Abstract
Stress fractures of the foot and ankle are common injuries in athletes. Management differs considerably based on fracture location and predisposing factors. Repetitive loading of the foot and ankle in athletes should result in physiologic bone remodeling in accordance with Wolff’s law. However, when there is not sufficient time for complete healing to occur before additional loads are incurred, this process can instead lead to stress fracture. Assessment of the athlete’s training regimen and overall bone health is paramount to both the discovery and treatment of these injuries, although diagnosis is often delayed in the setting of normal-appearing initial radiographs. While most stress fractures of the foot or ankle can usually be treated nonoperatively with a period of activity modification, fractures in certain locations are considered “high risk” due to poor intrinsic healing and may warrant more proactive operative management.
Keywords: stress fracture, foot, ankle, athlete
Commentary: Concise summary of the treatment of stress fractures of the foot and ankle including the tibia and fibula. Outlines recommended treatment for the various low risk fractures and in more depth discusses treatment of higher risk fractures such as talus, metatarsal base and anterior tibia fractures. Includes section on prevention, female athletes, pediatric patients and lab evaluation.
Stress fractures of the foot or ankle account for approximately 10% of injuries seen in recreational and competitive athletes.1,5,7,49,66 Repetitive submaximal mechanical loading triggers physiologic bone adaptation, but when such forces exceed a bone’s reparative ability, then the resulting imbalance between bone formation and resorption can lead to microscopic bone injury.11,17 As this microscopic damage accumulates, it creates an injury spectrum that can include reactive bone edema visible only by magnetic resonance imaging (MRI), an incomplete or nondisplaced fracture line seen on various imaging modalities, or a displaced fracture that is clearly visible on plain radiographs.
Both intrinsic and extrinsic factors contribute to development of a stress fracture. Intrinsic factors typically are nonmodifiable and include the athlete’s age, sex, genetics, hormonal imbalance, vascularity of the injured area, overall bone health, and bone density. Extrinsic factors, on the other hand, are modifiable and include the athlete’s diet, weight, medications, chosen sport, training regimen, protective equipment, biomechanics, and technique.
Clinical Evaluation
Stress fractures should be considered in any athlete presenting with the insidious onset of lower extremity pain over a period of days to weeks, especially in the setting of a sudden change in activity or training level. Generally, symptoms are activity dependent, and clinical history should focus on intrinsic and extrinsic risk factors.
Physical examination of the athlete should begin with assessment of overall lower extremity alignment, gait, and range of motion. Even mild overuse in the presence of subtle deviations from normal alignment can lead to overload of certain regions in the ankle and foot. Since overt swelling may or may not exist, explicit knowledge of anatomy can be critical in correlating direct palpation tenderness to the diagnosis of a particular stress fracture. Anatomically localizable discomfort is frequently present but requires careful examination and a high index of suspicion.
Imaging
Weightbearing orthogonal radiographs of the affected area are essential, bearing in mind that the sensitivity of plain radiographs for stress fracture at the time of symptom onset is poor; up to 85% can be negative.60,70,71 Repeat radiographs taken a few weeks later, however, may show periosteal new bone formation to confirm the diagnosis.
Historically, bone scintigraphy was the gold standard to diagnose stress fractures given its near 100% sensitivity within the first 48 to 72 hours of onset of symptoms.48,49,62 Today, however, MRI has largely replaced bone scans because of its higher specificity and concomitant ability to evaluate surrounding soft tissues for other potential injuries.3,37,48 MRI may be considered at the initial evaluation if there is clinical suspicion for a stress fracture that necessitates a restrictive treatment protocol, such as a period of nonweightbearing or cast immobilization (eg, navicular stress fracture). Importantly, MRI findings must be correlated with clinical signs and symptoms because stress reactions (bone bruises or generalized marrow edema) that are distinctive from overt stress fractures are equally common in athletes. One study of 21 asymptomatic college distance runners demonstrated a 43% incidence of bone marrow edema on MRI that did not predispose these athletes to later stress fracture at the edematous sites.10,51
Low-Risk Stress Fractures
Low-risk stress fractures are those with a high propensity to heal regardless of treatment strategy. Management typically entails a short period of activity modification with full weightbearing. Common locations of low-risk fractures include the posteromedial tibial shaft, fibula, calcaneus, cuneiforms, cuboid, and metatarsal neck or shafts (distinct from the metatarsal bases). Contributing intrinsic factors such as low bone density, especially in the setting of prior stress fractures or the female athletic triad, may necessitate more protective management.
Posteromedial Tibial Shaft
The posteromedial tibial shaft is the most common location for a stress fracture in athletes and can be seen in runners and military recruits.16,24,31,49,78 A combination of compressive load and tensile muscular forces of the gastrocnemius-soleus complex and deep plantar flexors is thought to contribute to this injury.27,43,48 Athletes often complain of posterior medial leg pain that worsens with activity and is generally tender to palpation along the posteromedial tibial shaft. MRI detects these fractures early and the Fredericson classification (with the Kijowski grade 4 subdivision) is helpful to grade the severity of these tibial stress injuries (see Table 1).27,35,45,68 Interestingly, histopathologic investigations underscore that the posteromedial tibial cortex is the initial site of injury in all these stress fractures—despite the fact that cortical changes are a late finding on MRI.2,13,48,58
Table 1.
