc. Sci. Med. 2016;153:107–115. doi: 10.1016/j.socscimed.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S., Hickson D.A., Kawachi I., Subramanian S.V., Earls F. Neighborhood Disadvantage and Cumulative Biological Risk Among a Socioeconomically Diverse Sample of African American Adults: An Examination in the Jackson Heart Study. J. Racial Ethn. Health Disparities. 2016;3(3):444–456. doi: 10.1007/s40615-015-0157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S., Hickson D.A., Wang X.u., Sims M., Nelson C., Diez-Roux A.V. Neighborhood Disadvantage, Poor Social Conditions, and Cardiovascular Disease Incidence Among African American Adults in the Jackson Heart Study. Am. J. Public Health. 2016;106(12):2219–2226. doi: 10.2105/AJPH.2016.303471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett, D.W., Barnett, A., Nathan, A., Van Cauwenberg, J., Cerin, E., Council on, E., Physical Activity - Older Adults working, g., 2017. Built environmental correlates of older adults' total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 14:103. [DOI] [PMC free article] [PubMed]
- Besser, L.M., Chang, L.C., Hirsch, J.A., Rodriguez, D.A., Renne, J., Rapp, S.R., Fitzpatrick, A.L., Heckbert, S.R., Kaufman, J.D., et al., 2021. Longitudinal Associations between the Neighborhood Built Environment and Cognition in US Older Adults: The Multi-Ethnic Study of Atherosclerosis. Int J Environ Res Public Health 18. [DOI] [PMC free article] [PubMed]
- Census Tracts, in: Branch, U.S.C.B.G.P. (Ed.).
- Chamberlain A.M., Finney Rutten L.J., Wilson P.M., Fan C., Boyd C.M., Jacobson D.J., Rocca W.A., St Sauver J.L. Neighborhood socioeconomic disadvantage is associated with multimorbidity in a geographically-defined community. BMC Public Health. 2020;20:13. doi: 10.1186/s12889-019-8123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian A.V., Bakris G.L., Black H.R., Cushman W.C., Green L.A., Izzo J.L., Jones D.W., Materson B.J., Oparil S., Wright J.T., Roccella E.J. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Diez Roux, A.V., 2015. Jackson Heart Study Neighborhood Environment Variable Summary and Recommendation Jackson Heart Study.
- Echeverría S., Diez-Roux A.V., Shea S., Borrell L.N., Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2008;14(4):853–865. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Frank L., Kerr J., Rosenberg D., King A. Healthy aging and where you live: community design relationships with physical activity and body weight in older Americans. J. Phys. Act. Health. 2010;7(Suppl 1):S82–S90. doi: 10.1123/jpah.7.s1.s82. [DOI] [PubMed] [Google Scholar]
- Gebreab S.Y., Hickson D.A., Sims M., Wyatt S.B., Davis S.K., Correa A., Diez-Roux A.V. Neighborhood social and physical environments and type 2 diabetes mellitus in African Americans: The Jackson Heart Study. Health Place. 2017;43:128–137. doi: 10.1016/j.healthplace.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Analysis goals, error-cost sensitivity, and analysis hacking: Essential considerations in hypothesis testing and multiple comparisons. Paediatr. Perinat. Epidemiol. 2021;35(1):8–23. doi: 10.1111/ppe.12711. [DOI] [PubMed] [Google Scholar]
- He W., Muenchrath M.N. In: American Community Survey Reports. Bureau U.S.C., editor. Washington D.C; 2011. 90+ in the United States: 2006–2008. [Google Scholar]
- Hirsch J.A., Diez Roux A.V., Rodriguez D.A., Brines S.J., Moore K.A. Discrete land uses and transportation walking in two U.S. cities: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2013;24:196–202. doi: 10.1016/j.healthplace.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt B.R., Tran G., Whitman S. Life Expectancy Varies in Local Communities in Chicago: Racial and Spatial Disparities and Correlates. J. Racial Ethn. Health Disparities. 2015;2(4):425–433. doi: 10.1007/s40615-015-0089-8. [DOI] [PubMed] [Google Scholar]
- Keats, M.R., Cui, Y., DeClercq, V., Grandy, S.A., Sweeney, E., Dummer, T.J.B., 2020. Associations between Neighborhood Walkability, Physical Activity, and Chronic Disease in Nova Scotian Adults: An Atlantic PATH Cohort Study. Int J Environ Res Public Health 17. [DOI] [PMC free article] [PubMed]
- Keku, E., Rosamond, W., Taylor, H.A., Jr., Garrison, R., Wyatt, S.B., Richard, M., Jenkins, B., Reeves, L., Sarpong, D., 2005. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis 15:S6-62-70. [PubMed]
- Lee H., Herbert R.D., McAuley J.H. Mediation Analysis. JAMA. 2019;321:697–768. doi: 10.1001/jama.2018.21973. [DOI] [PubMed] [Google Scholar]
