Abstract
Purpose
Anti-viral and anti-inflammatory therapies were effective in altering virus repletion and immune dysregulation in Coronavirus Disease 2019 (COVID-19) patients. This study aimed to explore the effect of combination therapy on disease progression in a real-world setting.
Patients and Methods
A total of 836 patients confirmed with SARS-CoV-2 infection participated in the study from 15 November to 25 December 2022 at Beijing Youan Hospital, Capital Medical University. A prospective cohort study was implemented to investigate the prognostic effect of the combination therapy on virus shedding and clinical recovery.
Results
About 78% of patients used nirmatrelvir/ritonavir (N/R, Paxlovid®, Pfizer) negatively, 16% of patients were prescribed nirmatrelvir/ritonavir beyond five days of symptom onset, 4% of patients received N/R monotherapy within five days of symptom onset and 2% of patients received N/R combined with dexamethasone. Compared with untreated patients, N/R monotherapy reduced the median time to 10.0 days from 12.0 days according to the negative conversion of nucleic acid amplification test (NAAT), and combination therapy reduced the time to 7.0 days, and increased to a 1.99 (95% CI 0.92, 4.32) and 14.23-fold (95% CI 4.50, 44.95) probability of negative NAAT, respectively. N/R monotherapy reduced the clinical recovery time to 10.0 days from 13.0 days. Single-use and combined-use non-significantly increased the recovery probability by 61% and 69%, respectively. In mild and moderate patients, the HRs for clinical recovery increased to 1.69 (95% CI 0.73, 3.94) and 2.18 (95% CI 0.29, 16.62), respectively.
Conclusion
Combination therapy of N/R and dexamethasone increased negative conversion of NAAT and was associated with a non-significant improvement in clinical recovery. Further studies are warranted to confirm this efficacy.
Keywords: N/R, dexamethasone, negative conversion of NAAT, clinical recovery
Introduction
Since the global outbreak of coronavirus disease 2019 (COVID-19), the adverse impact is enormous on both living a normal life and public health. Worldwide, 753.82 million individuals contracted the virus, and 6.81 million died as a result.1 Omicron, as a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variant of concern (VOC), has a stronger spreading ability and is now the dominant strain in China.2–4
Anti-viral agents and immunomodulatory drugs are the main treatments for COVID-19.5 Small molecule inhibitors,6 monoclonal antibodies,7 natural products,8 and traditional treatments9 are useful adjuncts to vaccinations in the clinical treatment of SARS-CoV-2. However, there are no promising medications.10 In this circumstance, combination medication regimens11 are essential in the treatment of SARS-CoV-2 infection. Nirmatrelvir co-packaged with ritonavir (N/R), as an oral novel antiviral agent, was authorized for emergency use in SARS-CoV-2 infection in many countries.12–15 Evidence has shown that N/R could decrease the risk of COVID-19 progression and death in high-risk patients. N/R was reported to reduce the risk of hospitalization or death by 89% in a phase 2/3 EPIC-HR randomized-controlled trial (RCT) in COVID-19 outpatients with high risk of progression.16 In addition, N/R was found to increase the negative conversion of NAAT and decrease the mortality and disease progression of mild/moderate hospitalized COVID-19 patients.17,18
The immune and inflammatory responses and cytokine storms (CS) induced by viral infections are important causes of lung damage, leading to critical illness and death in patients.19 Corticosteroids have anti-inflammatory, immunosuppressive effects and were widely used for severe COVID-19.20 Recently, the controversy over the role of corticosteroids in critically ill patients is ongoing and the combined therapy of N/R and corticosteroids is seldom reported.21–23
This prospective cohort study aimed to investigate the clinical effectiveness of the combined use of N/R and corticosteroids in hospitalized COVID-19 patients.
Materials and Methods
Ethical Approval
All procedures performed in this study involving human participants were approved by the ethical committee of the Beijing Youan Hospital, Capital Medical University (LL-2023-092-K), in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from the included subjects.
