Abstract
Objective
To explore health professionals’ perspectives on physical activity and sedentary behaviour of hospitalised adults to understand factors that contribute to these behaviours in this environment.
Data sources
Five databases (PubMed, MEDLINE, Embase, PsycINFO and CINAHL) were searched in March 2023.
Review methods
Thematic synthesis. Included studies explored perspectives of health professionals on the physical activity and/or sedentary behaviour of hospitalised adults using qualitative methods. Study eligibility was assessed independently by two reviewers and results thematically analysed. Quality was assessed using the McMaster Critical Review Form and confidence in findings assessed using GRADE-CERQual.
Results
Findings from 40 studies explored perspectives of over 1408 health professionals from 12 health disciplines. The central theme identified was that physical activity is not a priority in this setting due to the complex interplay of multilevel influences present in the interdisciplinary inpatient landscape. Subthemes, the hospital is a place for rest, there are not enough resources to make movement a priority, everyone's job is no one's job and policy and leadership drives priorities, supported the central theme. Quality of included studies was variable; critical appraisal scores ranged from 36% to 95% on a modified scoring system. Confidence in findings was moderate to high.
Conclusion
Physical activity in the inpatient setting is not a priority, even in rehabilitation units where optimising function is the key. A shift in focus towards functional recovery and returning home may promote a positive movement culture that is supported by appropriate resources, leadership, policy, and the interdisciplinary team.
Keywords: Physical activity, sedentary behaviour, hospitalised adults, inpatient setting, health professionals
Introduction
In certain circumstances, hospitalisation is required to deliver effective healthcare. However, even in circumstances of medical necessity, hospitalisation poses a risk of deleterious secondary effects such as functional decline1–3 that can persist after discharge. 4 Even in those who ambulate independently, high sedentary time and low levels of physical activity during hospitalisation is common,5–7 with an estimated 87–100% of time spent sitting or lying in bed 8 and a daily average of only 880 steps. 9 These patterns are similar even in inpatient settings where the purpose of admission is to optimise recovery, such as rehabilitation. Adults and older adults in inpatient rehabilitation are typically inactive10–20 and have high levels of sedentary time14–16,18,21–23 which are associated with adverse outcomes including functional decline and hospital-acquired disability.24–27 Inpatient environments tend to foster a focus on illness rather than recovery, contrary to modern perspectives that support the optimisation of functional recovery across the care continuum. 28 Given that greater physical activity is associated with a plethora of improved health and wellbeing outcomes 29 and supports recovery, the high levels of inactivity are important to investigate in inpatient populations.
To date there has been considerable investigation into the complex and multifactorial determinants of physical activity and sedentary time in the inpatient setting. Previous research exploring patient perspectives found that hospital staff have an important role in facilitating physical activity. 30 However, patients also reported that staff and the hospital environment can discourage physical activity and promote bed rest. 31 Evidence that physical activity levels can double immediately post discharge further support that hospital-related factors may limit mobility more than physical capacity.32,33 The World Health Organisation (WHO) has established a global action plan to optimise physical activity and sedentary time in hospital settings, citing a need for a ‘whole-of-system’ approach to target these behaviours. 34
Previous related systematic reviews have found that although health professionals recognise the value of improving these behaviours, there are complex multilevel influences that challenge effective implementation and promotion.35,36 Hospital culture, the physical environment, resource constraints and a lack of clarity around roles and responsibilities of team members have been highlighted to play a role.35,36 However, previous reviews were not specific to the inpatient setting, 37 combined patient, clinician and carer perspectives,35,36 explored single profession perspectives only 38 and excluded subacute and rehabilitation settings. 36 Additionally, previous reviews have captured the perspectives of a relatively limited number of health professionals (n = 269 36 and n = 145 35 ), possibly due to the diverse language used across disciplines to define physical activity and sedentary behaviour in this context. This review therefore focussed on synthesising health professional perspectives specifically utilising a broad search strategy to account for this diverse language, given the established important role of health professionals in supporting physical activity and sedentary behaviour change in inpatient settings. Therefore, the aim of this systematic review is to explore perspectives of health professionals on physical activity and sedentary behaviour of hospitalised adults (including older adults), using an extensive search strategy, to understand factors that may contribute to these behaviours in patients in the inpatient environment.
Materials and methods
This systematic review and thematic synthesis has been conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see Supplemental File 1 for checklist), 39 and was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 12/06/2021 (CRD42021254583). 40
Qualitative studies exploring perspectives of health professionals on physical activity and sedentary behaviour of hospitalised adults were eligible for inclusion. This included mixed-methods studies, however, only the qualitative data were extracted and synthesised. Similarly, where studies also explored other stakeholder perspectives (e.g. patient and unpaid caregivers), only data from health professionals were included. Studies that focused specifically on exercise prescription or structured exercise programmes were excluded, as the purpose of our review was to explore physical activity and sedentary behaviour across the entire 24-hour day, not only structured therapy. Studies based in outpatient, community, or other non-hospital settings, or where health professionals primarily work with paediatric or adolescent populations, were excluded. Hospital settings with special tailored environments such as mental health, oncology, palliative, COVID-19 or intensive care settings were also excluded, given these settings can have context-specific features that may influence physical activity and sedentary behaviour. Where studies included data from multiple settings, populations or wards, data from those areas/populations stipulated in our exclusion criteria were not extracted or used in the analysis.
The following databases were searched from their inception to the 2nd March 2023: PubMed, MEDLINE, Embase, PsycINFO and CINAHL. Searches were restricted to original studies published in English, in peer reviewed journals, with no date restrictions. Search terms included keywords, their synonyms and (where relevant) MeSH terms of ‘physical activity’, ‘sedentary behaviour’, ‘healthcare providers’, ‘hospitals’ and ‘qualitative research’. Synonyms applied were expansive to account for the diverse language used to define physical activity and/or sedentary behaviour across the literature in this population and setting. The full search terms are included in Supplemental File 2.
Following database searches, titles and abstracts of retrieved articles were independently screened by two reviewers (TA, JW) to establish eligibility. Remaining studies were reviewed in full-text independently by two reviewers (TA, SG, NM, IR). A third reviewer from the research team reviewed conflicts as required. Backward citation searching was used to screen reference lists of those studies included after the full-text screening stage. Data were extracted by one reviewer (TA) and checked for accuracy by a second reviewer (NM, IR). Disagreements were resolved by discussion with a third reviewer. Corresponding authors were contacted for further data as required.
Descriptive themes were derived from qualitative data using inductive thematic analysis based on the six stages proposed by Braun and Clarke.41–43 Two reviewers (TA, SB) independently became familiar with the data: reading and re-reading extracted data and generating initial ideas. Initial ideas were further refined and coded into preliminary themes based on recurring concepts, then grouped to establish key themes. Then, themes were reviewed across the entire dataset. Themes were further defined and named to produce collated results. All themes identified were discussed by the two reviewers at each of the stages to check for agreement and reach a consensus. This was repeated until the central themes were identified. Once this was completed, a third reviewer (IR) cross-checked the raw data against the themes identified to ensure accuracy. A series of follow up meetings were held with the various members of the research team (TA, SG, IR, SB) to further discuss and refine themes to ensure accuracy of the themes derived. Data extracted from included studies and other materials used for analysis are available on request.
Methodological quality of included studies was evaluated using the McMaster Critical Review Form: Qualitative Studies (Version 2.0). 44 This tool includes nine categories that evaluate study purpose, literature, study design, sampling, data collection, procedural rigour, data analyses, overall rigour and conclusions and implications. A scoring system previously used by Guerin et al. 45 was used to score studies out of a total score of 22, with positive criteria answered ‘yes’ scoring 1 point, and negative criteria answered ‘no’ or ‘not addressed’ scoring 0. The sum of scores was expressed as a percentage of applicable criteria met to allow for comparison of quality between studies. All studies were critically appraised by one reviewer (TA) and cross-checked for agreement by a second reviewer (SG).
