Abstract
Background:
Hallux valgus deformity consists of a lateral deviation of the great toe, metatarsus varus, and pronation of the first metatarsal. Most osteotomies only correct varus, but not the pronation of the metatarsal. Persistent postoperative pronation has been shown to increase deformity recurrence and have worse functional outcomes. The proximal rotational metatarsal osteotomy (PROMO) technique reliably corrects pronation and varus through a stable osteotomy, avoiding fusing any healthy joints. The objective of this research is to show a prospective series of the PROMO technique.
Methods:
Twenty-five patients (30 feet) were operated with the PROMO technique. The sample included 22 women and 3 men, average age 46 years (range 22-59), for a mean prospective follow-up of 1 year (range 9-14 months). Inclusion criteria included symptomatic hallux valgus deformities, absence of severe joint arthritis, or inflammatory arthropathies, with a metatarsal malrotation of 10 degrees or more, with no tarsometatarsal subluxation or arthritis on the anteroposterior or lateral foot radiograph views. The mean preoperative and postoperative Lower Extremity Functional Scale (LEFS) score, metatarsophalangeal angle, intermetatarsal angle, metatarsal malrotation, complications, satisfaction, and recurrence were recorded.
Results:
The mean preoperative and postoperative LEFS scores were 56 and 73. The median pre-/postoperative metatarsophalangeal angle was 32.5/4 degrees and the intermetatarsal angle 15.5/5 degrees. The metatarsal rotation was satisfactorily corrected in 24 of 25 patients. An Akin osteotomy was needed in 27 of 30 feet. All patients were satisfied with the surgery, and no recurrence or complications were found.
Conclusions:
PROMO is a reliable technique, with good short-term results in terms of angular correction, satisfaction, and recurrence. Long-term studies are needed to determine if a lower hallux recurrence rate occurs with the correction of metatarsal rotation in comparison with conventional osteotomies.
Level of evidence:
IV, prospective case series.
Keywords: hallux valgus, pronation, PROMO, osteotomy, recurrence
Commentary: Clinical paper reporting results of 30 feet treated with innovative bunion surgery. At short term follow up, excellent results with 24/25 have excellent deformity correction.
Introduction
More than 100 surgical techniques exist for the treatment of hallux valgus (HV). Numerous investigators have reported outcomes with different osteotomies and soft tissue procedures. Nevertheless, most of them only correct the metatarsal varus and not the internal rotation (pronation). Metatarsal pronation and its importance in the HV deformity has been known for more than 15 years.20,23,24,27 Just a few years ago publications started to appear again regarding the HV rotational component. Studies from Japan and South Korea were published in the last few years discussing different aspects of this metatarsal pronation. One study showed how postoperative sesamoid malposition had a negative influence on patient’s outcome after HV surgery. 3 It was also shown how metatarsal pronation could be evaluated analyzing the lateral shape of the first metatarsal head. 30 Regarding HV recurrence, incomplete reduction of the sesamoids and a round shape of the lateral edge of the first metatarsal head were demonstrated to be risk factors for HV recurrence.14,15 And finally, regarding metatarsal pronation incidence, it was shown that 87% of HV cases present with metatarsal internal rotation and that sesamoid subluxation and metatarsal pronation can coexist or not on a HV patient. 11 It is important to emphasize that sesamoids do not move from their original position. They are fixed in place by the flexor hallux brevis tendons to the proximal phalanx and by the intermetatarsal ligament to the second metatarsal. It is the metatarsal that primarily pronates and loses its original position.
Although there is a good amount of information regarding the importance of the rotational parameter in HV patients, no significant change in HV treatment has been seen in decades, with the same techniques being published repetitively. The authors’ interest in the tridimensional deformity involved in HV cases prompted the study and development of a new surgical technique that addresses both varus angulation and axial rotation of the metatarsal. This technique called the proximal rotational metatarsal osteotomy (PROMO) has been previously described.25,26
The goal of this study is to report the first prospective case series using this novel technique (PROMO) that accurately and reliably corrects the metatarsal pronation and varus. It is performed through a single proximal metatarsal oblique plane osteotomy, achieving any varus correction through rotation. No wedge resection is needed. The only requirement for this osteotomy to work is the coexistence of a metatarsal malrotation (87% of HV cases), given that only through derotation, coronal deformity can be corrected with this osteotomy. The direction of the oblique cut has to be precisely planned to achieve the desired rotational and varus correction.