Study Setting
Of COVID-19 patients hospitalized in Beijing Youan Hospital, Capital Medical University, 836 were recruited consecutively into the study from 15 November to 25 December 2022. The diagnosis and treatment protocol for COVID-19 patients (tentative version 9) was released by the National Health Commission’s Bureau of Medical Administration. The standards of hospital discharge included more than 3-day normal temperature, remission of respiratory symptoms, improvement of acute lung infiltrates on imaging, and two consecutive (interval of 24 hours at least) NAAT or cycle thresholds (Ct) values of ≥35.
Study Design
This was a prospective cohort study. Based on the N/R treatments, COVID-19 patients were divided into four groups: negative use of N/R, use of N/R beyond 5 days of symptom onset, N/R monotherapy within 5 days of symptom onset, and combination therapy of dexamethasone and N/R within 5 days of symptom onset. The effect on negative NAAT of SARS-CoV-2 and clinical recovery was compared between N/R treatment groups.
Patients
Patients with positive tests of nucleic acid amplification or antigen for SARS-CoV-2 were hospitalized. The onset of signs and symptoms of COVID-19, including fever, cough, sore throat, malaise, fatigue, headache, muscle pain, nausea, vomiting, diarrhea, loss of taste and smell, were collected. The patients were prescribed laboratory tests, including complete blood count, liver and renal function tests. They received anti-viral and symptomatic treatments, recommended by the protocol. The children and pregnant women were excluded from the study.
Variable
N/R treatment groups were defined according to the medical records. The combined use of dexamethasone and N/R was defined as N/R treatment prior to dexamethasone. The severity of illness categories was defined according to the COVID-19 treatment guidelines recommended by the National Institute of Health, including asymptomatic infection, mild illness, moderate illness, severe illness and critical illness, based on a range of clinical manifestations (https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/). The Ct value of real-time reverse-transcription polymerase chain reaction (RT-PCR) from NAAT at hospital admission was selected for further analysis. The diagnosis of comorbidities of COVID-19 included hypertension, diabetes, cancers, chronic liver diseases, chronic kidney diseases, cardio-cerebrovascular diseases, and chronic obstructive pulmonary diseases, collected from the medical records.
Outcome/Endpoints
Negative conversion of NAAT for SARS-CoV-2 was defined as Ct value increasing to ≥35 during the disease course. The median time to negative conversion of NAAT started from the positive test of NAAT or evidence of SARS-CoV-2 antigens.
Patients recovered to discharge standards were defined as being in clinical recovery. Clinical recovery meant more than 3-day normal temperature, remission of respiratory symptoms, improvement of acute lung infiltrates on imaging and two consecutive (interval of 24 hours at least) negative NAAT or a Ct value of ≥35. The median time to clinical recovery started from the symptom onset.
Statistical Analysis
All analyses were conducted by SPSS 23.0 software. Age, Ct value, and clinical classification were analyzed by the Kruskal–Wallis test between the four treatment groups. Gender and comorbidities were analyzed by chi-square test between four treatment groups. Kaplan–Meier curve was used to estimate the median time to negative conversion of NAAT and median time to clinical efficacy, with the log rank test. COX hazard regression model was used to estimate the hazard ratio (HR) and 95% confidence interval (95% CI) for N/R use on the negative conversion of NAAT and clinical efficacy, with adjustments for age, gender, clinical classification of COVID-19, Ct value, and comorbidity diagnosis. Subgroup analysis was conducted among patients with mild/moderate illness. All analyses were two-tailed, with a significance level of 0.05.
Results
Of patients diagnosed with SARS-CoV-2 infection, 836 were recruited into the study. Average age was 60 and male patients accounted for 51% (Table 1). The severity categories included 18% asymptomatic infection, 68% mild/moderate illness and 14% severe/critical illness (Table 1). Of COVID-19 patients, 78% had never used N/R during the disease course, 16% were prescribed N/R beyond five days of symptom onset, 4% patients received N/R within five days of symptom onset and 2% received N/R within five days of symptom onset combined with dexamethasone (Table 1). The admitting Ct value was 27 and the proportion of comorbidities was 43% (Table 1).
Table 1.