In addition, two authors (TA, SG) used the Confidence in the Evidence from Reviews of Qualitative Research (CERQual) tool 46 to assess confidence in the synthesised thematic findings of this review – that is, confidence that the findings of the review reflected the findings of the included studies. CERQual considers four components (the methodological limitations, the relevance, the coherence, and the adequacy of the data) to assess confidence (high, moderate, low, or very low) in each review finding. A high confidence rating indicates a high likelihood that the review finding reasonably represents the phenomenon of interest. 46
Results
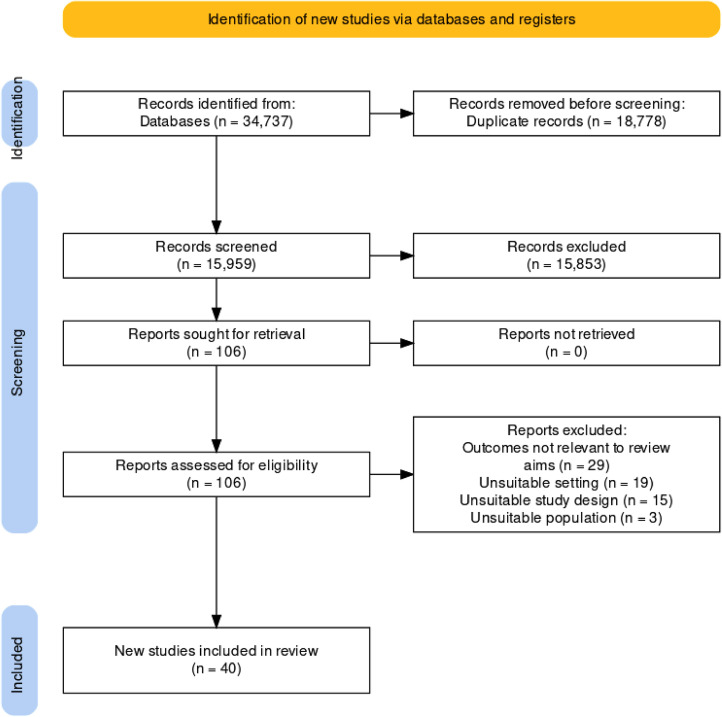
The search identified 34,737 studies, with 18,778 duplicates removed leaving 15,959 studies screened at title/abstract level, with 106 studies progressing to full-text screening (see Figure 1 for the flow diagram of study selection). Forty studies were included in the review, with study characteristics for these presented in Table 1, and more detailed characteristics summarised in Supplemental File 3. Twenty-five of the studies explored perspectives from multiple disciplines,31,47–70 and the remaining 15 included participants from a single profession only.71–85 Overall, studies explored the perspectives of a combined 1408 health professionals working across acute hospitals,31,48–52,54,57–59,61–65,67–74,76,78,80,82–84 rehabilitation,47,56,57,60,66,77 mixed53,55,75,79,81 or other settings 85 as nurses,31,47–52,54–62,64–66,68–78,80,83,84 physiotherapists,31,48,50,51,53–57,59,60,62,64–66,68–70,79,85 physicians or physician assistants31,49,50,52,55–57,59,62–64,66–70,81,82 and occupational therapists.51,55–57,60,62,64–66,68 Other professions included exercise therapy/sports scientists, 53 mobility technicians/instructors,58,68 unspecified therapists,47,78 social and healthcare assistants,55,65,68 respiratory therapists, 66 pharmacists, 68 social workers,56,57 speech pathologists 56 and other unspecified health professionals.63,65 No authors were required to be contacted for further data.
Figure 1.
PRISMA flow diagram of search, screening, and selection process. 101
Table 1.
Summary of included studies.
| Authors | Country | Methods | Setting a | Participants |
|---|---|---|---|---|
| Annemans, 2022 47 | Belgium | Focus groups | Inpatient rehabilitation | N = 6, nurses and therapists |
| Boltz, 2011 71 | United States | Focus groups | Various wards | N = 55, nurses and patient care associates |
| Bor, 2022 48 | Netherlands | Semi-structured interviews | Medical oncology, haematology, cardiology and cardiothoracic surgery | N = 16, nurses, physical therapists and unit managers |
| Brown, 2007 49 | United States | Semi-structured interviews | Medical ward | N = 19, nurses and physicians |
| Chan, 2019 72 | Singapore | Focus groups | General hospital | N = 30, registered and enrolled nurses |
| De Klein, 2021 50 | Netherlands | Semi-structured interviews | Geriatrics and gastroenterology wards | N = 9, physiotherapists, nurses and doctors |
| Doherty-King, 2011 73 | United States | Semi-structured interviews | Adult medical and surgical wards | N = 25, registered nurses |
| Doherty-King, 2013 74 | United States | Semi-structured interviews | Adult medical or surgical wards | N = 25, registered nurses |
| Frederiksen, 2022 51 | Denmark | Focus groups | Geriatric and infectious and pulmonary medical diseases departments in a Danish hospital | N = 8, nurse assistants, nurses, physical therapists and occupational therapists |
| Geelen, 2021 52 | Netherlands | Semi-structured interviews and focus groups | Gastrointestinal, oncology surgery, internal medicine haematology, infectious diseases and cardiology wards | N = 30, nurses, nursing assistants, physician assistant and physicians |
| Geidl, 2019 53 | Germany | Focus groups | Various facilities | N = 58, department heads with a background in physiotherapy, exercise therapy/sports science or other |
| Gustafson, 2021 54 | United Kingdom | Focus group | General hospital | N = 4, physiotherapists and nurses |
| Hazra, 2023 55 | Canada | Online survey with qualitative component | Hospitals and healthcare centres | N = 338, physicians, nurses, physiotherapists, occupational therapists and healthcare aides |
| Hills, 2021 75 | Australia | Individual interviews | Inpatient subacute wards | N = 11, ward nurses and nurse leaders |
| Janssen, 2022 56 | Australia | Semi-structured interviews | Rehabilitation units (two mixed caseload, one neurological rehabilitation, one comprehensive stroke unit) | N = 22, nurses, nursing unit managers, rehabilitation physicians, physiotherapists, occupational therapists, social workers and speech pathologists |
| Jasper, 2023 57 | Australia | Focus group | Subacute geriatric ward and acute orthopaedic ward at a general hospital | N = 7, physiotherapists, occupational therapists, doctor, nurse and social worker |
| Johnson, 2019 58 | United States | Semi-structured interviews | General medicine ward | N = 8, physicians, mobility technician and nurses |
| King, 2016 76 | United States | Focus groups, one semi-structured interview | General medicine ward | N = 15, registered nurses and certified nursing assistants |
| Kirk, 2019 59 | Denmark | Go-along interviews during observation | Endocrinology, infectious diseases, and emergency departments | N = 79, nursing assistants, registered nurses, physiotherapists and physicians |
| Klooster, 2022 69 | The Netherlands | Semi-structured interviews | Cardiothoracic surgery, cardiology, pulmonary diseases, orthopaedics and traumatology, neurosurgery, abdominal surgery, urology, obstetrics and gynaecology, oral and maxillofacial surgery, cardiac care unit, and medical oncology wards | N = 15, physicians, physiotherapists, nurses and nurse assistants |
| Kneafsey, 2015 77 | United Kingdom | Semi-structured interviews | General rehabilitation ward, spinal unit and stroke rehabilitation ward | N = 33, care support workers, registered nurses and ward sisters |
| Kneafsey, 2013 60 | United Kingdom | Semi-structured interviews | General rehabilitation ward, spinal unit and stroke rehabilitation ward | N = 39, registered nurses, ward sisters, care support workers, therapy assistants, occupational therapists and physiotherapists |
| Koenders, 2020 31 | Netherlands | Semi-structured interviews | Cardiology and orthopaedics/trauma wards | N = 24, physical therapists, nurse assistants, nurses, physicians and physicians assistants |
| Lim, 2020a 78 | Singapore | Semi-structured interviews | General medical ward | N = 10, senior enrolled nurses, senior staff nurses, acting nurse clinician and nurse managers |
| Lim, 2020b 61 | United Kingdom | Focus groups | Acute medical wards for older people | N = 13, therapists (unspecified) and nurses |
| Lowe, 2018 79 | United Kingdom | Semi-structured interviews | General secondary care | N = 12, physiotherapists |
| Moore, 2014 62 | Canada | Focus groups | General hospital wards | N = 261, nurses, nurse practitioners, occupational therapists, physiotherapists, physicians, managers, other allied healthcare staff, and other unit staff such as personal support workers and ward clerks |
| Myers, 2021 63 | United Kingdom | Semi-structured interviews | Renal unit and complex medical unit | N = 8, sports and exercise medicine consultants and other healthcare professionals (unspecified) |