Fredericson Classification of Posteromedial Tibial Shaft Stress Fractures With Kijowski Grade 4 Subdivision.
| Grade | Description |
|---|---|
| Grade 1 | Periosteal tibial edema with normal marrow signal |
| Grade 2 | Marrow edema evident on T2-weighted images |
| Grade 3 | More severe bone marrow edema on both T1- and T2-weighted images |
| Grade 4a | Features all grade 3 changes along with intracortical signal change |
| Grade 4b | Demonstrates a linear cortical fracture line |
Because the posteromedial tibia fracture has a high propensity for healing due to its location on the compression side of this bone, initial treatment consists of weightbearing in a brace or pneumatic boot until pain and tenderness have resolved.48,68,72 Conservative treatment lasts 4 to 8 weeks, followed by a gradual return to athletics. The Fredericson classification can be prognostic for athletes, with grade 1 injuries requiring an average of 16 days to return to sports; grades 2, 3, and 4a all requiring an average of 39 to 44 days; and grade 4b requiring an average of 71 days to return to sport.45,48,67
Fibula
Stress fractures of the fibula commonly occur along its distal third, immediately proximal to the incisura.48,69,81 This may represent a physiological weak point given the juxtaposition of strong ligamentous attachments at this site under conditions of repetitive axial load such as running (see Figure 1). Individuals with pes planus are susceptible due to the compressive force within the fibula caused by the hindfoot valgus malalignment.36,79 In addition to the standard differential diagnosis, athletes with these symptoms should be evaluated for peroneal tendon pathology or subfibular impingement, and exertional compartment syndrome. While most of these patients are generally allowed to weightbear, return to impact activity is usually restricted for at least 2 to 3 months.
Figure 1.

Female recreational runner and swimmer who originally presented with 1 month of left lateral ankle pain worse when weightbearing with lateral distal fibular stress fracture. She was treated with activity modification and a tall pneumatic boot. (A) Initial mortise x-ray of the left ankle demonstrates a transverse lucency at the distal fibula immediately above the incisura. (B) Left ankle mortise x-ray 1 month later demonstrates interval healing and callous formation.
Calcaneus
Stress fractures of the calcaneus are precipitated by a combination of repetitive heel strike and noncushioned surfaces, although the opposing pull of the Achilles tendon is also thought to contribute.28,40,48,49 Pain with weightbearing and a positive calcaneal squeeze (discomfort during tuberosity compression between the examiner’s thenar eminences) suggest the diagnosis. The differential diagnosis for heel pain in an adult includes insertional Achilles tendinosis, retrocalcaneal bursitis, plantar fasciitis, central heel pad syndrome, and Baxter’s nerve entrapment. Adolescents should also be evaluated for Sever disease and tarsal coalition. Fifty-six percent of calcaneal stress fractures occur within the posterior tuberosity, oriented perpendicular to the natural trabecular pattern from dorsoproximal to plantar-distal; they can also occur, however, in the middle (18%) or anterior (26%) portions of the calcaneus (see Figure 2).41,70 MRI can be helpful for diagnosis, especially in case of anterior and middle calcaneal stress fracture.5,48,70 Up to 65% of calcaneal stress injuries have been associated with an additional tarsal stress injury or fracture.70,71 Limited weightbearing with immobilization is the standard initial treatment, with advancement as pain allows.
Figure 2.

Young male recreational athlete who recently joined a running group with a quick increase in his running mileage presented with right heel pain that began abruptly on a 5-mile run 2 months prior to presentation with imaging demonstrating a posterior calcaneal stress fracture that was treated with activity modification and eventual gradual resumption to impact and running activities. Figure 2 shows a single-view lateral plain film of the right calcaneus with an area of boney sclerosis in the posterior tuberosity oriented perpendicular to the trabecula from dorsoproximal to plantar-distal. Therefore, at times these fractures require more proactive management, including restricted weightbearing, casting or immobilization, and even early operative intervention at initial presentation to optimize outcome.
Cuneiforms and Cuboid
Stress fractures of the cuneiforms and cuboid are uncommon. They result from the torsional and compressive forces between the planted forefoot and the relatively larger hindfoot. These often present as pain during push off in athletic activities. Given the proximity of the cuniforms and the cuboid to the metatarsals and other tarsal bones, the tenderness can be poorly localized. Other potential etiologies to be ruled out include sinus tarsi syndrome, proximal metatarsal stress fracture, and calcaneonavicular coalition. Due to a typical lack of periosteal callus formation on radiographs, MRI is often needed to confirm these midfoot stress injuries. 22 A 6-week period of activity modification generally leads to excellent clinical results. 48
Metatarsal Shaft
Running athletes, dancers, and military recruits are especially at risk for metatarsal stress fractures. Metatarsals are loaded perpendicular to their long axis, and the relatively fixed proximal anatomy of the second and third metatarsals makes them particularly prone to diaphyseal stress fracture. Due to its length and overall immobility, the distal second metatarsal shaft remains the most common location for fracture (Figure 3). Tenderness is usually localized to the shaft when metatarsal stress fractures occur and can be associated with dorsal swelling. Metatarsalgia, metatarsophalangeal synovitis, Freiberg’s infarction, and Morton’s neuroma should also be considered in the differential.22,28,37,48 Radiographs a few weeks after the onset of symptoms frequently demonstrate callus around a thin, transverse fracture line. MRI is generally unnecessary unless the diagnosis is in question, and symptom resolution guides a return to activity.
Figure 3.
A recreational female jogger and avid dancer presented with 5 weeks worsening forefoot pain that had not improved with change in shoewear or decreased running mileage. (A) Initial AP of the right foot demonstrates a transverse cortical lucency with surrounding callous formation at the distal 2nd metatarsal shaft. (B) Clinical photograph of plantar skin callous formation and (C) pressure mapping demonstrate increased 2nd and 3rd metatarsal head loading.
High-Risk Stress Fractures
High-risk stress fractures of the foot or ankle in athletes are those that carry a lower propensity to heal. Therefore at times these fractures require more proactive management, including restricted weightbearing, casting or immobilization, and even early operative intervention at initial presentation to optimize outcome. These particular injuries occur more commonly in areas of tensile stress and/or vascular watershed, predicating the potential for nonunion. A high index of suspicion facilitates early diagnosis. Common locations of high-risk fractures include the anterior tibial shaft; medial malleolus; talus; navicular; second, third, and fourth metatarsal bases; proximal fifth metatarsal metadiaphysis; and the hallux sesamoids.
