Abstract
Background
The emergency for the COVID-19 pandemic has led to greater use of home telemonitoring devices. The aim of this study was to assess the usability of continuous home-monitoring care with an oxygen saturation device on post-COVID-19 patients.
Method
The system consists of a digital continuous pulse oximeter and a smartphone with an App, which were provided to patients. A survey composed of a standard Post-Study System Usability Questionnaire, and a satisfaction questionnaire was exploited to conduct a usability and feasibility analysis of the service.
Results
A total of 29 patients (17.2% female) with a mean age of 65 ± 11.5 years were enrolled: 20 patients were smartphone users (69%) with a mean age of 60.2 ± 9.5 years, and 9 patients (31%) did not own a smartphone (mean age 76.8 ± 5.9). The monitoring period was 1 month: a total of 444 recordings were conducted, 15 recordings per patient averagely. In total, 82% of the recordings performed did not require any intervention, while 18% led to the production of a report and subsequent intervention by a nurse who verified, together with the specialist, the need to intervene (i.e. the patient accessed the clinic for medical control and/or modification of oxygen therapy). A total of 17 patients compiled a usability questionnaire. The service was perceived as useful and well-structured, although it often required caregiver support.
Conclusions
Using continuous home-monitoring care with an oxygen saturation device seems feasible and useful for patients who could be followed at home avoiding going back to the hospital every time a trend oximetry is needed. Further improvements in connections, data flow processes, and simplifications, based on patients’ feedback, are needed to scale up the service.
Keywords: Telemonitoring, usability, digital oximeter, COVID-19, wearable sensors
Introduction
The widespread SARS-CoV-2 infections in Italy1,2 during 2020–2021 have caused a huge growth in subjects suffering of problems affecting the respiratory system. 3
The Lombardy Region, in northern Italy, experienced a wide number of severe cases of COVID-19, 4 which caused rapid depletion of beds available in the hospitals. The increasing number of patients who needed hospitalization, and the resulting lack of beds, was a worldwide problem 5 that forced the early hospital discharge of patients who had not fully recovered.
This emergency resulted in many patients being hospitalized for SARS-CoV2-related pneumonia and having respiratory problems that persisted even after the patient tested negative for COVID-19 and during the hospitalization. Some patients were discharged with the support of oxygen for severe dyspnea during light or moderate physical activity and also for problems during rest in some cases. These patients did not have any pre-existing chronic respiratory diseases or require oxygen therapy prior to COVID-19.
Continuous monitoring of certain clinical parameters, 6 such as heart rate and blood oxygen saturation, enables a more precise description of the evolution of respiratory functions and gas exchanges in various daily life conditions, including rest, physical activity, and sleep. Also, the continuous monitoring allows for timely intervention in case of any deterioration in the patient's condition 7 and facilitates the rapid detection of the need for oxygen reduction or weaning off. In this context, a continuous pulse oximeter can be more useful and predictive than an instantaneous one.8,9
In a Telehealth and Telecare Service for chronic 10 and COVID-19 patients 11 discharged from the hospital, we included continuous telemonitoring of blood oxygen saturation through a digital oximeter. In this context, telemonitoring is pivotal to maintaining a continuity of adequate care and enables the anticipation and prevention of the worsening of clinical conditions.
Usability analysis is crucial in detecting the aspects affecting the patient's satisfaction and reaching good results. In particular, detecting some usability aspects can help medical personnel to identify the action needed to improve patient's monitoring and experience.
Despite many methods to benchmark usability, Broekhuis et al. 12 declared that only “some most summative usability tests consider eHealth-specific factors that could potentially affect the experience of a system.” To avoid this issue, a specific questionnaire has been designed in the presented research work by combining standard and ad-hoc defined questions for a more complete and objective evaluation of patients’ experience with the home-monitoring saturation system.
The aim of this study was to assess the usability of continuous home-monitoring care with an oxygen saturation device on post-COVID-19 patients.
Method
Population
In a single-center (Continuity of Care Service, ICS MAUGERI, Lumezzane, Brescia, Italy) pilot study, patients were enrolled after their hospital discharge if they have experienced residual respiratory issues such as dyspnea during either mild exertion or rest, as well as episodes of desaturation resulting from previous SARS-CoV2-associated pneumonia. The expected duration for the follow-up of the oxygen saturation values was 1 month following discharge, allowing for the possibility of modulating its length and intensity including the frequency of monitoring sessions based on the patient's clinical condition.
The inclusion criterion was patients aged over 18 years discharged after hospitalization for COVID-19.
Patients were excluded if they were unable to comprehend and perform the necessary actions required for independent monitoring, either on their own or with the assistance of a caregiver. Additionally, patients were also excluded if they were discharged to locations other than their home (e.g. Residential Care Facilities or other hospitals). All interventions were carried out in accordance with the Declaration of Helsinki, and the study was approved by the Ethics committees of the ICS Maugeri on 30 June 2020 (CE2455).
