Abstract
Objective
Among hospitalised geriatric patients, only half are computer users. However, many of them refrain from using telehealth solutions. This study aimed to investigate geriatric patients’ computer and Internet habits and digital literacy and their associations with stress levels and frequency of Internet use.
Methods
Inpatients and outpatients aged 65 years or older, all computer users, were consecutively surveyed. Besides information about computer and Internet habits, computer support, and computer stress, the survey also collected information about digital literacy using the electronic Health Literacy Assessment toolkit.
Results
A total of 124 computer users with a mean age of 80.6 ± 7.4 years participated in the study from 1 October to 1 December 2019. Most patients received computer support from their children and grandchildren, whereas 6% did not seek support. They found themselves ‘most familiar with using a keyboard’ (79%), 59% ‘were unfamiliar with the Copy Paste function’, and only one-third ‘were open to new ways of using computers’. Digital literacy was associated with the frequency of Internet use (P = 0.001), and higher digital literacy was associated with less computer stress (P = 0.01).
Conclusions
Geriatric computer users are challenged by their basic computer skills, which may influence their choice of participation in telehealth solutions. If telehealth solutions are to succeed among geriatric patients, individualised computer support based on their basic computer skills and user-friendly computer devices are a prerequisite. For ongoing support, it is also necessary to introduce people close to the patient to telehealth solutions.
Keywords: Geriatrics, digital health literacy, technology, health technology, telehealth, physical activity older
Introduction
Digital immigrants are described as ‘those who learned to use computers at some stage during their adult life’ 1 ; older people fall into this category. In contrast, younger people are far ahead when it comes to digital solutions, for instance, owning a smartphone or using social media.2,3 Lesauskaitė et al. 4 found that as compared to geriatric patients, healthy older community dwellers are more prone to using new technologies, such as cell phones, computers, and the Internet.
Digital literacy and electronic health literacy
The measurement of digital literacy can help identify challenges related to using computers and other technological devices. There are several definitions of digital literacy; for example, the European Commission defines digital literacy in five digital areas of competencies: (a) information, (b) communication, (c) digital content creation, (d) safety, and (e) problem-solving. This comprehensive framework primarily guides European digital educational programmes. 5 Karnoe et al. 6 defined digital literacy more simply by relating it to basic digital skills and motivation divided into digital confidence, digital familiarity, and incentive to use technologies such as computers.
Basic computer skills are required when attending electronic health (eHealth) portals, such as searching for blood test results or making appointments with a general practitioner. These eHealth solutions are referred to as eHealth, which according to the World Health Organization (WHO) is defined as the use of information and communication technologies in health and health-related fields. 7 Ensuring that digital health services are available to as many people as possible requires a certain level of eHealth literacy. a van Deursen and Helpser 8 suggested that because the Internet is primarily text-based, it also requires a certain level of traditional literacy, such as reading, writing, and text-understanding skills, which might be easier to access for those with a higher level of education.
Computer support
Facing new digital solutions challenges older people, and computer support plays a vital role in adopting technology. Both family members and professional information technology (IT) staff can initiate computer use and be technical supporters in older people.9–11 However, the support required is multifaceted. In addition to providing information on devices available in the market, support is required to get these devices installed and, not least, to show older persons how to use them.
In particular, the oldest generations, from 75 years and above, require support only because these solutions are digital, 9 for instance, when adopting new digital self-service solutions called e-governance solutions, which are being increasingly offered by countries to their citizens.10,12–14 These solutions cover areas such as health, education, social, and employment contexts. 14 For instance, written inquiries to the public are now made through a digital mailbox.
However, citizens who cannot use these solutions are still allowed to receive posts by surface mail. 15 Again, the Central Authority on Statistics, Statistics Denmark, found that the largest proportion of the Danish population who opt out of digital solutions is that of the oldest citizens, where 30% of the citizens in the age group between 74 and 84 years deselect these digital solutions; this proportion increases to 62% for the age group 85 and up. 16
Computer stress and cognitive impairment
Confronting new digital solutions may also result in computer stress, which may be another barrier to computer use among older people.17,18 Folkman and Lazarus 19 defined stress as the ‘relationship between the person and the environment that the person appraises as relevant to his or her well-being and in which the person's resources are taxed or exceeded’. Arcury et al. 17 revealed that people who experienced stress while using a computer were less inclined to use the Internet than those who experienced no stress.
Some older persons struggle with cognitive impairments, which induce previous computer users to become non-users. 20 Despite cognitive challenges, older people still need to access telehealth solutions. These solutions are often simple and intuitive, requiring basic computer skills,21–25 such as using a keyboard, a touch screen, or another computer than their own. 26
Telehealth and geriatric patients
Telehealth covers many audiovisual two-way telecommunication technologies, including telemedicine and telerehabilitation.27,28 In situations where physical presence is difficult, telerehabilitation is a solution.29,30 This was a problem during the COVID-19 pandemic due to stay-at-home orders and restrictions on face-to-face activities to prevent the disease's spread.31,32 These restrictions might have resulted in physical inactivity, a problem for older people and a risk factor for developing frailty. 33 However, telehealth studies, such as telerehabilitation involving geriatric patients, are limited. 34
A previous feasibility study found recruiting geriatric patients for a telerehabilitation intervention impossible. One of the cited reasons for this was that they did not consider themselves to possess sufficient primary computer skills, even though they had a computer at home. 21 For future telehealth programmes, it is necessary to determine geriatric patients’ levels of digital literacy. Measuring digital literacy can be a first step in assisting this population in taking advantage of similar interventions. Therefore, to our knowledge, previous studies have yet to investigate digital literacy among geriatric in- and outpatients. We used the eHealth Literacy Assessment toolkit (eHLA) questionnaire to fill this gap.