Methods
Twenty-five patients (30 feet), 22 women and 3 men of average age 46 years (range 22-59), were operated using this technique and prospectively followed for a minimum of 9 months (average 12 months). Inclusion criteria included symptomatic HV deformities with a metatarsal malrotation of 10 degrees or more and an intermetatarsal angle between 11 and 20 degrees (Figure 1). Exclusion criteria were Juvenile HV, joint arthritis, inflammatory disease, and tarsometatarsal subluxation. Pre- and postoperatively (immediate and at final follow-up), the following parameters were registered on weight-bearing anteroposterior (AP) foot radiographs and axial sesamoid views: metatarsophalangeal angle, intermetatarsal angle (IMA), distal metatarsal articular angle, 4 sesamoid position (Hardy and Clapham classification 9 ), metatarsal rotation (metatarsal head round sign), 30 Lower Extremity Functional Scale (LEFS) score, and patient satisfaction (dissatisfied, somewhat dissatisfied, somewhat satisfied, satisfied). Complications such as deep venous thrombosis, infection, and HV recurrence were registered. HV recurrence was defined as a difference of more than 10 degrees on the hallux valgus angle (HVA) comparing the immediate and the final follow-up films or an HVA above 15 degrees at final follow-up. All patients received 15 days of postoperative deep venous thrombosis prophylaxis with rivaroxaban or dabigatran.
Figure 1.

Anteroposterior weight-bearing feet radiograph. Intermetatarsal angle is measured on left foot: 15 degrees; hallux valgus angle is measured on right foot: 30 degrees.
Preoperative Planning
Our aim in HV surgery was to relocate the first metatarsal to its original location. To perform this correction, an accurate deformity measurement of the varus and malrotation components had to be performed. The IMA was measured to evaluate metatarsus varus and was obtained by measuring the divergence between the first and second metatarsal. To measure metatarsal rotation, 4 methods were available. One option was a weight-bearing axial sesamoid view. Talbot and Saltzman originally described this angle.24,25 The authors use the Bernard view with a small modification, using a 3-cm heel lift and placing the foot in 20 degrees of external rotation and 20 degrees of toes dorsiflexion. 13 The x-ray cassette is placed behind the heel, parallel to the floor. To measure the metatarsal malrotation angle, a line is drawn connecting the most inferomedial border of the medial sesamoid facet and the most lateral border of the lateral sesamoid facet. Another line is drawn along the weight-bearing surface. The angle between these lines is the first metatarsal rotation (Figure 2). Another option is to perform a preoperative weight-bearing computed tomographic scan. The last method is by using the AP foot radiograph. A round shape on the lateral border of the metatarsal head is evidence of pronation given that metatarsal condyles appear on an AP view as the metatarsal externally rotates (Figures 3 and 4). 30 Given that progressive degrees of rotation show a progressive head shape roundness, the latter can be used to estimate the former. The authors strongly recommend reviewing Yamaguchi’s work as this is the most frequently used method by the authors. 30
Figure 2.

Metatarsal rotation measurement: Modified Bernard view (see text for details). Angle between a line drawn parallel to the floor and a line from the medial ridge of the medial sesamoid facet to the lateral ridge of the lateral sesamoid facet. Value: 15 degrees.
Figure 3.

Anteroposterior first metatarsal weight bearing view on a normal foot: a sharp edge can be seen on the lateral edge of the first metatarsal head. Sesamoids located under the head.
Figure 4.