Characteristics of Covid-19 Patients
| Clinical Features (n=836) | |
|---|---|
| Age, mean (SD) | 59.7 (22.2) |
| Gender, n (%) | |
| Male | 428 (51.2) |
| Female | 408 (48.8) |
| Clinical classification of COVID-19, n (%) | |
| Asymptomatic infection | 152 (18.2) |
| Mild and moderate illness | 563 (67.6) |
| Severe and critical illness | 118 (14.2) |
| Paxlovid use, n (%) | |
| Negative use | 616 (78.4) |
| Use beyond five days of symptom onset | 124 (15.8) |
| Single use within five days of symptom onset | 33 (4.2) |
| Combining use with dexamethasone within five days of symptom onset | 13 (1.7) |
| Cycle threshold value, mean (SD) | 26.8 (6.7) |
| Comorbidities, n (%) | |
| Yes | 479 (57.3) |
| No | 357 (42.7) |
Patients receiving N/R treatment beyond five days of symptom onset tended to be older (68) and have a higher Ct value (35) than other treatment groups (p<0.001, Table 2). Male patients (29%) were more likely to receive N/R treatment than female patients (14%) (p<0.001, Table 2). Patients with serious severity of illness were more likely to receive N/R treatment, and the proportion of N/R use was 2%, 20% and 58% between asymptomatic, mild/moderate and severe/critical illness groups, respectively (p<0.001, Table 2). Of COVID-19 patients with comorbidities, 29% used N/R compared with 12% of patients without comorbidities (p<0.001, Table 2).
Table 2.
Distribution of Clinical Characteristics Between Paxlovid Treatment Groups
| Negative | Use Beyond Five Days of Symptom Onset | Single Use Within Five Days of Symptom Onset | Combining Use with Dexamethasone Within Five Days of Symptom Onset | p | |
|---|---|---|---|---|---|
| Age*, median (IQR) | 58.0 (33.0) | 68.0 (16.0) | 66.0 (21.0) | 58.0 (39.5) | <0.001 |
| Cycle threshold value*, median (IQR) | 26.2 (10.5) | 35.3 (7.5) | 25.0 (13.6) | 28.9 (19.7) | <0.001 |
| Gender†, n (%) | <0.001 | ||||
| Male | 277 (70.5) | 87 (22.1) | 18 (4.6) | 11 (2.8) | |
| Female | 339 (86.3) | 37 (9.4) | 15 (3.8) | 2 (0.5) | |
| Clinical classification of COVID-19*, n (%) | <0.001 | ||||
| Asymptomatic infection | 141 (97.9) | 2 (1.4) | 1 (0.7) | 0 (0) | |
| Mild and moderate illness | 435 (79.7) | 81 (14.8) | 25 (4.6) | 5 (0.9) | |
| Severe and critical illness | 40 (42.1) | 41 (43.2) | 7 (7.4) | 7 (7.4) | |
| Comorbidities†, n (%) | <0.001 | ||||
| Yes | 307 (70.7) | 93 (21.4) | 22 (5.1) | 12 (2.8) | |
| No | 309 (87.8) | 31 (8.8) | 11 (3.1) | 1 (0.3) |
Notes: *Kruskal–Wallis test, †Chi-square test.