This study aimed to determine the computer and internet habits of geriatric patients and whether their digital literacy is associated with the frequency of Internet use and related stress levels. Thus, this study sheds light on the challenges faced by older people when using digital solutions in an increasingly digitised future.
Research design and methods
We adopted a quantitative cross-sectional study design. The study period ran from 1 October to 1 December 2019. Inpatients and outpatients aged 65 years or older were consecutively included in the Department of Geriatrics at a hospital in Denmark. In this study, we assessed geriatric patients admitted to the emergency department (ED), inpatients from two geriatric wards, and outpatients referring to a geriatric falls clinic for eligibility.
The inclusion criterion was computer use before hospital admission. We excluded patients who did not understand Danish, were screened to be cognitively impaired, could not participate in the survey, or were terminally ill. All patients were screened for possible cognitive impairment using the Short Portable Mental Status Questionnaire (SPMSQ) to ensure valid patient responses. The SPMSQ, which comprises 10 items related to memory, orientation, attention, language, and calculation, was validated and translated into Danish. 35 The error range in the SPMSQ is 0–10, where four or more errors indicate possible impaired cognition. Since the SPMSQ only provides a momentary snapshot of the cognitive status and the interviews with some patients were conducted during their hospitalisation, the eHealth record (EHR) was reviewed for patients who made four or more errors in the SPMSQ. Patients whose records stated that they had normal cognitive function in everyday life before admission were included in the study; otherwise, they were deemed ineligible. We used the CROSS checklist for reporting survey studies from the EQUATOR network. 36
The primary outcome was the patients’ digital literacy, which was measured by the digital part of the eHLA questionnaire. Secondary outcomes involved stress related to computer use and the patients’ computer habits, such as frequency of internet use, computer support, digital services, and social networking, and whether digital literacy is associated with stress levels.
Data sources
The data in this study were obtained from three sources: one validated questionnaire, data collected via the EHR, and questions formulated by the authors:
-
Patient characteristics were retrieved from the patients’ EHRs, including information on age, sex, education level, state of frailty, habitation status, and housing.
Age was divided into three groups: (a) 65–74 years, (b) 75–84 years, and (c) ≥85 years.
Education level was categorised into four groups according to the former Danish education system: (a) those who had completed Grade 7, (b) those who had completed Grades 8–10, (c) trained workers, and (d) those who had completed high school and further or higher education.
Frailty was measured using the multidimensional prognostic index (MPI), a cumulative deficit model validated and translated into Danish based on the Comprehensive Geriatric Assessment.37,38 The MPI includes the following frailty predictors: social, medication, functional, cognitive, morbidity, nutritional, and pressure sore risk status. The MPI categorises patients into three levels: MPI-1, non-frail; MPI-2, moderately frail; and MPI-3, severely frail. 38
Habitation status was categorised into two groups: (a) living alone and (b) living with someone (spouse, next of kin, or partner).
Housing was categorised into three groups: (a) living in one's own home, (b) living in sheltered housing, and (c) living in an institution.
-
We measured digital literacy based on the eHLA questionnaire. eHLA was translated into English, validated, and tested on a general population sample and a sample referred to an outpatient clinic (N = 475), where 28% of the patients were 60 years or older. 6 eHLA is suitable for screening purposes in projects involving telehealth solutions 6 by ‘providing the means for gaining insight into people's health-related literacy as well as their confidence, familiarity, and motivation related to digital solutions’, such as computers. 6 The eHLA questionnaire is divided into seven tools that can be used together or separately: four with health literacy and the remaining three with digital literacy. We chose to use the three digital tools to investigate our respondents’ digital literacy, which primarily focused on basic computer skills and their incentives (motivation) to use computers. These tools comprise 14 questions reflecting (a) technology familiarity, (b) technology confidence, and (c) ‘incentive for engaging with technology’ in the analysis. 6 The items in the three digital tools in eHLA are rated on a 4-point Likert scale; the higher the score, the more digitally literate the participant is considered:
- Tool 5. Technology familiarity: ‘How familiar are you with the following items?’ The response options range from 1, not at all familiar, to 4, completely familiar (six questions).
- Tool 6. Technology confidence: ‘How confident do you feel…?’ The response options range from 1, very unconfident, to 4, very confident (four questions).
- Tool 7. Incentives for engaging with technology: ‘How much do you agree or disagree with the following statements?’ The response options range from 1, strongly disagree, to 4, strongly agree (four questions).
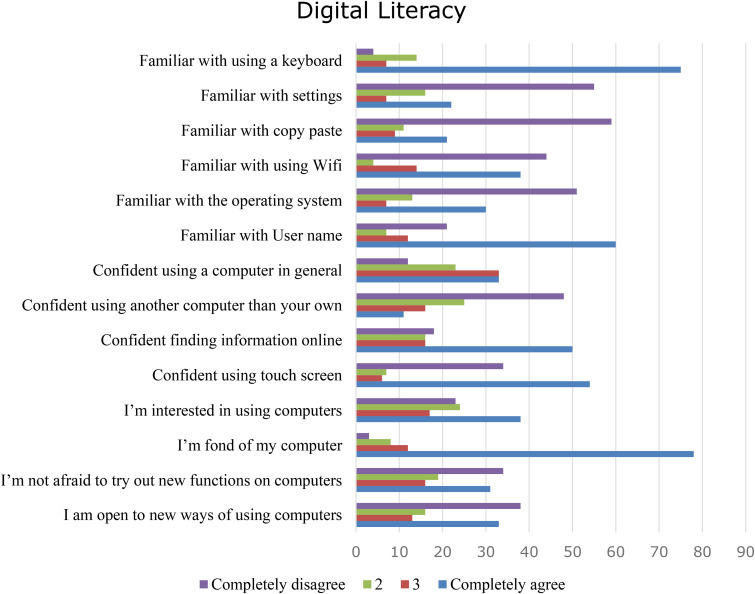
Words such as keyboard, user name, or touch screen were read in Danish and English if the respondents recognised only one of the languages. If the respondent was not conversant with the word technology, this was replaced with the word computer. All 14 questions are displayed in total length in Figure 1. 6
-
Additional questions collected information about the following:
Stress levels related to the use of the computer and internet were measured following Arcury et al.'s 17 study and divided into the following five levels: no, low, moderate, high, and very high stress.