Teleassistance service
The service was based on the model used by the Continuity of Care Service (Telemedicine Service) of the Maugeri Centre extensively described in previous research works.10,11 Briefly, a case manager nurse followed the patients for at least 1 month after discharge through a structured remote teleassistance program and telemonitoring of oxygen saturation.
The key element of the program was a structured nurse-managed telephone support and, when necessary, video consultations to see and speak with patients. During these phone calls, the nurse carried out a standardized interview inquiring about both the general clinical condition of the patient and drug therapy using assessment questions to detect if the patient's signs and symptoms were worsening or, on the contrary, improving. In the case of any symptom or problem, the patient could call the service during the operating hours of the service. The nurse relays the relevant information to the clinical specialist, who, based on the available information, can provide clinical feedback and, if necessary, modify the patient's drug or oxygen therapy.
Description of O2Ring device
Patients were provided with an oxygen saturation (SpO2) detection system, which included a digital trend oximeter (O2Ring™ Continuous Ring Oxygen Monitor, Wellue®). The oximeter has the form of an elastic ring with an inside circumference range of approximately 2.0–3.2 inches, intended to be worn preferably on the thumb or index finger. This placement ensured better sensor adhesion to the skin and minimized the risk of accidental movements. The O2Ring™ device could be used to monitor in continuous (up to 16 h) or for instant readings of the Sp02 and heart rate. The measurements were recorded every 4 s and stored in the internal memory of the O2Ring™ device. The recorded data were transmitted in real-time via Bluetooth to a designated smartphone provided to the patient along with the device. The data was then downloaded into an application called HTN (Health Telematic Network, Brescia, Italy), which allows easy access to the patient's electronic personal health record. The device measurement error was within 2% of the overall data recording, the calibration ranges of SpO2 was between 70% and 99%, and the heart rate was in the range 30–250 beats per minute.
If the patient consents, the app can be directly downloaded onto the personal smartphone. The app is available on both iOS (mobile app for iOS 9.0 or higher versions, iPhone 4s) and Android application stores (Android version 5.0 or above). Communication among devices via Bluetooth technology allows for an uninterrupted flow of data, which can be used for continuous monitoring of the patient's vital parameters.
The login procedure was done by a phone call to a Service Center to request the activation of the patient's personal credentials (i.e. email address, mobile number, and social security number), to guarantee their identity and privacy. After authentication, the patient was asked to accept the conditions for processing personal data directly within the App. The telemonitoring device records and sends the oximetry data continuously to a smartphone via Bluetooth connection. The measured vital signs are then stored in the “Pulse oximetry” section of the App and sent via a data connection to the web platform, directly uploaded into the patient's electronic medical record.
Finally, nurses can produce a graphic report that collects the parameters recorded by the digital oximeter. This report can be shared with specialists if required.
Figure 1 represents the workflow used for the continuous oxygen saturation device telemonitoring. At the time of delivery of the smartphone and digital oximeter, which is performed during the last few days before hospital discharge, a practical demonstration of their functions was carried out, and the method to get saturation data was illustrated.
Figure 1.
The figure illustrates the workflow of the continuous oxygen saturation telemonitoring device. The device records and sends oximetry data to a smartphone through a Bluetooth connection. The data is sent via a data connection to a web platform and uploaded to the patient's electronic medical record. The nurse can check the information, generate a graphical report, and share it with other healthcare professionals if needed.
More detailed and comprehensive training was provided to patients who did not use smartphones, ensuring their understanding of all the necessary procedures for recording oxygen saturation.
Patients were asked to perform monitoring tests during the last days before hospital discharge. For patients that showed difficulties, caregivers were involved in the training phase. Additionally, an illustrated user guide was provided to support patients, which includes contact details for the Continuity Care Service. The telemonitoring program, planned by the specialist and case manager nurse, involved at least one-night monitoring session and two sessions during physical activity per week. The program could be adjusted based on the patient's situation and specific needs.
For individuals undergoing respiratory support therapy such as Continuous Positive Airway Pressure (C-PAP) and oxygen therapy, saturation monitoring was conducted with adjusted dosages, as recommended by the specialist. This monitoring aimed to facilitate the weaning off process and the transition back to breathing in a regular environment.
Questionnaires
The defined survey was composed of two different parts: a standard Post-Study System Usability Questionnaire (PSSUQ) 13 and a satisfaction questionnaire (Supplementary material) specifically designed for the present study based on our previous experience. 14 The survey has been intended to be filled in at the end of the remote monitoring period. The combination of the two questionnaires allowed the personalization of the survey and the investigation of more detailed aspects.