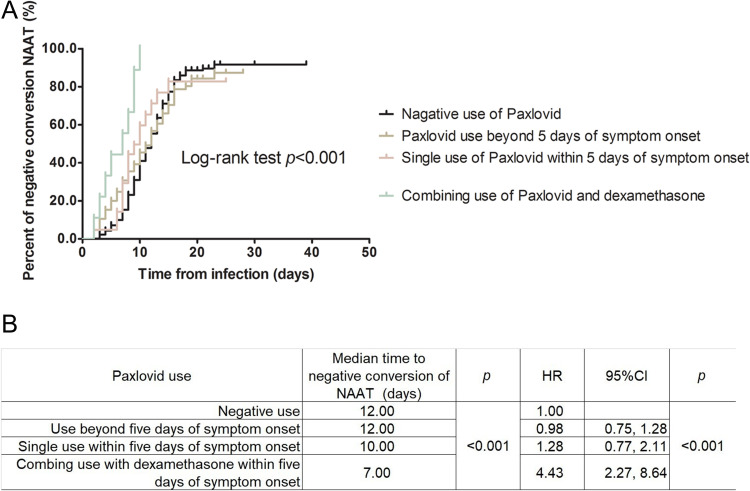
Since symptom onset, the median time of negative conversion of NAAT was 12.0, 12.0, 10.0, and 7.0 days for negative N/R use, N/R use beyond five days of symptom onset, N/R monotherapy within five days of symptom onset, and combined use of dexamethasone and N/R within five days of symptom onset, respectively (Figures 1A and B). The crude HR was 0.98 (95% CI 0.75, 1.28), 1.28 (95% CI 0.77, 2.11) and 4.43 (95% CI 2.27, 8.64), referring to negative N/R use (Figure 1B). With adjustment of confounding factors, combined use of dexamethasone and N/R within five days of symptom onset was associated with an HR of 14.23 (95% CI 4.50, 44.95, Table 3) for negative conversion of NAAT. Among subgroups of mild/moderate illness, N/R monotherapy and combined use of dexamethasone and N/R within five days of symptom onset were associated with a 3.37-fold and 23.94-fold higher probability of negative conversion of NAAT (p<0.001, Table 3), respectively. One-year increase in age was associated with a 1% reduction and one-cycle increase in Ct value was associated with a 6% increase in negative conversion of NAAT (p<0.001, Table 3).
Figure 1.
Survival analysis between Paxlovid use and negative conversion of nucleic acid amplification test. (A) Kaplan-Meier survival curve. (B) Log-rank test and univariate analysis of COX regression..
Table 3.
Multivariate Analysis Between Paxlovid Use and Negative Conversion of NAAT
| HR*adj. | 95% CI | p | HR†adj. | 95% CI | p | |
|---|---|---|---|---|---|---|
| Paxlovid use | <0.001 | <0.001 | ||||
| Negative use | 1.00 | — | 1.00 | — | ||
| Use beyond five days of symptom onset | 1.44 | 0.84, 2.44 | 1.68 | 0.92, 3.06 | ||
| Single use within five days of symptom onset | 1.99 | 0.92, 4.32 | 3.37 | 1.41, 8.06 | ||
| Use within five days of symptom onset plus dexamethasone | 14.23 | 4.50, 44.95 | 23.94 | 4.83, 118.62 | ||
| Age | 0.99 | 0.98, 0.99 | 0.009 | 0.99 | 0.98, 0.99 | 0.029 |
| Gender | 0.553 | 0.809 | ||||
| Female | 1.00 | — | 1.00 | — | ||
| Male | 0.90 | 0.63, 1.28 | 0.95 | 0.62, 1.45 | ||
| Clinical classification of COVID-19 | 0.899 | — | ||||
| Asymptomatic infection | 1.00 | — | ||||
| Mild and moderate illness | 0.93 | 0.60, 1.43 | ||||
| Severe and critical illness | 0.85 | 0.38, 1.91 | ||||
| Cycle threshold value | 1.07 | 1.04, 1.11 | <0.001 | 1.06 | 1.02, 1.10 | 0.002 |
| Comorbidities | 0.059 | 0.085 | ||||
| No | 1.00 | — | 1.00 | — | ||
| Yes | 0.66 | 0.43, 1.02 | 0.66 | 0.41, 1.06 |
Notes: *All subjects, †Subjects with mild and moderate illness.
