Scapular fractures comprise 3% of all fractures, and only 9% of these involve the acromion.4,6,24 Although the majority of acromial fractures occur traumatically, acromial stress fractures have been reported in cases involving reverse total shoulder arthroplasty,32 cuff tear arthropathy (CTA),3 sport activity,8,27,29,31 and manual wheelchair use.1 We describe a case of a stress-insufficiency acromial fracture in a weight-bearing shoulder of a 70-year-old female with Parkinson’s disease (PD) and osteoporosis who has required long-term use of a cane for ambulation. Our aim is to raise awareness of this potential but rare injury in mobility device users (MDUs) who progress to dependency of their upper extremities as weight-bearing limbs.
The patient was informed that information regarding her case would be submitted for publication and provided consent.
Case report
A 70-year-old right hand–dominant female presented with 6 days of atraumatic right shoulder pain. The pain was described as a nonradiating, constant ache that worsened with use of the right upper extremity. She denied recent fall, previous rotator cuff tear (RCT), prior shoulder surgery, or history of insufficiency fracture. Medical history includes osteoporosis diagnosed in 2013, midstage PD, characterized by disruption of balance, bradykinesia, and minimal functional dependence, as well as thoracic kyphoscoliosis. The patient has relied on cane use with her right hand for the past several years and therefore depends on her upper extremity for weight-bearing with ambulation. She is able to perform activities of daily living (ADLs) independently. Daily medications include rasagiline, carbidopa/levodopa, and pramipexole for PD and calcium and vitamin D supplementation for osteoporosis. Of note, she received an annual infusion of zoledronic acid for a 3-year duration, with the last dose given approximately one year before injury.
On physical examination, no swelling, open wounds, ecchymosis, or other signs of recent trauma were present about the right shoulder. Palpation at the posterior aspect of the acromion evoked acute pain. Active and passive forward flexion and abduction of the right shoulder to 90 degrees was achieved and limited by pain. Active external rotation of the shoulder to 50 degrees was present with the arm in the adducted position. Internal rotation, shoulder strength, and provocative examination maneuvers that test for rotator cuff, acromioclavicular joint, or shoulder impingement pathology could not be assessed secondary to severe pain. She maintained full range of motion of the contralateral shoulder. A resting tremor of the hands, cogwheel rigidity of the upper extremities, and truncal stiffness were present. She had a stooped, right-sided posture and relied on her cane to overcome imbalance with standing and walking (Fig. 1). A shuffling gait was noticed, as was slowness with purposeful activity.
Figure 1.

Clinical photo documentation. Upright stance of our patient demonstrates right-sided posturing and dependent weight-bearing of the right upper extremity.
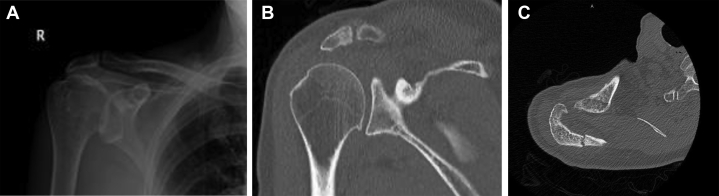
Standard radiographs revealed a nondisplaced fracture in the posterior aspect of the right acromion and slight narrowing of the acromial-humeral interval (Fig. 2, A).
Figure 2.
Radiologic imaging on the first consultation. (A) Anteroposterior radiograph of the right shoulder shows a slightly high-riding humeral head, mild glenohumeral arthritis, and an Ogawa type IIB acromion fracture. (B) Coronal and (C) axial CT shows a nondisplaced fracture at the posterior aspect of the acromion without the presence of pathologic lesions or evidence of fatty infiltration of the rotator cuff muscles. CT, computerized tomography.
The fracture line is located medial to the acromial angle and in the extremely lateral scapular spine and is therefore classified as a type IIB according to the Ogawa acromion fracture classification.20 Computerized tomography (CT) revealed no evidence of pathologic lesions at the fracture site or fatty infiltration within the rotator cuff muscles (Fig. 2, B and C). She was treated in a sling with gradual mobilization and was instructed to remain non-weight-bearing for 6 weeks. Her plan was to use the contralateral arm for use of her cane.