| Ohlsson-Nevo, 2020 80 | Sweden | Focus groups | Medical and surgical wards in three hospitals | N = 29, registered nurses and certified nursing assistants |
| Osinaike, 2021 81 | United Kingdom | Semi-structured interviews | Various; participants had spent at least 1 year in rotational foundation training. | N = 11, junior doctors |
| Pavon, 2021 64 | United States | Semi-structured interviews and focus groups | General medicine ward | N = 48, medical residents, nurses, certified nursing assistants, physical therapists and occupational therapists |
| Pedersen, 2020 82 | Denmark | Semi-structured interviews | Medical wards | N = 12, physicians |
| Pham, 2016 83 | Vietnam | Semi-structured interviews | Geriatrics, endocrinology, nephrology and urology departments | N = 25, nurses |
| Rasmussen, 2020 65 | Denmark | Focus groups | General hospital | N = 11, physiotherapists, occupational therapists, social and healthcare assistants, home-care workers and nurses |
| Scheerman, 2020 84 | The Netherlands | Semi-structured interviews | Internal medicine; traumatology; oncological surgery; and a combined ward of vascular surgery, nephrology and urology wards. | N = 51, nurses |
| van Dijk-Huisman, 2022 70 | The Netherlands | Semi-structured interviews | Combined university/tertiary internal medicine hospital wards | N = 16, nurses, physicians and physiotherapists |
| Williams, 2018 85 | United Kingdom/Ireland | Semi-structured interviews | Regional spinal cord injury centres | N = 18, physiotherapists |
| Wray, 2021 68 | United Kingdom | Focus groups | Geriatrics and combined orthogeriatric wards | N = 12, doctors, nurses, pharmacists, physiotherapists, occupational therapists, healthcare assistants and technical instructors |
| Wshah, 2021 66 | Canada | Semi-structured interviews | Pulmonary rehabilitation | N = 16, doctors, physiotherapists, occupational therapists, nurses and respiratory therapists |
| Zisberg, 2018 67 | Israel | Interviews and Focus Groups | Internal Medicine Wards | Unclear Total Sample Size, N = 116 Medical Professions However Multiphase Approach, Unclear Sample Size Of Qualitative Component. |
Data only extracted when relevant to the settings meeting the eligibility criteria of this review.
The thematic analysis identified one central theme ‘Physical activity is not a priority’, and four subthemes, which are described in Table 2. Additional supporting quotes to the results can be found in Supplemental File 4. Our level of confidence in the review findings ranged from moderate to high and has been noted throughout the results. Table 3 includes the CERQual summary of qualitative findings.
Table 2.
Central theme and subthemes with related key topics.
| Physical activity is not a priority | The hospital is a place for rest | A culture of bed rest |
| Risk-reductive approach | ||
| The physical environment | ||
| There are not enough resources to make movement a priority | Not enough time, personnel or equipment | |
| High workloads | ||
| Promoting physical activity is resource intensive, particularly in sick patients or patients with many attachments | ||
| Everyone's job is no one's job | Shared responsibility but no clear perceived ownership | |
| Need for effective team collaboration | ||
| Lack of knowledge/skills | ||
| Patient’s own responsibility | ||
| Policy and leadership drives priorities | Falls prevention, manual handling and mobility policies can deter from physical activity promotion | |
| Leadership in promotion of physical activity was important |
Table 3.
CERQual summary of qualitative findings.
| CERQual | |||||
|---|---|---|---|---|---|
| Main theme | Subthemes | Summary | Studies | Confidence | Explanation |
| Physical activity is not a priority | The hospital is a place for rest | The hospital was often seen to facilitate a culture of bed rest through the physical environment, staff, and systems, with favouritism towards a risk-reductive approach to care delivery. | 31,47–50,52,54,56,57,59,60,62–65,68–75,77,78,80,82–84 | High confidence | Twenty-nine studies contribute to this finding. There were minor concerns about methodological limitations and coherence of those studies. There were no/very minor concerns about adequacy and relevance. |
| There are not enough resources to make movement a priority | Health professionals felt that promotion of movement could be resource intensive in an already resource-limited (specifically lacking in time, personnel, or equipment), high workload setting. Subsequently, resources were allocated to other priority areas. | 31,48–52,54–56,58–64,66,68,70–75,78–80,82–85 | High confidence | Thirty-one studies contribute to this finding. There were minor concerns about methodological limitations and relevance, and no/very minor concerns about coherence and adequacy of data. | |
| Everyone's job is no one's job | Health professionals perceived there to be a shared responsibility, yet noted a lack of ownership, in supporting patient movement amongst the interdisciplinary team and the patient themselves. Reduced knowledge and skills amongst some team members was noted as a barrier to supporting movement. | 31,48,50–53,55,56,59–72,74,75,80–85 | Moderate confidence | Thirty studies contribute to this finding, with minor concerns with methodological limitations, coherence, adequacy, and relevance. | |
| Policy and leadership drives priorities | Health professionals practice, perspectives and prioritisation of movement support was influenced by policies and leaders. Falls prevention, manual handling and mobility-related policies prioritised safety over movement further contributing to a risk reductive approach | 48,56,59–64,67–69,71–73,76,77 | High confidence | Sixteen studies contribute to this finding. There were no/very minor concerns about methodological limitations, coherence, adequacy, and relevance. | |
Central theme: physical activity is not a priority
Health professionals frequently reported that they were aware of the benefits of physical activity promotion31,59,63,64,66,68,69,76,78,80–82,84,85 and the importance of optimising inpatient movement behaviour to prevent complications60,63,64,68–71,74,80,83,84 or functional decline,64,68,70,72,76,78,84 and to optimise recovery.64,69,72,80 They noted that the inpatient setting could be an opportunity to instil education and to promote long-term positive physical activity behaviour to patients,63,82,85 and that increasing physical activity during a patient's admission could improve other aspects of the patient's wellbeing and their general experience in hospital56,69,75,80:
‘It's staggering how much time they [patients] spend alone. There's a potential connection here. … If we tackle the boredom, we tackle the sedentary behaviour, there is a link, and we will solve the social isolation. …’ – Nurse leader 75
However, despite strong statements that physical activity is critical, optimising movement behaviours was overall not seen as a priority in the inpatient setting over other tasks.49–51,59,61,70,74,75,79,82,84 The subthemes showed a range of contributing, often interrelated, factors that reinforced that physical activity was not a priority, and also demonstrated potential contributing factors that resulted in this lack of prioritisation.