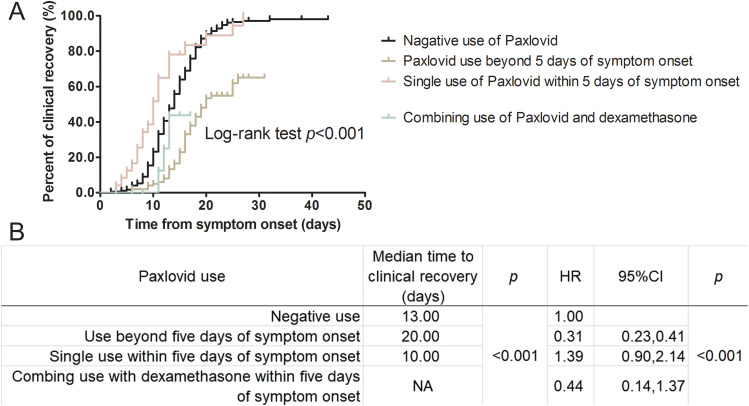
The median times of clinical recovery were 13.0, 20.0 and 10.0 days for negative N/R use, N/R use beyond five days of symptom onset, and single N/R use within five days of symptom onset, respectively (Figures 2A and B). The median recovery time was not achieved among patients receiving combined use of dexamethasone and N/R within five days of symptom onset. Compared with negative N/R use, the crude HR of N/R use beyond five days of symptom onset was 0.31 (95% CI 0.23, 0.41) (Figure 2B). In multivariate analysis, N/R use within five days of symptom onset seemed to improve the probability of clinical recovery, although the significane level was not observed (Table 4). Age and positive comorbidities have a significant association with clinical recovery, one-year increase in age and positive comorbidities associated with a 1% and 44% reduction in recovery probability, respectively (Table 4).
Figure 2.
Survival analysis between Paxlovid use and clinical recovery. (A) Kaplan-Meier survival curve. (B) Log-rank test and univariate analysis of COX regression.
Table 4.
Multivariate Analysis Between Paxlovid Use and Clinical Recovery
| HR*adj. | 95% CI | p | HR†adj. | 95% CI | p | |
|---|---|---|---|---|---|---|
| Paxlovid use | 0.472 | 0.512 | ||||
| Negative use | 1.00 | — | 1.00 | — | ||
| Use beyond five days of symptom onset | 0.85 | 0.48, 1.49 | 0.89 | 0.49, 1.62 | ||
| Single use within five days of symptom onset | 1.61 | 0.75, 3.42 | 1.69 | 0.73, 3.94 | ||
| Combining use with dexamethasone within five days of symptom onset | 1.69 | 0.47, 6.09 | 2.18 | 0.29, 16.62 | ||
| Age | 0.99 | 0.98, 0.99 | 0.037 | 0.99 | 0.98, 0.99 | 0.036 |
| Gender | 0.634 | 0.519 | ||||
| Female | 1.00 | — | 1.00 | — | ||
| Male | 0.92 | 0.64, 1.31 | 0.88 | 0.61, 1.29 | ||
| Clinical classification of COVID-19 | 0.663 | — | ||||
| Mild and moderate illness | 1.00 | — | ||||
| Severe and critical illness | 1.19 | 0.55, 2.55 | ||||
| Cycle threshold value | 0.98 | 0.95, 1.01 | 0.169 | 0.98 | 0.95, 1.01 | 0.173 |
| Comorbidities | 0.005 | 0.009 | ||||
| No | 1.00 | — | 1.00 | — | ||
| Yes | 0.54 | 0.35, 0.83 | 0.56 | 0.36, 0.86 |
Notes: *All subjects, †Subjects with mild and moderate illness.
Discussion
In this prospective cohort study, we demonstrate that combination therapy with N/R and dexamethasone within 5 days of SARS-CoV-2 infection is linked with a more rapid conversion to a negative respiratory SARS-CoV-2 RT-PCR test result, 3 days earlier than N/R monotherapy. In addition, compared to other treatments, single use of N/R within 5 days of symptom onset is associated with the shortest length of clinical recovery. However, single or combination therapy of N/R and dexamethasone did not produce a significant HR of clinical recovery.
N/R consists of nirmatrelvir and ritonavir. Nirmatrelvir, a main protease (Mpro) inhibitor targeting the 3C-like protease of SARS-CoV-2, is effective in reducing the replication of virus. Ritonavir, an inhibitor of cytochrome P450 3A4 (CYP3A4), is used to elevate blood concentrations of nirmatrelvir. The co-administration of two drugs resulted in a prolonged duration of drug effect.24 We observed an accelerating negative conversion of NAAT in hospitalized COVID-19 patients who received N/R; a similar result was reported from a previous study.25 SARS-CoV-2 shedding appeared to peak around the period of symptom onset and patients were most contagious at this period.26–29 Early use of N/R within 5 days of symptom onset can reduce transmission.30 Additionally, N/R could improve the clinical prognosis of mild/moderate hospitalized patients.18 Even among non-hospitalized patients from a phase 2/3 double-blind RCT (EPIC-HR study), N/R treatment was reported to improve the duration and severity of COVID-19.16 N/R treatment could control the transmission of SARS-CoV-2 and improve clinical recovery from COVID-19. In our study, single antivirus therapy did not increase the recovery rate in hospitalized patients, but combined use with dexamethasone was associated with a non-significant increase in clinical recovery, due to the limited sample size. Unlike the EPIC-HR study, our study focused on hospitalized patients and most patients received vaccination. Further studies are necessary to confirm these results.