The first part of the survey utilized the PSSUQ, which is a standard questionnaire widely used to assess the satisfaction perceived by the users in interacting with websites, software, and technological products after a period of testing or use. The most recent version consists of 16 questions that can be answered using a Likert scale ranging from 1 to 7 (with 1 indicating “Strongly Agree” and 7 indicating “Strongly Disagree”), in addition to the “NA” (“Not Applicable”) option when the user is not able to evaluate what is requested based on own experience. The structure of PSSUQ makes it particularly suitable for carrying out complete statistical analyzes, according to some rules tested and standardized through various studies.
PSSUQ is usually divided into three subcategories, useful for a deep investigation of the following aspects: utility of the system (average score of questions from 1 to 6), quality of information (average score of questions from 7 to 12), and quality of the interface (average score of questions from 13 to 15). Question 16 is used with the previous ones for the calculation of the general score.
The second part of the designed survey is composed of a satisfaction questionnaire, more specific to the O2Ring™ device instrumentation adopted during the trial: 13 questions have been defined to investigate the satisfaction generated using the device and its ease of use. Patients can answer the 13 questions by choosing one of the five smiley faces that better represent their mood while using the device. The representation is always combined with a written description of the possible answer, for a clearer interpretation.
To ensure methodological consistency, the survey was exclusively administered to patients who returned to the hospital for an outpatient pneumological visit upon completion of the telemonitoring program. Prior to completing the questionnaire, all patients participated in a brief educational session and independently filled it out. After completion, each answer has been added to an internal database that contains the information from all patients.
To be processed, the information from the questionnaires has been translated into a standardized numerical scale. While the answers of PSSUQs were already in numerical value from 1 to 7, the smiley faces of the satisfaction questionnaire have been converted into a scale 1 to 5, with increasing values corresponding to higher levels of user satisfaction. For each question, the average score has been calculated using the answers entered by all the study participants. Moreover, each average value has been converted into a percentage scale to ensure consistency and avoid the use of two different scales.
The answers from the questionnaires have been grouped in seven parameters in order to make the acquired data easier to read and understand. Figure 2 shows the approach used to determine objective parameters based on the items in the questionnaire.
Figure 2.
The figure shows the categories utilized to define and evaluate the seven parameters using the PSSUQ and satisfaction questionnaire. Panel a consists of 15 PSSUQ items that assess system usefulness, information quality, and interface quality, while item 16 allows to calculate the overall score. Panel b has 12 satisfaction questionnaire questions describing pulse oximeter use, accessibility, ease of use, and new functionalities. Question 13 refers to the duration of device usage.
PSSUQ has been subdivided into three parameters (Figure 2a) according to the standard classification previously described: system usefulness, information quality, and interface quality. Item 16 was solely utilized for calculating the overall score parameter, which represents the average of all survey items.
On the other hand, the parameters from the satisfaction questionnaire (Figure 2b) have been created by combining the items relating to the same aspect: use of pulse oximeter, accessibility, ease of use, and new functionalities. Question 13 has not been included in the parameters since it represents a frequency value and was not converted into a percentage scale. Instead, the medical staff directly utilized it for assessment purposes.
The score of each parameter was calculated through the average value of the responses included in each category. The graphical representation of the reached percentages facilitates a visual comparison of usability-related aspects, serving as a foundation for further discussion.
Results
Between February 2021 and March 2022, 29 patients were enrolled in the study (mean age, 65 ± 11.5 years), five patients (17.2%) were women. The patient's characteristics at baseline are described in Table 1. Out of the 29 enrolled patients, 20 (69%) were smartphone users with a mean age of 60 ± 10 years, while 9 (31%) did not use a personal smartphone (mean age 77 ± 6 years).
Table 1.
Overall patient demographics of the involved patients.
| Total number of patients N = 29 (%) | ||
|---|---|---|
| Demographic variables | ||
| Female | 5 (17.2) | |
| Mean age ± SD | 65.0 ± 12.0 | |
| Comorbidities | ||
| COPD | 1 (3.5) | |
| Diabetes | 5 (17.2) | |
| Lung cancer | 1 (3.5) | |
| 0xigen therapy | ||
| Oxygen therapy during rest, physical activity, and nocturnal periods | 2 (6.8) | |
| Oxygen therapy during physical activity and nocturnal periods | 2 (6.8) | |
| Nocturnal oxygen therapy | 1 (3.5) | |
| Oxygen therapy during physical activity | 2 (6.8) | |
| C-PAP | 2 (6.8) | |
| Dyspnea during physical activity | 3 (10.3) | |
| Desaturation during physical activity | 2 (6.8) | |
| Patients not on oxygen therapy | 15 (52.0) | |
| Ability to use smartphones | ||
| Smartphone users | 20 (69.0) | |
| Mean age ± SD of smartphone users | 60.0 ± 10.0 | |
| Non-smartphone users | 9 (31.0) | |
| Mean age ± SD of non-smartphone users | 77.0 ± 6.0 |
COPD: chronic obstructive pulmonary disease; C-PAP: continuous positive airway pressure; SD: standard deviation.