Anterior Tibial Shaft
Stress fractures of the anterior tibial shaft are commonly seen in repetitive jumping athletes. Injury to this hypovascular, tension side of the tibia predisposes it to fracture propagation, delayed union, and nonunion. Symptoms include anterior shin pain with tenderness along the tibial crest. Lateral radiographs taken 4 to 8 weeks after symptom onset may demonstrate a thickened anterior cortex and characteristic V-shaped fracture of the anterior tibial cortex known as the “dreaded black line.”3,15,37,48 MRI facilitates early diagnosis prior to radiographic changes.
Treatment is controversial and patient specific. Some recommend a trial of conservative management, and others advocate for early operative intervention.10,51,63 In the absence of clear radiographic nonunion, initial nonoperative management can be successful but may lead to a prolonged return to play of 8 to 12 months. Among those with delayed union or nonunion, reamed intramedullary nailing or open compression plating with bone graft has been shown to shorten return to sport by 4 to 6 months.12,15,16,24,78
Medial Malleolus
Repetitive torsion and shear across the medial ankle can lead to medial malleolar stress injury, especially in the setting of a cavovarus foot. Symptoms are generally activity dependent, with localized pain and swelling over the anteromedial ankle; these can mimic impingement-type symptoms to confound diagnosis (see Figure 4).23,43,57 Deltoid ligament pathology should also be considered. MRI is often necessary to diagnose stress reaction or fracture at the medial malleolar level, characteristically arising from the tibial plafond and running vertically or obliquely to the medial tibial cortex, although computed tomography (CT) scan may better define the actual fracture pattern and degree of healing.16,24,43,47 –49,63,68,78
Figure 4.

Young male recreational athlete who presented with 1 month of medial left ankle pain. (A) Initial anteroposterior x-ray of left ankle demonstrate a subtle vertical lucency arising from shoulder of the plafond. (B) Initial lateral x-ray. After loss to follow-up and persistent weightbearing, he again presented 1 month later with worsening symptoms. (C) Left ankle mortise x-ray demonstrated interval worsening of the fracture line with slight displacement.
Preferred treatment of medial malleolus stress fractures remains controversial and patient specific. Without any radiographically discernable facture line, a period of restricted weightbearing until symptom resolution is reasonable. Once the fracture becomes visible, however, even if nondisplaced, operative fixation is often recommended.35,45,67,68 Given the obliquity of this fracture orientation and its propensity for shear during routine load, buttress plating is biomechanically preferable to screw fixation.
Talus
The high joint reactive forces seen in the ankle are transmitted through the talus, which can lead to talar stress injury, especially of the head.48,69 Often seen in jumping athletes, talar stress fractures often present with vague symptoms that can be confused with ankle impingement. Plain radiographs are usually normal, but MRI is diagnostic.48,68,69,72 While highly sensitive, the specificity of MRI may be reduced in certain athletic populations such as gymnasts or professional ballet dancers, where upward of 75% of asymptomatic participants may demonstrate signal within the talus.34,67,72 A period of nonweightbearing should be considered until symptoms resolve, but degenerative change, osteochondral defect, or osteonecrosis may alter the prognosis. The use of a medially posted orthotic in athletes with hindfoot valgus may also be helpful.19,45,48,67 When the talar head is involved, operative intervention is often driven by the injury’s implications for the talonavicular joint. 69
Navicular
Navicular stress fractures, common among track-and-field participants, are likely potentiated by the compressive forces generated by the medial column of the foot; concomitant tensile forces generated by the spring ligament and posterior tibial tendon insertions, however, may also play a role. 9 Such fractures characteristically occur in the sagittal plane within the central third of the navicular, described as a watershed area between branches of the posterior tibial and dorsalis pedis arteries (see Figure 5). 50 Approximately 80% of patients complain of dorsal discomfort corroborated by tenderness along the proximal pole of the navicular (the so-called N spot), although symptoms can be vague. Radiographs may miss over two-thirds of incomplete fractures and up to one-fifth of complete fractures. 44 Even in the absence of clear x-ray findings, a high clinical suspicion should prompt additional imaging to delineate both fracture presence (MRI) and trajectory (CT). Incomplete fractures will typically begin along the dorsal cortex and thereafter propagate over time in the sagittal plane toward the distal plantar aspect. 28 Saxena et al 65 divided such fractures into 3 groups (see Table 2).
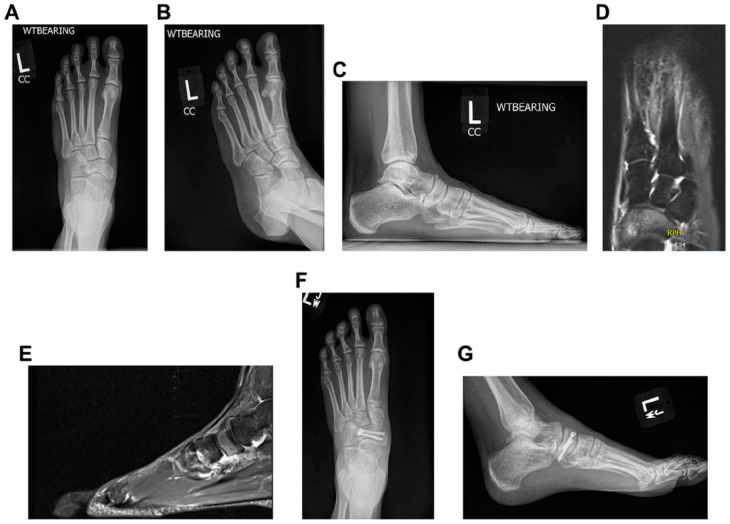
Figure 5.
Young female cross-country runner who presented with 1 month of left foot pain associated with running and weightbearing activity. Initial radiographs and magnetic resonance imaging demonstrate a fracture of the dorsal navicular with extension to the midbody, alongside a dorsal avulsion fragment. Initial left foot x-rays. (A) Anteroposterior (AP) view. (B) Oblique view. (C) Lateral view. (D) Left foot magnetic resonance imaging, axial slice at dorsal navicular. (E) Sagittal image at midbody of navicular. (F) She underwent surgical fixation of the fracture in situ with 2 cannulated headless screws and excision of the avulsion fragment. Postoperative x-rays 2 months after the procedure: AP view. (G) Lateral view.