Anteroposterior first metatarsal weight-bearing view on a hallux valgus foot: a round edge can be seen on the lateral edge of the first metatarsal head, which are the visible metatarsal condyles on a rotated metatarsal. Sesamoids rotated laterally from the head.
Once the rotational and varus deformity are measured, the osteotomy planning can take place. A geometrical principle describes that when rotation occurs through an oblique plane, a deformity appears. This concept was alreay used in the past to correct tibial Blount disease (varus, internal rotation).17,18 Hence, given that HV deformity includes a rotational and a frontal plane deformity, there is one specific oblique plane osteotomy that will correct both planes for any deformity. This was simplified in a Table (Table 1) that shows the osteotomy angulation that will correct a certain combination of metatarsal internal rotation and varus deformity.
Table 1.
Metatarsal Osteotomy Angle: Value Obtained from the IMA and Metatarsal Rotation Angles.
| Rotation Angles, degrees | ||||
|---|---|---|---|---|
| IMA angles, degrees | 10-19 | 20-29 | 30-39 | 40-50 |
| 8-10 | 38 | 28 | 23 | 13 |
| 11-12 | 47 | 33 | 28 | 18 |
| 13-14 | 55 | 38 | 33 | 23 |
| 15-17 a | 55 | 42 | 38 | 28 |
| 18-20 a | 55 | 47 | 42 | 33 |
Abbreviations: IMA, intermetatarsal angle.
Eventual tarsometatarsal (TMT) instability. Consider a screw or flexible suture device to the base of the second metatarsal through the plate, if TMT opens after the osteotomy. Add lateral displacement through osteotomy.
Surgical Technique
The surgical technique was slightly modified from the previous published technique (Wagner et al). 25 Once the varus and metatarsal rotation angle have been determined, on the calculations table (Table 1), the correct osteotomy angulation was located that the osteotomy needed to follow. In this case, an example with 15 degrees of metatarsal pronation and 12 degrees of IMA were analyzed. According to the table, an osteotomy in 47 degrees was needed.
Approach: A medial approach was performed from the metatarsal base to the mid-diaphysis (3 cm approximately). The metatarsal was exposed. A medial longitudinal line on the metatarsal equator was drawn from the base to the mid-diaphysis.
Positioning wire: Next, 1 cm distal to the tarsometatarsal joint (TMT), a No. 1.6 K-wire was drilled through the medial metatarsal cortex on the metatarsal midline. Then, under fluoroscopy, the lateral metatarsal cortex was drilled, making sure that the wire was perpendicular to the metatarsal bone on the AP plane and parallel to the foot sole on the axial plane. This was the most important step in the surgery. Aligning this wire correctly ensured an accurate deformity correction. Next, the positioning jig (Figure 5) was slid on the K-wire through the 0-degree hole and aligned along the metatarsal midline. A second K-wire was driven through the jig hole with the desired rotational correction (10-19 degrees hole in this case) while holding the jig onto the metatarsal. Then the 0-degree K-wire and positioning jig were removed.
Osteotomy: Next, the cutting jig (Figure 6) was taken and slid on the K-wire through the hole that matched the osteotomy calculated angulation (47 degrees in this case). A second K-wire was drilled through the distal jig hole on the metatarsal midline. Then, using a sawblade, the osteotomy was performed through the jig slot. The rotational jig (Figure 7) was then slid on the distal wire through the 0-degree hole. Then a second wire was driven through the rotation hole that matched the preoperative rotation (10-19 degree). The 0-degree wire was then removed.
Deformity correction: Then the distal bone segment was rotated to achieve parallel wires. A dorsal step-off occurred.
Osteotomy transient fixation: Two K-wires, plantar to dorsal, were driven through the osteotomy. These wires were driven parallel to each other and perpendicular to the osteotomy. Between these wires, enough space was left for an interfragmentary screw. The osteotomy was held with a clamp in case the wires did not stabilize the osteotomy enough. Radiography was used to check that the desired deformity correction was obtained (IMA and rotation through the metatarsal head shape). The lateral metatarsal head shape needed to be straight instead of round. At this point, the sesamoids could be not completely centered below the head. If this was the case, either more angular correction was needed, or a lateral metatarso-sesamoid ligament release needed to be performed. If more angular correction was desired, the distal metatarsal segment had to be displaced laterally (Chevron effect) to decrease the IMA. The rotation was not to be increased beyond the preoperative planning. Only a metatarsal head depression would have occurred if the rotation was exaggerated.