We supplied a dedicated smartphone to 25 of the enrolled patients, while four individuals (mean age 58 ± 8) opted to directly download the app onto their personal smartphones. They justified this decision by expressing discomfort in managing two smartphones, particularly during physical activity recordings.
It was necessary to involve caregivers during either the training phase or data recordings for nine patients (mean age 75 ± 8 years) in order to help in managing the monitoring system. Table 2 shows several variables of patient demographics according to the involvement of the caregiver. The level of education was similar between the two groups; however, the group that required caregiver support consisted of significantly older patients (p < 0.01). Within this group, 90% of the patients were retired and did not own a smartphone. On the other hand, the patients with no need of an early caregiver involvement mainly comprised employed individuals who were proficient in using smartphones.
Table 2.
Patient demographics according to the involvement of a caregiver.
| With
Caregiver N=20 (%) |
Without
Caregiver N=9 (%) |
P-value | ||
|---|---|---|---|---|
| Mean age ± SD | 61.0 ± 10.0 | 75.0 ± 8.0 | <0.01 | |
| Education | ||||
| Primary | 18 (90.0) | 8 (90.0) | ||
| Secondary | 2 (10.0) | 1 (10.0) | ||
| Employment Status | ||||
| Active working | 18 (90.0) | 1 (10.0) | ||
| Retired | 2 (10.0) | 8 (90.0) | ||
| Smartphone user | ||||
| Yes | 18 (90.0) | 2 (22.0) | ||
| No | 2 (10.0) | 7 (78.0) | ||
SD: standard deviation.
Recordings and reports
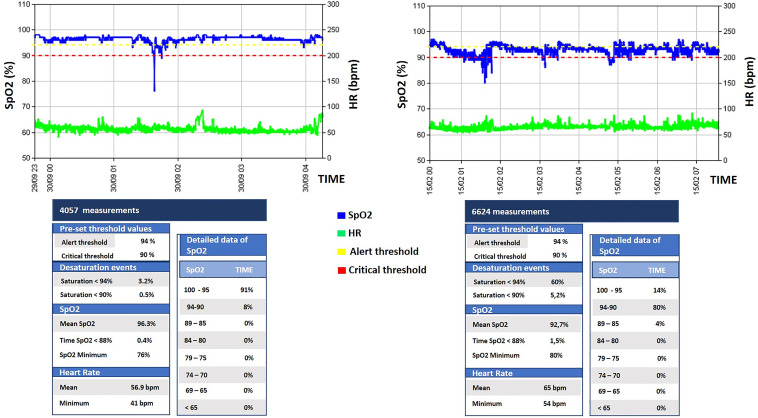
Out of 444 recordings, 271 (61%, averaging 9.3 ± 7.2 recordings per patient) were continuous SpO2 tracks obtained during both physical activity (148 recordings, 33%) and overnight monitoring (123 recordings, 28%). The remaining 173 (39%) were single instant measurements. Figure 3 shows two typical measured O2 profiles and reports produced in the patient's personal health record.
Figure 3.
The figure shows two typical measured O2 profiles and reports produced in the patient's personal health record.
Concerning continuous recordings, 46 (10.4%) were performed in oxygen therapy and 20 (4.5%) during C-PAP. Of the continuous recordings performed, 82% did not require any intervention, while 18% (80) led to the production of a report by the nurse and subsequent intervention of the specialist.
Out of the 80 reports generated, 45 (56.3%) indicated desaturations under 90% of blood oxygen.
Throughout the telemonitoring period, five patients (average age of 75.3 ± 7.6) were able to autonomously interrupt or reduce their oxygen therapy directly at home.
A total of 81 recordings (18.2%) were interrupted due to technical issues: the interruptions occurred either during overnight monitoring (62 recordings, 76.5%) or during physical activity (15 recordings, 18.5%). The absence or incomplete availability of certain measured data can be related to various issues that are described in Table 3.
Table 3.
Description of criticalities for lack of data.
| Percentage | |
|---|---|
| Difficulty faced by patients in interacting with a new system containing not familiar technological content. This leads to the inability to resolve unexpected situations (i.e. smartphone notifications, vibrations, and sounds), sometimes causing anxiety and distrust, up to the abandonment of the system. | 30% |
| Low receptivity of the internet connection at the patient's home. The lack of a stable connection made it impossible to send the detected data. | 10% |
| Disconnection or difficulty in reconnecting between the smartphone and the oximeter occurred when one of them was turned off, when the app was closed due to patient error or malfunction, when the devices were removed, or when reconnection failed. | 25% |
| High amount of data generated, resulting from the frequency of measurements taken every 4 s by the digital oximeter. It proved challenging to manage, especially in cases of difficulty accessing the Internet. | 10% |
| Insufficient battery level of the devices, which causes shutdown and the inability of detecting and sending the parameters: patients have been informed about the necessity of keeping the smartphone connected to the electricity network during night monitoring and of checking the charge level of the oximeter before measurements. | 5% |
| The need to keep the smartphone unlocked during monitoring, as the App was unable to receive and send data if in the background. | 20% |
During the remote monitoring period, patients requested technical assistance 16 times to address issues encountered during recordings: five requests were related to problems of the App, one to digital oximeter issues, seven to smartphone difficulties, and three to network problems.