Table 2.
Saxena Classification of Navicular Stress Fractures.
| Type | Description |
|---|---|
| Type I | A dorsal cortical break |
| Type II | A fracture propagation into the navicular body |
| Type III | A complete fracture with potential avascular, cystic, and sclerotic changes |
Acute nondisplaced partial or complete fractures can often be managed effectively with cast or pneumatic boot immobilization, activity modification, and weight offloading for approximately 6 weeks.19,28,34,48,69,75,76,81 Gradual resumption of weightbearing and other activities may be considered as symptoms resolve, but persistent symptoms or radiographic suggestion of delayed union at 3 months warrant repeat CT scanning and consideration of operative stabilization. Early operative fixation is recommended for displaced fractures or complete fractures with sclerotic change, using 2 to 3 crossed lag screws or a small dorsal buttress plate if gaps are evident. 20 One must avoid devascularizing the major bone fragments via excessive exposure, and bone grafting should be considered in any fracture that exhibits displacement or sclerosis. 33 Some authors advocate for operative fixation of even initially nondisplaced or incomplete fractures based on expedited return to sport (16.4 weeks) compared to nonoperative management (21.7 weeks) following systematic review. 46 Others theorize that fixation may act as “rebar” posthealing to minimize any chance of recurrent stress for athletes planning to resume high-impact sports. 32
Base of the Second, Third, and Fourth Metatarsals
Occurring most commonly at the base of the second metatarsal, proximal metatarsal fractures generally affect the central rays and are characterized by localized swelling and tenderness. Dancers who frequent the “en pointe” position, repetitive-impact athletes, and those with cavus feet appear predisposed (Figure 6). 53 Activity modification with short-term pneumatic boot immobilization frequently suffices to enable uneventful healing, but nonunion does occasionally occur and may require operative fixation. Both symptomatic and radiographic union should therefore precede any return to sport. 53
Figure 6.

A young male and recreational runner with a subtle cavus foot who presented with 6 weeks worsening lateral foot pain and inability to run his usual distances. (A) Initial AP of the left foot demonstrates a transverse cortical lucency at the base of the 4th metatarsal with local cortical thickening. (B) Left foot oblique x-ray re-demonstrates stress fracture and cortical thickening at the lateral aspect of the 4th metatarsal base.
Proximal Fifth Metadiaphysis Metatarsal
Fifth metatarsal stress fractures are potentiated by a cavus alignment, metatarsus adductus, and participation in cutting sports. Proposed bioetiologies include a vascular watershed area between the peroneus brevis insertion and the diaphyseal blood supply (see Figure 7). Torg et al 74 classified these fractures by acuity and radiograph characteristics (see Table 3). Pain and swelling are usually localizable, while radiographs are generally diagnostic. Acute type I fractures may be treated with a 6-week period of casting and offloading, but some have argued for immediate intramedullary screw fixation to facilitate earlier return to sports and decreased refracture rates, although definitive evidence for these opinions remains lacking.28,60 Predisposing cavus or adductus malalignment may influence any decision for early surgery and generates its own controversy in both athletes and nonathletes as to any role for concurrent realignment surgery. Type II and III fractures require operative repair, although canal obliteration may necessitate open plate fixation with bone grafting. Cavus realignment should be heavily considered in such settings, although recovery from its treatment remains difficult to justify in any elite athlete.
Figure 7.
Young male lacrosse player who presented with worsening left lateral foot pain after 3 years of prodromal symptoms. Radiographs demonstrate a proximal fifth metatarsal stress fracture in the setting of metatarsus adductus. (A) Anteroposterior (AP) view. (B) Oblique view. (C) Lateral view. (D) He underwent screw fixation and went on to successful union and pain-free return to sport. Postoperative radiographs 6 months after the procedure: AP view. (E) Oblique view. (F) Lateral view.
Table 3.
Torg Classification of Proximal Fifth Metatarsal Stress Fractures.
| Type | Description |
|---|---|
| Type I | Acute |
| Type II | Delayed union with periosteal and intramedullary bone formation |
| Type III | Nonunion |
Hallux Sesamoid
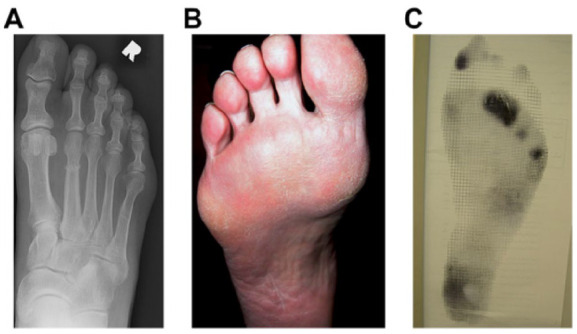
Repetitive compressive overload under the first metatarsal head as well as tension forces across the hallux sesamoids through the flexor hallucis brevis can lead to injury of especially the medial sesamoid. Predisposing factors include a plantarflexed first ray or history of repetitive forced dorsiflexion, as seen among football linemen or baseball catchers (Figure 8). Differential diagnosis includes turf toe caused by a singular dorsiflexion injury, sesamoiditis, gout, sesamoidal osteonecrosis, acute fracture, and first MTP arthritis. Bilateral foot radiographs may confirm bipartite sesamoids, which are bilateral in approximately 80% of individuals and involve the tibial sesamoid in 90% of patients. 27 In unclear cases, an MRI scan can demonstrate signal abnormality in the involved sesamoid, and a CT scan may be useful to delineate bony anatomy.
Figure 8.