- McNeill L.H., Kreuter M.W., Subramanian S.V. Social environment and physical activity: a review of concepts and evidence. Soc Sci Med. 2006;63(4):1011–1022. doi: 10.1016/j.socscimed.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Meijer M., Röhl J., Bloomfield K., Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- Melix B.L., Uejio C.K., Kintziger K.W., Reid K., Duclos C., Jordan M.M., Holmes T., Joiner J. Florida neighborhood analysis of social determinants and their relationship to life expectancy. BMC Public Health. 2020;20:632. doi: 10.1186/s12889-020-08754-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid M.S., Diez Roux A.V., Morenoff J.D., Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am. J. Epidemiol. 2007;165:858–867. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- Odden M.C., Shlipak M.G., Whitson H.E., Katz R., Kearney P.M., defilippi C., Shastri S., Sarnak M.J., Siscovick D.S., Cushman M., Psaty B.M., Newman A.B. Risk factors for cardiovascular disease across the spectrum of older age: the Cardiovascular Health Study. Atherosclerosis. 2014;237(1):336–342. doi: 10.1016/j.atherosclerosis.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odden M.C., Sims K.D., Newman A.B. In: Hazzard's Geriatric Medicine and Gerontology. 8th ed. Halter J., Ouslander J., Studenski S., High K., Supiano M., Ritchie C.S., Schmader K., editors. McGraw Hill; San Francisco: 2022. Demography and Epidemiology; pp. 23–46. [Google Scholar]
- Payne, T.J., Wyatt, S.B., Mosley, T.H., Dubbert, P.M., Guiterrez-Mohammed, M.L., Calvin, R.L., Taylor, H.A., Jr., Williams, D.R., 2005. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis 15:S6-38-48. [PubMed]
- Prochaska J.D., Jupiter D.C., Horel S., Vardeman J., Burdine J.N. Rural-urban differences in estimated life expectancy associated with neighborhood-level cumulative social and environmental determinants. Prev. Med. 2020;139:106214. doi: 10.1016/j.ypmed.2020.106214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S., Rae D.S. Susceptibility and precipitating factors in depression: sex differences and similarities. J. Abnorm. Psychol. 1979;88:174–181. doi: 10.1037//0021-843x.88.2.174. [DOI] [PubMed] [Google Scholar]
- Robinson J.C., Wyatt S.B., Dubbert P.M., May W., Sims M. The impact of neighborhood on physical activity in the Jackson Heart Study. Prev. Med. 2016;90:216–222. doi: 10.1016/j.ypmed.2016.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman K.J. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- Sallis J.F., Cain K.L., Conway T.L., Gavand K.A., Millstein R.A., Geremia C.M., Frank L.D., Saelens B.E., Glanz K., et al. Is Your Neighborhood Designed to Support Physical Activity? A Brief Streetscape Audit Tool. Prev. Chronic Dis. 2015;12:E141. doi: 10.5888/pcd12.150098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel L.J., Dennison Himmelfarb C.R., Szklo M., Seeman T.E., Echeverria S.E., Diez Roux A.V. Social engagement and chronic disease risk behaviors: the Multi-Ethnic Study of Atherosclerosis. Prev. Med. 2015;71:61–66. doi: 10.1016/j.ypmed.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims M., Wyatt S.B., Gutierrez M.L., Taylor H.A., Williams D.R. Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethn. Dis. 2009;19:56–64. [PMC free article] [PubMed] [Google Scholar]
- Smitherman T.A., Dubbert P.M., Grothe K.B., Sung J.H., Kendzor D.E., Reis J.P., Ainsworth B.E., Newton R.L., Jr., Lesniak K.T., et al. Validation of the Jackson Heart Study Physical Activity Survey in African Americans. J. Phys. Act. Health. 2009;6(Suppl 1):S124–S132. doi: 10.1123/jpah.6.s1.s124. [DOI] [PubMed] [Google Scholar]
- Tejada-Vera, B., Bastian, B., Arias, E., Escobedo, L.A., Salant, B., 2020. Life Expectancy Estimates by U.S. Census Tract, 2010-2015.
- Todd M., Adams M.A., Kurka J., Conway T.L., Cain K.L., Buman M.P., Frank L.D., Sallis J.F., King A.C. GIS-measured walkability, transit, and recreation environments in relation to older Adults' physical activity: A latent profile analysis. Prev. Med. 2016;93:57–63. doi: 10.1016/j.ypmed.2016.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele T.J. A unification of mediation and interaction: a 4-way decomposition. Epidemiology. 2014;25(5):749–761. doi: 10.1097/EDE.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls, D., Associates, 2011. NETS overview: National Establishment Time-Series (NETS) database.
- Wang X., Auchincloss A.H., Barber S., Mayne S.L., Griswold M.E., Sims M., Diez Roux A.V. Neighborhood social environment as risk factors to health behavior among African Americans: The Jackson Heart Study. Health Place. 2017;45:199–207. doi: 10.1016/j.healthplace.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield K.E., Neupert S.D., Bruce M.A., Sims M., Aiken-Morgan A.T., Thorpe R.J. Stress, longevity and cardiovascular outcomes among African American families in the Jackson Heart Study. Ethn. Dis. 2014;24:456–461. [PubMed] [Google Scholar]
- Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.