By 6 weeks, she had no pain at rest and only minimal pain with movement of the right shoulder. Active and passive forward flexions were 110 and 150 degrees, respectively. Abduction was 90 degrees. External rotation was 65 degrees and internal rotation was 20 degrees but still limited by pain. She admitted to poor compliance with non-weight-bearing protocol. Radiographs showed callus formation without fracture displacement (Fig. 3). She began physical therapy with focus on active range of motion and isometric shoulder strengthening.
Figure 3.
Radiographic imaging at 6-week follow-up. Anteroposterior radiograph shows significant bony callus formation at the fracture site.
By 3 months, she experienced full painless range of motion and strength. There was no point tenderness over the fracture site. Radiographs showed significant callus formation without fracture union (Fig. 4). By 6 months, she remained symptom-free with full return of baseline function. Radiographs revealed a hypertrophic nonunion (Fig. 5). Her clinical status remained consistent at 12-month follow-up.
Figure 4.
Radiographic imaging at 3-month follow-up. Anteroposterior radiograph shows a nonunited fracture with surrounding bony callus.
Figure 5.

Radiographic imaging at 6-month follow-up. Anteroposterior radiograph shows hypertrophic nonunion.
Discussion
PD is a progressive neuromuscular disease that leads to significant motor impairment and functional decline. Motor symptoms include shaking, rigidity, slowness of movement, postural instability, and gait imbalance.21 Symptoms worsen overtime and necessitate the use of mobility assistance devices, such as canes, wheeled walkers, manual wheelchairs, and motorized devices, based on one’s functional status.10
The shoulder is a common site of upper extremity pain in MDUs, with incidence 15%-50% greater than in able-bodied counterparts.23 Overtime, persistent load through the glenohumeral joint results in injury. Common diagnoses to consider in a painful weight-bearing shoulder include subacromial impingement syndrome, RCT, biceps tendinopathy, acromioclavicular arthrosis, glenohumeral arthritis, and osteonecrosis of the humeral head.23
Acromial stress fracture in MDUs is extremely rare. Only one case has been reported previously in a 22-year-old wheelchair-bound patient with Charcot-Marie-Tooth disease.1 She presented with 4 years of gradually worsening shoulder pain and was found to have a nonunited fracture of the anterior acromion. A superiorly closing wedge osteotomy with cancellous lag screw fixation was performed with successful outcomes at 6-month follow-up. Conversely, our patient presented acutely with 6 days of shoulder pain, leading to early conservative treatment measures which proved successful. Early diagnosis and treatment with restriction of causative activity may limit progression to fracture displacement or symptomatic nonunion, thereby bypassing the need for surgical fixation.26 Therefore, acromial stress fracture should be considered in the differential diagnosis of young or elderly MDUs who present with acute or insidious pain of the weight-bearing shoulder in the absence of trauma. Plain radiographs, CT scan, magnetic resonance imaging, and ultrasound have all been utilized successfully for the diagnosis.13,23,27
A common mechanism underlying the development of acromial stress fracture involves repetitive microtrauma during glenohumeral joint loading. This is common in cases of CTA, where compromise of static glenohumeral stabilization leads to superior migration of the humeral head. Overtime, repeated contact with the undersurface of the anterior and lateral acromion may lead to thinning and fracture.3
Although our patient’s initial radiographs revealed a slight decrease in the acromial-humeral interval, her clinical history was unsuggestive of a complete RCT. However, a partial degenerative RCT within the critical impingement zone of the supraspinatus tendon is possible. This region is relatively avascular and is most susceptible to injury during axial load with the arm extended,19 which occurs during cane strike. However, our patient’s fracture was located at the posterior aspect of the acromion. Therefore, repetitive microtrauma leading to a stress-fatigue fracture is an unlikely mechanism of injury in our patient. The force vector produced during cane strike—as the arm is outstretched and held in slight flexion—is directed toward the posterior aspect of the acromion and may have contributed to stress fracture in this region. However, our patient’s postural deformity likely alters the typical force vector imparted on the weight-bearing shoulder of a cane walker with normal spinal alignment. Thus, additional contributors to injury should be considered. In a published case report, a manual wheelchair user sustained fracture of the anterior acromion1 as a likely result of muscular imbalance. The ratio of abduction-to-adduction strength has been shown to be greater in this population, resulting in humeral head elevation and microtrauma to the anterior acromion.2
A number of recent studies have identified patient risk factors for the development of acromial stress fracture after reverse total shoulder arthroplasty (RTSA).18,22,32 Interestingly, osteoporosis and female sex were found to be patient-specific risk factors for acromial stress fracture independent of RTSA.18,22,32 Acromial stress fractures after RTSA are thought to occur as a result of altered mechanics about the shoulder as the deltoid and trapezium exert greater force on the acromion during movement to compensate for the lack of a rotator cuff.25 Although our patient did not undergo RTSA, her sex, history of osteoporosis, and persistent joint loading secondary to chronic cane use are the most likely clinical factors that led to her stress-insufficiency acromial fracture.