A middle-age male and recreational runner with a forefoot driven cavus foot and resultant “tripod” overload who presented with 8 weeks worsening pain under his 1st metatarsophalangeal joint with running and weight-bearing. (A) Initial sesamoid view of the left foot demonstrates a transverse cortical lucency through the tibial sesamoid. (B) Left foot lateral x-ray demonstrates the relative plantarflexed positioning of the first ray, often seen in a forefoot driven cavus.
Treatment for sesamoidal stress fractures can be prolonged. Initial treatment may entail offloading with immobilization, followed by a gradual return to sports in a rocker bottom shoe and an orthotic that incorporates a sesamoid recess and Morton’s extension. 27 In recalcitrant cases, many different operative procedures have been described, including open bone grafting, internal fixation, and sesamoid excision. In the presence of a preexisting gastrocnemius contracture or a forefoot-driven cavus, one may alternatively consider the performance of a gastrocnemius recession and/or first ray dorsiflexion osteotomy, respectively.6,29
Other Treatments and Considerations
Prevention
Stress fracture prevention focuses on modifying extrinsic risk factors. All athletes should be counseled on appropriate diet, training regimen, proper technique, and conditioning ramp-up. Equipment updates such as appropriate orthotics, if necessary, and new running shoes every 200 to 300 miles should be highlighted. 66 Involvement of multidisciplinary teams that incorporate endocrinologists for bone disorders or metabolic deficiencies and psychiatrists for eating disorders is also critical to success. With the patient’s permission, involving coaches and trainers in this discussion can be both educational and helpful for the patient’s success.
Female Athletes
Female predisposition to stress fractures can be biomechanical in origin, such as the presence of a higher Q-angle in the knee, but hormonal differences may also play a role.14,21,42,80 The female athlete triad deserves special mention, defined by the coexistence of an eating disorder, amenorrhea, and osteoporosis. Treatment of stress fractures in such scenarios requires additional focus on adequate caloric intake with a goal body mass index (BMI) more than 21 kg/m2, adequate calcium and vitamin D intake, and alterations in training. 59 Birth control pills may decrease the incidence of stress fractures by ensuring menstrual regularity. 56 Proactive referral to other specialists as above is crucial and should be particularly considered if a female athlete presents with more than 1 stress fracture over time.
Pediatrics
Year-round sport-specific programs with heightened athlete expectations and training intensity underlie the rising incidence of stress injuries across the pediatric population. 38 In skeletally immature athletes, prolonged stress may lead to growth deformities or physeal arrest, which warrants separate consideration compared to adults.38,55 Expedited referral to a pediatric orthopaedic surgeon is critical with even the slightest evidence of physeal arrest or bone deformity.
Laboratory Values
Vitamin D affects bone health via its regulation of serum calcium and phosphorous concentrations, and low vitamin D levels may be associated with an increased risk of stress fracture among military recruits. 30 Parathyroid hormone (PTH), via osteoclast stimulation, may also be higher among athletes who sustain stress fractures. 77 Measurement of vitamin D and PTH levels should therefore be considered in any athlete who sustains a high-risk or recurrent stress fracture with subsequent repletion of vitamin D as necessary. 39
Management and Workup of an Athlete With Repetitive Stress Fractures
In addition to the measurement of vitamin D and PTH levels, one should consider dual-energy x-ray absorptiometry (DEXA) scan to assess bone mineral density (BMD) after recurrent stress fractures. 25 Referral to a bone mineral specialist should be considered with any abnormality.
Medications
Adequate levels of calcium and vitamin D protect against the development of stress fractures, and deficiencies of vitamin D benefit from repletion accordingly. 54 The evolving understanding of bone metabolism and calcium homeostasis has introduced multiple other therapeutic options, including bisphosphonates, calcitonin, oral contraceptives, and PTH analogues. A prospective randomized clinical trial of competitive female runners demonstrated that daily use of an oral contraceptive pill may increase BMD by 1% a year but was unable to demonstrate a resultant reduction in stress fractures. 26 Others have trialed the use of preventative bisphosphonates among military recruits but did not demonstrate a reduced risk of stress fracture. 52 Calcitonin, which counters PTH’s peripheral effects, has not been demonstrated to be effective in any large clinical trial. Recently, a recombinant form of PTH called teriparatide (Forteo) has shown some promise in the treatment of osteoporosis, but its use in stress fractures in the athlete is controversial and deemed off-label.4,61
Other Nonoperative Treatments
Other commonly used modalities include orthotics, bone stimulators, pulsed ultrasound, and extracorporeal shock wave therapy (ESWT). A cadaveric study that suggested orthotics decrease metatarsal forces failed to gain in vivo support when applied to Israeli military recruits who demonstrated no difference in the rate of stress fractures.48,49,51 Electromagnetic bone stimulators, pulsed ultrasound bone stimulators, and ESWT are purported to aid healing and increase rates of bony union.8,18,64,73 The literature supporting such modalities, however, is fraught with small-scale studies, methodological flaws, and conflicts of interest. Therefore, these modalities are generally considered adjuvants to established treatment methods. Furthermore, emerging use of platelet-rich plasma and other autologous cell-based injections has not demonstrated efficacious treatment of foot and ankle stress fractures thus far.
Summary
Foot and ankle stress fractures are common among both recreational and elite athletes, and they can be associated with significant morbidity and loss of play. Caretakers must accordingly maintain a high index of suspicion for this population. Intrinsic factors pose treatment challenges in athletes with stress fractures, so focus on potentially modifiable extrinsic factors may improve outcome and be better tolerated by the athlete. Physical exam remains the cornerstone of diagnosis, and providers must maintain a thorough knowledge of foot and ankle anatomy to localize these injuries in a timely fashion—especially considering that early radiographs can often be negative and MRI can often be nonspecific. Distinguishing between low- and high-risk stress fractures helps guide treatment and educate patients regarding prognosis. Moreover, identifying and addressing predisposing factors such as malalignment, coalition, or metabolic abnormalities is also critical to this conversation. For certain subsets of patients, a multidisciplinary team that incorporates endocrinologists, mental health professionals, and the orthopaedist remains paramount for optimizing treatment outcome.