Internet use frequency was categorised by Arcury et al. 17 into three groups: never, less than once a day, and at least once a day.
We counted the number of electronic devices categorised into computers, tablets, landline phones, mobile phones, and smartphones. These devices were chosen to represent technologies that older people frequently are expected to use.
Computer support was categorised into no support and support from a spouse/cohabitant, children/grandchildren, friends/acquaintances, or professional IT staff.
We asked the responders what they were searching on the Internet—for example, news, health information, YouTube, search engines (e.g. Google or Bing), games, and recipes. All items were in the form of yes/no questions.
We also asked what type of digital services the responders used—for example, Internet banking or patients’ digital mailboxes (e-Boks), a Danish national email service. All items were in the form of yes/no questions.
To obtain information on the respondents’ social networking practices, we asked if they were using Facebook, Instagram, Skype, or FaceTime. All items were in the form of yes/no questions.
Figure 1.
Digital literacy in geriatric computer users.
Data collection
Before the study began, two interviewers were trained in surveying by pretesting the questionnaire in a sample of patients recruited from the same geriatric wards and falls clinics where the study occurred. The two interviewers reached an agreement after 10 patients.
We conducted interviews with inpatients in the patients’ private hospital rooms and outpatients in facilities appurtenant to the falls clinic. The survey took about 20 minutes. Moreover, to avoid a low response rate, especially among the frailest patients, 39 the questionnaire was conducted orally by reading the questions aloud to the patients. The interviewers were aware of being as neutral as possible regarding the questions and the answers. Patients discharged directly from the ED were asked to be contacted by phone shortly after discharge. A project therapist was responsible for data registration in a REDCap database. 40
Sample size
To calculate the sample size, we performed a power analysis based on numbers from the Central Authority on Statistics, where 87% of people aged 21–64 years and 52% of people aged 65–89 years responded to what extent they feel equipped to use the Internet with their IT skills. 41 We included the proportion that answers ‘to a great extent or some extent’ in the two age groups in this power calculation. The power analysis indicated that 80 respondents were needed based on these percentages. To obtain a sufficient number of respondents for an adjusted analysis, we added 10% per variable, resulting in another 32 respondents corresponding to the four variables used in the analysis for adjustment. 42 Two-sample comparisons of proportions required a minimum of 112 patients for a significance level of 0.05 and a power of 90%.
Statistical analysis
The respondents’ characteristics, computer and Internet habits, use of electronic devices, and need for computer support were described as frequencies and percentages for categorical variables and as means and standard deviations (SD) for continuous variables. Digital literacy (the eHLA questionnaire) was presented by means of first adding the scores and then dividing the total score by the number of questions within the individual item. Linear regression analysis was performed to investigate associations between technology familiarity, confidence, incentives and stress levels, and Internet use frequency. The model was adjusted stepwise for age, sex, frailty, and level of education and was examined for confounding factors and effect modification. No effect modification was found. We used Stata version 17.
Compliance with ethical standards
This study was approved by the Danish Data Protection Agency (1-16-02-201-17) and complied with the principles of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. 43 According to the Committees on Health Research Ethics in Denmark, written informed consent is not required for health science questionnaire surveys and interview surveys that do not include human biological materials. 44 Therefore, written informed consent was not obtained in this study. Verbal informed consent was obtained from all subjects before the start of the survey, and everyone was informed of their right to withdraw their participation at any time. All questionnaire responses were anonymised.
Results
Respondents
The response rate was 96%; 124 geriatric computer users out of 129 responded to the survey.
The computer users had a mean age of 80.6 ± 7.4 years, and 58% were female. A total of 39% of the responders had further or higher education. Most (91%) were living in their own homes. One patient was staying in a nursing home, as seen in Table 1
Table 1.
Patient characteristics among geriatric computer users.
| Patient characteristics | N = 124 |
|---|---|
| Age, mean (SD) | 80.6 (7) |
| Sex, n (%) | |
| Male | 52 (42) |
| Female | 72 (58) |
| Patient groups, n (%) | |
| Inpatients | 82 (66) |
| Outpatients | 42 (34) |
| Housing, n (%) | |
| Own home | 113 (91) |
| Sheltered home | 10 (8) |
| Nursing home | 1 (1) |
| Living status, n (%) | |
| Living with someone | 51 (41) |
| Living alone | 73 (59) |
| Education, n (%) | |
| ≤7 years | 22 (18) |
| 8–10 years | 24 (19) |
| Trained worker | 30 (24) |
| High school, further or higher education | 48 (39) |
| Frailty, n (%) | |
| Non-frail | 47 (38) |
| Moderately frail | 60 (49) |
| Severely frail | 16 (13) |
| Missing | 1 (0.8) |
| Prescribed medication, n (%) | |
| 0–3 | 10 (8) |
| 4–7 | 45 (37) |
| 8 or more | 68 (55) |
| Missing | 1 (0.8) |
| Home help, n (%) | |
| No help | 74 (60) |
| Receive home help | 35 (29) |
| Receive help from relatives or friends | 14 (11) |
| Missing | 1 (0.8) |
Digital literacy
The respondents had a mean score in the following: technology familiarity: mean (±SD) 2.5 (0.9), range (1–4); technology confidence: mean (±SD) 2.8 (0.88), range (1–4); and technology incentive: mean (±SD) 2.8 (0.86), range (1–4).