Plate application: Next, a locking plate was used medially to stabilize the osteotomy. It was ensured that no bumps or bone steps would avoid a flush position of the plate on the metatarsal. If this was the case, the sawblade was used to remove them. Before locking the plate, an interfragmentary screw was placed through the osteotomy. This screw had to be driven between the stabilizing K wires. The plate was applied and locked on the medial surface of the metatarsal. Fluoroscopy was used to check the desired bony correction and alignment.
Bunionectomy and/or Akin: Depending on the clinical appearance, it was decided whether a bunionectomy (medial eminence resection) and/or an Akin osteotomy was needed. If chosen, we proceeded with the usual metatarsophalangeal approach. Normally, no or minimal bunionectomy would be needed after the metatarsal rotational correction. Finally, the surgical approach was closed in the preferred fashion.
Figure 5.

First wire and positioning jig: Foot positioned over a flat surface. First wire is driven through the 0-degree hole on the jig, 1 cm distal to the joint on the metatarsal equator. It has to be parallel to the floor and perpendicular to the metatarsal.
Figure 6.

Cutting jig: Follow the cutting slot on the jig to perform the osteotomy at the desired angulation.
Figure 7.

Rotation jig: Slide the jig on the distal wire through the 0-degree hole. Add a new wire through the jig hole with the measured rotation. Then remove the 0-degree wire and the jig.
Postoperative Protocol
Immediate weight bearing was allowed as tolerated. As soon as wounds healed, daily active and passive hallux range of motion (especially plantar flexion) was recommended. Normally no physical therapy was necessary.
Results
All 25 patients were satisfied with the procedure at final follow up. The median pre and postoperative LEFS score was 56 (range 49-69) and 73 (range 65-80). Measurement on radiographs are shown in Table 2. All values significantly improved (Figure 8). Median preoperative / final postoperative HVA was 32.5/4 and IMA was 15.5/5 degrees respectively. Metatarsal length was not significantly altered (P = .13). Sesamoid position, metatarsal head round sign, metatarsal internal rotation and DMAA all significantly improved. There was one patient where a complete rotational correction was not achieved, without compromising the hallux valgus correction. This is one of the first patients in our series. No distal metatarsal osteotomy was performed in any case. An Akin osteotomy was needed in 27/30 feet and a bunionectomy in 7/30 feet. There was one patient who had signs of an abnormally increased TMT instability, given that after the osteotomy fixation there was an immediate increase of the IMA and recurrence of the HV deformity with an evident opening and gapping of the TMT. For this case, a screw was driven from the first to the second metatarsal base stabilizing the first metatarsal. No infections or deep venous thrombosis was seen. No patient had radiologic recurrence at final follow-up.
Table 2.
Radiologic Measures.
| Parameter | Preoperative Median (range) | Postopoperative Median (range) | Final Follow-up Median (range) | Significance Level (P Value) |
|---|---|---|---|---|
| Hallux valgus angle (degrees) | 32.5 (25-40) | 2 (-5-10) | 4 (1-11) | <.0001 |
| Intermetatarsal angle (degrees) | 15.5 (11-20) | 3 (1-8) | 5 (3-8) | <.001 |
| Metatarsal length (mm) | 63.5 (59-71) | 60 (58-70) | 60 (57-70) | .13 |
| Sesamoid position (Hardy and Clapham classification) | 5 (4-7) | 2 (1-4) | 3 (1-4) | <.01 |
| Metatarsal head round sign (present) | 25 (all) | 1/25 | 1/25 | <.001 |
| Metatarsal internal rotation (degrees) | 24 (18-30) | 8 (0-15) | 10 (3-18) | <.001 |
| Distal metatarsal articular angle (degrees) | 22.5 (5-45) | 5 (3-12) | 6 (4-12) | <.001 |
Figure 8.