Subtheme 1: ‘The hospital is a place for rest’
First, health professionals perceived that unit expectations and culture influenced how staff facilitated physical activity and/or discouraged sedentary time, with a culture that often reinforced the hospital as a place of rest (CERQual assessment: high confidence).48,50,64,69,71,73,74,76,80 This culture was often not conducive to physical activity, with a culture of bed rest (whereby some patients associated hospitalisation with rest)50,52,59,60,62,65,70,71,82–84 contributing to this concept of physical activity not being a priority:
‘Many of the older patients do not want to get out of bed. It seems that they were raised to believe that when you are ill, you must recover in bed’ – Nurse assistant 59
This bed rest culture and pacification of the patient was described as being influenced by families or caregivers, who could act as a barrier71,72,75,80 or an enabler to physical activity.49,52,56,57,71,72,75,80 Health professionals also perceived that some patients lacked motivation to move during hospitalisation,31,49,50,59,62,65,72,83,84 (particularly when patients were elderly49,50,59,80,82–84), which may further reinforce bed rest culture:
‘I just think he is older now, and he is not as motivated as younger people are, and he has been through so much. I just don’t think he wants to do it.’ – Unknown profession 49
A perceived fear of falling further influences this, where health professionals felt patients’ fear of falling discouraged them from moving more60,62,68,71,72:
‘They may have had a fall at home that warranted this admission. Consequently, the phobia is there as they refuse to get out of bed due to the fear of falling again.’ – Nurse 72
These fears were said to be exacerbated by health professionals who provide constant assistance, reinforcing the lack of confidence patients have in their mobility and thereby further reinforcing a culture of rest 68 :
‘…if we’re like mobilising patients and we’re clinging on to them like that, it does nothing for anyone's confidence, you know, them thinking I need someone to be on my hip the whole time, rather than if you just take a step back and you know.’ – Unknown profession 68
Subsequently, this culture was perceived to be reinforced by the preference for and reinforcement of a risk-reductive approach, where falls prevention was prioritised over patient physical activity47,49,56,60,64,68,72,77:
‘I think a big part of it is safety…part of the culture has become that the room seems like the safest place for the patient … … keep them in bed.’ – Physiotherapist 56
Health professionals perceived that the physical environment of the hospital reflected this culture of bed rest31,48,49,52,56,57,62,70,78,80,82,83; cited as promoting sedentary time and lacking in features to incentivise physical activity.48,56,70,82 The hospital environment was said to lack space for physical activity,59,62,70,71,78,82,83or available space was not fit for purpose, 56 appealing48,56 or known to patients that it was available for their use. 56 The hospital room and bed space in particular was thought of as somewhat of a centrepiece, where its design and layout promoted patients to spend time in bed31,49,52,57,70,82:
‘No, when the room is organized around the bed, and everything is within reach and the television is also free; which means it's available for everyone; then it's incredibly tempting for people to stay in their beds.’ – Nurse 52
Health professionals felt patients might engage in more physical activity if the ward environment was better designed to facilitate this,47,49,57,59,84 and in particular if the environment made patients feel safe57,82:
‘If you walk badly and are a little dizzy and so on, it's not interesting to walk in a hallway which is narrow and where people come rushing. Then I think you prefer staying in bed. There you’ll feel safe.’ – Physician 82
However, this culture of bed rest is perhaps not entirely unsubstantiated given in some cases, medical bed rest was indeed believed to be indicated. Health professionals were also clear that physical activity was not always an appropriate priority for all patients in the hospital setting during admission49,50,54,63,64,72,73,80,82 due to some patients being too unwell,50,54,64,70,72,73,82 in too much pain50,54,64,70,72,73,82 and/or limited in their capacity to move because of medical attachments.49,50,54,63,64,70,72,73,80,82
Taken together, the hospital was perceived as being a place for rest, where risk reduction was prioritised over physical activity, and so physical activity was subsequently not a priority in the inpatient setting.
Subtheme 2: ‘There are not enough resources to make movement a priority’
Despite strong beliefs overall that physical activity and minimising sedentary behaviour was important, staff most frequently cited that resource constraints were a barrier to promoting increased physical activity and reduced sedentary behaviour of their patients (CERQual assessment: high confidence).31,48–52,54–56,58–64,66,68–75,78–80,82–85 Many health professionals described a lack of time,31,49–52,56,60–62,66,68–72,75,79,80,82 personnel/staff49,51,54–56,58,60,61,63,68,70,71,74,75,78,80,84,85 and equipment.49,52,54,55,59,62,64,70,73,83 This was challenged further in the context of high workloads48,62,70,72,75,80,82,84:
‘…sometimes it is due to a high workload. You know it is important and benefits the patient, but you don't have enough time unfortunately… when other things have to be done, it is not a priority.’ – Nurse 84
Health professionals felt physical activity would be improved and/or sedentary time reduced if there were more staff available to promote these behaviours.51,55,56,62,73,74 Additionally, patients who were sicker, had more attachments and/or required assistance to mobilise49,54,56,70 were perceived to increase workloads49,72,74,75 in this already resource-stretched environment, leading to health professionals being less inclined to facilitate physical activity, and/or patients to feel restricted to move:
‘I hate to say it, but I think on some days, it does [affect mobility]. You have patients who have TPN [total parenteral nutrition] and blood and Foleys and chest tubes, you are probably less likely to [get people out of bed].’ – Nurse 49
Given facilitation of physical activity is considered resource intensive,60,68,75 health professionals sometimes compensated for a lack of resources (particularly when workloads were high50,59,74,84) by increasing the assistance provided beyond what was necessary in the interest of saving time60,68,70,72,80:
‘Things can be done faster if we provide total assistance. That's why we always helped them more than we should.’ – Nurse 72
A lack of resources (of time, personnel, and equipment) appeared, in some cases, to lead to not only an omission of promotion of optimal movement behaviours, but active obstruction to incidental movement as well.
Subtheme 3: ‘Everyone's job is no one's job’
There were conflicting views amongst health professionals regarding roles and responsibilities for promoting or facilitating physical activity and reducing sedentary behaviour. This indicates that perhaps these behaviours are not prioritised by members of the team due to the perception of a shared responsibility48,55,56,62,64,67,70,71,74,81,82,84,85 without effective clarification of roles in assessment and promotion of physical activity (CERQual assessment: moderate confidence). Although health professionals felt information and education should be provided to patients,55,57,58,61,66,70,71,83,85 they perceived their own reduced knowledge and skills as a barrier to promoting physical activity,50,54,55,62,64,66,70,73,75,83,85 perceiving this as a reason for why they attributed responsibility to others50,59,82,83:
‘I tell them they should get out of bed. But not like, “walk the stairs” or something. I don’t know what to advise them. I leave that to the physiotherapist.’ – Physician 50
In addition to this, health professionals felt a lack of knowledge of a patient's baseline mobility61,62,71 and/or current mobility status51,62,69–71 as barriers to facilitating physical activity. There were conflicting opinions as to which profession/s are responsible and/or capable of collecting and/or assessing this. Physiotherapists were frequently perceived as responsible for mobility assessment,80,82 with physicians 84 and nurses 67 reported as also being capable. This information was perceived as important for setting expectations for inpatient physical activity and could influence how health professionals promoted activity amongst different patients64,71,73:
‘We don’t know what the patient can do. Often, older patients look very frail. We don't know if they can stand, for instance.’ – Patient Care Associate 71
In terms of promotion of physical activity, physiotherapists51,52,59,60,64,70,80,82,84,85 and nurses50,52,67,72,75,80,82–84 were commonly described as the most appropriate health professionals to do so:
‘I think we play a pretty important role, we are with our patients every day and we have the time to get in there and encourage the exercises that [the] physio suggested.’ – Nurse 75
However, physicians were also noted by health professionals as having an important role in reinforcing these behaviours to patients,52,57,59,63,70,80,82 and it was perceived that patients would be more likely to listen to physicians over other members of the team59,70,80,82:
‘And even the doctors – sometimes we have to ask the physician doing the round, “Please, tell this patient how important it is that he gets up and moves around a bit.” Sometimes it helps and it's like they need that.’ – Nurse 80
Interestingly, health professionals also noted that activity was not always their responsibility as patients held an element of ownership over their movement behaviours and recovery31,47,50,52,53,80,84:
‘Well, I think: yeah right, I am not a cop. If someone really does not want to get out of bed because he feels to sick or does not want to. Well, at some point it is just the responsibility of the patient.’ – Nurse 50
However, it was also acknowledged that personal responsibility could be restricted in the inpatient environment 80 :
‘Suddenly, you find yourself in a hospital and you can’t really take any personal responsibility – you’re at the mercy of other people who make all the decisions’ – Certified Nursing Assistant 80
Subsequently, staff also acknowledged the need to take responsibility for making patients aware of the importance of increasing physical activity and reducing sedentary behaviour during their admission,50,62,71,82,84 as well as what they are expected to50,52 and are allowed to do68,82:
‘We (sic) probably maybe better at promoting what not to do rather than what you can do.’ – Profession unknown 68
Despite some uncertainty around key roles and responsibilities, health professionals felt there was a shared responsibility to facilitate these behaviours50–52,55,56,63,66,67,70,71,75,80,82 and a need for a team-based approach48,53,63,65,66,68–72,75,80 utilising interprofessional collaboration to effectively facilitate movement behaviours in this setting48,51,53,55,59,63,65,66,68–72,75:
‘Getting people out of bed and moving can’t happen if everyone doesn’t help.’ – Patient care associate 71
If this collaboration was poor (which may result in the presence of skewed roles and responsibilities), it was thought to compromise effective facilitation of these behaviours.59,62 Conflicting and unclear roles and responsibilities around the promotion of physical activity in this setting is likely to contribute to this lack of prioritisation of physical activity – where no clear ownership exists.