As seen in Figure 1, the responders found themselves ‘most familiar with using a keyboard’ (79%). The following most familiar function when using a computer was writing their ‘user name’ (63%). The function the responders found ‘not at all familiar’ with is the ‘Copy Paste’ function (59%). One-third found themselves ‘completely confident’ in ‘using a computer in general’, but 46% ‘were not at all confident’ when ‘using another computer’. A total of 51% of the responders were ‘utterly confident in searching for information online’. A more significant part of the respondents corresponding to almost 80% were ‘fond of their computers’. However, only 37% were ‘interested in using computers’, and only one-third were ‘open to new ways of using computers’ (see Figure 1).
Stress levels, electronic devices, and computer and Internet habits
A total of 61% of the respondents experienced no stress while using a computer, whereas around 9% experienced high or very high stress levels. More than 90% of the respondents used a desktop and laptop computer, half were landline users, and 59% owned a smartphone. Divided by age, 87% in the 65–74 age group owned a smartphone. In the age group 75–84 years, 66% were smartphone owners and 29% in the age group 85 years or older. A total of 63% went online at least once a day. Internet banking and email were the two most frequently used internet services, whereas YouTube was used by only 2% of the respondents (see Table 2).
Table 2.
Computer and Internet habits.
| Computer users | N = 124 |
|---|---|
| Computer support, n (%) | |
| No support | 7 (6) |
| Support from spouse | 18 (13) |
| Support from children/grandchildren | 84 (65) |
| Support from friends | 22 (17) |
| Support from professional IT employee | 12 (10) |
| Frequency of internet use, n (%) | |
| Never | 4 (4) |
| Less than once a day | 40 (34) |
| At least once a day | 75 (63) |
| Missing | 5 (3) |
| Stress when using computer, n (%) | |
| No stress | 72 (61) |
| Low stress level | 22 (14) |
| Moderate stress level | 14 (12) |
| High stress level | 7 (6) |
| Very high stress level | 4 (3) |
| Missing | 5 (4) |
| Search the Internet, n (%) | |
| Facebook/Instagram | 47 (38) |
| Skype/FaceTime | 27 (22) |
| Health information | 58 (47) |
| Search engine (Google/Bing) | 26 (21) |
| Online news | 65 (52) |
| Internet banking | 98 (79) |
| 90 (70) | |
| YouTube | 3 (2) |
| Online games | 29 (23) |
| Recipes | 5 (4) |
| Others | 15 (12) |
| Use of electronic devices, n (%) | |
| Desktop or laptop computer | 114 (92) |
| Tablet | 50 (40) |
| Landline phone | 61 (50) |
| Mobile phone | 50 (41) |
| Smartphone | 73 (59) |
Computer support, search the Internet, and use of electronic devices have more answer options.
Computer support
A total of 6% of the respondents did not seek computer support, whereas 65% sought support from their children and grandchildren (see Table 2). As seen in Table 1, 41% were living with a spouse or cohabitant. Of those, 33% sought support from their partners, while 48% also sought support from their children and grandchildren. Among those living alone, 74% sought support from their children and grandchildren.
Digital literacy and the association between digital literacy and stress levels and digital literacy and Internet use frequency
Technology familiarity was not associated with stress levels when adjusting for age, sex, state of frailty, and education level. In terms of confidence in using computers (e.g. using a computer other than one's own or finding information online), no associations were found with stress levels after adjusting for age, sex, state of frailty, and education level (see Table 3). As seen in Table 3, the third dimension, incentives for engaging with technology, was significantly associated with less stress after adjusting for the characteristics mentioned above.
Table 3.
Associations between digital literacy and level of computer stress and Internet frequency.
| Coefficient | 95% confidence interval | P-value | Adjusted coefficient | 95% confidence interval | P-value | |
|---|---|---|---|---|---|---|
| Technology familiarity (n = 117), mean (±SD) 2.5 (0.9), range (1–4) | ||||||
| Level of computer stress | −0.2 | (−1.08; −0.65) | 0.6 | −0.16 | (−0.98; 0.66) | 0.7 |
| Frequency of Internet use | 4.5 | (2.96; 6.02) | 0.001 | 3.3 | (1.78; 4.79) | 0.001 |
| Technology confidence (n = 118), mean (±SD) 2.8 (0.9), range (1–4) | ||||||
| Level of computer stress | −0.40 | (−1.06; 0.07) | 0.09 | −0.41 | (−0.96; 0.15) | 0.12 |
| Frequency of Internet use | 3.1 | (2.10; 4.07) | 0.001 | 2.6 | (1.65; 3.62) | 0.001 |
| Technology incentive (n = 117), mean (±SD) 2.8 (0.9), range (1–4) | ||||||
| Level of computer stress | −0.78 | (−1.35; −0.21) | 0.008 | −0.76 | (−1.30; −0.20) | 0.008 |
| Frequency of Internet use | 3.4 | (2.35; 4.36) | 0.001 | 2.7 | (1.69; 3.72) | 0.001 |
Significant associations between Internet use frequency and technology familiarity, confidence, and incentive were found after adjusting for age, sex, state of frailty, and education level, as seen in Table 3. The lower the technology familiarity, confidence, and incentive, the lower the Internet use frequency.