The role of caregivers proved essential for these patients since the caregivers’ higher proficiency in using technology and ability to provide precise problem descriptions assisted the involved health personel in delivering targeted and effective interventions.
As a result of difficulties faced during monitoring or the anxiety experienced from using the system, two patients decided to give back the devices before the end of the telemonitoring process.
During the period of the research study, none of the enrolled patients reported events such as emergency room access, hospitalization, or death.
Questionnaire analysis
In the group of participants, 17 (59%) patients returned to the hospital for a previously scheduled outpatient pneumological visit and compiled a questionnaire. Table 4 represents the average values related to each question of the survey.
Table 4.
Average value obtained in each question of the survey.
| PSSUQ | Score (out of 7) | Satisfaction questionnaire | Score (out of 5) |
|---|---|---|---|
| n.1 | 1.29 | n.1 | 4.53 |
| n.2 | 1.76 | n.2 | 4.24 |
| n.3 | 1.65 | n.3 | 4.53 |
| n.4 | 1.53 | n.4 | 4.35 |
| n.5 | 1.47 | n.5 | - |
| n.6 | 1.59 | n.6 | 4.53 |
| n.7 | 1.87 | n.7 | 4.71 |
| n.8 | 1.73 | n.8 | 4.65 |
| n.9 | 1.35 | n.9 | 4.65 |
| n.10 | 1.29 | n.10 | 4.76 |
| n.11 | 1.29 | n.11 | 4.00 |
| n.12 | 1.53 | n.12 | 3.59 |
| n.13 | 1.71 | n.13 | - |
| n.14 | 1.59 | ||
| n.15 | 1.29 | ||
| n.16 | 1.54 |
The PSSUQ achieves an average score of 1.54 ± 0.19 (i.e. 92.28%). Although slightly different from other results, patients assigned the best score of 1.29 ± 0.59 (i.e. 95.86%) to ease of use, ease of retrieving information, organization of information provided by the system, and overall satisfaction during the use of the monitoring device (questions number 1, 10, 11, and 16, respectively). On the other hand, the lowest score of 1.87 ± 1.36 (i.e. 87.57%) was related to the support given by the system to solve human mistakes.
The satisfaction questionnaire achieves an overall score of 4.41 ± 0.35 (i.e. 88.25%). Once again, individual responses showed similar values, ranging from 3.59 (i.e. 71.80%) to 4.76 (i.e. 95.20%). The highest score has been attributed to the ease of correctly positioning the O2Ring™ device during the oxygen saturation acquisition. On the other hand, patients considered additional features such as comprehensive day-long monitoring and non-essential reminders less critical, resulting in the lowest score.
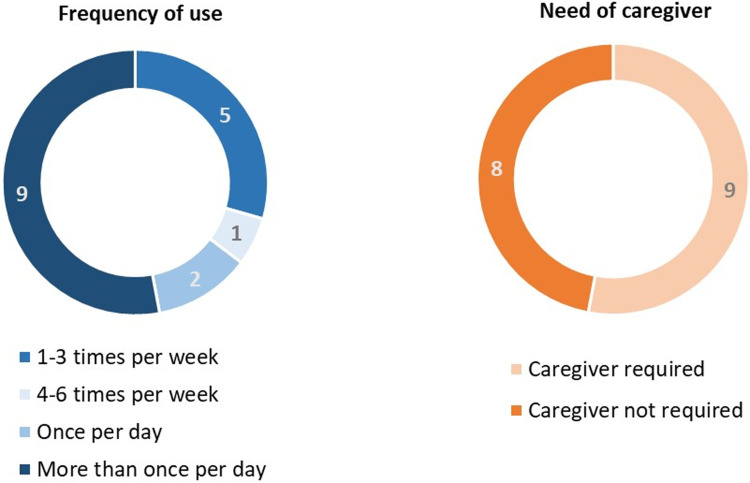
The answers to questions 5 and 13 have not been converted into a numerical scale; instead, their values have been used for other assessments. Question 13 indicates the frequency of patients’ telemonitoring system usage, while question 6 reveals how many participants needed assistance from a caregiver to perform tasks. As represented in Figure 4, many patients used the telemonitoring device more than once a day. Typically, they accessed the device during phone calls with the case manager to check their oxygen saturation values, during physical activity, or sleep. On the other hand, over 50% of patients have required assistance from a caregiver to perform tasks.