It is worth mentioning that our patient received an annual infusion of zoledronic acid for a 3-year duration, with the last dose given approximately one year before injury. This drug is a potent bisphosphonate that decreases bone turnover and increases bone mineral density in patients with postmenopausal osteoporosis.14 While bisphosphonates have been shown to reduce the risk of vertebral, nonspine, and hip fracture in this population,14 long-term therapy (3-10 years) is associated with stress fracture of the proximal femur.30 One case of acromial stress fracture secondary to bisphosphonate use has been reported.9 The patient was a 69-year-old female with a 10-year history of daily alendronate use who sustained an atraumatic fracture of the acromial base while showering. The medication was discontinued, resulting in symptom resolution 3 months later. At 1 year follow-up, she remained pain-free with full shoulder mobility. Therefore, our patient’s 3-year history of bisphosphonate use may have contributed to the development of her acromial stress fracture.
There is growing evidence to support the association of PD with osteoporosis.16 Several synergistic factors contribute to bone loss in PD, including immobility, decreased muscle strength, and low body weight.28 It has been speculated that hypokinesia in affected patients leads to bone loss as a result of diminished mechanical stimuli.7 In addition, deficiencies in 1α,25-dihytroxyvitamin D3 and vitamin K are often present in this population, which impedes bone remodeling.7 Hyperhomocysteinemia is prevalent in PD and serves as an independent risk factor for fracture and low bone mineral density.28 Aside from folate and B12 deficiency, a common cause for elevated levels of homocysteine in PD patients is levadopa7,28—the gold-standard treatment for PD and a medication used by our patient. Supplementation of B12 and folic acid have been shown to decrease homocysteine levels in levadopa-treated patients and may be considered as a useful adjunct to anti-osteoporotic medication in patients with PD.12 Therefore, our patient’s history of PD along with daily levodopa treatment are possible contributors to her diminished bone quality and stress-insufficiency fracture.
Nonsurgical management with an initial period of immobilization and gradual return to motion is the mainstay of treatment for acromial stress fractures.11 Compared with able-bodied counterparts, the rehabilitation course is more complex for those who rely on the limb for ambulation and balance.22 While primary surgical intervention may afford these patients with greater preservation of ADLs over the long term and decrease the risk of fracture displacement or nonunion, operative risk and extended postoperative dependence should not be ignored. However, lack of adherence to non-weight-bearing precautions leading to complication and the need for future surgery must also be considered. Perhaps further research regarding joint-sparing transfer,5 postural correction,5 and targeted shoulder muscle strengthening15,17 may aid in the prevention and treatment of acromial stress fracture in this particular patient population.
Conclusion
Acromial stress-insufficiency fracture is a rare injury with a multifactorial etiology and should be considered in the differential diagnosis of a painful weight-bearing shoulder in elderly mobility device users with osteoporosis. Furthermore, our case underscores potential associations between acromial stress-insufficiency fracture and PD, certain medications (ie, bisphosphonates and levodopa), thoracic kyphosis, and cane dependency.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional review board approval was not required for this case report.