SARS-CoV-2 infection could induce local/systemic immune responses, exacerbate cytokine storms and result in acute respiratory distress syndrome.31 The inflammatory markers were reported to correlate with the severity and prognosis of COVID-19.32–34 The diagnostic model constructed by C-reactive protein and procalcitonin had highly predictive efficacy for clinical outcomes of COVID-19.35 Immune/inflammatory responses regulated the clinical process of COVID-19 and anti-inflammatory therapy made it possible to modulate the prognosis.
From the clinical course of the asymptomatic incubation period, disease onset with respiratory symptoms, disease progression and severe disease phase, the patients experienced SARS-CoV-2 infection, immune responses, dysregulated inflammation and inflammation-mediated immunopathology.31,36 Anti-viral therapy was inadequate to cure the COVID-19 deterioration process, especially with immunopathology, and should be combined with anti-inflammatory therapy. Anti-viral and anti-inflammatory treatments were proposed to combine to fight against COVID-19.37 Hospitalized COVID-19 patients on dexamethasone and with invasive mechanical ventilation or oxygen, had a reduced risk of 28-day mortality, but not in those without respiratory support.21 Meanwhile, the beneficial effect on 28-day mortality from glucocorticoids was confirmed from a meta-analysis among patients with severe COVID-19.22,38 However, another meta-analysis reported that corticosteroid treatment for MERS-CoV and SARS-CoV infections did not improve clinical prognosis.23 In our study, combined therapy of N/R with dexamethasone improved the negative conversion of NAAT and clinical recovery.
Anti-inflammatory treatments are not recommended for use too early, in case they interfere with immune responses in patients with severe illness.21,22,38 Patients with mild/moderate illness also experienced dysregulated inflammation and cytokine storms and needed anti-inflammatory immunomodulators, ie, glucocorticoids.37 The recommendation of dexamethasone based on the severity of COVID-19 might miss some vulnerable patients. The biomarkers of inflammatory responses are of value to guide anti-inflammatory treatments. In this real-world study, we also found that the systemic inflammatory index was associated with the death from COVID-19, and aimed to explore the predictive factors for anti-inflammatory treatments.
Drug resistance to N/R was discovered in HIV-1 (human immunodeficiency virus-1) and HCV (hepatitis C virus) patients.39 As reported, accumulation of the Mpro mutation might increase drug resistance in vitro, and the resistant genes have been discovered in community isolates. Combination therapy is one of the potential options for reducing the possibility of N/R resistance.24
A limited sample size of combined use of N/R and dexamethasone was the first limitation of this study. This study did not investigate the 28-day mortality of COVID-19.
Conclusion
Early use of N/R could reduce virus shedding of SARS-CoV-2 significantly and, combined with dexamethasone, might improve clinical recovery from COVID-19. For the distinctive variations in immunological and clinical features of emerging SARS-CoV-2 variants in future, the clinical efficacy of anti-viral and immunomodulatory medicines warrants investigation.
Acknowledgments
This study was supported by Mr. Song Guo and Ms. Likun Yang from the Department of Internet, Beijing Youan Hospital, Capital Medical University.