Figure 4.
The figure represents, on the left side, the duration of telemonitoring device usage reported by the patients and, on the right side, the number of patients who sought assistance from a caregiver.
Figure 5 represents the results achieved by parameters. Higher scores have been associated with the usefulness and ease of use of the O2Ring oximeter, the quality of information, and the interface of the device and the smartphone app. The low score obtained by accessibility (i.e. 43.94%) is closely related to the calculation method, representing the percentage of patients who did not require support from a family member or a caregiver to perform the required tasks. However, the overall score, calculated as the average of the seven parameters, reached a high value, exceeding 80%.
Figure 5.
The figure shows the percentage scores reached by parameters derived from the PSSUQ (a) and the satisfaction questionnaire (b) categories. The total score (c) indicates the average value of the seven parameters.
Discussion
This study provides preliminary evidence of the feasibility of implementing a home program using a continuous oxygen saturation telemonitoring system. The program proves to be useful for monitoring the blood saturation of patients with residual respiratory problems at home, both during nighttime and physical activity. Furthermore, managing support at home appears beneficial in avoiding frequent hospital visits for patients requiring oxygen therapy or C-PAP.
Close support from operators with prompt feedback when needed and virtual services using digital devices contribute to making patients safer and more active also in disease management. 15 Patients were able to perform 81.8% of the recordings without interruptions, providing the case manager and medical specialists with a clear picture of their oxygen saturation and respiratory functions.
Some authors, however, highlight the importance of effectively controlling technological issues, as poorly managed problems could lead to patient rejection of the monitoring device.16,17 In this study, considering the patient's perspective, we evidenced critical issues that may hinder the transmission of clinical data from the patient's home. The mentioned problems were related to the connections and the data flow among the digital oximeter, smartphone, App, and web platform. These limitations usually complicate the use of the system, limiting the forward of parameters.
Most of the interrupted recordings occurred during overnight monitoring (76.5%). This issue is derived from the longer duration of the sessions and the increased amount of data, which amplifies the probability of technical difficulties. Moreover, the fact that patients were sleeping during recordings made it impossible to rectify any technical problems.
Approximately 30% of the involved patients were unaccustomed to smartphones and had never used apps and digital devices. Therefore, a caregiver supported them during the study. The mean age of this patients’ group was higher than the entire considered sample. On the contrary, the patients who had decided to download the App on their smartphones were younger. This result confirms the importance of adapting technology to the patient's needs, rather than vice versa. 16
This result emphasizes the key role of the well-known user experience design concepts and user-centered design approaches. 18 As described by Wang et al. 19 in their systemic review, experience is the sum of “interactions influenced by a patient's behavioral determinants, framed by digital technologies and shaped by organizational culture, which influence patient perceptions across the continuum of care that channels digital health.” It has already been highlighted that digital health cannot be equally effective for the whole population. 20 For example, some works show how older adults can benefit from digital health, 21 while others suggest that it is primarily suitable for relatively young patients and in specific situations.20,22
De La Cruz et al. 21 evidenced that it is also essential to understand the reasons why patients choose or not to engage or withdraw from using digital health. Since there is no single answer, Brunton et al. 23 suggest the importance of clear communication between experts, designers, healthcare professionals, and patients to interpret the patient's digital experience correctly. Healthcare professionals should play a more active role in the decision-making process when incorporating digital health into their current service delivery. Questionnaire analysis allowed us to state that patients were overall positively impressed by the service, perceiving it as useful in a period of emergency. Despite the absence of a comparison target, the very high scores reached by questionnaires justify using these data for an initial evaluation of satisfaction related to the provided monitoring services. Specifically, average answers to PSSUQs and satisfaction questionnaires are considered acceptable if higher than the respective threshold of 85% and 70% and guarantee a high usability and positive experience with the O2Ring pulse oximeter.
This result is in contrast with the low score obtained for accessibility: patients probably felt grateful for being monitored during a period of difficulty and fragility, which may have caused them to downplay the issues experienced with the system, resulting in a positive evaluation of the entire teleassistance service. Hence, troubleshooting was perceived by patients as crucial to properly monitoring their health, especially during the pandemic scenario. Consequently, they were more willing to go beyond their technological lack of competence. This phenomenon was previously described for smartwatches24,25 and explains how the health benefits derived from using devices can influence the acceptance of technology.
Although the official intervention of caregivers was 30%, many patients asked for help from a family member even if only occasionally. The need to involve caregivers in performing the required tasks by more than 50% of patients attests to the numerous issues found using the telemonitoring system. This difference represents the portion of caregivers who were able to independently resolve issues, without the need for health professionals’ support. These data demonstrated that many of the technical issues experienced by patients were due to their lack of competence in using smartphones and apps, and thus, this issue could be easily solved by a younger or more tech-savvy person.