Footnotes
This article was originally published as: Kaiser PB, Guss D, DiGiovanni CW. Stress fractures of the foot and ankle in athletes. Foot Ankle Orthop. 2018 Aug 24;3(3):2473011418790078. doi:10.1177/2473011418790078.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Philip B. Kaiser, MD, https://orcid.org/0000-0002-7379-3721
https://orcid.org/0000-0002-7379-3721
References
- 1. Albisetti W, Perugia D, De Bartolomeo O, Tagliabue L, Camerucci E, Calori GM. Stress fractures of the base of the metatarsal bones in young trainee ballet dancers. Int Orthop. 2010;34(1):51-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson RB, McBryde AM. Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18(5):293-296. [DOI] [PubMed] [Google Scholar]
- 3. Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16(2):291-306. [DOI] [PubMed] [Google Scholar]
- 4. Babu S, Sandiford NA, Vrahas M. Use of Teriparatide to improve fracture healing: what is the evidence? World J Orthop. 2015;6(6):457-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barrack MT, Gibbs JC, De Souza MJ, et al. Higher incidence of bone stress injuries with increasing female athlete triad-related risk factors: a prospective multisite study of exercising girls and women. Am J Sports Med. 2014;42(4):949-958. [DOI] [PubMed] [Google Scholar]
- 6. Barske HL, DiGiovanni BF, Douglass M, Nawoczenski DA. Current concepts review: isolated gastrocnemius contracture and gastrocnemius recession. Foot Ankle Int. 2012;33(10):915-921. [DOI] [PubMed] [Google Scholar]
- 7. Beck BR. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26(4):265-279. [DOI] [PubMed] [Google Scholar]
- 8. Beck BR, Matheson GO, Bergman G. Do capacitively coupled electric fields accelerate tibial stress fracture healing? A randomized controlled trial. Am J Sports Med. 2008;36(3):545-553. [DOI] [PubMed] [Google Scholar]
- 9. Bennell KL, Malcolm SA, Thomas SA. The incidence and distribution of stress fractures in competitive track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24(2):211-217. [DOI] [PubMed] [Google Scholar]
- 10. Bergman AG, Fredericson M, Ho C, Matheson GO. Asymptomatic tibial stress reactions: MRI detection and clinical follow-up in distance runners. AJR Am J Roentgenol. 2004;183(3):635-638. [DOI] [PubMed] [Google Scholar]
- 11. Bernstein A, Stone JR. March fracture: a report of three hundred and seven cases and a new method of treatment. J Bone Joint Surg Am. 1944;26(4):743-750. [Google Scholar]
- 12. Bianchi S, Luong DH. Stress fractures of the calcaneus diagnosed by sonography: report of 8 cases. J Ultrasound Med. 2017;159(suppl 2):245. [DOI] [PubMed] [Google Scholar]
- 13. Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003;24(2):137-141. [DOI] [PubMed] [Google Scholar]
- 14. Bijur PE, Horodyski M, Egerton W, Kurzon M, Lifrak S, Friedman S. Comparison of injury during cadet basic training by gender. Arch Pediatr Adolesc Med. 1997;151(5):456-461. [DOI] [PubMed] [Google Scholar]
- 15. Boden BP, Osbahr DC. High–risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8(6):344-353. [DOI] [PubMed] [Google Scholar]
- 16. Borens O, Sen MK, Huang RC, et al. Anterior tension band plating for anterior tibial stress fractures in high-performance female athletes: a report of 4 cases. J Orthop Trauma. 2006;20(6):425-430. [DOI] [PubMed] [Google Scholar]
- 17. Breithaupt MD. Fur pathologie des menschlichen fusses [Pathology of the human foot]. Med Zeitung. 1855;24:169-171. [Google Scholar]
- 18. Brighton CT, Wang W, Seldes R, Zhang G, Pollack SR. Signal transduction in electrically stimulated bone cells. J Bone Joint Surg Am. 2001;83(10):1514-1523. [DOI] [PubMed] [Google Scholar]
- 19. Brockwell J, Yeung Y, Griffith JF. Stress fractures of the foot and ankle. Sports Med Arthrosc. 2009;17(3):149-159. [DOI] [PubMed] [Google Scholar]
- 20. Browner BD, Jupiter JB, Krettek C, Anderson PA. Foot injuries. In: Richter M, Kwon JY, DiGiovanni CW, eds. Skeletal Trauma E-Book. Philadelphia, PA: Saunders; 2014:2251-2387. [Google Scholar]
- 21. Brudvig TJ, Gudger TD, Obermeyer L. Stress fractures in 295 trainees: a one-year study of incidence as related to age, sex, and race. Mil Med. 1983;148(8):666-667. [PubMed] [Google Scholar]
- 22. Bui-Mansfield LT, Thomas WR. Magnetic resonance imaging of stress injury of the cuneiform bones in patients with plantar fasciitis. J Comput Assist Tomogr. 2009;33(4):593-596. [DOI] [PubMed] [Google Scholar]
- 23. Caesar BC, McCollum GA, Elliot R, Williams A, Calder JDF. Stress fractures of the tibia and medial malleolus. Foot Ankle Clin. 2013;18(2):339-355. [DOI] [PubMed] [Google Scholar]
- 24. Chang PS, Harris RM. Intramedullary nailing for chronic tibial stress fractures: a review of five cases. Am J Sports Med. 1996;24(5):688-692. [DOI] [PubMed] [Google Scholar]
- 25. Chen Y-T, Tenforde AS, Fredericson M. Update on stress fractures in female athletes: epidemiology, treatment, and prevention. Curr Rev Musculoskelet Med. 2013;6(2):173-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cobb KL, Bachrach LK, Sowers M, et al. The effect of oral contraceptives on bone mass and stress fractures in female runners. Med Sci Sports Exerc. 2007;39(9):1464-1473. [DOI] [PubMed] [Google Scholar]