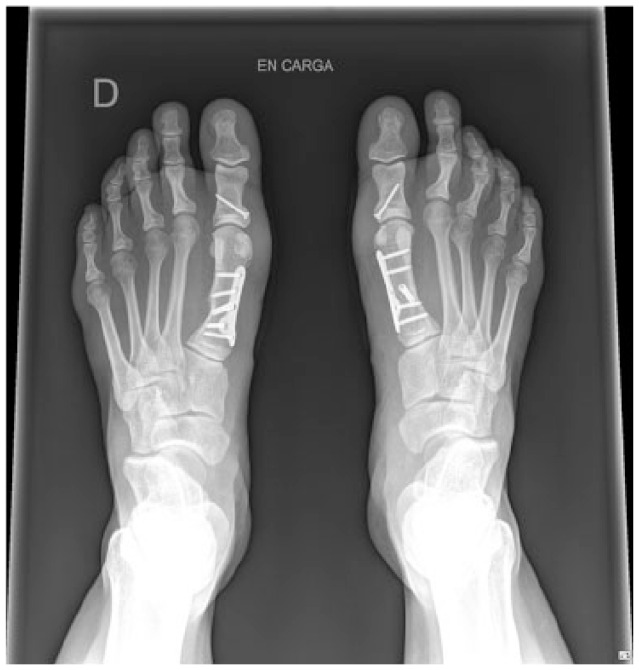
Anteroposterior weight bearing feet view: Postoperative image showing the deformity correction. The sesamoids are located under the head and the metatarsal head recovered its lateral sharp edge thanks to the rotational correction.
Discussion
Hallux valgus deformity consists of a first metatarsal varus, great toe valgus, and first ray pronation (present in 87% of HV) 11 The surgical techniques try to address HV deformity by reorienting the metatarsal through soft tissue procedures, metatarsal and/or phalangeal osteotomies, and through joint fusions. HV postoperative recurrence rate varies between different publications from 3% to 30%.1,2,6,7,19 There is even a long-term study that showed a recurrence rate higher than 50%. 10 As recurrence rate is evidently an outcome of utmost importance for HV patients, some of its factors have been studied. Two of them are the postoperative sesamoids reduction and lateral head shape.14,15 These factors are exclusively secondary to metatarsal malrotation and, therefore, is a deformity component that must be taken into account when planning an HV surgical correction. As previously said, Saltzman et al discussed the importance of the first ray rotation as part of HV deformity and how to measure it.20,21,23,24,27 5 to 10 years ago, a series of papers were published regarding the importance of the metatarsal pronation on functional outcomes and recurrence rate and how rotation could be evaluated by the lateral shape of the metatarsal head.3,11,14,15,30,31 Few studies recently showed how rotational correction can be achieved when performing a TMT fusion 12 or through a crescentic osteotomy 31 and how many degrees should be corrected to achieve rotational correction. 5 No technique has been described that reliably and accurately corrects both the metatarsal varus and pronation, with a stable osteotomy and with no unintended metatarsal shortening.