Subtheme 4: ‘Policy and leadership drives priorities’
Finally, health professionals noted the influence of policies and leaders and that these ultimately trickled down to how their own day-to-day tasks were prioritised (CERQual assessment: high confidence). Falls prevention, manual handling and/or other mobility-related policies were found to promote a risk reductive approach that prioritised safety over movement, thereby reinforcing a culture of bed rest and acting as a barrier to optimising physical activity and reducing sedentary behaviour.56,60–62,64,68,71–73,77 This was reinforced by other related barriers such as organisational quality indicators,60,67,68,72 with health professionals expressing a fear of patients falling or injuring themselves while moving,47,49,56,60–62,64,68,71–73,77 and concerns about sustaining work related injuries while assisting patients60,62,73:
‘While they are in bed they are not giving trouble to anybody. It is less work and, second, because of liability issues in terms of patients falling and hurting themselves while they are in the hospital. I think everybody is very concerned with that, but I think mainly because it is less work.’ – Physician 49
Beyond those related to falls, additional hospital policies were perceived as restrictive to the capacity of health professionals to promote patient physical activity.59,60,67,71,77 These included manual handling policies that favoured passive patient transport60,71,77 and policies that required physician and/or physiotherapy clearance before patients were allowed to be mobilised.71,77 Health professionals reported they felt hesitant to facilitate physical activity of their patients in the interest of safety, as well as due to a fear of repercussions should policy or quality indicators be compromised.60,67,68,72
‘I walk a lot of steps during the day because the patients call for more coffee, which I have to pick up in the corridor where we have placed the coffee machine for self-supporting patients and their relatives or they want me to change their sheets. It is interesting because a lot of the patients do it by themselves at home’ – Nurse 59
Additionally, health professionals reported that leadership support from senior clinicians and/or management was important to enable and motivate staff to promote physical activity48,63,69,71,76:
‘On my unit, preventing physical decline is an important goal. We review functional status during rounds, and everyone sees this as a priority. I think this is because the leadership here believes that older people deserve to stay functional.’ – Nurse 71
This demonstrates that health professionals may look to policies and leadership in developing their priorities in clinical practice, and thus contribute to the overarching theme of physical activity not being a priority in the inpatient setting.
Study quality and reporting
The methodological quality of the included studies in this review was variable, with critical appraisal scores ranging from 36 to 95%. Consensus agreement was reached by two reviewers. Common methodological issues related to a lack of clearly defined theoretical perspective, not mentioning whether data collection continued until thematic saturation, limited disclosure of the role of the researcher and/or relationship with participants and a lack of disclosure of identified assumptions and biases of researcher.
Discussion
The aim of this systematic review was to explore the perspectives of health professionals on physical activity and sedentary behaviour of hospitalised adults, using an extensive search strategy, to understand factors that may contribute to these behaviours in patients in the inpatient environment. The review findings, which synthesise findings from 40 studies inclusive of over 1408 health professionals, indicate that despite knowing the benefits, physical activity is not perceived as a priority in inpatient settings by health professionals. Contributing factors are multifactorial and occur across multiple levels of the healthcare system. This builds on findings from similar related reviews35,36,86 and suggests current physical activity interventions are not translatable to the hospital setting. 87 In particular, this review highlights the influence of prioritisation on the provision of physical activity and sedentary behaviour change support in this setting, notably, that health professionals recognise the benefits of movement for their patients but are met with challenges in managing competing demands.
There was a tendency to prioritise risk reduction over physical activity. This approach contributes to a culture of bed rest to promote safety that aligns with an outdated biomedical model of care.36,86 Physical activity was perceived to increase falls risk and unsuitable for patients who were unwell or older in age,36,38,86 resulting in avoidance.88,89 However, increased physical activity is associated with improved function, 88 reduced falls risk 89 and shorter length of stay. 90 Importantly, these improvements are not associated with an increase in falls. 89 The priority for safety and risk reduction should be acknowledged when designing interventions for this setting, while falls prevention policies could also explore ways of ensuring physical activity is not unnecessarily restricted during implementation.
Inconsistencies in how physical activity is defined by health professionals,31,52,67,79 together with the absence of clear guidelines for physical activity in hospitalised adults, may create uncertainty on how to promote these behaviours in this setting. To date, there is only one Delphi study that recommends increased physical activity and reduced sedentary time in hospitalised older adults. 91 Strategies for implementation are unclear and what targets should be aimed for in other hospitalised populations (e.g. rehabilitation). Further, health professionals often describe physical activity being accumulated through structured therapy when in hospital,36,48,60 rather than identifying opportunities such as transfers, bed mobility, walking and showering as potentially beneficial incidental activity and opportunities to break up sitting time. 92 These incidental opportunities may also have health benefits without the same resource requirements as structured therapy, and could be a feasible way to address this problem of low activity and high sedentary behaviour observed in hospitalised adults. Clear definitions of strategies used to increase activity in the hospital setting will be important.
Hospital resourcing, processes and environments may not be conducive to support patients to move more and sit less. Resource constraints are commonly reported by health professionals as barriers to physical activity interventions. Identifying the potential benefits at a system level may assist in resource allocation within organisations for staff and time to invest in these interventions. For example, interventions to increase physical activity during acute hospitalisation has shown cost savings of up to $300 USD per patient, per hospital stay. 93 Considering this cost-benefit during planning, prioritisation and resourcing will be important in future hospital design. Further, processes such as meals being brought to the bedside 52 and environments with limited communal spaces and dining rooms94,95 reduce opportunities for activity and encourage patients to remain in bed, accumulating high volume of sedentary behaviour. These should be considered in future hospital design.21,95–98
This review found that health professionals perceived patients to have low motivation to be physically active.31,49,50,59,62,65,72,83,84 However, previous literature has disputed this, with patients reporting that health professionals do not value mobility, are not interested in it and/or find it burdensome to assist.36,49,86 Hospitalised adults express a desire to engage in meaningful physical activity,31,99,100 value the encouragement from health professionals and feel inactivity exacerbates feelings of a loss of freedom during hospitalisation. 31 Improving physical activity has the potential to induce not only physical benefits, but also help patients feel ‘liberated from the bed and more independent’, 31 regaining a sense of autonomy and reducing boredom. 36
This review has several strengths. Firstly, we used a comprehensive search strategy and to our knowledge this is the largest qualitative review on this topic. Secondly, the research team has combined experience in qualitative research, physical activity, and clinical experience in hospital and rehabilitation settings. A limitation of this review was that qualitative work embedded within interventional studies were included,48,54,61–63,67,76,82 so findings from these studies may have been influenced by participant involvement with an intervention. A single author extracted data; however, this was cross-checked by a second author with conflicts resolved by a third author. Our inclusion criteria of studies published in English subjects this research to potential publication and English language bias, and this should be considered when interpreting the findings of this research. This review was undertaken during the COVID-19 pandemic, and although we excluded COVID-19 specific studies, it is important to note that most included studies explored this phenomenon pre-COVID-19. Factors such as isolation protocols, visitor restrictions and staffing restraints have likely impacted on inpatient physical activity and sedentary behaviour. Finally, the included studies ranged in quality, and we did not exclude low-quality studies from the analysis. However, we did not find grossly different conclusions in low-quality studies and would not expect excluding based on quality to have changed the findings of this review.