References
- 1.Aujla R.S., Gulihar A., Taylor G.J. Acromial stress fracture in a young wheelchair user with Charcot-Marie-Tooth disease: a case report. Cases J. 2008;1:359. doi: 10.1186/1757-1626-1-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burnham R.S., May L., Nelson E., Steadward R., Reid D.C. Shoulder pain in wheelchair athletes: The role of muscle imbalance. Am J Sports Med. 1993;21:238–242. doi: 10.1177/036354659302100213. [DOI] [PubMed] [Google Scholar]
- 3.Dennis D.A., Ferlic D.C., Clayton M.L. Acromial stress fractures associated with cuff-tear arthropathy. A report of three cases. J Bone Joint Surg Am. 1986;68:937–940. [PubMed] [Google Scholar]
- 4.Egol K.A., Koval K.J., Zuckerman J.D. 2019. Handbook of Fractures. Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA. ISBN: 9781605477602. [Google Scholar]
- 5.Fattal C., Coulet B., Gelis A., Rouays-Mabit H., Verollet C., Mauri C., Ducros J.L., Teissier J. Rotator cuff surgery in persons with spinal cord injury: relevance of a multidisciplinary approach. J Shoulder Elbow Surg. 2014;23:1263–1271. doi: 10.1016/j.jse.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Goodrich J.A., Crosland E., Pye J. Acromion fracture associated with posterior shoulder dislocation. J Orthop Trauma. 1998;12:521–523. doi: 10.1097/00005131-199809000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Handa K., Kiyohara S., Yamakawa T., Ishikawa K., Hosonuma M., Sakai N., Negishi-Koga T. Bone loss caused by dopaminergic degeneration and levodopa treatment in Parkinson’s disease model mice. Sci Rep. 2019;9:13768. doi: 10.1038/s41598-019-50336-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall R.J., Calvert P.T. Stress fracture of the acromion: an unusual mechanism and review of the literature. J Bone Joint Surg Br. 1995;77:153–154. [PubMed] [Google Scholar]
- 9.Haque S., Pandey R. Case report of bisphosphonate-associated atypical scapular fracture and brief literature review. Int J Shoulder Surg. 2016;10:92–93. doi: 10.4103/0973-6042.180723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kader M., Jonasson S.B., Iwarsson S., Odin P., Nilsson M.H. Mobility device use in people with Parkinson's disease: A 3-year follow-up study. Acta Neurol Scand. 2018;138:70–77. doi: 10.1111/ane.12942. [DOI] [PubMed] [Google Scholar]
- 11.Kuhn J., Blasier R., Carpenter J. Fractures of the Acromion Process: A Proposed Classification System. J Orthop Trauma. 1994;8:6–13. doi: 10.1097/00005131-199402000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Lamberti P., Zoccolella S., Armenise E., Lamberti S., Fraddosio A., de Mari M. Hyperhomocysteinemia in L-dopa treated Parkinson's disease patients: effect of cobalamin and folate administration. Eur J Neurol. 2005;12:365–368. doi: 10.1111/j.1468-1331.2004.00973.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee C.H., Choi Y.A., Lee S.U. Ultrasonographic Diagnosis of Non-displaced Avulsion Fracture of the Acromion: A Case Report. Ann Rehabil Med. 2015;39:473–476. doi: 10.5535/arm.2015.39.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liberman U.A., Weiss S.R., Bröll J., Minne H.W., Quan H., Bell N.H., Rodriguez-Portales J., Downs R.W., Jr., Dequeker J., Favus M. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med. 1995;333:1437–1443. doi: 10.1056/NEJM199511303332201. [DOI] [PubMed] [Google Scholar]