The rotational osteotomy presented here was initially described by Rab in 1988 for tibial Blount disease.17,18 In Blount disease there is a tibial varus and internal rotation deformity, therefore needing a 2-plane correction. Its main advantages are a broad bone contact, deformity correction capacity in 2 planes, and no loss of bone length. Its main downside is that the orientation of the osteotomy is paramount to obtain the desired correction. It consists of a single oblique cut, through which rotation is corrected. Because of the oblique nature of this osteotomy, while rotating the bone through this oblique plane the coronal deformity is corrected. Mathematical models, 22 graphical analysis 16 and 3-D planning 7 have been used to prove its utility in correcting long bone multiple plane deformities. 25
Our study is the first series with this novel technique. The PROMO technique shows excellent results. It significantly corrects the metatarsal varus and internal rotation. When analyzing the metatarsal rotation, sesamoid reduction and the lateral head shape, they all significantly correct postoperatively (Table 2). Standard hallux valgus angles (ie, HVA and IMA) greatly correct with this technique too. Surprisingly, the DMAA normalizes after the PROMO. One probable explanation for this normalization is that an abnormal DMAA, in the context of an adult patient with HV, is evidence of metatarsal rotation, and not a head dysplasia as commonly believed. Nevertheless, the authors recognize that an abnormal DMAA, in an adolescent or juvenile bunion, could be the result of a dysplastic head. A bunionectomy was seldom required, fact that shows that the medial head eminence is mostly evidence of metatarsal malrotation and not a real exostosis. Metatarsal length was not significantly altered, therefore minimizing the metatarsalgia risk, common after most of the other HV techniques (especially Lapidus). In case metatarsal shortening is desired, it can be performed through the osteotomy or by resecting a 2 mm bone slice using the cutting jig. The Akin osteotomy was performed in almost every patient. This fact is not explained by the concomitant presence of an interphalangeal deformity. Rather it is explained by the metatarsophalangeal deformity, as long-standing deformities change the soft tissue balance at the joint and therefore a rebalancing is needed to avoid persistent lateral subluxation of soft tissues and therefore possible recurrence of the deformity. The authors believe that the Akin osteotomy is indicated to manage the soft tissue imbalance present at the metatarsophalangeal joint and to achieve a better cosmetically looking foot. Although this is a very small series of patients, the authors have seen a reliable and rapid bone consolidation. This could be due to a large bone apposition area, a biomechanically well-oriented osteotomy that may compress with weight bearing, and an interfragmentary screw that gives better stability and osteotomy compression.
There is a small subgroup of patients with no preoperative radiologic evidence of tarsometatarsal instability, where after performing the metatarsophalangeal capsulotomy and/or metatarsal osteotomy an evident subluxation of the tarsometatarsal joint occurs, increasing the metatarsal varus deformity. These patients generally present with an IMA greater than 16 degrees. For the previously mentioned reason, when operating on severe HV cases, the authors recommend to be prepared in case an occult tarsometatarsal instability is evident intraoperatively. We recommend adding a first TMT stabilizing staple, a screw or flexible suture device between the first and second metatarsal base for these tarsometatarsal instability cases, which in our series was needed in 1 foot (1/30). Some surgeons would argue that a Lapidus is the procedure of choice for severe hallux valgus cases given its high correction power and that it addresses the TMT instability. Nevertheless, like all joint fusions, it has many drawbacks. Nonunions in joint arthrodesis happen in 10% to 20% of cases. The first TMT joint participates in gait, being part of the shock absorption mechanism. The foot deforms at heel contact, absorbing shock and distributing the plantar pressure to the heel and the heads of the metatarsals. A mobile first ray will dorsiflex on weight acceptance to prevent traumatizing the head of the first metatarsal. 8
Limited dorsal mobility after a Lapidus procedure can increase the plantar pressure beneath the first ray (up to 37% increase in midstance), and increases in contact pressures have been found also in the naviculocuneiform joint and fifth metatarsocuboid joint (27% and 40%, respectively). 28 Second metatarsal stress fractures may also occur because of stress increase in the second metatarsal bone after a Lapidus procedure (can also make the second metatarsal bone more susceptible to stress fractures, as stresses under the second metatarsal bone can increase up to 22% at the midstance phase of gait). 29 For all these reasons, fusing a joint (that is absolutely healthy) should not be taken lightly and should be thoroughly studied and analyzed before proceeding with it.
Drawbacks of this research are the small numbers of patients included, the short follow-up, and that the authors are the designers of the technique. An independent study with longer follow-up is needed to confirm the good results found in this research. This independent evaluation will be of use to evaluate the difficulty of this new technique and to identify areas that should be improved.