In conclusion, physical activity is not a priority in the hospital setting. Instead, the hospital is often considered a place for rest, and encourages a risk reductive approach that can promote immobility despite the evidenced benefits of physical activity and risks of inactivity and high sedentary time. Multilevel challenges with resources, role clarification, a lack of clear leadership and policies that foster bed rest culture and immobility must be addressed to comprehensively enable delivery of evidence-based, person-centred care.
Clinical messages.
Physical activity is not a priority in the inpatient setting despite the evidenced benefits.
Multilevel considerations are required in developing interventions to target these behaviours.
An interdisciplinary teams-based approach is recommended, however, requires supportive clinical environments that provide the appropriate resources, leadership, and policy support to promote cultural change.
Supplemental Material
Supplemental material, sj-docx-1-cre-10.1177_02692155231170451 for Perspectives of health professionals on physical activity and sedentary behaviour in hospitalised adults: A systematic review and thematic synthesis by Tahlia Alsop, James Woodforde, Ingrid Rosbergen, Niruthikha Mahendran, Sandra Brauer, and Sjaan Gomersall in Clinical Rehabilitation
Footnotes
Author contributions: All authors contributed to the research design and development of a search strategy. TA and JW completed all title and abstract screening. TA, IR and NM completed full-text screening and data extraction. TA and SG completed quality appraisal. TA and SB completed data analysis, with cross-checking with IR and SG as appropriate. TA and SG completed the CERQual assessment. The final manuscript was compiled by TA. All authors read and approved of the final manuscript.
Availability of data and materials: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: TA is supported by an Australian Government and University of Queensland Research Training Programme (RTP) Scholarship.
ORCID iD: Tahlia Alsop https://orcid.org/0000-0003-3717-703X
Supplemental material: Supplemental material for this article is available online.
References
- 1.Buurman BM, Hoogerduijn JG, de Haan RJ, et al. Geriatric conditions in acutely hospitalized older patients: prevalence and one-year survival and functional decline. PLOS ONE 2011; 6: e26951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chodos AH, Kushel MB, Greysen SR, et al. Hospitalization-associated disability in adults admitted to a safety-net hospital. J Gen Intern Med 2015; 30: 1765–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc 2020; 21: 455–461.e455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taraldsen K, Thingstad P, Sletvold O, et al. The long-term effect of being treated in a geriatric ward compared to an orthopaedic ward on six measures of free-living physical behavior 4 and 12 months after a hip fracture – a randomised controlled trial. BMC Geriatr 2015; 1: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown CJ, Redden DT, Flood KL, et al. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc 2009; 57: 1660–1665. [DOI] [PubMed] [Google Scholar]
- 6.Lim SER, Dodds R, Bacon D, et al. Physical activity among hospitalised older people: insights from upper and lower limb accelerometry. Aging Clin Exp Res 2018; 30: 1363–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirk AG, Behm KJ, Kimmel LA, et al. Levels of physical activity and sedentary behavior during and after hospitalization: a systematic review. Arch Phys Med Rehabil 2021; 102: 1368–1378. [DOI] [PubMed] [Google Scholar]
- 8.Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? A systematic review and meta-analysis. Appl Nurs Res 2020; 51: 151189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scott J, Abaraogu UO, Ellis G, et al. A systematic review of the physical activity levels of acutely ill older adults in hospital at home settings: an under-researched field. Eur Geriatr Med 2021; 12: 227–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith P, Galea M, Woodward M, et al. Physical activity by elderly patients undergoing inpatient rehabilitation is low: an observational study. Aust J Physiother 2008; 54: 209–213. [DOI] [PubMed] [Google Scholar]
- 11.Bernhardt J, Borschmann K, Crock D, et al. Stand up and be counted: measuring time spent upright after hip fracture and comparison with community dwelling older people. Physiotherapy 2005; 91: 215–222. [Google Scholar]
- 12.Esmonde T, McGinley J, Wittwer J, et al. Stroke rehabilitation: patient activity during non-therapy time. Aust J Physiother 1997; 43: 43–51. [DOI] [PubMed] [Google Scholar]
- 13.Peiris CL, Taylor NF, Shields N. Patients receiving inpatient rehabilitation for lower limb orthopaedic conditions do much less physical activity than recommended in guidelines for healthy older adults: an observational study. J Physiother 2013; 59: 39–44. [DOI] [PubMed] [Google Scholar]
- 14.Simpson DB, Breslin M, Cumming T, et al. Go home, sit less: the impact of home versus hospital rehabilitation environment on activity levels of stroke survivors. Arch Phys Med Rehabil 2018; 99: 2216–2221.e2211. [DOI] [PubMed] [Google Scholar]
- 15.McRae P, Bew P, Smith S, et al. An observational study of physical, cognitive and social activities in rehabilitation inpatients. Australas J Ageing 2020; 39: 217–224. [DOI] [PubMed] [Google Scholar]
- 16.de Jong AU, Smith M, Callisaya ML, et al. Sedentary time and physical activity patterns of stroke survivors during the inpatient rehabilitation week. Int J Rehabil Res 2021; 2: 44. [DOI] [PubMed] [Google Scholar]
- 17.Denkinger MD, Flick SE, Nikolaus T, et al. Assessing physical activity in inpatient rehabilitation—sensor-based validation of the PAIR. Eur Rev Aging Phys Act 2014; 11: 133–139. [Google Scholar]
- 18.Grant PM, Granat MH, Thow MK, et al. Analyzing free-living physical activity of older adults in different environments using body-worn activity monitors. J Aging Phys Act 2010; 18: 171–184. [DOI] [PubMed] [Google Scholar]
- 19.Garner J, Smith M. Activity levels of inpatients admitted to two rehabilitation units in regional hospitals: an observational study. Aust J Rural Health 2021; 3: 399–407. [DOI] [PubMed] [Google Scholar]
- 20.Hassett L, Wong S, Sheaves E, et al. Time use and physical activity in a specialised brain injury rehabilitation unit: an observational study. Brain Inj 2018; 32: 850–857. [DOI] [PubMed] [Google Scholar]
- 21.Scrivener K, Pocovi N, Jones T, et al. Observations of activity levels in a purpose-built, inpatient, rehabilitation facility. HERD: Health Environ Res Design J 2019; 12: 26–38. [DOI] [PubMed] [Google Scholar]
- 22.Sjöholm A, Skarin M, Churilov L, et al. Sedentary behaviour and physical activity of people with stroke in rehabilitation hospitals. Stroke Res Treat 2014; 2014: 591897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barrett M, Snow JC, Kirkland MC, et al. Excessive sedentary time during in-patient stroke rehabilitation. Top Stroke Rehabil 2018; 25: 366–374. [DOI] [PubMed] [Google Scholar]
- 24.Hartley P, Romero-Ortuno R, Wellwood I, et al. Changes in muscle strength and physical function in older patients during and after hospitalisation: a prospective repeated-measures cohort study. Age Ageing 2021; 50: 153–160. [DOI] [PubMed] [Google Scholar]
- 25.Suesada MM, Martins MA, Carvalho CR. Effect of short-term hospitalization on functional capacity in patients not restricted to bed. Am J Phys Med Rehabil 2007; 86: 455–462. [DOI] [PubMed] [Google Scholar]
- 26.Agmon M, Zisberg A, Gil E, et al. Association between 900 steps a day and functional decline in older hospitalized patients. JAMA Intern Med 2017; 177: 272–274. [DOI] [PubMed] [Google Scholar]
- 27.Tasheva P, Vollenweider P, Kraege V, et al. Association between physical activity levels in the hospital setting and hospital-acquired functional decline in elderly patients. JAMA Netw Open 2020; 3: e1920185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stucki G, Bickenbach J, Gutenbrunner C, et al. Rehabilitation: the health strategy of the 21st century. J Rehabil Med 2018; 50: 309–316. [DOI] [PubMed] [Google Scholar]
- 29.Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose–response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. Br Med J 2019; 366: l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mealy B. The perceptions of older patients and their family or caregivers towards physical activity and exercise on a specialist geriatric ward: a qualitative study. Royal College of Surgeons in Ireland, 2020. [Google Scholar]
- 31.Koenders N, van Oorsouw R, Seeger JPH, et al. “I’m not going to walk, just for the sake of walking…”: a qualitative, phenomenological study on physical activity during hospital stay. Disabil Rehabil 2020; 42: 78–85. [DOI] [PubMed] [Google Scholar]
- 32.Kolk D, Aarden JJ, Macneil-Vroomen JL, et al. Factors associated with step numbers in acutely hospitalized older adults: the hospital-activities of daily living study. J Am Med Dir Assoc 2021; 22: 425–432. [DOI] [PubMed] [Google Scholar]
- 33.Chastin SFM, De Craemer M, Lien N, et al. The SOS-framework (systems of sedentary behaviours): an international transdisciplinary consensus framework for the study of determinants, research priorities and policy on sedentary behaviour across the life course: a DEDIPAC-study. Int J Behav Nutr Phys Activity 2016; 13: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization. Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: World Health Organization, 2018. [Google Scholar]
- 35.Koenders N, Marcellis L, Nijhuis-Van Der Sanden MW, et al. Multifaceted interventions are required to improve physical activity behaviour in hospital care: a meta-ethnographic synthesis of qualitative research. J Physiother 2021; 67: 115–123. [DOI] [PubMed] [Google Scholar]
- 36.Stutzbach J, Jones J, Taber A, et al. Systems approach is needed for in-hospital mobility: a qualitative metasynthesis of patient and clinician perspectives. Arch Phys Med Rehabil 2021; 102: 984–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Albert FA, Crowe MJ, Malau-Aduli AEO, et al. Physical activity promotion: a systematic review of the perceptions of healthcare professionals. Int J Environ Res Public Health 2020; 17: 4358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Hell-Cromwijk M, Metzelthin SF, Schoonhoven L, et al. Nurses’ perceptions of their role with respect to promoting physical activity in adult patients: a systematic review. J Clin Nurs 2021; 30: 2540–2562 [DOI] [PubMed] [Google Scholar]
- 39.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021; 88: 105906. [DOI] [PubMed] [Google Scholar]
- 40.Alsop T, Woodforde J, Rosbergen-Wildemors I, et al. Perspectives of health professionals on physical activity and sedentary behaviour of hospitalised adults. PROSPERO: International prospective register of systematic reviews. 2021.