- 27. Cohen BE. Hallux sesamoid disorders. Foot Ankle Clin. 2009;14(1):91-104. [DOI] [PubMed] [Google Scholar]
- 28. Coughlin MJ, Saltzman CL, Mann RA. Mann’s Surgery of the Foot and Ankle E-Book: Expert Consult-Online. Philadelphia, PA: Saunders/Elsevier; 2013. [Google Scholar]
- 29. Cychosz CC, Phisitkul P, Belatti DA, Glazebrook MA, DiGiovanni CW. Gastrocnemius recession for foot and ankle conditions in adults: evidence-based recommendations. Foot Ankle Surg. 2015;21(2):77-85. [DOI] [PubMed] [Google Scholar]
- 30. Davey T, Lanham-New SA, Shaw AM, et al. Low serum 25-hydroxyvitamin D is associated with increased risk of stress fracture during Royal Marine recruit training. Osteoporos Int. 2015;27(1):171-179. [DOI] [PubMed] [Google Scholar]
- 31. DeLee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 1983;11(5):349-353. [DOI] [PubMed] [Google Scholar]
- 32. DiGiovanni CW. Fractures of the navicular. Foot Ankle Clin. 2004;9(1):25-63. [DOI] [PubMed] [Google Scholar]
- 33. DiGiovanni CW, Lin SS, Daniels TR, et al. The importance of sufficient graft material in achieving foot or ankle fusion. J Bone Joint Surg Am. 2016;98(15):1260-1267. [DOI] [PubMed] [Google Scholar]
- 34. Elias I, Zoga AC, Raikin SM, et al. Bone stress injury of the ankle in professional ballet dancers seen on MRI. BMC Musculoskelet Disord. 2008;9:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472-481. [DOI] [PubMed] [Google Scholar]
- 36. Friedman MA, Draganich LF, Toolan B, Brage ME. The effects of adult acquired flatfoot deformity on tibiotalar joint contact characteristics. Foot Ankle Int. 2001;22(3):241-246. [DOI] [PubMed] [Google Scholar]
- 37. Gross TS, Bunch RP. A mechanical model of metatarsal stress fracture during distance running. Am J Sports Med. 1989;17(5):669-674. [DOI] [PubMed] [Google Scholar]
- 38. Heyworth BE, Green DW. Lower extremity stress fractures in pediatric and adolescent athletes. Curr Opin Pediatr. 2008;20(1):58-61. [DOI] [PubMed] [Google Scholar]
- 39. Holick MF. Vitamin D and bone health. J Nutr. 1996;126(4)(suppl):1159S-1164S. [DOI] [PubMed] [Google Scholar]
- 40. Hulkko A, Orava S. Stress fractures in athletes. Int J Sports Med. 1987;8(3):221-226. [DOI] [PubMed] [Google Scholar]
- 41. Hunt KJ, Hurwit D, Robell K, Gatewood C, Botser IB, Matheson G. Incidence and epidemiology of foot and ankle injuries in elite collegiate athletes. Am J Sports Med. 2016;45(2):426-433. [DOI] [PubMed] [Google Scholar]
- 42. Jones BH, Harris JM, Vinh TN, Rubin C. Exercise-induced stress fractures and stress reactions of bone: epidemiology, etiology, and classification. Exerc Sport Sci Rev. 1989;17:379-422. [PubMed] [Google Scholar]
- 43. Jowett AJL, Birks CL, Blackney MC. Medial malleolar stress fracture secondary to chronic ankle impingement. Foot Ankle Int. 2008;29(7):716-721. [DOI] [PubMed] [Google Scholar]
- 44. Khan KM, Fuller PJ, Brukner PD, Kearney C, Burry HC. Outcome of conservative and surgical management of navicular stress fracture in athletes: eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20(6):657-666. [DOI] [PubMed] [Google Scholar]
- 45. Kijowski R, Choi J, Shinki K, Del Rio AM, De Smet A. Validation of MRI classification system for tibial stress injuries. AJR Am J Roentgenol. 2012;198(4):878-884. [DOI] [PubMed] [Google Scholar]
- 46. Mallee WH, Weel H, van Dijk CN, van Tulder MW, Kerkhoffs GM, Lin C-WC. Surgical versus conservative treatment for high-risk stress fractures of the lower leg (anterior tibial cortex, navicular and fifth metatarsal base): a systematic review. Br J Sports Med. 2015;49(6):370-376. [DOI] [PubMed] [Google Scholar]
- 47. Mandell JC, Khurana B, Smith SE. Stress fractures of the foot and ankle, part 1: biomechanics of bone and principles of imaging and treatment. Skeletal Radiol. 2017;46(8):1021-1029. [DOI] [PubMed] [Google Scholar]
- 48. Mandell JC, Khurana B, Smith SE. Stress fractures of the foot and ankle, part 2: site-specific etiology, imaging, and treatment, and differential diagnosis. Skeletal Radiol. 2017;46(9):1165-1186. [DOI] [PubMed] [Google Scholar]
- 49. Matheson GO, Clement DB. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15(1):46-58. [DOI] [PubMed] [Google Scholar]
- 50. McKeon KE, McCormick JJ, Johnson JE, Klein SE. Intraosseous and extraosseous arterial anatomy of the adult navicular. Foot Ankle Int. 2012;33(10):857-861. [DOI] [PubMed] [Google Scholar]
- 51. Meardon SA, Edwards WB, Ward E, Derrick TR. Effects of custom and semi-custom foot orthotics on second metatarsal bone strain during dynamic gait simulation. Foot Ankle Int. 2009;30(10):998-1004. [DOI] [PubMed] [Google Scholar]
- 52. Milgrom C, Finestone A, Novack V, et al. The effect of prophylactic treatment with risedronate on stress fracture incidence among infantry recruits. Bone. 2004;35(2):418-424. [DOI] [PubMed] [Google Scholar]
- 53. Muscolo L, Migues A, Slullitel G, Costa-Paz M. Stress fracture nonunion at the base of the second metatarsal in a ballet dancer: a case report. Am J Sports Med. 2004;32(6):1535-1537. [DOI] [PubMed] [Google Scholar]