Discussion
To the best of our knowledge, this survey is the first research study to investigate computer and internet use among a population of geriatric patients. The survey results indicated that most of the respondents were fond of their computers but only a few were confident in using others’ computers. More than a third were open to new ways of using computers. We found that internet banking and email were the most common reasons geriatric patients went online. Stress-related to computer use was not pervasive in this population. Higher digital literacy levels were associated with more frequent internet use. Children and grandchildren most commonly provided computer support to the elderly.
Digital literacy
In this survey, we evaluated the responders’ digital literacy based on the basic computer skills often required in telerehabilitation or other telehealth solutions. We found that older people faced challenges in these basic skills. Most respondents were fond of their computers, but they did not feel motivated enough to use others’ systems or to try new features on their own computers. However, using other systems or trying new features on their own computers can become a reality if they have to use a computer for telehealth solutions, such as telerehabilitation, if there, for instance, is a requirement for a specific exercise application or a particular screen size. They might also be required to operate in ‘Computer Settings’ and, for instance, add an external camera or a load speaker. 26 These are all essential skills for younger computer users. However, the telehealth solutions offered to older people can provide support in advance for setting up a computer and installing various computer devices. This support could be based on their level of digital computer literacy.
We assessed the digital literacy level using the eHLA questionnaire's digital part. 6 Holt et al. 45 used eHLA among entry-level nursing students with a mean age of 24.6 years. These young students achieved a mean score of 3.52 (3.25–4.00) for technology familiarity, 3.41 (3.00–4.00) for technology confidence, and 3.46 (3.16–4.00) for technology incentive. These authors achieved similar results for an older population with a mean age of 56.5 (18–89 years) while examining differences in eHealth literacy levels between users and non-users of digital health services. 46 A four-patient case study succeeded in conducting telerehabilitation in a geriatric population and found, like the two studies mentioned above, an almost 1-point higher score in all three dimensions of the digital part of the eHLA questionnaire than in the present study. 26 However, whether the scores found in the three studies indicate an appropriate level of digital literacy to adopt a digital solution has yet to be further discovered, for example, by developing cut-off scores. These cut-off scores can be applied to selected populations before introducing a new digital solution.
Stress levels
The adoption of computer technology is complex. Learning ‘computer language’ can be challenging; older people even forget the key to press on the keyboard. 47 For some, this may be stressful and associated with less frequent use of the Internet and lower eHealth literacy. 17 Only approximately 10% of the respondents in the present study experienced high or very high stress levels when using a computer. Yagil et al. 48 examined everyday technologies (EDTs) and their associations with self-efficacy, stress appraisal, and coping strategies. They defined self-efficacy as ‘a personal resource significantly affecting stress and coping’. They hypothesised that high EDT self-efficacy generates an inner and social responsibility to at least try to use the technology, which might generate stress. Contrary to their expectations, they found a positive association between EDT self-efficacy and stress related to EDT use. In our study, the observed lack of stress in geriatric patients with low digital literacy may be because they know they can ask for support or drop out of the technology and seek another solution. In an interview, Schreurs and Quan-Haase 12 found that older adults did not worry about their less experience with technology compared to younger generations; instead, their reactions were of being amazed and staying positive. We cannot rule out the fact that the same reasons for not experiencing stress also apply to our population. However, referring to the last tool in the eHLA questionnaire, which investigates motivation or incentives for engaging with computer technology, we found that lower motivation led to increased stress levels among the respondents. Arcury et al. 17 found an association between computer stress and the degree of eHealth literacy. The less literate they believed they were, the more computer-related stress they experienced. Czaja et al. 49 investigated the relationship between computer use and anxiety and found that those who did not believe in their computer skills experienced more anxiety related to computer use. Ellis et al. 50 found a negative association between computer interest and anxiety. The fact that respondents in the present study could see an advantage in using computers and were curious and dared to learn more digital skills can be a motivating factor, 51 which may primarily come from those who already have a certain degree of digital literacy and vice versa. For those with weak digital skills, the motivation disappears and computer stress arises.
Frequency of Internet use
Unsurprisingly, we found strong associations between the frequency of internet use and digital literacy. The higher the degree of digital literacy, the more frequent the Internet use. Frequency of internet use was also related to age, with 86% of the respondents aged 65–74 years going online at least once a day but only 55% of those aged 75 years or older going online on a daily basis. In 2017–2018, Statistics Denmark found somewhat lower percentages, with 51% of people aged 65–74 years and 23% of people aged 75 years or older going online several times a day. Whether this difference in proportions in the same age groups is due to our study asking about going online once a day and Statistics Denmark asking about several times a day cannot be determined. However, it seems that this population of cognitively well-functioning geriatric patients’ frequency of computer use does not lag behind that of the older population in general.
Computer support
In the present study, most geriatric patients receive computer support from their children or grandchildren; only 10% rely on professional IT assistance, and 6% receive no support. Arcury et al. 17 found that computer support was linked to being married. Berner et al. 52 concluded that living with someone allows computer users to seek support from their partners if necessary. In our study, 13% sought computer support from their partners. However, almost half of those living with someone also sought support from their children or grandchildren. Similarly, Luijkx et al. 11 found in an interview that children and grandchildren were more often involved in providing IT solutions to older relatives, even though the older persons were married. This support suggests that older people depend on younger generations even if they live with someone. This may be because their spouse is of the same age, and their computer skills are no better, perhaps even worse.