- 41.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 42.Braun V, Clarke V, Cooper H. Thematic analysis. In: Cooper H, Camic PM, Long DL, et al. (eds) APA Handbook of research methods in psychology. Washington, DC: American Psychological Association, 2012, pp.57–71. [Google Scholar]
- 43.Clarke V, Braun V, Hayfield N. Thematic analysis. Qualitat Psychol: Pract Guide Res Methods 2015; 222: 248. [Google Scholar]
- 44.Letts L, Wilkins S, Law M, et al. Critical review form – qualitative studies (version 2.0). Hamilton, Canada: McMaster University; 2007. [Google Scholar]
- 45.Guerin M, Grimmer K, Kumar S. Community services’ involvement in the discharge of older adults from hospital into the community. Int J Integr Care 2013; e032: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lewin S, Booth A, Glenton C, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018; 1: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Annemans M, Van Dyck D, Heylighen A. What affects physical activity in a rehabilitation centre? Voices of patients, nurses, therapists, and activity trackers. Disabil Rehabil 2022: 1–10. [DOI] [PubMed] [Google Scholar]
- 48.Bor P, Van Delft L, Valkenet K, et al. Perceived factors of influence on the implementation of a multidimensional project to improve patients’ movement behavior during hospitalization: a qualitative study. Phys Ther 2022; 2: 102. [DOI] [PubMed] [Google Scholar]
- 49.Brown CJ, Williams BR, Woodby LL, et al. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. J Hosp Med 2007; 2: 305–313. [DOI] [PubMed] [Google Scholar]
- 50.De Klein K, Valkenet K, Veenhof C. Perspectives of patients and health-care professionals on physical activity of hospitalized patients. Physiother Theory Pract 2021; 37: 307–314. [DOI] [PubMed] [Google Scholar]
- 51.Frederiksen KO, Nørgaard B, Bruun IH. How to improve hospitalized older adults’ activity level: a mixed methods study. Phys Occup Ther Geriatr 2022; 41: 1–18. [Google Scholar]
- 52.Geelen SJG, Giele BM, Engelbert RHH, et al. Barriers to and solutions for improving physical activity in adults during hospital stay: a mixed-methods study among healthcare professionals. Disabil Rehabil 2021; 15: 1–10. [DOI] [PubMed] [Google Scholar]
- 53.Geidl W, Wais J, Fangmann C, et al. Physical activity promotion in daily exercise therapy: the perspectives of exercise therapists in German rehabilitation settings. BMC Sports Sci Med Rehabil 2019; 1: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gustafson OD, Vollam S, Morgan L, et al. A human factors analysis of missed mobilisation after discharge from intensive care: a competition for care? Physiotherapy 2021; 113: 131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hazra D, Mohamed M, Hyde AM, et al. Nutrition and physical activity knowledge, attitudes, and practices of inpatient cirrhosis care providers. Eur J Gastroenterol Hepatol 2023; 4: 35. [DOI] [PubMed] [Google Scholar]
- 56.Janssen H, Bird M-L, Luker J, et al. Impairments, and physical design and culture of a rehabilitation unit influence stroke survivor activity: qualitative analysis of rehabilitation staff perceptions. Disabil Rehabil 2022; 26: 1–6. [DOI] [PubMed] [Google Scholar]
- 57.Jasper U, Visvanathan R, Dollard J, et al. Exploring the perspectives of clinicians on solutions to tackling physical inactivity and sedentary behaviour in older hospital patients. Health Promot J Austr 2023; 34: 41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson AM, Howell DM. Mobility bridges a gap in care: findings from an early mobilisation quality improvement project in acute care. J Clin Nurs 2019; 28: 4044–4052. [DOI] [PubMed] [Google Scholar]
- 59.Kirk JW, Bodilsen AC, Sivertsen DM, et al. Disentangling the complexity of mobility of older medical patients in routine practice: an ethnographic study in Denmark. PLOS ONE 2019; 14: e0214271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kneafsey R, Clifford C, Greenfield S. What is the nursing team involvement in maintaining and promoting the mobility of older adults in hospital? A grounded theory study. Int J Nurs Stud 2013; 50: 1617–1629. [DOI] [PubMed] [Google Scholar]
- 61.Lim SH, Ang SY, Ong HK, et al. Promotion of mobility among hospitalised older adults: an exploratory study on perceptions of patients, carers and nurses. Geriatr Nurs 2020; 41: 608–614. [DOI] [PubMed] [Google Scholar]
- 62.Moore JE, Mascarenhas A, Marquez C, et al. Mapping barriers and intervention activities to behaviour change theory for mobilization of vulnerable elders in ontario (MOVE ON), a multi-site implementation intervention in acute care hospitals. Implement Sci 2014; 1: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Myers A, Quirk H, Lowe A, et al. The active hospital pilot: a qualitative study exploring the implementation of a trust-wide sport and exercise medicine-led physical activity intervention. PLOS ONE 2021; 16: e0257802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pavon JM, Fish LJ, Colón-Emeric CS, et al. Towards “mobility is medicine”: socioecological factors and hospital mobility in older adults. J Am Geriatr Soc 2021; 69: 1846–1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rasmussen RL, Holst M, Nielsen L, et al. The perspectives of health professionals in Denmark on physical exercise and nutritional interventions for acutely admitted frail older people during and after hospitalisation. Health Soc Care Community 2020; 28: 2140–2149. [DOI] [PubMed] [Google Scholar]
- 66.Wshah A, Selzler AM, Ellerton L, et al. Reducing sedentary behavior in individuals with COPD: healthcare professionals’ perspectives. Physiother Theory Pract 2021; 11: 1–12. [DOI] [PubMed] [Google Scholar]
- 67.Zisberg A, Agmon M, Gur-Yaish N, et al. No one size fits all – the development of a theory-driven intervention to increase in-hospital mobility: the “WALK-FOR” study. BMC Geriatr 2018; 18: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wray F, Coleman S, Clarke D, et al. Risk factors for manifestations of frailty in hospitalized older adults: a qualitative study. J Adv Nurs 2021; 6: 1688–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Klooster E, Koenders N, Vermeulen-Holsen J, et al. Healthcare professionals feel empowered by implementing a hospital-based multifaceted intervention: a qualitative study using inductive thematic analysis. BMC Health Serv Res 2022; 22: 903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Van Dijk-Huisman HC, Raeven-Eijkenboom PH, Magdelijns FJH, et al. Barriers and enablers to physical activity behaviour in older adults during hospital stay: a qualitative study guided by the theoretical domains framework. BMC Geriatr 2022; 22: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boltz M, Capezuti E, Shabbat N. Nursing staff perceptions of physical function in hospitalized older adults. Appl Nurs Res 2011; 24: 215–222. [DOI] [PubMed] [Google Scholar]