Funding Statement
This study was supported by Beijing Natural Science Foundation (L222120) and High Level Public Health Technical Talents Construction Project from Beijing Municipal Health Commission (2022-2-025). The supporting organizations had no role in study design, data collection, analysis, and interpretation.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
All procedures performed in this study involving human participants were approved by the ethical committee of the Beijing Youan Hospital, Capital Medical University (LL-2023-092-K), in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from the included subjects.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) pandemic; 2023. [PubMed]
- 2.Viana R, Moyo S, Amoako DG, et al. Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in Southern Africa. Nature. 2022;603(7902):679–686. doi: 10.1038/s41586-022-04411-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callaway E, Ledford H. How bad is Omicron? What scientists know so far. Nature. 2021;600(7888):197–199. doi: 10.1038/d41586-021-03614-z [DOI] [PubMed] [Google Scholar]
- 4.Tan Z, Chen Z, Yu A, et al. The first two imported cases of SARS-CoV-2 Omicron variant — Tianjin Municipality, China, December 13, 2021. China CDC Weekly. 2022;4(4):76. doi: 10.46234/ccdcw2021.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Update to living WHO guideline on drugs for covid-19. BMJ. 2022;378:57. [DOI] [PubMed] [Google Scholar]
- 6.Yang L, Wang Z. Bench-to-bedside: innovation of small molecule anti-SARS-CoV-2 drugs in China. Eur J Med Chem. 2023;257:115503. doi: 10.1016/j.ejmech.2023.115503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tuekprakhon A, Nutalai R, Dijokaite-Guraliuc A, et al. Antibody escape of SARS-CoV-2 Omicron BA.4 and BA.5 from vaccine and BA.1 serum. Cell. 2022;185(14):2422–2433. doi: 10.1016/j.cell.2022.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Wang N, Yang L, Song XQ. Bioactive natural products in COVID-19 therapy. Front Pharmacol. 2022;13:926507. doi: 10.3389/fphar.2022.926507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Z, Yang L. Chinese herbal medicine: fighting SARS-CoV-2 infection on all fronts. J Ethnopharmacol. 2021;270:113869. doi: 10.1016/j.jep.2021.113869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Z, Yang L, Song XQ. Oral GS-441524 derivatives: next-generation inhibitors of SARS-CoV-2 RNA-dependent RNA polymerase. Front Immunol. 2022;13:1015355. doi: 10.3389/fimmu.2022.1015355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang L, Wang Z. Natural products, alone or in combination with FDA-approved drugs, to treat COVID-19 and lung cancer. Biomedicines. 2021;9(6):689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NMPA. National Medical Products Administration of China. Emergency conditional approval of Pfizer’s COVID-19 therapy: nirmatrelvir tablet/ritonavir tablet combination package importation registration; 2022.
- 13.EMA. COVID-19: EMA recommends conditional marketing authorisation for Paxlovid; 2022.
- 14.FDA. Emergency use authorization 105; 2021.
- 15.FDA. Fact sheet for healthcare providers: emergency authorization for Paxlovid; 2022.
- 16.Hammond J, Leister-Tebbe H, Gardner A, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N Engl J Med. 2022;386(15):1397–1408. doi: 10.1056/NEJMoa2118542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li H, Gao M, You H, et al. Association of nirmatrelvir/ritonavir treatment on upper respiratory SARS-CoV-2 RT-PCR negative conversion rates among high-risk patients with COVID-19. Clin Infect Dis. 2022;2022:ciac600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong C, Au I, Lau K, Lau E, Cowling BJ, Leung GM. Real-world effectiveness of early molnupiravir or nirmatrelvir-ritonavir in hospitalised patients with COVID-19 without supplemental oxygen requirement on admission during Hong Kong’s omicron BA.2 wave: a retrospective cohort study. Lancet Infect Dis. 2022;22(12):1681–1693. doi: 10.1016/S1473-3099(22)00507-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the “Cytokine Storm” in COVID-19. J Infect. 2020;80(6):607–613. doi: 10.1016/j.jinf.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20(5):269–270. doi: 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Horby P, Lim WS, Emberson JR, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne J, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324(13):1330–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li H, Chen C, Hu F, et al. Impact of corticosteroid therapy on outcomes of persons with SARS-CoV-2, SARS-CoV, or MERS-CoV infection: a systematic review and meta-analysis. Leukemia. 