Inconclusive recordings could lead patients to use the systems more frequently than necessary, even in the absence of exacerbations or symptoms, causing stress and anxiety instead proving them a sense of safety and monitoring.
New functionalities are not perceived as necessary because they probably might add complexity to the monitoring system, making it more challenging to perform recordings.
Lastly, all the patients expressed satisfaction with the device's ease of use and the system's usefulness. Hence, the O2Ring device was perceived as a comfortable object to wear, even during extended monitoring periods while engaging in physical activity or during sleep.
In the literature, several studies have already investigated patient satisfaction in monitoring. 26 However, the present study offers a novel perspective, including an assessment of the entire care service provided to patients. The proposed approach is not limited to investigating O2Ring™ device usability and experience; it also evaluates the complete patient care and the comprehensive support service associated with the tested monitoring equipment. For this reason, the assistance offered by the case manager plays a crucial role in enhancing the patient experience and usability level, as shown in the results and questionnaires.
The limitations of this study are related to the size of the examined population and the presence of a single recruitment center. To mitigate the difficulties arising from inexperience in using technology, enrolled patients were often younger than the average age of the subjects hospitalized in the facility involved in this study, deemed more suitable for autonomously monitoring and reporting any technical problems. Consequently, the clinical situations and comorbidities of the participants may not fully represent those of the broader patient population that could potentially benefit from this type of service. The study was therefore conducted on a sample that may not be entirely representative of the patient population who could benefit from this type of service. Further randomized studies should be conducted to improve results.
Conclusion
Implementing a SpO2 continuous telemonitoring model within a telemedicine service appears feasible and useful for patients with residual breathing problems, enabling remote monitoring at home and reducing the need for frequent hospital visits when oximetry trends are required. To scale up the service, further improvements in connections, data flow processes, and simplifications, based on patients’ and healthcare operators’ feedback are required.
Regardless of the specific device studied, exploring these topics with the patient is crucial to understand his availability toward new technologies, technological capabilities, etc. Future research is required to evaluate the feasibility of large-scale implementation.
Supplemental Material
Supplemental material, sj-pdf-1-dhj-10.1177_20552076231194547 for Usability of a continuous oxygen saturation device for home telemonitoring by Francesco Bonometti, Palmira Bernocchi, Andrea Vitali, Anna Savoldelli, Caterina Rizzi and Simonetta Scalvini in DIGITAL HEALTH
Acknowledgments
The authors express their gratitude to the nursing staff for their valuable contribution to the project.
Footnotes
Contributorship: FB was involved in the investigation, methodology, validation, and writing—original draft. AV and AS were involved in the methodology, validation, and writing—original draft. CR was involved in the supervision. PB and SS were involved in the conceptualization, supervision, and writing—reviewed editing. All authors read and approved the final version of the manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: All interventions were carried out in accordance with the Declaration of Helsinki, and the study was approved by the ethics committees of the ICS Maugeri on 30 June 2020 (CE2455).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Regione Lombardia, Italy, within the research grant n. RLJ12020012390 – “Bando della DG welfare per il finanziamento di progetti di ricerca in ambito sanitario connessi all’emergenza da COVID-19- DGR XI/3017 del 30.03.2020” – Title: “Supporto MIRATO ai pazienti dimessi dopo un ricovero per infezione da Coronavirus SARS-CoV-2 e comorbidità.”
Guarantor: PB
Informed consent: Written informed consent was obtained from all subjects involved in the study.
ORCID iDs: Palmira Bernocchi https://orcid.org/0000-0003-0875-2007
Andrea Vitali https://orcid.org/0000-0001-9261-4357
Supplemental material: Supplemental material for this article is available online.
References
- 1.World Health Organisation. WHO Coronavirus Disease (COVID-19) Dashboard [Available from: https://covid19.who (last accessed September 2022 2. Characteristics of COVID-19 patients dying in Italy. Report based on available data on October 5th, 2021. Istituto Superiore di Sanità. https://www.epicentro.iss.it/coronavirus/).
- 2.Characteristics of COVID-19 patients dying in Italy. Report based on available data on October 5th, 2021. Istituto Superiore di Sanità. (https://www.epicentro.iss.it/coronavirus/).