- 72.Chan DE-Y, Hong MLI, Tan MY, et al. Older patients’ participation in physical activity during hospitalization: a qualitative study of ward nurses’ perceptions in an Asian context. Geriatr Nurs 2019; 40: 91–98. [DOI] [PubMed] [Google Scholar]
- 73.Doherty-King B, Bowers B. How nurses decide to ambulate hospitalized older adults: development of a conceptual model. Gerontologist 2011; 51: 786–797. [DOI] [PubMed] [Google Scholar]
- 74.Doherty-King B, Bowers BJ. Attributing the responsibility for ambulating patients: a qualitative study. Int J Nurs Stud 2013; 50: 1240–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hills D, Ekegren C, Plummer V, et al. Nursing perspectives on reducing sedentary behaviour in sub-acute hospital settings: a mixed methods study. J Clin Nurs 2021; 31: 1348–1368. [DOI] [PubMed] [Google Scholar]
- 76.King BJ, Steege LM, Winsor K, et al. Getting patients walking: a pilot study of mobilizing older adult patients via a nurse-driven intervention. J Am Geriatr Soc 2016; 64: 2088–2094. [DOI] [PubMed] [Google Scholar]
- 77.Kneafsey R, Clifford C, Greenfield S. Perceptions of hospital manual handling policy and impact on nursing team involvement in promoting patients’ mobility. J Clin Nurs 2015; 24: 289–299. [DOI] [PubMed] [Google Scholar]
- 78.Lim S, Ibrahim K, Dodds R, et al. Physical activity in hospitalised older people: the feasibility and acceptability of a volunteer-led mobility intervention in the SoMoVe™ study. Age Ageing 2020; 49: 283–291. [DOI] [PubMed] [Google Scholar]
- 79.Lowe A, Littlewood C, McLean S. Understanding physical activity promotion in physiotherapy practice: a qualitative study. Musculoskelet Sci Prac 2018; 35: 1–7. [DOI] [PubMed] [Google Scholar]
- 80.Ohlsson-Nevo E, Andersson G, Nilsing Strid E. In the hands of nurses: a focus group study of how nurses perceive and promote inpatients’ needs for physical activity. Nurs Open 2020; 7: 334–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Osinaike J, Hartley SE. Physical activity counselling among junior doctors in the UK: a qualitative study. Health Educ J 2021: 001789692199907.80: 584–595. [Google Scholar]
- 82.Pedersen MM, Brødsgaard R, Nilsen P, et al. Is promotion of mobility in older patients hospitalized for medical illness a physician’s job? – an interview study with physicians in Denmark. Geriatrics 2020; 5: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pham L, Ziegert K. Ways of promoting health to patients with diabetes and chronic kidney disease from a nursing perspective in Vietnam: a phenomenographic study. Int J Qualit Stud Health Well-Being 2016; 11: 30722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scheerman K, Mesters JW, Borger JN, et al. Tasks and responsibilities in physical activity promotion of older patients during hospitalization: a nurse perspective. Nurs Open 2020; 7: 1966–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Williams TL, Smith B, Papathomas A. Physical activity promotion for people with spinal cord injury: physiotherapists’ beliefs and actions. Disabil Rehabil 2018; 40: 52–61. [DOI] [PubMed] [Google Scholar]
- 86.Geelen SJG, Van Dijk - Huisman HC, De Bie RA, et al. Barriers and enablers to physical activity in patients during hospital stay: a scoping review. Syst Rev 2021; 10: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seeger JPH, Koenders N, Staal JB, et al. Effects of general physical activity promoting interventions on functional outcomes in patients hospitalized over 48 hours: a systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health 2021; 18: 1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dahlke SA, Hunter KF, Negrin K. Nursing practice with hospitalised older people: safety and harm. Int J Older People Nurs 2019; 14: e12220. [DOI] [PubMed] [Google Scholar]
- 89.Valenzuela PL, Morales JS, Castillo-García A, et al. Effects of exercise interventions on the functional status of acutely hospitalised older adults: a systematic review and meta-analysis. Ageing Res Rev 2020; 61: 101076. [DOI] [PubMed] [Google Scholar]
- 90.Cortes OL, Delgado S, Esparza M. Systematic review and meta-analysis of experimental studies: in-hospital mobilization for patients admitted for medical treatment. J Adv Nurs 2019; 75: 1823–1837. [DOI] [PubMed] [Google Scholar]
- 91.Baldwin CE, Phillips AC, Edney SM, et al. Recommendations for older adults’ physical activity and sedentary behaviour during hospitalisation for an acute medical illness: an international Delphi study. Int J Behav Nutr Phys Activity 2020; 17: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Resnick BPC, Boltz MPC. Optimizing function and physical activity in hospitalized older adults to prevent functional decline and falls. Clin Geriatr Med 2019; 35: 237–251. [DOI] [PubMed] [Google Scholar]
- 93.de Morton N, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev 2007; 1: 1–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hokstad A, Indredavik B, Bernhardt J, et al. Hospital differences in motor activity early after stroke: a comparison of 11 Norwegian stroke units. J Stroke Cerebrovasc Dis 2015; 24: 1333–1340. [DOI] [PubMed] [Google Scholar]
- 95.Ribbe Kelso L, Stockton K, Mahendran N, et al. The influence of communal spaces on patient activity in rehabilitation: a mixed methods study. Disabil Rehabil 2023; 1: 1–13. [DOI] [PubMed] [Google Scholar]
- 96.Shannon MM, Elf M, Churilov L, et al. Can the physical environment itself influence neurological patient activity? Disabil Rehabil 2019; 41: 1177–1189. [DOI] [PubMed] [Google Scholar]
- 97.Rosbergen IC, Grimley RS, Hayward KS, et al. Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: a controlled before–after pilot study. Clin Rehabil 2017; 31: 1516–1528. [DOI] [PubMed] [Google Scholar]
- 98.Rosbergen ICM, Tonello I, Clark RA, et al. Does hospital design impact on patient activity levels and time spent alone? Disabil Rehabil 2022; 44: 3173–3180. [DOI] [PubMed] [Google Scholar]
- 99.Luker J, Lynch E, Bernhardsson S, et al. Stroke survivors’ experiences of physical rehabilitation: a systematic review of qualitative studies. Arch Phys Med Rehabil 2015; 96: 1698–1708. e1610. [DOI] [PubMed] [Google Scholar]
- 100.Scheerman K, Schoenmakers AHC, Meskers CGM, et al. Physical, motivational and environmental factors influencing physical activity promotion during hospitalization: older patients’ perspective. Geriatr Nurs 2021; 42: 599–604. [DOI] [PubMed] [Google Scholar]
- 101.Haddaway NR, Page MJ, Pritchard CC, et al. PRISMA2020: an R package and shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and open synthesis. Campbell Systematic Reviews 2022; 18: e1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cre-10.1177_02692155231170451 for Perspectives of health professionals on physical activity and sedentary behaviour in hospitalised adults: A systematic review and thematic synthesis by Tahlia Alsop, James Woodforde, Ingrid Rosbergen, Niruthikha Mahendran, Sandra Brauer, and Sjaan Gomersall in Clinical Rehabilitation