Conclusion
We found that the PROMO technique succesfully and accurately corrects the metatarsal varus and pronation deformity without bone resection. It addresses the HV deformity as a tridimensional problem correcting a well-known recurrence factor (metatarsal pronation). Long-term follow-up studies will be needed to demonstrate whether this technique maintains correction and prevents recurrence over time.
Footnotes
This article was originally published as: Wagner P, Wagner E. Proximal rotational metatarsal osteotomy for hallux valgus (PROMO): short-term prospective case series with a novel technique and topic review. Foot Ankle Orthop. 2018 Aug 30;3(3):2473011418790071. doi:10.1177/2473011418790071.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Pablo Wagner, MD, and Emilio Wagner, MD, have a patent pending relating to this research. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Pablo Wagner, MD,  https://orcid.org/0000-0003-4896-4434
https://orcid.org/0000-0003-4896-4434
References
- 1. Adam SP, Choung SC, Gu Y, O’Malley MJ. Outcomes after scarf osteotomy for treatment of adult hallux valgus deformity. Clin Orthop Relat Res. 2011;469(3):854-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bock P, Kluger R, Kristen KH, Mittlböck M, Schuh R, Trnka HJ. The scarf osteotomy with minimally invasive lateral release for treatment of hallux valgus deformity: intermediate and long-term results. J Bone Joint Surg Am. 2015;97(15):1238-1245. [DOI] [PubMed] [Google Scholar]
- 3. Chen JY, Rikhraj K, Gatot C, Lee JY, Singh Rikhraj I. Tibial sesamoid position influence on functional outcome and satisfaction after hallux valgus surgery. Foot Ankle Int. 2016;37(11):1178-1182. [DOI] [PubMed] [Google Scholar]
- 4. Coughlin MJ, Saltzman CL, Nunley JA, 2nd. Angular measurements in the evaluation of hallux valgus deformities: a report of the Ad Hoc Committee of the American Orthopaedic Foot & Ankle Society on Angular Measurements. Foot Ankle Int. 2002;23(1):68-74. [DOI] [PubMed] [Google Scholar]
- 5. Dayton P, Kauwe M, DiDomenico L, Feilmeier M, Reimer R. Quantitative analysis of the degree of frontal rotation required to anatomically align the first metatarsal phalangeal joint during modified tarsal-metatarsal arthrodesis without capsular balancing. J Foot Ankle Surg. 2016;55(2):220-225. [DOI] [PubMed] [Google Scholar]
- 6. Deveci A, Firat A, Yilmaz S, et al. Short-term clinical and radiologic results of the scarf osteotomy: what factors contribute to recurrence? J Foot Ankle Surg. 2013;52(6):771-775. [DOI] [PubMed] [Google Scholar]
- 7. Dobbe JG, Pre’ KJ, Kloen P, et al. Computer-assisted and patient specific 3-D planning and evaluation of a single-cut rotational osteotomy for complex long-bone deformities. Med Biol Eng Comput. 2011;49(12):1363-1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Glasoe WM, Yack HJ, Saltzman CL. Anatomy and biomechanics of the first ray. Phys Ther. 1999;79(9):854-859. [PubMed] [Google Scholar]
- 9. Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33:376-391. [DOI] [PubMed] [Google Scholar]
- 10. Jeuken RM, Schotanus MG, Kort NP, Deenik A, Jong B, Hendrickx RP. Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int. 2016;37(7):687-695. [DOI] [PubMed] [Google Scholar]
- 11. Kim Y, Kim JS, Young KW, Naraghi R, Cho HK, Lee SY. A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int. 2015;36(8):944-952. [DOI] [PubMed] [Google Scholar]