- 3.Tabacof L, Wood J, Mohammadi N, et al. Remote patient monitoring identifies the need for triage in patients with acute COVID-19 infection. Telemed J E Health 2022; 28: 495–500. [DOI] [PubMed] [Google Scholar]
- 4.Grasselli G, Zangrillo A, Zanella A, et al. ; for the COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA 2020; 323: 1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keesara S, Jonas A, Schulman K. COVID-19 and health care's digital revolution. N Engl J Med 2020; 382: 82. [DOI] [PubMed] [Google Scholar]
- 6.Quer G, et al. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat Med 2020; 27: 1–5. [DOI] [PubMed] [Google Scholar]
- 7.Joshi M, Ashrafian H, Aufegger L, et al. Wearable sensors to improve detection of patient deterioration. Expert Rev Med Devices 2019; 16: 145–154. [Medline:30580650]. [DOI] [PubMed] [Google Scholar]
- 8.Buekers J, Theunis J, De Boever P, et al. Wearable finger pulse oximetry for continuous oxygen saturation measurements during daily home routines of patients with chronic obstructive pulmonary disease (COPD) over one week: observational study. JMIR Mhealth Uhealth 2019; 7: e12866. PMID: 31199331; PMCID: PMC6594211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downey CL, Chapman S, Randell R, et al. The impact of continuous versus intermittent vital signs monitoring in hospitals: a systematic review and narrative synthesis. Int J Nurs Stud 2018; 84: 19–27. Epub 2018 Apr 21. PMID: 29729558. [DOI] [PubMed] [Google Scholar]
- 10.Scalvini S, Bernocchi P, Zanelli E, et al. ; Maugeri Centre for Telehealth and Telecare (MCTT). Maugeri centre for telehealth and telecare: a real-life integrated experience in chronic patients. J Telemed Telecare 2018; 24: 500–507. Epub 2017 May 24. PMID: 28537509. [DOI] [PubMed] [Google Scholar]
- 11.Bernocchi P, Bonometti F, Serlini M, et al. Telehealth and telecare: a real-life integrated experience in the COVID-19 pandemic. Telemed J E Health 2022; 28: 720–727. [DOI] [PubMed] [Google Scholar]
- 12.Broekhuis M, van Velsen L, Peute L, et al. Conceptualizing usability for the eHealth context: content analysis of usability problems of eHealth applications. JMIR Form Res 2021; 5: e18198. URL: https://formative.jmir.org/2021/7/e18198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis JR. IBM Computer usability satisfaction questionnaires: psychometric evaluation and instructions for use. Int J Human Comput Interact. 1995;7:57–78. [CrossRef] [Google Scholar]. [Google Scholar]
- 14.Savoldelli A, Vitali A, Remuzzi Aet al. et al. Improving the user experience of televisits and telemonitoring for heart failure patients in less than 6 months: a methodological approach. Int J Med Inform 2022; 161: 104717. Epub 2022 Feb 19. PMID: 35259670. [DOI] [PubMed] [Google Scholar]
- 15.Nissen L, Lindhardt T. A qualitative study of COPD-patients’experience of a telemedicine intervention. IJMI 2017; 107: 11–17. [DOI] [PubMed] [Google Scholar]
- 16.Gorst SL, Armitage CJ, Brownsell Set al. et al. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med 2014; 48: 323–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. The law of attrition. JMed Internet Res 2005; 7: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lesselroth B, Monkman H, Adams K, et al. User experience theories, models, and frameworks: a focused review of the healthcare literature. Stud Health Technol Inform 2020; 270: 1076–1080. [DOI] [PubMed] [Google Scholar]
- 19.Wang T, Giunti G, Melles Met al. et al. Digital patient experience: umbrella systematic review. J Med Internet Res 2022; 24: e37952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker RC, Tong A, Howard Ket al. et al. Patient expectations and experiences of remote monitoring for chronic diseases: systematic review and thematic synthesis of qualitative studies. Int J Med Inform 2019; 124: 78–85. [DOI] [PubMed] [Google Scholar]
- 21.De La Cruz Monroy MF, Mosahebi A. The use of smartphone applications (apps) for enhancing communication with surgical patients: a systematic review of the literature. Surg Innov 2019; 26: 244–259. [DOI] [PubMed] [Google Scholar]
- 22.Greenhalgh T, A'Court C, Shaw S. Understanding heart failure; explaining telehealth - a hermeneutic systematic review. BMC Cardiovasc Disord 2017; 17: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brunton L, Bower P, Sanders C. The contradictions of telehealth user experience in chronic obstructive pulmonary disease (COPD): a qualitative meta-synthesis. PLoS One 2015; 10: e0139561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsiao K-L. What drives smartwatch adoption intention? Comparing apple and non-apple watches. Libr Hi Tech 2017; 35: 186–206. 10.1108/LHT-09-2016-0105 . [DOI] [Google Scholar]
- 25.Beukenhorst AL, Howells K, Cook L, et al. Engagement and participant experiences with consumer smartwatches for health research: longitudinal, observational feasibility study. JMIR Mhealth Uhealth 2020; 8: e14368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehraeen E, SeyedAlinaghi S, Heydari M, et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: a systematic review. Health Informatics J 2023; 29: 14604582231167431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dhj-10.1177_20552076231194547 for Usability of a continuous oxygen saturation device for home telemonitoring by Francesco Bonometti, Palmira Bernocchi, Andrea Vitali, Anna Savoldelli, Caterina Rizzi and Simonetta Scalvini in DIGITAL HEALTH