Among those living alone, who constituted the majority of our population, 74% sought computer support from their children and grandchildren. Thus, both groups frequently resorted to these younger generations for their computer problems. These findings are in line with those obtained by Schreurs and Quan-Haase 12 and Hayat et al., 53 who postulated that older people achieve the best introduction to and learning for computer devices and support access to online health information in a social context through family, friends, and peers. All of this could result in improved health outcomes. Therefore, it is important to ask patients from whom they seek support and suggest that those ‘helpers’, if possible, participate when the patients are introduced to telehealth solutions. For those for whom social ties are not always present, involving a caregiver might be a more viable solution.
Education level
The education level of geriatric computer users in the present study was higher than that of computer non-users found in a previous study conducted among the same population. 54 In that study, 50% had finished seventh grade, while only 16% had undertaken further education. 54 In the present study, only 18% had finished seventh grade, whereas a more significant proportion (39%) had a higher education level. These differences can be explained by the exclusion of computer non-users in the present study. Other studies have found that education level influences computer and internet usage.17,52 Berner et al. 52 postulated that a higher education level suggests curiosity to learn new skills, thus facilitating familiarisation with using a computer. A recent study by Bevilacqua et al. 55 has shown that eHealth training in older people has improved digital competence related to health.
Age-related cognitive challenges
We excluded patients with an SPMSQ of four or more errors in this study. This decision was made for the following reasons: to ensure that we got valid answers from the responders and because we expected cognitively impaired older people to be too challenged when it came to computer use and telehealth solutions, such as telerehabilitation. Instead, they need a face-to-face training offer, for instance, at a community centre for older people or in their own homes under the supervision of a physiotherapist. However, the COVID-19 pandemic forced many older people to avoid social contact; thus, this physical training was not possible. 31 In the future, it is essential to be more proactive and to develop telehealth solutions that can be used in connection with, for instance, telerehabilitation interventions directed at older people with cognitive impairment. The equipment used must be as intuitive and user-friendly as possible, just as turning on the television. 56
Strengths and limitations
All patients in contact with the geriatric ward during the specified period were consecutively screened for eligibility, resulting in a response rate of 96%. Research within this population is often challenging.57,58 We could have expected a low response rate in this study, too, and thus lower generalisability, as only the non-frail patients responded to the questionnaire. A low response rate was avoided by reading the questions aloud to all the participants. This high response rate has ensured good external validity.
Using the eHLA questionnaire gives specific examples of computer functions that the responders find challenging, such as the Copy Paste function or using a computer other than their own. More studies in the future where eHLA is used may give a more precise indication of which score indicates that the person is digitally literate to use a computer without the need for support and which scores indicate that the person needs support.
Older people are challenged by age-related cognitive changes. 20 As the average life expectancy increases, there will similarly be an increase in the number of older people with cognitive challenges. Czaja et al. 20 discuss the impact of age-related changes in cognition on the use of computers and other technological solutions. To screen for cognitive abilities, we used the SPMSQ. However, the SPMSQ is only a screening tool. We chose to exclude cognitively weak geriatric patients. We did not make an in-depth examination of the responders’ cognitive abilities. Cognitive disorders not captured by the SPMSQ might contribute to the explanation of this older population's level of digital literacy.
Conclusion
This study found cognitively well-functioning geriatric computer users to be fond of their computers, but only about a third were interested in computers and open to new ways of using them. The digital literacy rate decreases with age, and the frequency of internet use is associated with digital literacy. In general, most geriatric computer users do not experience computer stress, but they are challenged by their basic computer skills, which may influence their choice of participation in telehealth solutions. Therefore, ongoing support shall be provided if possible by family or caregivers or other persons close to the older person.
Perspective
Knowing the computer and internet habits of the oldest population is vital to help this group move towards more digitally connected lives.
Although most patients in this study used a desktop computer, it should be possible to access telehealth solutions from other devices, such as tablets or smartphones. These devices may be more manageable for some patients to use. User involvement in the earliest stages may be crucial when developing computer devices. Older potential telehealth users are a very heterogeneous group; therefore, there must be representatives from different age groups and education levels, and the least educated must also be involved. It may be necessary to make more targeted efforts to offer courses in the use of computers and the Internet among older citizens. These courses could be based on a measurement of their digital literacy. Future studies should explore initiatives that can increase digital literacy among older computer users, as well as what motivates them to use a computer and what they need to develop their computer skills, all of which can contribute to increasing the adoption of telehealth solutions.
Acknowledgements
The authors would like to thank all who contributed to this study, including the patients, the staff in the falls clinic, and the two geriatric wards at Aarhus University Hospital.
eHealth literacy is defined as ‘the ability to seek, find, understand and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem’.
Footnotes
Authors’ note: According to the Committees on Health Research Ethics in Denmark, written informed consent is not required for health science questionnaire surveys and interview surveys that do not include human biological materials. All questionnaire responses were anonymised. The patients provided verbal consent and were informed of their right to withdraw their participation at any time.