- 15.Ludewig P.M., Cook T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 16.Malochet-Guinamand S., Durif F., Thomas T. Parkinson's disease: A risk factor for osteoporosis. Joint Bone Spine. 2015;82:406–410. doi: 10.1016/j.jbspin.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Morrow M.M., Kaufman K.R., An K.N. Scapula kinematics and associated impingement risk in manual wheelchair users during propulsion and a weight relief lift. Clin Biomech (Bristol, Avon) 2011;26:352–357. doi: 10.1016/j.clinbiomech.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moverman M.A., Menendez M.E., Mahendraraj K.A., Polisetty T., Jawa A., Levy J.C. Patient risk factors for acromial stress fractures after reverse shoulder arthroplasty: a multicenter study. J Shoulder Elbow Surg. 2021;30:1619–1625. doi: 10.1016/j.jse.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Neer C.S., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 20.Ogawa K., Naniwa T. Fractures of the acromion and the lateral scapular spine. J Shoulder Elbow Surg. 1997;6:544–548. doi: 10.1016/s1058-2746(97)90087-2. [DOI] [PubMed] [Google Scholar]
- 21.Opara J., Małecki A., Małecka E., Socha T. Motor assessment in Parkinson`s disease. Ann Agric Environ Med. 2017;24:411–415. doi: 10.5604/12321966.1232774. [DOI] [PubMed] [Google Scholar]
- 22.Otto R.J., Virani N.A., Levy J.C., Nigro P.T., Cuff D.J., Frankle M.A. Scapular fractures after 371 reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed 372 classification. J Shoulder Elbow Surg. 2013;22:1514–1521. doi: 10.1016/j.jse.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Patel R.M., Gelber J.D., Schickendantz M.S. The Weight-Bearing Shoulder. J Am Acad Orthop Surg. 2018;26:3–13. doi: 10.5435/jaaos-d-15-00598. [DOI] [PubMed] [Google Scholar]
- 24.Rockwood C.A., Bucholz R.W., Court-Brown C.M., Heckman J.D., Tornetta P. 2010. Rockwood and Green's Fractures in Adults. Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA. ISBN: 9781605476773. [Google Scholar]
- 25.Shindle M.K., Wanich T., Pearle A.D., Warren R.F. Atraumatic scapular fractures in the setting of chronic rotator cuff tear arthropathy: a report of two cases. J Shoulder Elbow Surg. 2008;17:e4–e8. doi: 10.1016/j.jse.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 26.Tagliapietra J., Fantoni I., Taglialavoro G., Angelini A., Berizzi A., Belluzzi E., Pozzuoli A., Ruggieri P. Symptomatic pseudoarthrosis secondary to a stress fracture of the acromion. Acta Biomed. 2019;90:603–605. doi: 10.23750/abm.v90i4.7778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taneja A.K., Negromonte F.P., Skaf A. Stress injury of the acromion: case report and literature review. Eur J Orthop Surg Traumatol. 2013;23:S189–S192. doi: 10.1007/s00590-013-1181-6. [DOI] [PubMed] [Google Scholar]
- 28.Van den Bos F., Speelman A., Samson M., Munneke M., Bloem B., Verhaar H. Parkinson’s disease and osteoporosis. Age Ageing. 2009;42:156–162. doi: 10.1093/ageing/afs161. [DOI] [PubMed] [Google Scholar]
- 29.Ward W.G., Sr., Carter C.J., Wilson S.C., Emory C.L. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res. 2012;470:759–765. doi: 10.1007/s11999-011-2194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ward W.G., Bergfeld J.A., Carson W.G., Jr. Stress fracture of the base of the acromial process. Am J Sports Med. 1994;22:146–147. doi: 10.1177/036354659402200123. [DOI] [PubMed] [Google Scholar]
- 31.Warner J.J., Port J. Stress fracture of the acromion. J Shoulder Elbow Surg. 1994;3:262–265. doi: 10.1016/S1058-2746(09)80045-1. [DOI] [PubMed] [Google Scholar]
- 32.Zmistowski B., Gutman M., Horvath Y., Abboud J.A., Williams G.R., Jr., Namdari S. Acromial stress fracture following reverse total shoulder arthroplasty: incidence and predictors. J Shoulder Elbow Surg. 2020;29:799–806. doi: 10.1016/j.jse.2019.08.004. [DOI] [PubMed] [Google Scholar]