- 54. Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113(10):754-759. [DOI] [PubMed] [Google Scholar]
- 55. Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nattiv A, Armsey TD. Stress injury to bone in the female athlete. Clin Sports Med. 1997;16(2):197-224. [DOI] [PubMed] [Google Scholar]
- 57. Papalada A, Malliaropoulos N, Tsitas K, et al. Ultrasound as a primary evaluation tool of bone stress injuries in elite track and field athletes. Am J Sports Med. 2012;40(4):915-919. [DOI] [PubMed] [Google Scholar]
- 58. Pathria MN, Chung CB, Resnick DL. Acute and stress-related injuries of bone and cartilage: pertinent anatomy, basic biomechanics, and imaging perspective. Radiology. 2016;280(1):21-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pester S, Smith PC. Stress fractures in the lower extremities of soldiers in basic training. Orthop Rev. 1992;21(3):297-303. [PubMed] [Google Scholar]
- 60. Quill GE, Jr. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26(2):353-361. [PubMed] [Google Scholar]
- 61. Raghavan P, Christofides E. Role of teriparatide in accelerating metatarsal stress fracture healing: a case series and review of literature. Clin Med Insights Endocrinol Diabetes. 2012;5:39-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Reese K, Litsky A, Kaeding C, Pedroza A, Shah N. Cannulated screw fixation of Jones fractures: a clinical and biomechanical study. Am J Sports Med. 2004;32(7):1736-1742. [DOI] [PubMed] [Google Scholar]
- 63. Rettig AC, Shelbourne KD, McCarroll JR, Bisesi M, Watts J. The natural history and treatment of delayed union stress fractures of the anterior cortex of the tibia. Am J Sports Med. 1988;16(3):250-255. [DOI] [PubMed] [Google Scholar]
- 64. Rue J-PH, Armstrong DW, Frassica FJ, Deafenbaugh M, Wilckens JH. The effect of pulsed ultrasound in the treatment of tibial stress fractures. Orthopedics. 2004;27(11):1192-1195. [DOI] [PubMed] [Google Scholar]
- 65. Saxena A, Fullem B, Hannaford D. Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J Foot Ankle Surg. 2000;39(2):96-103. [DOI] [PubMed] [Google Scholar]
- 66. Schwellnus MP, Jordaan G, Noakes TD. Prevention of common overuse injuries by the use of shock absorbing insoles: a prospective study. Am J Sports Med. 1990;18(6):636-641. [DOI] [PubMed] [Google Scholar]
- 67. Shabat S, Sampson KB, Mann G, et al. Stress fractures of the medial malleolus—review of the literature and report of a 15-year-old elite gymnast. Foot Ankle Int. 2002;23(7):647-650. [DOI] [PubMed] [Google Scholar]
- 68. Shelbourne KD, Fisher DA, Rettig AC. Stress fractures of the medial malleolus. Am J Sports Med. 1988;16(1):60-63. [DOI] [PubMed] [Google Scholar]
- 69. Sormaala MJ, Niva MH, Kiuru MJ. Outcomes of stress fractures of the talus. Am J Sports Med. 2006;34(11):1809-1814. [DOI] [PubMed] [Google Scholar]
- 70. Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM. Stress injuries of the calcaneus detected with magnetic resonance imaging in military recruits. J Bone Joint Surg Am. 2006;88(10):2237-2242. [DOI] [PubMed] [Google Scholar]
- 71. Spitz DJ, Newberg AH. Imaging of stress fractures in the athlete. Radiol Clin North Am. 2002;40(2):313-331. [DOI] [PubMed] [Google Scholar]
- 72. Swenson EJ, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J Sports Med. 1997;25(3):322-328. [DOI] [PubMed] [Google Scholar]
- 73. Taki M, Iwata O, Shiono M, Kimura M, Takagishi K. Extracorporeal shock wave therapy for resistant stress fracture in athletes: a report of 5 cases. Am J Sports Med. 2007;35(7):1188-1192. [DOI] [PubMed] [Google Scholar]
- 74. Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC. Fractures of the base of the fifth metatarsal distal to the tuberosity: classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984;66(2):209-214. [PubMed] [Google Scholar]
- 75. Torg JS, Moyer J, Gaughan JP. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38(5):1048-1053. [DOI] [PubMed] [Google Scholar]
- 76. Torg JS, Pavlov H, Cooley LH, et al. Stress fractures of the tarsal navicular: a retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982;64(5):700-712. [PubMed] [Google Scholar]
- 77. Välimäki V-V, Alfthan H, Lehmuskallio E, et al. Risk factors for clinical stress fractures in male military recruits: a prospective cohort study. Bone. 2005;37(2):267-273. [DOI] [PubMed] [Google Scholar]
- 78. Varner KE, Younas SA, Lintner DM, Marymont JV. Chronic anterior midtibial stress fractures in athletes treated with reamed intramedullary nailing. Am J Sports Med. 2005;33(7):1071-1076. [DOI] [PubMed] [Google Scholar]
- 79. Wang Q, Whittle M, Cunningham J, Kenwright J. Fibula and its ligaments in load transmission and ankle joint stability. Clin Orthop Relat Res. 1996;(330):261-270. [DOI] [PubMed] [Google Scholar]
- 80. Wentz L, Liu P-Y, Haymes E, Ilich JZ. Females have a greater incidence of stress fractures than males in both military and athletic populations: a systemic review. Mil Med. 2011;176(4):420-430. [DOI] [PubMed] [Google Scholar]
- 81. Woods M, Kijowski R, Sanford M, Choi J, De Smet A. Magnetic resonance imaging findings in patients with fibular stress injuries. Skeletal Radiol. 2008;37(9):835-841. [DOI] [PubMed] [Google Scholar]