Contributorship: BBJ researched the literature, and BBJ, MG, and EMSD conceived the study. BBJ was involved in protocol development and patient recruitment and wrote the overall manuscript, and BBJ and MG made the data analysis. MG, SHP, and EMSD wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Compliance with ethical standards: This study was approved by the Danish Data Protection Agency (1-16-02-201-17) and complied with the principles of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. 43 According to the Committees on Health Research Ethics in Denmark, written informed consent is not required for health science questionnaire surveys and interview surveys that do not include human biological materials. 44 Therefore, written informed consent was not obtained in this study. Verbal informed consent was obtained from all subjects before the start of the survey, and everyone was informed of their right to withdraw their participation at any time. All questionnaire responses were anonymised.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: BBJ, at the Department of Geriatrics, Aarhus University Hospital, Denmark, is the guarantor for the article.
ORCID iD: Bodil B Jørgensen https://orcid.org/0000-0002-0447-5578
References
- 1.Wang Q, Myers MDP, Sundaram D. Digital natives and digital immigrants: towards a model of digital fluency. Bus Inf Syst Eng 2013; 5: 409–419. [Google Scholar]
- 2.The Danish Agency for Culture and Palaces. The development of the media in Denmark. Social media, https://mediernesudvikling.kum.dk/fileadmin/user_upload/dokumenter/medier/Mediernes_udvikling/2019/Specialrapporter/Sociale_medier_indhold/Sociale_medier_-_brug__indhold_og_relationer.pdf (2020).
- 3.Pew Research Center. Internet/Broadband Fact Sheet, https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ (2020, accessed 07 April 2021).
- 4.Lesauskaitė V, Damulevičienė G, Knašienė J, et al. Older adults-potential users of technologies. Medicina (Kaunas, Lithuania) 2019; 55: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vuorikari R, Punie Y, Van den Brande L. DigComp 2.0: the European Digital Competence Framework for Citizens. Update Phase 1: the conceptual reference model. 2016.
- 6.Karnoe A, Furstrand D, Christensen KB, et al. Assessing competencies needed to engage with digital health services: development of the eHealth literacy assessment toolkit. J Med Internet Res 2018; 20: e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Digital health for the end TB strategy: progress since 2015 and future perspectives: meeting report, 7-8 February 2017. Geneva: World Health Organization, 2017. [Google Scholar]
- 8.van Deursen AJAM, Helsper EJ. A nuanced understanding of Internet use and non-use among the elderly. Eur J Commun 2015; 30: 171–187. [Google Scholar]
- 9.Statistisk Denmark. IT anvendelse i befolkningen [ICT use in households and by individuals 2021], https://www.dst.dk/Site/Dst/Udgivelser/GetPubFile.aspx?id=39431&sid=itbef2021 (2021, accessed 01 March 2022).
- 10.Peek STM, Luijkx KG, Rijnaard MD, et al. Older adults’ reasons for using technology while aging in place. Gerontology (Basel) 2016; 62: 226–237. [DOI] [PubMed] [Google Scholar]
- 11.Luijkx KG, Peek STM, Wouters EJM. “Grandma, you should do it—it’s cool”: older adults and the role of family members in their acceptance of technology. Int J Environ Res Public Health 2015; 12: 15470–15485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schreurs K, Quan-Haase A, Martin K. Problematizing the digital literacy paradox in the context of older adults’ ICT use: aging, media discourse, and self-determination. Can J Commun 2017; 42: 359–377. [Google Scholar]
- 13.Anderson M, Perrin A. Tech adoption climbs among older adults, https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/ (2017, accessed 17 May 2017).
- 14.Digital Nations. Leading digital nations, https://www.leadingdigitalgovs.org/organization (2020, accessed 17 November 2020).
- 15.Tassy A, Nielsen MB, Jakobsen DT. It-anvendelse i befolkningen 2017, Danmarks Statistik, https://www.dst.dk/Site/Dst/Udgivelser/GetPubFile.aspx?id=20739&sid=itbef2017 (2018, accessed 09 May 2018).
- 16.Digitaliseringsstyrelsen. It-løsninger, https://digst.dk/it-loesninger/digital-post/om-loesningen/tal-og-statistik-om-digital-post/ (2020, accessed 17 November 2020).
- 17.Arcury TA, Sandberg JC, Melius KP, et al. Older adult Internet use and eHealth literacy. J Appl Gerontol 2020; 39: 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peel NM, Russell TG, Gray LC. Feasibility of using an in-home video conferencing system in geriatric rehabilitation. J Rehabil Med 2011; 43: 364–366. [DOI] [PubMed] [Google Scholar]
- 19.Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985; 48: 150–170. [DOI] [PubMed] [Google Scholar]
- 20.Czaja SJ, Lee CC. The impact of aging on access to technology. Univers Access Inf Soc 2007; 5: 341–349. [Google Scholar]
- 21.Jørgensen BB, Gregersen M, Pallesen SH, et al. A group-based real-time videoconferencing telerehabilitation programme in recently discharged geriatric patients: a feasibility study. Eur Geriatr Med 2021; 12: 801–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hong J, Kong HJ, Yoon HJ. Web-based telepresence exercise program for community-dwelling elderly women with a high risk of falling: randomized controlled trial. JMIR mHealth uHealth 2018; 6: e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smaerup M, Grönvall E, Larsen SB, et al. Computer-assisted training as a complement in rehabilitation of patients with chronic vestibular dizziness—a randomized controlled trial. Arch Phys Med Rehabil 2015; 96: 395–401. [DOI] [PubMed] [Google Scholar]
- 24.Tsai LL, McNamara RJ, Moddel C, et al. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR study. Respirology (Carlton, VIC) 2017; 22: 699–707. [DOI] [PubMed] [Google Scholar]
- 25.Crotty M, Killington M, van den Berg M, et al. Telerehabilitation for older people using off-the-shelf applications: acceptability and feasibility. J Telemed Telecare 2014; 20: 370–376. [DOI] [PubMed] [Google Scholar]