2020;34(6):1503–1511. doi: 10.1038/s41375-020-0848-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Focosi D, McConnell S, Shoham S, Casadevall A, Maggi F, Antonelli G. Nirmatrelvir and COVID-19: development, pharmacokinetics, clinical efficacy, resistance, relapse, and pharmacoeconomics. Int J Antimicrob Agents. 2023;61(2):106708. doi: 10.1016/j.ijantimicag.2022.106708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li H, Gao M, You H, et al. Association of Nirmatrelvir/Ritonavir treatment on upper respiratory Severe Acute Respiratory Syndrome Coronavirus 2 Reverse Transcription-Polymerase Chain Reaction (SARS-Cov-2 RT-PCR) negative conversion rates among high-risk patients with Coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2023;76(3):e148–e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wölfel R, Corman VM, Guggemos W, et al. Author correction: virological assessment of hospitalized patients with COVID-2019. Nature. 2020;588(7839):E35. doi: 10.1038/s41586-020-2984-3 [DOI] [PubMed] [Google Scholar]
- 27.Zhou R, Li F, Chen F, et al. Viral dynamics in asymptomatic patients with COVID-19. Int J Infect Dis. 2020;96:288–290. doi: 10.1016/j.ijid.2020.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He X, Lau EHY, Wu P, et al. Author correction: temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(9):1491–1493. doi: 10.1038/s41591-020-1016-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ge Y, Martinez L, Sun S, et al. COVID-19 transmission dynamics among close contacts of index patients with COVID-19: a population-based cohort study in Zhejiang Province, China. JAMA Intern Med. 2021;181(10):1343–1350. doi: 10.1001/jamainternmed.2021.4686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marc A, Kerioui M, Blanquart F, et al. Quantifying the relationship between SARS-CoV-2 viral load and infectiousness. eLife. 2021;10. doi: 10.7554/eLife.69302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu BM, Martins TB, Peterson LK, Hill HR. Clinical significance of measuring serum cytokine levels as inflammatory biomarkers in adult and pediatric COVID-19 cases: a review. Cytokine. 2021;142:155478. doi: 10.1016/j.cyto.2021.155478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Darmadi D, Pakpahan C, Ruslie RH, Rezano A. Inflammatory laboratory findings associated with severe illness among hospitalized individuals with COVID-19 in Medan, Indonesia: a cross-sectional study. F1000Res. 2021;10:1246. doi: 10.12688/f1000research.74758.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaushal K, Kaur H, Sarma P, et al. Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis. J Crit Care. 2022;67:172–181. doi: 10.1016/j.jcrc.2021.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rokni M, Ahmadikia K, Asghari S, Mashaei S, Hassanali F. Comparison of clinical, para-clinical and laboratory findings in survived and deceased patients with COVID-19: diagnostic role of inflammatory indications in determining the severity of illness. BMC Infect Dis. 2020;20(1):869. doi: 10.1186/s12879-020-05540-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hariyanto TI, Japar KV, Kwenandar F, et al. Inflammatory and hematologic markers as predictors of severe outcomes in COVID-19 infection: a systematic review and meta-analysis. Am J Emerg Med. 2021;41:110–119. doi: 10.1016/j.ajem.2020.12.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghosh P, Nagaraja S, Basavaraju S, Kesavardhana S. Dysregulated innate immune and inflammatory responses in SARS-CoV-2 infection and COVID-19 severity. Crit Rev Immunol. 2021;41(3):43. doi: 10.1615/CritRevImmunol.2021039716 [DOI] [PubMed] [Google Scholar]
- 37.Feuillet V, Canard B, Trautmann A. Combining antivirals and immunomodulators to fight COVID-19. Trends Immunol. 2021;42(1):31–44. doi: 10.1016/j.it.2020.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Siemieniuk RA, Bartoszko JJ, Zeraatkar D, et al. Drug treatments for covid-19: living systematic review and network meta-analysis. BMJ. 2020;370:m2980. doi: 10.1136/bmj.m2980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Motyan JA, Mahdi M, Hoffka G, Tozser J. Potential resistance of SARS-CoV-2 Main Protease (Mpro) against protease inhibitors: lessons learned from HIV-1 protease. Int J Mol Sci. 2022;23(7). doi: 10.3390/ijms23073507 [DOI] [PMC free article] [PubMed] [Google Scholar]