- 12. Klemola T, Leppilahti J, Kalinainen S, Ohtonen P, Ojala R, Savola O. First tarsometatarsal joint derotational arthrodesis. A new operative technique for flexible hallux valgus without touching the first metatarsophalangeal joint. J Foot Ankle Surg. 2014;53(1):22-28. [DOI] [PubMed] [Google Scholar]
- 13. Mortier JP, Bernard JL, Maestro M. Axial rotation of the first metatarsal head in a normal population and hallux valgus patients. Orthop Traumatol Surg Res. 2012;98(6):677-683. [DOI] [PubMed] [Google Scholar]
- 14. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009;91(7):1637-1645. [DOI] [PubMed] [Google Scholar]
- 15. Okuda R, Kinoshita M, Yasuda T, et al. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011;16(6):760-764. [DOI] [PubMed] [Google Scholar]
- 16. Paley D. Principles of Deformity Correction. Berlin: Springer; 2002:256-268. [Google Scholar]
- 17. Rab GT. Oblique tibial osteotomy for Blount’s disease (tibia vara). J Pediatr Orthop. 1988;8(6):715-720. [DOI] [PubMed] [Google Scholar]
- 18. Rab GT. Oblique tibial osteotomy revisited. J Child Orthop. 2010;4(2):169-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Raikin SM, Miller AG, Daniel J. Recurrence of hallux valgus: a review. Foot Ankle Clin. 2014;19:259-274. [DOI] [PubMed] [Google Scholar]
- 20. Saltzman CL, Brandser EA, Anderson CM, Berbaum KS, Brown TD. Coronal plane rotation of the first metatarsal. Foot Ankle Int. 1996;17(3):157-161. [DOI] [PubMed] [Google Scholar]
- 21. Saltzman CL, Aper RL, Brown TD. Anatomic determinants of first metatarsophalangeal flexion moments in hallux valgus. Clin Orthop Relat Res. 1997;339:261-269. [DOI] [PubMed] [Google Scholar]
- 22. Sangeorzan BJ, Sangeorzan BP, Hansen ST, Jr, et al. Mathematically directed single-cut osteotomy for correction of tibial malunion. J Orthop Trauma. 1989;3(4):267-275. [DOI] [PubMed] [Google Scholar]
- 23. Talbot KD, Saltzman CL. Assessing sesamoid subluxation: how good is the AP radiograph? Foot Ankle Int. 1998;19(8):547-554. [DOI] [PubMed] [Google Scholar]
- 24. Talbot KD, Saltzman CL. Hallucal rotation: a method of measurement and relationship to bunion deformity. Foot Ankle Int. 1997;18(9):550-556. [DOI] [PubMed] [Google Scholar]
- 25. Wagner P, Ortiz C, Wagner E. Rotational osteotomy for hallux valgus. A new technique for primary and revision cases. Tech Foot Ankle. 2017;16:3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wagner P, Ortiz C, Zanolli D, Keller A, Wagner E. Hallux valgus treatment. A tridimensional problem. Tobillo y pie. 2016;8(2):128-132. [Google Scholar]
- 27. Walsh SM, Saltzman CL, Talbot KD, Aper RL, Brown TD. In vivo validation of in vitro testing of hallucal flexor mechanics. Clin Biomech (Bristol, Avon). 1996;11(6):328-332. [DOI] [PubMed] [Google Scholar]
- 28. Wang Y, Li Z, Zhang M. Biomechanical study of tarsometatarsal joint fusion using finite element analysis. Med Eng Phys. 2014;36:1394-1400. [DOI] [PubMed] [Google Scholar]
- 29. Wong D, Zhang M, Yu J, Leung A. Biomechanics of first ray hypermobility: an investigation on joint force during walking using finite element analysis. Med Eng Phys. 2014;36:1388-1393. [DOI] [PubMed] [Google Scholar]
- 30. Yamaguchi S, Sasho T, Endo J, et al. Shape of the lateral edge of the first metatarsal head changes depending on the rotation and inclination of the first metatarsal: a study using digitally reconstructed radiographs. J Orthop Sci. 2015;20(5):868-874. [DOI] [PubMed] [Google Scholar]
- 31. Yasuda T, Okuda R, Jotoku T, Shima H, Hida T, Neo M. Proximal supination osteotomy of the first metatarsal for hallux valgus. Foot Ankle Int. 2015;36(6):696-704. [DOI] [PubMed] [Google Scholar]