- 26.Jørgensen BB, Gregersen M, Holm-Pallesen S, et al. Tele-rehabilitation in community-dwelling older people with reduced functional capacity: a 4-patient case report. Gerontol Geriatr Med 2022; 8: 233372142211098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manocchia A. Telehealth: enhancing care through technology. R I Med J (2013) 2020; 103: 18–20. [PubMed] [Google Scholar]
- 28.Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 1595–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buvik A, Bugge E, Knutsen G, et al. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare 2018; 25: 451–459. [DOI] [PubMed] [Google Scholar]
- 30.Zhou F, Wang Z, Mai X, et al. Online clinical consultation as a utility tool for managing medical crisis during a pandemic: retrospective analysis on the characteristics of online clinical consultations during the COVID-19 pandemic. J Prim Care Community Health 2020; 11: 2150132720975517–2150132720975517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goethals L, Barth N, Guyot J, et al. Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: qualitative interview study. JMIR Aging 2020; 3: e19007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inf Assoc: JAMIA 2020; 27: 1147–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A 2001; 56: M146–M157. [DOI] [PubMed] [Google Scholar]
- 34.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975; 23: 433–441. [DOI] [PubMed] [Google Scholar]
- 36.Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med 2021; 36: 3179–3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pilotto A, Ferrucci L, Franceschi M, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res 2008; 11: 151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gregersen M, Hansen TK, Jørgensen BB, et al. Frailty is associated with hospital readmission in geriatric patients: a prognostic study. Eur Geriatr Med 2020; 11: 783–792. [DOI] [PubMed] [Google Scholar]
- 39.Keränen NS, Kangas M, Immonen M, et al. Use of information and communication technologies among older people with and without frailty: a population-based survey. J Med Internet Res 2017; 19: e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.University V. REDCap, https://www.project-redcap.org/ (2017, accessed 2017).
- 41.Statistics of Denmark. IT anvendelse i befolkningen 2017 [ICT use in households and by individuals 2017], https://www.dst.dk/da/Statistik/Publikationer/VisPub?cid=20739 (2017, 2018).
- 42.Kirkwood BR, Sterne JAC. Essential medical statistics. Hoboken, UK: John Wiley & Sons, Incorporated, 2003. [Google Scholar]
- 43.Cantín M. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Reviewing the latest version. Int J Med Surg Sci 2018; 1: 339–346. [Google Scholar]
- 44.Sundheds- og Ældreministeriet. Bekendtgørelse af lov om videnskabsetisk behandling af sundhedsvidenskabelige forskningsprojekter og sundhedsdatavidenskabelige forskningsprojekter, https://www.retsinformation.dk/eli/lta/2020/1338 (2020, accessed 01 September 2020).
- 45.Holt KA, Overgaard D, Engel LV, et al. Health literacy, digital literacy and eHealth literacy in Danish nursing students at entry and graduate level: a cross sectional study. BMC Nurs 2020; 19: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holt KA, Karnoe A, Overgaard D, et al. Differences in the level of electronic health literacy between users and nonusers of digital health services: an exploratory survey of a group of medical outpatients. Interact J Med Res 2019; 8: e8423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Terp R, Kayser L, Lindhardt T. Older patients’ competence, preferences, and attitudes toward digital technology use: explorative study. JMIR Hum Factors 2021; 8: e27005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yagil D, Cohen M, Beer JD. Older adults’ coping with the stress involved in the use of everyday technologies. J Appl Gerontol 2016; 35: 131–149. [DOI] [PubMed] [Google Scholar]
- 49.Czaja SJ, Charness N, Fisk AD, et al. Factors predicting the use of technology: findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychol Aging 2006; 21: 333–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ellis D, Allaire JC. Modeling computer interest in older adults: the role of age, education, computer knowledge, and computer anxiety. Hum Factors 1999; 41: 345–355. [DOI] [PubMed] [Google Scholar]
- 51.Norgaard O, Furstrand D, Klokker L, et al. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowl Manage e-Learning 2015; 7: 522–540. [Google Scholar]
- 52.Berner J, Rennemark M, Jogréus C, et al. Factors influencing Internet usage in older adults (65 years and above) living in rural and urban Sweden. Health Inf J 2015; 21: 237–249. [DOI] [PubMed] [Google Scholar]
- 53.Hayat TZ, Brainin E, Neter E. With some help from my network: supplementing eHealth literacy with social ties. J Med Internet Res 2017; 19: 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jørgensen BD, Damsgaard EM, Simonsen MMet al. et al. Prevalence of computer use among geriatric in- and outpatients. Gerontol Geriatr Med 2022; 8: 233372142211006. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bevilacqua R, Strano S, Di Rosa M, et al. eHealth literacy: from theory to clinical application for digital health improvement. Results from the ACCESS training experience. Int J Environ Res Public Health 2021; 18: 11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soendergaard M, Kristensen K. Videolink, a real-life videoconferencing system where relatives or health professionals can get in touch with older persons via their television, https://careware.dk/p-dage/praesentationsdage/praesentationsdag-naervaer-paa-afstand-juni-2020/videolink/ (2020, accessed 2020).
- 57.Zulman DM, Sussman JB, Hayward RA. Inclusion and analysis of older adults in RCTs. J Gen Intern Med: JGIM 2011; 26: 832–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Veronese N, Petrovic M, Benetos A, et al. Underrepresentation of older adults in clinical trials on COVID-19 vaccines: a systematic review. Ageing Res Rev 2021; 71: 101455–101455. [DOI] [PMC free article] [PubMed] [Google Scholar]